Abstract
In view of advances in early detection and treatment, the 5-year relative survival rate for all cancer patients combined is now approximately 66%. As a result, there are more than 13.7 million cancer survivors in the United States, with this number increasing by 2% annually. For many patients, improvements in survival have been countered by therapy-associated adverse effects that may seriously impair long-term functional status, workplace productivity, and quality of life. Approximately 20% to 40% of cancer patients given neurotoxic chemotherapy develop chemotherapy-induced peripheral neurotoxicity (CIPN), which represents one of the most common and potentially permanent nonhematologic side effects of chemotherapy. Permanent bilateral hearing loss and/or tinnitus can result from several ototoxic therapies, including cisplatin- or carboplatin-based chemotherapy. CIPN and ototoxicity represent important challenges because of the lack of means for effective prevention, mitigation, or a priori identification of high-risk patients, and few studies have applied modern genomic approaches to understand underlying mechanisms/pathways. Translational genomics, including cell-based models, now offer opportunities to make inroads for the first time to develop preventive and interventional strategies for CIPN, ototoxicity, and other treatment-related complications. This commentary provides current perspective on a successful research strategy, with a focus on cisplatin, developed by an experienced, transdisciplinary group of researchers and clinicians, representing pharmacogenomics, statistical genetics, neurology, hearing science, medical oncology, epidemiology, and cancer survivorship. Principles outlined herein are applicable to the construction of research programs in translational genomics with strong clinical relevance and highlight unprecedented opportunities to understand, prevent, and treat long-term treatment-related morbidities.
In view of advances in early detection, supportive care, and treatment, the 5-year relative survival rate for all cancer patients combined is now approximately 66% (1). As a result, there are more than 13.7 million cancer survivors, comprising approximately 4% of the United States population (2), with this number expected to increase by 2% annually (3). For many patients, these marked improvements in survival have been countered by serious therapy-associated adverse effects. These include sequelae that not only may be fatal [eg, second malignant neoplasms (4)] but also those that may impair long-term functional status, workplace productivity, and quality of life such as chemotherapy-induced peripheral neurotoxicity (CIPN) and permanent bilateral hearing loss (5).
CIPN is one of the most common and potentially permanent side effects of modern chemotherapy, second only in frequency to hematopoietic toxicity (6). Approximately 20% to 40% of cancer patients treated with neurotoxic chemotherapy develop CIPN (7). For painful neuropathies, most drugs fall short of providing adequate relief (7,8). CIPN represents an important challenge because of the lack of treatment that can effectively prevent or mitigate this adverse drug effect (9,10). Management is further complicated by the lack of reliable means to identify at-risk patients. CIPN may develop as a consequence of treatment with platinum analogs (cisplatin, oxaliplatin, carboplatin), taxanes (paclitaxel, docetaxel), vinca alkaloids (vincristine), thalidomide, epothilones, and bortezomib (10). Differences in structural and mechanistic properties between various chemotherapeutic agents contribute to variations in clinical presentation (11). Mechanisms underlying CIPN remain largely unclear (11) and include damage to neuronal cell bodies in the dorsal root ganglion and axonal toxicity through transport deficits or energy failure [reviewed in (10)]. Whereas CIPN may be reversible for some cytotoxic drugs (eg, taxanes), for other chemotherapeutic agents (eg, cisplatin), the persistence of CIPN in long-term cancer survivors is well-documented (12–14). In a recent review of CIPN (10), incidence rates also varied greatly between studies. These wide ranges likely reflect not only differences in study populations, drug-related factors (eg, dose intensity), and potential confounders but also genetic susceptibility (15). CIPN associated with all major groups of neurotoxic drugs was recently reviewed by Argyriou et al. (10).
Hearing loss can result from the use of several potentially ototoxic therapies used in cancer treatment, including cisplatin- or carboplatin-based chemotherapy and cranial radiotherapy (16). Cisplatin results in serious, permanent, bilateral sensorineural hearing loss in 19% to 77% of patients, with 19% to 42% developing permanent tinnitus (13). Cisplatin is one of the most ototoxic drugs in clinical use and is estimated by Mukherjea et al. (17) to result in hearing loss in approximately half a million new US cancer patients each year. Cisplatin-induced hearing loss is especially detrimental in children because even minor compromises in hearing can adversely impact academic and social development (18). Achievement of low blood concentrations of cisplatin several hours after infusion through intense intravenous hydration can minimize ototoxicity, but to our knowledge no drugs have been approved by the US Food and Drug Administration to prevent cisplatin ototoxicity during curative cancer treatment (19,20). Amifostine initially showed encouraging results for ovarian cancer (21) but was not found to lessen the risk of hearing loss in pediatric studies (22,23). A recent Cochrane analysis (24) of possible medical interventions for the prevention of platinum-induced hearing loss in children with cancer also found no evidence of an effect for amifostine, but methodologic limitations of the reviewed studies were noted.
Although inroads have been made into the description of risk factors for CIPN and iatrogenic hearing loss, few studies have applied modern genomic approaches (25) to further our understanding of associated genetic variants and underlying mechanisms. An in-depth understanding of pathways for CIPN and ototoxicity could provide the basis for the development of preventive and interventional strategies (5). The purpose of this commentary is to provide perspective on an approach intended to facilitate a comprehensive understanding of molecular pathways for CIPN and ototoxicity in cancer survivors. The current perspective represents 4 years of thoughtful deliberations, meetings, and discussions by an interdisciplinary group of experts in neurology, hearing science, pharmacogenomics, statistical genetics, medical oncology, radiation oncology, epidemiology, and survivorship research. This comprehensive approach was recently highlighted as one model for translational research at a National Cancer Institute–sponsored workshop (5) and is described here to foster the development of other programs in translational genomics with strong clinical relevance for cancer survivors. We review our rationale for the choice of cisplatin as a prototype drug to drive forward translational genomic research in CIPN and iatrogenic ototoxicity, summarize recent research progress in these areas to date, describe epidemiologic and genomic approaches, and highlight opportunities for the cross-validation of results using preclinical cell-based model systems.
Methodologic Considerations in Translational Genomics
Translational genomics in cancer survivorship relies on the integration of classic epidemiologic study design [reviewed in (26)] with modern genomic technologies. Investigations of CIPN and drug-induced ototoxicity also invoke principles used in traditional pharmacogenomic studies, such as uniformity of drug exposure (27). For these studies, typically germline DNA is collected for phenotyped patients given a specified drug regimen. Genetic variation is then compared between patients who do and do not develop the toxicity. The achievement of inroads into understanding genetic mechanisms for treatment-related morbidities in cancer survivors builds on this model and adapts it to considerably more complex environments, with various considerations described below.
Selection of Cytotoxic Drug to Study
Of chemotherapeutic agents in use today, to our knowledge only cisplatin is associated with both CIPN and permanent bilateral sensorineural hearing loss. Cisplatin also causes irreversible tinnitus. A heavy metal, cisplatin provides the prototype drug for a class of compounds known as the platinating agents. Cisplatin was first introduced into clinical oncology in 1977 (28), but the remarkable ability of cytotoxic drugs such as this to cure patients with selected disseminated cancers remains featured on the National Cancer Institute’s List of Provocative Questions (29). Overall, platinum compounds now represent one of the most widely used and successful groups of cytotoxic drugs worldwide. Each year more than 5.8 million patients worldwide are diagnosed with cancers (colon, rectum, cervix, endometrium, bladder, stomach, head and neck, lung, esophagus, pancreas, osteosarcoma, ovary, testis) for which first-line therapy potentially includes platinating agents (30,31). Platinum now also shows promise for triple-negative breast cancer (32–35). In view of their effectiveness, platinum compounds, predominantly cisplatin, are used to treat a number of childhood cancers, including neuroblastoma, osteosarcoma, hepatoblastoma, germ cell tumors, and brain tumors. Despite more than 30 years of clinical use (28), there are few means of identifying patients at risk for developing important platinum toxicities, and the extent to which underlying molecular pathways for various side effects may differ or overlap is not known.
Cisplatin-Induced Peripheral Neurotoxicity
Cisplatin-induced peripheral neurotoxicity is due largely to toxic effects on the dorsal root ganglia (36), although other mechanisms may be involved (37–39). The dorsal root ganglion and peripheral nerves are especially vulnerable to platinum accumulation (40–42), and the severity of symptoms is also associated with long-term serum cisplatin levels (14). Cisplatin-generated overproduction of reactive oxygen species may contribute in part to cisplatin neurotoxicity, which is reviewed by Argyriou et al. (10). The incidence and severity of long-term paresthesias are determined mainly by cumulative cisplatin dose (38,43), as well as dose intensity (13), and affect 14% to 57% of cancer survivors (median follow-up = 5–12 years; range = 1–28 years) (13,43–50). The wide range of percentages reflects not only differences in dose and dose intensity but also the influence of underlying medical conditions (eg, diabetes) and the use of other neurotoxic drugs, as well as genetic susceptibility. In a systematic review of 16 randomized trials for nine potential chemoprotectant reagents (acetylcysteine, amifostine, calcium, magnesium, diethyldithiocarbamate, glutathione, Org 2766, oxycarbazepine, and vitamin E), Albers et al. (9) concluded that insufficient evidence existed that any of these agents could either prevent or limit the neurotoxicity of platinating drugs. To our knowledge, there are no US Food and Drug Administration–approved drugs to either prevent or treat CIPN.
Few studies have addressed genetic susceptibility to long-term cisplatin neurotoxicity (51). An early study by Oldenburg et al. (51) focused on glutathione-S-transferases (GSTs), which are expressed in dorsal root ganglia and may protect against cisplatin-generated overproduction of reactive oxygen species. Among 238 testicular cancer survivors, self-reported neurotoxicity using the validated Scale for Chemotherapy-Induced Long-Term Neurotoxicity (52) was assessed according to functional polymorphisms in GSTP1 and GSTM1 in lymphocyte DNA (51). The 37 patients expressing GSTP1-GG were statistically significantly less symptomatic for distal paresthesias (hands: odds ratio [OR] = 0.46, 95% confidence interval [CI] = 0.22 to 0.96; feet: OR = 0.42, 95% CI = 0.20 to 0.88) compared with those with GSTP1-AA and GSTP1-AG (51). Other study comparisons were in terms of the total Scale for Chemotherapy-Induced Long-Term Neurotoxicity score, which also includes self-reported hearing loss and tinnitus. An investigation of polymorphisms in GSTs and several DNA repair genes in 104 ovarian cancer patients given cisplatin and cyclophosphamide found that neuropathy (measured in terms of National Cancer Institute criteria that were not further specified) was less frequent among women with the GSTM-null (OR = 0.37; 95% CI = 0.15 to 0.92) or GSTM3 AGG/AGG (OR = 0.34; 95% CI = 0.12 to 0.96) genotypes (53). To our knowledge, and according to a recent review (54), there have been no other pharmacogenomic studies of CIPN in which cisplatin was given alone or in combination with a non-neurotoxic chemotherapeutic agent.
Whereas genomic studies targeted toward cisplatin-related CIPN have been limited, a comprehensive genome-wide association study (GWAS) approach was recently applied by Baldwin et al. (25) to investigate paclitaxel-induced CIPN among 855 breast cancer patients administered single-agent paclitaxel in CALGB 40101. A single nucleotide polymorphism in FGD4 was associated with the onset of sensory peripheral neuropathy (rs10771973; hazard ratio [HR] = 1.57; 95% CI = 1.30 to 1.91) and replicated in European and black cohorts (25). FGD4 is a causal gene for the inherited peripheral neuropathy syndrome, Charcot-Marie-Tooth disease. In a separate study, genotyping of 214 patients treated with paclitaxel demonstrated that TUBB2A promoter polymorphisms located at -101 and -112 were associated with decreased paclitaxel neuropathy risk (HR = 0.64; 95% CI = 0.43 to 0.96; P = .03) (55). In preliminary data, Beutler et al. (56) identified two possible hereditary neuropathy genes (ARHGEF [OR = 3.62] and PRX [OR = 6.4]) as candidate genes using patient-reported outcome data and exome sequencing analysis in 73 women with paclitaxel-related CIPN and 46 control subjects. These results support the hypothesis that paclitaxel-associated CIPN and hereditary neuropathy might share genetic roots in a subset of patients.
Cisplatin-Induced Ototoxicity
Cisplatin-induced ototoxicity is associated with cumulative dose and dose intensity (13,57–59), although considerable interindividual variability exists (51,58–60). Studies of long-term cisplatin ototoxicity that include audiometry (median follow-up = 4–6 years; range = 1–13 years) (61,62) show altered hearing thresholds in 28% to 77% of patients. Although cisplatin hearing loss initially involves higher frequencies, it eventually affects a broader range, particularly those critical for speech perception (63). In a study of 1713 adult survivors of childhood cancer, hearing loss was detected in 62.1% of those given either cisplatin, carboplatin, or radiation doses to the ear of >30 Gy, although estimates were not stratified by treatment type (64). Long-term tinnitus after cisplatin affects 19% to 42% of patients (13).
Cisplatin ototoxicity can result from the overproduction of reactive oxygen species in the cochlea (58), causing irreversible free radical–related apoptosis of outer hair cells, spiral ganglion cells, and the stria vascularis (58,65). Data from animal models suggest that upregulation of antioxidant pathway activity, such as glutathione-S-transferases (GST) that are expressed in the mammalian cochlea (66), may help protect against ototoxicity (67). Oldenburg et al. (59) studied genotypes of GSTM1, GSTT1, and GSTP1 in 173 cisplatin-treated long-term testicular cancer survivors. Risk of hearing impairment was 4.21-fold (95% CI = 1.99 to 8.88) higher in testicular cancer survivors with 105Ile/105Ile-GSTP1 or 105Val/105Ile-GSTP1 compared with those with 105Val/105Val-GSTP1. Two combined genotypes were related to hearing loss. Pattern 1 (“GSTT1 positive, GSTM1 positive, 105Ile/105Ile-GSTP1”) was associated with 2.76-fold (95% CI = 1.35 to 5.64) higher risk of hearing impairment. Pattern 2 (“GSTT1 positive, GSTM1 positive, 105Val/105Val-GSTP1”) was related to a 5.35-fold (95% CI = 2.25 to 12.76) increase in protective effect. These results were not confirmed by Ross et al. (60), who examined 220 genes linked to the absorption, distribution, metabolism, and elimination of medications and their metabolites in 176 children with hearing loss after cisplatin-based regimens and found sixfold to 17-fold risks associated with methyltransferase activity (COMT, TPMT). A report (68) of 213 children from the St. Jude Medulloblastoma 96 and 03 protocols, however, did not replicate the above TPMT and COMT results, although subsequent analyses by Pussegoda et al. (69) replicated prior findings for TPMT (rs12201199; P = .001; OR = 6.1) and ABCC3 (rs 1051640; P = .04; OR = 1.8). A recent commentary underscored challenges in interpreting evidence for genetic predictors of ototoxicity, including the importance of taking into consideration concomitant medications, population stratification, and other influences (70).
Other candidate gene investigations of long-term cisplatin ototoxicity, restricted to variants in GSTM3 (71), mitochondrial DNA (72), or LRP2 (73), were inconclusive and limited to only 20 to 25 patients total with impaired hearing. An investigation of 204 lung cancer patients in China given cisplatin-based chemotherapy suggested that the copper transport protein 1 (CTR1) rs10981694 A>C polymorphism might be associated with enhanced ototoxicity, but methods used to evaluate hearing were not described (74). To our knowledge, no other studies address genetic susceptibility to long-term cisplatin ototoxicity in survivors of adult-onset cancer. GWASs of ototoxicity in a single disease treated with uniform therapies will constitute an important next step to further our understanding of the molecular underpinnings of cisplatin ototoxicity.
Epidemiologic Considerations
Several important epidemiologic considerations warrant attention in translational survivorship research, including study design, the selection of an optimal population, and characterization and quantification of exposures of interest and relevant outcomes (5). In addition, careful a priori consideration must be given to potential confounders and effect modifiers to maximize the scientific potential of the investigation to address clinically relevant hypotheses of interest.
Study Design
Classic epidemiologic designs with direct application to survivorship research include the prospective cohort, retrospective cohort, and case–control studies (26). An especially cost- and time-efficient choice for investigations of long-term toxicity is the retrospective cohort study (75,76), which enables the measurement of multiple outcomes (77). This study design also facilitates the later conduct of nested case–control investigations to examine associations of specific endpoints with antecedent treatments (78,79).
Selection of Optimal Population
It has been increasingly recognized that long-term toxicities typically have the most impact on younger cancer patients who receive curative therapy. Several investigations of childhood cancer survivors (80), including the US Childhood Cancer Survivor Study (76), are published or underway. In contrast, despite recommendations urging further studies of patients with adolescent and young adult cancer (aged 18–39 years) (81), few investigations have targeted this age group. The establishment of long-term cancer survivorship studies in young to middle-aged adults is especially important because patients are often cured and thus remain at lifelong risk for the emergence of either the late effects of cancer therapy or the long-term persistence of acute-onset toxicity. Given the deficit of research in this age group, an international consensus conference was convened in 2009 that focused on testicular cancer survivors, with the proceedings published in the Journal of the National Cancer Institute (82). Among the many identified unmet research needs in these patients, further study of genetic variants that underlie the long-term effects of cancer treatment was recommended. It was also pointed out that testicular cancer survivors are unique in that they develop both ototoxicity and CIPN after curative chemotherapy after a limited number of cisplatin-based regimens (82) and then gain many decades of life (83). Moreover, cisplatin-based chemotherapy in this population has also been associated with the development of the metabolic syndrome, cardiovascular disease and related vascular phenotypes (84–88), and secondary malignant neoplasms (89–91). Thus, the establishment of a cohort of testicular cancer survivors serves as a future study base for the investigation of genetic variants associated with late-onset cisplatin-associated toxicities that will likely evolve with the aging of these patients (92).
Characterization and Quantification of Exposures of Interest and Outcomes
Whereas GWASs of cancer etiology have typically yielded small odds ratios of 1.05 to 1.4 (93), those reported in pharmacogenomic GWASs of drug toxicity range from fivefold to 1000-fold (genotype RR) (94). Thus, the sixfold to 17-fold risk estimates (60) noted for cisplatin are typical of those found in other pharmacogenomic toxicity studies. These include the 80-fold risk associated with HLA-B*5701 and flucoxacillin-induced liver injury (95), the fivefold risk associated with variation in ABCG2 and gefitinib-associated diarrhea (94), and the 1023-fold risk of HLA-B*1502 and carbamazepine-induced Steven’s Johnson syndrome (94). These large magnitudes of effect reflect the fact that the specific potent etiologic exposure (ie, drug) is known and appropriately accounted for in the analysis. Thus, it is critical to collect accurate, detailed information on drug dose. For testicular cancer survivors, this task is simplified given the relatively homogeneous cisplatin-based regimens and number of cycles that most patients receive. These regimens typically include cisplatin, bleomycin, and etoposide (3 cycles) or cisplatin and etoposide (4 cycles). Given the possible influence of one cytotoxic drug on the pharmacokinetic properties of another drug or the effect of drug interactions on endpoints, it is important to obtain detailed information on all drugs administered in chemotherapy regimens. Similar strategies have been successfully applied in analytic studies of therapy-related leukemia after cisplatin-based chemotherapy for either ovarian (96) or testicular (97) cancer. The conduct of studies within cancer centers that use standardized testicular cancer treatment regimens and maintain detailed chemotherapy records increases the availability of detailed information on administered drug dose, schedule, and the dose intensity of each cytotoxic drug.
The choice of measurement instruments for CIPN warrants careful consideration. The selection of validated and reproducible measures of CIPN is critically important (98). Patient self-reports of neurotoxicity symptoms are frequently selected as endpoints, with various instruments critically reviewed by Cavaletti et al. (99). A number of options currently exist, including instruments customized to measure CIPN due to cisplatin (52), oxaliplatin (100), and taxanes (99). A question frequently arises as to whether to incorporate detailed neurologic evaluations into CIPN assessments, and the yield of these studies must be considered in view of the expense and difficulty involved in standardizing detailed neurologic examinations and the issue of patient compliance, especially in large multicenter studies. Moreover, patient-reported outcomes may represent the most pertinent measure of CIPN because they directly address the extent to which symptoms interfere with quality of life rather than rely on the detection of subclinical effects. However, measures of quality of life do not always reflect the underlying severity of neuropathic impairment. The use of two or more validated instruments selected in close collaboration with a study neurologist, reflecting both impairment (eg, the Total Neuropathy score or the abbreviated reduced or clinical version) and quality of life (eg, the disease-specific European Organization for Research and Treatment of Cancer QLQ-Chemotherapy-Induced Peripheral Neuropathy 20) to reliably measure the degree of peripheral neurotoxicity and its impact upon patients, is desirable (98). Such an approach is important to minimize variability that may be introduced into pharmacogenomic studies through a lack of reproducible CIPN endpoints (99).
An objective measure of ototoxicity is air threshold audiometry measured in decibels at 3000 Hz, 4000 Hz, and 6000 Hz, averaged for both ears (59). These frequencies represent the upper limit of the language communication range and are especially vulnerable to cisplatin toxicity. Audiometric results can be compared with normative age-specific values divided into percentiles of normal thresholds in collaboration with the study hearing scientist (101). For analyses, methods similar to those of Brydoy (13) and Oldenburg (59) can be used, whereby patients with bilateral sensorineural hearing impairment of >20 db at 3000 Hz, 4000 Hz, and 6000 Hz are classified as ototoxic, whereas those with normal hearing for their age group are classified as not ototoxic. Cisplatin-related damage is typified by thresholds at 6 to 8kHz that are worse than lower frequencies (16). Because noise damage shows hearing thresholds that improve at 6 to 8kHz, relative to 3 to 4kHz (102,103), potential noise-induced ototoxicity can be distinguished from cisplatin-induced ototoxicity.
Consideration of Potential Confounders and Effect Modifiers
Potentially important confounders and effect modifiers that might influence the development of CIPN and/or ototoxicity should also be identified and measured. For example, possible neurotoxic risk factors or effect modifiers include diabetes, other metabolic or immunologic conditions, excess alcohol use, smoking, concurrent diseases affecting peripheral nerves, and concomitant medications (54). Possible confounders for ototoxicity include familial hearing disorders, excess alcohol use (104), diabetes (13), tobacco use (13,43,51,61,105), age (43,57,61,106), underlying malignancy [eg, multiple myeloma (107)], and medications such as the aminoglycosides (108). A study limited to survivors of testicular cancer controls for sex, although data collection on race, even in a disease that predominantly affects whites, is important to account for any role of ethnic variation on drug pharmacokinetics or pharmacodynamics.
Leveraging Preclinical Data in Translational Survivorship Research
Many researchers have used cell-based models for pharmacogenomic discovery using International HapMap human Epstein-Barr virus–transformed lymphoblastoid cell lines (LCLs) because these cells provide a cost-effective testing system in which other exposures (eg, concomitant medications) can be controlled (109–111). Using this preclinical model, the degree to which genetics contributes to cisplatin-induced cytotoxicity is 0.32% to 0.45% (112). In addition to heritability estimates, the cell model allows the identification of genetic variants associated with susceptibility to cytotoxic agents (ie, cisplatin). This is because HapMap LCLs include publicly available genotype and sequencing data, which permits GWASs between genetic variants and pharmacologic phenotypes (ie, cytotoxicity, apoptosis) in LCLs after chemotherapy exposure. The LCL model is highly valuable because, in addition to the freely available genomic data, there is baseline expression data using Affymetrix exon array (113), Exiqon miRNA data (114), and Illumina 450K methylation data (115); these resources importantly allow assignment of function to genetic variants associated with pharmacologic phenotypes measured in LCLs such as cisplatin-induced cytotoxicity. Genetic variants that are identified can be evaluated further with studies designed according to whether the single-nucleotide polymorphisms (SNPs) are also associated with mRNA, miRNA, modified cytosines, or proteins. Using population panels of diverse ancestry totaling 608 LCLs, Wheeler et al. (116) performed meta-analyses of more than 3 million SNPs and identified GSTM1 (glutathione S-transferase mu 1), GSTT1, ERCC2 and ERCC6 as associated with platinum cytotoxicity.
Analytic Approaches in Pharmacogenomic and Genomic Research
A primary challenge in identifying pharmacogenomic markers from clinical trials is that the most secure inferences require a homogenous population treated with the same dosage regimen and minimal confounding variables, including other drugs. In clinical oncology care this is difficult, if not impossible, given the diversity of cancer types and also taking into account disease presentations and patient factors. The standard of care for many cancers also changes as new therapies emerge, with the vast majority of patients receiving various drug combinations. A notable exception, as reviewed above, is the ongoing use of only two major cisplatin-based chemotherapy regimens for testicular cancer (82).
Clinical trials frequently provide only short-term patient follow-up. A major goal in cancer survivorship research is to improve the understanding of long-term toxicities. The integration of epidemiologic data with cell-based models for pharmacogenomic marker identification represents a critical step forward in translational medicine to improve the power of discovery research and expand opportunities for replication, validation, and follow-up. For example, Wheeler et al. (27) compared the results of genetic studies of cytotoxicity in LCLs to the results of genome studies conducted in a prospective human clinical trial using the same chemotherapeutic drug. SNPs with nominally statistically significant associations for paclitaxel sensitivity in LCLs were tested for enrichment among those SNPs most strongly related to paclitaxel-induced peripheral neuropathy using novel analytic approaches conditioned on factors likely to influence enrichment (eg, SNP minor allele frequency, distance to nearest gene). Statistically significant enrichment among a relatively large number of top SNPs is consistent with the hypothesis that the cell-based model and the human phenotype (ie, long-term peripheral neuropathy) share at least a proportion of genetic architecture. It should be noted that evidence for shared genetic architecture invariably involves large numbers of SNPs with small effects. Cumulatively, large numbers of common variants with small effects can account for substantial heritability (117); this general model appears to be most consistent with the heritability studies conducted in both preclinical cell-based model systems and investigations of efficacy and common adverse events in data from prospective studies (117).
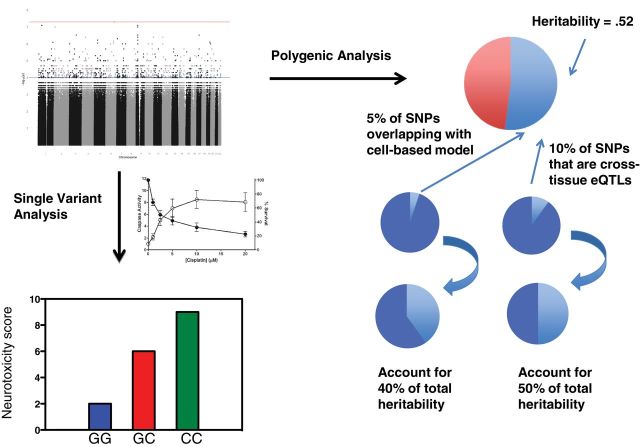
As described above (27), results of a GWAS of SNPs in LCLs associated with paclitaxel-induced cytotoxicity were compared with results of a GWAS of CIPN in breast cancer patients (n = 859) given paclitaxel alone in CALGB 40101. An enrichment of LCL cytotoxicity-associated SNPs in the CIPN-associated SNPs from the clinical trial with concordant allelic direction of effect was observed (empirical P = .007). No such enrichment was observed when evaluating either capecitabine- or carboplatin-induced cytotoxicity SNPs, which were tested as negative controls. Of the 24 SNPs that overlapped between the clinical trial (P < .05) and the preclinical cytotoxicity study (P < .001), 19 of them were expression quantitative trait loci, which represent a statistically significant enrichment of this functional class (empirical P = .05). This type of statistically significant LCL enrichment result is a critical observation because it implies that an enhanced understanding of the genetic architecture of cell-based models will inform an understanding of the genetic architecture of CIPN (27). Figure 1 illustrates this type of research strategy. In addition, SNPs associated with CIPN can also be studied for enrichment in diabetes-induced neuropathy to test for common genetic architecture across neuropathy phenotypes generated by different exposures. These approaches allow for the prioritization of SNPs and potentially DNA variants for functional studies.
Figure 1.
Example of translational genomic approach. After a genome-wide association study of drug-induced neurotoxicity in patients to identify associated single nucleotide polymorphisms (SNPs; left panel, upper portion), an enrichment analysis for drug-induced cytotoxicity in lymphoblastoid cell line (LCL) models can be performed (117). This analysis identifies single overlapping SNPs correlated with neurotoxicity in patients and drug sensitivity in vitro (left panel, lower portion). Additional analyses determine the degree of heritability explained by the clinical phenotype (ie, drug-induced neurotoxicity) (right panel, top portion). Of SNPs associated with the clinical phenotype, the fraction that overlap with the LCL-based model and the fraction that are cross-tissue expression quantitative trait loci (eQTL) using genome-tissue expression datasets can be estimated (right panel, bottom portion) (137).
Risk Prediction Modeling and Future Applications
Early results of first generation GWASs appeared to discourage genetic epidemiologists from considering prediction as a primary rationale for genome discovery research. This was because effect sizes for DNA variants meeting genome-wide criteria for statistical significance (5×10–8) were so modest that even dozens of such variants tended to account for only 5% to 10% of the interindividual variation in liability to disease (118,119) and a comparably small fraction of the heritability that was expected based on prior twin and family studies. More recent, it has become clear that appropriately calculating the contribution of all tested genetic variants (rather than only those with established association) can account for a sizable amount of the substantial interindividual variability in disease development. Although the subset of variants identified through GWASs as having genome-wide statistically significant association to disease account for less than 10% of expected heritability (and often less than 5%), it is common for all interrogated variants to account for 50% or more of expected heritability (120).
A variety of approaches to prediction that leverage large-scale genome information and potentially other -omics data are now being developed with meaningful potential impact on patient care because of changing models in how genome information is being collected and used within health-care systems. Point-of-care genotyping for a single polymorphism, which can cost less than $500 (121), is now considered standard of care for prescribing a number of drugs (121,122). Similarly, preemptive large-scale genome studies on millions of DNA variants (including many, if not all, of those commonly required for routine pharmacogenetic testing) in certified laboratories are now becoming comparable in cost. Many health-care systems are assessing the cost-effectiveness of routine collection of large-scale genome information for all patients in or entering their systems (122). Costs of sequencing (123) are rapidly decreasing and may, within a couple of years, be less than that for magnetic resonance imaging. Theoretically large-scale genome information can then be generated on each patient shortly after cancer diagnosis, from which these data would inform and optimize treatment decisions.
As an example of the level of prediction that is now possible, Wheeler et al. (124) applied a novel large-scale prediction approach called OmicKriging (which translates similarity in genotype and any other -omic data into phenotypic data similarity to predict complex traits, such as CIPN or ototoxicity) to type 1 diabetes data from the Wellcome Trust Case Control Consortium. The area under the curve for the receiver operator characteristics for the out-of-sample prediction was in the range of 0.7 to 0.8, an area-under-the-curve result that has clear clinical utility. Although we look forward to the day that genomic (and other -omic discoveries) fully illuminate the biology underlying the development of adverse events and efficacy in ways that allow us to improve therapies in more informed ways, medicine benefits even today from the use of biomarker predictors whose biological basis remains poorly understood. Thus, there is clear value in using every bit of the predictive power that can be drawn from results of early genome studies to improve patient care, even as simultaneously these discoveries enhance an understanding of biology.
Comment
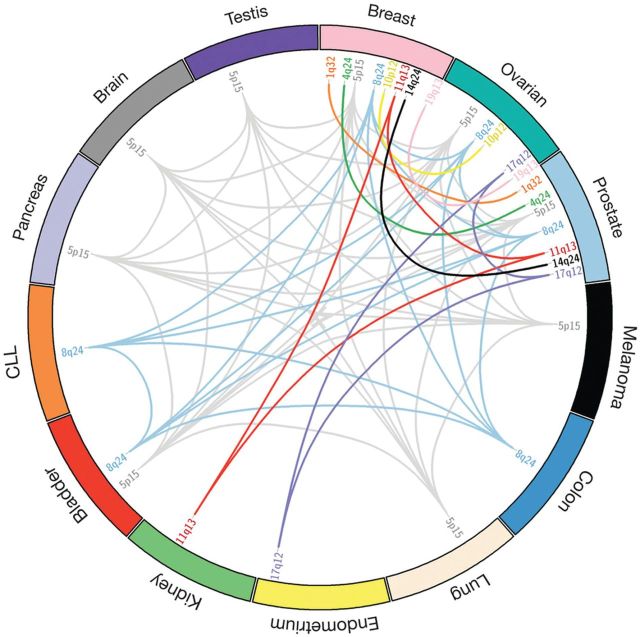
The number of cancer survivors in the United States has steadily increased, and the field of genomic research has also grown rapidly. Commensurately, the cost of genotyping has decreased considerably, with ongoing trends monitored by the National Human Genome Research Institute (123). Whereas, for some early and late effects of cancer and its therapy, preventive and interventional strategies exist, to our knowledge these types of approaches are not yet available for CIPN and ototoxicity. The knowledge gained from application of translational genomics to these toxicities holds considerable promise to improve the quality of life for cancer survivors. Moreover, it is likely that, as we discover in cancer survivors the molecular underpinnings for treatment-associated disorders for which subsequent risks are increased, such as cardiovascular disease (125), metabolic syndrome (126), osteoporosis (127), and second malignant neoplasms (4), these insights may also contribute to our understanding of the general biology of these common diseases in humans. Recent results from the Collaborative Oncological Gene–Environment Study, which showed common pathways between a number of different cancer types (Figure 2) (128), will likely in the future be expanded to show common pathways for a number of disorders, including cardiovascular disease, type 2 diabetes, cancer, and many others. For example, Gadalla et al. (129) recently demonstrated that patients with myotonic muscular dystrophy (an autosomal-dominant neuromuscular disorder characterized by unstable nucleotide repeat expansions) also have a statistically significantly increased risk of cancer. It is recognized already that long-term inflammation plays a role in many chronic diseases (130,131).
Figure 2.
Pleiotropy among different cancers detected by the Collaborative Oncological Gene–Environment Study (COGS) and previous association studies. Risk-associated loci for each cancer are indicated by chromosomal location, and sharing is indicated by colored lines connecting different cancers. For example, loci at 8q24 are associated with breast, ovarian, prostate, colon, and bladder cancers and with chronic lymphocytic leukemia (CLL) (light-blue lines). Reprinted with permission from Sakoda et al. (128).
Further research on the contribution of DNA variants to the temporal pattern of toxicities, as noted for the association of FGD4 with early-onset paclitaxel-related CIPN (25), will also be highly informative. It is already established that increased risks of iatrogenic lung cancer in survivors of Hodgkin lymphoma show markedly different temporal trends depending on whether the antecedent carcinogenic exposure is chemotherapy or radiotherapy (132). Such variability likely reflects the operation of different underlying molecular pathways, as well as the influence of other factors (4). In a similar vein, the comparison of genetic pathways for life-threatening treatment-associated complications [eg, second malignant neoplasms and cardiovascular disease (133,134)] in patients diagnosed with cancer at different ages (ie, childhood vs adult) will also be informative.
The importance of future research among the growing number of cancer survivors worldwide was underscored as early as 1998 by Li and Stovall (135), and since this time the number of survivors has at least tripled and continues to grow (2). Cancer survivors comprise a growing population in the United States, with the management of morbidities in these patients likely to constitute a substantial financial cost to the health-care system. The burden of chronic morbidities in subgroups of cancer survivors for whom risks have been estimated to date is sobering, with the 30-year cumulative incidence of a chronic health condition in US childhood cancer survivors estimated at 62.3%, compared with 36.8% in sibling controls (77). Future research in cancer survivors to optimally manage long-term morbidities (5) will become important not only in terms of patient welfare but also in the control of health-care expenses (136). Given the recent emergence of translational genomics, the scientific community now has an unprecedented opportunity to make major inroads into the prevention and treatment of toxicities that adversely affect short- and long-term patient outcomes (5).
Funding
This work was supported by the National Cancer Institute (1R01 CA157823-01A1 to LBT).
The study sponsor had no role in the writing of this manuscript or the decision to submit it for publication.
We are indebted to Mrs. Laura Finger for expert editorial support.
The Platinum Study Group consists of Howard D. Sesso (Brigham and Women’s Hospital, Boston, MA); Clair J. Beard and Stephanie Curreri (Dana-Farber Cancer Institute); Lawrence H. Einhorn, Mary Jacqueline Brames, and Somer Case-Eads (Indiana University); Robert C. Miller (Mayo Clinic); Lance C. Pagliaro (MD Anderson Cancer Center); Darren R. Feldman, Erin Jacobsen, and Deborah Silber (Memorial Sloan-Kettering Cancer Center); Malcolm Moore and Lynn Anson-Cartwright (Princess Margaret Hospital); Nancy J. Cox, M. Eileen Dolan (University of Chicago); David J. Vaughn, Linda Jacobs, SarahLena Panzer, and Donna Pucci (University of Pennsylvania); Lois B. Travis, Debbie Baker, John D. Bisognano, Cindy Casaceli, Chunkit Fung, David N. Herrmann, Eileen Johnson, Kris Kuryla, Derick R. Peterson, Deepak Sahasrabudhe, Marissa Velez, and Melissa Worman (University of Rochester); and Robert D. Frisina (University of South Florida). The Platinum Study Group Advisory Committee consists of George Bosl (Memorial Sloan-Kettering Cancer Center); Sophie D. Fossa (Norwegian Radium Hospital); Mary Gospodarowicz (Princess Margaret Hospital); Leslie L. Robison (St. Jude Children’s Research Hospital); Steven E. Lipshultz (Wayne State University); and David Oakes (University of Rochester).
References
- 1. Altekruse S, Kosary C, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2007. National Cancer Institute, Bethesda, MD: National Cancer Institute; 2010. http://seer.cancer.gov/csr/1975_2007/ Accessed February 18, 2014.
- 2. Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62(4):220–241. [DOI] [PubMed] [Google Scholar]
- 3.Anonymous. Cancer survivors: living longer, and now, better. Lancet. 2004;364(9452):2153–2154. [DOI] [PubMed] [Google Scholar]
- 4. Travis LB, Demark Wahnefried W, Allan JM, et al. Aetiology, genetics and prevention of secondary neoplasms in adult cancer survivors. Nat Rev Clin Oncol. 2013;10(5):289–301. [DOI] [PubMed] [Google Scholar]
- 5. Elena JW, Travis LB, Simonds NI, et al. Leveraging epidemiology and clinical studies of cancer outcomes: recommendations and opportunities for translational research. J Natl Cancer Inst. 2013;105(2):85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grisold W, Cavaletti G, Windebank AJ. Peripheral neuropathies from chemotherapeutics and targeted agents: diagnosis, treatment, and prevention. Neuro Oncol. 2012;14(Suppl 4):iv45–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smith EM, Pang H, Cirrincione C, et al. Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. JAMA. 2013;309(13):1359–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hammack JE, Michalak JC, Loprinzi CL, et al. Phase III evaluation of nortriptyline for alleviation of symptoms of cis-platinum-induced peripheral neuropathy. Pain. 2002;98(1–2):195–203. [DOI] [PubMed] [Google Scholar]
- 9. Albers JW, Chaudhry V, Cavaletti G, et al. Interventions for preventing neuropathy caused by cisplatin and related compounds. Cochrane Database Syst Rev. 2011;2:CD005228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Argyriou AA, Bruna J, Marmiroli P, et al. Chemotherapy-induced peripheral neurotoxicity (CIPN): an update. Crit Rev Oncol Hematol. 2012;82(1):51–77. [DOI] [PubMed] [Google Scholar]
- 11. Park SB, Goldstein D, Krishnan AV, et al. Chemotherapy-induced peripheral neurotoxicity: a critical analysis [published online ahead of print October 31, 2013]. CA Cancer J Clin. 2013; 10.1002/caac.21204. [DOI] [PubMed] [Google Scholar]
- 12. Mykletun A, Dahl AA, Haaland CF, et al. Side effects and cancer-related stress determine quality of life in long-term survivors of testicular cancer. J Clin Oncol. 2005;23(13):3061–3068. [DOI] [PubMed] [Google Scholar]
- 13. Brydoy M, Oldenburg J, Klepp O, et al. Observational study of prevalence of long-term Raynaud-like phenomena and neurological side effects in testicular cancer survivors. J Natl Cancer Inst. 2009;101(24):1682–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sprauten M, Darrah TH, Peterson DR, et al. Impact of long-term serum platinum concentrations on neuro- and ototoxicity in cisplatin-treated survivors of testicular cancer. J Clin Oncol. 2012;30(3):300–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bhatia S. Role of genetic susceptibility in development of treatment-related adverse outcomes in cancer survivors. Cancer Epidemiol Biomarkers Prev. 2011;20(10):2048–2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schell MJ, McHaney VA, Green AA, et al. Hearing loss in children and young adults receiving cisplatin with or without prior cranial irradiation. J Clin Oncol. 1989;7(6):754–760. [DOI] [PubMed] [Google Scholar]
- 17. Mukherjea D, Jajoo S, Whitworth C, et al. Short interfering RNA against transient receptor potential vanilloid 1 attenuates cisplatin-induced hearing loss in the rat. J Neurosci. 2008;28(49):13056–13065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Knight KR, Kraemer DF, Neuwelt EA. Ototoxicity in children receiving platinum chemotherapy: underestimating a commonly occurring toxicity that may influence academic and social development. J Clin Oncol. 2005;23(34):8588–8596. [DOI] [PubMed] [Google Scholar]
- 19. Grewal S, Merchant T, Reymond R, et al. Auditory late effects of childhood cancer therapy: a report from the Children’s Oncology Group. Pediatrics. 2010;125(4):e938–e950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Langer T, am Zehnhoff-Dinnesen A, Radtke S, et al. Understanding platinum-induced ototoxicity. Trends Pharmacol Sci. 2013;34(8):458–469. [DOI] [PubMed] [Google Scholar]
- 21. Kemp G, Rose P, Lurain J, et al. Amifostine pretreatment for protection against cyclophosphamide-induced and cisplatin-induced toxicities: results of a randomized control trial in patients with advanced ovarian cancer. J Clin Oncol. 1996;14(7):2101–2112. [DOI] [PubMed] [Google Scholar]
- 22. Marina N, Chang KW, Malogolowkin M, et al. Amifostine does not protect against the ototoxicity of high-dose cisplatin combined with etoposide and bleomycin in pediatric germ-cell tumors: a Children’s Oncology Group study. Cancer. 2005;104(4):841–847. [DOI] [PubMed] [Google Scholar]
- 23. Gallegos-Castorena S, Martinez-Avalos A, Mohar-Betancourt A, et al. Toxicity prevention with amifostine in pediatric osteosarcoma patients treated with cisplatin and doxorubicin. Pediatr Hematol Oncol. 2007;24(6):403–408. [DOI] [PubMed] [Google Scholar]
- 24. van As JW, van den Berg H, van Dalen EC. Medical interventions for the prevention of platinum-induced hearing loss in children with cancer. Cochrane Database Syst Rev. 2012;5:CD009219. [DOI] [PubMed] [Google Scholar]
- 25. Baldwin RM, Owzar K, Zembutsu H, et al. A genome-wide association study identifies novel loci for paclitaxel-induced sensory peripheral neuropathy in CALGB 40101. Clin Cancer Res. 2012;18(18):5099–5109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Travis LB. The epidemiology of second primary cancers. Cancer Epidemiol Biomarkers Prev. 2006;15(11):2020–2026. [DOI] [PubMed] [Google Scholar]
- 27. Wheeler HE, Gamazon ER, Wing C, et al. Integration of cell line and clinical trial genome-wide analyses supports a polygenic architecture of paclitaxel-induced sensory peripheral neuropathy. Clin Cancer Res. 2013;19(2):491–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Einhorn LH, Donohue J. Cis-diamminedichloroplatinum, vinblastine, and bleomycin combination chemotherapy in disseminated testicular cancer. Ann Intern Med. 1977;87(3):293–298. [DOI] [PubMed] [Google Scholar]
- 29. National Cancer Institute. Provocative questions: identifiying problems to drive progress against cancer. http://provocativequestions.nci.nih.gov/ Accessed February 18, 2014.
- 30. Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. [DOI] [PubMed] [Google Scholar]
- 31. IARC. Globocan 2008 fact sheet. http://globocan.iarc.fr/factsheets/cancers/breast.asp Accessed February 18, 2014. [Google Scholar]
- 32. Sirohi B, Arnedos M, Popat S, et al. Platinum-based chemotherapy in triple-negative breast cancer. Ann Oncol. 2008;19(11):1847–1852. [DOI] [PubMed] [Google Scholar]
- 33. Bosch A, Eroles P, Zaragoza R, et al. Triple-negative breast cancer: molecular features, pathogenesis, treatment and current lines of research. Cancer Treat Rev. 2010;36(3):206–215. [DOI] [PubMed] [Google Scholar]
- 34. Isakoff SJ. Triple-negative breast cancer: role of specific chemotherapy agents. Cancer J. 2010;16(1):53–61. [DOI] [PMC free article] [PubMed]
- 35. Uhm JE, Park YH, Yi SY, et al. Treatment outcomes and clinicopathologic characteristics of triple-negative breast cancer patients who received platinum-containing chemotherapy. Int J Cancer. 2009;124(6):1457–1462. [DOI] [PubMed] [Google Scholar]
- 36. McDonald ES, Randon KR, Knight A, et al. Cisplatin preferentially binds to DNA in dorsal root ganglion neurons in vitro and in vivo: a potential mechanism for neurotoxicity. Neurobiol Dis. 2005;18(2):305–313. [DOI] [PubMed] [Google Scholar]
- 37. Meijer C, de Vries EG, Marmiroli P, et al. Cisplatin-induced DNA-platination in experimental dorsal root ganglia neuronopathy. Neurotoxicology. 1999;20(6):883–887. [PubMed] [Google Scholar]
- 38. Hausheer FH, Schilsky RL, Bain S, et al. Diagnosis, management, and evaluation of chemotherapy-induced peripheral neuropathy. Semin Oncol. 2006;33(1):15–49. [DOI] [PubMed] [Google Scholar]
- 39. Quasthoff S, Hartung HP. Chemotherapy-induced peripheral neuropathy. J Neurol. 2002;249(1):9–17. [DOI] [PubMed] [Google Scholar]
- 40. Gregg RW, Molepo JM, Monpetit VJ, et al. Cisplatin neurotoxicity: the relationship between dosage, time, and platinum concentration in neurologic tissues, and morphologic evidence of toxicity. J Clin Oncol. 1992;10(5):795–803. [DOI] [PubMed] [Google Scholar]
- 41. Krarup-Hansen A, Rietz B, Krarup C, et al. Histology and platinum content of sensory ganglia and sural nerves in patients treated with cisplatin and carboplatin: an autopsy study. Neuropathol Appl Neurobiol. 1999;25(1):29–40. [DOI] [PubMed] [Google Scholar]
- 42. Thompson SW, Davis LE, Kornfeld M, et al. Cisplatin neuropathy. Clinical, electrophysiologic, morphologic, and toxicologic studies. Cancer. 1984;54(7):126–1275. [DOI] [PubMed] [Google Scholar]
- 43. Bokemeyer C, Berger CC, Kuczyk MA, et al. Evaluation of long-term toxicity after chemotherapy for testicular cancer. J Clin Oncol. 1996;14(11):2923–2932. [DOI] [PubMed] [Google Scholar]
- 44. Aass N, Kaasa S, Lund E, et al. Long-term somatic side-effects and morbidity in testicular cancer patients. Br J Cancer. 1990;61(1):151–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hansen SW, Helweg-Larsen S, Trojaborg W. Long-term neurotoxicity in patients treated with cisplatin, vinblastine, and bleomycin for metastatic germ cell cancer. J Clin Oncol. 1989;7(10):1457–1461. [DOI] [PubMed] [Google Scholar]
- 46. von Schlippe M, Fowler CJ, Harland SJ. Cisplatin neurotoxicity in the treatment of metastatic germ cell tumour: time course and prognosis. Br J Cancer. 2001;85(6):823–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Boyer M, Raghavan D, Harris PJ, et al. Lack of late toxicity in patients treated with cisplatin-containing combination chemotherapy for metastatic testicular cancer. J Clin Oncol. 1990;8(1):21–26. [DOI] [PubMed] [Google Scholar]
- 48. Bissett D, Kunkeler L, Zwanenburg L, et al. Long-term sequelae of treatment for testicular germ cell tumours. Br J Cancer. 1990;62(4):655–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Petersen PM, Hansen SW. The course of long-term toxicity in patients treated with cisplatin-based chemotherapy for non-seminomatous germ-cell cancer. Ann Oncol. 1999;10(12):1475–1483. [DOI] [PubMed] [Google Scholar]
- 50. Roth BJ, Greist A, Kubilis PS, et al. Cisplatin-based combination chemotherapy for disseminated germ cell tumors: long-term follow-up. J Clin Oncol. 1988;6(8):1239–1247. [DOI] [PubMed] [Google Scholar]
- 51. Oldenburg J, Kraggerud SM, Brydoy M, et al. Association between long-term neuro-toxicities in testicular cancer survivors and polymorphisms in glutathione-s-transferase-P1 and -M1, a retrospective cross sectional study. J Transl Med. 2007;5:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Oldenburg J, Fossa SD, Dahl AA. Scale for chemotherapy-induced long-term neurotoxicity (SCIN): psychometrics, validation, and findings in a large sample of testicular cancer survivors. Qual Life Res. 2006;15(5):791–800. [DOI] [PubMed] [Google Scholar]
- 53. Khrunin AV, Moisseev A, Gorbunova V, et al. Genetic polymorphisms and the efficacy and toxicity of cisplatin-based chemotherapy in ovarian cancer patients. Pharmacogenomics J. 2010;10(1):54–61. [DOI] [PubMed] [Google Scholar]
- 54. Cavaletti G, Alberti P, Marmiroli P. Chemotherapy-induced peripheral neurotoxicity in the era of pharmacogenomics. Lancet Oncol. 2011;12(12):1151–1161. [DOI] [PubMed] [Google Scholar]
- 55. Leandro-Garcia LJ, Leskela S, Jara C, et al. Regulatory polymorphisms in B-tubulin IIa are associated with paclitaxel-induced peripheral neuropathy. Clin Cancer Res. 2012;18(16):4441–4448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Beutler AS, Kulkarni A, Kanwar R, et al. Sequencing symptom control: Results from the Alliance N08C1 and N08CA genetics of chemotherapy neuropathy trials. In: 104th Annual Meeting of the American Association for Cancer Research; Washington, DC; 2013. http://www.abstractsonline.com/Plan/ViewAbstract.aspx?sKey=d4332bf8-005b-4cb2-a378-921ae4782081&cKey=52268d6b-7335-4aca-9338-653d6c27ffdb&mKey=%7b9B2D28E7-24A0-466F-A3C9-07C21F6E9BC9%7d Accessed February 18, 2014.
- 57. Rademaker-Lakhai JM, Crul M, Zuur L, et al. Relationship between cisplatin administration and the development of ototoxicity. J Clin Oncol. 2006;24(6):918–924. [DOI] [PubMed] [Google Scholar]
- 58. Rybak LP. Mechanisms of cisplatin ototoxicity and progress in otoprotection. Curr Opin Otolaryngol Head Neck Surg. 2007;15(5):364–369. [DOI] [PubMed] [Google Scholar]
- 59. Oldenburg J, Kraggerud SM, Cvancarova M, et al. Cisplatin-induced long-term hearing impairment is associated with specific glutathione s-transferase genotypes in testicular cancer survivors. J Clin Oncol. 2007;25(6):708–714. [DOI] [PubMed] [Google Scholar]
- 60. Ross CJ, Katzov-Eckert H, Dube MP, et al. Genetic variants in TPMT and COMT are associated with hearing loss in children receiving cisplatin chemotherapy. Nat Genet. 2009;41(12):1345–1349. [DOI] [PubMed] [Google Scholar]
- 61. Bokemeyer C, Berger CC, Hartmann JT, et al. Analysis of risk factors for cisplatin-induced ototoxicity in patients with testicular cancer. Br J Cancer. 1998;77(8):1355–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Osanto S, Bukman A, Van Hoek F, et al. Long-term effects of chemotherapy in patients with testicular cancer. J Clin Oncol. 1992;10(4):574–579. [DOI] [PubMed] [Google Scholar]
- 63. Biro K, Noszek L, Prekopp P, et al. Characteristics and risk factors of cisplatin-induced ototoxicity in testicular cancer patients detected by distortion product otoacoustic emission. Oncology. 2006;70(3):177–184. [DOI] [PubMed] [Google Scholar]
- 64. Hudson MM, Ness KK, Gurney JG, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013;309(22):2371–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. van Ruijven MW, de Groot JC, Klis SF, et al. The cochlear targets of cisplatin: an electrophysiological and morphological time-sequence study. Hear Res. 2005;205(1–2):241–248. [DOI] [PubMed] [Google Scholar]
- 66. van Ruijven MW, de Groot JC, Smoorenburg GF. Time sequence of degeneration pattern in the guinea pig cochlea during cisplatin administration. A quantitative histological study. Hear Res. 2004;197(1–2):44–54. [DOI] [PubMed] [Google Scholar]
- 67. el Barbary A, Altschuler RA, Schacht J. Glutathione S-transferases in the organ of Corti of the rat: enzymatic activity, subunit composition and immunohistochemical localization. Hear Res. 1993;71(1–2):80–90. [DOI] [PubMed] [Google Scholar]
- 68. Yang JJ, Lim JY, Huang J, et al. The role of inherited TPMT and COMT genetic variation in cisplatin-induced ototoxicity in children with cancer. Clin Pharmacol Ther. 2013;94(2):252–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Pussegoda K, Ross CJ, Visscher H, et al. Replication of TPMT and ABCC3 genetic variants highly associated with cisplatin-induced hearing loss in children. Clin Pharmacol Ther. 2013;94(2):243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ratain MJ, Cox NJ, Henderson TO. Challenges in interpreting the evidence for genetic predictors of ototoxicity. Clin Pharmacol Ther. 2013;94(6):631–635. [DOI] [PubMed] [Google Scholar]
- 71. Peters U, Preisler-Adams S, Hebeisen A, et al. Glutathione S-transferase genetic polymorphisms and individual sensitivity to the ototoxic effect of cisplatin. Anticancer Drugs. 2000;11(8):639–643. [DOI] [PubMed] [Google Scholar]
- 72. Peters U, Preisler-Adams S, Lanvers-Kaminsky C, et al. Sequence variations of mitochondrial DNA and individual sensitivity to the ototoxic effect of cisplatin. Anticancer Res. 2003;23(2B):1249–1255. [PubMed] [Google Scholar]
- 73. Riedemann L, Lanvers C, Deuster D, et al. Megalin genetic polymorphisms and individual sensitivity to the ototoxic effect of cisplatin. Pharmacogenomics J. 2008;8(1):23–28. [DOI] [PubMed] [Google Scholar]
- 74. Xu X, Ren H, Zhou B, et al. Prediction of copper transport protein 1 (CTR1) genotype on severe cisplatin induced toxicity in non-small cell lung cancer (NSCLC) patients. Lung Cancer. 2012;77(2):438–442. [DOI] [PubMed] [Google Scholar]
- 75. Dores GM, Metayer C, Curtis RE, et al. Second malignant neoplasms among long-term survivors of Hodgkin’s disease: a population-based evaluation over 25 years. J Clin Oncol. 2002;20(16):3484–3494. [DOI] [PubMed] [Google Scholar]
- 76. Robison LL, Armstrong GT, Boice JD, et al. The Childhood Cancer Survivor Study: a National Cancer Institute-supported resource for outcome and intervention research. J Clin Oncol. 2009;27(14):2308–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–1582. [DOI] [PubMed] [Google Scholar]
- 78. Travis LB, Hill DA, Dores GM, et al. Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA. 2003;290(4):465–475. [DOI] [PubMed] [Google Scholar]
- 79. Inskip PD, Robison LL, Stovall M, et al. Radiation dose and breast cancer risk in the childhood cancer survivor study. J Clin Oncol. 2009;27(24):3901–3907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Reulen RC, Frobisher C, Winter DL, et al. Long-term risks of subsequent primary neoplasms among survivors of childhood cancer. JAMA. 2011;305(22):2311–2319. [DOI] [PubMed] [Google Scholar]
- 81. US Department of Health and Human Services, Alliance LYA. Closing the Gap: Research and Care Imperatives for Adolescents and Young Adults with Cancer—Report of the Adolescent and Young Adult Oncology Progress Review Group. Bethesda, MD: National Cancer Institute; 2006. [Google Scholar]
- 82. Travis LB, Beard C, Allan JM, et al. Testicular cancer survivorship: research strategies and recommendations. J Natl Cancer Inst. 2010;102(15):1114–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Li C, Ekwueme DU, Rim SH, et al. Years of potential life lost and productivity losses from male urogenital cancer deaths—United States, 2004. Urology. 2010;76(3):528–535. [DOI] [PubMed] [Google Scholar]
- 84. Vaughn DJ, Palmer SC, Carver JR, et al. Cardiovascular risk in long-term survivors of testicular cancer. Cancer. 2008;112(9):1949–1953. [DOI] [PubMed] [Google Scholar]
- 85. Nuver J, Smit AJ, van der Meer J, et al. Acute chemotherapy-induced cardiovascular changes in patients with testicular cancer. J Clin Oncol. 2005;23(36):9130–9137. [DOI] [PubMed] [Google Scholar]
- 86. Haugnes HS, Aass N, Fossa SD, et al. Components of the metabolic syndrome in long-term survivors of testicular cancer. Ann Oncol. 2007;18(2):241–248. [DOI] [PubMed] [Google Scholar]
- 87. Meinardi MT, Gietema JA, van der Graaf WT, et al. Cardiovascular morbidity in long-term survivors of metastatic testicular cancer. J Clin Oncol. 2000;18(8):1725–1732. [DOI] [PubMed] [Google Scholar]
- 88. Huddart RA, Norman A, Shahidi M, et al. Cardiovascular disease as a long-term complication of treatment for testicular cancer. J Clin Oncol. 2003;21(8):1513–1523. [DOI] [PubMed] [Google Scholar]
- 89. Travis LB, Fossa SD, Schonfeld SJ, et al. Second cancers among 40,576 testicular cancer patients: focus on long-term survivors. J Natl Cancer Inst. 2005;97(18):1354–1365. [DOI] [PubMed] [Google Scholar]
- 90. van den Belt-Dusebout AW, de Wit R, Gietema JA, et al. Treatment-specific risks of second malignancies and cardiovascular disease in 5-year survivors of testicular cancer. J Clin Oncol. 2007;25(28):4370–4378. [DOI] [PubMed] [Google Scholar]
- 91. Fung C, Fossa SD, Beard CJ, et al. Second malignant neoplasms in testicular cancer survivors. J Natl Compr Canc Netw. 2012;10(4):545–556. [DOI] [PubMed] [Google Scholar]
- 92. Bajorin DF. The graying of testis cancer patients: what have we learned? J Clin Oncol. 2007;25(28):4341–4343. [DOI] [PubMed] [Google Scholar]
- 93. National Human Genome Research Institute. A Catalog of Published Genome-Wide Association Studies. http://www.genome.gov/26525384 Accessed Febraury 18, 2014. [Google Scholar]
- 94. Nelson MR, Bacanu SA, Mosteller M, et al. Genome-wide approaches to identify pharmacogenetic contributions to adverse drug reactions. Pharmacogenomics J. 2009;9(1):23–33. [DOI] [PubMed] [Google Scholar]
- 95. Daly AK, Donaldson PT, Bhatnagar P, et al. HLA-B*5701 genotype is a major determinant of drug-induced liver injury due to flucloxacillin. Nat Genet. 2009;41(7):816–819. [DOI] [PubMed] [Google Scholar]
- 96. Travis LB, Holowaty EJ, Bergfeldt K, et al. Risk of leukemia after platinum-based chemotherapy for ovarian cancer. N Engl J Med. 1999;340(5):351–357. [DOI] [PubMed] [Google Scholar]
- 97. Travis LB, Andersson M, Gospodarowicz M, et al. Treatment-associated leukemia following testicular cancer. J Natl Cancer Inst. 2000;92(14):1165–1171. [DOI] [PubMed] [Google Scholar]
- 98. Cavaletti G, Cornblath DR, Merkies IS, et al. The chemotherapy-induced peripheral neuropathy outcome measures standardization study: from consensus to the first validity and reliability findings. Ann Oncol. 2013;24(2):454–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Cavaletti G, Frigeni B, Lanzani F, et al. Chemotherapy-induced peripheral neurotoxicity assessment: a critical revision of the currently available tools. Eur J Cancer. 2010;46(3):479–494. [DOI] [PubMed] [Google Scholar]
- 100. Leonard GD, Wright MA, Quinn MG, et al. Survey of oxaliplatin-associated neurotoxicity using an interview-based questionnaire in patients with metastatic colorectal cancer. BMC Cancer. 2005;5:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Allen PD, Eddins DA. Presbycusis phenotypes form a heterogeneous continuum when ordered by degree and configuration of hearing loss. Hear Res. 2010;264(1–2):10–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. McBride D, Williams S. Characteristics of the audiometric notch as a clinical sign of noise exposure. Scand Audiol. 2001;30(2):106–111. [DOI] [PubMed] [Google Scholar]
- 103. McBride DI, Williams S. Audiometric notch as a sign of noise induced hearing loss. Occup Environ Med. 2001;58(1):46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Mellion M, Gilchrist JM, de la Monte S. Alcohol-related peripheral neuropathy: nutritional, toxic, or both? Muscle Nerve. 2011;43(3):309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Cruickshanks KJ, Klein R, Klein BE, et al. Cigarette smoking and hearing loss: the epidemiology of hearing loss study. JAMA. 1998;279(21):1715–1719. [DOI] [PubMed] [Google Scholar]
- 106. Glendenning JL, Barbachano Y, Norman AR, et al. Long-term neurologic and peripheral vascular toxicity after chemotherapy treatment of testicular cancer. Cancer. 2010;116(10):2322–2331. [DOI] [PubMed] [Google Scholar]
- 107. Broyl A, Corthals SL, Jongen JL, et al. Mechanisms of peripheral neuropathy associated with bortezomib and vincristine in patients with newly diagnosed multiple myeloma: a prospective analysis of data from the HOVON-65/GMMG-HD4 trial. Lancet Oncol. 2010;11(11):1057–1065. [DOI] [PubMed] [Google Scholar]
- 108. Palomar Garcia V, Abdulghani Martinez F, Bodet Agusti E, et al. Drug-induced otoxicity: current status. Acta Otolaryngol. 2001;121(5):569–572. [DOI] [PubMed] [Google Scholar]
- 109. Wheeler HE, Dolan ME. Lymphoblastoid cell lines in pharmacogenomic discovery and clinical translation. Pharmacogenomics. 2012;13(1):55–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Madian AG, Wheeler HE, Jones RB, et al. Relating human genetic variation to variation in drug responses. Trends Genet. 2012;28(10):487–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Welsh M, Mangravite L, Medina MW, et al. Pharmacogenomic discovery using cell-based models. Pharmacol Rev. 2009;61(4):413–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Shukla SJ, Duan S, Badner JA, et al. Susceptibility loci involved in cisplatin-induced cytotoxicity and apoptosis. Pharmacogenet Genomics. 2008;18(3):253–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Duan S, Huang RS, Zhang W, et al. Genetic architecture of transcript-level variation in humans. Am J Hum Genet. 2008;82(5):1101–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Huang RS, Gamazon ER, Ziliak D, et al. Population differences in microRNA expression and biological implications. RNA Biol. 2011;8(4):692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Moen EL, Zhang X, Mu W, et al. Genome-wide variation of cytosine modifications between European and African populations and the implications for complex traits. Genetics. 2013;194(4):987–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Wheeler HE, Gamazon ER, Stark AL, et al. Genome-wide meta-analysis identifies variants associated with platinating agent susceptibility across populations. Pharmacogenomics J. 2013;13(1):35–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Cox NJ, Gamazon ER, Wheeler HE, et al. Clinical translation of cell-based pharmacogenomic discovery. Clin Pharmacol Ther. 2012;92(4):425–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Manolio TA, Collins FS, Cox NJ, et al. Finding the missing heritability of complex diseases. Nature. 2009;461(7265):747–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Eichler EE, Flint J, Gibson G, et al. Missing heritability and strategies for finding the underlying causes of complex disease. Nat Rev Genet. 2010;11(6):446–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Lee SH, Wray NR, Goddard ME, et al. Estimating missing heritability for disease from genome-wide association studies. Am J Hum Genet. 2011;88(3):294–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. O’Donnell PH, Bush A, Spitz J, et al. The 1200 patients project: creating a new medical model system for clinical implementation of pharmacogenomics. Clin Pharmacol Ther. 2012;92(4):446–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Bell GC, Crews KR, Wilkinson MR, et al. Development and use of active clinical decision support for preemptive pharmacogenomics. J Am Med Inform Assoc. 2014;21(e1):e93–99. 10.1136/amiajnl-2013-001993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Wetterstrand KA. DNA Sequencing costs: data from the NHGRI Genome Sequencing Program (GSP). http://www.genome.gov/sequencingcosts/ Accessed February 18, 2014.
- 124. Wheeler HE, Aquino-Michaels K, Gamazon ER, et al. Poly-omic prediction of complex traits: OmicKriging. http://arxiv.org/abs/1303.1788 Accessed February 18, 2014. [DOI] [PMC free article] [PubMed]
- 125. Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53(24):2231–2247. [DOI] [PubMed] [Google Scholar]
- 126. de Haas EC, Oosting SF, Lefrandt JD, et al. The metabolic syndrome in cancer survivors. Lancet Oncol. 2010;11(2):193–203. [DOI] [PubMed] [Google Scholar]
- 127. Tichelli A, Socie G. Considerations for adult cancer survivors. Hematology Am Soc Hematol Educ Program 2005;516–22. [DOI] [PubMed] [Google Scholar]
- 128. Sakoda LC, Jorgenson E, Witte JS. Turning of COGS moves forward findings for hormonally mediated cancers. Nat Genet. 2013;45(4):345–348. [DOI] [PubMed] [Google Scholar]
- 129. Gadalla SM, Lund M, Pfeiffer RM, et al. Cancer risk among patients with myotonic muscular dystrophy. JAMA. 2011;306(22):2480–2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Braun S, Bitton-Worms K, LeRoith D. The link between the metabolic syndrome and cancer. Int J Biol Sci. 2011;7(7):1003–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Khandekar MJ, Cohen P, Spiegelman BM. Molecular mechanisms of cancer development in obesity. Nat Rev Cancer. 2011;11(12):886–895. [DOI] [PubMed] [Google Scholar]
- 132. Travis LB, Gospodarowicz M, Curtis RE, et al. Lung cancer following chemotherapy and radiotherapy for Hodgkin’s disease. J Natl Cancer Inst. 2002;94(3):182–192. [DOI] [PubMed] [Google Scholar]
- 133. Travis LB, Ng AK, Allan JM, et al. Second malignant neoplasms and cardiovascular disease following radiotherapy. J Natl Cancer Inst. 2012;104(5):357–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Ng AK, Kenney LB, Gilbert ES, et al. Secondary malignancies across the age spectrum. Semin Radiat Oncol. 2010;20(1):67–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Li FP, Stovall EL. Long-term survivors of cancer. Cancer Epidemiol Biomarkers Prev. 1998;7(4):269–270. [PubMed] [Google Scholar]
- 136. World Bank. Health expenditure, total (% of GDP). http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS Accessed February 18, 2014. [Google Scholar]
- 137. GTEx Consortium. The Genotype-Tissue Expression (GTEx) project. Nat Genet. 2013;45(6):580–585. [DOI] [PMC free article] [PubMed] [Google Scholar]