Abstract
Objective:
The aim of this study was to evaluate the influence of removable partial dentures (RPD) on the periodontal health of abutment and non-abutment teeth.
Materials and Methods:
A total 107 patients with RPD participated in this study. It was examined 138 RPD, they were 87 with clasp-retained and 51 were RPD with attachments. The following periodontal parameters were evaluated for abutment and non-abutment teeth, plaque index (PLI), calculus index (CI), bleeding on probing (BOP), probing depth (PD) (mm) and tooth mobility (TM) index. These clinical measurements were taken immediately before insertion the RPD, then one and 3 months after insertion. The level of significance was set at (P < 0.05).
Results:
The mean scores for PLI, CI, BOP, PD, and TM index, of the abutment teeth and non-abutment teeth were no statistically significant at the time of insertion of RPD. After 1-month, PLI was statistically significant (0.57 ± 0.55 for abutment and 0.30 ± 0.46 for non-abutment teeth). After 3 months, there were significant differences between abutment and non-abutment teeth with regard to the BOP (1.53 ± 0.50 and 1.76 ± 0.43 respectively), PD (0.28 ± 0.45 and 0.12 ± 0.33 respectively) and PLI (1.20 ± 0.46 and 0.75 ± 0.64 respectively). No significant mean difference in TM and CI was found between the abutment and non-abutment teeth (P > 0.05).
Conclusions:
With carefully planned prosthetic treatment and adequate maintenance of the oral and denture hygiene, we can prevent the periodontal diseases.
Keywords: Abutment teeth, periodontal disease, removable partial denture
INTRODUCTION
Removable partial dentures (RPD) have an important role in the health of periodontium. Glickman[1] in 1948 reported that from periodontal viewpoint, fixed prostheses are most suitable for replacement of missing teeth, but there are certain clinical situations where RPD are the only possible way to restore the function of teeth, as is the case of Kennedy class I and II. Some patients are unable to afford treatment with implants either anatomical or economic reasons, therefore RPD can be considered a simple, noninvasive, and relatively cheap treatment option for the shortened dental arch.[2]
One of the most popular methods since 1970 for the replacement of missing teeth was RPD, whereas many dentists consider a prosthetic rehabilitation of the second class. Also according to some studies RPD are not recommended for all patients, especially in patients where teeth mobility had movement is not >1 mm.[3,4,5] RPD are generally attached to the abutment natural teeth by clasps or attachments that hold the denture in place.[6] RPD in the mouth has the potential of increase plaque formation on tooth surface in contact with RPD, especially to abutment teeth, to which clasps or attachments are attached.[7,8,9,10]
Epidemiological studies in animals and in humans have shown that dental plaque is an essential factor in the etiology of periodontitis.[11] RPD can increase the incidence of caries; damage the periodontium, relatively large amounts of plaque and the amount of stress on natural teeth.[12,13,14] According to Preshaw et al. and Rodan et al.,[15,16] RPD can increase the risk of dental plaque, gingivitis and especially root caries; however, the risk of periodontitis is not large by them.[15] Kennedy classification, denture base shape, denture construction and especially the number of position of the clasps and occlusal rests also influence periodontal deterioration.[17]
Therefore, the control of dental plaque is important to obtain good denture prognosis and performance for a long period. Many studies have investigated the effect of regular checkups on oral health and denture hygiene with carefully planned prosthetic treatment. All periodontal parameters appeared with better results in patients who were going to receive RPDs, and they should be motivated and instructed in order to prevent periodontal diseases.[13,18] According to Akaltan et al. during 30 months study concluded that adequate oral hygiene and systemic controls can improve periodontal health of patients with RPD.[19]
The aim of this study was to evaluate the influence of RPD on periodontal health of abutment and non-abutment teeth, recorded by plaque index (PLI), Calculus index (CI), Blending on probing (BOP), probing depth (PD), Tooth mobility (TM), before insertion, one and after 3 months of wearing.
MATERIALS AND METHODS
A total of 107 patients with RPD made by different clinicians at the Prosthodontics Department at University Dentistry Clinical Center, Prishtina, Kosovo, have participated in this study.
Inclusion criteria were patients with partially non-RPD wearers who were candidates for RPD rehabilitation with no history of recent extractions within 3 months.[20] Before the prosthetic treatment, all patients were motivated and given oral hygiene instruction as well as periodontal therapy where indicated. Denture design for each individual patient was based on oral health statute and remaining teeth; where mobility of abutment teeth movement was not >1 mm. The study has been reviewed and approved by Joint Ethic Committee (no 1551) in the University Dentistry Clinical Centre of Kosovo. All patients gave written informed consent.
Abutment teeth used as direct or indirect retainer for the RPD were a study group, while the non-abutment teeth in the same jaw were used as a control group. Periodontal examination was conducted and the following variables were determined: (PLI) (Silness/Löe), (CI) (Green-Vermilion), bleeding on probing (BOP), PD and TM.
Plaque index according to Silness/Löe Index 1964.[21] Calculus index according to Green-Vermilion Index 1964.[22] BOP according to Ainamo and Bay 1975.[23] Measurements were made in mesial and distal surface in abutment and non-abutment teeth and deemed positive if it occurred within 20 s after probing while a negative was given for nonbleeding site.
Probing pocket depth (PD) was measured from the crest of the gingival margin to a probable pocket depth using a Williams Probe and read to the nearest millimeters (mm). Measurements were made in the fourth surfaces in abutment teeth: Mesial, oral, distal and vestibular surfaces. Scores ranging from 0 to 3 represented the highest PD observed: 0 - Normal probe depth of 2 mm or less; 1 - Probe depth of about 2 mm, but not >3 mm; 2 - Probe depth >3 mm but <5 mm and 3 - Probe depth greater than 5 mm or more.[24]
Tooth mobility (TM) was recorded according to Miller 1985 a scale from 0 to 3: 0 - No mobility; 1 - mobility smaller than 1 mm in the horizontal direction; 2 - Mobility >1 mm in the horizontal direction; 3 - mobility in the apical-vertical directions.[25]
These clinical measurements were taken immediately before insertion the RPD, then one and 3 months after insertion. All patients received the motivation and instructions for their oral hygiene in order to create a high level of co-operation.
Statistical analysis was performed using Statistical Package for Social Science 22 for Windows (SPSS Inc., Chicago, Illinoiss, USA). The study results are presented in table form. Statistical parameters were calculated from the structure index, arithmetic average and standard deviation, minimum, and maximum values. Testing data were done with Mann-Whitney test. Differences were considered significant when P < 0.05.
RESULTS
Study population characteristics
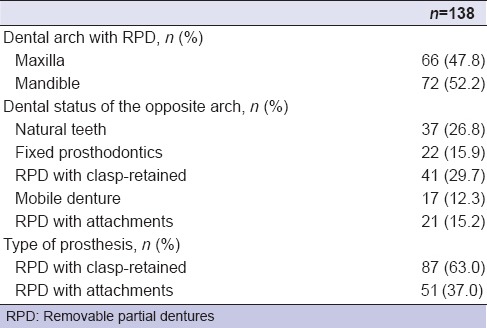
The 107 patients presented with 342 abutment teeth and 610 non-abutment teeth in this study. In total, it was examined 138 RPD, and each prosthesis was considered statistically independent case. They were 87 partial dentures with clasp-retained and 51 were RPD with attachments, 49 females and 58 males, aged between 33–80 years. The examined RPD were 66 from maxillary arch and 72 from mandibles arch. Other demographic parameters have shown in Tables 1 and 2.
Table 1.
Study population demographics
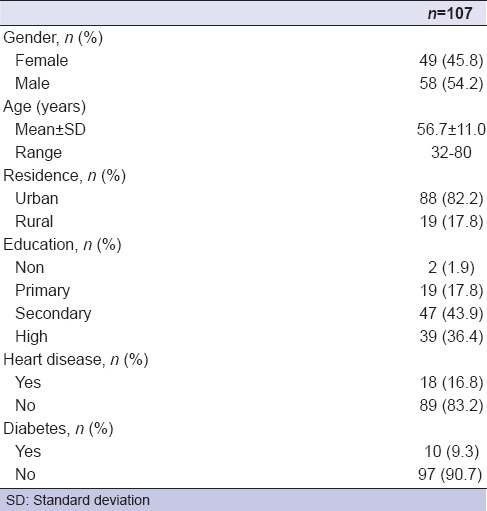
Table 2.
Clinical characteristics of the sample
Clinical periodontal parameters
The mean values and standard deviation of periodontal parameters of abutment and non-abutment teeth of RPD wearing are shown in Tables 3–5.
Table 3.
Comparison of periodontal parameters between abutment and non-abutment teeth at the time of insertion RPD
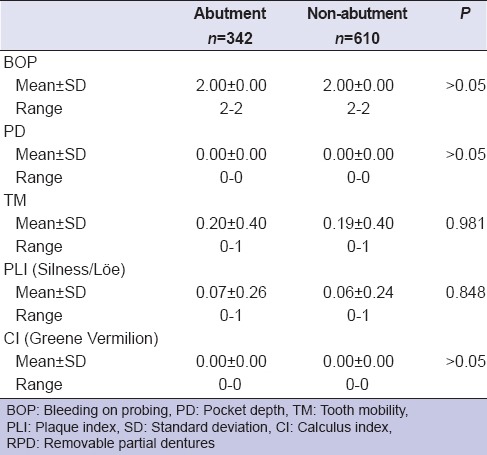
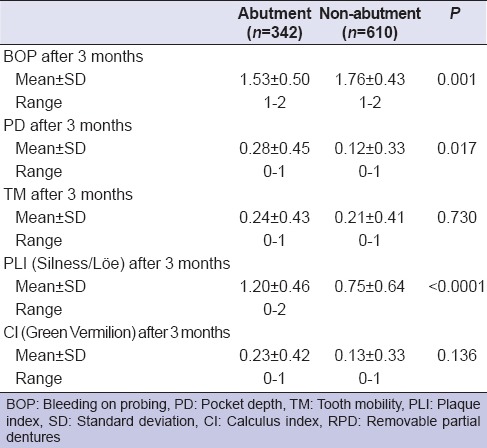
Table 5.
Comparison of periodontal parameters between abutment and non-abutment teeth after 3 months of insertion RPD
The mean scores for PLI, CI, BOP, PD, and TM index, of the abutment teeth and non-abutment teeth were no statistically significant at the time of insertion of RPD and after 1-month, except PLI index were statistically significant 0.57 ± 0.55 for abutment and 0.30 ± 0.46 for non-abutment teeth [Tables 3 and 4].
Table 4.
Comparison of periodontal parameters between abutment and non-abutment teeth after 1-month of insertion RPD
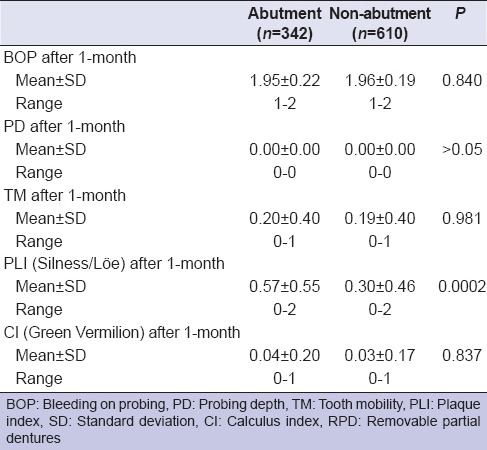
Table 5 shows that after 3 months of wearing of the RPD's, there were significant differences between abutment and non-abutment teeth with regard to the BOP (1.53 ± 0.50 and 1.76 ± 0.43 for abutment and non-abutment teeth respectively), PD (0.28 ± 0.45 and 0.12 ± 0.33 for abutment and non-abutment respectively) and PLI (1.20 ± 0.46 and 0.75 ± 0.64 for abutment and non-abutment respectively). There was found no significant mean difference in TM and CI between the abutment and non-abutment teeth (P > 0.05).
DISCUSSION
The influence of RPD's was studied on the periodontal parameter (BOP, PD, PLI, CI and TM) of abutment and non-abutment teeth. The results of our study showed PLI index were statistically significant after 1-month (P < 0.0001). Mean scores for BOP, PD, PLI index of the abutment teeth were significantly greater compared to non-abutment teeth after 3 months (P < 0.001). This difference can be explained, because 9.3% of patients were with diabetes, 16.8% with heart disease and 37% with RPD's with attachment that affect periodontal changes, while most recent studies have excluded cases with diabetes and heart diseases. High scores of PLI and a maintenance interval longer than 3 months were significant predictors for positive changes in periodontium. Our results agree with Mine K that the microbiological risk for periodontitis of abutment teeth is greater than at non-abutment teeth in RPD's wearers after 6 months that were significant predictors for positive red complex scores (P < 0.05). In the pocket depth, there was found no significant mean difference found between the abutment and non-abutment teeth.[26]
Yeung et al.[14] analyzed a total of 87 patients 5–6 years after placement cobalt–chromium RPD's wearers and concluded there was a high prevalence of gingivitis, plaque, and gingival recession, especially in dentogingival surfaces in close proximity (within 3 mm) to the dentures. Furthermore, according to the author do Amaral BA, PLI values significantly increased after 1-year of RPD's wearing in abutment teeth, comparing with non-abutment teeth. It was also confirmed that PD and GI mean values increased from the initial assessment to 1-year of RPD's.[27]
Samir et al., according to their study for at least 3 years in 36 patients with RPD's, concluded that direct abutments teeth are more periodontal affected than non-abutment teeth between regular and irregular attendants. Due to not assess of education, motivation and awareness during the stage of RPD's construction in their study, they may founded significant difference in clinical attachment level and plaque accumulation, between study and control group of teeth.[28] Further, according to Bergman et al., it was concluded that there were no periodontal changes in patients after a 10 years period of wearing the RPD's. These results are a consequence of conventional oral hygiene programs, uncontrolled chemical or additional technique. This study does not support the concept that the RPD's will increase the incidence of caries or periodontal disease.[13]
In our study, we have assessed education, motivation and awareness of the patients during the stage of RPD's construction. Although minor difference could be regarded as initial stage in periodontal changes which is important to diagnose and halt further destruction. These results could be attributed to planned prosthetic treatment, so with an appropriate designs and good oral hygiene can reduce changes that may affect in periodontal disease of abutment teeth.[29,30,31]
The results indicate that RPD's wearers should be motivated for extra adequate oral hygiene instructions. In order to eliminate the periodontal damages caused by RPD's regular recall system is strongly recommended.[32] Some clinical studies have shown that after the regular examinations, reinstructions and the patient's remotivation oral hygiene maintenance, RPD's will not cause changes in periodontal abutment teeth.[28,33,34] Shigeto et al. Concluded that patients who received periodic maintenance care 4 times/year were effective to maintain good periodontal conditions for the wearers of PRD.[35]
CONCLUSIONS
The lack of oral hygiene and health care management may be the cause of the loss of abutment teeth for elderly patients. With carefully planned prosthetic treatment and adequate maintenance of the oral and denture hygiene, we can prevent the periodontal diseases. Regular recall of appointments plays an important role in preventing changes of abutment tooth.
ACKNOWLEDGMENTS
The authors acknowledge all the patients of the University Dentistry Clinical Center, Pristina, Kosova that have facilitated in this study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Glickman I. The periodontal structures and removable partial denture prosthesis. J Am Dent Assoc. 1948;37:311–6. [PubMed] [Google Scholar]
- 2.Nassani MZ, Tarakji B, Baroudi K, Sakka S. Reappraisal of the removable partial denture as a treatment option for the shortened dental arch. Eur J Dent. 2013;7:251–6. doi: 10.4103/1305-7456.110199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Körber E, Lehmann K, Pangidis C. Control studies on periodontal and periodontal-gingival retention of partial prosthesis. Dtsch Zahnarztl Z. 1975;30:77–84. [PubMed] [Google Scholar]
- 4.Addy M, Bates JF. Plaque accumulation following the wearing of different types of removable partial dentures. J Oral Rehabil. 1979;6:111–7. doi: 10.1111/j.1365-2842.1979.tb01271.x. [DOI] [PubMed] [Google Scholar]
- 5.Mojon P, Rentsch A, Budtz-Jørgensen E. Relationship between prosthodontic status, caries, and periodontal disease in a geriatric population. Int J Prosthodont. 1995;8:564–71. [PubMed] [Google Scholar]
- 6.Dosumu OO, Dosumu EB, Arowojolu MO, Babalola SS. Rehabilitative management offered Nigerian localized and generalized aggressive periodontitis patients. J Contemp Dent Pract. 2005;6:40–52. [PubMed] [Google Scholar]
- 7.Vacaru R, Podariu AC, Jumanca D, Galuscan A, Muntean R. Periodontal-restorative interrelationships. Oral Health Dent Med Bas Sci. 2003;3:12–5. [Google Scholar]
- 8.Davenport JC, Basker RM, Heath JR, Ralph JB, Glantz PO. A clinical guide to removable partial dentures. The removable partial denture equation. Br Dent J. 2000;189:414–24. doi: 10.1038/sj.bdj.4800787. [DOI] [PubMed] [Google Scholar]
- 9.Sesma N, Laganá DC, Morimoto S, Gil C. Effect of denture surface glazing on denture plaque formation. Braz Dent J. 2005;16:129–34. doi: 10.1590/s0103-64402005000200008. [DOI] [PubMed] [Google Scholar]
- 10.Davenport JC, Basker RM, Heath JR, Ralph JB, Glantz PO, Hammond P. A clinical guide to removable partial dentures. Connectors. Br Dent J. 2001;190:184–91. doi: 10.1038/sj.bdj.4800919a. [DOI] [PubMed] [Google Scholar]
- 11.Bergman B. Periodontal reactions related to removable partial dentures: A literature review. J Prosthet Dent. 1987;58:454–8. doi: 10.1016/0022-3913(87)90275-7. [DOI] [PubMed] [Google Scholar]
- 12.de Baat C. Elderly people and removable partial dentures. Ned Tijdschr Tandheelkd. 2009;116:665–8. [PubMed] [Google Scholar]
- 13.Bergman B, Hugoson A, Olsson CO. Caries, periodontal and prosthetic findings in patients with removable partial dentures: A ten-year longitudinal study. J Prosthet Dent. 1982;48:506–14. doi: 10.1016/0022-3913(82)90352-3. [DOI] [PubMed] [Google Scholar]
- 14.Yeung AL, Lo EC, Chow TW, Clark RK. Oral health status of patients 5-6 years after placement of cobalt-chromium removable partial dentures. J Oral Rehabil. 2000;27:183–9. doi: 10.1046/j.1365-2842.2000.00512.x. [DOI] [PubMed] [Google Scholar]
- 15.Preshaw PM, Walls AW, Jakubovics NS, Moynihan PJ, Jepson NJ, Loewy Z. Association of removable partial denture use with oral and systemic health. J Dent. 2011;39:711–9. doi: 10.1016/j.jdent.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Rodan R, Al-Jabrah O, Ajarmah M. Adverse effects of removable partial dentures on periodontal status and oral health of partially edentulous patients. JRMS. 2012;19:53–8. [Google Scholar]
- 17.Zlataric DK, Celebic A, Valentic-Peruzovic M. The effect of removable partial dentures on periodontal health of abutment and non-abutment teeth. J Periodontol. 2002;73:137–44. doi: 10.1902/jop.2002.73.2.137. [DOI] [PubMed] [Google Scholar]
- 18.Yap UJ, Ong G. Periodontal considerations in restorative dentistry. Part 2: Prosthodontic considerations. Dent Update. 1995;22:13–6. [PubMed] [Google Scholar]
- 19.Akaltan F, Kaynak D. An evaluation of the effects of two distal extension removable partial denture designs on tooth stabilization and periodontal health. J Oral Rehabil. 2005;32:823–9. doi: 10.1111/j.1365-2842.2005.01511.x. [DOI] [PubMed] [Google Scholar]
- 20.Kapur K, Shklar G. The effect of complete dentures on alveolar mucosa. J Prosthet Dent. 1963;13:1030–7. [Google Scholar]
- 21.Silness J, Loe H. Periodontal disease in pregnancy. ii. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 22.Greene JC, Vermillion JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:7–13. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 23.Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25:229–35. [PubMed] [Google Scholar]
- 24.Mombelli A. Clinical parameters: Biological validity and clinical utility. Periodontol 2000. 2005;39:30–9. doi: 10.1111/j.1600-0757.2005.00117.x. [DOI] [PubMed] [Google Scholar]
- 25.Miller PD., Jr A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5:9–13. [PubMed] [Google Scholar]
- 26.Mine K, Fueki K, Igarashi Y. Microbiological risk for periodontitis of abutment teeth in patients with removable partial dentures. J Oral Rehabil. 2009;36:696–702. doi: 10.1111/j.1365-2842.2009.01982.x. [DOI] [PubMed] [Google Scholar]
- 27.do Amaral BA, Barreto AO, Gomes Seabra E, Roncalli AG, da Fonte Porto Carreiro A, de Almeida EO. A clinical follow-up study of the periodontal conditions of RPD abutment and non-abutment teeth. J Oral Rehabil. 2010;37:545–52. doi: 10.1111/j.1365-2842.2010.02069.x. [DOI] [PubMed] [Google Scholar]
- 28.Qudah SA, Nassrawin N. Effect of removable partial denture on periodontal health. JRMS. 2004;11:17–9. [Google Scholar]
- 29.Rissin L, Feldman RS, Kapur KK, Chauncey HH. Six-year report of the periodontal health of fixed and removable partial denture abutment teeth. J Prosthet Dent. 1985;54:461–7. doi: 10.1016/0022-3913(85)90413-5. [DOI] [PubMed] [Google Scholar]
- 30.Santos MB, Carvalho RM, Guimarães TS, Santos JF, Marchini L. Longitudinal study of removable partial dentures and hygiene habits. Cien Odontol Bras. 2007;10:38–43. [Google Scholar]
- 31.Agrali OB, Kuru BE. Periodontal treatment in a generalized severe chronic periodontitis patient: A case report with 7-year follow-up. Eur J Dent. 2015;9:288–92. doi: 10.4103/1305-7456.156844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kern M, Wagner B. Periodontal findings in patients 10 years after insertion of removable partial dentures. J Oral Rehabil. 2001;28:991–7. doi: 10.1046/j.1365-2842.2001.00788.x. [DOI] [PubMed] [Google Scholar]
- 33.Kapur KK, Deupree R, Dent RJ, Hasse AL. A randomized clinical trial of two basic removable partial denture designs. Part I: Comparisons of five-year success rates and periodontal health. J Prosthet Dent. 1994;72:268–82. doi: 10.1016/0022-3913(94)90340-9. [DOI] [PubMed] [Google Scholar]
- 34.Bergman B, Ericson A, Molin M. Long-term clinical results after treatment with conical crown-retained dentures. Int J Prosthodont. 1996;9:533–8. [PubMed] [Google Scholar]
- 35.Koyama S, Hanabuchi S, Fuji T, Ina Y, Yoda N, Hanawa S, et al. The difference between baseline and 5-year examinations at recall in PCR, PD, tooth mobility, and BRL of abutment teeth in subjects who had received periodic maintenance care more than 4 times/year. Ann Jpn Prosthodont Soc. 2012;4:59–67. [Google Scholar]


