Abstract
Objectives
The objectives of this community-wide observational study were to describe nearly two decade long (1986–2003) trends in the use of lipid lowering therapy in patients hospitalized with acute myocardial infarction (AMI) and clinical and demographic factors associated with underutilization of this treatment regimen.
Methods
A total of 9,429 greater Worcester (MA) residents hospitalized with confirmed AMI at all metropolitan Worcester medical centers in 10 annual periods between 1986 and 2003 comprised the study population. Hospital medical records were reviewed to ascertain the prescribing of lipid lowering agents during hospitalization for AMI.
Results
The mean age of the study sample was 70 years, 58% were men, and the average total and LDL serum cholesterol levels were 203 and 114 mg/dL, respectively. There was a marked increase in the use of lipid lowering therapy in greater Worcester residents hospitalized with AMI between 1986 (<1%) and 2003 (76%). Increasing use of lipid lowering medication was observed both with regards to the maintenance of this therapy in patients who were already on this treatment regimen and in the new initiation of lipid lowering medication in patients who had not been previously treated with this therapy. Several patient demographic and clinical factors, including advanced age and an initial AMI, were associated with the failure to be prescribed lipid lowering therapy during hospitalization for AMI.
Conclusions
The results of this study suggest encouraging increases over time in the use of lipid lowering therapy in patients hospitalized with AMI. Despite these encouraging trends, several high-risk patient groups remain suboptimally treated.
Keywords: lipid lowering therapy, acute myocardial infarction, community-based
INTRODUCTION
Hyperlipidemia is recognized as a major modifiable risk factor for the development and progression of coronary heart disease (CHD). Considerable evidence also suggests that lipid-lowering therapy reduces the risk of recurrent coronary events and improves survival in patients with acute myocardial infarction (AMI) (1–4).
Despite the availability of effective lipid lowering treatment regimens, several studies have documented low treatment rates of elevated serum cholesterol levels in patients with established coronary artery disease (5,6). The National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) guidelines call for the earlier and more aggressive lowering of LDL cholesterol levels in patients with confirmed CHD (7). These guidelines also suggest that serum lipids should be measured at an early time during hospitalization for an acute coronary syndrome in order that patient’s serum lipid profile can be adequately characterized and appropriate treatment prescribed.
The Worcester Heart Attack Study is an ongoing observational study of greater Worcester (MA) residents hospitalized with confirmed AMI at all metropolitan Worcester medical centers (8–10). This population-based investigation offers a unique opportunity to examine recent, and more than decade long (1986 to 2003), trends in the use of lipid lowering therapy in metropolitan Worcester residents hospitalized with AMI. An additional objective of the present study was to characterize the demographic and clinical profile of patients in whom lipid lowering therapy was underutilized.
METHODS
Residents of the Worcester metropolitan area hospitalized with a primary or secondary discharge diagnosis of AMI (International Classification of Disease [ICD-9] code 410) from all Worcester Standard Metropolitan Statistical Area (SMSA) hospitals during 1986, 1988, 1990, 1991, 1993, 1995, 1997, 1999, 2001, and 2003 comprised the study population of this report (8–10). The present study is part of an ongoing investigation that is examining changing trends in the incidence, hospital, and long-term case-fatality rates in residents of the Worcester SMSA hospitalized with independently confirmed AMI (8–10). While additional earlier study years were included in this investigation, we restricted our study sample to patients hospitalized with AMI from 1986 to the most recent year of data collection in 2003. This period was selected for purposes of examining relatively contemporary, and more than decade long, trends in lipid lowering medication patterns. This period was also selected for purposes of capturing the introduction of lipid lowering therapy, particularly statins, to clinical practice beginning in the mid-1980’s. The 10 study periods were originally selected due to the availability of grant funding and for purposes of examining changes over time in our principal study endpoints on an approximate alternate yearly basis. All hospitals (n=11) in the Worcester SMSA (2000 census population = 478,000) participated in this study.
The medical records of greater Worcester residents with a discharge diagnosis of AMI from these Central Massachusetts hospitals were individually reviewed and validated according to pre-established diagnostic criteria that have been previously described (8–10). In brief, these criteria included a clinical history of prolonged chest pain not relieved by rest or use of nitrates, increases in serum CPK-MB levels in excess of the upper limit of normal as specified by the laboratory at each greater Worcester hospital, and serial electrocardiographic tracings during hospitalization showing changes in the ST segment and/or Q waves typical of AMI. At least 2 of these 3 criteria needed to be satisfied for study inclusion. Elevation of troponin findings was not a criterion for the diagnosis of AMI in the cohorts included in this analysis. Geographically eligible (resident of Worcester metropolitan area) patients included in our study sample were identified based on the review of computerized hospital discharge printouts and male and female patients were included irrespective of their hospital survival status, age, or presence of other comorbidities. All autopsy-proven cases of AMI were included irrespective of the other criteria. Patients with perioperative-associated AMI were not included. For the different periods under study, the development of clinical complications associated with AMI, including heart failure and atrial fibrillation, was assessed on the basis of information available from clinical charts (8–10).
Data collection
The hospital records of patients with independently validated AMI were abstracted for demographic, medical history, and clinical data by our trained team of nurse and physician data abstractors. This included information about patient’s age, sex, prior comorbidities (e.g., angina, diabetes, heart failure, hypertension, stroke), occurrence of clinical complications during hospitalization, and AMI order (initial vs prior) and type (Q wave or non-Q wave). Information about the use of cardiac medications, including lipid lowering therapy, during the acute hospitalization was ascertained through the review of hospital medical records and physician’s and nurse’s progress notes by our trained nurse and physician abstractors (11,12). Lipid lowering therapy was defined as the prescribing of statins or other lipid lowering agents (e.g., cholestyramine, ezetimibe, niacin) during the index hospitalization based on the review of data contained in hospital charts. For purposes of this study, we defined “medication maintainers” as patients that were on lipid lowering medication prior to their hospitalization for AMI and who continued to be prescribed this medication during hospitalization. On the other hand, we characterized as “new medication initiators” patients in whom lipid lowering medication was initiated during hospitalization for AMI who were not previously on this therapy based on the review of information contained in hospital medical records.
Data analysis
Differences in the distribution of demographic, medical history, and clinical characteristics between patients prescribed and not prescribed lipid lowering therapy were examined by using chi-square tests of statistical significance for discrete variables and t tests for continuous variables. Changes over time in the proportion of patients treated with lipid lowering therapy were examined through the use of chi square tests for trends. Since multiple comparisons of the data were carried out, we considered a p value of <.01 to be statistically significant. A logistic multiple regression approach was used to examine demographic (e.g., age, sex), medical history (e.g., prior angina, hypertension, heart failure, stroke, or diabetes), and clinical factors (e.g., AMI order, type, hospital clinical complications, hospital procedures) associated with the failure to be prescribed lowering therapy during hospitalization for AMI. These variables were included either because they have been shown to be associated with the development of, or prognosis after, AMI in prior studies or because they differed between our two principal comparison groups of those who were and were not prescribed lipid lowering therapy during their acute hospitalization. Multivariable adjusted odds ratios and accompanying 95% confidence intervals were calculated in a standard manner.
RESULTS
The study sample consisted of 9,429 greater Worcester residents hospitalized with independently validated AMI during the period under study (1986 – 2003). The average age of the study sample was 70 years, 58% were men, the average total serum cholesterol level was 203 mg/dL, and the average LDL cholesterol level was 114 mg/dL. The initial (measured during the first 24 hours of hospitalization) average total serum cholesterol level in the study population declined over time from 228 mg/dL in 1986 to 179 mg/dL in 2003; initial LDL levels also declined over time from 123 mg/dL in 1995, when information about this lipoprotein fraction was first abstracted from laboratory reports, to 110 mg/dL in 2003.
Virtually no patients (<1%) who were hospitalized with AMI in 1986 were on lipid lowering medication prior to their AMI nor was it prescribed for them during their hospitalization; on the other hand, 76% of patients hospitalized with AMI in 2003 were classified as medication maintainers. In 1986, less than 1% of study patients were considered as new medication initiators and this proportion increased to 38% in 2003.
Trends in lipid lowering medication use
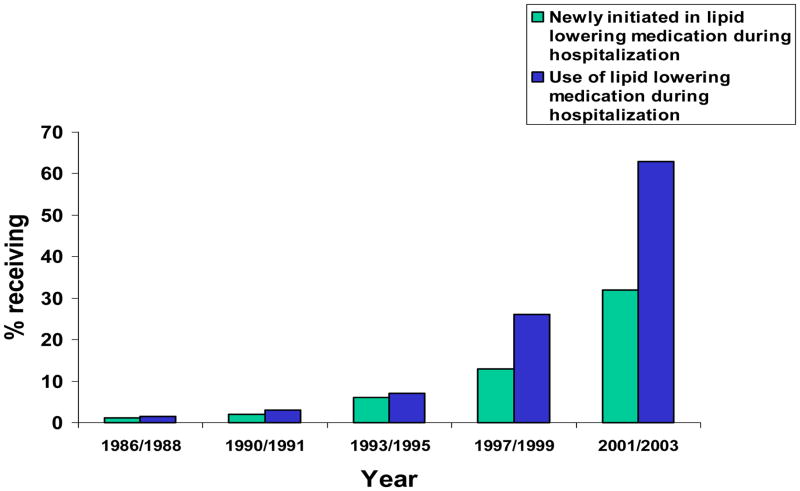
Marked increases in the use of lipid lowering medication during hospitalization for AMI were observed over time (Figure 1). The use of lipid lowering medication remained relatively stable, and infrequently prescribed during the acute hospitalization, over the initial decade of this study. Use of lipid lowering medication increased markedly, however, between 1995 (10%) and 1997 (22%), after which time there was a consistent increase in the proportion of patients treated with lipid lowering therapy. In 2003, approximately 3 out of every 4 patients with AMI were treated with lipid lowering therapy.
Figure 1.
Use of lipid lowering medication in patients hospitalized with acute myocardial infarction
The initiation of lipid lowering therapy during hospitalization for AMI in patients who were not previously on this medication paralleled previously observed trends. In 1986, less than 1% of patients who had not been previously treated with lipid lowering medication were newly prescribed this therapy; approximately 2 out of every 5 patients in 2003 who were not previously on lipid lowering therapy were started on this treatment regimen during their acute hospitalization (Figure 1).
Characteristics of patients not receiving lipid lowering therapy
Overall, in our crude, unadjusted findings, older patients and women were significantly less likely to be treated with lipid lowering therapy in comparison with younger patients and men (Table 1). Patients with fewer previously diagnosed comorbid conditions were significantly less likely to be treated with lipid lowering medication in comparison with patients that had 3 or more prior comorbidities. Patients that presented with an initial or Q-wave AMI were less likely to be treated with lipid lowering therapy than patients with a previous or non-Q wave AMI. Patients with higher total serum cholesterol levels were less likely to be prescribed lipid lowering therapy during hospitalization whereas patients with higher LDL levels were more likely to be prescribed this class of agents. Patients who developed important clinical complications were significantly less likely to be treated with lipid lowering medications than patients who did not develop these complications. Patients who received fewer effective cardiac medications during hospitalization, and those who did not undergo cardiac catheterization, coronary artery bypass graft surgery, and/or a percutaneous coronary intervention, were significantly less likely to be prescribed lipid lowering treatment than patients who were less aggressively managed.
Table 1.
Differences in the Receipt of Lipid Lowering Therapy in Patients With Acute Myocardial Infarction (AMI) According to Selected Characteristics
| Total Study Sample
|
Patients Hospitalized in 2001/2003
|
|||
|---|---|---|---|---|
| Proportion Prescribed Lipid Lowering Therapy | Proportion Prescribed Lipid Lowering Therapy | |||
| % | P value° | % | P value° | |
| Age (yrs) | ||||
| <55 | 36.0 | 83.2 | ||
| 55–64 | 32.0 | 79.2 | ||
| 65–74 | 26.3 | <0.001 | 72.4 | <0.001 |
| ≥75 | 21.4 | 52.4 | ||
| Sex | ||||
| Men | 28.6 | <.001 | 70.8 | <0.001 |
| Women | 24.4 | 59.8 | ||
| Comorbid conditions* | ||||
| None | 23.4 | 71.6 | ||
| One | 24.3 | 69.3 | ||
| Two | 25.8 | <0.001 | 62.4 | <0.05 |
| Three or more | 32.8 | 64.0 | ||
| AMI characteristics | ||||
| Initial | 25.4 | <0.001 | 64.5 | <0.05 |
| Prior | 29.4 | 68.6 | ||
| Q-wave | 20.8 | <0.001 | 73.6 | <0.001 |
| Non-Q-wave | 30.1 | 64.0 | ||
| Total serum cholesterol level (mg/dL) | ||||
| <200 | 32.7 | 75.4 | ||
| 200–239 | 24.6 | <0.001 | 83.3 | <0.001 |
| ≥240 | 23.9 | 93.2 | ||
| LDL cholesterol level (mg/dl) | ||||
| <100 | 56.8 | 69.1 | ||
| 100–129 | 67.5 | <0.001 | 82.7 | <0.001 |
| ≥130 | 75.6 | 86.8 | ||
| Clinical complications | ||||
| Heart failure | <0.001 | <0.001 | ||
| + | 22.1 | 59.4 | ||
| − | 29.7 | 70.2 | ||
| Cardiogenic shock | <0.001 | <0.001 | ||
| + | 15.8 | 49.6 | ||
| − | 27.6 | 66.8 | ||
| Atrial fibrillation | <0.005 | <0.001 | ||
| + | 23.9 | 55.7 | ||
| − | 27.4 | 68.8 | ||
| Effective Cardiac Therapy | ||||
| Any 1** | 8.2 | 33.5 | ||
| Any 2 | 24.8 | <0.001 | 60.4 | <0.001 |
| Any 3 | 43.7 | 75.7 | ||
| Any 4 | 40.1 | 88.1 | ||
| Hospital procedures | ||||
| Cardiac catheterization | <0.001 | <0.001 | ||
| + | 44.2 | 81.2 | ||
| − | 16.6 | 48.8 | ||
| Coronary artery bypass graft | <0.001 | <0.05 | ||
| + | 45.1 | 76.1 | ||
| − | 25.9 | 65.2 | ||
| Percutaneous coronary intervention | <0.001 | <0.001 | ||
| + | 59.9 | 85.3 | ||
| − | 20.0 | 55.3 | ||
Presence of either angina, heart failure, diabetes mellitus, hypertension, stroke, or peripheral vascular disease.
Prescribing of any cardiac medication = aspirin, ACE inhibitors, beta blocker, or thrombolytics
Differences in the proportion of patients in each subgroup who were prescribed lipid lowering therapy.
Relatively similar demographic and clinical factors were associated with the failure to have lipid lowering therapy initiated in individuals who had not been previously on lipid lowering medication. When we restricted our study sample to patients hospitalized with AMI during our 2 most recent study years of 2001 and 2003 in order to provide a contemporary perspective into the profile of patients who were not treated with lipid lowering therapy, relatively similar factors were associated with the failure to be prescribed lipid lowering medication (Table 1). In contrast to the overall results, patients with more comorbidities, a non-Q-wave AMI, and lower cholesterol levels were less likely to receive lipid lowering medication than their respective counterparts.
Across all study years, and after adjustment for a variety of demographic, medical history, and clinical factors potentially associated with the failure to be prescribed lipid lowering therapy (including study year and survival status during the first 48 hours of hospitalization), increasing age (≥65 years), presence of fewer prior comorbidities, and presentation with an initial AMI were associated with a significantly decreased likelihood of being prescribed lipid lowering therapy (Table 2). An increased likelihood of not being prescribed lipid lowering medication was observed in patients who developed heart failure, atrial fibrillation, or cardiogenic shock during hospitalization. Patients that were not treated with effective cardiac medications, as well as those who did not undergo a coronary revascularization procedure, were less likely to be maintained on lipid lowering medication than respective comparison groups. Virtually identical factors were associated with the failure to be prescribed lipid lowering agents in patients who were not on these therapies previously as well as in patients hospitalized with AMI during our 2 most recent study years (Table 2).
Table 2.
Factors Associated with Failure to be Prescribed Lipid Lowering Medication in Patients with Acute Myocardial Infarction (AMI)
| Clinical Characteristics* | Total Study Sample | Patients Hospitalized in 2001/2003 | ||
|---|---|---|---|---|
| Adjusted Odds Ratio | 95% CI | Adjusted Odds Ratio | 95% CI | |
| Age (yrs) | ||||
| 55–64 | 1.16 | 0.95,1.41 | 1.14 | 0.76,1.72 |
| 65–74 | 1.38 | 1.14,1.68 | 1.30 | 0.88,1.92 |
| 75–84 | 2.50 | 2.04,3.06 | 2.00 | 1.37,2.91 |
| ≥85 | 3.76 | 2.93,4.83 | 2.88 | 1.91,4.35 |
| Women | 1.02 | 0.90,1.15 | 1.13 | 0.93,1.39 |
| Medical history | ||||
| Comorbid conditions | ||||
| 0–1 | 1.31 | 1.10,1.55 | 0.97 | 0.74,1.27 |
| 2 | 1.18 | 1.00,1.39 | 1.15 | 0.89,1.49 |
| AMI Characteristics | ||||
| Initial | 1.51 | 1.30,1.74 | 1.76 | 1.40,2.23 |
| Non-Q wave | 1.02 | 0.89,1.18 | -- | -- -- |
| Clinical complication | ||||
| Heart Failure (+) | 1.35 | 1.18,1.54 | 1.11 | 0.90,1.38 |
| Cardiogenic shock (+) | 1.78 | 1.33,2.38 | 2.45 | 1.57,3.81 |
| Clinical Characteristics | Adjusted Odds Ratio | 95% CI | Adjusted Odds Ratio | 95% CI |
| Atrial fibrillation (+) | 1.22 | 1.03,1.44 | 1.41 | 1.12,1.78 |
| No effective cardiac medications** | 4.98 | 2.87,8.65 | 10.33 | 4.23,25.18 |
| No revascularization procedures° | 2.11 | 1.86,2.41 | 3.19 | 2.56,3.97 |
Respective referent groups = age <55 years, men, presence of 3 or more comorbid conditions, history of AMI, Q wave AMI, absence of selected clinical complications, hospital receipt of effective cardiac medications or coronary revascularization procedures.
Aspirin, beta blockers, ACE inhibitors, or thrombolytics
Revascularization procedures = cardiac catheterization, coronary artery bypass graft surgery, and percutaneous coronary intervention.
Measurement of Serum Cholesterol Levels During Hospitalization for AMI
During our initial study years of 1986 and 1988, 63% of patients had their total serum cholesterol measured on admission to greater Worcester hospitals for AMI; total cholesterol levels were measured in 53% of patients hospitalized with AMI in 1993/1995 and in 49% of patients hospitalized with AMI during 2001 and 2003.
Characteristics of Patients with Serum Lipid Measurements
Older patients, women, patients with 3 or more comorbid conditions, and those having a prior, non-Q wave AMI were less likely to have their serum lipid levels determined than respective comparison groups (Table 3). Patients who developed heart failure or cardiogenic shock during the acute hospitalization, and those who were less frequently prescribed cardiac medications were less likely to have had an initial lipid profile measured during the first 24 hours of hospitalization. We also examined the contemporary profile of patients not having a serum lipid profile measured, restricting our analysis to patients hospitalized in our 2 most recent study years of 2001 and 2003 (Table 3). Consistent with the findings in our total study sample, relatively similar demographic and clinical factors were associated with the failure to have their serum lipids characterized.
Table 3.
Differences in the Characteristics of Patients with a Total Serum Cholesterol Profile Assessed
| Total Study Sample
|
Patients Hospitalized in 2001/2003
|
|||
|---|---|---|---|---|
| Proportion With a Lipid Profile Measured % | P value° | Proportion With a Lipid Profile Measured % | P value | |
| Age (yrs) | ||||
| <55 | 69.0 | 72.9 | ||
| 55–64 | 61.7 | 61.0 | ||
| 65–74 | 55.5 | <0.001 | 51.0 | <0.001 |
| ≥75 | 46.7 | 38.5 | ||
| Sex | ||||
| Men | 58.6 | <.001 | 56.2 | <0.001 |
| Women | 50.4 | 41.5 | ||
| Medical history | ||||
| Comorbid conditions* | ||||
| None | 66.4 | 71.6 | ||
| 1 | 59.5 | 57.9 | ||
| 2 | 53.6 | <0.001 | 47.8 | <0.001 |
| ≥3 | 44.0 | 36.4 | ||
| AMI characteristics | ||||
| Initial | 58.3 | <0.001 | 55.6 | <0.001 |
| Prior | 49.1 | 38.9 | ||
| Q-wave | 61.2 | <0.001 | 62.3 | <0.001 |
| Non-Q-wave | 51.7 | 46.5 | ||
| Clinical complications | ||||
| Heart failure | <0.001 | <0.001 | ||
| + | 51.1 | 40.3 | ||
| − | 57.6 | 55.9 | ||
| Cardiogenic shock | <0.001 | <0.05 | ||
| + | 48.3 | 39.0 | ||
| − | 55.6 | 50.3 | ||
| Atrial fibrillation | 0.07 | <0.001 | ||
| + | 53.1 | 41.4 | ||
| − | 55.5 | 52.1 | ||
| Therapy** | ||||
| None | 55.7 | 15.8 | ||
| Any 1 | 53.4 | 21.8 | ||
| Any 2 | 54.6 | <0.001 | 46.7 | <0.001 |
| Any 3 | 55.9 | 56.0 | ||
| All 4 | 58.4 | 72.5 | ||
| Procedures | ||||
| Cardiac catheterization | <0.001 | <0.001 | ||
| + | 59.4 | 61.6 | ||
| − | 52.6 | 36.4 | ||
| Coronary artery bypass graft | 0.60 | 0.27 | ||
| + | 56.3 | 53.9 | ||
| − | 55.1 | 49.4 | ||
| Percutaneous coronary intervention | <0.001 | <0.001 | ||
| + | 61.2 | 65.0 | ||
| − | 53.9 | 41.4 | ||
Presence of either angina, heart failure, diabetes mellitus, hypertension, stroke, or peripheral vascular disease
Prescribing of any cardiac medication = aspirin, ACE inhibitors, beta blockers, or thrombolytics
Differences in the proportion of patients in each subgroup who had their serum lipids measured.
After adjustment for a variety of demographic and clinical factors, we found a decreased likelihood of having a lipid profile measured in young patients, women, those with 3 or more comorbid conditions, and in those who had a prior, or Q wave AMI. A decreased likelihood of not having a lipid profile measured was observed in patients that developed clinical complications during hospitalization for AMI, who were treated with fewer effective cardiac medications, and in those who did not undergo coronary revascularization during hospitalization for AMI (data not shown).
DISCUSSION
The results of this large community-wide observational study suggest marked increases over time in the use of lipid lowering medication in patients hospitalized with AMI, particularly during the most recent decade under study. In addition, we identified a variety of demographic and clinical characteristics associated with the failure to be prescribed lipid lowering therapy in this high risk patient population.
Trends in the Use of Lipid Lowering Medication
Data from the large multi-hospital National Registry of Myocardial Infarction (NRMI 3) suggest that the use of lipid-lowering therapy increased between 1998 (29%) and 1999 (36%) in patients hospitalized with AMI (13). Other investigators have examined changing trends in the use of evidence-based therapies for AMI (e.g., beta blockers, aspirin, ACE inhibitors) from the late 1970’s until late 1990’s at the community level and/or in disease registries (14,15). However, the use of lipid lowering medication has either not been specifically examined in these studies or reported on (14) or the study of its use has been limited to overall utilization during a given time period (e.g., Medicare beneficiaries discharged with AMI between 1998 and 2001) (15). Some community-based coronary disease registries or surveillance programs (e.g., ARIC, Minnesota Heart Survey) have examined changes in serum cholesterol levels over time, but have not reported changing trends in the use of lipid lowering therapy in patients hospitalized with AMI (16,17). The Minnesota Heart Survey has provided information on 20 year (1980–1982 to 2000–2002) trends in population-wide serum cholesterol levels showing declining average total cholesterol concentrations in middle-aged and older (45 to 74 years) men and women residing in the Twin Cities metropolitan area. During this 20-year study period, increases in the use of lipid lowering medication were observed in all Twin Cities residents (17).
In the present study, we observed increases in both the maintenance of prior lipid lowering therapy as well as in the initiation of new lipid lowering treatment regimens in patients hospitalized with AMI. We also observed declining total serum cholesterol levels in patients who presented to greater Worcester hospitals over time, findings which may be attributed to the greater use of lipid lowering medication in patients at increased risk for coronary disease. Our data are consistent with the population level changes found in the Minnesota Heart Survey in which declining total serum cholesterol levels were associated with increasing use of lipid lowering medication (17). Nationally, recent findings from the NHANES survey indicate significant declines in total serum cholesterol and LDL levels in surveys carried out between 1990 to 1994 and 1999 and 2002, findings which were attributed to an expanded use of lipid lowering medication in the U.S. population (18).
Measurement of Serum Cholesterol Levels
Using data from the Framingham Heart Study, investigators from the Worcester Heart Attack Study had previously observed no significant differences in the total cholesterol values measured between the 2 years prior to the development of an AMI, within 24 hours of hospitalization for AMI, and within 2 years after hospital discharge (19). These data suggested that total serum cholesterol levels obtained during the first 24 hours of hospitalization for AMI accurately reflect usual levels and should remove a perceived barrier to the hospital initiation of lipid lowering therapy. Many physicians may have been previously reluctant to characterize patient’s lipid profile at this time under the impression that misleading results may have been obtained (20).
Surprisingly, our findings suggest that a greater proportion of patients had their total serum cholesterol levels measured during hospitalization for AMI in the mid to late 1980’s than in 2003. It is possible that greater Worcester physicians may be postponing the measurement of serum cholesterol to the outpatient setting and the patient’s first outpatient visit with their cardiologist after being discharged from the hospital after AMI. At this time, patient’s medication regimens are typically reassessed and new therapies possibly introduced or dosage regimens to existing therapies modified.
Factors Associated with the Failure to be Prescribed Lipid Lowering Medication
Many American adults have undiagnosed dyslipidemia. Among patients with diagnosed hyperlipidemia, many are often treated suboptimally or are prescribed medication inconsistent with their risk of CHD (13,21). Despite the widespread dissemination of national treatment guidelines for the treatment of hyperlipidemia, and publicized results of major clinical trials demonstrating the value of lipid lowering medication in the primary and secondary prevention of CHD, we identified several patient demographic and clinical characteristics associated with the failure to receive lipid lowering medication during hospitalization for AMI. The elderly and patients with an initial AMI were least likely to receive these agents than respective comparison groups.
Numerous studies have shown that elderly patients are less aggressively treated with effective cardiac therapies than younger patients (22). The results of our study clearly demonstrate that advancing age was inversely associated with the receipt of lipid lowering medications during hospitalization for AMI.
Findings from the Framingham Heart Study suggest that the lifetime risk of CHD increases sharply with higher total cholesterol levels for men and women at all ages (23). There appears to be ample evidence supporting the use of lipid lowering medication for secondary prevention in elderly patients with established CHD (24). In the CARE trial, the benefits of cholesterol lowering in patients 60 years and older were similar to that noted in younger patients (25). Similarly, the percentage reduction in the risk of subsequent cardiac events after treatment in the HEART Protection Study was essentially the same in middle-aged and elderly patients (26).
We found that lipid lowering medications were used less often in patients with, as compared to those without, a history of diabetes. This is of concern since the results of several trials have shown benefits associated with the use of lipid lowering medications in these high risk patients with acute coronary disease (26,27). Several previous studies have demonstrated that patients with various comorbidities, including angina, heart failure or stroke, are less likely to receive lipid lowering medications, singly or in combination with other cardiac therapies, after MI (11,28). Similar associations were observed in the present investigation. These findings are of concern since patients with these serious comorbidities remain at increased risk for recurrent coronary events in whom lipid lowering therapy might be beneficial.
In our study, increasing total and LDL serum cholesterol levels were associated with an increased likelihood of receiving lipid lowering medication; this was particularly noted in patients with the highest total and LDL cholesterol levels during our 2 most recent study years. These findings are consistent with the results of 2 prior community-based investigations in the U.S. and Canada that were carried out between the mid-1980’s and mid-1990’s and 1999–2001, respectively (29,30). The data from these studies suggest an evolving, more aggressive, approach towards the management of hyperlipidemia during hospitalization for AMI among community-based physicians.
Study Strengths and Limitations
The strengths of our study include the large and well characterized sample of patients with confirmed AMI and the inclusion of residents from a representative New England metropolitan area who were treated by a variety of physicians. The use of multivariable analytic techniques to examine the association between several demographic and clinical characteristics with the receipt of lipid lowering medication strengthens the interpretation of any associations observed. The inclusion of male and female patients of all ages hospitalized with AMI at all area hospitals minimizes the potential for selection bias which may occur in studying more select patient populations.
Our study has several limitations, however. The data concerning in-hospital evaluation and management were collected by retrospective chart review and the findings are dependent on the accuracy of the information contained in medical records. We were not able to collect additional information about the characteristics of the physicians involved in the management of patients with AMI. We have, however, previously examined the attitudes and practices toward the management of hyperlipidemia in patients hospitalized with MI among greater Worcester physicians and have also examined trends in the medical treatment of patients with AMI by these practitioners (11,31). Findings from these studies have suggested that the practice patterns of greater Worcester physicians reflect those of physicians in the nation as a whole, enhancing the potential generalizability of the present findings. Finally, the prescribing of lipid lowering medication does not necessarily imply that the patient was treated with the most appropriate agent or dosage or that the patient had achieved desirable serum LDL or total cholesterol levels.
Conclusions
The results of our study suggest that the use of lipid lowering medication in a community sample of patients hospitalized with AMI has increased over time. These trends likely reflect the growing scientific literature that has demonstrated the effectiveness of lipid lowering drugs over the past several decades. However, in specific at-risk populations, such as women, the elderly, and patients with previous comorbidities, lipid lowering medication remains underutilized. Reasons for the underuse of this effective treatment strategy in specific high risk groups need to be explored. Use of educational interventions, as well as computerized reminder systems, need to be developed and increasingly applied to enhance the use of lipid lowering medication in those at greatest need for this effective treatment modality.
Acknowledgments
Grant support for this project was provided by the National Heart, Lung, and Blood Institute (RO1 HL35434, KO1-HL-04047).
Footnotes
Author Contributions:
Author Name: Jorge Yarzebski and Robert J. Goldberg: study concept and design, acquisition of data, analysis and interpretation of data, and preparation of manuscript.
Author Name: Edgard Granillo, Frederick A. Spencer, Darleen Lessard, Jerry H. Gurwitz, and Joel M. Gore: study concept and design, interpretation of data and preparation of manuscript.
Sponsor’s Role: None
Financial Disclosure(s): This study was made possible through the cooperation of the administration, medical records and cardiology departments of participating Worcester metropolitan area hospitals. Grant support for this project was provided by the National Heart, Lung, and Blood Institute (RO1 HL35434, KO1-HL-04047).
Author Name: Jorge Yarzebski, M.D., M.P.H. (none)
Author Name: Edgard Granillo, M.D. (none)
Author Name: Frederick A. Spencer, M.D. (none)
Author Name: Darleen Lessard, M.S. (none)
Author Name: Jerry H. Gurwitz, M.D. (none)
Author Name: Joel M. Gore, M.D. (none)
Author Name: Robert J. Goldberg, Ph.D. (none)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study. (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 2.The Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 3.LaRosa JC, He J, Vupputuri S. Effect of statin on risk of coronary disease; a meta-analysis of randomized controlled trials. JAMA. 1999;282:2340–2346. doi: 10.1001/jama.282.24.2340. [DOI] [PubMed] [Google Scholar]
- 4.Heart Protection Study Collaboration Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomized placebo-controlled trial. Lancet. 2002;360:7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 5.McBride P, Schrott HG, Plane MB, et al. Primary care practice adherence to National Cholesterol Education Program guidelines for patients with coronary heart disease. Arch Intern Med. 1998;158:1238–1244. doi: 10.1001/archinte.158.11.1238. [DOI] [PubMed] [Google Scholar]
- 6.Majumdar SR, Gurwitz JH, Soumerai SB. Undertreatment of hyperlipidemia in the secondary prevention of coronary artery disease. J Gen Intern Med. 1999;14:711–717. doi: 10.1046/j.1525-1497.1999.02229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Expert Panel on the Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in the attack rates and survival rates of acute myocardial infarction (1975–1981); The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 9.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Incidence and case fatality rates of acute myocardial infarction (1975–1984): The Worcester Heart Attack Study. Am Heart J. 1988;115:761–767. doi: 10.1016/0002-8703(88)90876-9. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg RJ, Yarzebski J, Lessard D, et al. A two-decades (1975–1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: A community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 11.Spencer FA, Lessard D, Yarzebski J, et al. Decade-long changes in the use of combination evidence-based medical therapy at discharge for patients surviving acute myocardial infarction. Am Heart J. 2005;150:838–44. doi: 10.1016/j.ahj.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 12.Spencer F, Scleparis G, Goldberg RJ, et al. Decade-long trends (1986 to 1997) in the medical treatment of patients with acute myocardial infarction: A community-wide perspective. Am Heart J. 2001;142:594–603. doi: 10.1067/mhj.2001.117776. [DOI] [PubMed] [Google Scholar]
- 13.Rogers WJ, Canto JG, Lambrew CT, et al. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the U.S. from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–63. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 14.Perschbacher JM, Reeder GS, Jacobsen SJ, et al. Evidence-based therapies for myocardial infarction: Secular trends and determinants of practice in the community. Mayo Clin Proc. 2004;79:983–991. doi: 10.4065/79.8.983. [DOI] [PubMed] [Google Scholar]
- 15.Foody JM, Rathore SS, Galusha D, et al. Hydroxymethylglutaryl-CoA Reductase Inhibitors in Older Persons with Acute Myocardial Infarction: Evidence for an Age-Statin Interaction. Am Geriatr Soc. 2006;54:421–430. doi: 10.1111/j.1532-5415.2005.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Szklo M, Chambless LE, Folsom AR, et al. Trends in Plasma Cholesterol Levels in the Atherosclerosis Risk in Communities (ARIC) Study. Preventive Medicine. 2000;30:252–259. doi: 10.1006/pmed.1999.0612. [DOI] [PubMed] [Google Scholar]
- 17.Arnett DK, Jacobs DR, Luepker RV, et al. Twenty-year trends in serum cholesterol, hypercholesterolemia, and cholesterol medication use. The Minnesota Heart Survey, 1980–1982 to 2000–2002. Circulation. 2005;112:3884–3891. doi: 10.1161/CIRCULATIONAHA.105.549857. [DOI] [PubMed] [Google Scholar]
- 18.Carroll MD, Lacher DA, Sorlie PD, et al. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA. 2005;294:1773–81. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 19.Gore JM, Goldberg RJ, Matsumoto AS, et al. Validity of serum total cholesterol level obtained within 24 hours of acute myocardial infarction. Am J Cardiol. 1984;54:722–725. doi: 10.1016/s0002-9149(84)80197-6. [DOI] [PubMed] [Google Scholar]
- 20.Fonarow GC. In-hospital initiation of statin therapy in patients with acute coronary events. Current Atherosclerosis Reports. 2003;5:394–402. doi: 10.1007/s11883-003-0011-4. [DOI] [PubMed] [Google Scholar]
- 21.Pearson TA, Laurora I, Chu H, et al. The Lipid Treatment Assessment Project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000;160:459–467. doi: 10.1001/archinte.160.4.459. [DOI] [PubMed] [Google Scholar]
- 22.Krumholz HM, Radford MJ, Wang Y, et al. National use and effectiveness of beta-blockers for the treatment of elderly patients after acute myocardial infarction: National Cooperative Cardiovascular Project. JAMA. 1998;280:623–9. doi: 10.1001/jama.280.7.623. [DOI] [PubMed] [Google Scholar]
- 23.Lloyd-Jones DM, Wilson PWF, Larson MG, et al. Lifetime risk of coronary heart disease by cholesterol levels at selected ages. Arch Intern Med. 2003;163:1966–1972. doi: 10.1001/archinte.163.16.1966. [DOI] [PubMed] [Google Scholar]
- 24.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143. [PubMed] [Google Scholar]
- 25.Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial Investigators. N Engl J Med. 1996;335:1001. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 26.MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomized placebo-controlled trial. Lancet. 2002;360:7. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 27.Sacks FM, Tonkin AM, Craven T, et al. Coronary heart disease in patients with low LDL-cholesterol: benefit of pravastatin in diabetic and enhanced role for HDL-cholesterol and triglycerides as risk factors. Circulation. 2002;105:1424. doi: 10.1161/01.cir.0000012918.84068.43. [DOI] [PubMed] [Google Scholar]
- 28.Fonarow C, French WJ, Parsons LS, et al. Use of lipid-lowering medications at discharge in patients with acute myocardial infarction. Data from the National Registry of Myocardial Infarction 3. Circulation. 2001;103:38–44. doi: 10.1161/01.cir.103.1.38. [DOI] [PubMed] [Google Scholar]
- 29.Goldberg RJ, Ockene IS, Yarzebski J, Savageau J, Gore JM. Use of lipid-lowering medication in patients with acute myocardial infarction (Worcester Heart Attack Study) Am J Cardiol. 1997;79:1095–1097. doi: 10.1016/s0002-9149(97)00051-9. [DOI] [PubMed] [Google Scholar]
- 30.Ko DT, Alter DA, Newman AM, Donovan LR, Tu JV. Association between lipid testing and statin therapy in acute myocardial infarction patients. Am Heart J. 2005;150:419–25. doi: 10.1016/j.ahj.2004.09.057. [DOI] [PubMed] [Google Scholar]
- 31.Yarzebski J, Bujor CF, Goldberg RJ, et al. A community-wide survey of physician practices and attitudes toward cholesterol management in patients with recent acute myocardial infarction. Arch Intern Med. 2002;162:797–804. doi: 10.1001/archinte.162.7.797. [DOI] [PubMed] [Google Scholar]