Abstract
The American Geriatrics Society has recommended a reexamination of the roles and deployment of providers with expertise in geriatric medicine. Healthcare systems use a variety of strategies to maximize their geriatric expertise. In general, these health systems tend to focus geriatric medicine resources on a group of older adults that are locally defined as the most in need. This article describes a model of care within an academic urban public health system and describes how local characteristics interact to define the domain of geriatric medicine. This domain is defined using 4 years of data from an electronic medical record combined with data collected from clinical trials.
From January 2002 to December 2005, 31,443 adults aged 65 and older were seen at any clinical site within this healthcare system. The mean age was 75 (range 65–105); 61% were women; 35% African American, and 2% Hispanic. The payer mix was 80% Medicare and 17% Medicaid. The local geriatric medicine program includes sites of care in inpatient, ambulatory, nursing home, and home-based settings.
By design, this geriatric medicine clinical practice complements the care provided to older adults by the primary care practice. Primary care physicians tend to cede care to geriatric medicine for older adults with advanced disability or geriatric syndromes. This is most apparent for older adults in nursing facilities or those requiring home-based care. There is a dynamic interplay between design features, reputation, and capacity that modulates volume, location, and type of patients seen by geriatrics.
Keywords: geriatric medicine, healthcare system, physician manpower
One of the explicit goals of geriatric medicine is “to ensure that every older person receives high-quality, patient-centered health care.”1 For at least 30 years, leaders in geriatric medicine have recognized that primary care physicians and not specialists in geriatric medicine would provide most of this care.2–5 Despite important improvements in the national production of specialists in geriatric medicine, including the growth of academic geriatric medicine faculty,6–8 the American Geriatrics Society concluded that “the shortages of geriatricians demand a reexamination of the roles of geriatricians and better leveraging of the scarce resources of a small geriatrician workforce.”1 The appropriate stewardship of this scare resource remains unclear, and thus the clinical domain of geriatric medicine remains controversial. A 2008 Institute of Medicine report recommended support for research that promotes the development of new models of care and promotes “the effective use of the workforce to care for older adults.”9
Although common elements of successful models of geriatric care can now be identified,9 there has been no widespread implementation of these models. Variable workforce resources and payment schemes result in variable availability and deployment of the geriatric workforce across different healthcare systems. This seemingly spurious variation in the deployment of the geriatric workforce has naturally raised questions about the appropriate domain of geriatric medicine. Clinical program leaders generally deploy geriatric medicine expertise by emphasizing one of three overlapping approaches. In the first approach, geriatric physicians and their interdisciplinary teams focus their expertise on older adults most in need. This approach is consistent with other specialty models that recognize a subset of patients or procedures as the purview of a medical specialty. Within the realm of geriatric medicine, “most in need” has been variably defined according to disability (e.g., limitations in activities of daily living), a specific geriatric syndrome (e.g., dementia), or a site of care (e.g., skilled nursing facilities), among other strategies. Although these “most in need” definitions also have considerable overlap, they result in important differences in how a health system uses its geriatric manpower. A second approach is to deploy geriatric medicine expertise in a consultancy and co-management model where geriatric medicine specialists assist generalist physicians in the care of a broader range of older adults. This approach emphasizes consultancy at the level of individual patients and deemphasizes the geriatrician's role as a primary care provider. This second approach requires the geriatric medicine physician to improve the care of older adults through the care provided by generalist physicians. The third approach is to move geriatricians decisively toward healthcare administration and health system design. Through system redesign, rather than direct care, geriatricians arguably have the capacity to reach the greatest number of older adults, but in this approach, geriatric medicine physicians tend to touch older adults through other providers, and they may become increasingly invisible to their patients and colleagues. Many programs employ all three but tend to emphasize one strategy over the others, and there are other possible models. The financial viability of these models differs across different third-party payment schemes and other forms of incentives or disincentives.
This article describes a model of care within an urban public health system that uses all three strategies but with an emphasis on co-management with primary care. The purpose of this report is to provide a picture of a single healthcare system's deployment of geriatric expertise as an example of a successful model that employs several state-of-the-art approaches. This particular healthcare system is well suited to a case study for three reasons. First, the healthcare system provides care to a diverse population of older adults in an urban setting. Thus, the healthcare system serves a vulnerable population characterized by a heavy burden of illness and disability. Second, this healthcare system has been the site of several randomized trials of new models of geriatric care focusing on primary care.10–12 Thus, access was available to important measures of patient outcomes not typically available from routine practice. Third, one of the nation's oldest and most comprehensive electronic medical records serves this healthcare system.13 Thus, even outside the context of clinical trials, access was available to data describing the process of care.
This article describes the 10-year history of clinical program development of geriatric medicine, with particular emphasis on data documenting how primary care physicians use geriatric medicine expertise. First, the local geriatric medicine practice is described. Next, the volume and types of older adults seen by primary care and geriatrician providers at various practice sites are described. Finally, challenges and future plans are described. Through this process, the domain of geriatric medicine at a local level and in the face of a limited geriatric medicine workforce is defined.
CURRENT GERIATRIC MEDICINE PROGRAM DESCRIPTION
In addition to third-party payment schemes, local strengths and other realities influence the appropriate design of geriatric medicine clinical programs. This local ecology influences the potential success of design strategies regardless of whether these same strategies have been successful elsewhere. Established in 1997, the Indiana University (IU) geriatrics program is administratively located within the Division of General Internal Medicine and Geriatrics in the Department of Medicine at the School of Medicine. The geriatrics faculty coordinates geriatric educational programs at the medical student, resident, fellowship, and practicing physician levels. These faculty also lead research programs within the Center for Aging Research. There are currently 14 physicians with a Certificate of Added Qualifications (CAQ) in the IU geriatrics program. Ten nurse practitioners, six nurses, and seven social workers are also important members of the team. Because these providers participate in activities other than direct clinical care, the actual full-time equivalent (FTE) for clinical care translates to 3.3 FTE for physicians, 6.0 FTE for nurse practitioners, 4.2 FTE for nurses, and 5.2 FTE for social workers. Examples of other activities other than direct clinical care include education, research, administration, and clinical work outside the geriatric program.
Geriatric clinical care sites that together represent “Senior Care at Wishard” include the outpatient IU Center for Senior Health, an inpatient Acute Care for Elders (ACE) Unit and consultation service, a network of approximately 20 skilled nursing facilities, and a home visit program called House Calls for Seniors. There were multiple rationales for establishing these practices, including attention to best practices across the continuum of care, a clinical needs assessment in consultation with the primary care and health system leadership, educational requirements for trainees, and as important sites of research. The IU Center for Senior Health provides primary care to frail older adults and geriatric medicine consultative services for patients referred from the primary care practice, subspecialty clinics, and community-based physicians. The ACE Unit in Wishard Memorial Hospital was established in 1998 to provide hospitalized elderly patients with a specially designed environment and expert geriatrics interdisciplinary team, led by a geriatrician medical director, to complement their inpatient care as provided by hospital attending physicians.14 The ACE consultation service provides proactive services supporting the medical care of acutely ill older patients throughout the hospital. Clinical sites also include a network of approximately 20 community-based nursing homes where IU geriatricians and nurse practitioners provide continuity of care for patients discharged from Wishard. In 1999, program leadership established House Calls for Seniors to better meet the needs of severely dependent and homebound seniors who otherwise are unable to access primary care.
In addition to providing service as teachers, researchers, and clinicians, IU geriatrics faculty also serve in key leadership roles within the Wishard administration and on visible local committees such as the pharmacy and therapeutic committee, the tenure and promotion committee, the institutional review board, and the Curriculum Council, among others. Participation on these committees is critical for influencing policy and for an early warning system for policies likely to affect the geriatrics program. Before turning to data on the clinical operations of this academic geriatric program, it should be emphasized that the design of the program is based on the local ecology and local needs. Because it is an expectation that the environment will change, the program design has also changed over time.
VOLUME OF CARE PROVIDED TO OLDER ADULTS
According to 2000 U.S. census data, there are approximately 94,000 adults aged 65 and older (12.5% of population) in the Indianapolis metropolitan area; 34,500 of these are aged 75 and older (4.4% of population). The volume-of-care data below come primarily from clinical data routinely collected and stored in the Regenstrief Medical Record System. This electronic medical record has been in operation at Wishard Health Services since 1972. The system captures all diagnoses, diagnostic studies, and orders, including requests for consultation, in a coded form. It also captures clinical encounter information and the full text of all dictated reports, as well as discharge diagnoses, dates, and lengths of stay. To provide a longitudinal view of clinical services for older adults, the focus is on the most recent 4 years of complete data. At this time, the comprehensive geriatric clinical services described above were in full operation.
From January 2002 to December 2005, 31,443 adults aged 65 and older were seen at any clinical site by any provider affiliated with Wishard Health Services. Although this figure represents approximately one in three older adults accounted for in the 2000 U.S. Census data noted above, not all of these patients are accounted for in the 2000 census, and some patients may have had only a single contact with the healthcare system (e.g., an emergency department visit.) The mean age of these older adults was 75 (range 65–105); 61% were women, 35% were African American, and 2% were Hispanic. The payer mix was 80% Medicare, 17% Medicaid, and 17% local county assistance. This group of older adults represents the largest potential population of older adults who the geriatric medicine clinical program could have served. Of this group, 11,224 (36%) were seen at least once in an ambulatory primary care clinic, and 1,395 (4.4%) were seen in an ambulatory geriatric medicine clinical site. (Skilled nursing facility visits are not included as Wishard Health Services ambulatory geriatric medicine clinical sites for the purposes of this report.) These 1,395 older adults generated 3,651 visits to the geriatric outpatient consultation clinic, 4,445 visits to the geriatric primary care clinic, and 4,669 home visits (12,765 total ambulatory care visits) between January 2002 and December 2005.
In addition, Wishard Health Services–based geriatric medicine providers logged 6,700 skilled nursing facility visits per year (>25,000 over 4 years) to older adults over this same period. These visits occurred at 20 different skilled nursing facilities in the Indianapolis metropolitan area. Older adults become a part of this nursing home practice when they have been hospitalized at Wishard Health Services and subsequently require nursing home care on discharge. Most of these patients are rehospitalized at Wishard if future hospital care is required. The primary care practice largely cedes this nursing facility care to the geriatric medicine clinical practice. Although maintaining this patient base is important to the hospital and for quality care, clinical care provided by the geriatric medicine team at the area nursing facilities is largely invisible to other providers, including trainees.
Figure 1 shows the number of older adult admissions to Wishard hospital, including the number of hospitalized older adults receiving Medicare and the number seen by the ACE inpatient geriatrics services. By 2005, the ACE team was participating in the care of 43% of the hospitalized older adults in this healthcare system. To provide some perspective on the size of the geriatric medicine consultation service, Figure 2 compares the volume of geriatric medicine consultations with that of those provided by the nephrology and cardiology services. For comparison purposes, this figure limits nephrology and cardiology consultations to those provided to patients aged 65 and older, even though these specialty services also provide consultation to younger adults.
Figure 1.
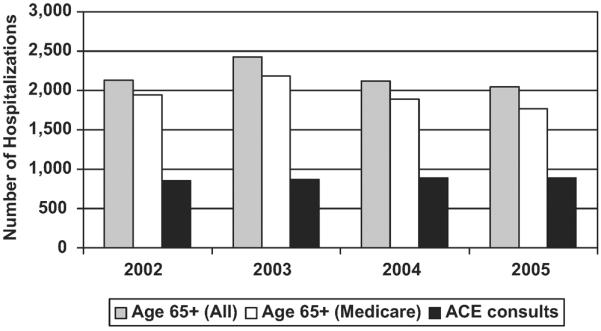
Geriatric admissions to Wishard Hospital: 2002–2005.
Figure 2.
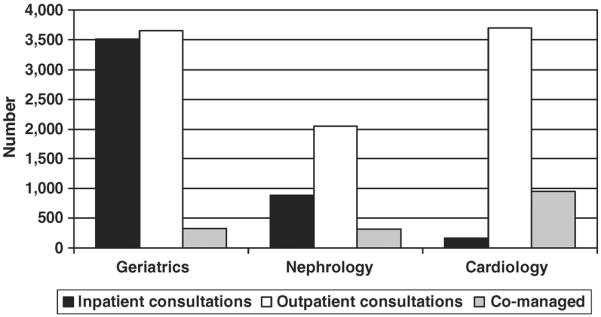
Volume comparisons with other specialty providers for older adults: 2002–2005.
Figure 2 also compares the number of older adults co-managed by these three services with primary care physicians. Because the data were limited to those retrievable from the electronic medical record, an operational and liberal definition of co-management was used. Co-managed patients are defined as patients cared for in the primary care and the relevant specialty care ambulatory clinics in the same calendar year. Although geriatricians provide a large number of inpatient consultations, outpatient consultations and co-managed older adults are greater for the cardiology service.
USE OF GERIATRIC MEDICINE EXPERTISE BY PRIMARY CARE PROVIDERS
Requests for physician consultation throughout Wishard Health Services are accomplished through physician's orders using the electronic medical record. This computerized order-entry system also requests the reason for the consultation. To facilitate order entry, the relevant specialty service provides fixed-choice menus representing common reasons for consultations to their service. Providers may also enter free-text reasons for consultation or may opt not to record a reason for the consultation. Table 1 shows the primary reason for 964 outpatient geriatric medicine consultations as recorded by the physician requesting the consultation. Memory and functional impairment accounted for 55% of all requests for consultation from geriatric medicine.
Table 1.
Primary Reason for 964 Outpatient Geriatric Consultations (2002–2005)
| Reason | % |
|---|---|
| Memory loss | 28 |
| Functional impairment | 27 |
| Unspecified | 12 |
| Falls | 8 |
| Multiple comorbidity | 7 |
| Depression | 6 |
| Polypharmacy | 3 |
| Social | 2 |
| Weight loss | 2 |
| Assume primary care | 2 |
| Urinary incontinence | 1 |
Although the number of older adults cared for by primary care physicians is much greater than the number of older adults cared for by geriatric medicine physicians, the geriatric medicine ambulatory practice provides care for a different group of older adults. Figure 3 compares the percentage of older adults diagnosed with common geriatric syndromes in primary care with those diagnosed in the geriatric medicine ambulatory consultation practice and the geriatric medicine primary care practice. Consistent with the referral patterns described above, older adults cared for by geriatricians are more likely to suffer from these common geriatric syndromes.
Figure 3.
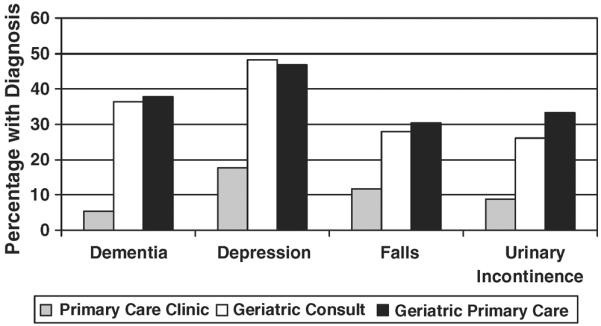
Prevalence of geriatric syndrome diagnoses in primary care and geriatric care clinics.
CHALLENGES
There are three notable challenges facing the program currently. First, the size and structure of the program limits how many older adults can be cared for and what types of older persons geriatric medicine providers in this healthcare system care for. Through interactions with other providers and because of the defined scope of the clinical program, the geriatric medicine program “trains” primary care physicians as to which patients geriatric medicine providers would like to see and which patients benefit from geriatric care. Geriatric medicine physicians' available clinical time is a critical rate-limiting factor in determining the number of older adults seen by geriatricians. For geriatric principled care to reach the greatest number of older adults, geriatric medicine physicians must work through other physicians. How much geriatrician effort to devote to hands-on primary care as opposed to co-management or system redesign is an ongoing debate.
The second challenge is the ever-changing landscape of payers, regulations, and other nongeriatric clinical programs. To the extent that a clinical service depends upon the financial support of the healthcare system, that clinical service is vulnerable to the financial struggles of the healthcare system. Such struggles are inevitable in an urban public hospital whose finances federal, state, and county revenue streams influence. The effect of these changes is so severe that relatively minor changes in financial incentives may dictate fundamental changes in the design and priorities of a geriatric clinical program.
The third challenge is the ongoing quality-of-care problems that primary care providers face. Like geriatric medicine, the primary care providers face serious resource limitations. The primary care practice at Wishard Health Services has served as an important laboratory for collaborative care research among older adults cared for in primary care practices.10–12 Figure 4 provides a summary of previously published outcome data across three different clinical trials.10–12 The intervention group in each of these three separate clinical trials received collaborative care as a mechanism to promote the standard of care in diagnosis and treatment for the targeted geriatric syndrome or condition. As shown in Figure 4, usual care in this practice often falls short of recommended standards of care for common geriatric syndromes. These studies further demonstrate that care can be improved if the resources and support available to primary care physicians can be improved. Unfortunately, there is still a great deal of room for quality improvement, and there is no clear pathway forward for the financial support of these new care models.9 The persistent quality gap inevitably fuels debate about how to best deploy limited geriatric medicine expertise, although this expertise typically involves not only geriatric medicine knowledge, but also team approaches to care that require resources for the rest of the geriatric care team.9,15
Figure 4.
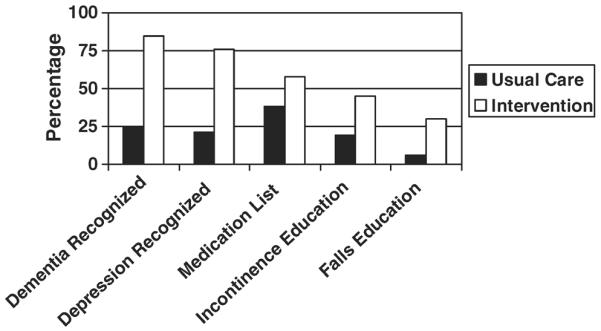
Potential to improve quality of care.
CONCLUSIONS
By design and by recognizing practical resource limitations, the geriatric medicine clinical practice described here serves to complement the care that the primary care practice provides to older adults. By design, geriatric medicine physicians participate in the care of a large percentage of hospitalized older adults. By design, geriatric medicine provides consultation for frailer older adults with geriatric syndromes and provides primary care to a small number of older adults. In recognition of clinical expertise and ongoing professional interactions, primary care physicians tend to cede care to geriatric medicine physicians for older adults with more-advanced disability and geriatric syndromes. This is perhaps most apparent for older adults in skilled nursing facilities but also includes older adults with geriatric syndromes whose primary care shifts to the ambulatory geriatric medicine clinic or to home-based care.
The primary limitation of this report is the focus on a single case history of a single academic geriatric medicine program, although this particular program provides an excellent illustration of the problems and prospects of a considered approach to deploying a limited geriatrics workforce. This particular program affords an opportunity to explore a real-world scenario, because this practice recognized early the role of primary care in delivering the foundation of care for older adults, there was access to practice pattern data through a comprehensive electronic medical record, and this primary care practice has been the site of several clinical trials testing innovations in new models of care. Finally, this clinical practice operates in a low-resource safety net environment providing care to underserved and poor older adults. Thus, implementation of state-of-the-art models of geriatric care tested in this environment would seem to be highly relevant to more-resource-rich healthcare systems.
The mixed rewards of the geriatric medicine team providing care to a large population of older adults in skilled nursing facilities have been noted. This activity is largely invisible to clinical colleagues and tends to pull the geriatricians away from the main hub of clinical activity. There is a dynamic interplay between design features, reputation, and capacity that modulates volume, location, and type of patients seen by geriatrics. Changes in health system revenue streams and incentives also influence the number and type of patients touched by the geriatric medicine service.
ACKNOWLEDGMENTS
Sponsors' Role: None.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this article. Supported in part by the Indiana University John A. Hartford Foundation Center of Excellence in Geriatric Medicine and by National Institute on Aging Grants P30AG024967, K24 AG024078, and K23 AG020088.
Author Contributions: All listed authors warrant authorship by their contribution to the conception and design of the study and analysis and interpretation of the data; writing of the manuscript; and approval of the final version.
This is one of the three papers presented at the Association of Directors of Geriatrics Academic Programs symposium at the American Geriatrics Society annual meeting in 2007. An accompanying editorial and commentary are included in this brief series.
REFERENCES
- 1.Besdine R, Boult C. American Geriatrics Society Task Force on the Future of Geriatric Medicine. et al. Caring for older Americans: The future of geriatric medicine. J Am Geriatr Soc. 2005;53:S245–S256. doi: 10.1111/j.1532-5415.2005.53350.x. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine . Report of a Study. National Academy Press; Washington, DC: 1978. Aging and Medical Education. [Google Scholar]
- 3.Rowe JW, Grossman E, Institute of Medicine Committee on Leadership for Academic Geriatric Medicine et al. Academic geriatrics for the year 2000: An Institute of Medicine report. N Engl J Med. 1987;316:1425–1428. doi: 10.1056/NEJM198705283162229. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine . Strengthening Training in Geriatrics for Physicians. National Academy Press; Washington, DC: 1993. [Google Scholar]
- 5.Institute of Medicine . In: Training Physicians to Care for Older Americans: Progress, Obstacles, and Future Directors. Reuben DB, Beck JC, editors. National Academy Press; Washington, DC: 1994. [PubMed] [Google Scholar]
- 6.Warshaw GA, Bragg EJ, Thomas DC, et al. Association of Directors of Geriatric Academic Programs. Are internal medicine residency programs adequately preparing physicians to care for the baby boomers? A national survey from the Association of Directors of Geriatric Academic Programs status of geriatrics workforce study. J Am Geriatr Soc. 2006;54:1603–1609. doi: 10.1111/j.1532-5415.2006.00895.x. [DOI] [PubMed] [Google Scholar]
- 7.Reuben DB, Lee M, Katz D, et al. Building academic geriatric capacity: An evaluation of the John A. Hartford Foundation Centers of Excellence initiative. J Am Geriatr Soc. 2004;52:1384–1390. doi: 10.1111/j.1532-5415.2004.52373.x. [DOI] [PubMed] [Google Scholar]
- 8.Warshaw GA, Bragg EJ. The training of geriatricians in the United States: Three decades of progress. J Am Geriatr Soc. 2003;51:S338–S345. doi: 10.1046/j.1365-2389.2003.51345.x. [DOI] [PubMed] [Google Scholar]
- 9.Institute of Medicine (IOM) Retooling for an Aging America: Building the Health Care Workforce. The National Academies Press; Washington, DC: 2008. [PubMed] [Google Scholar]
- 10.Unutzer J, Katon W, Callahan CM, et al. Improving mood-promoting access to collaborative treatment. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 11.Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: A randomized controlled trial. JAMA. 2006;295:2148–2157. doi: 10.1001/jama.295.18.2148. [DOI] [PubMed] [Google Scholar]
- 12.Counsell SR, Callahan CM, Clark DO, Tu W, Buttar AB, Stump TE, Ricketts GD. Geriatric care management for low-income seniors. JAMA. 2007;298:2623–2633. doi: 10.1001/jama.298.22.2623. [DOI] [PubMed] [Google Scholar]
- 13.McDonald CJ, Overhage JM, Tierney WM, et al. The Regenstrief medical record system: A quarter century experience. Int J Med Inform. 1999;54:225–53. doi: 10.1016/s1386-5056(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 14.Counsell SR, Holder CM, Liebenauer LL, et al. Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older patients: A randomized controlled trial of Acute Care for Elders (ACE) in a community hospital. J Am Geriatr Soc. 2000;48:1572–1581. doi: 10.1111/j.1532-5415.2000.tb03866.x. [DOI] [PubMed] [Google Scholar]
- 15.Callahan CM, Counsell SR. Measuring and communicating the value of geriatrics. J Am Geriatr Soc. 2002;50:1741–1743. doi: 10.1046/j.1532-5415.2002.50471.x. [DOI] [PubMed] [Google Scholar]


