Abstract
Introduction Various lateral and anterior approaches to access the infratemporal fossa (ITF) have been described. We provide our observations regarding the endoscopic transpterygoid and preauricular subtemporal approaches, listing their respective advantages and limitations through cadaveric dissection.
Methods A cadaver study was performed on five adult specimens. An endoscopic transpterygoid approach to the ITF was completed bilaterally in three specimens, and an open preauricular ITF approach was performed bilaterally in two specimens.
Results After completing the cadaveric dissections, we studied differences between the endoscopic transpterygoid approach and open preauricular subtemporal approaches in regard to exposure and ease of dissection of different structures in the ITF.
Conclusions In comparison with a lateral approach, the endonasal endoscopic transpterygoid approach provides better visualization and more direct exposure of median structures such as the nasopharynx, eustachian tube, sella, and clivus. We concluded that the endoscopic transpterygoid approach can be utilized to resect benign lesions and some select group of malignancies involving the infratemporal and middle cranial fossae. Open approaches continue to play an important role, especially in the resection of extensive malignant tumors extending to these regions.
Keywords: infratemporal fossa, transpterygoid approach, preauricular subtemporal approach, V2, V3
Introduction
The infratemporal fossa (ITF) is a deep quadrangular space inferior to the base of the middle cranial fossa. Its limits are represented anteriorly by the maxillary tuberosity and the maxillary sinus, superiorly by the greater wing of the sphenoid bone and part of the temporal bone, medially by the lateral plate of the pterygoid process and the lateral wall of the pharynx; laterally by the temporalis muscle and the mandibular ramus; and inferiorly by a horizontal plane passing through the inferior border of the angle of the mandible.1 2 3 4 Current skull base surgical approaches to the ITF, notably those used for the resection of large voluminous tumors, are the product of successive technical innovations such as the transmandibular approach reported by Conley and by Crockett,5 6 the transzygomatic approaches reported by Barbosa and by Samii et al, and the posterolateral infratemporal approaches reported byFisch.7 8 9 Deriving from surgical techniques used in craniomaxillofacial traumatology, in particular those of Obwegeser, Sekhar et al described a preauricular anterolateral infratemporal approach.10 11 12 This lateral approach offers a large exposure of the entire ITF, which is important not solely for a satisfactory extirpation of a tumor but also for the reduction of functional and cosmetic consequences.13 In addition, concomitant progress in imaging techniques has added to our anatomical understanding as well as to more effective surgical planning.
Endoscopic endonasal transpterygoid approaches have recently provided new corridors to access a variety of pathologies in the paramedian and lateral skull base. An endoscopic endonasal transpterygoid approach was first described to access the lateral recess of the sphenoid sinus and was subsequently modified and expanded to manage lesions of the petrous apex, middle cranial fossa, and ITF.14 15 16 17 Understanding the complex anatomical relationships of the ITF from the endoscopic perspective is mandatory before attempting an endoscopic endonasal transpterygoid approach.18 19 20 Familiarity with microsurgical anatomy of the ITF and dissection techniques via anterior and lateral approaches is helpful but may not be sufficient to dominate all aspects of endonasal endoscopic surgery in this area.21 22 23 24 25 26
Our aim was to demonstrate the differences between both approaches that are used to reach the ITF via cadaveric dissection to study the exposure and limitations of each approach.
Materials and Methods
Our cadaveric study received an institutional review board exemption because the dissections were performed on deidentified cadaveric specimens. However, both the Anatomy Laboratory Toward Visuospatial Surgical Innovations in Otolaryngology and Neurosurgery, Wexner Medical Center at Ohio State University, and researchers are certified by regulatory agencies dealing with the use of human tissues and cadaveric studies. Using standardized methods, all specimens were injected through the internal carotid artery and internal jugular vein with red and blue silicone, respectively.
We dissected the ITF and pterygopalatine fossa (PPF) bilaterally in five human anatomical specimens, performing endoscopic dissections in three and open preauricular approaches in two. Visualization, photographs, and videos were made possible by the use of 0-, 30-, and 45-degree rod lens endoscopes coupled to a high-definition camera and monitor (Storz Endoscopy, Tuttlingen, Germany). The surgical dissections were performed using paranasal sinus and skull base/neurosurgical endoscopic instruments (Storz Endoscopy, Tuttlingen, Germany), and a high-speed drill with angled handpiece, and diamond and cutting 4-mm burrs (Total Performance System, Stryker, Kalamazoo, Michigan, United States).
Endoscopic Endonasal Approach
Access to the PPF and ITF was obtained after performing an endoscopic medial maxillectomy and complete removal of the posterior wall of the maxillary antrum using Kerrison rongeurs. We extended the medial maxillectomy anteriorly to increase the exposure of the lateral wall of the antrum and, subsequently the lateral aspect of the ITF. However, for maximal exposure, the pyriform aperture and ascending process of the maxilla were removed, dissecting and sharply transecting the nasolacrimal duct (endoscopic Denker or Sturman-Canfield approach).To further enhance the angle of the approach, we completed a posterior septectomy to manipulate instruments from the contralateral nasal cavity. Dissection of the investing periosteum and removal of the fat of the PPF allowed the identification of the main terminal branches of the maxillary artery including the infraorbital, posterior nasal, sphenopalatine, and descending palatine arteries. Transection of these branches allowed the exposure of the underlying neural structures. Resection of the lateral pterygoid muscle and drilling the lateral pterygoid plate allowed exposure of V3 that lies posterior to the lateral pterygoid plate (Figs. 1 and 2).
Fig. 1.
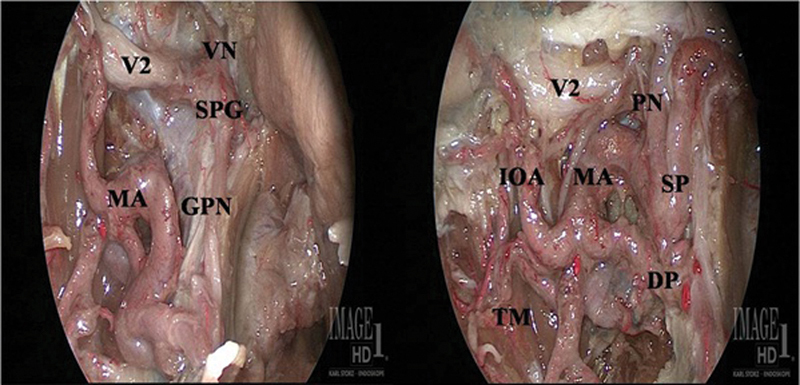
Endoscopic 0-degree view after dissection of right infratemporal fossa. DP, descending palatine artery; GPN, greater palatine nerve; IOA, infraorbital artery; MA, maxillary artery; PN, posterior nasal artery; SP, sphenopalatine artery; SPG, sphenopalatine ganglion; TM, temporalis muscle; V2, maxillary nerve; VN, vidian nerve.
Fig. 2.
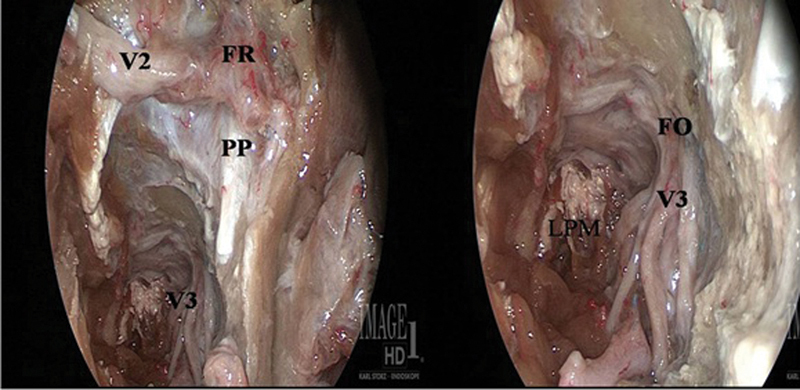
Endoscopic 0-degree view after dissection of right infratemporal fossa. FO, foramen ovale; FR, foramen rotundum; LPM, lateral pterygoid muscle; PP, pterygoid plate; V2, maxillary nerve; V3, mandibular nerve.
Identification of the portion of the infraorbital nerve traversing the infraorbital fissure and dissection of the nerve medially and posteriorly allowed us to reach the maxillary nerve and foramen rotundum. Two prominent muscles came in full view: the temporalis and the lateral pterygoid muscles that could be differentiated by their respective vertically and horizontally oriented fibers Then, we dissected and identified of the second part of the internal maxillary artery superficial or deep to lateral pterygoid muscle. The middle meningeal artery could be seen medial to the lateral pterygoid muscle, coursing superiorly toward the foramen spinosum.
Preauricular Temporal- Subtemporal Approach
A coronal incision was made extending from the tragus of the ear on one side to the contralateral temporoparietal suture. The scalp flap was elevated in the subgaleal plane. The deep temporalis fascia was incised down to the zygomatic arch identifying the layer of fat lying between the superficial and deep layers of the deep temporal fascia. An oblique incision was then made through the superficial layer of the deep temporal fascia, following an imaginary line connecting the temporal root of the zygoma to the orbital rim. The superficial layer of the deep temporal fascia, which is continuous with the orbitozygomatic periosteum, was raised en bloc with the skin flap protecting the zygomatic branches of the facial nerve. The supraorbital neurovascular bundle was identified and, if necessary, released from its bony canal with an osteotome.
The extent of orbitozygomatic osteotomies is variable and may involve the complete translocation, including the lateral orbit, or the arch alone and the orbital rim. The posterior cut is made just flush to the temporal squama just posterior and superior to the articular eminence of the mandibular (i.e., glenoid) fossa. The need for translocating the isolated arch or the entire orbitozygomatic complex dictates the level of the anterior osteotomy. After transecting the masseter muscle, the orbitozygomatic segment was removed revealing the temporalis insertion into the coronoid process of the mandible. The coronoid process was dissected, transecting the insertion of the temporalis muscle and improving the ability to retract the muscle inferiorly, therefore widening the corridor into the ITF. Elevation of the temporalis muscle superior to the infratemporal crest of the greater wing of the sphenoid exposes the middle and deep temporal vessels. The temporalis muscle was then dissected off the squama of the temporal bone.
Elevation of the temporalis muscle exposed the medial and lateral pterygoid muscles. The lateral pterygoid muscle was divided. The maxillary artery muscular segment (second part) was encountered and divided. Following resection of the upper (infratemporal) head of the lateral pterygoid muscle, it was possible to identify the mandibular nerve and its branches, which could be followed proximally to the foramen ovale. The pterygoid plates are immediately anterior to the foramen ovale. The lateral aspect of the lateral pterygoid plate was exposed superiorly by gentle stripping of the lateral pterygoid muscle off the bony surface. The dissection was then taken anteriorly and the pterygomaxillary fissure exposed. Exposure of the maxillary nerve at the level of the foramen rotundum was augmented by removing the root of the lateral pterygoid plate (greater wing of the sphenoid) with a high-speed drill.
For complete exposure of the foramen ovale and foramen spinosum, a low temporal craniotomy was opened. This allows the safe removal of the greater wing of the sphenoid under direct vision and the exposure of the contents of the foramen ovale, foramen spinosum, and foramen rotundum by resection of the greater wing of the sphenoid lateral to these foramina (i.e., floor of the middle fossa) (Figs. 3 and 4).
Fig. 3.
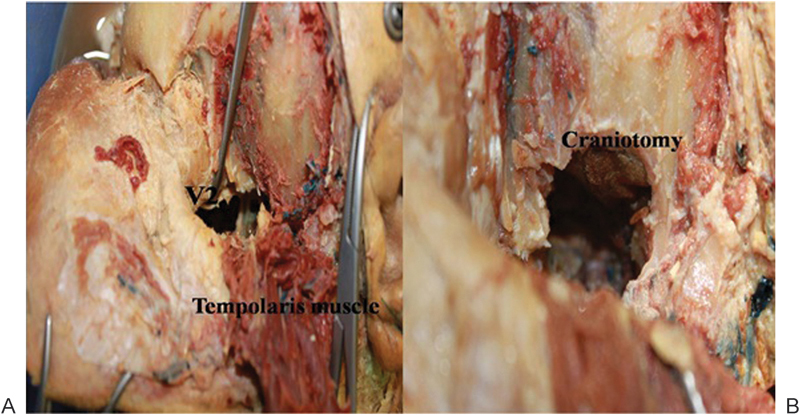
Exposure seen from above via preauricular subtemporal approach. (A) Exposure of maxillary nerve. (B) Craniotomy for exposure of foramen rotundum and foramen ovale.
Fig. 4.
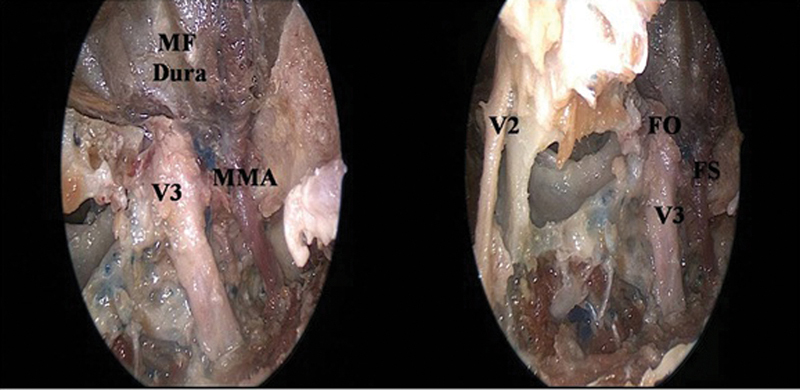
Exposure of the infratemporal fossa via the preauricular subtemporal approach (photograph taken with the aid of a 0-degree endoscope [left side]). FO, foramen ovale; FS, foramen spinosum; MF, middle fossa; MMA, middle meningeal artery; V2, maxillary nerve; V3, mandibular nerve.
Results
Table 1 shows the differences between the endoscopic transpterygoid approach and open preauricular subtemporal approaches in regard to the exposure and dissection of different structures in the ITF.
Table 1. Critical differences in anatomical dissection of the infratemporal fossa: endoscopic versus open approach.
| Endoscopic transpterygoid approach | Preauricular subtemporal approach | |
|---|---|---|
| Exposure in relation to depth of dissection | Better exposure of midline and paramedian structures with deeper dissection | Restricted exposure of these structures with deeper dissection |
| External skin incision | No | Bicoronal skin incision |
| Risk of facial nerve injury | No | Risk if dissection in superficial plane |
| Injury to temporalis muscle | Minimal risk | Yes; postoperative pain and trismus are common |
| Injury to pterygoid muscles | Lateral pterygoid is usually divided | Sometimes divided |
| Maxillary artery exposure | Mainly for third part with its terminal branches like sphenopalatine and infraorbital branches | Mainly for the second part with muscular and buccal branches |
| Foramen rotundum and maxillary nerve | Easily visualized and dissected without orbital entrance | Requires removal of lateral orbital rim for exposure |
| Nerve of pterygoid canal | Easily visualized | Not visualized |
| Foramen ovale and spinosum | Requires drilling out the lateral pterygoid plate | Easily visualized from above after craniotomy |
| Exposure of middle fossa dura | Difficult except for medial aspect (Meckel cave) | Easy to perform complementary craniotomy for wide exposure |
| Risk of injury to Internal carotid artery | Possible to injure the parapharyngeal part of internal carotid artery if the dissection continues deep and lateral or the petrous part of the internal carotid artery, if the dissection extends to the middle cranial fossa | Also possible according to the extent of dissection but could be controlled from this approach |
Discussion
Multiple surgical approaches to the ITF have been described. They may be classified as anterior, lateral, or the recently advanced endoscopic endonasal transpterygoid approach. Selection of the approach depends on the histopathology, location of the lesion, extensions of the lesion, and also the experience of the surgeon.
Among the anterior approaches, access to the ITF is best afforded by the extended maxillotomy/maxillectomy and the facial translocation approach. Hitotsumatsu and Rhoton21 reviewed the surgical anatomy of both of these approaches and their combination with other approaches to access lesions of the skull base. The facial translocation approach seems best because it provides unhindered access to the anterior and middle cranial base, the ITF, nasopharynx, and clivus. It is perhaps best described as an anterolateral approach that extends medially to include the maxillary sinus and nasopharynx. However, this approach carries the risk of facial deformity, transection of the temporalis muscle, and injury to the frontal branch of the facial nerve and infraorbital nerve. In addition, reconstruction of the lacrimal system may be required.27 28 29 30 31 32
Various lateral approaches have been the mainstay surgery management for lesions of the ITF. Classically, the approaches described by Fisch and Pillsbury, alone or in combination with subtemporal/infratemporal approaches, yielded good access to the region of the temporal bone and ITF.33 34 However, facial nerve trauma secondary to its translocation, conductive hearing loss, and mandibular malocclusion due to disarticulation of the temporomandibular joint (TMJ) remain significant drawbacks to these approaches.
Obwegeser described a (subcranial) lateral transzygomatic approach to the ITF, posterior maxilla, and orbits and labeled it a “temporal” approach.10 Obwegeser's approach is suitable for pathology confined to the ITF itself or invading the ITF from adjacent areas (other than the base of the skull/middle cranial fossa).Orbital exposure is limited compared with the more extensive exposure possible with a craniotomy and resection of the greater wing of the sphenoid. A major disadvantage of this approach is that the exposure becomes more restricted as the depth of dissection increases.
In view of its limited medial access, this approach is best for the treatment of benign pathology in the superior aspect of the ITF. Malignant disease is most commonly and adequately approached through either a transmaxillary or transmandibular approach as previously described. As mentioned, the role of a lateral transzygomatic approach in the treatment of malignant disease involving the ITF is mainly a supplementary approach combined with other more extensive approaches for tumor resection.35
Clinical implications of endoscopic endonasal approaches for the management of lesions of the anterior skull base from the planum sphenoidale to clivus were previously described.17 36 37 38
A transpterygoid dissection expands the lateral exposure, thus gaining access to the ITF, middle cranial fossa, and petrous apex.16 39 40 41 Compared with lateral approaches to the ITF, the endonasal endoscopic transpterygoid approach provides better visualization and direct exposure of midline structures such as the nasopharynx, eustachian tube, sella, and clivus. In addition, it provides excellent exposure of the foramen rotundum, maxillary nerve, vidian nerve, foramen ovale, and V3 by drilling of the lateral pterygoid plate and dissection of the lateral pterygoid muscle. Some bleeding from the pterygoid venous plexus is expected; therefore hemostatic agents, bipolar cautery, and warm saline irrigation need to be available.41 One of the possible sequelae of transpterygoid approach to the ITF is loss of sensation to the hard palate and ipsilateral upper dentition after sacrifice of the palatine nerves and dental branches of V2. Some trismus can occur as a result from scarring after resection of the lateral pterygoid muscle.
Furthermore, endoscopic endonasal transpterygoid approaches avoid morbidities that are inherent to lateral and anterior open approaches such as cosmetic issues regarding skin incision, bony osteotomies, or TMJ pain and dysfunction, paralysis of facial nerve itself or its branches, craniotomy, and possible brain retraction. An important drawback of the endoscopic endonasal transpterygoid approaches is the limited exposure of the parapharyngeal internal carotid artery (ICA). We need to mobilize the medial pterygoid muscle and eustachian tube to identify the ICA in the medial wall of the ITF. Sometimes we need to expose the ICA proximally in the neck to gain adequate control.
Most benign tumors like juvenile angiofibromas and schwannomas can be resected completely using an endoscopic approach. Some malignant tumors, especially those displacing rather than invading important neurovascular structures in the ITF, can be removed safely through the endoscopic approach. Invasive malignant tumors extending to the ITF, such as maxillary sinus cancer or mandibular cancer, most often mandate a traditional open surgical approach as and extended preauricular subtemporal approach combined with an anterior approach that enables proximal ICA control, resection of primary tumor, and exenteration of the soft tissues of the ITF.
Postoperative cerebrospinal fluid leak and possible intracranial infections are of great concern. However, the introduction of the nasoseptal flap has dramatically lowered the incidence of postoperative cerebrospinal fluid leak and the incidence of meningitis following transpterygoid approach to the ITF.42 Open combined approaches are often associated with large defects that frequently require either a regional or even a microvascular free flap reconstructive method such as an anterolateral thigh free flap. This markedly increases the time of surgery and may cause morbidity for the patients. However, this corresponds mainly to the extent of the disease and is not a caveat of the approach.
Conclusions
Endoscopic transpterygoid approaches have become standard for most benign and select malignant tumors that involve the ITF and middle cranial fossa. Open approaches play an important role, especially in the resection of large malignant tumors of the maxilla and mandible, and combined with other craniofacial approaches for tumors resection. A large multicenter clinical study is recommended to illustrate the role of each approach in tumor resection and their long-term effects especially in tumor recurrence.
References
- 1.Guerrier Y. La fosse infra-temporale et la fosse ptérygo-palatine. Cahiers d'ORL de Chir Cervico-Faciale Audiophonol. 1985;20:655–663. [Google Scholar]
- 2.Legent F, Beauvillain C, De Kersaint-Gilly A, Leroy G, Rousseau A. Fosse ptérygo-maxillaire (fossa infra-temporalis). Division topographique. Moyens d'exploration. Abord trans-mandibulaire de la région des ptérygoïdiens. Ann Otol Laryngol (Paris) 1981;98:435–442. [PubMed] [Google Scholar]
- 3.Rabischong P, Guerrier Y, Vignaud J, Trassera J, Tolosa F. Bases anatomiques de l'abord de la fosse ptérygo-palatine. Anat Clin. 1980;2:209–222. [Google Scholar]
- 4.Robert R, Legent F, Rogez J M. et al. The infratemporal fossa: a trial clarification. Surg Radiol Anat. 1989;11(4):307–311. doi: 10.1007/BF02098703. [DOI] [PubMed] [Google Scholar]
- 5.Conley J J. The surgical approach to the pterygoid area. Ann Surg. 1956;144(1):39–43. doi: 10.1097/00000658-195607000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crockett D J. Surgical approach to the back of the maxilla. Br J Surg. 1963;50:819–821. doi: 10.1002/bjs.18005022613. [DOI] [PubMed] [Google Scholar]
- 7.Barbosa J F. Surgery of extensive cancer of paranasal sinuses. Presentation of a new technique. Arch Otolaryngol. 1961;73:129–138. doi: 10.1001/archotol.1961.00740020135001. [DOI] [PubMed] [Google Scholar]
- 8.Samy L L, Girgis I H. Transzygomatic approach for nasopharyngeal fibromata with extrapharyngeal extension. J Laryngol Otol. 1965;79(9):782–795. doi: 10.1017/s0022215100064379. [DOI] [PubMed] [Google Scholar]
- 9.Fisch U. Infratemporal fossa approach to tumours of the temporal bone and base of the skull. J Laryngol Otol. 1978;92(11):949–967. doi: 10.1017/s0022215100086382. [DOI] [PubMed] [Google Scholar]
- 10.Obwegeser H L. Temporal approach to the TMJ, the orbit, and the retromaxillary-infracranial region. Head Neck Surg. 1985;7(3):185–199. doi: 10.1002/hed.2890070302. [DOI] [PubMed] [Google Scholar]
- 11.Sekhar L N, Schramm V L Jr, Jones N F. Subtemporal-preauricular infratemporal fossa approach to large lateral and posterior cranial base neoplasms. J Neurosurg. 1987;67(4):488–499. doi: 10.3171/jns.1987.67.4.0488. [DOI] [PubMed] [Google Scholar]
- 12.Shibuya T Y, Doerr T D, Mathog R H. et al. Functional outcomes of the retromaxillary-infratemporal fossa dissection for advanced head and neck/skull base lesions. Skull Base Surg. 2000;10(3):109–117. doi: 10.1055/s-2000-9319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tiwari R, Quak J, Egeler S. et al. Tumors of the infratemporal fossa. Skull Base Surg. 2000;10(1):1–9. doi: 10.1055/s-2000-6789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bolger W E. Endoscopic transpterygoid approach to the lateral sphenoid recess: surgical approach and clinical experience. Otolaryngol Head Neck Surg. 2005;133(1):20–26. doi: 10.1016/j.otohns.2005.03.063. [DOI] [PubMed] [Google Scholar]
- 15.DelGaudio J M. Endoscopic transnasal approach to the pterygopalatine fossa. Arch Otolaryngol Head Neck Surg. 2003;129(4):441–446. doi: 10.1001/archotol.129.4.441. [DOI] [PubMed] [Google Scholar]
- 16.Fortes F S, Sennes L U, Carrau R L. et al. Endoscopic anatomy of the pterygopalatine fossa and the transpterygoid approach: development of a surgical instruction model. Laryngoscope. 2008;118(1):44–49. doi: 10.1097/MLG.0b013e318155a492. [DOI] [PubMed] [Google Scholar]
- 17.Kassam A B, Gardner P, Snyderman C, Mintz A, Carrau R. Expanded endonasal approach: fully endoscopic, completely transnasal approach to the middle third of the clivus, petrous bone, middle cranial fossa, and infratemporal fossa. Neurosurg Focus. 2005;19(1):E6. [PubMed] [Google Scholar]
- 18.Herzallah I R, Germani R, Casiano R R. Endoscopic transnasal study of the infratemporal fossa: a new orientation. Otolaryngol Head Neck Surg. 2009;140(6):861–865. doi: 10.1016/j.otohns.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 19.Theodosopoulos P V, Guthikonda B, Brescia A, Keller J T, Zimmer L A. Endoscopic approach to the infratemporal fossa: anatomic study. Neurosurgery. 2010;66(1):196–202; discussion 202–203. doi: 10.1227/01.NEU.0000359224.75185.43. [DOI] [PubMed] [Google Scholar]
- 20.Zimmer L A, Hart C, Theodosopoulos P V. Endoscopic anatomy of the petrous segment of the internal carotid artery. Am J Rhinol Allergy. 2009;23(2):192–196. doi: 10.2500/ajra.2009.23.3292. [DOI] [PubMed] [Google Scholar]
- 21.Hitotsumatsu T, Rhoton A L Jr. Unilateral upper and lower subtotal maxillectomy approaches to the cranial base: microsurgical anatomy. Neurosurgery. 2000;46(6):1416–1452; discussion 1452–1453. doi: 10.1097/00006123-200006000-00025. [DOI] [PubMed] [Google Scholar]
- 22.Isolan G R, Rowe R, Al-Mefty O. Microanatomy and surgical approaches to the infratemporal fossa: an anaglyphic three-dimensional stereoscopic printing study. Skull Base. 2007;17(5):285–302. doi: 10.1055/s-2007-985193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vrionis F D, Cano W G, Heilman C B. Microsurgical anatomy of the infratemporal fossa as viewed laterally and superiorly. Neurosurgery. 1996;39(4):777–785; discussion 785–786. doi: 10.1097/00006123-199610000-00027. [DOI] [PubMed] [Google Scholar]
- 24.Falcon R T, Rivera-Serrano C M, Miranda J F. et al. Endoscopic endonasal dissection of the infratemporal fossa: anatomic relationships and importance of eustachian tube in the endoscopic skull base surgery. Laryngoscope. 2011;121(1):31–41. doi: 10.1002/lary.21341. [DOI] [PubMed] [Google Scholar]
- 25.Hosseini S M, Razfar A, Carrau R L. et al. Endonasal transpterygoid approach to the infratemporal fossa: correlation of endoscopic and multiplanar CT anatomy. Head Neck. 2012;34(3):313–320. doi: 10.1002/hed.21725. [DOI] [PubMed] [Google Scholar]
- 26.Prosser J D, Figueroa R, Carrau R I, Ong Y K, Solares C A. Quantitative analysis of endoscopic endonasal approaches to the infratemporal fossa. Laryngoscope. 2011;121(8):1601–1605. doi: 10.1002/lary.21863. [DOI] [PubMed] [Google Scholar]
- 27.Cocke E W, Jr, Robertson J H. Philadelphia, PA: Lippincott-Raven; 1998. Extended unilateral maxillotomy approach; pp. 207–237. [Google Scholar]
- 28.Cocke E W Jr, Robertson J H, Robertson J T, Crook J P Jr. The extended maxillotomy and subtotal maxillectomy for excision of skull base tumors. Arch Otolaryngol Head Neck Surg. 1990;116(1):92–104. doi: 10.1001/archotol.1990.01870010096026. [DOI] [PubMed] [Google Scholar]
- 29.James D, Crockard H A. Surgical access to the base of skull and upper cervical spine by extended maxillotomy. Neurosurgery. 1991;29(3):411–416. doi: 10.1097/00006123-199109000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Janecka I P, Sen C N, Sekhar L N, Arriaga M. Facial translocation: a new approach to the cranial base. Otolaryngol Head Neck Surg. 1990;103(3):413–419. doi: 10.1177/019459989010300312. [DOI] [PubMed] [Google Scholar]
- 31.Janecka I P. Classification of facial translocation approach to the skull base. Otolaryngol Head Neck Surg. 1995;112(4):579–585. doi: 10.1177/019459989511200412. [DOI] [PubMed] [Google Scholar]
- 32.Janecka I P, Sen C N, Sekhar L N, Nuss D W. New York, NY: Raven Press; 1993. Facial translocation approach to the nasopharynx, clivus, and infratemporal fossa; pp. 245–259. [Google Scholar]
- 33.Fisch U, Pillsbury H C. Infratemporal fossa approach to lesions in the temporal bone and base of the skull. Arch Otolaryngol. 1979;105(2):99–107. doi: 10.1001/archotol.1979.00790140045008. [DOI] [PubMed] [Google Scholar]
- 34.Sekhar L N, Møller A R. Operative management of tumors involving the cavernous sinus. J Neurosurg. 1986;64(6):879–889. doi: 10.3171/jns.1986.64.6.0879. [DOI] [PubMed] [Google Scholar]
- 35.Mickey B, Close L, Schaefer S, Samson D. A combined frontotemporal and lateral infratemporal fossa approach to the skull base. J Neurosurg. 1988;68(5):678–683. doi: 10.3171/jns.1988.68.5.0678. [DOI] [PubMed] [Google Scholar]
- 36.Kassam A, Snyderman C H, Mintz A, Gardner P, Carrau R L. Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to the sella turcica. Neurosurg Focus. 2005;19(1):E3. [PubMed] [Google Scholar]
- 37.Kassam A, Snyderman C H, Mintz A, Gardner P, Carrau R L. Expanded endonasal approach: the rostrocaudal axis. Part II. Posterior clinoids to the foramen magnum. Neurosurg Focus. 2005;19(1):E4. [PubMed] [Google Scholar]
- 38.Kassam A B Snyderman C Gardner P Carrau R Spiro R The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process: technical case report Neurosurgery 200557(1, Suppl):E213; discussion E213 [DOI] [PubMed] [Google Scholar]
- 39.Kassam A B Prevedello D M Carrau R L et al. The front door to Meckel's cave: an anteromedial corridor via expanded endoscopic endonasal approach- technical considerations and clinical series Neurosurgery 200964(3, Suppl):ons71–ons82.; discussion ons82–ons83 [DOI] [PubMed] [Google Scholar]
- 40.Zanation A M, Snyderman C H, Carrau R L, Gardner P A, Prevedello D M, Kassam A B. Endoscopic endonasal surgery for petrous apex lesions. Laryngoscope. 2009;119(1):19–25. doi: 10.1002/lary.20027. [DOI] [PubMed] [Google Scholar]
- 41.Kassam A, Snyderman C H, Carrau R L, Gardner P, Mintz A. Endoneurosurgical hemostasis techniques: lessons learned from 400 cases. Neurosurg Focus. 2005;19(1):E7. [PubMed] [Google Scholar]
- 42.Kassam A B Thomas A Carrau R L et al. Endoscopic reconstruction of the cranial base using a pedicled nasoseptal flap Neurosurgery 200863101ONS44–ONS52.; discussion ONS52–ONS53 [DOI] [PubMed] [Google Scholar]


