Abstract
Background
The National Weight Control Registry (NWCR) was established to examine characteristics of successful weight loss maintainers. This study compares the diet and behavioral characteristics and weight regain trajectories of NWCR members with differing physical activity (PA) levels at baseline.
Methods
Participants (n=3591) were divided into 4 levels of self-reported PA at registry entry (<1000, 1000 to <2250, 2250 to <3500, and ≥3500 kcals/week). We compared self-reported energy intake (EI), macronutrient composition, eating behaviors (dietary restraint, hunger, and disinhibition), weight loss maintenance strategies, and 3 year weight regain between these 4 activity groups.
Results
Those with the highest PA at registry entry had lost the most weight, and reported lower fat intake, more dietary restraint, and greater reliance on several specific dietary strategies to maintain weight loss. Those in the lowest PA category maintained weight loss despite low levels of PA and without greater reliance on dietary strategies. There were no differences in odds of weight regain at year 3 between PA groups.
Conclusions
These findings suggest that there is not a “one size fits all strategy” for successful weight loss maintenance and that weight loss maintenance may require the use of more strategies by some individuals than others.
Keywords: Obesity, Physical Activity, Weight Loss Maintenance, Weight Regain, Weight Management
Background
The NWCR, established in 1993, is an ongoing longitudinal study of successful weight loss maintainers and is a unique resource for evaluating associations between diet and activity and weight regain over time. Previous studies have shown that National Weight Control Registry (NWCR) members report high levels of physical activity: 2621 ± 2255 kcals per week (1). However, as suggested by the large standard deviation in self-reported activity, there is significant inter-individual variability in amount of activity reported by NWCR subjects. Based on data obtained at registry entry, almost a quarter of NWCR subjects (25.3%) report < 1000 kcal/wk and over a third (34.9%) report > 3000 kcal/wk (1). Substantial individual variability in activity level was also observed in a small sub-study in which activity was objectively measured using accelerometers (2). On average, NWCR subjects in the sub-study engaged in 41.5 ± 35.1 min/day (or roughly 290 minutes per week) of sustained (bouts ≥ 10 minutes) moderate-to-vigorous physical activity (MVPA). However, nearly a third (31%) engaged in < 150 minutes per week of sustained MVPA, while nearly a quarter (23%) engaged in > 420 minutes per week.
Although never examined in the NWCR at large, it appears that a subset of individuals is able to maintain a weight loss with relatively low levels of activity, while others may require significantly higher levels of activity. Moreover, the characteristics and weight control strategies of individuals maintaining weight loss with differing levels of activity has never been evaluated. Dietary habits (energy intake, macronutrient composition of the diet, and eating behaviors) may contribute to the variability in the amount of activity required for weight loss maintenance. We hypothesized that those reporting lower levels of PA might rely more on dietary strategies (i.e. report lower energy intake, lower fat intake, and more restrained eating) to maintain their weight loss as compared to those reporting higher levels of PA, and thus would not differ from higher exercisers in terms of long term weight maintenance success. The aim of this study was to compare eating behaviors, weight control behaviors, and 3 year weight maintenance success among NWCR members reporting low, medium, high and very high levels of physical activity.
Methods
Participants
Participants were 3591 (868 men and 2723 women) who enrolled in the NWCR between 1993 and 2004, had lost weight without bariatric surgery, and had complete self-reported physical activity data at entry into the NWCR. To be eligible for enrollment, an individual must be ≥ 18 years old, and have maintained a weight loss ≥13.6 kg (30 lbs) for ≥ one year. NWCR members were recruited through coverage of the NWCR provided by local and national media sources describing the registry and its entry criteria, physician and dietitian referrals, mailings sent by several commercial weight loss programs to their current members, and articles placed in health newsletters and magazines. Interested individuals were directed to call a 1-800 number or visit the study website to receive NWCR enrollment information. A consent form (approved by The Miriam Hospital Institution Review Board) and questionnaire packets were then sent to these subjects. Entry into the registry was based on self-reported height, weight and weight change.
Measures
Data were collected at initial enrollment into the NWCR and at 3 year follow up. Registry members complete questionnaire-based assessments of weight and/or behavioral factors. These questionnaires include the core measures of physical activity (Paffenbarger Physical Activity Questionnaire) (3), dietary intake (Block Food Frequency Questionnaire) (4), and eating behaviors (Eating Inventory) (5) used for the analysis in this study. These core measures were chosen at registry inception in 1993, and have remained stable over time. Compensation for completing the questionnaires was not provided.
Demographics and Weight
Participants were asked to provide basic demographic information (age, gender, ethnicity, education level and marital status) and details about weight history (current weight and current height, maximum adult weight, duration of maintenance of required minimum 13.6 kg weight loss). Using this information, current and maximum body mass index (BMI; in kg/m2) was calculated. In addition, weight change (i.e. magnitude of weight loss) was calculated as the maximum pre-enrollment weight minus the enrollment weight for each subject. Three year weight regain was calculated as the enrollment weight minus the weight reported at year 3. The reliability and validity of NWCR subjects self-reported weight information has been documented previously by McGuire et al (6). A sub-sample (n=95) of NWCR participants were asked to report their maximum and current weight information again 1-2 months after registry entry. Correlations between the reports of maximum and current weight were high (0.98 and 0.99 respectively, p <0.01 for both) (6). Self-reported measures of maximum weight (n=307) and current weight (n=407) were also compared with documentation of weight provided by a physician or weight loss counselor. Correlations between self-reported and documented maximum weight and current weight were also high (0.97 and 0.98 respectively, p <0.001 for both) with a mean weight discrepancy of 2.4 kg for maximum weight and 0.7 kg for current weight (6).
Physical Activity
Physical activity (PA) was assessed using the Paffenbarger Physical Activity Questionnaire (3). This measure yields estimates of total energy expended in leisure time PA per week. This questionnaire has been shown to have high test-retest reliability (7) and has been found to be significantly correlated with physiologic measures known to be affected by PA including measures of cardiovascular fitness (7, 8). Participants are asked to report their activity for the previous week (if the previous week was “unusual”, they are asked to report data for a “typical” week). Specifically they are asked to quantify flights of stairs they climbed on average each day, blocks they walked on average each day, as well as any sports, recreational, or physical activities they participated in during the past week. An estimate of the weekly energy expended through leisure time PA was calculated using the scoring system devised for this questionnaire as described by Paffenbarger and colleagues (3) in which kilocalories scores are assigned for each of these three components (blocks walked, flights of stairs climbed, and sports/recreational activities). The kilocalorie values assigned for blocks, flights and sports/recreational activities are derived from a 68 kg (150 lb) male, and there is no correction factor for gender or body weight. Thus, the calculation of Paffenbarger activity kcals/wk is the same for all individuals regardless of gender or body weight. A detailed description of the scoring and coding methods used in the NWCR as well as the cut off values used to eliminate implausible data points has been described previously (9). Because the Paffenbarger activity kcals/wk are not adjusted for gender or body weight we chose to divide subjects into relative levels of activity, rather than rely on absolute kcal values in our analyses. Data from the Paffenbarger questionnaire were thus used to divide subjects into four levels of self-reported PA as follows: low (<1000 kcal/wk, n=910), medium (1000 to <2500 kcal/wk, n=934), high (2250 to <3500 kcal/wk, n=779) and very high (3500+ kcal/wk, n=968). These activity levels were chosen based on rough correspondence to levels of activity we thought were clinically relevant to current activity guidelines for general health (30 min/day) and for weight loss/maintenance (60 min/day) (10). Assuming moderate intensity activity of 5-6 kcals per minute, these activity levels equated to < 30 min per day (low), 30-60 min per day (medium), 60-90 min per day (high) and > 90 min per day (very high).
Dietary Intake
Dietary intake was assessed with the Block Food-Frequency Questionnaire (Block FFQ) (4). Energy and macronutrient intakes from the Block FFQ have been shown to correlate significantly (p<0.01) with 4-day food records (11). Data were used to calculate total energy intake (kcals/day) and intake of macronutrients (fat, CHO and protein) in absolute (grams) and relative (% daily energy) terms. Under-reporting of energy intake (EI) is recognized as a common problem when intake is assessed by self-report (12). As in prior studies in the NWCR (13), basal metabolic rate (BMREST) was estimated using the Harris-Benedict equation (14) and we classified participants with a EI/BMREST < 0.9) as under-reporters (15, 16).
Eating Behavior
The Eating Inventory (5) was used to assess 3 dimensions of eating behavior: cognitive restraint (degree of conscious control over eating), disinhibition (susceptibility to loss of control over eating), and hunger (subjective feelings of hunger and food cravings). Within cognitive restraint, subscales of flexible and rigid control were also scored (17). All three scales as well as the two subscales have been shown to have good test-retest reliability and internal consistency (5, 17, 18).
Weight Loss Maintenance Strategies and Perceptions of Difficulty in Maintaining Weight
At enrollment, NWCR participants were asked to provide a detailed weight-loss history including questions about the participant's current weight control strategies and perceptions about weight loss maintenance. Participants were asked to indicate whether they had used a specific strategy to maintain or lose weight during the past year. Participants were also asked to report the number of days per week they eat breakfast, the number of fast food meals they eat per week, and whether they are currently using a liquid formula (e.g. Optifast or Slim-fast). Participants were also asked to indicate on a scale of 1-7 (where 1 is extremely easy and 7 is extremely hard) how difficult it is to maintain their weight and to indicate on a scale of 1-8 (where 1 is not important at all and 8 is extremely important) how important it is to them to follow their exercise routine and follow their diet routine.
Statistical Analysis
All analyses were conducted using SAS Version 9.3 (SAS Institute Inc., Cary, NC, USA.) Pearson's chi-square tests were used for an overall comparison of demographic characteristics (ethnicity, marital status, education level) across groups reporting different levels of activity at enrollment. General linear models (ANCOVA) were used to estimate adjusted means for continuous variables and test for between-group differences across the four groups reporting different levels of activity at enrollment. Subject characteristics for the overall sample and unadjusted group means are presented as mean ± standard deviation, adjusted means as mean ± standard error. Weight characteristics, weight loss methods/strategies and results from the Block FFQ and the Eating Inventory were adjusted to the sample mean age and proportion male. Contrast statements were used to test for linear trends across activity groups and to identify significant pairwise differences, using a Bonferroni adjustment for multiple comparisons. Analyses were repeated for men and women separately; patterns across PA categories were similar so only the combined data is presented. Supplemental analyses were also performed excluding EI under-reporters (EI/BMRest < 0.9) (15, 16). General linear models were also used to examine 3-year weight regain by activity level and caloric intake at baseline, as well as to examine 3 year weight regain by change in activity level and caloric intake from baseline to year 3. The analyses of weight regain were adjusted for enrollment weight, in addition to age and gender, to examine the effects of activity level and caloric intake independent of their relationship to enrollment weight. To utilize all potential data, available case analyses were performed using all available data for each variable at each time point. The median number of cases available for each group of variables is reported in the respective tables. Missing weight data at 3 years was characterized by baseline levels of physical activity and caloric intake and is reported in the results section below.
Results
Missing and Incomplete Data
The 3591 subjects included in the study had complete baseline Paffenbarger data. Of these, 7% had incomplete baseline Block FFQ data. The maximum amount of missing data was 13% for variables regarding eating behaviors and 19% for variables related to weight loss maintenance strategies and perceptions. The overall response rate at 3-years was 77%, with no notable differences by baseline activity or caloric intake. Of these, 3% were missing complete 3 year Paffenbarger data and 13% were missing complete 3 year Block FFQ data.
Subject Characteristics
Participants averaged (mean ± SD) 46.8 ±12.4 years of age; 95.5% were Caucasian and the majority were married (64.4%), and highly educated (60.7% have a college degree or higher). BMI reported at registry entry was 25 ±4.6 and maximum (pre weight loss) BMI was 36.3 ±8.1. Weight loss reported on registry entry was 32.3 ± 16.7 kg and weight maintenance duration of the 13.6 kg minimum weight loss was 5.7±7.4 years. Average weekly energy expenditure on registry entry was 2621 ± 2252 kcal/wk and average daily energy intake on registry entry was 1400±584 kcals/day.
Subject characteristics as well as mean and median level of energy expenditure within the 4 levels of activity level are shown in Table 1. About one fourth of the participants were within each of the 4 categories. Within the higher activity levels, there was a higher percentage of male subjects (p for linear trend <0.0001), a lower average age of subjects (p for linear trend 0.002), and a higher percentage of unmarried and highly educated subjects (p for linear trend <0.0001). There were no significant differences in ethnicity across activity level category. Percent of subjects in the lowest activity group who were smokers (∼13%) was approximately twice that seen in the other activity groups.
Table 1. Participant Characteristics at National Weight Control Registry Enrollment by Self-Reported Physical Activity Level.
| Total Kcals/Week PA at Enrollment | P-Value for Linear Trend† | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| <1000 (n = 910) | 1000-<2250 (n = 934) | 2250-<3500 (n = 779) | 3500+ (n = 968) | |||
| Weekly Energy Expenditure (kcal/day) Mean ±SE (Median) | 416.13±10.40 (364) | 1614.55±11.62 (1602) | 2255.92±19.85 (2850) | 5476.87±70.04 (4853) | <0.0001 | |
|
| ||||||
| Age * | 49.39 ±13.02 | 47.94 ±12.74 | 45.51 ±11.97 | 44.35 ±11.26 | <.0001 | |
| Gender | Female | 78.4% | 78.5% | 73.9% | 72.4% | .002‡ |
| Male | 21.6% | 21.5% | 26.1% | 27.6% | ||
| Ethnicity | Caucasian | 95.6% | 95.6% | 96.1% | 94.7% | .751⊥ |
| African-American | 2.3% | 2.3% | 1.7% | 1.8% | ||
| Asian | .1% | .2% | .4% | .4% | ||
| Hispanic | 1.1% | 1.1% | 1.2% | 1.8% | ||
| Other | .9% | .9% | .6% | 1.3% | ||
| Marital Status | Married | 66.5% | 64.7% | 65.7% | 61.1% | <.0001⊥ |
| Separated | 1.2% | 2.4% | 1.8% | 1.4% | ||
| Divorced | 12.0% | 12.4% | 10.4% | 11.1% | ||
| Widowed | 5.2% | 3.5% | 2.1% | 2.0% | ||
| Never married | 12.0% | 13.0% | 15.6% | 18.5% | ||
| Not married (living w/significant other) | 2.7% | 3.4% | 3.6% | 4.2% | ||
| Other | .4% | .5% | .9% | 1.7% | ||
| Education Level | Grade school | .0% | .0% | .0% | .0% | <.0001⊥ |
| Junior high school | .2% | .2% | .3% | .0% | ||
| High school | 15.3 | 10.3% | 7.2% | 6.5% | ||
| Vocational training | 7.9% | 5.6% | 4.2% | 5.3% | ||
| Some college (< 4 yrs) | 27.2% | 22.8% | 21.2% | 22.2% | ||
| College/university degree | 23.9% | 26.1% | 29.6% | 30.7% | ||
| Graduate or professional | 25.4% | 35.0% | 37.5% | 35.3% | ||
| Enrollment Weight (kg) †† | 73.47±0.48 | 71.93±0.47 | 70.98±0.52 | 70.12±0.46 | <.0001 | |
| Enrollment BMI (kg/m²)†† | 25.77±0.15 | 25.20±0.15 | 24.68±0.17 | 24.51±0.15 | <.0001 | |
| Maximum Pre-Enrollment Weight (kg) †† | 104.33±0.83 | 103.75±0.81 | 103.51±0.89 | 105.14±0.80 | .553 | |
| Maximum Pre-Enrollment BMI (kg/m²)†† | 36.69±0.27 | 36.36±0.27 | 36.05±0.29 | 36.76±0.27 | .940 | |
| Weight Change (Maximum-Enrollment, kg) †† | 30.86±0.55 | 31.82±0.54 | 32.07±0.60 | 35.02±0.54 | <.0001 | |
| Weight Maintenance Duration (months) †† | 67.26±2.90 | 65.96±2.85 | 68.95±3.14 | 70.22±2.82 | .359 | |
| Smoker (%) | 12.72±0.97 | 7.50±0.95 | 6.44±1.04 | 6.52±0.94 | <.0001 | |
Data reported as mean ± standard deviation
p-values calculated from a general linear model with polynomial contrasts.
p-values calculated from logistic regression model with polynomial contrasts
Pearson's chi-square p-value
Data reported as mean ± standard error, adjusted to the sample mean age and proportion male estimated using a general linear model.
Enrollment body weight in subjects reporting very high levels of activity (3500+ kcal/week) was on average 3.4 kg lower than those reporting low levels of activity (<1000 kcal/wk) after adjustment for age and gender (p for linear trend <0.0001). Maximum pre-enrollment BMI and body weight (adjusted for age and gender) were not significantly different across activity level category (p for linear trend 0.553). There were also no significant differences in weight maintenance duration across activity groups (p for linear trend 0.359). However, amount of weight loss (maximum pre-enrollment body weight minus enrollment body weight) was significantly greater in subjects reporting higher levels of activity (p for linear trend <0.0001). Those subjects reporting very high levels of activity (>3500 kcal/week) were maintaining on average a 4.2 kg greater weight loss than those reporting low levels of activity (<1000 kcal/wk) after adjustment for age and gender.
Dietary Intake
Energy intake (mean ± SE) within activity category at entry into the NWCR is shown in Table 2. After adjusting for age and gender, a significant non-linear U shaped relationship was observed for calories (1440.25±19.36, 1384.53±18.73, 1373.55±21, 1438.18±18.51 kcals/day, overall p 0.0190, p for linear trend 0.8408) with higher EI in those reporting the lowest and highest levels of activity. However, pairwise comparisons using a Bonferroni adjustment for multiple comparisons found no significant differences among the 4 groups. Data were also similar when repeated for kcal/kg/day (Table 2).
Table 2. Dietary Habits (Estimated Mean±SE) By Level of Physical Activity at Enrollment*.
| Level of Physical Activity at Enrollment (kcals/week) | p-value | |||||
|---|---|---|---|---|---|---|
| <1000 (n = 826) ŧ | 1000-2249 (n=876) | 2250-3499 (n=731) | ≥3500 (n=905) | Overall | Linear Trend | |
| Calories (kcals/day) | 1440.25 ±19.36 | 1384.53±18.73 | 1373.55±20.47 | 1438.18±18.53 | 0.0190 | 0.8408 |
| Calories (kcals/kg/day) | 20.03±0.29 | 19.68±0.28 | 19.76±0.31 | 20.85±0.28 | 0.0137 | 0.0511 |
| Protein (grams/day) | 68.51±1.03 | 64.69±0.99 | 63.29±1.09 | 66.97±0.98 | 0.0017 | 0.1829 |
| Fat (grams/day) | 56.36±1.16 | 46.99±1.12 | 42.62±1.23 | 42.14±1.11 | <.0001 | <.0001 |
| Carbohydrate (grams/day) | 158.72±2.85 | 169.15±2.76 | 178.39±3.02 | 191.62±2.73 | <.0001 | <.0001 |
| % Calories from Fat | 33.41±0.42 | 29.07±0.41 | 27.14±0.45 | 25.66±0.40 | <.0001 | <.0001 |
| % Calories from Protein | 19.08±0.15 | 18.88±0.15 | 18.66±0.16 | 18.87±0.15 | 0.3230 | 0.2146 |
| % Calories from Carbohydrate | 45.77±0.49 | 50.09±0.47 | 52.54±0.52 | 53.88±0.47 | <.0001 | <.0001 |
| % Calories from Sweets | 5.05±0.21 | 5.19±0.20 | 5.31±0.22 | 4.21±0.20 | 0.0003 | 0.0082 |
Data reported as mean ± standard error, adjusted to the sample age and gender (age = 46.8; proportion male = 24%) estimated using a general linear model.
Linear trend p-values calculated using polynomial contrasts
7% of participants were missing Block FFQ.
Macronutrient content of the diet within activity category is shown in Table 2. After adjusting for age and gender, percent calories from fat showed a linear relationship, with those reporting higher levels of activity reporting lower levels of dietary fat (p for linear trend <0.0001). A similar pattern was observed with total fat grams (p for linear trend <0.0001). Percent of calories from CHO also showed linear relationship with those reporting higher levels of activity reporting higher intake of CHO (p for linear trend <0.0001). Percent calories from protein was not different between groups (overall p 0.3230).
Supplemental analyses were conducted excluding individuals classified as under-reporters based on an EI/BMREST ratio of < 0.9. With this definition, 54% of subjects (n=1921) were classified as under-reporters. The percent subjects classified as under-reporters did not differ between 4 activity groups. Analyses of dietary intake were repeated excluding individuals classified as under-reporters and yielded the same statistical conclusions.
Eating Behaviors
Dimensions of eating behaviors are shown in Table 3. Cognitive restraint (measured on a scale of 0-21) increased linearly such that those reporting higher levels of activity scored higher on this measure (p for linear trend < 0.0001). Short forms of flexible and rigid control subscales showed a similar pattern (p for linear trend < 0.0001 for both). Levels of disinhibition (measured on a scale of 0-16) and hunger (measured on a scale of 0-14) were not significantly different between groups (overall p 0.1308 and 0.1720 respectively).
Table 3. Eating Behaviors (Estimated Mean±SE) By Level of Physical Activity at Enrollment*.
| Level of Physical Activity at Enrollment (kcals/week) | p-value | |||||
|---|---|---|---|---|---|---|
| <1000 (n = 806) | 1000-2249 (n=819) | 2250-3499 (n=696) | ≥3500 (n=838) | Overall | Linear Trend | |
| Cognitive Restraint | 13.94±0.13 | 15.04±0.13 | 15.28±0.14 | 15.69±0.13 | <.0001 | <.0001 |
| Disinhibition | 6.56±0.12 | 6.95±0.12 | 6.89±0.13 | 6.74±0.12 | 0.1308 | 0.4016 |
| Flexible Control | 4.53±0.06 | 4.90±0.06 | 5.00±0.06 | 5.17±0.06 | <.0001 | <.0001 |
| Rigid Control | 4.44±0.06 | 4.91±0.05 | 5.10±0.06 | 5.21±0.05 | <.0001 | <.0001 |
| Hunger | 4.36±0.11 | 4.66±0.11 | 4.67±0.12 | 4.57±0.11 | 0.1720 | 0.1905 |
Data reported as mean ± standard error, adjusted to the sample age and gender (age = 46.8; proportion male = 24%) estimated using a general linear model.
Linear trend p-values calculated using polynomial contrasts
Median sample size for variables shown. Maximum of 13% missing for any one variable.
Weight Loss Maintenance Strategies and Perceptions of Difficulty in Maintaining Weight
Strategies and perceptions related to weight loss maintenance over the past year were compared between groups and adjusted for age and gender and enrollment weight (Table 4). Those reporting higher levels of PA were more likely to report using a variety of different weight loss strategies compared to those with lower physical activity levels. Those reporting higher levels of PA also reported fewer fast food meals per week and more frequent consumption of breakfast (p for linear trend <0.0001 for both). There was no significant linear trend across activity groups in the percent of participants who reported weighing themselves on a regular basis or in the percent in the percent of participants who reported they joined or continued to participate in any weight loss or weight loss maintenance program (p for linear trend 0.2168 and 0.1838 respectively). Those reporting higher levels of PA indicated greater difficulty maintaining weight (p for linear trend 0.0021) and a greater importance of both following their diet regimen (p for linear trend <0.0001) and following their exercise routine (p for linear trend <0.0001).
Table 4. Weight Loss Maintenance Strategies and Perceptions (Estimated Mean±SE) By Level of Physical Activity at Enrollment*.
| Level of Physical Activity at Enrollment (kcals/week) | p-value | |||||
|---|---|---|---|---|---|---|
| <1000 (n = 732) | 1000-2249 (n=761) | 2250-3499 (n=655) | ≥3500 (n=769) | Overall | Linear Trend | |
| Strategies Used For Weight Loss Maintenance Over the Past Year | ||||||
| Kept few high-fat foods in house (%) | 67.66 +1.58 | 76.87 +1.54 | 80.74 +1.66 | 80.17 +1.54 | <.0001 | <.0001 |
| Kept healthy foods in house (%) | 90.47 +0.83 | 94.73 +0.81 | 96.28 +0.87 | 97.15 +0.81 | <.0001 | <.0001 |
| Decreased restaurant meals (%) | 46.24 +1.86 | 48.77 +1.82 | 52.82 +1.96 | 50.70 +1.82 | 0.0915 | 0.0362 |
| Contact with normal weight friends (%) | 21.03 +1.59 | 25.52 +1.55 | 21.99 +1.67 | 27.11 +1.55 | 0.0189 | 0.0386 |
| Contact with friends who exercise (%) | 26.04 +1.80 | 40.81 +1.75 | 44.57 +1.89 | 55.28 +1.75 | <.0001 | <.0001 |
| Keep picture of self (%) | 30.79 +1.74 | 32.69 +1.70 | 30.97 +1.83 | 38.19 +1.69 | 0.0067 | 0.0084 |
| Weigh self regularly (%) | 86.78 +1.16 | 90.41 +1.13 | 90.16 +1.22 | 89.00 +1.13 | 0.1052 | 0.2168 |
| Keep written food record (%) | 41.97 +1.83 | 57.64 +1.79 | 60.16 +1.93 | 59.22 +1.79 | <.0001 | <.0001 |
| Purchase books/magazines related to nutrition or exercise (%) | 62.94 +1.63 | 71.69 +1.59 | 76.11 +1.71 | 80.28 +1.59 | <.0001 | <.0001 |
| Participate in weight loss or maintenance program(s) (%) | 36.44 +1.78 | 41.38 +1.73 | 38.80 +1.87 | 33.78 +1.73 | 0.0142 | 0.1838 |
| Currently use liquid formula (%) | 7.81±0.96 | 6.89±0.95 | 11.84±1.03 | 10.52±0.93 | 0.0009 | 0.0023 |
| Consume breakfast (days/week) | 6.00 +0.06 | 6.35 +0.06 | 6.41 +0.06 | 6.40 +0.05 | <.0001 | <.0001 |
| Fast food meals per week | 0.94 +0.05 | 0.73 +0.05 | 0.63 +0.05 | 0.60 +0.05 | <.0001 | <.0001 |
| Perceptions Related to Weight Loss Maintenance Over the Past Year | ||||||
| Difficulty Maintaining Weight (1-7) | 3.71±0.04 | 3.82±0.04 | 3.93±0.05 | 3.87±0.04 | 0.0048 | 0.0021 |
| Importance of Exercise (1-8) | 5.80±0.05 | 7.13±0.05 | 7.46±0.06 | 7.66±0.05 | <.0001 | <.0001 |
| Importance of Diet (1-8) | 7.03±0.05 | 7.23±0.04 | 7.31±0.05 | 7.33±0.04 | <.0001 | <.0001 |
Data reported as mean ± standard error, adjusted to the sample age and gender (age = 46.8; proportion male = 24%) estimated using a general linear model.
Linear trend p-values calculated using polynomial contrasts
Median sample size for variables shown. Maximum of 19% missing for any one variable.
3 Year Weight Regain
Average (mean ± SD) weight regain in the overall sample over three years of follow-up (adjusted for age and gender) was 5.1±8.9 kg or 16.1±26.1% of initial weight loss. In analyses that adjusted for age, gender and enrollment weight, we found no difference in 3 year weight regain by PA category at registry entry (Table 5, n=2564 subjects with complete Paffenbarger and Block FFQ data at registry entry, and weight regain data at year 3). Similarly, across 4 levels of reported daily EI: <1000 kcal (n=617), 1000-1300 kcals (n=649), 1300-1700 kcals (n=680), and > 1700 kcals (n=618), no significant effect was observed (Table 5). We repeated these analysis dividing subjects into 4 levels of reported % calories from fat: <20% (n=630), 20-27.5% (n=818), 27.5-35% (n=618), and >35% (n=498) and found no differences in weight regain by baseline level of fat intake (p 0.6122, data not shown).
Table 5. Estimated 3 Year Weight Regain (Mean±SE) by Levels of Caloric Intake and Physical Activity at Enrollment*.
| Caloric Intake at Enrollment (kcals) | Level of Physical Activity at Enrollment (kcals/week) | ||||
|---|---|---|---|---|---|
| <1000 (n=615) | 1000-2249 (n=672) | 2250-3499 (n=589) | ≥3500 (n=688) | Combined | |
| < 1000 (n=617) | 5.17±0.70 | 5.58±0.68 | 5.30±0.77 | 5.75±0.69 | 5.45±0.36 |
| 1000-1300 (n=649) | 5.39±0.72 | 4.39±0.68 | 5.98±0.66 | 5.35±0.70 | 5.28±0.35 |
| 1300-1700 (n=680) | 4.68±0.70 | 4.42±0.63 | 5.29±0.74 | 5.13±0.63 | 4.88±0.34 |
| >1700 (n=618) | 5.65±0.71 | 4.73±0.72 | 5.23±0.73 | 5.59±0.67 | 5.30±0.36 |
| Combined | 5.22±0.36 | 4.78±0.34 | 5.45±0.36 | 5.45±0.34 | |
Data reported as mean ± standard error, adjusted for Gender (24% male), Age (46.8), Enrollment Weight (71.4 kg) estimated using a general linear model, Linear trend p-values calculated using polynomial contrasts.
Expenditure: p = .4632; p = .3818 Linear Trend
Intake: p = .6794; p = .6099 Linear Trend
Expenditure*Intake: p = .9733
n=2564 with complete Paffenbarger and Block FFQ data at registry entry, and weight regain data at year 3
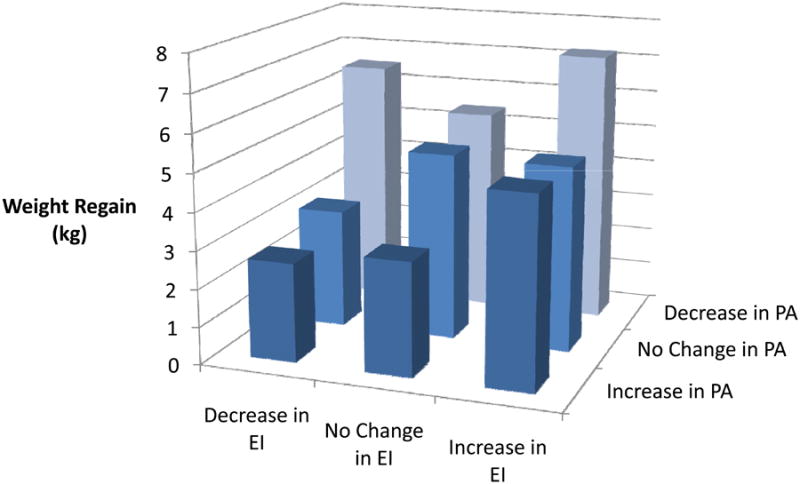
We examined the impact of change in reported level of PA and EI from registry entry to year 3 on weight regain (Table 6 and Figure 1, n= 2155 subjects with complete Paffenbarger, Block FFQ, and weight data at registry entry and year 3). Approximately 44% of participants decreased PA (defined as a decrease of > 500 kcal/week) and approximately 36% increased EI (defined as an increase of > 150 kcals/day) over the 3 year follow up period. Although baseline levels of PA and EI were not predictive of weight regain, greater weight regain was observed in those with detrimental changes in PA (p <0.0001) and EI (p=0.0002) over time. Looking at the combined impact of these changes, those who both decreased PA and increased EI regained the most weight (mean ± SE 7.2 ± 0.45 kg) over the 3 year follow up period. Those who both increased PA and decreased EI regained the least weight (mean ± SE 2.63 ± 0.60 kg) over the 3 year follow up period.
Table 6. Estimated 3 Year Weight Regain By 3 Year Change in Energy Intake and Physical Activity*.
| Change in Energy Intake (kcals/day) | Change in Physical Activity (kcals/week) | ||||
|---|---|---|---|---|---|
| < -500 | -500 to +500 | >500+ | Combined | Linear Trend (effect of EE within EI) | |
| <-150 | 6.52±0.46 (n=322) | 3.16±0.53 (n=234) | 2.63±0.60 (n=183) | 4.10±0.31 (n=739) | <.0001 |
| -150 to +150 | 5.42±0.48 (n=286) | 4.97±0.58 (n=200) | 3.01±0.64 (n=162) | 4.47±0.34 (n=648) | .0024 |
| >+150 | 7.20±0.45 (n=328) | 4.92±0.51 (n=252) | 5.02±0.59 (n=188) | 5.71±0.30 (n=768) | .0032 |
| Combined | 6.38±0.27 (n=936) | 4.35±0.32 (n=686) | 3.55±0.36 (n=533) | ||
| Linear Trend (effect of EI within EE) | .2848 | .0166 | .0044 | ||
Data reported as mean ± standard error, adjusted for Gender (24% male), Age (46.8), Enrollment Weight (71.4 kg) estimated using a general linear model, Linear trend p-values calculated using polynomial contrasts
Expenditure: p <0.0001 ; p <0.0001 Linear Trend
Intake: p =0.0004; p =0.0002 Linear Trend
Expenditure*Intake: p = .0387
n= 2155 with complete data (Paffenbarger, Block FFQ, and weight) at registry entry and year 3.
Figure 1. Estimated 3 Year Weight Regain by 3 Year Change in Energy Intake (EI) and Physical Activity (PA).
Discussion
We found that participants reporting higher levels of physical activity appear to report more extreme behaviors to maintain their weight loss across many domains. Those reporting higher levels of PA reported engaging in more dietary weight control behaviors (including a lower intake of dietary fat, and a greater degree of cognitive restraint) and relying to a greater degree on several specific dietary strategies to maintain their weight loss. Despite a higher level of reported activity, self-reported EI was not significantly higher in the high PA group, even when differences in body weight between groups were accounted for by comparing EI in kcals/kg/day. Thus, those who report higher activity maintain their body weight with similar levels of dietary restriction as those with less activity.
At enrollment, higher levels of PA were associated with greater amounts of weight loss and a lower body weight; those in the highest PA group weighed on average 3.3 kg less than those in the lowest PA group and were maintaining a 4.2 kg greater weight loss. This is consistent with prior interventional and observational studies (19-22) and suggests that greater magnitude of weight loss is maintained with higher levels of physical activity. These finding are also consistent with research that suggest that while PA is important for weight loss maintenance, it does not function independently of eating behaviors and that both sides of the energy balance equation may be important in successful weight loss maintenance (19). Given the greater weight loss achieved in this group, it is likely that the high use of multiple weight control strategies (and not solely the high PA) that allowed this group to achieve greater success.
Interestingly, those in the higher PA groups also perceive weight loss maintenance to be more difficult, and place greater importance on following both their diet regimen and exercise routine suggesting that this may be a group from who weight loss maintenance may be more difficult and thus requires the use of multiple strategies. Recent studies suggest that physiologic changes favoring the regain of lost weight persist well beyond the period of dynamic weight loss. Both a decline in 24-hour energy expenditure greater than that expected due to weight loss alone (23) and alterations in circulating hormonal mediators of appetite (24) have been shown to persist in persons who have maintained a reduced body weight for more than 1 year. Perhaps individuals in the higher PA groups may have a stronger biological adaptation to weight loss and thus require multiple strategies to counteract these changes and prevent obesity relapse.
As reported previously (9), there is a wide range of self-reported PA in in the NWCR. While many reported very high (over 3500 kcals/week) or high (2250-3499 kcals/week) levels of PA, 25% reported successful weight loss maintenance and low PA (<1000 kcals/week) on registry entry. We were surprised to observe that those reporting low levels of activity did not appear to rely more on dietary strategies to achieve and maintain their weight loss relative to those reporting higher levels of activity. This suggests there may be a subset of individuals that may be able to maintain a weight loss with lower levels of activity and less of a focus on traditionally held dietary strategies (low fat and calorie restricted diets). However, it is important to note that this group also weighed more, was maintaining a lesser amount of weight loss, and was almost twice as likely to be smokers.
Other studies in the NWCR have also explored the variability in diet and PA reported by individuals successful at weight loss maintenance. Phelan et al (13) reported that a subset of NWCR entrants (11%) achieved and maintained weight loss using a low carbohydrate diet. These individuals also reported a higher energy intake, and expending fewer calories in physical activity. A study using accelerometers to assess free living PA in NWCR members found that while on average NWCR members engage in high levels of physical activity (285 min/week of moderate to vigorous PA), there was substantial variability in levels of objectively measured PA in NWCR members (25).
While there is substantial evidence that caloric restriction and physical activity are key determinants of success in weight loss maintenance (20, 22, 26-32), there may be a minority of individuals that do not adhere to these traditionally held tenets and can still achieve success. Thus, a single approach to weight loss maintenance may not fit all individuals. Recently published studies suggest there may be a variety of alternative approaches to weight management. For example, diets of varying composition (not just low fat) such as low carbohydrate diets (33, 34) and low energy density diets (35, 36) have been associated with some success in weight loss maintenance.
Neither baseline PA nor dietary intake (total calories or percent fat) was predictive of 3 year weight regain. However, detrimental changes in either PA or dietary behaviors over time were associated with weight regain, as observed in other studies in the NWCR (37). Thus, while different levels of PA and dietary behaviors may work for different individuals, it appears that what seems to matter the most is to find a set of behaviors that works for weight loss maintenance and maintaining these behaviors long-term.
It is important to point out that participants in this study were derived from the NWCR, a self-selected sample of successful weight loss maintainers who may be more determined in their weight loss efforts than the general population of successful weight loss maintainers. Moreover, 23% of subjects did not return 3 year follow up weight data. Participants lost to follow-up may have regained more weight than those who responded, however, failure to complete the 3-year follow-up was not strongly associated with baseline physical activity or caloric intake. In the present study, 95% of the sample was Caucasian and 63% highly educated (college degree or higher). Thus, findings from the present study may not be applicable to all individuals desiring to maintain a weight loss. Caution should therefore be used in making recommendations for all groups based on this homogeneous sample. There is also a potential for inaccuracy and bias in the self-report measures of energy intake (Block FFQ) and energy expenditure (Paffenbarger questionnaire) used in the NWCR. While correlations of the Block FFQ with 4 day food records for % calories from fat are reasonable (r=0.65-0.67), correlation for total energy intake is lower (r=0.51) (11). The Paffenbarger questionnaire relies on self-reported PA which could lead to overestimation of the actual amount of PA performed (38). This questionnaire was also designed to assess planned leisure time activity and thus may not fully capture work related or lifestyle PA (39) which could lead to underestimation of the actual amount of PA performed. Energy expenditure data obtained from this questionnaire is not adjusted for subject gender or body weight which could lead to overestimation or underestimation in actual PA kcals/week.
Conclusions
Participants in the NWCR reporting high levels of PA are maintaining a greater weight loss and a lower current body weight, supporting the important role of PA in weight loss maintenance. Participants reporting higher levels of PA on registry entry also engage in more dietary habits important for long term weight loss maintenance (i.e. report lower fat intake, more restrained eating), report a greater reliance on several important dietary strategies for weight loss maintenance, and perceive weight loss maintenance to be more difficult suggesting that this is a group that is overall doing more to maintain their weight loss. While the majority of NWCR participants report relatively high levels of PA, there is a substantial subset of participants (∼25%) that appears to be able to maintain a weight loss (albeit a lower amount) while engaging in relatively low levels of physical activity and with less of a focus on dietary habits. These findings suggest that there is not a “one size fits all strategy” for successful weight loss maintenance and that weight loss maintenance may require the use of more strategies by some individuals than others. Neither baseline levels of PA or dietary intake were predictive of weight regain at year 3; however detrimental changes in dietary and PA behaviors over time were associated with weight regain. Thus, a key to successful weight loss maintenance appears to be finding a set of behaviors that works for each individual and maintaining these behaviors over time.
Acknowledgments
Funding Source: The primary funding source for this analysis was Dr. Catenacci's National Institute of Health (NIH) K23 Career Development Award (K23DK078913). Additional funding to support the NWCR comes from NIH DK42549 and DK48520.
Footnotes
Competing Interests: The authors do not have any competing interests to disclose.
Contributor Information
Lorraine G. Ogden, Email: lorri.ogden@ucdenver.edu, Department of Biostatistics and Informatics, University of Colorado Denver, Denver CO.
Suzanne Phelan, Email: sphelan@calpoly.edu, Department of Kinesthesiology, California Polytechnic State University, San Luis Obispo CA.
J. Graham Thomas, Email: jthomas4@lifespan.org, Department of Psychiatry and Human Behavior, Warren Alpert Medical School of Brown University, Brown University, Providence, RI.
James O Hill, Email: james.hill@ucdenver.edu, Anschutz Health and Wellness Center, University of Colorado Denver, Denver, CO.
Rena R. Wing, Email: rwing@lifespan.org, Department of Psychiatry and Human Behavior, Warren Alpert Medical School of Brown University, Brown University, Providence, RI.
Holly R. Wyatt, Email: holly.wyatt@ucdenver.edu, Division of Endocrinology, Metabolism and Diabetes, Anschutz Health and Wellness Center, University of Colorado Denver, Denver, CO.
References
- 1.Catenacci VA, Ogden LG, Stuht J, et al. Obesity. 1. Vol. 16. Silver Spring, Md: 2008. Jan, Physical activity patterns in the National Weight Control Registry; pp. 153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Catenacci VA, Grunwald GK, Ingebrigtsen JP, et al. Obesity. Vol. 28. Silver Spring, Md: Oct, Physical Activity Patterns Using Accelerometry in the National Weight Control Registr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paffenbarger RS, Jr, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978 Sep;108(3):161–75. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 4.Block G, Hartman AM, Naughton D. A reduced dietary questionnaire: development and validation. Epidemiology. 1990 Jan;1(1):58–64. doi: 10.1097/00001648-199001000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 6.McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? J Consult Clin Psychol. 1999 Apr;67(2):177–85. doi: 10.1037//0022-006x.67.2.177. [DOI] [PubMed] [Google Scholar]
- 7.Washburn RA, Smith KW, Goldfield SR, McKinlay JB. Reliability and physiologic correlates of the Harvard Alumni Activity Survey in a general population. J Clin Epidemiol. 1991;44(12):1319–26. doi: 10.1016/0895-4356(91)90093-o. [DOI] [PubMed] [Google Scholar]
- 8.Siconolfi SF, Lasater TM, Snow RC, Carleton RA. Self-reported physical activity compared with maximal oxygen uptake. Am J Epidemiol. 1985 Jul;122(1):101–5. doi: 10.1093/oxfordjournals.aje.a114068. [DOI] [PubMed] [Google Scholar]
- 9.Catenacci VA, Ogden LG, Stuht J, et al. Physical activity patterns in the National Weight Control Registry. Obesity. 2008 Jan;16(1):153–61. doi: 10.1038/oby.2007.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.United States Department of Health and Human Services. Physical Activity Guidelines for Americans. [cited December 15, 2011];2008 Available from: www.health.gov/paguidelines.
- 11.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43(12):1327–35. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 12.Schoeller DA. How accurate is self-reported dietary energy intake? Nutr Rev. 1990 Oct;48(10):373–9. doi: 10.1111/j.1753-4887.1990.tb02882.x. [DOI] [PubMed] [Google Scholar]
- 13.Phelan S, Wyatt H, Nassery S, et al. Obesity. 10. Vol. 15. Silver Spring, Md: 2007. Oct, Three-year weight change in successful weight losers who lost weight on a low-carbohydrate diet; pp. 2470–7. [DOI] [PubMed] [Google Scholar]
- 14.Harris J, Benedict FA. Biometric Study of Basal Metabolism in Man. WAshington DC: Carnegie Institute of Washington; 1919. Publication No. 279. [Google Scholar]
- 15.Goldberg GR, Black AE, Jebb SA, et al. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr. 1991 Dec;45(12):569–81. [PubMed] [Google Scholar]
- 16.Briefel RR, Sempos CT, McDowell MA, Chien S, Alaimo K. Dietary methods research in the third National Health and Nutrition Examination Survey: underreporting of energy intake. The American journal of clinical nutrition. 1997 Apr;65(4 Suppl):1203S–9S. doi: 10.1093/ajcn/65.4.1203S. [DOI] [PubMed] [Google Scholar]
- 17.Westenhoefer J. Dietary restraint and disinhibition: is restraint a homogeneous construct? Appetite. 1991 Feb;16(1):45–55. doi: 10.1016/0195-6663(91)90110-e. [DOI] [PubMed] [Google Scholar]
- 18.Shearin EN, Russ MJ, Hull JW, Clarkin JF, Smith GP. Construct validity of the Three-Factor Eating Questionnaire: flexible and rigid control subscales. Int J Eat Disord. 1994 Sep;16(2):187–98. doi: 10.1002/1098-108x(199409)16:2<187::aid-eat2260160210>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 19.Unick JL, Jakicic JM, Marcus BH. Contribution of behavior intervention components to 24-month weight loss. Medicine and science in sports and exercise. 2010 Apr;42(4):745–53. doi: 10.1249/MSS.0b013e3181bd1a57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss maintenance in overweight women. Arch Intern Med. 2008 Jul 28;168(14):1550–9. doi: 10.1001/archinte.168.14.1550. discussion 9-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schoeller DA, Shay K, Kushner RF. How much physical activity is needed to minimize weight gain in previously obese women? The American journal of clinical nutrition. 1997 Sep;66(3):551–6. doi: 10.1093/ajcn/66.3.551. [DOI] [PubMed] [Google Scholar]
- 22.Tate DF, Jeffery RW, Sherwood NE, Wing RR. Long-term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain? The American journal of clinical nutrition. 2007 Apr;85(4):954–9. doi: 10.1093/ajcn/85.4.954. [DOI] [PubMed] [Google Scholar]
- 23.Rosenbaum M, Hirsch J, Gallagher DA, Leibel RL. Long-term persistence of adaptive thermogenesis in subjects who have maintained a reduced body weight. The American journal of clinical nutrition. 2008 Oct;88(4):906–12. doi: 10.1093/ajcn/88.4.906. [DOI] [PubMed] [Google Scholar]
- 24.Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011 Oct 27;365(17):1597–604. doi: 10.1056/NEJMoa1105816. [DOI] [PubMed] [Google Scholar]
- 25.Catenacci VA, Grunwald GK, Ingebrigtsen JP, et al. Physical activity patterns using accelerometry in the National Weight Control Registry. Obesity. 2011 Jun;19(6):1163–70. doi: 10.1038/oby.2010.264. PMCID In Progress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005 Feb;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 27.McGuire MT, Wing RR, Klem ML, Hill JO. Behavioral strategies of individuals who have maintained long-term weight losses. Obes Res. 1999 Jul;7(4):334–41. doi: 10.1002/j.1550-8528.1999.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 28.Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. The American journal of clinical nutrition. 2001 Nov;74(5):579–84. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 29.Befort CA, Stewart EE, Smith BK, Gibson CA, Sullivan DK, Donnelly JE. Weight maintenance, behaviors and barriers among previous participants of a university-based weight control program. Int J Obes (Lond) 2008 Mar;32(3):519–26. doi: 10.1038/sj.ijo.0803769. [DOI] [PubMed] [Google Scholar]
- 30.Kayman S, Bruvold W, Stern JS. Maintenance and relapse after weight loss in women: behavioral aspects. The American journal of clinical nutrition. 1990 Nov;52(5):800–7. doi: 10.1093/ajcn/52.5.800. [DOI] [PubMed] [Google Scholar]
- 31.Pronk NP, Wing RR. Physical activity and long-term maintenance of weight loss. Obes Res. 1994 Nov;2(6):587–99. doi: 10.1002/j.1550-8528.1994.tb00110.x. [DOI] [PubMed] [Google Scholar]
- 32.Shick SM, Wing RR, Klem ML, McGuire MT, Hill JO, Seagle H. Persons successful at long-term weight loss and maintenance continue to consume a low-energy, low-fat diet. J Am Diet Assoc. 1998 Apr;98(4):408–13. doi: 10.1016/S0002-8223(98)00093-5. [DOI] [PubMed] [Google Scholar]
- 33.Due A, Larsen TM, Mu H, Hermansen K, Stender S, Astrup A. Comparison of 3 ad libitum diets for weight-loss maintenance, risk of cardiovascular disease, and diabetes: a 6-mo randomized, controlled trial. The American journal of clinical nutrition. 2008 Nov;88(5):1232–41. doi: 10.3945/ajcn.2007.25695. [DOI] [PubMed] [Google Scholar]
- 34.Foster GD, Wyatt HR, Hill JO, et al. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: a randomized trial. Ann Intern Med. 2010 Aug 3;153(3):147–57. doi: 10.1059/0003-4819-153-3-201008030-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Raynor HA, Van Walleghen EL, Bachman JL, Looney SM, Phelan S, Wing RR. Dietary energy density and successful weight loss maintenance. Eat Behav. 2011 Apr;12(2):119–25. doi: 10.1016/j.eatbeh.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raynor HA, Looney SM, Steeves EA, Spence M, Gorin AA. The effects of an energy density prescription on diet quality and weight loss: a pilot randomized controlled trial. Journal of the Academy of Nutrition and Dietetics. 2012 Sep;112(9):1397–402. doi: 10.1016/j.jand.2012.02.020. [DOI] [PubMed] [Google Scholar]
- 37.Phelan S, Wyatt HR, Hill JO, Wing RR. Obesity. 4. Vol. 14. Silver Spring, Md: 2006. Apr, Are the eating and exercise habits of successful weight losers changing? pp. 710–6. [DOI] [PubMed] [Google Scholar]
- 38.Lichtman SW, Pisarska K, Berman ER, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992 Dec 31;327(27):1893–8. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- 39.Strath SJ, Bassett DR, Jr, Swartz AM. Comparison of the college alumnus questionnaire physical activity index with objective monitoring. Ann Epidemiol. 2004 Jul;14(6):409–15. doi: 10.1016/j.annepidem.2003.07.001. [DOI] [PubMed] [Google Scholar]


