Abstract
Background
Sister Mary Joseph nodule refers to metastatic malignancy of the periumbilical region. Umbilical metastasis is an indicator of advanced malignant disease.
Case Report
We present the case of an 88-year-old patient presenting with postmenopausal vaginal bleeding, inguinal lymphadenopathy, and physical findings of a palpable umbilical nodule (Sister Mary Joseph nodule). Further workup was consistent with metastatic squamous cell carcinoma of the cervix.
Conclusion
Because Sister Mary Joseph nodule may be the only manifestation of underlying malignancy, thorough physical examination plays an important role in diagnosing the malignancy in a more confined state that may have a positive impact on the patient's length of survival.
Keywords: Carcinoma–squamous cell, neoplasm metastasis, Sister Mary Joseph nodule, uterine cervical neoplasms
INTRODUCTION
Sister Mary Joseph nodule refers to metastatic malignancy of the periumbilical region. The term was coined in 1949 by Sir Hamilton Bailey in honor of Sister Mary Joseph Dempsey (born Julia Dempsey, 1856-1939), Dr William J. Mayo's surgical assistant from 1890 to 1915 at St. Mary's Hospital (presently the Mayo Clinic) in Rochester, MN.1,2 She noted the frequent presence of a nodule in the umbilicus in conjunction with advanced malignancy.
Umbilical metastasis usually signifies a poor prognosis and is an indicator of advanced malignant disease. The survival of these patients is reported to be 2-11 months from diagnosis.3
We present the case of an elderly patient with postmenopausal vaginal bleeding, physical findings of a palpable umbilical nodule (Sister Mary Joseph nodule), and inguinal lymphadenopathy.
CASE REPORT
An 88-year-old African American woman with a medical history of hypertension, diabetes mellitus type 2, chronic obstructive pulmonary disease, stroke, and coronary artery disease status post double coronary artery bypass graft surgery and stent placement presented with a syncopal episode. She had had postmenopausal bleeding for more than 6 months. She also reported loss of appetite and weight but no abdominal pain or change in bowel movements. Physical examination was remarkable for a hard subcutaneous mass in the umbilical area (Sister Mary Joseph nodule), lower abdominal mass, and inguinal lymphadenopathy. The patient refused vaginal examination. Laboratory results revealed a hemoglobin level of 9.6 g/dL, consistent with combined anemia of inflammation and iron deficiency (low iron, low total iron-binding capacity, high ferritin, and low iron saturation).
X-ray of the pelvis showed a large calcified structure, suspicious for a uterine fibroid (Figure 1). Computed tomography (CT) scan of the head without intravenous contrast revealed an ill-defined high-attenuation lesion at the midline and to the right of the midline of the occipital region, suspicious for a neoplasm (Figure 2). Noncontrast CT scan of the chest, abdomen, and pelvis revealed a 2.3 × 2 cm umbilical soft-tissue nodule; a large peripherally calcified uterine mass (8.4 × 8.7 × 8.9 cm); thickening of the cervix with an irregular appearance measuring 5.2 × 3.6 cm; extensive thoracic, retroperitoneal, pelvic, and inguinal lymphadenopathy; and moderate left-sided hydronephrosis (Figure 3).
Figure 1.
X-ray shows a large calcified structure in the pelvis, suspicious for a uterine fibroid.
Figure 2.
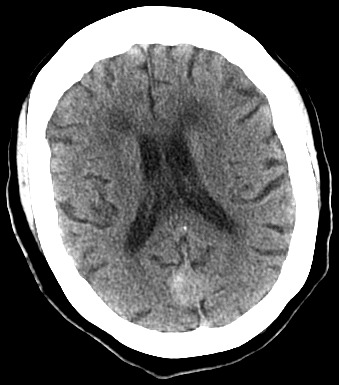
Computed tomography scan of the head without intravenous contrast reveals an ill-defined high attenuation lesion at the midline and to the right of the midline of the occipital region, suspicious for a neoplasm.
Figure 3.
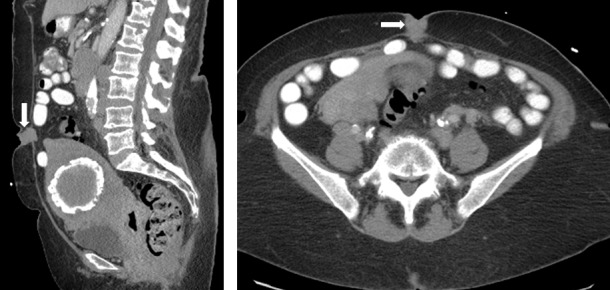
Noncontrast computed tomography scan of the abdomen and pelvis reveals a 2.3 × 2 cm umbilical soft tissue nodule (arrows); a large peripherally calcified uterine mass (8.4 × 8.7 × 8.9 cm); and thickening of the cervix with an irregular appearance measuring 5.2 × 3.6 cm.
Left inguinal lymph node biopsy showed metastatic poorly differentiated squamous cell carcinoma. A diagnosis of advanced metastatic squamous cell carcinoma of the cervix was entertained. The oncology team discussed the diagnosis with the patient and her family, who agreed on best supportive care in view of the patient's poor prognosis and comorbidities.
Later in the course of her hospital stay, the patient experienced increasing abdominal pain, chest pain, and tachycardia. Repeat contrast-enhanced CT scans of the chest, abdomen, and pelvis approximately 8 weeks after initial presentation showed no evidence of acute pulmonary emboli; interval increase in the number and size of mediastinal, abdominal, and pelvic lymphadenopathy; and interval development of moderate ascites and peritoneal and omental implants.
During the night of repeat imaging, the patient became less responsive, developed ventricular fibrillation, and died. An autopsy, excluding head and neck examination, was performed at the family's request and demonstrated large tumoral masses in the abdominal wall, omentum, peritoneum, pelvic wall, and uterus; a markedly thickened cervix; and widespread lymphadenopathy. Histology revealed poorly differentiated squamous cell carcinoma of the uterine-cervical mass with extensive necrosis and metastatic tumors involving the abdominal and pelvic walls, mesentery, bladder, and mediastinal and retroperitoneal lymph nodes.
DISCUSSION
Our case demonstrates a rare finding of Sister Mary Joseph nodule secondary to metastatic squamous cell carcinoma of the cervix. To our knowledge, few similar cases are mentioned in the literature.4,5 Sister Mary Joseph nodule usually represents an adenocarcinoma.3 In a case series of 77 patients with umbilical malignancies, 88% originated outside the umbilicus; the remainder were primary skin tumors.6 The ovary, endometrium, and pancreatobiliary tree are the three most common primary sites in women, whereas the genitourinary tract, pancreatobiliary tree, and the gastrointestinal tract are the three most common sites in men.6 Women are more likely than men to have malignant tumors affecting the umbilicus.6 The histologic grade of the tumors tends to be poorly differentiated.3 Sister Mary Joseph nodule may occur as a dermal, subcutaneous, or peritoneal deposit.7 The mean age of diagnosis is approximately 50 years, with a range of 18-87 years.8 Therefore, our patient may represent the oldest reported case of Sister Mary Joseph nodule.
The possible mechanisms of metastatic spread to the umbilical region include direct extension from a contiguous tumor; hematogenous spread; lymphatic spread; and direct extension along the vestigial remnants of embryonal ligaments, including the round ligament, the urachus, the vitellointestinal duct remnant, and the obliterated vitelline artery.3 Specifically, the umbilical region is connected by the lymphatic system to the axillary, inguinal, and paraaortic lymph nodes and exhibits a rich arterial supply that includes the inferior epigastric and deep circumflex iliac branches of the external iliac artery and the superior epigastric branch of the internal mammary artery.8 In addition are the several venous anastomotic branches from the internal mammary vein, the superficial epigastric vein, and the portal system of the liver.8
The differential diagnosis of an umbilical nodule includes metastasis, primary carcinoma, and other benign causes such as umbilical hernia, endometriosis, lymphangioma, pilonidal sinus, granuloma, fibroepithelial papilloma, dermatofibroma, fibroma, epithelial inclusion cyst, urachal duct cyst, seborrheic keratosis, keloid, foreign body, myxoma, omphalitis, polyp, and abscess.3,7
CONCLUSION
Because Sister Mary Joseph nodule may be the only manifestation of an underlying malignancy, thorough physical examination plays an important role in diagnosing the malignancy in a more confined metastatic state that may have a positive impact on the patient's length of survival.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Windsor LL. Dempsey, Sister Mary Joseph. In: Women in Medicine: an Encyclopedia. Santa Barbara, CA: ABC-CLIO. 2002:58–59. http://books.google.com/books?id=QtZtkf35CF0C&lpg=PP1&pg=PP1#v=onepage&q&f=false. Accessed October 15, 2014. [Google Scholar]
- 2.Bailey H. Demonstrations of Physical Signs in Clinical Surgery. 11th ed. Baltimore, MD: Williams and Wilkins; 1949. [Google Scholar]
- 3.Chalya PL, Mabula JB, Rambau PF, McHembe MD. Sister Mary Joseph's nodule at a university teaching hospital in northwestern Tanzania: a retrospective review of 34 cases. World J Surg Oncol. 2013 Jul 5;11:151. doi: 10.1186/1477-7819-11-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kemfang Ngowa JD, Bechem E, Yomi J, Kasia JM, Kabeyene A. Sister Mary Joseph's nodule originating from carcinoma of uterine cervix: case report at Yaounde General Hospital, Cameroon. Afr J Cancer. 2013 Feb 1;5(1):48–50. [Google Scholar]
- 5.Soares LC, Almeida JP. Sister Mary Joseph nodule and peritoneal carcinomatosis from squamous cell cervical carcinoma. Proc Obstet Gynecol. 2013 Dec 31;3(3):5. [Google Scholar]
- 6.Papalas JA, Selim MA. Metastatic vs primary malignant neoplasms affecting the umbilicus: clinicopathologic features of 77 tumors. Ann Diagn Pathol. 2011 Aug;15(4):237–242. doi: 10.1016/j.anndiagpath.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Coll DM, Meyer JM, Mader M, Smith RC. Imaging appearances of Sister Mary Joseph nodule. Br J Radiol. 1999 Dec;72(864):1230–1233. doi: 10.1259/bjr.72.864.10703486. [DOI] [PubMed] [Google Scholar]
- 8.Iavazzo C, Madhuri K, Essapen S, Akrivos N, Tailor A, Butler-Manuel S. Sister Mary Joseph's nodule as a first manifestation of primary peritoneal cancer. Case Rep Obstet Gynecol. 20122012:467240. doi: 10.1155/2012/467240. [DOI] [PMC free article] [PubMed] [Google Scholar]



