Abstract
Background
Endometriosis can be intrapelvic or, rarely, extrapelvic. Endometriosis involving the rectus abdominis muscle on the trocar port site is a rare event; until now, only 16 cases have been reported in the literature. The majority of cases were associated with previous abdominal surgery such as diagnostic laparoscopy, cyst excision, appendectomy, myomectomy, or cholecystectomy. We review all the reported cases of this unusual form of extrapelvic endometriosis.
Case Report
We report a new case of abdominal wall endometriosis at the trocar port site in the rectus abdominis muscle in a woman who had undergone 2 laparoscopies for endometriosis in the 3 years before coming to our attention. The diagnosis was made by sonography. We performed a surgical resection of the lesion with a free macroscopic margin of 5-10 mm.
Conclusion
Endometriosis should be considered in the differential diagnosis of any abdominal swelling. In our experience, surgery is the treatment of choice.
Keywords: Abdominal wall, endometriosis, laparoscopy
INTRODUCTION
Endometriosis, classically defined as the presence of endometrial glands and stroma in extrauterine locations, affects 6%-10% of women of reproductive age.1 The most common symptoms of endometriosis include dysmenorrhea, dyspareunia, chronic pelvic pain, and infertility.2 Endometriosis can be classified as intrapelvic or extrapelvic. Intrapelvic endometriosis includes primarily the pelvic peritoneum, ovaries, and rectovaginal septum. The extrapelvic implantation of endometrial tissue has been described in various organs,3 but abdominal endometriosis is the most common extrapelvic localization.4 Abdominal wall endometriosis indicates the presence of ectopic endometriosis located far from the peritoneum, embedded in the subcutaneous fatty tissue and the abdominal wall muscle layers.5 Endometriosis involving the rectus abdominis muscle on the trocar port sites is rare; to our knowledge, only 16 cases have been reported in the literature since the first case in 1990.6 We present an additional case of endometriosis of the trocar port site, followed by a review of the literature about this often-misdiagnosed condition.
CASE REPORT
A 38-year-old woman presented with a palpable nodule in the context of the scar of a previous laparoscopic right trocar port site. The patient's history was significant for endometriosis. She had undergone a laparoscopic removal of an endometriotic cyst from the left ovary and endometriotic nests of the bladder peritoneum in 2011. She reported that the pain in the abdominal wall had started 1 year after the laparoscopic surgery and worsened during the menstrual cycle. She reported heavy intake of nonsteroidal antiinflammatory drugs during the days of severe pain.
During clinical examination, a consistent, painful, round mass approximately 2 cm in diameter was detected at the 5 mm right trocar port site. It was fixed to the surrounding tissues and evoked slight pain with pressure. A transabdominal ultrasound performed with a convex probe (1-5.0 MHz) revealed a 12 × 10 mm hypoechoic lobulated lesion in the subcutaneous tissue close to the muscular plane in the right lower abdominal quadrant. Power-Doppler examination revealed poor and inhomogeneous vascularization. Transvaginal pelvic ultrasound showed adenomyosis but no foci of pelvic endometriosis. The serum level of carcinoma antigen (Ca-125) was within the normal range (12.7 UI/mL).
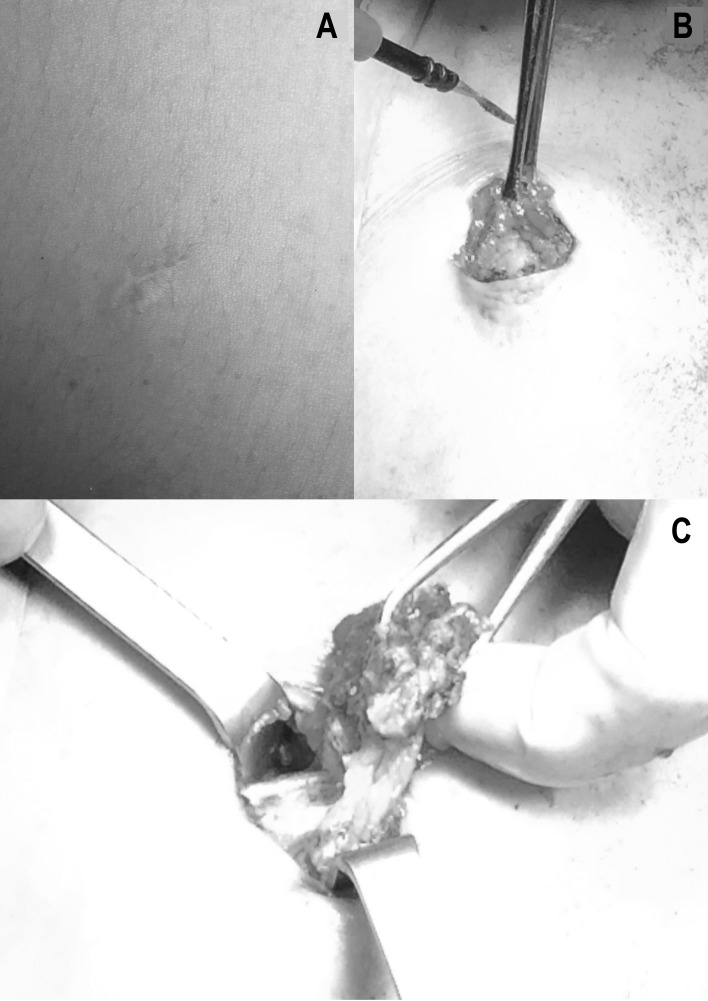
Surgical exploration revealed a 2.5 cm dense mass fixed to the surrounding tissues and extending to the posterior rectus fascia. Through a 3 cm cutaneous incision, a wide excision of the lesion was performed, leaving 5-10 mm of free tissue as surgical margins to prevent recurrences (Figures 1 and 2). The defect was closed with a Safil Quick 2/0 suture (B. Braun Group). A tissue graft was not necessary. The patient's postoperative course was good, and she was discharged the day after surgery. No recurrence of endometriosis was found at a follow-up visit 6 months later. The pathology report confirmed the suspected diagnosis (Figure 3).
Figure 1.
A: Previous scar on the port site. B, C: Removal of the endometriotic nodule through a small incision.
Figure 2.
Removed endometriotic nodule.
Figure 3.
Histologic analysis of the lesion with hematoxylin-eosin staining, showing the glandular stroma with hemorrhagic features.
DISCUSSION
As previously stated, intrapelvic endometriosis includes lesions of fallopian tubes, ovaries, and the pelvic peritoneum. Extrapelvic endometriosis refers to endometriotic implants found in other areas of the body, including the gastrointestinal tract, pulmonary structures, urinary system, abdominal wall, skin, and even the central nervous system.
Abdominal wall endometriosis is a rare localization and is often related to a surgical scar. As the use of laparoscopy has increased, some cases of abdominal wall endometriosis on the trocar port site have been reported in the literature.7,8 Cesarean section is the surgical procedure most frequently associated with abdominal wall endometriosis, with an incidence of approximately 0.03%-1%.9,10
The exact etiopathogenesis of endometriosis remains controversial, and several theories have been proposed, including aerosolization, cellular immunity, coelomic metaplasia, implantation or retrograde menstruation, vascular and lymphatic metastasis, dissemination, and direct transplantation.11
The implantation theory is based on the usual presence (in 80%-90% of cases) of a retrograde menstrual reflux through the fallopian tubes. Normally, refluxed endometrial tissue is cleared from the peritoneum by the immune system, and the dysregulation of this clearance mechanism has been implicated in the implantation and growth of endometrial cells.
The ectopic implant probably requires a combination of several genetic and immunologic factors.12 Endometriosis appears to be a disease related to dysfunctions of immunologic defense mechanisms with a genetic component.13,14
Trocar port site endometriosis might develop from the peritoneal dissemination of cells because of pneumoperitoneum or from direct contact of the excised lesion with the port tract.7,15 Another proposal is that cutaneous endometriosis may arise from endometrial tissue transported via lymphatic or vascular channels.16
In our patient's previous laparoscopy, the endometriotic lesion was removed through the sheath of the instruments. Thus, our case supports the aerosolization theory that pneumoperitoneum influences the implantation of free intraperitoneal endometriotic cells.
Routinely using techniques such as introducing and removing instruments and excised lesions within the sheath to avoid contact with the abdominal wall, using an Endobag (Covidien, PLC) for removal of endometriotic lesions, and exsufflating or washing the abdomen while the trocars are in place may help to prevent endometriotic implants, especially in patients with a history of endometriosis or in whom pelvic endometriosis is revealed during laparoscopy.
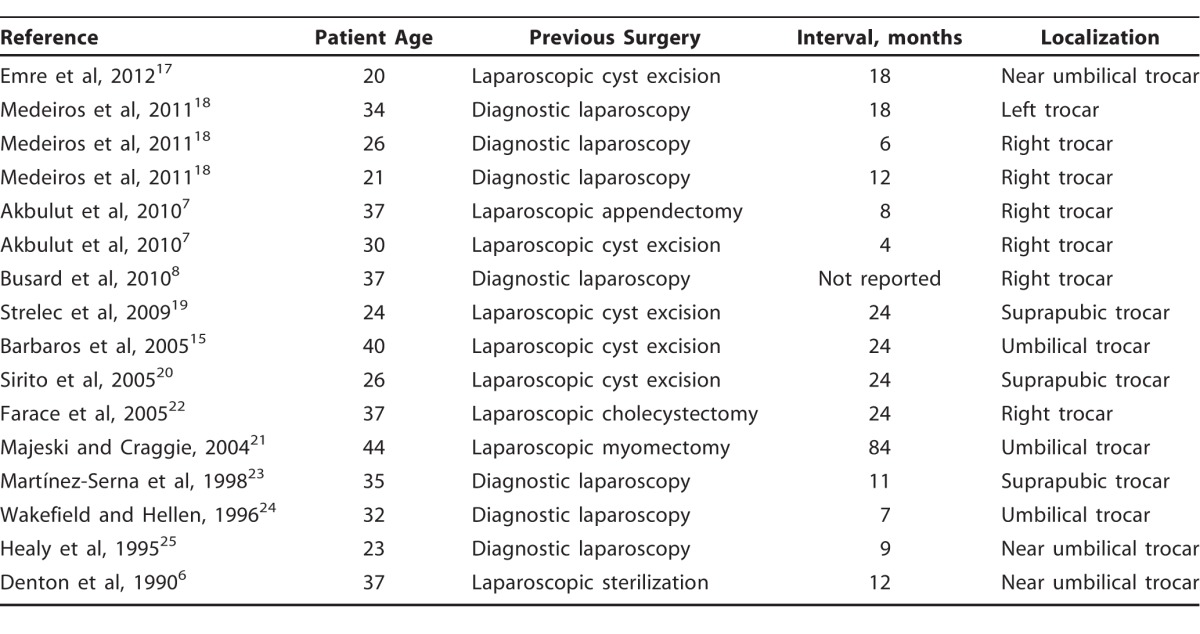
Endometriotic lesions exclusively confined at the trocar site are rare. As far as we know, 16 cases have been described in the literature since the first report by Denton et al.6-8,15,17-25 We report all 16 cases in the Table.
Table.
Cases of Endometriosis on Port Site Described in the Literature
Computed tomograpy (CT) and magnetic resonance imaging (MRI) are not pathognomonic for endometriosis because its appearance depends on the phase of the menstrual cycle, the proportion of stromal and glandular elements, the amount of bleeding, and the degree of inflammatory and fibrotic response.26 In our case, we used ultrasound and not CT or MRI; a high resolution ultrasound is a simple, inexpensive, and safe method and is considered sufficient to indicate the need for surgery.3 MRI and CT are expensive examinations and may also cause a delay in diagnosis. Furthermore, power-Doppler examination revealed a poor and inhomogeneous peripheral vascularization, according to the endometriosis features described in the literature.27
In this rare condition, symptoms are often unspecific, but chronic pain is described as worsening during menses as a typical catamenial pain.
The serum level of Ca-125 can be normal or slightly increased;27 our patient's negative serum level of Ca-125 is in agreement with the literature.
The treatment of choice for endometriosis of the trocar site is a wide local excision of the lesion with at least 5-10 mm of healthy tissue as surgical margin. Great attention must be paid not to break the mass during excision to prevent the reimplantation of microscopic endometrial cells.3,28 We performed as conservative a surgery as possible with a minimal incision on the abdominal wall.
This unusual location of endometriosis should be included in the differential diagnosis with several clinical forms, benign and malignant, including hernia, hematoma, lymphoma, lipoma, abscess, lymphadenopathy, subcutaneous cysts, neuroma, soft tissue sarcoma, desmoid tumor, and metastasis.
CONCLUSION
Our experience agrees with the literature, and we think endometriosis of the trocar port site should be listed in the differential diagnosis of abdominal wall mass in a fertile woman. In particular, it should be suspected in the presence of a typical catamenial pain in women with a history of abdominal-pelvic surgery. Wide excision is the treatment of choice, even for recurrent disease.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012 Sep;98(3):511–519. doi: 10.1016/j.fertnstert.2012.06.029. doi: 10.1016/j.fertnstert.2012.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eskenazi B, Warner ML. Epidemiology of endometriosis. Obstet Gynecol Clin North Am. 1997 Jun;24(2):235–258. doi: 10.1016/s0889-8545(05)70302-8. [DOI] [PubMed] [Google Scholar]
- 3.Calò PG, Ambu R, Medas F, Longheu A, Pisano G, Nicolosi A. Rectus abdominis muscle endometriosis Report of two cases and review of the literature. Ann Ital Chir. 2012 Jun 20;pii: [Epub ahead of print] [PubMed] [Google Scholar]
- 4.Dordevic M, Jovanovic B, Mitrovic S, Dordevic G, Radovanovic D, Sazdanovic P. Abdominal rectus muscle endometriosis after Cesarean section. Extrapelvic localization of endometriosis. Bratisl Lek Listy. 2010;111(6):345–348. [PubMed] [Google Scholar]
- 5.Savelli L, Manuzzi L, Di Donato N, et al. Endometriosis of the abdominal wall: ultrasonographic and Doppler characteristics. Ultrasound Obstet Gynecol. 2012 Mar;39(3):336–340. doi: 10.1002/uog.10052. doi: 10.1002/uog.10052. [DOI] [PubMed] [Google Scholar]
- 6.Denton GW, Schofield JB, Gallagher P. Uncommon complications of laparoscopic sterilisation. Ann R Coll Surg Engl. 1990 May;72(3):210–211. [PMC free article] [PubMed] [Google Scholar]
- 7.Akbulut S, Sevinc MM, Bakir S, Cakabay B, Sezgin A. Scar endometriosis in the abdominal wall: a predictable condition for experienced surgeons. Acta Chir Belg. 2010 May-Jun;110(3):303–307. doi: 10.1080/00015458.2010.11680621. [DOI] [PubMed] [Google Scholar]
- 8.Busard MP, Mijatovic V, van Kuijk C, Hompes PG, van Waesberghe JH. Appearance of abdominal wall endometriosis on MR imaging. Eur Radiol. 2010 May;20(5):1267–1276. doi: 10.1007/s00330-009-1658-1. doi: 10.1007/s00330-009-1658-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horton JD, Dezee KJ, Ahnfeldt EP, Wagner M. Abdominal wall endometriosis: a surgeon's perspective and review of 445 cases. Am J Surg. 2008 Aug;196(2):207–212. doi: 10.1016/j.amjsurg.2007.07.035. doi: 10.1016/j.amjsurg.2007.07.035. [DOI] [PubMed] [Google Scholar]
- 10.Hensen JH, Van Breda Vriesman AC, Puylaert JB. Abdominal wall endometriosis: clinical presentation and imaging features with emphasis on sonography. AJR Am J Roentgenol. 2006 Mar;186(3):616–620. doi: 10.2214/AJR.04.1619. [DOI] [PubMed] [Google Scholar]
- 11.Chang Y, Tsai EM, Long CY, Chen YH, Kay N. Abdominal wall endometriomas. J Reprod Med. 2009 Mar;54(3):155–159. [PubMed] [Google Scholar]
- 12.Zhao X, Lang J, Leng J, Liu Z, Sun D, Zhu L. Abdominal wall endometriomas. Int J Gynaecol Obstet. 2005 Sep;90(3):218–222. doi: 10.1016/j.ijgo.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Esinler I, Guven S, Akyol D. Guvendag Guven ES, Taskiran C, Ayhan A. Abdominal wall endometriosis without previous surgery. J Obstet Gynaecol. 2004 Nov;24(8):931. doi: 10.1080/0144361040019187. [DOI] [PubMed] [Google Scholar]
- 14.Haim N, Shapiro-Feinberg M, Zissin R. Incisional endometriomas: CT findings. Emerg Radiol. 2005 Apr;11(3):162–163. doi: 10.1007/s10140-004-0366-z. [DOI] [PubMed] [Google Scholar]
- 15.Barbaros U, Iyibozkurt AC, Gulluoglu M, et al. Endometriotic umbilical port site metastasis after laparoscopy. Am J Obstet Gynecol. 2005 Nov;193(5):1761–1763. doi: 10.1016/j.ajog.2005.05.088. [DOI] [PubMed] [Google Scholar]
- 16.Friedman PM, Rico MJ. Cutaneous endometriosis. Dermatol Online J. 2000 Sep;6(1):8. [PubMed] [Google Scholar]
- 17.Emre A, Akbulut S, Yilmaz M, Bozdag Z. Laparoscopic trocar port site endometriosis: a case report and brief literature review. Int Surg. 2012 Apr-Jun;97(2):135–139. doi: 10.9738/CC124.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medeiros Fd, Cavalcante DI, Medeiros MA, Eleutério J Jr. Fine-needle aspiration cytology of scar endometriosis: study of seven cases and literature review. Diagn Cytopathol. 2011 Jan;39(1):18–21. doi: 10.1002/dc.21319. [DOI] [PubMed] [Google Scholar]
- 19.Strelec M, Dmitrovic R, Matkovic S. Trocar scar endometriosis. Gynaecol Perinatol. 2009;18(1):34–35. [Google Scholar]
- 20.Sirito R, Puppo A, Centurioni MG, Gustavino C. Incisional hernia on the 5-mm trocar port site and subsequent wall endometriosis on the same site: a case report. Am J Obstet Gynecol. 2005 Sep;193((3 Pt 1)):878–880. doi: 10.1016/j.ajog.2005.02.121. [DOI] [PubMed] [Google Scholar]
- 21.Majeski J, Craggie J. Scar endometriosis developing after an umbilical hernia repair with mesh. South Med J. 2004 May;97(5):532–534. doi: 10.1097/00007611-200405000-00024. [DOI] [PubMed] [Google Scholar]
- 22.Farace F, Gallo A, Rubino C, Manca A, Campus GV. Endometriosis in a trocar tract: is it really a rare condition? A case report. Minerva Chir. 2005 Feb;60(1):67–69. [PubMed] [Google Scholar]
- 23.Martínez-Serna T, Stalter KD, Filipi CJ, Tomonaga T. An unusual case of endometrial trocar site implantation. Surg Endosc. 1998 Jul;12(7):992–994. doi: 10.1007/s004649900763. [DOI] [PubMed] [Google Scholar]
- 24.Wakefield SE, Hellen EA. Endometrioma of the trocar site after laparoscopy. Eur J Surg. 1996 Jun;162(6):523–524. [PubMed] [Google Scholar]
- 25.Healy JT, Wilkinson NW, Sawyer M. Abdominal wall endometrioma in a laparoscopic trocar tract: a case report. Am Surg. 1995 Nov;61(11):962–963. [PubMed] [Google Scholar]
- 26.Coeman V, Sciot R, Van Breuseghem I. Case report. Rectus abdominis endometriosis: a report of two cases. Br J Radiol. 2005 Jan;78(925):68–71. doi: 10.1259/bjr/28183033. [DOI] [PubMed] [Google Scholar]
- 27.Luisi S, Gabbanini M, Sollazzi S, Calonaci F, Razzi S, Petraglia F. Surgical scar endometriosis after Cesarean section: a case report. Gynecol Endocrinol. 2006 May;22(5):284–285. doi: 10.1080/09513590600777578. [DOI] [PubMed] [Google Scholar]
- 28.Toullalan O, Baqué P, Benchimol D, et al. Endometriosis of the rectus abdominis muscles [in French] Ann Chir. 2000 Nov;125(9):880–883. doi: 10.1016/s0003-3944(00)00014-6. [DOI] [PubMed] [Google Scholar]