Abstract
Although the scientific community has recognized the effects of prenatal alcohol exposure on development for over 40 years, the empirical study of positive behavioral interventions and family support programs for people with fetal alcohol spectrum disorders (FASD) has only just emerged over the last 10 to 15 years. In this time, dedicated researchers have developed innovative programs that have generally produced large effects and have been acceptable to children with FASD and their families. This body of work demonstrates that children with FASD can benefit from interventions that are appropriately tailored to their neurodevelopmental disabilities. Despite this progress, much work lies ahead to meet the significant needs of people with FASD. This review evaluates available sources of information, including theoretical and Lived Experience models, empirical evidence on existing programs, and best practice guidelines, to guide future research priorities and clinical practice. Three priorities for future intervention research are offered.
Keywords: fetal alcohol spectrum disorders, intervention, positive behavior support, family support, empirically-supported interventions
Introduction
The effects of prenatal alcohol exposure on development have been recognized by the scientific community for over 40 years [1]. Research has documented that prenatal alcohol exposure alters brain structure and functioning and can produce lifelong impairments in cognition and behavior [2,3]. Fetal alcohol spectrum disorders (FASD) are currently estimated to affect 2 to 5 percent of the US population [4], and are associated with high service utilization and a large cost burden to society [5–7]. Despite our growing understanding of the effects of prenatal alcohol exposure and the magnitude of this public health problem, the empirical study of interventions for people with FASD has only begun over the last decade. Several reviews have been published in the last few years evaluating the evidence base of interventions for FASD (e.g., [8,9]). Although a number of exciting intervention studies are underway, data on only a few additional studies have been published since. Rather than a sole focus on critically evaluating data from each published study, this review emphasizes available sources of information that can guide clinical practice and future research priorities. These sources of information include current theoretical and Lived Experience [10] models of intervention development for FASD, existing interventions with empirical support, and best practice guidelines. Recommendations for next steps in intervention development are made throughout and three priorities for intervention research in the field are offered.
Theoretical Models for FASD Intervention
Two complementary theoretical models have been proposed by innovative researchers to guide the development of interventions for people with FASD. The first model [8,11] is based on a neuroconstructivisim perspective that recognizes the dynamic reciprocal relationship between experience and neural systems. An efficacious intervention thus aims to induce neural activity through planned and guided experiences that with repetition lead to plasticity of neural structures and progressive formation of the neural circuitry to support the targeted outcome. To optimally induce neural plasticity to support behavior change, Kodituwakku provides several guidelines. First, interventions for people with FASD must take into account the pattern of cognitive and behavioral strengths and weaknesses seen in this population. Enriched experiences should be provided in a guided fashion that target the person’s “zone of proximal development” [12]. Interventions are likely to be most successful when they include direct child intervention and parent support. Kodituwakku proposes that early intervention in attention and self-regulation is likely to have more far-reaching effects than specific training in other domains. Combined interventions including pharmacological and behavioral approaches are also recommended.
The conceptual framework put forth by Olson and colleagues [13] integrates developmental and family systems theories to guide intervention development for FASD. Individual differences can influence how disabling characteristics are manifested for each person. Developmental theory posits that these individual characteristics transact with those of their broader ecological context, including family and other social systems in which persons belong. Risk and protective factors within each ecological level can be identified that influence the developmental trajectories of people and these factors can differ or change in importance at various stages across the lifespan. In this model, interventions attempt to reduce risk and increase protective factors to divert the person onto a more adaptive developmental trajectory. The integration of family systems theory to this model highlights the importance of family-level factors on the trajectories of affected persons and emphasizes the need to intervene at the level of the family system to affect and maintain long-term change. As applied to FASD, this integrated model supports family-focused interventions that aim to alter identified family-level risk and protective factors including a stable and nurturing home, attachment, parent-child interaction patterns, caregiver cognitive appraisal, self-efficacy, parent stress, and family resource needs. A previous meta-analysis provides support for combining interventions on parent training and stress management for families raising children with developmental disabilities as the combination has larger effects than either parent training or stress management interventions alone [14].
The theoretical models outlined by Kodituwakku [11] and Olson and colleagues [13] share several similarities. Both employ complex conceptualization that goes beyond matching areas of deficit with intervention strategies. They recognize the importance of developmental level and the need to consider the individual factors that influence outcome. Both models also emphasize reciprocal relationships between individuals and their experiences in their social environment. The primary difference lies in the levels of analysis emphasized in each model. Developmental psychopathology provides a unifying perspective that can readily encapsulate both models. The discipline of developmental psychopathology emphasizes the importance of conceptualizing the reciprocal transactions of risk and protective factors across ecological levels (e.g., individual, family, community, culture; as emphasized by Olson and colleagues) and multiple levels of analysis (e.g., genetic, neural, physiological, behavioral, interpersonal; as emphasized by Kodituwakku) [15]. Understanding these transactions provides greater insight into the types of interventions needed to facilitate change across levels. It also informs theories of the mechanisms of change and the constructs that should be measured to document intervention efficacy. Unifying the models proposed by Kodituwakku and Olson and colleagues provides strong theoretical support for multi-component interventions integrating pharmacotherapy, child-focused training in self-regulation, and family-focused intervention targeting the pattern of parent-child interactions, parenting self-efficacy and stress, and family needs. When funding permits, researchers should consider measuring intervention effects at levels of analysis beyond standard cognitive and behavioral measures, such as changes in brain structure or function (e.g., magnetic resonance imaging, event related potentials, e.g., [16–18]), physiological regulation or reactivity (e.g., cortisol, vagal tone, e.g., [19]), or observations of interpersonal functioning. Examination of moderators will also help identify for whom interventions are most effective and can guide the most efficient deployment of interventions and further efforts to improve interventions for whom they are less effective. A growing literature is amassing evidence for differential susceptibility to intervention response based on genetic or other biological factors [20]. Intervention effects could also plausibly be moderated by an interaction between a person’s genotype and environment (i.e., gene x environment x treatment), although this effect is more difficult to detect statistically unless sample sizes are quite large.
Lived Experience Model for FASD Intervention
Another source of valuable information to guide intervention development lies in the lived experiences of parents of individuals with FASD and providers who serve this population [10]. These two groups have first hand experience with the current systems of care and have insight into what is beneficial and what is needed to meet the needs of people with FASD and their families. They also represent the primary consumers of interventions in the community. Service providers must first “buy-in” and adopt intervention programs within their agencies, and people with FASD and their families must perceive these programs as acceptable. Understanding the perspectives of these key stakeholders can inform the development or selection of intervention approaches to ensure acceptability and facilitate sustainability and dissemination.
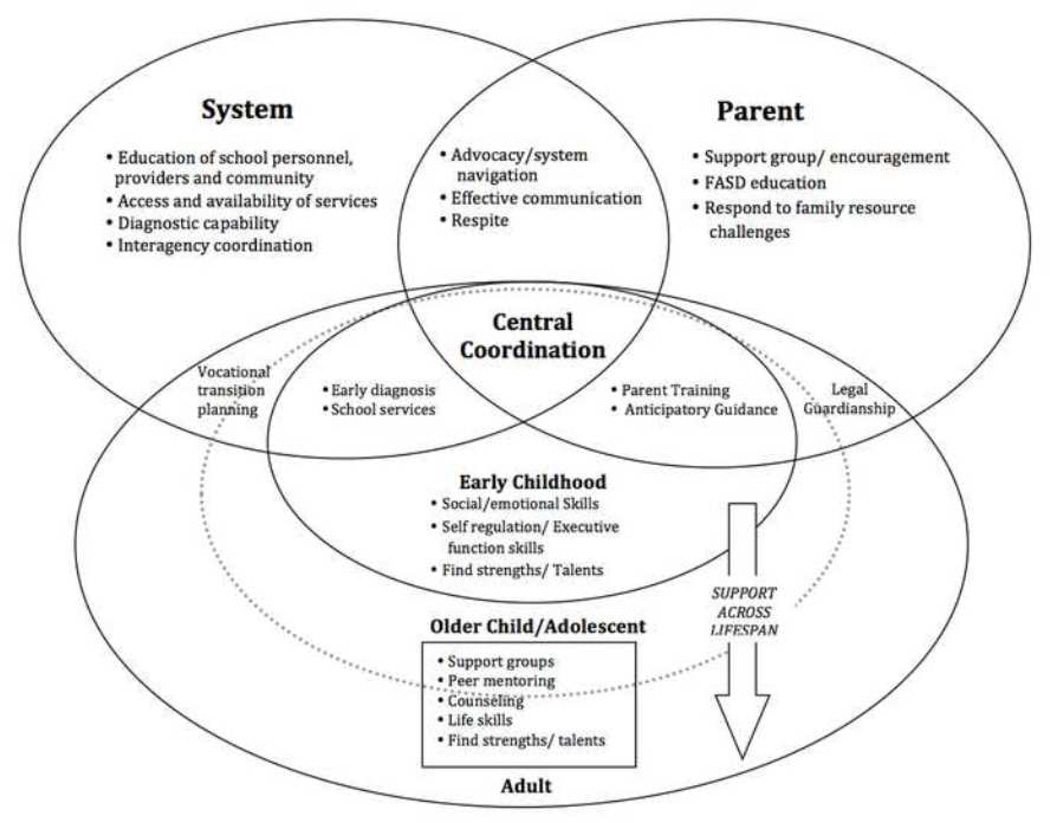
A systematic, qualitative study was recently completed in upstate New York to identify intervention characteristics to prevent secondary conditions in people with FASD from the lived experiences of parents and service providers [10]. Results from this study were organized into five overarching themes and a visual model of specific intervention approaches for people with FASD and their families (see Figure 1 [10]). Parents and service providers emphasized that FASD is a life-long condition and therefore appropriate services are needed across the lifespan. In addition, they recommended a proactive or preventive approach, when possible. Putting appropriate supports in place before a person begins to struggle is likely to lead to more positive outcomes than requiring people to meet a certain threshold of severity to access services. Due to the variability of functioning of people with FASD and their families, participants recognized that a one-size-fits-all approach is not optimal for this population and recommended that interventions be individualized or have the ability to be tailored to match the person’s pattern of strengths and weaknesses and family or living environment. Parents and service providers also expressed a need for comprehensive interventions that account for the complex needs and diverse experiences of people with FASD. Lastly, participants emphasized the importance of coordination of services across systems and developmental stages. These five overarching themes are consistent with the positive behavioral support (PBS) framework [21]. The PBS framework emerged from the blending of the practical science of applied behavioral analysis, the inclusion movement, and person-centered planning. Its emphasis is on adapting the environment to enhance a person’s quality of life, with reduction of problem behaviors as a secondary goal. Figure 1 illustrates the specific intervention needs and approaches across the lifespan that were recommended by participants to meet these overarching themes for people with FASD.
Figure 1.
Lived experience model of identified program characteristics and specific intervention strategies for the prevention of secondary conditions in individuals with fetal alcohol spectrum disorders (FASD). (Reprinted with permission from: Petrenko CLM, Tahir N, Mahoney EC, Chin NP: Qualitative Assessment of Program Characteristics for Preventing Secondary Conditions in Individuals with Fetal Alcohol Spectrum Disorders. J Popul Ther Clin Pharmacol 2014, Vol 21(2):e246-e259. Copyright 2014 Canadian Society of Pharmacology and Therapeutics) [10].
This model represents a good fit with the movement towards integrated care models to more effectively coordinate and manage the complex medical and behavioral health care needs of children and adults [22,23]. The SAMHSA-HRSA Center for Integrated Health Solutions identifies five core competencies of integrated care models: 1) family and person-centered teams with care coordination capability, 2) individualized and coordinated care plans, 3) use of evidence-based guidelines, 4) established and accountable relationships with other entities, and 5) data-informed planning. The FASD Toolkit established by the American Academy of Pediatrics and resources through the SAMHSA-HRSA Center for Integrated Health Solutions provide some practical guidelines and recommendations for how to accomplish integrated care in different settings. One challenge in developing integrated care for people with FASD is that they often interface with multiple existing systems of care (e.g., child welfare, special education, developmental disabilities, mental health), and in most parts of the US, no single system is currently structured well to serve this population. This challenge is present across the lifespan, but is even more salient for older adolescents and adults with FASD. Innovation and collaboration between policymakers and community providers will be needed to establish the infrastructure and funding to overcome these challenges, especially given the under recognition of FASD in the US.
Evidence from Empirically Studied Interventions
Empirical evidence for the efficacy of interventions for people with FASD has been gradually mounting over the last decade. Exciting and innovative programs are also currently under study and the next decade promises to build on the evidence base of effective interventions for people with FASD across the lifespan. The majority of interventions evaluated to date have focused on the preschool and school-age developmental periods (see Table 1 for a list of programs with published data). The following sections will discuss available evidence for intervention approaches by developmental level and their fit within the prevailing theoretical and conceptual models discussed above.
Table 1.
Studies on positive behavior interventions and family support programs for children with FASD
| Program Name | Format | Age Range |
References | Design* (Total N) |
|---|---|---|---|---|
| Parent Education and Training Programs | ||||
| Caregiver Education and Training for Behavioral Regulation | Two 2hr workshops or online content | 3–10 | Kable et al., 2007; Coles et al., 2009 | C (61) |
| Kable et al., 2012 | A (59) | |||
| Triumph Through the Challenges of Fetal Alcohol Syndrome | Six 2hr workshops for parents | Not specified | Fisher, 2005 | C (160- 322) |
| Coaching Families (CF) | Paraprofessional mentoring for the family | 0–23 | Leenaars et al., 2011 | C (186) |
| Parenting Support and Management (PSM) | 14-week parent psychoeducation group | 3–7 | Study #4 in Bertrand, 2009 | A (46) |
| Parent-Child Interaction Therapy (PCIT) | 14-week intervention delivered to parent-child dyad | |||
| Families Moving Forward (FMF) | 9–11 month in-home parent consultation program | 5–11 | Study #5 in Bertrand, 2009 | A (52) |
| Child Attention, Meta-Cognition, & Self-Regulation Interventions | ||||
| Computerized Progressive Attention Training (CPAT) | 16 hours of computerized training with 1:1 coaching | 8–15 | Kerns et al., 2010 | C (10) |
| Cognitive Control Therapy (CCT) | Weekly, 1 hour sessions over 10-month school year | Mean 8.5 | Adnams et al. as published in Riley et al., 2003 | A (10) |
| Alert Program for Self- Regulation | 12-week child intervention by trained therapist | 8–12 | Nash et al., 2014; Soh et al., 2015 | B (25) |
| Parents and Children Together (PACT) | 12-week concurrent child and parent groups | 6–12 | Study #3 in Bertrand, 2009; Wells et al., 2012 | A (78) |
| Child Adaptive Functioning | ||||
| Fire and Street Safety Virtual Training | Videogame played until mastery (< 30 minutes) | 4–10 | Coles et al., 2007 | A (32) |
| Good Buddies | 12-week concurrent child and parent groups | 6–12 | Study #1 in Bertrand, 2009; Frankel et al., 2006; Keil et al., 2010; O’Connor et al., 2006 | B (100) |
| O’Connor et al., 2011 | B (85) | |||
| Language and Literacy Training (LLT) | Twice a week small group intervention over 9 months | 9–10 | Adnams et al., 2007 | A (40) |
| Math Interactive Learning Experience (MILE) | 6-week child tutoring, parent training, and consultation | 3–10 | Study #2 in Bertrand, 2009; Coles et al., 2009; Kable et al., 2007 | A (61) |
| Kable et al., 2015 | A (60) | |||
Study design codes: A = randomized controlled trial; B = controlled trial using alternating assignment to targeted intervention and comparison group; C = single group pre-post intervention comparison
Infancy & Early Childhood
Seminal work conducted by O’Connor and colleagues documents the influence of early mother-child interactions and attachment during infancy to the later development of psychiatric symptoms in children with FASD (for a review see [24]). This body of work provides support for the use of relationship-focused dyadic interventions in infancy and early childhood to improve family functioning and prevent later problems. Although dyadic interventions have strong theoretical and basic research support in FASD and other populations, only two known programs have been developed and subjected to study for infants and toddlers with FASD and their parents. Both programs focus on the parent-child relationship, but differ in the type of families targeted. The Breaking the Cycle (BTC) program in Toronto, Canada delivers a relationship-focused intervention to substance-abusing mothers and their young children. This program has been delivered in community settings since 1994. Recently, a comparison study was undertaken to document the evidence of BTC relative to standard treatment offered in a neighboring city. Preliminary data suggest BTC’s superiority in decreasing maternal substance use, improving maternal mental health, increasing relationship capacity, and improving child outcomes [25]. The second program, Strategies for Enhancing Early Development Success – Infants and Toddlers (SEEDS-IT), was developed for foster and adoptive parents raising infants and toddlers with FASD and is currently under study [26].
Based on available evidence and prevailing theory, other evidence-based interventions that focus on early parent-child relationships or attachment such as Child-Parent Psychotherapy (CPP, [27]) or Attachment and Biobehavioral Catch-up (ABC; [28]), might be appropriate for young children with FASD and their families. Families of young children with FASD would also likely benefit from psychoeducation on FASD, assistance with accessing early intervention and developmental disability systems if needed, and anticipatory guidance on risk and protective factors to consider for upcoming developmental stages [29].
Preschool and School-Age Children
Parent education and training programs
As emphasized by Olson and colleagues [13], there is a strong theoretical rationale for parent training and support programs for families raising children with FASD. Good quality caregiving and a stable, nurturing home environment are two protective factors against secondary conditions [30]. However, achieving these protective factors can be challenging for families as typical interpretations of behavior and parenting approaches may be a poor fit for the brain-based disabilities of children with FASD. In addition, caregivers of children with FASD often experience high levels of stress that differ in magnitude and contributing factors relative to caregivers of children with other disabilities, such as autism [31–34]. Families raising children with FASD also face significant systems-level barriers and often have to assume the role of advocate and service coordinator for their children [35].
Consistent with the broader field of developmental disabilities [36], interventions targeting behavior and mental health problems in preschool and school-aged children with FASD have predominately focused on parent training interventions. A range of parent-training programs have been developed for parents of children with FASD, including brief workshops to intensive in-home interventions combining positive behavior support, motivational interviewing, and cognitive behavioral therapy for caregivers (see Table 1). Most of the programs listed in this category have been implemented with diverse family types and structures. Curricula for brief parent training workshops (ranging from 2 to 6 sessions) focus on psychoeducation about FASD, information on effective behavior management strategies for this population, and advocacy tools. Pre-post data from parent training workshops suggests that the content is beneficial and acceptable for families regardless of the format in which it is delivered (e.g., in person workshops, online materials; [37–40]). Moderate-level intensity interventions have involved individual family goal-based mentoring [41] or group-based psychoeducation and support (Study 4 in [42]). Both of these interventions have yielded pre-post change on targeted outcomes and were satisfactory to families. The two highest-intensity interventions have received the most rigorous study using controlled designs. Parent-child interaction therapy produced improvements in pre-post levels of child behavior problems and parent stress, but attrition rates were high and effects did not differ from the moderate intensity psychoeducation and support group (Study 4 in [42]). The Families Moving Forward (FMF) program has been evaluated relative to a community standard of care control group in both university and community settings (Study 5 in [42]). FMF was designed to modify specific parenting attitudes and parenting responses toward the child’s problem behavior with the ultimate goals of reducing child behavior problems and improving child and family functioning. Positive intervention effects have been documented for parenting self-efficacy, self-care, family needs met, and reduced child behavior problems. FMF has been rated very acceptable to families and studies have had very high retention rates. A study is currently underway by Petrenko and colleagues that integrates FMF with a 30-week child skills group targeting self-regulation and socio-emotional skills based on the Promoting Alternative THinking Strategies (PATHS) curriculum [43,44]. This integrated intervention for children ages 4 to 8 was informed by the Lived Experience and the theoretical models described above.
Attention, meta-cognition, and self-regulation interventions
Consistent with the guidelines put forth by Kodituwakku [11], several investigators have developed and evaluated interventions targeting attention and self-regulation skills in children with FASD. One small pilot study [45] utilized a computerized attention training program to improve children’s attentional skills. While completing the program, children were provided individual support and coaching in metacognitive strategies, which is critical for generalization. Relative to their pre-intervention performance, children demonstrated improvements in multiple aspects of attention and spatial working memory, as well as generalized gains in reading and math fluency. A larger study is currently underway on a similar program called Caribbean Quest developed by this research team. Training in meta-cognitive strategies has also been evaluated in a small pilot study in South Africa using Cognitive Control Therapy [46]. Although sample sizes limited the ability to detect effects in meta-cognitive skills and neuropsychological functioning, greater improvements in behavior and adaptive functioning in the classroom were observed in the intervention group. Coles and colleagues are currently studying an intervention called GoFAR, which teaches children affective and metacognitive control strategies through the use of a computer game and behavioral training.
Two studies [47,48] have been published on children with FASD using the Alert Program for Self-Regulation [49]. The Alert program was originally developed by occupational therapists for children with difficulties with self-regulation and utilizes sensory integration and cognitive strategies to help children increase their abilities to monitor and modify their behavior to meet the demands of the situation. Nash and colleagues [47] evaluated the standard 12-session, individually-delivered Alert program with children with FASD. Compared to children on the waitlist, children who received the intervention demonstrated improvements in some aspects of inhibitory control and socioemotional functioning based on child testing and parent report. Changes in brain structure were also documented in the intervention group, including increases in gray matter in several regions of the frontal lobe and anterior cingulate [16]. Wells and colleagues [48] developed a group-based program that incorporates aspects of the Alert curriculum and treatment strategies used with children with traumatic brain injuries. Children’s parents also participated in a concurrent psychoeducation group. Overall group differences were identified on a measure of parent-reported executive functioning, although mean score changes were smaller than on the same measure in the Nash study. In both studies, although treatment changes were documented, mean parent-reported executive functioning scores remained in the at-risk or clinically significant ranges post-intervention.
Functional and adaptive skills interventions
Research has demonstrated that children with FASD have significant impairment in adaptive functioning and patterns differ from those of children with other disabilities [50,51]. Several innovative intervention programs have been developed to improve the adaptive skills of children with FASD in the areas of safety awareness, social functioning and friendship, and academic achievement. Fire and street safety skills have been taught to children using computer games using “virtual worlds” [52]. Children who completed training in these skills had improved knowledge and were able to demonstrate what they were supposed to do in behavioral settings. A group based friendship and social skills training program has also been evaluated in both University and community settings with school aged children with FASD [53,54]. The Children’s Friendship Training (CFT; [55]) program was adapted for children with FASD based on the neurodevelopmental and behavioral needs of this population [56]. This 12-week intervention called Good Buddies includes concurrent child and parent skills groups. Children learn concrete skills on how to enter peer group situations and be a good friend to others. Parents learn how to support their children’s social development and use the specific skills children are learning to help their children build friendships with others. Results from both the controlled efficacy trial and the community effectiveness trial demonstrated that children with FASD had improved social skills and fewer behavior problems after intervention. Studies have documented that the intervention was more effective for children who had better behavior regulation or were taking neuroleptic medications [57,58]. In the community trial, children with FASD showed similar improvements to children without prenatal alcohol exposure seeking treatment at the community mental health center [54]. Further research on Good Buddies has documented that the intervention may work in part through reductions in children’s hostile attribution biases for peer group entry situations [59].
Given documented difficulties with academic achievement for children with FASD [60,61], two research groups have developed and evaluated intervention programs targeting academic functioning. Adnams and colleagues [62] investigated the efficacy of a literacy intervention for 9 to 10 year old students in South Africa. After 9 months of small-group instruction (twice per week) at school, children who were randomized into the intervention group showed greater gains in targeted aspects of language and early literacy than children in the control groups. Math functioning has been an area of considerable interest in FASD given disproportionate impairments relative to other academic subjects [63]. Kable, Coles, and Taddeo [38,40] developed a socio-cognitive habilitation program focused on improving behavior and math functioning. The Math Interactive Learning Experience (MILE) program includes parent workshops, 6 weeks of individual tutoring for the child, and instruction to parents in how to generalize tutoring activities at home. Children who were randomized to receive MILE demonstrated greater gains in math functioning and parents reported reductions in behavior problems. Findings were replicated in a second trial in which both University-based and community implementations of MILE were superior to parent education alone [64]. An adaptation of the MILE program for use in the school setting with limited parent involvement has also shown positive intervention effects in math functioning [65].
Summary
Research demonstrates thus far that children with FASD can learn skills through positive behavioral interventions that are appropriately adapted to their neurodevelopmental strengths and weaknesses. Many interventions during this developmental period have provided direct training to parents or teachers working with these children to enact behavior change and/or to support generalization of skills. Parent support has also been an integral component in several interventions. Although good progress has been made documenting the evidence of interventions for children with FASD and their families during this developmental period, much work is needed to increase the availability of these interventions in the community so they are accessible to children and families. Research on trauma-informed or trauma-specific interventions, such as trauma focused cognitive behavioral therapy (tf-CBT; [66]), that are appropriately adapted to the neurodevelopmental profile of FASD is a logical next step given the high rates of trauma and other adverse postnatal experiences in this population [67].
Adolescence/Young Adulthood
Although no peer-reviewed publications are available on the efficacy of intervention programming at the time of this review, two CDC funded trials have recently completed and several additional studies are underway for this developmental period. The first CDC trial called Project Step-Up delivered a 6-week intervention to adolescents with FASD and their parents in concurrent groups with the primary aim of preventing or reducing alcohol and substance abuse. Several rigorous studies have documented adolescents and adults with FASD are at increased risk for alcohol use disorders above and beyond their family history of alcoholism [68,69]. Preliminary findings from Project Step-Up indicate that adolescents in the intervention were more likely to cut down or abstain from drinking and engaged in less risky drinking, with fewer negative consequences [70]. The intervention also resulted in an increase of expectancies of the negative consequence of alcohol use, although no changes were found between groups on positive expectancies. The CDC also funded a multi-component intervention for adolescents and young adults (ages 13–25) with FASD and their families called Partners for Success [71]. This intervention includes family therapy, individual mentoring, and a caregiver support group. Preliminary results did not show any positive intervention effects on youth outcomes, but did find changes in parent positive coping and self-controlling behaviors. However, there were a number of problems with recruitment and implementation that may have negatively impacted the researchers’ abilities to identify effects.
Much work is needed to address the significant challenges facing adolescents and young adults with FASD. The risk for secondary conditions dramatically increases during these developmental periods and fewer community-based supports are available in general for adolescents and adults [30]. Several research groups are starting to investigate the efficacy of yoga or mindfulness-based interventions for adolescents or young adults with FASD to help with difficulties with self-regulation. Other evidence-based interventions, such as dialectical behavioral therapy (DBT; [72,73]), might work well for people with FASD if appropriately adapted to their neurodevelopmental needs. People with FASD often struggle to live independently and function adaptively in everyday settings [30,74]. Research is needed on the type of services and supports that are most beneficial to people with FASD and for their families, who often end up filling this role given the dearth of services currently available. Interventions targeting social support, employment coaching, supportive living, and mental health and substance use programming would be particularly relevant for people with FASD. Family guidance focusing on adolescent and adult issues and assistance with social support and self-care are also relevant.
Parenting Interventions for Adults with FASD
Interventions have been adapted and evaluated with adults with FASD to help support them in parenting their young children based on research showing elevated rates of out-of-home placement [30]. Both programs are based on the Parent-Child Assistance Program (P-CAP), which provides women with alcohol and substance use problems a paraprofessional advocate case manager for 3 years to improve outcomes for the mother and child. A 12-month pilot study was conducted on the P-CAP program with women with FASD [75]. Case managers were provided with training in FASD and were given extra supports to work with this population. The pilot study suggested P-CAP helped women reduce their drug and alcohol use and increase their utilization of medical and mental health case services, greater use of contraception, and acquisition of stable housing. The Step by Step program, delivered by Catholic Social Services in Alberta, Canada, is loosely based on the P-CAP program and uses family mentors to help parents meet family needs and achieve individualized goals. A retrospective review of closed case files revealed parents with FASD in the Step by Step program had a significant reduction in identified needs and an increase in achieved goals across the program [76]. Participants with a formal FASD diagnosis had a greater reduction in needs. Results from these two pilot studies suggest that paraprofessional case managers and mentors have good acceptability to parents with FASD and can help them achieve positive outcomes for themselves and their children. Future research should also determine if standard or adapted parenting programs might be effective for parents with FASD. This knowledge is especially relevant as these types of programs are often mandated for parents whose children are at-risk for or are in out-of-home care, which is the case for many parents with FASD.
Existing Clinical Resources and Guidelines
Policymakers and service providers can also access existing guidelines and resources to guide their selection and implementation of positive behavioral interventions and family support for people with FASD across the lifespan. For example, SAMHSA recently published a Treatment Improvement Protocol (TIP 58) for Addressing Fetal Alcohol Spectrum Disorders [77]. This TIP provides information and concrete resources to help guide FASD informed care for substance abuse and mental health care providers as well as strategies and example policies to facilitate agency adoption of critical competencies to deliver FASD informed care. Building agency capacity and competence in FASD-informed care is an important first step to adopting evidence-based interventions for people with FASD. A number of other useful publications have been prepared by researchers, experienced clinicians, and family members about the types of strategies and approaches that seem beneficial in everyday settings to support people with FASD (e.g., [78–82]).
Future Research Directions
Research Priority 1: Continue to Build the Evidence-base for Empirically Supported Interventions for FASD across the Lifespan
Much more research is needed on the efficacy of interventions for people with FASD, especially during infancy and early childhood, adolescence, and adulthood. Recommendations for the types of intervention programs that might be most appropriate for each developmental period are offered above in each section of the review of empirical studies. In addition, greater efforts are needed to study interventions or strategies that are being provided to people with FASD and their families in the community. These types of studies are needed to determine whether interventions being used are effective. In addition, they will help facilitate transmission of knowledge and replication of interventions across sites and regions.
Researchers face a number of challenges in studying interventions for FASD. These include the relatively small number of investigators focused on this topic in the field, the difficulty of recruiting large samples to have sufficient power to detect effects, ethical considerations of study designs (e.g., randomization, control condition), and funding constraints. With the exception of researchers in very large cities with well-established FASD clinics, few researchers have the ability to conduct reasonably powered randomized controlled trials, which are considered the “gold-standard” in intervention research. Sample sizes available for studies published for preschool and school-aged children have ranged from 10 to 186, with a median of 59. Existing interventions have typically produced large effects that can be detected with these modest samples. However, identifying moderators and mediators of intervention effects are very difficult with these sample size limitations. Infrastructure and funding capacity for multi-site intervention trials would help address this challenge. Larger multi-site trials would also give researchers the power to test adaptive interventions (e.g., using Sequential, Multiple Assignment, Randomized Trails [SMART], [83]) that are responsive to the variability in needs of clients and their families.
Researchers can also consider alternate, systematic methodologies to rigorously make the most efficient use of current resources in developing and evaluating interventions. For example, systematic qualitative research can help inform the development of interventions that will facilitate their uptake and implementation in the community, as was done by Petrenko and colleagues [10,35]. Community-based participatory research (CBPR; [84]), which involves a collaborative partnership between researchers, community members, and organizational representatives in all aspects of the research process, may also be helpful in this regard. Rigorous single case designs [85,86] are another option that might be particularly useful given sample size and funding limitations. Single case methodology can meet the design standards established by multiple regional and national bodies in education and psychology that review the evidence for the efficacy of interventions [86,87].
Research Priority 2: Increase Access to Empirically-Supported Interventions for FASD in the Community using Implementation Science Research
Implementation science is the study of methods to promote the integration of research evidence into policy and clinical practice [88,89]. It aims to understand the behavior of providers and other stakeholders as it relates to the uptake, adoption, and implementation of evidence-based interventions. This information is critical to facilitate systematic dissemination and implementation of evidence-based interventions in the community. One major challenge impacting the uptake of evidence based interventions for FASD is the lack of knowledge about this condition by providers and the community in general [35]. FASD is also under recognized and under diagnosed, which prevents children and adults with this condition getting the appropriate services to prevent secondary conditions [35,90]. Another challenge is that children with FASD are often served by multiple systems of care and there is typically a lack of coordination in services across systems [10]. Systematic investigation on the adoption and effective implementation of integrated care systems for FASD is a clear need for this population. Implementation science can also aid in understanding how interventions can be packaged or adapted for specific populations in certain settings. One strategy that might be effective for FASD is to develop and package interventions that are appropriate for a range of neurodevelopmental disabilities. Agencies may be more likely to adopt and implement interventions if they perceive them to have broader applicability for a wider client base, especially when the cost of the materials and training investment is high. This approach may also be successful in convincing providers of the benefits of recognizing and serving people with FASD, which they may not have been doing previously. However, as Kodituwakku [11] cautions, the full benefits of interventions will likely only be reaped when they are tailored to the profile of strengths and weaknesses of a given disorder. Thus, interventions will likely be most effective when they allow for flexibility to respond to different profiles and needs.
Research Priority 3: Investigate the Risk and Protective Factors that Influence Outcomes and the Mechanisms of Change of Empirically Supported Interventions
Other areas for growth are the documentation of risk and protective factors that influence intervention outcomes and the study of mechanisms of change by which interventions work. These sources of information are important for identifying for whom interventions are most effective and whether modifications can be made to improve efficacy for different subgroups. Consistent with the developmental psychopathology perspective, intervention and theory can be mutually informative [15]. Controlled intervention trials can serve as an empirical test of underlying theory and can inform further development or adaptations of intervention design or content. Measuring outcomes and theoretical processes at multiple levels of analysis (e.g., genetic, physiological, behavioral, interpersonal) expands our understanding of the effects of interventions on the health and well being of people and the social contexts in which they live.
Conclusions
The last decade has witnessed steady growth in the evidence base for interventions for children with FASD and this growth is expected to continue over the next decade with more emphasis on developing interventions across the lifespan and increasing access to evidence-based interventions for people with FASD in the community. Future success in accomplishing these aims will depend on continued funding priorities by governmental and regional institutions and public and private foundations in the US and other parts of the world. Increased collaboration between researchers, clinicians, and policymakers will facilitate the success of our efforts in meeting the great needs of people with FASD and their families.
Acknowledgments
This research was supported by a Career Development Award (K01AA020486) from the National Institute on Alcohol Abuse and Alcoholism. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
Christie L. M. declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain new data from any studies with human or animal subjects performed by the author.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Riley EP, Infante MA, Warren KR. Fetal alcohol spectrum disorders: an overview. Neuropsychol Rev. 2011;21:73–80. doi: 10.1007/s11065-011-9166-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moore EM, Migliorini R, Infante MA, et al. Fetal alcohol spectrum disorders: recent neuroimaging findings. Curr Dev Disord Rep. 2014;1:161–172. doi: 10.1007/s40474-014-0020-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mattson SN, Crocker N, Nguyen TT. Fetal alcohol spectrum disorders: neuropsychological and behavioral features. Neuropsychol Rev. 2011;21:81–101. doi: 10.1007/s11065-011-9167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.May PA, Baete A, Russo J, et al. Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics. 2014;134:855–866. doi: 10.1542/peds.2013-3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Popova S, Stade BC, Johnston M, et al. Evaluating the cost of fetal alcohol spectrum disorder. J Stud Alcohol Drugs. 2011;72:163–164. doi: 10.15288/jsad.2011.72.163. [DOI] [PubMed] [Google Scholar]
- 6.Popova S, Lange S, Burd L, et al. Health care burden and cost associated with fetal alcohol syndrome: based on official Canadian data. PLoS One. 2012;7:e43024. doi: 10.1371/journal.pone.0043024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amendah DD, Grosse SD, Bertrand J. Medical expenditures of children in the United States with fetal alcohol syndrome. Neurotoxicol Teratol. 2011;33:322–324. doi: 10.1016/j.ntt.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 8.Kodituwakku PW, Kodituwakku EL. From research to practice: an integrative framework for the development of interventions for children with fetal alcohol spectrum disorders. Neuropsychol Rev. 2011;21:204–223. doi: 10.1007/s11065-011-9170-1. [DOI] [PubMed] [Google Scholar]
- 9.Paley B, O'connor MJ. Intervention for individuals with fetal alcohol spectrum disorders: treatment approaches and case management. Dev Disabil Res Rev. 2009;15:258–267. doi: 10.1002/ddrr.67. [DOI] [PubMed] [Google Scholar]
- 10. Petrenko CLM, Tahir N, Mahoney EC, et al. A qualitative assessment of program characteristics for preventing secondary conditions in individuals with fetal alcohol spectrum disorders. J Popul Ther Clin Pharmacol. 2014;21:e246–e259. This study presents a rigorous qualitative assessment of intervention characteristics to prevent secondary conditions in FASD from the lived experiences of families and service providers. The resulting model can inform intervention design and evaluation.
- 11. Kodituwakku PW. A neurodevelopmental framework for the development of interventions for children with fetal alcohol spectrum disorders. Alcohol. 2010;44:717–728. doi: 10.1016/j.alcohol.2009.10.009. This review presents a theoretical framework and guidelines based on a neuroconstructivism perspective to guide intervention development for FASD.
- 12.Vygotsky LS. Mind in society: the development of higher psychological processes. Cambridge, MA: Harvard University Press; 1978. [Google Scholar]
- 13. Olson HC, Oti R, Gelo J, et al. “Family matters:” fetal alcohol spectrum disorders and the family. Dev Disabil Res Rev. 2009;15:235–249. doi: 10.1002/ddrr.65. This article synthesizes multiple sources of information to emphasize the role of family factors on outcomes of people with FASD and the importance of developing interventions with family systems in mind. The authors present a conceptual framework that joins a developmental systems perspective and family systems approach.
- 14.Singer GHS, Ethridge BL, Aldana SI. Primary and secondary effects of parenting and stress management interventions for parents of children with developmental disabilities: a meta-analysis. Ment Retard Dev Disabil Res Rev. 2007;13:357–369. doi: 10.1002/mrdd.20175. [DOI] [PubMed] [Google Scholar]
- 15.Cicchetti D, Toth SL. The past achievements and future promises of developmental psychopathology: the coming of age of a discipline. J Child Psychol & Psychiat. 2009;50:16–25. doi: 10.1111/j.1469-7610.2008.01979.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soh DW, Skocic J, Nash K, et al. Self-regulation therapy increases frontal gray matter in children with fetal alcohol spectrum disorder: evaluation by voxel-based morphometry. Front Hum Neurosci. 2015;9:1–12. doi: 10.3389/fnhum.2015.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dawson G, Jones EJH, Merkle K, et al. Early behavioral intervention is associated with normalized brain activity in young children with autism. J Am Acad Child Adolesc Psychiatry. 2012;51:1150–1159. doi: 10.1016/j.jaac.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chaddock-Heyman L, Erickson KI, Voss MW, et al. The effects of physical activity on functional MRI activation associated with cognitive control in children: a randomized controlled intervention. Front Hum Neurosci. 2013;7:1–13. doi: 10.3389/fnhum.2013.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slopen N, McLaughlin KA, Shonkoff JP. Interventions to improve cortisol regulation in children: a systematic review. Pediatrics. 2014;133:312–326. doi: 10.1542/peds.2013-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van IJzendoorn MH, Bakermans-Kranenburg MJ. Genetic differential susceptibility on trial: meta-analytic support from randomized controlled experiments. Dev Psychopathol. 2015;27:151–162. doi: 10.1017/S0954579414001369. [DOI] [PubMed] [Google Scholar]
- 21.Carr EG, Dunlap G, Horner RH, et al. Positive behavior support: evolution of an applied science. J Posit Behav Interv. 2002;4:4–16. [Google Scholar]
- 22.SAMHSA-HRSA Center for Integrated Health Solutions. A standard framework for levels of integrated health care. Washington D.C: SAMHSA-HRSA Center for Integrated Health Solutions; 2013. [Google Scholar]
- 23.SAMHSA-HRSA Center for Integrated Health Solutions. Integrating behavioral health and primary care for children and youth: concepts and strategies. Washington D.C: SAMHSA-HRSA Center for Integrated Health Solutions; 2013. [Google Scholar]
- 24.O'Connor MJ. Mental health outcomes associated with prenatal alcohol exposure: genetic and environmental factors. Curr Dev Disord Rep. 2014;1:181–188. [Google Scholar]
- 25.Koren G. Breaking the Cycle (BTC) - 20 years of breaking records in managing addicted mothers and their young children. J Popul Ther Clin Pharmacol. 2014;21:e505–e507. [PubMed] [Google Scholar]
- 26.Paley B. Taking the Next Steps: Innovative Interventions for FASD. Atlanta, GA: New approaches to treating FASD in young children. Marcus Autism Center and Emory University School of Medicine Conference; p. 2010. [Google Scholar]
- 27.Liberman AF, Van Horn P. Psychotherapy with infants and young children: repairing the effects of stress and trauma on early development. New York: Guiliford; 2008. [Google Scholar]
- 28.Dozier M, Lindhiem O, Lewis E, et al. Effects of a foster parent training program on young children's attachment behaviors: preliminary evidence from a randomized clinical trial. Child Adolesc Social Work J. 2009;26:321–332. doi: 10.1007/s10560-009-0165-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Olson HC, Jirikowic T, Kartin D, et al. Responding to the challenge of early intervention for fetal alcohol spectrum disorders. Infants Young Child. 2007;20:172–189. [Google Scholar]
- 30.Streissguth AP, Barr HM, Kogan J, et al. Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE) Seattle, WA: 1996. [Google Scholar]
- 31.Paley B, O'Connor MJ, Frankel F, et al. Predictors of stress in parents of children with fetal alcohol spectrum disorders. J Dev Behav Pediatr. 2006;27:396–404. doi: 10.1097/00004703-200610000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Paley B, O'Connor MJ, Kogan N, et al. Prenatal alcohol exposure, child externalizing behavior, and maternal stress. Parenting Science and Practice. 2005;5:29–56. [Google Scholar]
- 33.Watson SL, Coons KD, Hayes SA. Autism spectrum disorder and fetal alcohol spectrum disorder Part I: A comparison of parenting stress. J Intellect Dev Dis. 2013;38:95–104. doi: 10.3109/13668250.2013.788136. [DOI] [PubMed] [Google Scholar]
- 34.Watson SL, Hayes SA, Coons KD, et al. Autism spectrum disorder fetal alcohol spectrum disorder Part II: A qualitative comparison of parenting stress. J Intellect Dev Dis. 2013;38:105–113. doi: 10.3109/13668250.2013.788137. [DOI] [PubMed] [Google Scholar]
- 35.Petrenko CLM, Tahir N, Mahoney EC, et al. Prevention of secondary conditions in fetal alcohol spectrum disorders: identification of systems-level barriers. Matern Child Health J. 2013;18:1496–1505. doi: 10.1007/s10995-013-1390-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Petrenko CLM. A review of intervention programs to prevent and treat behavioral problems in young children with developmental disabilities. J Dev Phys Disabil. 2013;25:651–679. doi: 10.1007/s10882-013-9336-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fisher S. Double ARC Final Report to the CDC - Fetal Alcohol Syndrome Awareness & Education Project. Toledo, OH: 2005. [Google Scholar]
- 38.Coles CD, Kable JA, Taddeo E. Math performance and behavior problems in children affected by prenatal alcohol exposure: intervention and follow-up. J Dev Behav Pediatr. 2009;30:7–15. doi: 10.1097/DBP.0b013e3181966780. [DOI] [PubMed] [Google Scholar]
- 39.Kable JA, Coles CD, Strickland D, et al. Comparing the effectiveness of on-line versus in-person caregiver education and training for behavioral regulation in families of children with FASD. Int J Ment Health Addiction. 2012;10:791–803. doi: 10.1007/s11469-012-9376-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kable JA, Coles CD, Taddeo E. Socio-cognitive habilitation using the math interactive learning experience program for alcohol-affected children. Alcohol Clin Exp Res. 2007;31:1425–1434. doi: 10.1111/j.1530-0277.2007.00431.x. [DOI] [PubMed] [Google Scholar]
- 41.Leenaars LS, Denys K, Henneveld D, et al. The impact of fetal alcohol spectrum disorders on families: evaluation of a family intervention program. Community Ment Health J. 2012;48:431–435. doi: 10.1007/s10597-011-9425-6. [DOI] [PubMed] [Google Scholar]
- 42. Bertrand J. Interventions for children with fetal alcohol spectrum disorders (FASDs): overview of findings for five innovative research projects. Res Dev Disabil. 2009;30:986–1006. doi: 10.1016/j.ridd.2009.02.003. This article presents data from five intervention studies for preschool and school-aged children with FASD funded by the Centers of Disease Control. These five interventions have generally received the most rigorous evaluation to date in the field.
- 43.Greenberg MT, Kusché CA, Cook ET, et al. Promoting emotional competence in school-aged children: The effects of the PATHS curriculum. Dev Psychopathol. 1995;7:117–136. [Google Scholar]
- 44.Domitrovich CE, Cortes RC, Greenberg MT. Improving young children’s social and emotional competence: a randomized trial of the preschool “PATHS” curriculum. J Primary Prevent. 2007;28:67–91. doi: 10.1007/s10935-007-0081-0. [DOI] [PubMed] [Google Scholar]
- 45.Kerns KA, Macsween J, Vander Wekken S, et al. Investigating the efficacy of an attention training programme in children with foetal alcohol spectrum disorder. Dev Neurorehabil. 2010;13:413–422. doi: 10.3109/17518423.2010.511421. [DOI] [PubMed] [Google Scholar]
- 46.Riley EP, Mattson SN, Li T-K, et al. Neurobehavioral consequences of prenatal alcohol exposure: an international perspective. Alcohol Clin Exp Res. 2003;27:362–373. doi: 10.1097/01.ALC.0000052703.38558.B2. [DOI] [PubMed] [Google Scholar]
- 47.Nash K, Stevens S, Greenbaum R, et al. Improving executive functioning in children with fetal alcohol spectrum disorders. Child Neuropsychol. 2014;21:191–209. doi: 10.1080/09297049.2014.889110. [DOI] [PubMed] [Google Scholar]
- 48.Wells AM, Chasnoff IJ, Schmidt CA, et al. Neurocognitive habilitation therapy for children with fetal alcohol spectrum disorders: an adaptation of the alert program®. Am J Occup Ther. 2012;66:24–34. doi: 10.5014/ajot.2012.002691. [DOI] [PubMed] [Google Scholar]
- 49.Williams MS, Shellenberger S. How does your engine run?: A leader’s guide to the alert program for self-regulation. Albuquerque, NM: TherapyWorks; 1996. [Google Scholar]
- 50.Fagerlund Å, Autti-Rämö I, Kalland M, et al. Adaptive behaviour in children and adolescents with foetal alcohol spectrum disorders: a comparison with specific learning disability and typical development. Eur Child Adolesc Psychiatry. 2012;21:221–231. doi: 10.1007/s00787-012-0256-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Crocker N, Vaurio L, Riley EP, et al. Comparison of adaptive behavior in children with heavy prenatal alcohol exposure or attention-deficit/hyperactivity disorder. Alcohol Clin Exp Res. 2009;33:2015–2023. doi: 10.1111/j.1530-0277.2009.01040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Coles CD, Strickland DC, Padgett L, et al. Games that “work”: using computer games to teach alcohol-affected children about fire and street safety. Res Dev Disabil. 2007;28:518–530. doi: 10.1016/j.ridd.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 53.O'Connor MJ, Frankel F, Paley B, et al. A controlled social skills training for children with fetal alcohol spectrum disorders. J Consult Clin Psychol. 2006;74:639–648. doi: 10.1037/0022-006X.74.4.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.O'Connor MJ, Laugeson EA, Mogil C, et al. Translation of an evidence-based social skills intervention for children with prenatal alcohol exposure in a community mental health setting. Alcohol Clin Exp Res. 2012;36:141–152. doi: 10.1111/j.1530-0277.2011.01591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Frankel F, Myatt R. Children's friendship training. New York: Brunner-Routhledge; 2003. [Google Scholar]
- 56.Laugeson EA, Paley B, Schonfeld AM, et al. Adaptation of the children's friendship training program for children with fetal alcohol spectrum disorders. Child & Family Behavior Therapy. 2007;29:57–69. [Google Scholar]
- 57.Schonfeld AM, Paley B, Frankel F, et al. Behavioral regulation as a predictor of response to Children's Friendship Training in children with fetal alcohol spectrum disorders. Clin Neuropsychol. 2009;23:428–445. doi: 10.1080/13854040802389177. [DOI] [PubMed] [Google Scholar]
- 58.Frankel F, Paley B, Marquardt R, et al. Stimulants, neuroleptics, and children's friendship training for children with fetal alcohol spectrum disorders. J Child Adolesc Psychopharmacol. 2006;16:777–789. doi: 10.1089/cap.2006.16.777. [DOI] [PubMed] [Google Scholar]
- 59.Keil V, Paley B, Frankel F, et al. Impact of a social skills intervention on the hostile attributions of children with prenatal alcohol exposure. Alcohol Clin Exp Res. 2010;34:231–241. doi: 10.1111/j.1530-0277.2009.01086.x. [DOI] [PubMed] [Google Scholar]
- 60.Howell KK, Lynch ME, Platzman KA, et al. Prenatal alcohol exposure and ability, academic achievement, and school functioning in adolescence: A longitudinal follow-up. J Pediatr Psychol. 2005;31:116–126. doi: 10.1093/jpepsy/jsj029. [DOI] [PubMed] [Google Scholar]
- 61.Goldschmidt L, Richardson GA, Stoffer DS, et al. Prenatal alcohol exposure and academic achievement at age six: a nonlinear fit. Alcohol Clin Exp Res. 1996;20:763–770. doi: 10.1111/j.1530-0277.1996.tb01684.x. [DOI] [PubMed] [Google Scholar]
- 62.Adnams CM, Sorour P, Kalberg WO, et al. Language and literacy outcomes from a pilot intervention study for children with fetal alcohol spectrum disorders in South Africa. Alcohol. 2007;41:403–414. doi: 10.1016/j.alcohol.2007.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rasmussen C, Bisanz J. Exploring mathematics difficulties in children with fetal alcohol spectrum disorders. Child Dev Perspect. 2009;3:125–130. [Google Scholar]
- 64.Kable JA, Taddeo E, Strickland D, et al. Community translation of the Math Interactive Learning Experience Program for children with FASD. Res Dev Disabil. 2015;39:1–11. doi: 10.1016/j.ridd.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 65.Kully-Martens K, Rasmussen C, Coles C. Canadian implementation of a mathematics intervention for children prenatally exposed to alcohol: current findings and future initiatives; Vancover, BC. 6th International Conference on FASD. [Google Scholar]
- 66.Child Sexual Abuse Task Force and Research Practice Core, National Child Traumatic Stress Network. How to implement trauma-focused cognitive behavioral therapy. Durham, NC and Los Angeles, CA: National Center for Child Traumatic Stress; 2008. [Google Scholar]
- 67.Hyter YD. Prologue: understanding children who have been affected by maltreatment and prenatal alcohol exposure. Lang Speech Hear Serv Sch. 2007;38:93. doi: 10.1044/0161-1461(2007/009). [DOI] [PubMed] [Google Scholar]
- 68.Alati R, Mamun Al A, Williams GM, et al. In utero alcohol exposure and prediction of alcohol disorders in early adulthood: a birth cohort study. Arch Gen Psychiatry. 2006;63:1009–1016. doi: 10.1001/archpsyc.63.9.1009. [DOI] [PubMed] [Google Scholar]
- 69.Baer JS, Sampson PD, Barr HM, et al. A 21-year longitudinal analysis of the effects of prenatal alcohol exposure on young adult drinking. Arch Gen Psychiatry. 2003;60:377–385. doi: 10.1001/archpsyc.60.4.377. [DOI] [PubMed] [Google Scholar]
- 70.O'Connor MJ. New treatments for children and adolescents with FASD. National Organization on Fetal Alcohol Syndrome Webinar Series. Washington, DC: 2014. [Google Scholar]
- 71.Tennku Lepper T. Partners for success intervention for youth and young adults with FASD; Vancover, BC. 6th International Conference on FASD. [Google Scholar]
- 72.Linehan MM. DBT® Skills Training Manual. second edition. Guilford Publications; 2014. [Google Scholar]
- 73.Miller AL, Rathus JH, Linehan MM. Dialectical behavior therapy with suicidal adolescents. Guilford Press; 2006. [Google Scholar]
- 74.Spohr H-L, Willms J, Steinhausen H-C. Fetal alcohol spectrum disorders in young adulthood. J Pediatr. 2007;150:175–179. doi: 10.1016/j.jpeds.2006.11.044. 179.e1. [DOI] [PubMed] [Google Scholar]
- 75.Grant T, Huggins JE, Connor PD, et al. A pilot community intervention for young women with fetal alcohol spectrum disorders. Community Ment Health J. 2004;40:499–511. doi: 10.1007/s10597-004-6124-6. [DOI] [PubMed] [Google Scholar]
- 76.Denys K, Rasmussen C, Henneveld D. The effectiveness of a community-based intervention for parents with FASD. Community Ment Health J. 2009;47:209–219. doi: 10.1007/s10597-009-9273-9. [DOI] [PubMed] [Google Scholar]
- 77. Substance Abuse and Mental Health Services Administration. Addressing fetal alcohol spectrum disorders (FASD) Treatment Improvement Protocol (TIP) Series 58. HH Publication No. (SMA) 13–4803. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. This guide provides important background knowledge and practical guidelines for front line clinicians, administrators, and policy makers in building agency capacity and competence in FASD-informed care.
- 78.Streissguth AP. Fetal alcohol syndrome. 1997 Brookes Pub. [Google Scholar]
- 79.Malbin D. Trying differently rather than harder. Second edition. Portland, OR: Tectrice, Inc; 2002. [Google Scholar]
- 80.Kalberg WO, Buckley DG. FASD: what types of intervention and rehabilitation are useful? Neurosci Biobehav Rev. 2007;31:278–285. doi: 10.1016/j.neubiorev.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 81.Watson S, Westby CE. Strategies for addressing the executive function impairment of students prenatally exposed to alcohol and other drugs. Commun Disord Q. 2003;24:194–204. [Google Scholar]
- 82.Reach to teach: educating elementary and middle school children with fetal alcohol spectrum disorders. DHHS Pub No. SMA-4222. Rockville, MD: Center for Substance Abuse Prevention, Substance Abuse and Mental Health Services Administration; 2007. [Google Scholar]
- 83.Lei H, Nahum-Shani I, Lynch K, et al. A “SMART” design for building individualized treatment sequences. Annu Rev Clin Psychol. 2012;8:21–48. doi: 10.1146/annurev-clinpsy-032511-143152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bermúdez Parsai M, Castro FG, Marsiglia FF, et al. Using community based participatory research to create a culturally grounded intervention for parents and youth to prevent risky behaviors. Prev Sci. 2011;12:34–47. doi: 10.1007/s11121-010-0188-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kazdin AE. Single-case research designs. New York: Oxford University Press; 2011. [Google Scholar]
- 86.Kratochwill TR, Hitchcock JH, Horner RH, et al. Single-case intervention research design standards. Remedial Spec Educ. 2012;34:26–38. [Google Scholar]
- 87.Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- 88.National Institutes of Health Fogarty International Center. [Accessed 15 Mar 2015];Implementation Science Information and Resources. http://www.fic.nih.gov/ResearchTopics/Pages/ImplementationScience.aspx.
- 89.Kelly B, Perkins DF. Handbook of implementation science for psychology in education. New York: Cambridge University Press; 2012. [Google Scholar]
- 90.Chasnoff IJ, Wells AM, King L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics. 2015;135:264–270. doi: 10.1542/peds.2014-2171. [DOI] [PubMed] [Google Scholar]