Abstract
Context and Objective:
Insulin resistance and chronic inflammation are key elements in the pathogenesis of type 2 diabetes. We hypothesized that similar mechanisms could have a role in the development of diabetic retinopathy (DR), an important microvascular complication in Latinos with type 2 diabetes.
Design and Setting:
A cross-sectional, family-based, observational cohort study.
Patients:
Latino subjects with type 2 diabetes (n = 507), ascertained in families via a proband with known diabetes duration of 10 years or more and/or with DR, were included.
Main Outcome Measures:
Serum adiponectin was measured and insulin sensitivity was estimated using homeostasis model assessment of insulin resistance (HOMA-IR). DR was assessed by seven-field digital fundus photography and graded using the modified Airlie House classification and the Early Treatment Diabetic Retinopathy Scale (range of severity levels, 10–85).
Results:
Fasting adiponectin concentrations were elevated in patients with DR compared to those without (12.9 ± 0.5 vs 10.5 ± 0.5 μg/mL; P = .0004) and remained significant after adjusting for multiple covariates (age, gender, body mass index, glycosylated hemoglobin, diabetes duration, statin use, blood pressure, and renal function; P = .013 to .018). Adiponectin was also positively correlated with severity of DR in patients with nonproliferative DR (P < .0003), significant also after all covariate adjustments (P = .018). When the proliferative DR group was included, this relationship was attenuated by adjustments, possibly an influence of estimated glomerular filtration rate reduction in the proliferative DR group. HOMA-IR was not different in the DR and non-DR groups. Although elevated, adiponectin retained a typical inverse relationship with HOMA-IR in DR, similar to that seen in the non-DR group.
Conclusions:
Serum adiponectin is elevated in DR, is positively correlated with DR severity in Latinos with type 2 diabetes, and maintains a relationship to insulin sensitivity. Adiponectin, whether as a marker or biological mediator, may play an important role in DR, which appears to be independent of its relationship to insulin sensitivity.
Diabetic retinopathy (DR), an important microvascular complication of diabetes, is a leading cause of blindness in working-age adults. Latinos are the fastest growing ethnic minority in the United States, and they have a higher risk of developing type 2 diabetes (1) and DR (2) than non-Hispanic whites. This difference is not explained by previously well-established risk factors such as glycemic control and blood pressure (2). Our prior biomarker study demonstrates that levels of both soluble TNF receptors 1 and 2 (TNF-R1 and TNF-R2) are positively correlated with severity of DR, suggesting that inflammation and insulin sensitivity may play a role in the development of DR (3). To further explore these mechanisms in DR, we evaluated circulating adiponectin concentrations in relation to the presence or absence of DR in a large group of Latinos with type 2 diabetes.
Little is known about the relationship between adiponectin and DR. Adiponectin is a protein secreted by adipocytes that regulates insulin sensitivity and may also be involved in the inflammatory process (4). Levels of adiponectin are decreased in obese diabetic mice (5), and replacement of adiponectin improves insulin sensitivity (6). Low levels of circulating adiponectin are found in subjects with obesity, insulin resistance, type 2 diabetes, and cardiovascular diseases (7, 8), and this relationship is also seen in Latinos (9). We therefore sought to study the relationship between adiponectin, insulin sensitivity, and DR in type 2 diabetes.
The purpose of this study was to investigate the relationship of fasting adiponectin in Latinos with type 2 diabetes, with and without DR, and further to examine whether there was a possible relationship with different levels of DR severity.
Subjects and Methods
Ethics
This study was performed in accordance with the tenets of the Declaration of Helsinki and approved by the institutional review boards of each participating center. Informed consent was obtained from each subject.
Study participants
The GOLDR (Genetics of Latino Diabetic Retinopathy) study is a family-based study assessing diabetes and diabetic complications in families (siblings and/or parents) of a proband, defined as having type 2 diabetes and either known DR or a diabetes duration of ≥10 years. Participants are all Latinos recruited and studied at the Los Angeles BioMedical Research Institute (LA Biomed) at Harbor-UCLA Medical Center.
Siblings and parents with unknown diabetes status at the time of the study were offered an oral glucose tolerance test. The diagnosis of diabetes was based on standard criteria from the American Diabetes Association (10). Subjects who were determined to be nondiabetic by oral glucose tolerance test or by fasting plasma glucose <126 mg/dL (<7.0 mmol/L) and glycosylated hemoglobin (HbA1c) <6.5% at the initial study visit and/or those with undetermined DR status from fundus photography were removed from the analysis. In total, there were 507 subjects with type 2 diabetes from 191 families whose data were used in the analyses for this study.
The participants' demographics, pedigree information, medical history, family history, and current medications were collected. Anthropometric measurements (height, weight, waist circumference), vital signs (blood pressure and pulse), and blood and urine samples (fasting serum glucose, HbA1c, serum lipids, serum creatinine, and urinary albumin-to-creatinine ratio) were measured. Body mass index (BMI) was calculated using height and weight. The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease (MDRD) study equation (11).
Biochemical assays
Fasting total adiponectin (EMD Millipore) was measured using commercially available ELISA. The lower limit of sensitivity of this assay is 0.78 μg/mL, and coefficients of variation were: intra-assay, 1–7.4%; and interassay, 2.4–8.4%. Fasting plasma insulin concentration was measured by Dissociation-Enhanced Lanthanide Fluorescent Immunoassay (DELFIA; PerkinElmer Life Sciences). The lower limit of sensitivity of this assay is 1.12 μU/mL. Homeostasis model assessment of insulin resistance (HOMA-IR) was estimated in every participant where an insulin result was available, using the following equation (12): HOMA-IR = (I*G)/22.5, where I is fasting insulin (μU/mL) and G is fasting glucose (mmol/L).
Eye phenotypes
All participants received dilated ophthalmic eye examinations with seven standard 30° fields using digital stereoscopic color fundus photography at LA Biomed. Retinal images were evaluated by two independent masked photograders at the Ocular Epidemiology Reading Center at the University of Wisconsin, Madison, using the modified Airlie House classification scheme and the Early Treatment Diabetic Retinopathy Study (ETDRS) severity scale (13).
Analyses
DR status
Subjects were first grouped as diabetes without retinopathy vs diabetes with retinopathy. Levels of fasting adiponectin were compared between these two groups using the Student's t test, adjusting for family relationships. Analysis of HOMA-IR was conducted in subjects without exogenous insulin usage (n = 356).
DR severity
We examined the association of adiponectin to severity of DR using the retinopathy severity score from the ETDRS scale in both categorical and quantitative analyses. In the categorical analysis, subjects were grouped into five categories of increasing DR severity as follows: no DR (levels 10–13), mild nonproliferative DR (NPDR) (levels 14–20), moderate NPDR (levels 31–43), severe NPDR (levels 47–53), and proliferative DR (PDR) (levels 60–85), as previously described (13). In the quantitative analysis, the retinopathy score from the ETDRS severity scale was utilized. The eye with the more severe retinopathy score was used for assigning the retinopathy level for each participant.
Analyses
Statistical analyses were performed using SAS 9.1 (SAS Institute Inc). A log or squared-root transformation was applied to normalize the quantitative traits of interest, and then a normal distribution was assumed in the analysis. The generalized estimating equation methods as implemented in the GENMOD procedure of SAS were used to determine the relationship of adiponectin to severity of DR. This approach uses “family” as a unit of clustering factor to account for the dependency of familial relationship that may bias the outcome of a study. A correlation matrix based on family relationship is then estimated for participants in this study, assuming that members from the same family are correlated and members from a different family are independent. A detailed explanation of this approach is described elsewhere (14). Logistic regression with multilevel link function (multinomial distribution) was used for categorical data.
To determine whether the association was independent of known DR risk factors, different models were used to analyze the relationship of adiponectin to severity of DR, adjusting for potential covariates. For example, in model 1, the association was analyzed without any covariate adjustments except for family structure. In model 2, the significance of this trend was analyzed adjusting for family structure, age, gender, and BMI. In model 3, the significance of this trend was analyzed adjusting for family structure, age, gender, BMI, HbA1c, diabetes duration, statin use, and systolic blood pressure. And finally, in model 4, the significance of this trend was analyzed adjusting for family structure, age, gender, BMI, HbA1c, diabetes duration, statin use, systolic blood pressure, and one of three parameters for renal function: serum creatinine, urinary albumin-to-creatinine ratio, or eGFR.
All statistical analyses were performed with GENMOD in SAS, adjusting for family relationship. A P < .05 was considered statistically significant. Data are presented as mean ± SEM or median (interquartile range [IQR]).
Results
Adiponectin and DR
A total of 507 subjects were included in this study, and the demographics are summarized in Table 1. As expected, cases, defined as diabetes with retinopathy (n = 290), exhibited a higher level of HbA1c (P < .0001), a longer diabetes duration (P < .0001), a higher percentage of subjects using exogenous insulin injections (P < .0001), a higher systolic blood pressure (P = .0008), and a worse renal function (P = .0002, P < .0001, and P = .0168 for serum creatinine, urinary albumin-to-creatinine ratio, and eGFR, respectively), compared to the controls, defined as diabetes without retinopathy (n = 217). Patients with DR had higher serum adiponectin (12.9 ± 0.5 vs 10.5 ± 0.5 μg/mL; P = .0004) (Table 1). This difference remained significant after adjustment for covariates including age, gender, BMI (model 2, P = 3 × 10−5), and duration of diabetes, HbA1c, statin use, and systolic blood pressure (model 3, P = .0054). On further adjusting for parameters of renal function, the association of adiponectin concentrations and DR severity remained significant (model 4). We adjusted individually for each of the following: 1) serum creatinine (P = .013); 2) urinary albumin-to-creatinine ratio (P = .018); or 3) eGFR (P = .013) (Table 2). Serum total cholesterol, triglyceride, high-density lipoprotein, and low-density lipoprotein were similar between the two groups (data previously published in Ref. 3).
Table 1.
Demographics and Laboratory Results of Cohort
| Controls (Diabetes + No Retinopathy) | Cases (Diabetes + Retinopathy) | P Value | |
|---|---|---|---|
| n | 217 | 290 | |
| Demographics | |||
| Age, y | 54.1 ± 0.7 | 53.3 ± 0.6 | NS |
| Gender, % male | 30.9 | 41.7 | .01 |
| BMI, kg/m2 | 33.4 ± 0.5 | 32.2 ± 0.4 | NS |
| HbA1c, % | 7.8 ± 0.1 | 9.0 ± 0.1 | <.0001 |
| DM duration, y | 7.2 ± 0.5 | 13.7 ± 0.4 | <.0001 |
| Exogenous insulin usage, % | 15.7 | 40.3 | <.0001 |
| Blood pressure | |||
| SBP, mm Hg | 127 ± 1.2 | 133 ± 1.1 | .0008 |
| DBP, mm Hg | 70 ± 0.7 | 71 ± 0.6 | NS |
| Renal function | |||
| Serum creatinine, mg/dL | 0.77 ± 0.07 | 1.1 ± 0.06 | .0002 |
| Urinary albumin/creatinine ratio | 34 ± 87 | 521 ± 76 | <.0001 |
| MDRD eGFR, mL/min per 1.73 m2 | 98.0 ± 1.7 | 91.0 ± 2.2 | .0168 |
| Metabolic markers | |||
| Adiponectin, μg/mL | 10.5 ± 0.5 | 12.9 ± 0.5 | .0004 |
| HOMA-IRa | 4.5 ± 0.2 | 4.4 ± 0.3 | NS |
Abbreviations: DBP, diastolic blood pressure; DM, diabetes mellitus; MDRD, Modification of Diet in Renal Disease Study equation; NS, not significant; SBP, systolic blood pressure. Values are expressed as mean ± SEM. P value is adjusted for family structure.
HOMA-IR was calculated only in participants who were not receiving insulin (n = 356; of these, non-DR = 183 and DR = 173).
Table 2.
Comparison of Adiponectin Concentrations in Controls (Non-DR) and Cases (DR) With Different Models of Covariate Adjustments
| Controls (n = 217) |
Cases (n = 290) |
P Value | Model | Covariates | |||
|---|---|---|---|---|---|---|---|
| Meana | SEM | Mean | SEM | ||||
| Adiponectin, μg/mL | 10.29 | 0.78 | 12.97 | 1.04 | .00003 | 2 | Family structure, age, gender, BMI |
| 10.30 | 0.79 | 12.95 | 1.00 | .0054 | 3 | Family structure, age, gender, BMI, HbA1c, DM duration, statin use, SBP | |
| 10.31 | 0.75 | 12.94 | 0.95 | .0134 | 4 | Model 3 plus Cr | |
| 10.11 | 0.71 | 12.82 | 1.00 | .0184 | 4 | Model 3 plus ACR | |
| 10.31 | 0.78 | 12.94 | 0.97 | .0132 | 4 | Model 3 plus eGFR | |
Abbreviations: DM, Diabetes Mellitus; SBP, Systolic Blood Pressure; Cr, creatinine; ACR, albumin to creatinine ratio. Models and significance, adjusting for: 1 = family structure; 2 = family structure, age, gender, BMI; 3 = family structure, age, gender, BMI, diabetes duration, statin use, systolic blood pressure, and HbA1c; and 4 = family structure, age, gender, BMI, diabetes duration, statin use, systolic blood pressure, HbA1c, and creatinine or albumin-to-creatinine ratio, or eGFR, respectively.
Mean adiponectin concentrations, adjusted for covariates, in the different models.
Adiponectin and severity of DR
To delineate the relationship of adiponectin with severity of DR, we first examined our data by DR phenotype, with severity defined categorically. Of the 290 cases with DR, 85 subjects (30%) had mild NPDR, 114 (39%) had moderate NPDR, 23 (8%) had severe NPDR, and 68 (23%) had PDR. Categorical analysis showed a linear relationship between serum adiponectin level and increasing severity of DR (median [IQR]) as follows: 9.2 [7.1–12], 8.9 [6.8–12.7], 10.4 [7.9–14.3], 12.2 [7.4–19.8], and 12.1 [8.3–19.7] μg/mL for no DR, mild NPDR, moderate NPDR, severe NPDR, and PDR, respectively (P = 3.4 × 10−6, adjusting for family structure; Table 3).
Table 3.
Adiponectin Concentrations and Renal Function by Severity of DR
| No DR | Mild NPDR | Moderate NPDR | Severe NPDR | PDR | |
|---|---|---|---|---|---|
| n | 217 | 85 | 114 | 23 | 68 |
| Adiponectin, μg/mL | 9.2 (7.1–12.0) | 8.9 (6.8–12.7) | 10.4 (7.9–14.3) | 12.2 (7.4–19.8) | 12.1 (8.3–19.7) |
| eGFR, mL/min/1.73 m2 | 98.3 (82.1–109.8) | 101.3 (84.5–121.0) | 97.6 (80.1–119.0) | 100.3 (72.2–112.9) | 67.7 (24.8–93.3) |
Data are expressed as median (IQR) of adiponectin and eGFR by severity of DR.
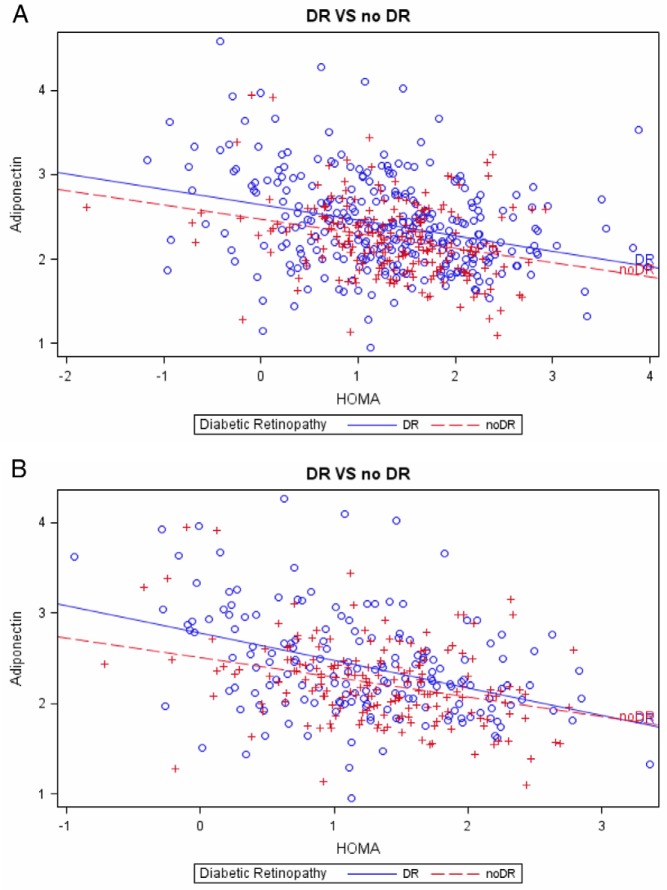
To determine whether the identified association was independent of other risk factors, we then analyzed the data, adjusting for potential covariates. The relationship of DR severity with adiponectin remained significant even after additionally adjusting for age, gender, BMI (model 2, P = 2.5 × 10−7), and duration of diabetes, HbA1c, statin use, and systolic blood pressure (model 3, P = .004). On further adjusting for parameters of renal function, the association of adiponectin concentrations and DR severity remained only borderline significant (model 4). We adjusted for each of the following: 1) serum creatinine (P = .089); 2) urinary albumin-to-creatinine ratio (P = .048); or 3) eGFR (P = .069) (Table 4 and Figure 1A).
Table 4.
Statistical Analysis of Adiponectin by DR Severity in NPDR, or in All DR, With Different Models of Covariate Adjustments
|
P Value of Different Models |
||||||||
|---|---|---|---|---|---|---|---|---|
| NPDR |
All DR |
|||||||
| 1 | 2 | 3 | 4a | 1 | 2 | 3 | 4a | |
| Categorical | 8.65E-04 | 5.69E-05 | .004 | .018 | 3.37E-06 | 2.50E-07 | .004 | .089 |
| .011 | .048 | |||||||
| .009 | .069 | |||||||
| Quantitative | 2.21E-03 | 1.07E-04 | .009 | .048 | 1.01E-05 | 3.55E-07 | .004 | .068 |
| .036 | .070 | |||||||
| .019 | .069 | |||||||
All DR includes both NPDR and PDR. Models and significance, adjusting for: 1 = family structure; 2 = family structure, age, gender, BMI; 3 = family structure, age, gender, BMI, diabetes duration, HbA1c, statin usage, and systolic blood pressure;
4 = model 3 plus 1 of 3 different measures of renal function (creatinine or albumin-to-creatinine ratio or eGFR, respectively).
Figure 1.
Graphs of adiponectin with severity of DR, analyzed categorically (A) and quantitatively (B). Reported P values are analyses conducted in model 3 (*) (defined as adjusting for family relationship, age, gender, BMI, diabetes duration, statin use, systolic blood pressure, and HbA1c) and model 4 (†) (defined as adjustment with model 3 plus one of three different measures of renal function).
We also analyzed the data quantitatively using the ETDRS scale. Quantitative analysis of the relationship between DR severity and adiponectin concentrations also demonstrated a borderline significant relationship with severity of DR after adjusting for family structure, age, gender, BMI, HbA1c, diabetes duration, statin use, systolic blood pressure, and renal function parameters (model 4, P = .068, P = .070, and P = .069, adjusting for creatinine, urinary albumin-to-creatinine ratio, and eGFR, respectively; Table 4 and Figure 1B).
Adiponectin, severity of DR, and renal function
To better understand the role of kidney function in the relationship between DR and adiponectin, we evaluated the non-PDR groups, where eGFR was unchanged with increasing severity of DR, 98.3–100.3 mL/min per 1.73 m2 (Table 3). Despite the similarity in eGFR across the different NPDR groups, adiponectin progressively and significantly increased (P = 8.7 × 10−7) and remained significant also after adjustment for the same cofactors used in the previous analyses (P = .009 to .018 for categorical analysis, and P = .019 to .048 for quantitative analysis) (Table 4).
Relationship of insulin sensitivity to DR and adiponectin
The finding of an increase in adiponectin concentrations in patients with DR raises the possibility that regulation of adiponectin is abnormal in this group. To address this possibility, we evaluated the relationship between DR and insulin sensitivity; mean HOMA-IR in DR (4.4 ± 0.3) was not statistically different from non-DR patients (4.5 ± 0.2) (n = 356; Table 1). Also, adiponectin concentrations were elevated in this noninsulin-treated subset (10.29 ± 0.8 vs 13.57 ± 0.5 μg/mL in non-DR and DR, respectively; P = .0004), which was similar to the findings in the entire cohort. Thus, elevated adiponectin in DR patients is not explained by a difference in insulin sensitivity between the two groups. Increased adiponectin appears to be independent of the degree of insulin sensitivity.
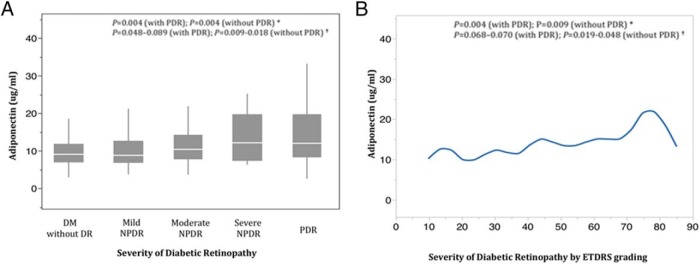
We then examined the relationship between adiponectin and insulin sensitivity to determine whether abnormal regulation might account for the higher adiponectin concentrations in the DR group. This was also not found to be the explanation. In both DR and non-DR groups, there was a statistically significant, and apparently intact, negative correlation between fasting serum adiponectin and insulin resistance, measured as HOMA-IR (DR, r = −0.40, P < .0001; non-DR, r = −0.31, P < .0001) (Figure 2). The intercepts were significantly different (P = .038), although the slopes of the regressions were not.
Figure 2.
Scatter plots of the relationship between lnAdiponectin and lnHOMA-IR in participants with DR (○—○; solid line) and without DR (+—+; dotted line), conducted in all patients (n = 507) (A) and in a subset of patients not using exogenous insulin (n = 356) (B). Slopes of the regressions in each panel are similar. Intercepts are different in panels A and B.
Discussion
This study provides evidence that in Latinos with type 2 diabetes, serum adiponectin concentrations are significantly elevated in patients with DR compared to those without DR, and furthermore, are cross-sectionally associated with DR severity. This relationship remains significant after controlling for previously known confounding risk factors for DR, including age, gender, BMI, glycemic control, diabetes duration, statin use, systolic blood pressure, and renal function. These results are consistent with our prior finding that inflammation may have an important role in the development and progression of DR (3). In that earlier study, elevated soluble TNF-R1 and TNF-R2 in DR were found, suggesting that insulin resistance, which is closely associated with inflammation in type 2 diabetes, may be integral to DR and its severity (3).
The mechanism for the increase in serum adiponectin is not clear. Typical influences on adiponectin concentrations do not explain elevated levels in the DR group. Thus, elevated adiponectin observed in DR was independent of gender, which was adjusted for in the regression analysis. Also, adiponectin was elevated despite a greater percentage of males in the DR group, which would typically be associated with lower adiponectin levels. Alteration in insulin sensitivity also does not explain elevated adiponectin because mean HOMA-IR is similar in each group. Furthermore, the relationship of insulin sensitivity and adiponectin is intact, reflected by our data that higher levels of HOMA are associated with lower levels of adiponectin. This relationship was similar whether or not the patients had DR.
Elevated adiponectin has been described in other diabetic settings (15–19). Adiponectin concentrations are higher in patients with type 1 diabetes (15). DR in type 1 diabetes is also associated with elevated adiponectin when compared with non-DR patients (16). Increasing adiponectin levels were observed with larger excretion of albuminuria (17). In a study of Japanese type 2 diabetes patients, Kato et al (18) found that adiponectin was elevated in patients with PDR. Moreover, adiponectin concentrations are increased in the aqueous humor and plasma of PDR subjects (19). DR and diabetic nephropathy are closely associated, but the elevated adiponectin seen in DR is likely independent of alterations in kidney function. Elevation of adiponectin in persons with DR in this study remained significant after adjustment for renal function covariates, reflecting the findings that adiponectin clearance is predominantly hepatic (20). Adiponectin was also positively correlated with severity of DR in patients with NPDR, significant also after all covariate adjustments. When the PDR group was included, this relationship was attenuated by adjustments, possibly an influence of the severe eGFR reduction in the PDR group.
An explanation for the paradoxical finding of elevated adiponectin in DR is that adiponectin may have a dual role, both proinflammatory and anti-inflammatory (21). Several reports demonstrated a negative correlation of adiponectin and markers of inflammation for conditions such as type 2 diabetes, obesity, metabolic syndrome, and cardiovascular diseases, where adiponectin levels are usually low (22). In these conditions, adiponectin can exert a number of anti-inflammatory activities, including inhibition of proinflammatory cytokines (TNF-α, IL-6), prevention of vascular cell adhesion molecule 1 (VCAM-1) expression, induction of anti-inflammatory cytokines (IL-10), and endothelial cell protection (4, 22, 23). On the other hand, adiponectin is positively correlated with markers of inflammation in classic chronic inflammatory and autoimmune diseases (21) and type 1 diabetes (16). In addition, adiponectin has been shown to be angiogenic (24). It is unclear whether this plays any role at all in the angiogenesis associated with PDR. Thus, adiponectin exerts differential functions, and its effect in DR, a complication of both type 1 and type 2 diabetes, remains unclear.
An alternate explanation for the increased concentration of adiponectin in DR is a possible role in tissue injury and repair. A number of studies have shown that adiponectin is up-regulated in damaged tissues. For example, adiponectin mRNA is detected in the liver of a mouse model of hepatic injury (25) and is up-regulated in skeletal muscle cells with oxidative stress in a type 2 diabetes mouse model (26). Adiponectin has been shown to regulate myocardial remodeling after acute injuries and has cardioprotective mechanisms (27), and it may act in a protective role in states of injury. Finally, and importantly for any putative direct role in retinal physiology or disease, adiponectin receptors were recently demonstrated in the human and mouse retina (28).
If increased adiponectin is a physiological rather than pathological response to injury, one might expect that physiological regulation may be retained. Therefore, our finding of an intact adiponectin/insulin-sensitivity relationship is a potentially important corollary if the elevated levels of adiponectin represent a physiological response in DR. Another example of a residual normal relationship between adiponectin and insulin sensitivity in the face of hyperadiponectinemia is type 1 diabetes (15). It was suggested that the adiponectin/insulin sensitivity relationship may be set at a different level, with higher adiponectin concentrations for a given level of insulin sensitivity (15). An altered set-point, or adiponectin resistance, could also apply to our cohort of Latinos with type 2 diabetes, where we demonstrate higher levels of adiponectin in DR for any given level of insulin sensitivity, yet with similar relationships between adiponectin and insulin sensitivity in DR and non-DR groups.
The strengths of the present study include a large cohort of Latinos with type 2 diabetes with well-characterized phenotypes and a standardized DR grading system using the modified Airlie House classification and the ETDRS scale. A few limitations should be addressed. First, the cross-sectional nature of the study design cannot indicate a causal relationship between adiponectin and DR. Second, using the generalized estimating equation methods needed to adjust for family relationship is a less powerful approach compared to a standard case-control analysis. Third, HOMA-IR is a useful surrogate for more sophisticated measures of insulin sensitivity and is appropriate for large studies of this sort, but it is not as good a model as the “gold standard” euglycemic clamp method. Type 2 diabetes and its treatment may also influence insulin and glucose concentrations used to calculate HOMA-IR. However, our finding of an intact relationship between adiponectin and HOMA-IR provides a measure of validity for using this estimate for insulin sensitivity in this cohort.
In summary, we found that serum adiponectin concentrations are elevated in DR of Latinos with type 2 diabetes and are significantly associated with DR severity after adjusting for potential covariates. This elevation of adiponectin in DR patients occurs despite a similar degree of insulin resistance in the non-DR group, and while retaining an intact relationship to insulin sensitivity in both groups. Although adiponectin is a useful marker for insulin resistance, it also exerts pleiotropic effects. In DR, it is possible that adiponectin is a marker for retinal injury, that it mediates angiogenesis, or that elevated adiponectin may represent a state of adiponectin resistance with an altered set-point in relation to insulin sensitivity. These findings should be examined further in mechanistic studies.
Acknowledgments
Current affiliation for J.Z.K: Ambry Genetics, Aliso Viejo, CA 92656.
This study was supported by the National Institutes of Health, the National Eye Institute, the National Institute of Diabetes and Digestive and Kidney Disease, Diabetes Research Center Grant P30 DK063491 (to the Southern California Diabetes Endocrinology Research Center), and the National Center for Advancing Translational Sciences (CTSI Grant UL1TR000124).
Author Contributions: All authors made substantial contributions to the concept and design of this study, acquisition of data or analysis, interpretation of data, and to drafting the article and revising it critically for intellectual content. All authors gave final approval of the version to be published.
Disclosure Summary: The authors have nothing to declare.
Footnotes
- BMI
- body mass index
- DR
- diabetic retinopathy
- eGFR
- estimated glomerular filtration rate
- HbA1c
- glycosylated hemoglobin
- HOMA-IR
- homeostasis model assessment of insulin resistance
- IQR
- interquartile range
- NPDR
- nonproliferative DR
- PDR
- proliferative DR
- TNF-R
- TNF receptor.
References
- 1. Cusi K, Ocampo GL. Unmet needs in Hispanic/Latino patients with type 2 diabetes mellitus. Am J Med. 2011;124:S2–S9. [DOI] [PubMed] [Google Scholar]
- 2. Harris MI, Klein R, Cowie CC, Rowland M, Byrd-Holt DD. Is the risk of diabetic retinopathy greater in non-Hispanic blacks and Mexican Americans than in non-Hispanic whites with type 2 diabetes? A U.S. population study. Diabetes Care. 1998;21:1230–1235. [DOI] [PubMed] [Google Scholar]
- 3. Kuo JZ, Guo X, Klein R, et al. Systemic soluble tumor necrosis factor receptors 1 and 2 are associated with severity of diabetic retinopathy in Hispanics. Ophthalmology. 2012;119:1041–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ye R, Scherer PE. Adiponectin, driver or passenger on the road to insulin sensitivity? Mol Metab. 2013;2:133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Maeda N, Shimomura I, Kishida K, et al. Diet-induced insulin resistance in mice lacking adiponectin/ACRP30. Nat Med. 2002;8:731–737. [DOI] [PubMed] [Google Scholar]
- 6. Yamauchi T, Kamon J, Waki H, et al. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med. 2001;7:941–946. [DOI] [PubMed] [Google Scholar]
- 7. Lindsay RS, Funahashi T, Hanson RL, et al. Adiponectin and development of type 2 diabetes in the Pima Indian population. Lancet. 2002;360:57–58. [DOI] [PubMed] [Google Scholar]
- 8. Kumada M, Kihara S, Sumitsuji S, et al. Association of hypoadiponectinemia with coronary artery disease in men. Arterioscler Thromb Vasc Biol. 2003;23:85–89. [DOI] [PubMed] [Google Scholar]
- 9. Hanley AJ, Wagenknecht LE, Norris JM, et al. Adiponectin and the incidence of type 2 diabetes in Hispanics and African Americans: the IRAS Family Study. Diabetes Care. 2011;34:2231–2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. American Diabetes Association. Standards of medical care in diabetes–2014. Diabetes Care. 2014;37(suppl 1):S14–S80. [DOI] [PubMed] [Google Scholar]
- 11. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. [DOI] [PubMed] [Google Scholar]
- 12. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. [DOI] [PubMed] [Google Scholar]
- 13. Grading diabetic retinopathy from stereoscopic color fundus photographs–an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98(5 suppl):786–806. [PubMed] [Google Scholar]
- 14. SAS/STAT 9.1 User's Guide. Cary, NC: SAS Institute Inc; 2004. [Google Scholar]
- 15. Pereira RI, Snell-Bergeon JK, Erickson C, et al. Adiponectin dysregulation and insulin resistance in type 1 diabetes. J Clin Endocrinol Metab. 2012;97:E642–E647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hadjadj S, Aubert R, Fumeron F, et al. Increased plasma adiponectin concentrations are associated with microangiopathy in type 1 diabetic subjects. Diabetologia. 2005;48:1088–1092. [DOI] [PubMed] [Google Scholar]
- 17. Looker HC, Krakoff J, Funahashi T, et al. Adiponectin concentrations are influenced by renal function and diabetes duration in Pima Indians with type 2 diabetes. J Clin Endocrinol Metab. 2004;89:4010–4017. [DOI] [PubMed] [Google Scholar]
- 18. Kato K, Osawa H, Ochi M, et al. Serum total and high molecular weight adiponectin levels are correlated with the severity of diabetic retinopathy and nephropathy. Clin Endocrinol (Oxf). 2008;68:442–449. [DOI] [PubMed] [Google Scholar]
- 19. Mao D, Peng H, Li Q, et al. Aqueous humor and plasma adiponectin levels in proliferative diabetic retinopathy patients. Curr Eye Res. 2012;37:803–808. [DOI] [PubMed] [Google Scholar]
- 20. Halberg N, Schraw TD, Wang ZV, et al. Systemic fate of the adipocyte-derived factor adiponectin. Diabetes. 2009;58:1961–1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fantuzzi G. Adiponectin and inflammation: consensus and controversy. J Allergy Clin Immunol. 2008;121:326–330. [DOI] [PubMed] [Google Scholar]
- 22. Ouchi N, Shibata R, Walsh K. Cardioprotection by adiponectin. Trends Cardiovasc Med. 2006;16:141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lara-Castro C, Fu Y, Chung BH, Garvey WT. Adiponectin and the metabolic syndrome: mechanisms mediating risk for metabolic and cardiovascular disease. Curr Opin Lipidol. 2007;18:263–270. [DOI] [PubMed] [Google Scholar]
- 24. Shibata R, Ouchi N, Kihara S, Sato K, Funahashi T, Walsh K. Adiponectin stimulates angiogenesis in response to tissue ischemia through stimulation of AMP-activated protein kinase signaling. J Biol Chem. 2004;279:28670–28674. [DOI] [PubMed] [Google Scholar]
- 25. Yoda-Murakami M, Taniguchi M, Takahashi K, et al. Change in expression of GBP28/adiponectin in carbon tetrachloride-administrated mouse liver. Biochem Biophys Res Commun. 2001;285:372–377. [DOI] [PubMed] [Google Scholar]
- 26. Delaigle AM, Senou M, Guiot Y, Many MC, Brichard SM. Induction of adiponectin in skeletal muscle of type 2 diabetic mice: in vivo and in vitro studies. Diabetologia. 2006;49:1311–1323. [DOI] [PubMed] [Google Scholar]
- 27. Ouchi N, Walsh K. Adiponectin as an anti-inflammatory factor. Clin Chim Acta. 2007;380:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lin T, Qiu Y, Liu Y, Mohan R, Li Q, Lei B. Expression of adiponectin and its receptors in type 1 diabetes mellitus in human and mouse retinas. Mol Vis. 2013;19:1769–1778. [PMC free article] [PubMed] [Google Scholar]