Abstract
An implant-supported hybrid prosthesis is an acrylic resin complete fixed dental prosthesis and supported by implants might be a solution in extreme cases that the need of the restoration for esthetics, function, lip support, and speech. This clinical report aims to present the esthetic and functional prosthetic rehabilitation of three borderline cases with implant-supported hybrid prostheses. Patient 1 (62-year-old man) and Patient 2 (61-year-old man) presented a chief complaint of a compromised esthetic. After clinical evaluations, in Patient 1, 8 implants in the maxilla and 7 implants in mandibula were observed. Patient 2 had 7 implants in the maxilla and 7 implants in mandibula, which were previously placed. The intra-arch dimension of both patients was excessive and an insufficient peri-oral soft tissue support was observed. Patient 3 was a 61-year-old man had 2 implants with a history of previously implanted graft infection and implant loss on his maxillary posterior jaw. An excessive intra-arch dimension was observed in clinical examination. In addition, massive bone defect and insufficient soft tissue support were examined. In all patients, implant-supported hybrid prostheses were successfully performed. The clinical and radiologic findings were satisfactory. After 3 years of follow-up, no functional, phonetic, or esthetic problems with the restorations were noted. These case reports suggest that implant-supported hybrid prostheses can be a reliable alternative treatment procedure when a porcelain-fused metal fixed restoration does not satisfy a patient's requirements for esthetics, phonetics, oral hygiene, and oral comfort.
Keywords: Dental implants, hybrid prosthesis, intra-arch distance
INTRODUCTION
Dental implants have become increasingly important in oral reconstruction. The high rate of success of rehabilitation with implant-supported prostheses has increased esthetic demands of patients and clinicians.[1] To obtain satisfactory functional and esthetic results, it is essential to achieve osseointegration and the ideal location of implants to support the intended restoration.[2]
The main objective in implant therapy is either to avoid complete removable dentures by placement of implant-supported fixed prostheses or to improve the retention and stability of removable complete dentures.[3] Basically, two approaches for an implant-supported fixed prosthesis exist. The first one is a metal-ceramic implant-supported fixed prosthesis consists of a ceramic layer bonded to a cast metal framework that can be cemented to transmucosal abutments or secured with prosthetic retention screws.[3] An alternative to this type of fixed prosthesis is an implant-supported hybrid prosthesis.[2] Implant supported metal-acrylic resin complete fixed dental prosthesis, originally referred to as a hybrid prosthesis was introduced to address the problems caused by unstable and uncomfortable mandibular dentures. The primary factor that determines the restoration type is the amount of intra-arch space.[2] In addition, other patient-relevant clinical parameters such as lip support, high maxillary lip line during smiling, a low mandibular lip line during a speech or the patient's greater esthetic demands should be evaluated.[2]
Hybrid prostheses have a great number of advantages including reducing the impact force of dynamic occlusal loads, being less expensive to fabricate and highly esthetic restorations.[2] Furthermore, they may be successfully used by a combination of tilted and axially placed implants in partial edentulism in the posterior part of resorbed maxillae.[3] However, food impaction, speech problems or difficulties in dealing with hygiene were reported by authors.[2]
Despite the favorable long-term outcomes achieved with prosthetic rehabilitations with implants, biological and technical complications such as surgical complications, implant loss, bone loss, peri-implant soft-tissue complications, mechanical complications, and aesthetic/phonetic complications are frequent.[4] The authors implied that such complications are affected by many factors, including the operator's skills and judgments in treatment planning, prosthesis design, materials, patient-specific factors, and local and systemic conditions and habits such as bruxism, smoking, presence of periodontal disease, and maintenance.[3] Furthermore, the communication between the prosthodontist and surgeon is emphasized as critical to ensure adequate restorative space for the various prosthetic designs, appropriate implant angulation, and minimizing cantilevers.[3]
The purpose of this clinical report is to present the clinical experience and positive outcomes of treating three patients who previously had biologic and technical complications in their implant therapy by means of the implant-supported hybrid prosthesis.
CASE REPORT
This clinical report included three male patients (mean age of 61 years) who were referred to our clinic with their previously placed dental implants (Straumann AG, Basel, Switzerland) on their complete/partial edentulous jaws. The reviews of the patients’ medical histories revealed no significant findings.
Clinical and radiographical evaluations before the prosthetic phase
Patient 1
A 62-year-old presented with a chief complaint of a compromised esthetic. The patient expressed a desire for fixed restorations and also needed to construct the collapse of his lip and cheek. At the clinical evaluations, it was seen that 8 implants in maxilla and 7 implants in mandibula had been placed previously, in sites #11, 13, 14, 17, 21, 23, 24, 27, 33, 34, 35, 37, 43, 44, 47 and complete-arch temporary fixed prostheses were fabricated in his upper and lower jaws. Figure 1 shows an intraoral view of the patient and the panoramic radiograph taken at the initial examination.
Figure 1.
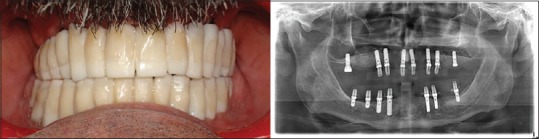
Intraoral view of the Patient 1 and a panoramic radiograph taken at the initial examination
Patient 2
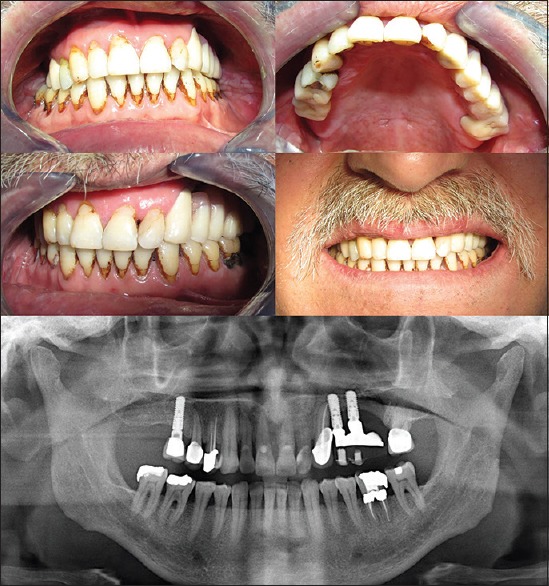
A 61-year-old was referred to our clinic with a previous history as he attended a private dental office seeking full prosthetic rehabilitation. The patient also presented with a chief complaint of compromised esthetic and indicated that implants were placed into his jaws 5 months before the appointment. Clinical evaluations represented that, 7 implants in maxilla and 7 implants in mandibula had been placed in sites #11, 13, 14, 21, 23, 24, 27, 33, 34, 36, 37, 43, 44, 46. Healing screws were in his mouth. Figure 2 shows an intraoral view of the patient and a panoramic radiograph taken at the initial examination.
Figure 2.
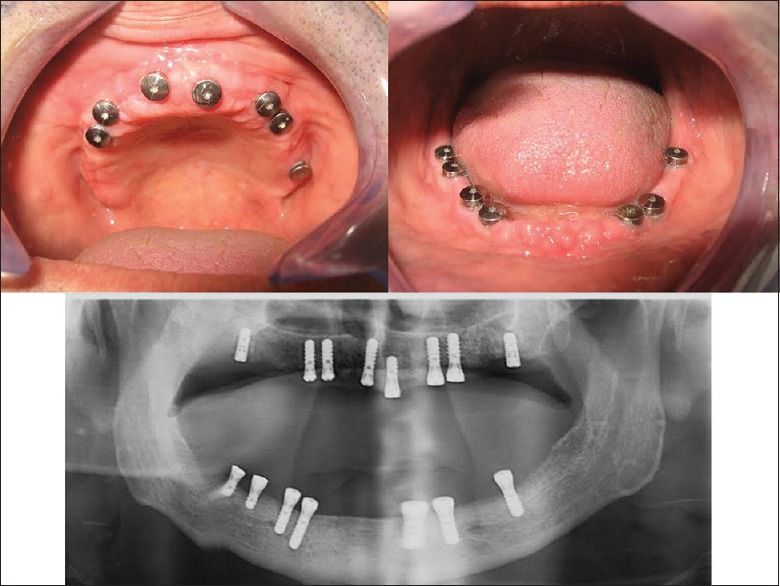
Intraoral view of the Patient 2 and a panoramic radiograph taken at the initial examination
Patient 3
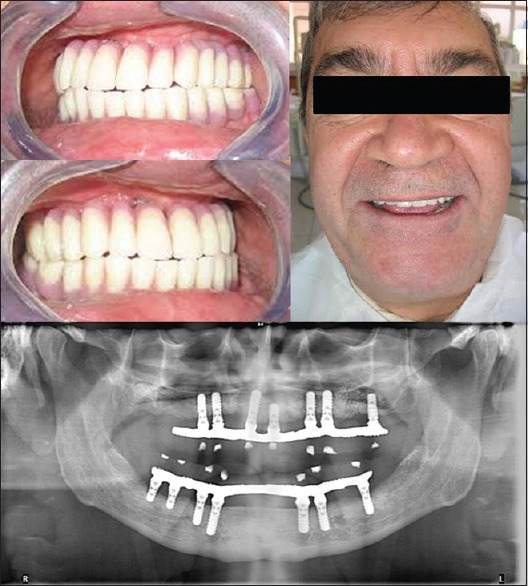
A 61-year-old was referred to our clinic after a series of implant surgery complications. Patient's dental history presented that, one implant was placed in the right posterior maxillary jaw and two implants in the left posterior area following the left maxillary sinus elevation operation at the same appointment. The patient mentioned that 1-month after the sinus surgery, the graft material was infected and the distal implant was failed. Additionally, he reported that, 1 month after these complications occurred, another implant was placed next to the mesial implant on that area. Clinical evaluations demonstrated that the implants were in sites #16, 24, 25 and an implant supported crown restoration had been fabricated in #16 implant when he referred to our clinic. Figure 3 shows intraoral view and diagnostic model of the patient, and a panoramic radiograph taken at the initial examination. Maxillofacial surgeon evaluated all the patients about the complications and surgical treatment modalities.
Figure 3.
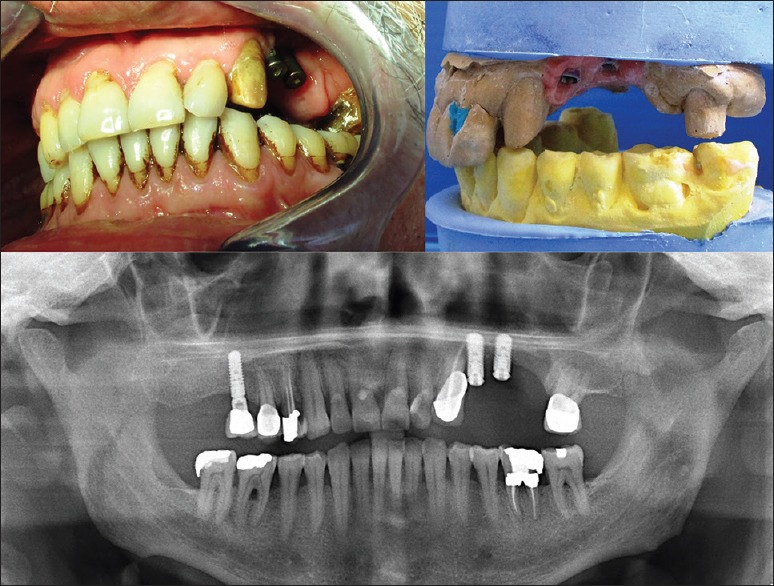
Intraoral view, diagnostic model of the Patient 3 and a panoramic radiograph taken at the initial examination
Informed consent was obtained from each patient before the prosthetic phase. In Patient 1, temporary prostheses and implant abutments were removed, then healing screws were placed. In all patients, maxillary and mandibular preliminary impressions were made with irreversible hydrocolloid impression material (Cavex Color Change, Haarlem, The Netherlands) with stock metal trays (CEO; GC America, Alsip, Ill). The impressions were poured with Type III dental stone (Whip Mix Dental Stone, Whip Mix Corp, Louisville, Kentucky, USA).
For Patients 1 and 2, light-cured acrylic resin (Vertex Light Curing Trayplates, Vertex-Dental B.V., Zeist, The Netherlands) record bases were fabricated and baseplate wax was used to add occlusion rims. Occlusal vertical dimensions were established. Centric relation records were made with modeling wax (Modeling wax, Dentsply DeTrey, Surrey, England) and impression compound (Kerr Corp, California, USA). For patient C, polyether inter-occlusal bite registration material (Ramitec, 3M Espe AG, Seefeld, Germany) was used to record centric relation. Maxillary and mandibular diagnostic casts were mounted on an average-value articulator (Stratos 100, Ivoclar Vivadent AG, Schaan, Liechtenstein) with Type IV dental stone (GC Fujirock, GC Corporation, Leuven, Belgium).
Diagnostic model analysis showed that, intra-arch distance was 32 mm for Patient 1; 30 mm for Patient 2, and 26 mm for Patient 3. Therefore, it was decided to fabricate implant-supported metal-acrylic resin screw-retained fixed dental prostheses for the treatment of patients.
Radiographic evaluations confirmed that the implant fixtures had successfully integrated with the bone, so the prosthetic phase was started.
Prosthetic phase
Healing screws were removed, and impression copings with appropriate diameters were placed. Implant level impressions were made by using the open tray technique in Patients 1 and 2 with individual trays, and closed tray technique in Patient 3 with a stock tray and polyvinylsiloxane (Imprint™ 3 VPS, 3 M ESPE, St. Paul, MN, USA). Implant analogs were attached to the copings in the completed impressions before pouring. Soft tissue was reproduced in the impression with soft tissue moulage material (Kerr, Orange, CA, USA), and maxillary and mandibular definitive working casts were poured with type III dental stone (Microstone, Whip Mix Corp., Louisville, KY, USA).
In Patients 1 and 2, occlusal vertical dimension was established and centric relation records were made with record bases, occlusal rims, and inter-occlusal bite registration material. Esthetics and phonetics were used to establish the position of the anterior teeth. In Patient 3, inter-occlusal bite registration material was used to record inter-occlusal relation. Then, face-bow transfers (UTS 3D Transferbow, Ivoclar Vivadent AG, Schaan, Liechtenstein) were made. In all patients, maxillary definitive casts were mounted on a fully adjustable articulator (Stratos 300, Ivoclar Vivadent AG, Schaan, Liechtenstein) with Type III mounting stone (Mounting Stone; Whip Mix Corp, Louisville, Kentucky, USA). Mandibular diagnostic casts were mounted by using the centric relation record. The protrusive records were made to adjust the articulator settings for the horizontal and lateral condylar indications. A verification index for each prosthesis was fabricated with pattern resin (GC pattern resin, GC America, Alsip, IL, USA) connecting the impression copings. The verification indexes were checked intraorally to confirm the accuracy of the master cast. Then, the metal frameworks were fabricated in the dental laboratory. They were checked intraorally to confirm their passively seating over the implants [Figure 4a–c]. The tooth setting was done over each framework using prefabricated resin teeth (SR Phonares II, Ivoclar Vivadent AG, Schaan, Liechtenstein) and evaluated clinically, verifying that the midline, occlusal plane, vertical dimension of occlusion, and centric relation. Esthetics and phonetics were evaluated, and the patient's acceptance was obtained at the trial insertion appointments. The prostheses were fabricated and adjusted to maintain occlusal point contacts in centric relation and anterior guidance in protrusion and canine guidance in lateral excursions, in Patients 1 and 2. In Patient 3, the prosthesis was in harmony with his existing habitual occlusion. The prostheses were also fabricated to have slight contact with mucosa to avoid speech difficulties while permitting access for proper hygiene measures.
Figure 4.
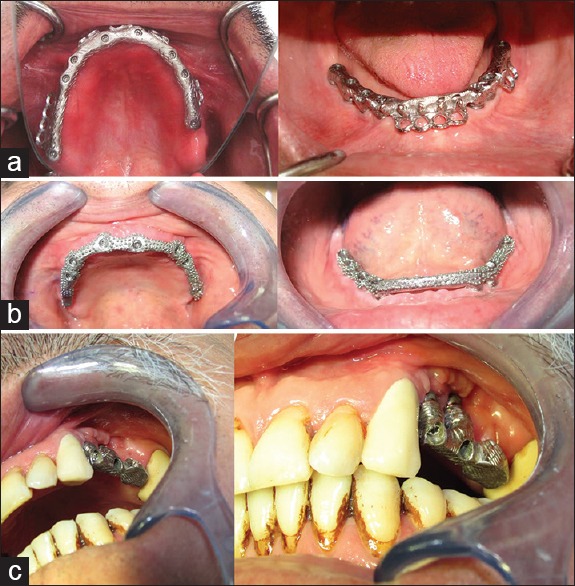
The metal frameworks of the patients those were fabricated and checked intraorally. (a) Patient 1, (b) Patient 2, (c) Patient 3
At delivery, the abutments (RC Multi-Base Abutment, Institut Straumann AG, Basel, Switzerland) were screwed in and torqued according to manufacturer's recommendation. The screw access holes of the mandibular prostheses were sealed with polytetrafluoroethylene strips and then filled with shade A2 composite resin (Clearfil Majesty Esthetic, Kuraray Europe GmbH, Frankfurt, Germany). The occlusion was verified using articulating paper visualization [Figures 5–7].
Figure 5.
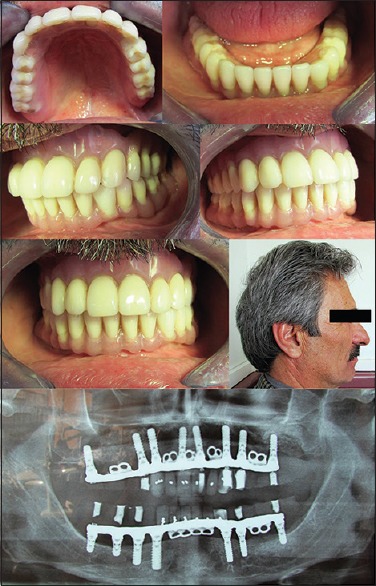
Intraoral view and panoramic radiograph of the final prosthesis of Patient 1
Figure 7.
Intraoral view and panoramic radiograph of the final prosthesis of Patient 3
Figure 6.
Intraoral view and panoramic radiograph of the final prosthesis of Patient 2
Following delivery, instructions on how to use and maintain the prostheses were given to the patients. The use of super floss (Oral-B, Inc, Iowa City, Iowa, USA) and a water jet (Braun Oral-B Oxyjet MD 15, Frankfurt/Main, Germany) to clean underneath the prostheses was demonstrated to the patients. The patients were seen after 24 h and minor adjustments were made.
Follow-up care
Routine clinical assessments were made 1, 2, 6, and 12 months after the delivery of the prostheses and then annually with visual and radiographic examinations. Criteria for success included the following: Stability of the implant (lack of mobility), absence of pain or any subjective sensation at each visit, lack of peri-implant infection with suppuration, and lack of continuous radiolucency around the implants.[11] Also, prosthetic complications and predictability were examined. The minimal bone loss was observed radiographically in all the patients. No implants failed in any patient after prosthetic rehabilitation during the 3-year follow-up period, and all patients remained in continuous function with fixed prostheses. Occlusal access filling material dislodged in Patient 1, but this was rectified by placing undercuts in the openings with an inverted cone bur to mechanically lock the composite resin in place. Another complication in Patient 1 was the replacement of right mandibular canine acrylic resin tooth because of fracture. No other complications were seen in the patients. The patients agreed that their new denture looked nice, their speech was improved, it was easy to perform hygiene around the new prosthesis and their ability to chew had improved. The positive attitude of the patients and their satisfaction with the treatment that addressed their chief complaints and desires contributed to a good prognosis.
DISCUSSION
Accurate and precise planning in dental implantology includes detecting any existing clinical difficulties prior to the treatment and foreseeing the final results before the treatment.[1] Planning for esthetic cases requires different diagnostic perspective; it should include additional factors such as smile patterns and lip size, etc.[1] In addition, the restorative space for the prostheses, which is measured from the platform of the implant to the opposing occlusion, is often overlooked when implant positions are planned.[5] The intra-arch distance which implant components, metal substructure, the acrylic resin, and the denture teeth are placed plays a major role on selecting appropriate restoration. With mandibular implant-supported fixed prostheses, a minimum of 12–15 mm of space has been suggested.[2] When more intra-arch space is present, a hybrid restoration is recommended.[4] In the present case reports, implant supported hybrid prostheses were decided to be fabricated since the intra-arch distance was 32 mm for Patient 1; 30 mm for Patient 2; and 26 mm for Patient 3.
Reconstruction of the atrophic jaws for implant placements is usually staged with implant placement after graft healing.[6] However, sites to be treated with dental implants are frequently affected with either acute or chronic localized infections.[7] Patient 3 reported herein had a history of a previously failed implant due to the graft infection. Clinical observations revealed that there was massive bone destruction on the infected area. Owing to the advantage of replacing soft tissue defects, the acrylic screw-retained hybrid prosthesis was decided to be fabricated in this patient.
Cantilever length is also an important parameter that is to be evaluated when deciding to fabricate implant supported acrylic screw-retained hybrid prosthesis.[8] The researchers suggested a mandibular extension of between 15 and 20 mm to minimize the risk of framework fracture.[8] Other authors recommended a cantilever length of 1.5 or 2 times of the anterior, posterior curve of the implants.[2] Besides, the opposing occlusion and the number and distribution of implants should also be considered, before the determination of cantilever length.[3] In the current clinical report, cantilever lengths were 12 and 10 mm in Patients 2 and 3, respectively which is in line with the suggested values.
The other important factor during the manufacturing of implant-supported hybrid prosthesis is obtaining a passive fit of the framework. Without the passive fit, mechanical or biological complications such as peri-implant bone loss, screws loosening or fracture of abutment or the implant were reported.[2] In the current clinical report, verification index with pattern resin for each prosthesis was fabricated, and they were checked intraorally to confirm the accuracy of the master cast. Moreover, the metal frameworks were checked intraorally to confirm their passively seating over the implants in the presented patients.
No implant failure, peri-implantitis, a soft-tissue complication related to prosthesis design, fracture of prosthesis frameworks, screw fractures or screw loosening or difficulty in oral hygiene were noted in the patients during the follow-up period. However, only in Patient 1, occlusal access filling material dislodged, and one mandibular anterior tooth had to be replaced due to the fracture. It was found that lost fillings in screw-access openings and mobile prostheses were the most common complications associated with the mandibular hybrid prosthesis.[9] In addition, it was reported that, although implant and prosthesis survival rates remained high, the wear and fracture of denture teeth has been a significant problem[9] Moreover, the researchers found that anterior tooth fracture was more common than posterior tooth fracture.[9] In the current report, the loss of filling material from the prosthetic screw access and fracture of the mandibular canine resin tooth occurred only once. These results are in contrast to the high incidence of tooth fracture presented by the previous report.[9] The disparity in these results may be the result of differing reporting methods or the differences in the follow-up periods. Furthermore, this case report represents the treatment of three patients with a follow-up of only 3 years which might be an important limit in the evaluation of these results.
Another important aspect to consider when fabricating implant supported fixed complete prosthesis is the framework material. Frameworks are made using a spectrum of metal alloys ranging from conventional high noble to titanium or base metal alloys.[9] Additionally, zirconia frameworks are proposed to be a promising alternative. However, veneering porcelain fracture and chipping has emerged as a reported complication for the bilayered ceramic restorations.[9] In the current clinical report, base metal alloys were used to fabricate the frameworks of the prostheses. Cost and the possible need to section and solder to attain a passive framework fit were considered for the choice of framework material. Furthermore, relevant studies have argued that a rigid material can minimize the bending moment of the framework thus, they have shown that cobalt-chromium frameworks generate the least amount of strain on the implants as a result of the accuracy of fit of the framework.[10]
The treatment plan in this clinical report was based on the splinting all implants together with the frameworks. This may be evaluated as a suspicious decision particularly in the mandible when considering the reality of mandibular flexion concurrently with jaw movement.[2] However, the significance of mandibular flexure on the success of implant treatment is currently unclear.[10] A recent study demonstrated that mandibular flexure occurred during unilateral loading, and extra strain was transmitted at the bone-implant interface.[10] It was, however, implied that the amount of strain introduced by mandibular flexure alone was not significant enough to stimulate bone modeling or remodeling.[10] In the light of these findings, we speculated that splinting the implants in the mandible would not jeopardize the longevity of implant-supported prostheses. Minimal complications that occurred during our follow-up results seem to support this idea.
Implant supported hybrid prosthesis can provide satisfactory results where esthetic and functional requirements are demanding and challenging as in increased intra-arch space that remains following conventional implant replacements, the dentist needs to plan for an alternative treatment procedure that best suits the situation.[2] The patients’ acceptance of the prosthetic treatment plan and restorative solution were certainly promoted by the fabrication of implant supported hybrid prosthesis.
The other important aspect to consider is the maintenance of prosthetic rehabilitation as well as the implants by supporting the structure.[2] Regular checks are recommended every 6 or 12 months to avoid complications and to assess the status of the peri-implant tissue.[2] Moreover, the measurement of radiographic peri-implant marginal bone loss during the follow-up period is also recommended. Clinical assessments, in line with a previous report,[2] were made 1, 2, 6, and 12 months after the delivery of the prostheses and then annually with visual and radiographic examinations.
CONCLUSIONS
This clinical report has documented the esthetic and functional rehabilitation of three patients with implant supported hybrid prostheses. The main limitation of this case report is to represent the treatment of a small number of patients with a follow-up period of only 3 years which might be an important limit in the evaluation of these results. However, it was concluded that this type of prosthesis can provide satisfactory results in patients of whom dental implants were placed regardless careful treatment planning. The authors also believe that it is essential to evaluate the patient not only with a surgical perspective, but also from a prosthodontic point of view.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.El Askary AE. 2nd ed. Ames, Iowa, USA: Munksgaard, Blackwell; 2007. Fundamentals of Esthetic Implant Dentistry; p. 13. [Google Scholar]
- 2.Misch CE. St. Louis, MO: Mosby Elsevier; 2008. Contemporary Implant Dentistry; p. 99.p. 100. [Google Scholar]
- 3.Thalji G, Bryington M, De Kok IJ, Cooper LF. Prosthodontic management of implant therapy. Dent Clin North Am. 2014;58:207–25. doi: 10.1016/j.cden.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Pjetursson BE, Thoma D, Jung R, Zwahlen M, Zembic A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res. 2012;23(Suppl 6):22–38. doi: 10.1111/j.1600-0501.2012.02546.x. [DOI] [PubMed] [Google Scholar]
- 5.Tourah A, Moshaverinia A, Chee WW. Mandibular implant-supported fixed dental prosthesis with a modified design: A clinical report. J Prosthet Dent. 2014;111:91–5. doi: 10.1016/j.prosdent.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Dym H, Pierse J. Advanced techniques in bone grafting procedures. Dent Clin North Am. 2011;55:453–60. doi: 10.1016/j.cden.2011.02.003. vii. [DOI] [PubMed] [Google Scholar]
- 7.Beagle JR. Surgical Essentials of Immediate Implant Dentistry. Oxford, UK: Wiley-Blackwell; 2013. p. 32. [Google Scholar]
- 8.Sertgöz A, Güvener S. Finite element analysis of the effect of cantilever and implant length on stress distribution in an implant-supported fixed prosthesis. J Prosthet Dent. 1996;76:165–9. doi: 10.1016/s0022-3913(96)90301-7. [DOI] [PubMed] [Google Scholar]
- 9.Priest G, Smith J, Wilson MG. Implant survival and prosthetic complications of mandibular metal-acrylic resin implant complete fixed dental prostheses. J Prosthet Dent. 2014;111:466–75. doi: 10.1016/j.prosdent.2013.07.027. [DOI] [PubMed] [Google Scholar]
- 10.Law C, Bennani V, Lyons K, Swain M. Influence of implant framework and mandibular flexure on the strain distribution on a Kennedy class II mandible restored with a long-span implant fixed restoration: A pilot study. J Prosthet Dent. 2014;112:31–7. doi: 10.1016/j.prosdent.2013.08.012. [DOI] [PubMed] [Google Scholar]
- 11.Demarosi F, Leghissa GC, Sardella A, Lodi G, Carrassi A. Localised maxillary ridge expansion with simultaneous implant placement: A case series. Br J Oral Maxillofac Surg. 2009;47:535–40. doi: 10.1016/j.bjoms.2008.11.012. [DOI] [PubMed] [Google Scholar]


