Abstract
Background
Lipopolysaccharide (LPS)/Endotoxin is hypothesized to play an important role in chronic inflammation associated with Type-1 diabetes (T1DM) and its complications. Endotoxin core antibodies (EndoCAb), LPS binding protein (LBP) and soluble CD14 (sCD14) act as modulators of LPS induced activation of innate immune system in vivo. For the present study we estimated the levels of LPS and its translocation markers in T1DM subjects with and without microvascular complications (MVC) and correlate them with clinical parameters of T1DM and serum inflammatory cytokine levels (TNF-α, IL-6, IL-1β and GM-CSF).
Methods
A total of 197 subjects (64 normal glucose tolerance (NGT) subjects, 97 T1DM subjects without MVC and 36 with MVC) were included in this study and the levels of serum LPS, its translocation markers and cytokines measured by immunoassays.
Results
Compared to NGT, T1DM subjects (both with and without MVC) had significantly higher levels of LPS, reduced levels of LBP and EndoCAb along with significant increase in the levels of IL-1β, IL-6, TNF-α and GM-CSF (p<0.05). No significant change was seen in the levels of these biomarkers between T1DM subjects with and without MVC.
Conclusions
Decreased levels of EndoCAb and LBP suggest sustained endotoxin activity in T1DM subjects even before the onset of microvascular complications.
Background
Type-1 diabetes mellitus (T1DM) is a bonafide autoimmune disorder characterized by chronic inflammation with rapid loss of pancreatic beta cells leading to insulin deficiency [1]. However, the exact cause of autoimmunity is not known, even though, both genetic [2] and environmental factors have been implicated [3]. The prevalence of T1DM and other autoimmune diseases has increased dramatically over the past few decades [4]. Although genetic factors may play an important role in the susceptibility to T1DM, the dramatic worldwide increase in prevalence is likely due to changes in the environmental factors [5]. One environmental factor which has gained prominence in recent years is the alterations in gut microbiota which leads to increased gut permeability and metabolic endotoxemia [6]. Bacterial Lipopolysaccaride (LPS)/ endotoxin, a unique glycolipid located at the outer membrane of gram negative bacteria can induce inflammation [7]. More than the actual endotoxin levels, the levels of endogenous anti-endotoxin core antibodies (EndoCAb), LPS binding protein (LBP) and soluble CD14 (sCD14) were found to be more important in determining the activity of endotoxin under in vivo conditions [8]. Studies reporting levels of EndoCAb, LBP and sCD14 in T1DM subjects are not available. While EndoCAb antibodies can neutralize LPS, sCD14 and LPB can augment/antagonize LPS activity in a dose dependent manner. Recent studies have demonstrated chronic inflammation in T1DM subjects with microvascular complications (MVC) with systemic increase in the levels of pro-inflammatory cytokines [9]. We hypothesized that a systemic increase in endotoxemia could aggravate inflammation and promote MVC. The objective of the present study was to estimate the levels of LPS and its translocation markers in T1DM subjects with/without MVC (DN and/or DR) and correlate them with clinical parameters for T1DM and serum inflammatory cytokines (TNF-α, IL-6, IL-1β and GM-CSF).
Materials and Methods
Study participants
Patients with T1DM (n = 133; 97 T1DM without MVC and 36 T1DM with MVC) were recruited from Dr. Mohan’s Diabetes Specialties Centre, Chennai, India. T1DM was diagnosed by the absence of insulin reserve shown by C-peptide assay (C-peptide values < 0.3 pg/ml) and requiring insulin from the time of diagnosis. Subjects with serum glutamic acid decarboxylase (GAD)–specific autoantibody levels ≥ 10 IU/ml were classified as GAD+. Only fasting blood samples were used for all analysis. Institutional Ethical Committee approval was obtained from the Madras Diabetes Research Foundation Ethics Committee (Ref. No.MDRF-EC/SOC/2009/05), and written informed consent was obtained from all the study participants. The study was conducted as per principles of the declaration of Helsinki as revised in 2008.
Study Design and sample size calculation
It is a cross-sectional observational study. Initially, 20 normal glucose tolerant (NGT) and 20 age and gender matched T1DM subjects with and without MVC were used for analysis. On the basis of the preliminary results, with a confidence interval of 95%, an estimated p value < 0.05, and a power of 80%, the sample size was estimated to be 150 ie, 60 NGT subjects, 60 T1DM subjects without MVC and 30 T1DM with MVC. Few more samples were included to account for the large variation seen in serum biomarker levels.
Estimation of biochemical parameters
Blood parameters were measured using a Hitachi-912 Autoanalyser (Hitachi, Mannheim, Germany). Glycated hemoglobin (HbA1c) was estimated by high pressure liquid chromatography (Bio-Rad, Hercules, CA). Urine samples were collected in the early morning after an overnight fast. Urine creatinine was measured using Jaffe’s method. Urine microalbumin concentration was measured using commercially available immunoturbidometric assay kits from Randox (Randox, UK) on Opera Technicon Auto Analyser (Bayer Diagnostics, USA). The urine sample was added to a buffer containing anti-albumin antibody. The turbidity of the resulting solution was measured and the albumin concentration was determined by constructing a standard curve with known concentrations of albumin. The mean inter-assay and intra-assay coefficient of variation were 3.4% and 2.4% respectively. Microalbuminuria was diagnosed if the albumin excretion was between 30 and 299 μg/mg of albumin [10]. The expected protein excretion (EPE) was calculated as the urinary protein to creatinine ratio [11]. The intra- and inter assay coefficient of variation for the biochemical assays ranged between 3.1% and 5.6%.
Screening for microvascular and macrovascular complications
All T1DM subjects were screened for both microvascular (diabetic retinopathy/DR, diabetic nephropathy/DN and diabetic neuropathy) and macrovascular complications (diabetic coronary artery disease/ DM-CAD and perivascular diseases/DM-PVD).
Doppler screening
Doppler screening for PVD was performed by recording of pressure tracings while in the supine position by doppler probe using the KODY Vaslab Machine (Kody Labs, Chennai, India). The ankle–brachial index (ABI) ratio was calculated in every subject as previously described [12].
Retinal photography
Screening for retinopathy was done using four-field stereo colour retinal photography (Zeiss FF 450 plus camera) which were graded by an ophthalmologist using the Early Treatment Diabetic Retinopathy Study (ETDRS) grading system as previously described [13].
Biothesiometry studies
Biothesiometer (Biomedical Instrument Co., Newbury, OH, USA) was used to assess vibratory perception threshold (VPT) of the great toes in a standardized fashion as previously described [12].
Electrocardiogram
Resting 12-lead electrocardiogram (ECG) was performed using Myocard R electrocardiograph (Marks Electronics, Chennai, India) to asses CAD. Carotid Intimal Medial Thickness (IMT) was measured as previously described [13].
Arterial stiffness measurement
Arterial stiffness was measured using the Sphygmocor apparatus (Sphygmocor BPAS-1; PWV Medical, Sydney, Australia). Augmentation index was defined as the difference between the first and second peaks of the central arterial waveform, expressed as a percentage of the pulse pressure as previously described [13].
Definitions and cutoffs
Hypertension
It was diagnosed in subjects who were on antihypertensive medication or had systolic BP≥140 mmHg or diastolic BP ≥90 mmHg as previously described [12, 13].
Diabetic Perivascular disease
An ABI of ≤0.9 was the criterion used for the diagnosis of PVD as per American College of Cardiology Foundation/American Heart Association Task Force (ACCF/AHA) 2011 Guidelines as previously described [12, 13].
Diabetic Coronary Artery Disease
This was diagnosed based on a past history of documented myocardial infarction and/or drug treatment for CAD (aspirin or nitrates) and/or electrocardiographic changes suggestive of ST segment depression and/or Q-wave changes and/or T-wave changes using appropriate Minnesota codes as previously described [12, 13].
Diabetic Retinopathy
The minimum criteria for diagnosis of DR were the presence of at least one definite microaneurysm in any field photographed as previously described [12, 13].
Diabetic Neuropathy
Diagnosed if VPT of the great toe exceeded mean + 2 SD of a healthy nondiabetic population aged 20–45 years (cut point ≥20 V) as previously described [12, 13].
Diabetic Nephropathy
Microalbuminuria was diagnosed if the albumin excretion was between 30 and 299 μg/mg of creatinine and macroalbuminuria/overt nephropathy was diagnosed if albumin excretion was ≥300 μg/mg of creatinine as previously described [12, 13].
Inclusion and exclusion criteria
Only adult type-1 diabetic subjects (age 30–50) were included in the study. The exclusion criteria were patients with type-2 diabetes and T1DM subjects with macrovascular complications including cardiovascular disease and perivascular disease. Patients with a previous diagnosis of urolithiasis or any known renal disease, liver cirrhosis, congestive heart failure, chronic lung diseases, chronic infections and viral hepatitis were also excluded.
Detection of serum LPS and translocation markers
Serum lipopolysaccaride (LPS) activity was determined with a Limulus amoebocyte lysate assay (Hycult Biotechnology). Serum LBP (Hycult Biotechnology), IgG antibody to LPS core (EndoCAb) (Hycult Biotechnology) and sCD14 (R&D Systems, Abingdon, United Kingdom) levels were measured by ELISA. The detection limit for LPS, LBP, sCD14 and EndoCAb were 0.04 Endotoxin Units (EU) /ml, 4.4 ng/ml, 0.125ng/ml and 0.125 EndoCAb Median Unit (EMU)/ml respectively. One EU equals approximately 0.1 to 0.2ng endotoxin/mL.
Estimation of serum pro-inflammatory cytokines
Serum levels of IL-1beta, IL-6, TNF-alpha and GM-CSF were determined by ELISA following kit protocol (Invitrogen CytoSetTM for IL-1β, IL-6 and TNF-α; R&D DuoSet Antibody pair for GM-CSF). The lowest detection limits were: TNF-α-1.0 pg/ml, IL-6- 0.1 pg/ml, IL-1β -0.01 pg/ml and GM-CSF-0.01pg/ml.
Statistical analysis
Student t-test was used to compare groups for continuous variables, whereas χ2 test or Fisher exact test (as appropriate) was used to compare proportions. Mann–Whitney U test was used for multiple pair-wise comparisons that did not show normal distribution. Multiple comparisons were corrected using the Holm’s correction. Spearman’s Correlation analysis was performed between serum inflammatory markers and clinical parameters with the diabetic group. Since there was no statistical difference in the levels of inflammatory markers between the T1DM and T1DM-MVC groups, both groups were pooled for the correlation analysis. All the analyses were done using GraphPad Prism version 5.0 (GraphPad Software, CA, USA) and SPSS statistical package (Version 20.0; SPSS, Chicago, IL). p value less than 0.05 was considered significant.
Results and Discussion
Table 1 shows the clinical and biochemical characteristics of the study subjects. Compared with the NGTs, T1DM subjects (both with/without MVC) had significantly higher levels of FPG and EPE and lower levels of total cholesterol and LDL cholesterol. In general, the serum cholesterol levels as seen in this study (total, LDL and HDL), were 2–3 times higher compared to those values reported in the Caucasian population. This is due to genetic susceptibility of the Asian Indians to hypercholestremiea which is part of the “Asian Indian” or “south-Asian” phenotype. Systolic BP, diastolic BP, serum urea and microalbuminuria were significantly elevated only in the T1DM-MVC group. 3% of T1DM and 5% (T1DM-MVC) had hypertension and were under hypertensive drugs. 37% of T1DM and 28% T1DM-MVC were GAD antibody positive. All the T1DM subjects had well established disease with minimal pancreatic beta cell reserve (as determined by C-peptide assay) and were under insulin. Among subjects with MVC, 42% had diabetic retinopathy (DR), 44% had diabetic nephropathy (DN) and 14% had both DN and DR.
Table 1. Clinical characteristics of the study population.
| Parameters | NGT (n = 64) | T1DM without MVC a (n = 97) | T1DM with MVC b (n = 36) |
|---|---|---|---|
| Gender (male/female) | 32/32 | 49/48 | 19/17 |
| Age [Years] | 30.40 ± 15.76 | 29.02 ± 16.94 | 34.47 ± 16.03 |
| Body mass index [kg/m 2 ] | 20.19 ± 4.07 | 19.66 ± 5.60 | 20.74 ± 4.3 |
| FPG (mmol/L) | 4.72 ±0.33 | 11.3 ± 6.02 *** | 10.4 ± 4.2 *** |
| HbA1c (mmol/mol) | 31.24±12.6 | 93.81 ± 18.17 *** | 93.31 ±25.50 *** |
| 5.0±3.3 | 10.7±3.8 *** | 10.7±4.5 *** | |
| Systolic BP [mm Hg] | 108.7 ± 11.02 | 111.9 ± 15.7 | 119 ± 15.98 ** |
| Diastolic BP [mmHg] | 69.95 ± 8.17 | 71.12 ± 7.57 | 74.67 ± 6.12 * |
| % Hypertensives | Nil | 3% | 5% |
| Total Cholesterol(mmol/L) | 9.38 ± 1.38 | 8.7 ± 2.02 ** | 9.0 ± 1.87 * |
| HDL Cholesterol (mmol/L) | 2.71 ± 0.42 | 2.6 ± 0.65 | 2.86 ± 0.88 |
| LDL Cholesterol (mmol/L) | 6.08 ± 1.59 | 5.1 ± 1.89 ** | 5.08 ± 1.54 ** |
| Serum Triglycerides(mmol/L) | 4.41 ± 1.55 | 4.71 ± 1.91 | 4.79 ± 2.04 |
| GAD positivity [%] | 0 | 37 | 28 |
| Micro albuminuria (mg/dL) | 7.87 ± 12.28 | 8.98 ± 7.61 | 97±107 *** |
| Serum Urea (mmol/L) | 1.12 ± 0.25 | 1.38 ± 0.85 | 1.57 ±1.12* |
| EPE(mg/day) | 103.4 ± 100.5 | 124.9 ± 48.2 *** | 282 ± 397 *** |
| Diabetic Retinopathy(DR) (%) | 0 | 0 | 42 |
| Diabetic Nephropathy(DN) (%) | 0 | 0 | 44 |
| DN + DR (%) | 0 | 0 | 14 |
| Disease duration [Years] | 8.23 ± 7.14 | 13.54 ± 6.57 | |
| Treatment | - | Insulin Anti-hypertensive drugs | Insulin Anti-hypertensive drugs |
a- Comparison between NGT and T1DM;
b- Comparison between NGT and T1DM-MVC.
Data are given as mean± SD for continuos variables and as % for proportions. Statistical significance was determined by One-way ANOVA.
* p< 0.05;
**p< 0.01;
***p<0.0001.
FPG-fasting plasma glucose; HbA1C-glycated hemoglobin. Letters in bold highlight values which are significant.
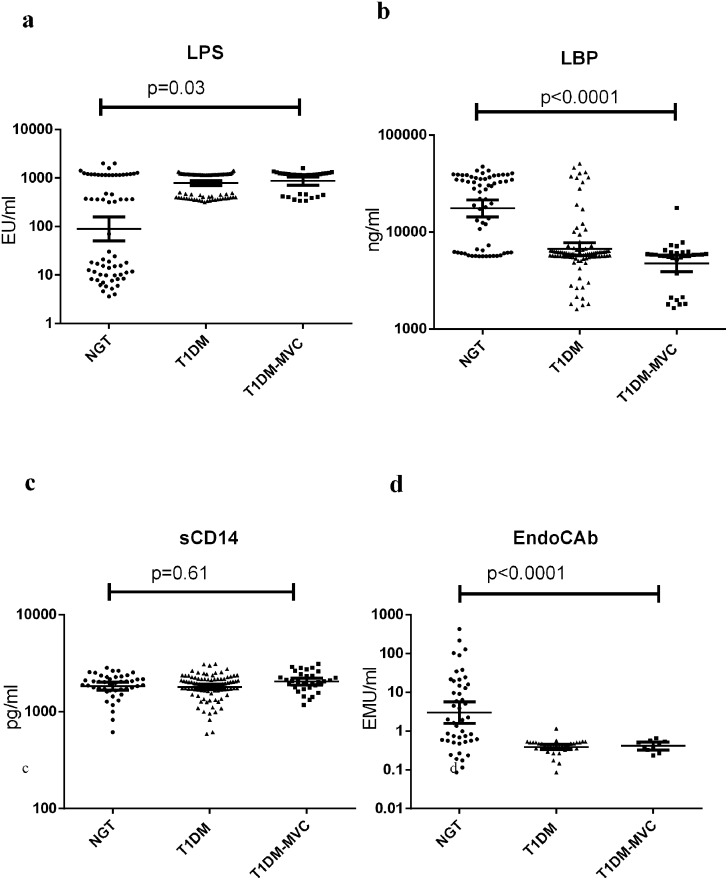
Fig 1 shows the serum levels of LPS, LBP, sCD14 and EndoCAb in NGT and T1DM subjects (with and without MVC). Compared to NGT, T1DM subjects (both with and without MVC) had significantly higher levels of LPS, reduced levels of LBP and EndoCAb with no major difference in the sCD14 levels. T1DM subjects had undetectable levels of EndoCAb. No significant difference was seen in these biomarkers between T1DM subjects with and without MVC. At least among the NGT subjects (Fig 1a), two distinct sub-sects could be identified: one with high levels (MEAN 915 EU/ml) and another with low levels (MEAN 12 EU/ml) of LPS. On further analysis it was found that subjects who had high levels of endotoxemia also had high levels of IL-6, TNF-α and GM-CSF and low levels of LBP and EndoCAb. Interestingly this group also had significantly elevated levels of triglyceridemia (data not shown). Within the T1DM-MVC group, LPS, LBP, sCD14 and EndoCAb levels were not significantly different between those who had retinopathy from those who had microalbuminuria (LPS: DR(Mean ± SD)-1035±354 EU/ml, DN (Mean ± SD)- 943.8±441 EU/ml, p = 0.4; LBP:DR(Mean ± SD)-5± 1.8 μg/ml, DN(Mean ± SD)-6±3.9 μg/ml, p = 0.5; sCD14: DR(Mean ± SD)- 2.2±0.48 μg/ml and DN(Mean ± SD)-2.0±0.46 μg/ml, p = 0.2 and EndoCAb: DR(Mean ± SD)- 0.38±0.16 EMU/ml and DN(Mean ± SD)- 0.43±0.09 EMU/ml, p = 0.7).
Fig 1. T1DM is characterized by systemic endotoxemia with significantly decreased levels of LBP and EndoCAb.
Serum levels of LPS (a), LBP (b), sCD14 (c) and EndoCAb (d) were determined in NGT (n = 64), T1DM without MVC (n = 97) and T1DM subjects with MVC (n = 36) by immune-assays. Each dot represents individual values with the horizontal line representing the geo mean. 36 T1DM subjects without MVC and 26 with MVC had undetectable levels of EndoCAb. Significance was calculated by non-parametric Mann–Whitney U test and p<0.05 was considered significant. The indicated p values are for pair-wise comparisons.
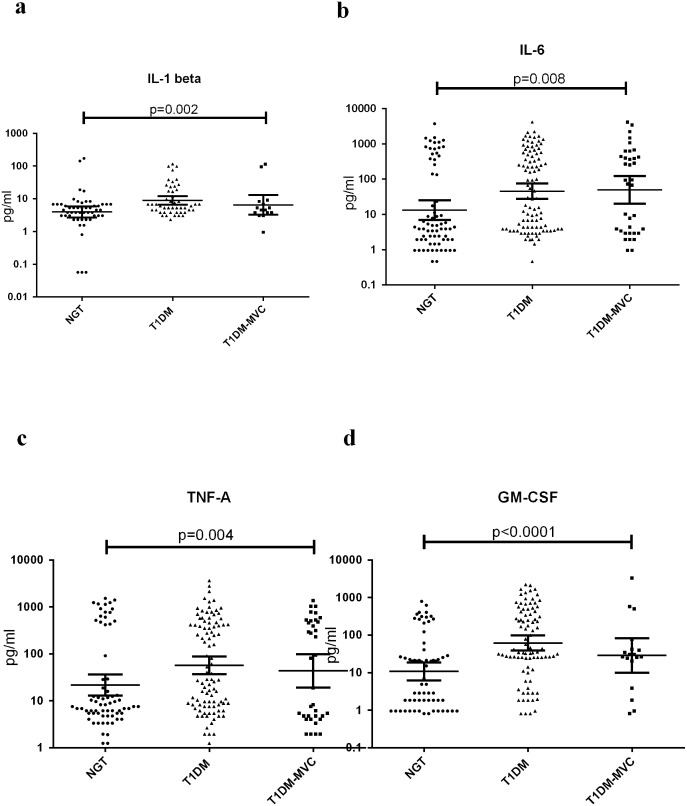
Fig 2 shows the serum levels of TNF-α, IL-6, IL-1β and GM-CSF in NGT and T1DM subjects (with and without MVC). Compared to NGT, TIDM subjects (both with and without MVC) had significantly elevated levels of TNF-α, IL-6, IL-1β and GM-CSF in the serum. No significant difference was seen in cytokine levels between T1DM subjects with and without MVC. Spearman’s correlation analysis within the diabetic group (S1 Table) showed positive correlation of LPS levels with FGP, EPE, IL-1β, IL-6, TNF-α and GM-CSF. LBP levels showed a negative correlation with BMI, FPG, SBP, DBP, TGL, EPE, IL-1β and IL-6 levels. EndoCAb showed negative correlation with FPG, EPE TNF-α and GM-CSF levels.
Fig 2. T1DM is characterized by systemic inflammation with high levels of serum pro-inflammatory cytokines.
Serum levels of IL-1β (a), IL-6 (b), TNF-α (c), and GM-CSF (d) were determined in NGT (n = 64), T1DM without MVC (n = 97) and T1DM subjects with MVC (n = 36) by ELISA. Each dot represents individual values with the horizontal line representing the geo mean. Significance was calculated by non-parametric Mann–Whitney U test and p<0.05 was considered significant. The indicated p values are for pair-wise comparisons.
In the present study, we attempted to investigate LPS and its translocation markers in T1DM subjects with/without MVC by measuring serum LPS, EndoCAb, sCD14 and LBP along with serum cytokines and other clinical parameters. The major findings of the study are: 1. T1DM subjects with/without MVC had significantly higher levels of LPS and lower levels of LBP and EndoCAb with no significant change in the sCD14 levels compared to NGT. 2. However, even for these markers, there was no significant difference between T1DM subjects with and without MVC and 3. While LPS showed a positive correlation FPG and pro-inflammatory cytokines (IL-1β, IL-6 and TNF-α), LBP and EndoCAb showed negative association with these markers.
Changes in gut microbiota leading to leaky gut have now been identified as a major etiological factor for chronic inflammation as seen in T1DM [14]. Previously, increased levels of serum Zonulin, a gap-junction protein which serves as a marker for gut permeability was found to be significantly elevated in T1DM subjects indicating leaky gut [15]. However, comparatively very few studies have looked at the end result of leaky gut which is the metabolic endotoxemia and associated inflammation. Recently, increased levels of serum LPS in T1DM subjects with metabolic syndrome and/or kidney disease was reported [16, 17]. However, the levels of sCD14, LBP and EndoCAb which are the major regulators of LPS activity under in vivo conditions were not reported in these subjects. LBP is an acute-phase protein that enhances the LPS responsiveness of immune cells by transferring LPS to CD14 [18]. Even though an acute-phase protein, LPB levels were not significantly elevated in T1DM subjects. Previously, we have reported metabolic endotoxemia with no significant change in serum LBP levels in coronary artery disease (CAD) patients [19], which is a classical chronic inflammatory condition. However, others have reported significantly elevated LBP levels under conditions of chronic inflammation like obesity [20], Type-2 diabetes [21] and non-alcoholic fatty-liver disease [22]. The disparity could be due to the biphasic role of LBP in LPS induced chronic inflammation: At lower concentrations it can actually fuel inflammation while at higher concentrations it tends to neutralize LPS activity and promotes its degradation [23]. High levels of LBP inhibit the LPS responses in monocytes and can protect both humans [24] and mice [25] from septic shock caused by LPS or gram-negative bacterial infection. The low level of LBP seen in the T1DM subjects suggests increased activity of LPS in these subjects. Low levels of LBP has also been reported under conditions of extra-pulmonary tuberculosis [26] and active filariasis [27]. However, this is the first report, to the best of our knowledge, to show low LBP levels in autoimmunity. Serum EndoCAb levels serve as good prognostic marker for post-operative mortality rate associated with acute inflammation as seen in septicemia and endotoxemia [28]. But the significance of EndoCAb levels under conditions of autoimmunity is less well explored. Our study for the first time showed low levels of EndoCAb in T1DM subjects.
The moderate endotoxemia with decreased EndoCAb and LBP together suggests sustained immune activation resulting in chronic inflammation. The end result is a systemic increase in the levels of IL-1β, TNF-α, IL-6 and GM-CSF, as seen in this study. Several immune and non-immune cells express LPS receptor (TLR4) and respond to LPS stimulation by secreting pro-inflammatory cytokines [29]. The end result is a systemic increase in the levels of IL-1β, TNF-α, IL-6 and GM-CSF in the T1DM subjects as seen in this study. Our results are in agreement with previous reports were in elevated levels of IL-1β and IL-6 were reported in T1DM subjects [30]. Recently we reported increased levels of serum GM-CSF levels in T2DM subjects which were associated with the activated phenotype of dendritic cells [31]. Like T2DM, GM-CSF levels were found to be elevated even in T1DM subjects as can be seen in this study.
Conclusion
To summarize, chronic low-grade endotoxemia, as seen in the case of T1DM, was associated with decreased levels of LBP and EndoCAb and with elevated levels of TNF-α, IL-6, IL-1β and GM-CSF, indicating chronic inflammation. The most important finding of this study is that, this phenomenon was seen even during the early stages of the disease and seems to persist till the late stages of the disease were in MVC sets in, indicating that, yet to be identified factors may play a role in the onset of MVC in T1DM subjects. One of the limitations of this study is that, being cross-sectional in nature, no conclusions regarding a causal relationship between autoimmunity, endotoxemia and inflammation can be made. Further, since the prevalence of T1DM is less than 1% [32] this study was performed in a limited sample size with known diabetic subjects. However, the strength of this study is that, it systematically reviews all the components of microbial translocation in age and gender matched T1DM subjects in a non-Caucasians population were in the incidence of T1DM has started increasing. In summary, this study suggests that T1DM in Asian Indians is characterized by high levels of LPS and pro-inflammatory cytokines and low levels of EndoCAb and LBP.
Supporting Information
(DOC)
Acknowledgments
The project was partially funded by DST FAST TRACK (http://www.serb.gov.in/home.php) grant obtained by VA (SR/FT/LS-105/2009). This study was also supported by the Intramural Research Program of the Division of Intramural Research, NIAID, NIH, US. The Dept of Genetics, University of Madras has received funds for infrastructural support from DST-FIST and UGC-SAP programs. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Abbreviations
- T1DM
Type-1 diabetes mellitus
- MVC
microvascular complication
- NGT
Normal glucose tolerance
- LPS
Lipopolysaccharide
- LBP
Lipopolysaccharide binding protein
- sCD14
Soluble cluster differentiation 14
- EndoCAb
Endotoxin core antibody
- TNF-α
Tumor necrosis factor- alpha
- IL-1β
Interleukin-1 beta
- GM-CSF
Granulocyte macrophage colony stimulating factor
- IL-6
Interleukin-6
- FPG
Fasting Plasma Glucose
- SBP
Systolic Blood Pressure
- DBP
Diastolic Blood Pressure
- LDL
Low Density Lipoprotein
- HDL
High Density Lipoprotein
- TGL
Triglyceride Lipids
- DN
Diabetic Nephropathy
- DR
Diabetic Retinopathy
- EPE
Expected Protein Excretion
- GAD
Glutamate decarboxylase
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The project was partially funded by DST FAST TRACK (http://www.serb.gov.in/home.php) grant obtained by VA (SR/FT/LS-105/2009). This study was also supported by the Intramural Research Program of the Division of Intramural Research, NIAID, NIH, US. The Dept of Genetics, University of Madras has received funds for infrastructural support from DST-FIST and UGC-SAP programs. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Knip M, Siljander H. Autoimmune mechanisms in type 1 diabetes. Autoimmun Rev 2008;7: 550–7. 10.1016/j.autrev.2008.04.008 [DOI] [PubMed] [Google Scholar]
- 2. Notkins AL. Immunologic and genetic factors in type 1 diabetes. J Biol Chem 2002;277: 43545–8. [DOI] [PubMed] [Google Scholar]
- 3. Peng H, Hagopian W. Environmental factors in the development of Type 1 diabetes. Rev Endocr Metab Disord 2006;7: 149–62. [DOI] [PubMed] [Google Scholar]
- 4. Cooper GS, Bynum ML, Somers EC. Recent insights in the epidemiology of autoimmune diseases: improved prevalence estimates and understanding of clustering of diseases. J Autoimmun 2009;33: 197–207. 10.1016/j.jaut.2009.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nistico L, Iafusco D, Galderisi A, Fagnani C, Cotichini R, Toccaceli V, et al. Emerging effects of early environmental factors over genetic background for type 1 diabetes susceptibility: evidence from a Nationwide Italian Twin Study. J Clin Endocrinol Metab 2012;97: E1483–91. [DOI] [PubMed] [Google Scholar]
- 6. Vaarala O. Leaking gut in type 1 diabetes. Curr Opin Gastroenterol 2008;24: 701–6. 10.1097/MOG.0b013e32830e6d98 [DOI] [PubMed] [Google Scholar]
- 7. Bosshart H, Heinzelmann M. Targeting bacterial endotoxin: two sides of a coin. Ann N Y Acad Sci 2007;1096: 1–17. [DOI] [PubMed] [Google Scholar]
- 8. Mussap M, Noto A, Fravega M, Fanos V. Soluble CD14 subtype presepsin (sCD14-ST) and lipopolysaccharide binding protein (LBP) in neonatal sepsis: new clinical and analytical perspectives for two old biomarkers. J Matern Fetal Neonatal Med 24 Suppl 2: 12–4. [DOI] [PubMed] [Google Scholar]
- 9. Navarro-Gonzalez JF, Mora-Fernandez C. The role of inflammatory cytokines in diabetic nephropathy. J Am Soc Nephrol 2008;19: 433–42. 10.1681/ASN.2007091048 [DOI] [PubMed] [Google Scholar]
- 10. Unnikrishnan RI, Rema M, Pradeepa R, Deepa M, Shanthirani CS, Deepa R, et al. Prevalence and risk factors of diabetic nephropathy in an urban South Indian population: the Chennai Urban Rural Epidemiology Study (CURES 45). Diabetes Care 2007;30: 2019–24. [DOI] [PubMed] [Google Scholar]
- 11. Mohan V, Shah S, Saboo B. Current glycemic status and diabetes related complications among type 2 diabetes patients in India: data from the A1chieve study. J Assoc Physicians India 2013;61: 12–5. [PubMed] [Google Scholar]
- 12. Eshcol J, Jebarani S, Anjana RM, Mohan V, Pradeepa R. Prevalence, incidence and progression of peripheral arterial disease in Asian Indian type 2 diabetic patients. J Diabetes Complications 2014;28: 627–31. 10.1016/j.jdiacomp.2014.04.013 [DOI] [PubMed] [Google Scholar]
- 13. Pradeepa R, Surendar J, Indulekha K, Chella S, Anjana RM, Mohan V. Relationship of diabetic retinopathy with coronary artery disease in Asian Indians with type 2 diabetes: the Chennai Urban Rural Epidemiology Study (CURES) Eye Study—3. Diabetes Technol Ther 2015;17: 112–8. 10.1089/dia.2014.0141 [DOI] [PubMed] [Google Scholar]
- 14. Vaarala O, Atkinson MA, Neu J. The "perfect storm" for type 1 diabetes: the complex interplay between intestinal microbiota, gut permeability, and mucosal immunity. Diabetes 2008;57: 2555–62. 10.2337/db08-0331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sapone A, de Magistris L, Pietzak M, Clemente MG, Tripathi A, Cucca F, et al. Zonulin upregulation is associated with increased gut permeability in subjects with type 1 diabetes and their relatives. Diabetes 2006;55: 1443–9. [DOI] [PubMed] [Google Scholar]
- 16. Nymark M, Pussinen PJ, Tuomainen AM, Forsblom C, Groop PH, Lehto M. Serum lipopolysaccharide activity is associated with the progression of kidney disease in finnish patients with type 1 diabetes. Diabetes Care 2009;32: 1689–93. 10.2337/dc09-0467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lassenius MI, Pietilainen KH, Kaartinen K, Pussinen PJ, Syrjanen J, Forsblom C, et al. Bacterial endotoxin activity in human serum is associated with dyslipidemia, insulin resistance, obesity, and chronic inflammation. Diabetes Care 34: 1809–15. 10.2337/dc10-2197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vreugdenhil AC, Rousseau CH, Hartung T, Greve JW, van 't Veer C, Buurman WA. Lipopolysaccharide (LPS)-binding protein mediates LPS detoxification by chylomicrons. J Immunol 2003;170: 1399–405. [DOI] [PubMed] [Google Scholar]
- 19. Aravindhan V, Madhumitha H, Valarmathi S, Babu S. Increased Levels of Endotoxin Core Antibodies and Decreased Levels of sCD 14 Indicate Chronic Endotoxemia in Coronary Artery Disease (CURES-127). Journal of Clinical & Experimental Cardiology 2013;4: 1–6. [Google Scholar]
- 20. Gonzalez-Quintela A, Alonso M, Campos J, Vizcaino L, Loidi L, Gude F. Determinants of serum concentrations of lipopolysaccharide-binding protein (LBP) in the adult population: the role of obesity. PLoS One 2013;8: e54600 10.1371/journal.pone.0054600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Monte SV, Caruana JA, Ghanim H, Sia CL, Korzeniewski K, Schentag JJ, et al. Reduction in endotoxemia, oxidative and inflammatory stress, and insulin resistance after Roux-en-Y gastric bypass surgery in patients with morbid obesity and type 2 diabetes mellitus. Surgery 2012;151: 587–93. 10.1016/j.surg.2011.09.038 [DOI] [PubMed] [Google Scholar]
- 22. Ruiz AG, Casafont F, Crespo J, Cayon A, Mayorga M, Estebanez A, et al. Lipopolysaccharide-binding protein plasma levels and liver TNF-alpha gene expression in obese patients: evidence for the potential role of endotoxin in the pathogenesis of non-alcoholic steatohepatitis. Obes Surg 2007;17: 1374–80. [DOI] [PubMed] [Google Scholar]
- 23. Gutsmann T, Muller M, Carroll SF, MacKenzie RC, Wiese A, Seydel U. Dual role of lipopolysaccharide (LPS)-binding protein in neutralization of LPS and enhancement of LPS-induced activation of mononuclear cells. Infect Immun 2001;69: 6942–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zweigner J, Gramm HJ, Singer OC, Wegscheider K, Schumann RR. High concentrations of lipopolysaccharide-binding protein in serum of patients with severe sepsis or septic shock inhibit the lipopolysaccharide response in human monocytes. Blood 2001;98: 3800–8. [DOI] [PubMed] [Google Scholar]
- 25. Lamping N, Dettmer R, Schroder NW, Pfeil D, Hallatschek W, Burger R, et al. LPS-binding protein protects mice from septic shock caused by LPS or gram-negative bacteria. J Clin Invest 1998;101: 2065–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pavan Kumar N, Anuradha R, Andrade BB, Suresh N, Ganesh R, Shankar J, et al. Circulating biomarkers of pulmonary and extrapulmonary tuberculosis in children. Clin Vaccine Immunol 2013;20: 704–11. 10.1128/CVI.00038-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Anuradha R, George PJ, Pavan Kumar N, Fay MP, Kumaraswami V, Nutman TB, et al. Circulating microbial products and acute phase proteins as markers of pathogenesis in lymphatic filarial disease. PLoS Pathog 2012;8: e1002749 10.1371/journal.ppat.1002749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moretti EW, Newman MF, Muhlbaier LH, Whellan D, Petersen RP, Rossignol D, et al. Effects of decreased preoperative endotoxin core antibody levels on long-term mortality after coronary artery bypass graft surgery. Arch Surg 2006;141: 637–41; discussion 642. [DOI] [PubMed] [Google Scholar]
- 29. Alkanani AK, Rewers M, Dong F, Waugh K, Gottlieb PA, Zipris D. Dysregulated Toll-like receptor-induced interleukin-1beta and interleukin-6 responses in subjects at risk for the development of type 1 diabetes. Diabetes 2012;61: 2525–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cavallo MG, Pozzilli P, Bird C, Wadhwa M, Meager A, Visalli N, et al. Cytokines in sera from insulin-dependent diabetic patients at diagnosis. Clin Exp Immunol 1991;86: 256–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Surendar J, Mohan V, Pavankumar N, Babu S, Aravindhan V. Increased levels of serum granulocyte-macrophage colony-stimulating factor is associated with activated peripheral dendritic cells in type 2 diabetes subjects (CURES-99). Diabetes Technol Ther 2012;14: 344–9. 10.1089/dia.2011.0182 [DOI] [PubMed] [Google Scholar]
- 32. Amutha A, Datta M, Unnikrishnan IR, Anjana RM, Rema M, Narayan KM, et al. Clinical profile of diabetes in the young seen between 1992 and 2009 at a specialist diabetes centre in south India. Prim Care Diabetes 2011;5: 223–9. 10.1016/j.pcd.2011.04.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.