Abstract
Background
An ethnobotanical survey was conducted on the Caribbean island of Trinidad to identify medicinal plants commonly used in traditional medicine to treat a variety of medical conditions.
Methods
A pilot survey was conducted to identify the top ten most common ailments where medicinal plants were used. The results of the foregoing study guided a wider national survey conducted between October 2007 and July 2008. A total of 450 households from 50 rural communities were interviewed using the TRAMIL (Traditional Medicine in the Islands) questionnaire for data collection. Details of plants, part(s) used, and remedy formulations were elicited from informants and voucher specimens collected for identification at the National Herbarium of Trinidad and Tobago. The TRAMIL methodology set a limit of a plant with 20 % or more citations for any particular ailment as having significant or popular use.
Results
At the end of the survey 917 single plant remedies were identified. The majority of species were from the following families; Asteraceae, Lamiaceae, Leguminosae, Verbenaceae and Poaceae. Applying the TRAMIL 20 % citation of a plant for popular use as significant, Leonotis nepetifolia (for cough/common cold), Gomphrena globosa (for “stoppage-of-water”), Curcuma longa and Senna occidentalis (for “afterbirth”), Cymbopogon citratus and Neurolaena lobata (for fever), and Citrus limon (for kidney stones) qualified in our study. Those not reaching the TRAMIL 20 % significant (popular) use were Stachytarpheta jamaicensis (L.) Vahl, Senna alata (L.) Roxb.and Momordica charantia L. which were widely used as “‘cooling/cleanser’” in our survey.
Conclusions
Our survey showed significant retention of traditional knowledge of medicinal plants in rural Trinidad. More interestingly, a large remnant of medico-cultural concepts such as “cooling/cleanser”, “afterbirth”, “stoppage-of-water” and “womb infection” persist in the rural population. Although the scientific literature show that some of the cited plants possessed antimicrobial, anti-inflammatory and related pharmacological activities in laboratory studies, these results must be taken with caution until clinical trials are conducted to establish safety and efficacy.
Keywords: ‘Cooling/cleanser’, ‘Stoppage of water’, ‘Afterbirth’, ‘Womb infection’, Kidney stones, Leonotis nepetifolia, Gomphrena globosa, Senna occidentalis, Cymbopogon citratus
Background
The island of Trinidad which lies approximately 13 km off the coast of the Paria Peninsula of Venezuela is the larger of the twin-island state of the Republic of Trinidad and Tobago. The island has a population of approximately 1.3 million people with about 77 % being either of African or Asian Indian ancestry or an admixture of these major ethnic groups [1]. Unlike other Caribbean islands, Trinidad is a continental island sharing its geology, flora and fauna, with South America having recently separated from the mainland ca. 10,000 years ago [2]. This gives Trinidad a unique mix of Antillean and South American elements in its flora and fauna. However, the natural vegetation has been significantly transformed in the post-Columbian era with the arrival of the Europeans, West Africans and the East Indians [3]. Today, approximately one-third of the flora is made up of exotic species which are fully incooperated into the modern herbal medicine repertoire, for example, ginger (Zingiber officinale Roscoe) (Baksh-Comeau YS, Maharaj SS, Harris SA, Filer DL, Hawthorne WD: An annotated checklist to the vascular plants of Trinidad and Tobago, unpublished).
The Caribbean region has a long history of using herbal medicine for disease management and maintenance of health. The native Amerindians incorporated indigenous ]species of medicinal plants in their rituals as part of their healthcare system. These First Nation people were gradually replaced by the sequential arrivals of European settlers, enslaved Africans, indentured Asian Indians and other minority ethnic groups. By and large the peoples who came to the region brought with them inherent knowledge of the use of medicinal plants, substituting with the local flora, which over time has led to the development of herbal pharmacopeias in the region [4–6]. There has been a significant loss of this folkloric knowledge, which depended on the oral tradition, for its transmission to successive generations. The main causes of this loss were due to migration, urbanization, modernization and the acceptance of western medicine strongly rooted over the last century. Therefore it is imperative that a concerted effort be made to document and preserve this residual knowledge [7].
Earlier ethnobotanical surveys in Trinidad were mostly qualitative in nature, and restricted in scope with regard to health conditions and localities. One of the first published works on the island described an ethnobotanical survey conducted by Wong [6] over 40 years ago in Blanchisseuse, a small remote village, in north Trinidad. This was followed by a more extensive survey of medicinal plants undertaken between 1979 and 1980 conducted by Seaforth and colleagues across 18 localities on the island. The findings of this survey resulted in the publication of A guide to the medicinal plants of Trinidad & Tobago by the Commonwealth Secretariat [8]. Over the last decade, a survey by Lans used a small sample size of 30 persons across 13 sites [9]. During that period, and a group led by Clement [10–12] focused on complementary use of herbal remedies in a few hundred patients attending over 20 modern primary public healthcare facilities spread across the island, who were being managed with the chronic diseases namely, hypertension, diabetes mellitus and asthma.
Overall, the global trend indicates that knowledge of traditional folkloric medicine is fast disappearing, especially in the urban communities. Similarly, in Trinidad which is relatively industrialized most of the population reside in urban communities and have access to modern healthcare and medicines. We therefore assumed that people living in rural agricultural communities, with restricted access to transportation and healthcare facilities, would retain more traditional knowledge and more likely to use herbal remedies rather than those in urban areas. This assumption is supported by other studies [13-15], and hence the rationale for focusing our survey in these communities.
The objectives of our survey were to; i) determine the most common ailments treated with herbal remedies, ii) identify the plants used to treat these common ailments, plant part(s) used, and their mode of preparation, iii) determine which of these plants met the 20 % criteria for popular (significant) use according to TRAMIL criterion and iv) assess the literature regarding the pharmacological evidence that could support the traditional use of these popular (significant) plants.
Materials and methods
An ethnobotanical survey was conducted in 450 households across 50 randomly selected rural communities on the island of Trinidad between October 2007 and July 2008 (Fig. 1). We used the TRAMIL (Traditional Medicine in the Islands) questionnaire to collect data regarding medicinal plant use Appendix 1. (See http://www.tramil.net/english/TramilModelo.html).
Fig. 1.
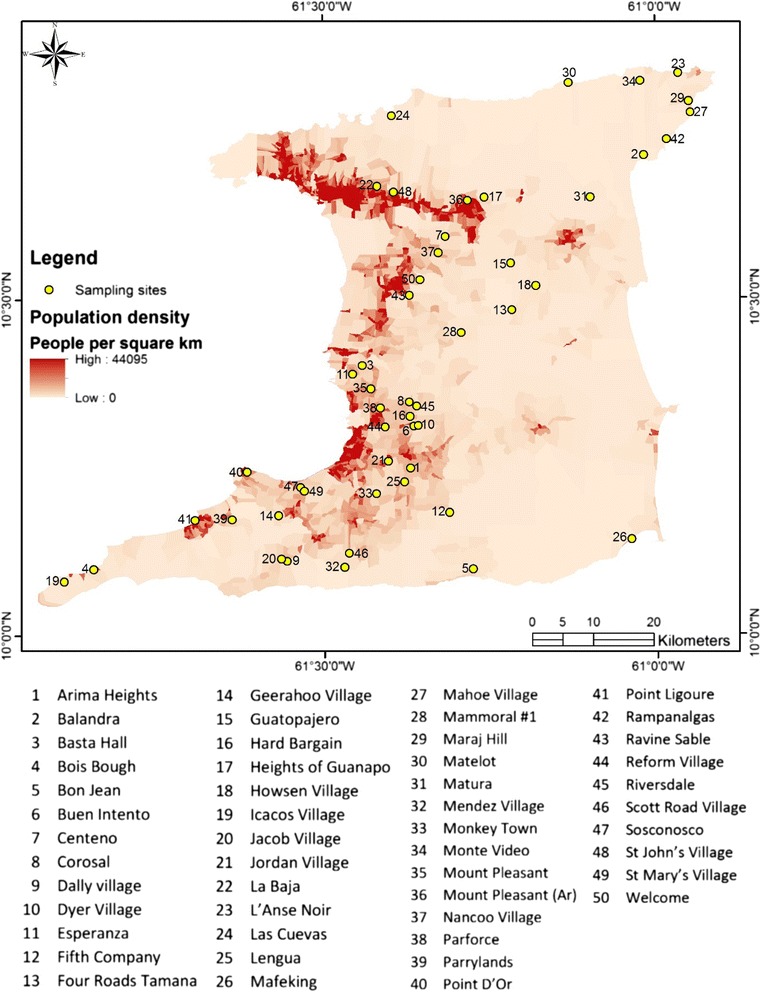
Map showing localities where ethnobotanical survey was conducted in Trinidad
TRAMIL is a non-governmental network established in the Caribbean Basin since 1982 whose goals include the documentation of Caribbean folkloric knowledge of herbal medicine for the preservation of such ‘home remedy’ knowledge [16]. The network is administrated from Santo Domingo in the Dominican Republic.
Survey instrument
The structured TRAMIL questionnaire required participants to provide information about the herbal remedies used as first treatment for the most common ailments. This instrument was used as the primary data collection tool in face-to-face interviews with respondents, following their verbal consent. The questionnaire is very simple in design and respondents were asked to describe the complaint, the plant(s) used, the preparation description, precautions and contraindications in children. The questionnaire, however, does not collect demographic details, such as sex, age, income, etc. TRAMIL defines a remedy with significant (popular) use as the combination of plant species, plant part and form of preparation that is identified by 20 % or more of the study population as a primary treatment resource for a given ailment.
Pilot study
The pilot survey was undertaken to validate the use of the TRAMIL survey instrument in the island to determine the top ten aliments most commonly treated with ‘herbal remedies’.
Using data provided by the Central Statistical Office [1] and the Elections and Boundaries Commission [17] in Trinidad and Tobago regarding the population distribution, and the locations of healthcare facilities (provided by the Ministry of Health), we identified over 200 communities that satisfied the inclusion criteria for selection as a rural community. The criteria were
(1) having a population of less than 1500 inhabitants and (2) limited access to amenities, particularly healthcare services. The name of each community was written on equally sized pieces of paper, folded uniformly, placed in a pot and the five communities were randomly selected for the pilot study. For each community ten randomly selected households were interviewed. From each household the individual with the most knowledge about herbal medicine was interviewed. The top ten ailments most commonly treated with herbal remedies were then selected from the full range of ailments recorded from all the informants.
Site selection and plant collection
The selection of the 50 rural communities for the wider national survey were randomly chosen using the same method as for the pilot study, and the distribution of communities across the island is given in Fig. 1. Using the detailed maps (including house location) provided by the Elections and Boundaries Commission for each randomly selected community, a house at the start of the main street was purposefully chosen to initiate the survey. At that house, field officers introduced themselves and explained the nature of the study and asked for the person (this could have been either male or female) in that household with the most knowledge about medicinal plant use. Subsequently, we used a snowball approach to obtain the sample size from each community; with this approach the preceding interviewee would identify someone else in the community whom they regarded as having had good knowledge of medicinal plant use.
The unmodified TRAMIL questionnaire was used in both the pilot and wider national survey; TRAMIL assumed that the eldest woman in the household had the most knowledge about herbal medicine use and would be the person of interest. However, the field officers asked for the person (which could be either male or female) with the most knowledge about herbal medicine. Although our field officers noted the names and ages of some of the respondents, this was not consistently collected and we therefore could not include any demographic details in our results. Respondents provided vernacular names for plants and the field interviewers collected specimens which were subsequently taken to the National Herbarium of Trinidad and Tobago for identification by a plant taxonomist. The website www.theplantlist.org was accessed to verify the accepted nomenclature for each species.
Results
From the pilot survey the top ten ailments emerging from the informants were cough/common cold, asthma, “stoppage-of-water”, “womb infection”, kidney stones, “afterbirth”, diabetes, hypertension, “cooling/cleanser” and fever, where herbal remedies were frequently used in rural communities in Trinidad. In the wider national survey, 1590 questionnaires were completed from 450 interviews in 50 randomly selected rural communities. These included mixtures, but we present the data for only single plant remedies. Most of the mixtures contained two or more plants, and in some cases up to eight plants with additional ingredients, such as, olive oil, “soft candle” (local name for a paraffin mixture), salt and honey. A major objective of the study was to link the individual plants with relevant pharmacological evidence to support their traditional use. Hence dealing with mixtures would prove almost impossible to determine which plant was responsible for producing the biological activity to correlate with its traditional use.
At the end of the survey 917 single plant remedies, in different formulations, as either infusions or decoctions came from 96 species in 43 families (Table 1). The major plant families were Asteraceae (125 citations, 12 species), Lamiaceae (99 citations, 4 species), Leguminosae (88 citations, 10 species), Verbenaceae (62 citations, 3 species) and Poaceae (52 citations, 2 species). Most plant species were used for multiple ailments. The top five plant species were Leonotis nepetifolia (89 citations; most commonly used for cough/common cold), Neurolaena lobata (77 citations; most commonly used for fever), Cymbopogon citratus (50 citations; most commonly used for fever), Momordica charantia (44 citations; most commonly used for “cooling/cleanser”) and Stachytarpheta jamaicensis (38 citations, mostly for “cooling/cleanser’), Table 2. According to TRAMIL methodology significant plants (with 20 % or more citations by respondents for a specific ailment) were Leonotis nepetifolia for cough/common cold (Fig. 2a shows voucher specimen and Fig. 2b shows localities), Gomphrena globosa (Fig. 3a shows voucher specimen and Fig. 3b shows localities) for “stoppage of water”, Curcuma longa (Fig. 4a voucher specimen and Fig. 4b shows localities) and Senna occidentalis (Fig. 5a voucher specimen and Fig. 5b shows localities) for “afterbirth”, Cymbopogon citratus (Fig. 6a shows voucher specimen and Fig. 6b shows localities) and Neurolaena lobata (Fig. 7a shows voucher specimen and Fig. 7b shows localities) for fever, and Citrus limon (Fig. 8a shows voucher specimen and Fig. 8b shows localities) for kidney stones. Stachytarpheta jamaicensis, Senna alata, Momordica charantia and Tournefortia hirsutissima (although not reaching significant use by TRAMIL criterion) were also widely used as “‘cooling/cleanser’.
Table 1.
List of plants collected in ethnobotanical survey in Trinidad
| TRIN Voucher number | Family | Species | Local names | Part(s) used and preparation | Administration | Condition treated | No. of informants |
|---|---|---|---|---|---|---|---|
| 40251 | Acanthaceae | Justicia pectoralis Jacq. | Carpenter bush, St. John’s bush | Stem and leaves, decoction | Oral | Common cold & cough | 14 |
| Acanthaceae | Justicia pectoralis Jacq. | Carpenter bush, St. John’s bush | Stem and leaves, decoction | Oral | Cooling/cleanser | 4 | |
| 40242 | Acanthaceae | Justicia secunda Vahl | St. John’s bush | Leaves; decoction | Oral | Afterbirth | 1 |
| 40241 | Acanthaceae | Thunbergia alata Boj. ex Sims | Yellow flower vine | Flowers; infusion | Oral | Kidney stones | 1 |
| 40245 | Amaranthaceae | Achyranthes indica (L.) Mill. | Man-better-man | Leaves, soak in water and bathe | Topical | Fever | 1 |
| Amaranthaceae | Achyranthes indica (L.) Mill. | Man-better-man | Leaves; decoction | Oral | Womb infection | 1 | |
| 40236 | Amaranthaceae | Dysphania ambrosioides (L.) Mosyakin & Clemants | Worm grass | Stem and leaves, decoction | Oral | Fever | 1 |
| Amaranthaceae | Dysphania ambrosioides (L.) Mosyakin & Clemants | Worm grass | Stem and leaves, decoction | Oral | Cooling/cleanser | 1 | |
| 40246 | Amaranthaceae | Gomphrena globosa L. | White bachelor button | Flowers; decoction | Oral | Diabetes | 1 |
| Amaranthaceae | Gomphrena globosa L. | White bachelor button | Flowers; infusion or decoction | Oral | Stoppage of water | 17 | |
| Amaranthaceae | Gomphrena globosa L. | White bachelor button | Flowers; infusion or decoction | Oral | Kidney stones | 8 | |
| Amaranthaceae | Gomphrena globosa L. | White bachelor button | Flowers; infusion or decoction | Oral | Womb infection | 1 | |
| 40243 | Anacardiaceae | Spondias mombin L. | Hog plum | Leaves; boil and add to bath water | Topical | Cooling/cleanser | 1 |
| Anacardiaceae | Spondias mombin L. | Hog plum | Leaves; as above and drink decoction after bath | Topical/Oral | Womb infection | 1 | |
| Anacardiaceae | Spondias mombin L. | Hog plum | Leaves; steaming decoction placed in container and mother sits over | Topical | Afterbirth | 7 | |
| 40244 | Anacardiaceae | Mangifera indica L. | Mango vere | Bark; decoction | Oral | High blood pressure | 1 |
| 40248 | Annonaceae | Annona muricata L. | Soursop | Leaves, infusion or decoction | Oral | Cooling/cleanser | 4 |
| Annonaceae | Annona muricata L. | Soursop | Leaves, infusion or decoction | Oral | High blood pressure | 8 | |
| 40248 | Apocynaceae | Catharantus roseus (L.) G.Don | Old maid, periwinkle | Leaves and flowers; infusion or chew and swallow | Oral | Diabetes | 7 |
| Apocynaceae | Catharantus roseus (L.) G.Don | Old maid, periwinkle | Leaves and flowers; infusion or chew and swallow | Oral | Stoppage of water | 1 | |
| 40250 | Aristolochiaceae | Aristolochia rugosa Lam. | Matt root | Roots, decoction or soak in alcohol | Oral | Fever | 1 |
| Aristolochiaceae | Aristolochia rugosa Lam. | Matt root | Roots, decoction or soak in alcohol | Oral | Common cold & cough | 1 | |
| Aristolochiaceae | Aristolochia rugosa Lam. | Matt root | Roots, decoction or soak in alcohol | Oral | Diabetes | 1 | |
| 40249 | Aristolochiaceae | Aristolochia rugosa Lam. | Tref | Leaves, chew raw leaves or soak in alcohol with caterpillar that feeds on leaves | Oral | Fever | 1 |
| Aristolochiaceae | Aristolochia rugosa Lam. | Tref | Leaves, chew raw leaves or soak in alcohol with caterpillar that feeds on leaves | Oral | Common cold & cough | 3 | |
| 40253 | Asteraceae | Ageratum conyzoides L. | Zebafam | Leaves, stem and flowers; decoction | Oral | Common cold & cough | 1 |
| Asteraceae | Ageratum conyzoides L. | Zebafam | Leaves, stem and flowers; decoction | Oral | Cooling/cleanser | 1 | |
| Asteraceae | Ageratum conyzoides L. | Zebafam | Leaves, stem and flowers; decoction | Oral | Womb infection | 4 | |
| Asteraceae | Ageratum conyzoides L. | Zebafam | Leaves, stem and flowers; decoction | Oral | Afterbirth | 2 | |
| 40255 | Asteraceae | Ambrosia peruviana Willd. | Altamis | Leaves; infusion or steamed and woman sits over | Oral/Topical | Womb infection | 2 |
| Asteraceae | Ambrosia peruviana Willd. | Altamis | Leaves; infusion | Oral | Afterbirth | 1 | |
| 40252 | Asteraceae | Ayapana triplinervis (Vahl) R.M. King & H.Rob. | Japana | Leaves; infusion | Oral | Common cold & cough | 1 |
| 40256 | Asteraceae | Bidens pilosa L. | Railway daisy, rabbit grass. Needle grass | Leaves, Decoction or chew and swallow juice | Oral | Common cold & cough | 1 |
| Asteraceae | Bidens pilosa L. | Railway daisy, rabbit grass. Needle grass | Leaves, Decoction or chew and swallow juice | Oral | High blood pressure | 6 | |
| Asteraceae | Bidens pilosa L. | Railway daisy, rabbit grass. Needle grass | Leaves, Decoction or chew and swallow juice | Oral | Diabetes | 2 | |
| Asteraceae | Bidens pilosa L. | Railway daisy, rabbit grass. Needle grass | Leaves, Decoction or chew and swallow juice | Oral | Stoppage of water | 1 | |
| 40254 | Asteraceae | Chaptalia nutans (L.) Polák | Doblan | Whole plant; infusion | Oral | High blood pressure | 1 |
| 40257 | Asteraceae | Chromolaena odorata (L.) R.M.King & H.Rob. | Christmas bush | Leaves, infusion or decoction or crush leaves and drink juice | Oral | Common cold & cough | 7 |
| Asteraceae | Chromolaena odorata (L.) R.M.King & H.Rob. | Christmas bush | Leaves, infusion or decoction or crush leaves and drink juice | Oral | High blood pressure | 1 | |
| 40258 | Asteraceae | Eclipta prostrata (L.) L. | Congolalla | Stem and leaves; decoction | Oral | Cooling/cleanser | 2 |
| Asteraceae | Eclipta prostrata (L.) L. | Congolalla | Stem and leaves; decoction | Oral | Diabetes | 2 | |
| Asteraceae | Eclipta prostrata (L.) L. | Congolalla | Stem and leaves; decoction | Oral | Asthma | 1 | |
| 40260 | Asteraceae | Hebeclinium macrophyllum DC. | Zebchat | Leaves; pounded in cloth and inserted in vagina | Topical | Womb infection | 1 |
| 40261 | Asteraceae | Neurolaena lobata (L.) Cass. | Zebapique | Leaves, infusion or decoction or soak in alcohol or crush leaves and drink juice | Oral | Fever | 30 |
| Asteraceae | Neurolaena lobata (L.) Cass. | Zebapique | Leaves, infusion or decoction or soak in alcohol or crush leaves and drink juice | Oral | Common cold & cough | 43 | |
| Asteraceae | Neurolaena lobata (L.) Cass. | Zebapique | Leaves, infusion or decoction or soak in alcohol or crush leaves and drink juice | Oral | Diabetes | 2 | |
| Asteraceae | Neurolaena lobata (L.) Cass. | Zebapique | Leaves, infusion or decoction or soak in alcohol or crush leaves and drink juice | Oral | Womb infection | 2 | |
| 40262 | Asteraceae | Parthenium hysterophorus L. | White top | Leaves; decoction | Oral | Diabetes | 1 |
| 40263 | Asteraceae | Pluchea carolinensis (Jacq.) G.Don | Geritout, pressure bush | Leaves, infusion or decoction | Oral | Fever | 2 |
| Asteraceae | Pluchea carolinensis (Jacq.) G.Don | Geritout, pressure bush | Leaves, infusion or decoction | Oral | Common cold & cough | 5 | |
| Asteraceae | Pluchea carolinensis (Jacq.) G.Don | Geritout, pressure bush | Leaves, infusion or decoction | Oral | High blood pressure | 1 | |
| 40264 | Asteraceae | Vernonia amygdalina Delile | Africana | Leaves; chewed and juice swallowed | Oral | High blood pressure | 1 |
| Asteraceae | Vernonia amygdalina Delile | Africana | Leaves; chewed and juice swallowed | Oral | Diabetes | 1 | |
| 40229 | Begoniaceae | Begonia humilis Dryand. | Lozei | Leaves, decoction | Oral | Common cold & cough | 1 |
| Begoniaceae | Begonia humilis Dryand. | Lozei | Leaves, decoction | Oral | Stoppage of water | 1 | |
| 40227 | Bignoniaceae | Crescentia cujete L. | Calabash | Fruit (guts); decoction with honey to make thick “lock” | Oral | Common cold & cough | 1 |
| Bignoniaceae | Crescentia cujete L. | Calabash | Fruit (pulp); decoction with honey to make thick “lock” | Oral | High blood pressure | 3 | |
| Bignoniaceae | Crescentia cujete L. | Calabash | Leaves; infusion | Oral | Diabetes | 1 | |
| Bignoniaceae | Crescentia cujete L. | Calabash | Leaves; infusion | Oral | Asthma | 1 | |
| 40228 | Bignoniaceae | Dolichandra unguis-cati (L.) L.G.Lohmann | Cat’s claw | Stem and leaves; hot or cold infusion, decoction | Oral | Common cold & cough | 1 |
| Bignoniaceae | Dolichandra unguis-cati (L.) L.G.Lohmann | Cat’s claw | Stem and leaves; hot or cold infusion, decoction | Oral | Cooling/cleanser | 3 | |
| Bignoniaceae | Dolichandra unguis-cati (L.) L.G.Lohmann | Cat’s claw | Stem and leaves; hot or cold infusion, decoction | Oral | Kidney stones | 2 | |
| Bignoniaceae | Dolichandra unguis-cati (L.) L.G.Lohmann | Cat’s claw | Stem and leaves; hot or cold infusion, decoction | Oral | Diabetes | 1 | |
| 40357 | Boraginacece | Tournefortia hirsutissima L. | Jigger bush | Stem and leaves; hot or cold infusion, decoction | Oral | Common cold & cough | 1 |
| Boraginacece | Tournefortia hirsutissima L. | Jigger bush | Stem and leaves; hot or cold infusion, decoction | Oral | Cooling/cleanser | 20 | |
| Boraginacece | Tournefortia hirsutissima L. | Jigger bush | Stem and leaves; hot or cold infusion, decoction | Oral | Diabetes | 1 | |
| 40226 | Bixaceae | Bixa orellana L. | Roucou | Leaves, fruits and roots; decoction | Oral | High blood pressure | 1 |
| Bixaceae | Bixa orellana L. | Roucou | Leaves, fruits and roots; decoction | Oral | Diabetes | 4 | |
| 40225 | Boraginaceae | Cordia curassavica (Jacq.) Roem. & Schult. | Black sage, blister bush | Leaves, infusion or crush and drink juice | Oral | Fever | 1 |
| Boraginaceae | Cordia curassavica (Jacq.) Roem. & Schult. | Black sage, blister bush | Leaves, infusion or crush and drink juice | Oral | Common cold & cough | 7 | |
| Boraginaceae | Cordia curassavica (Jacq.) Roem. & Schult. | Black sage, blister bush | Leaves, infusion or crush and drink juice | Oral | Cooling/cleanser | 1 | |
| Boraginaceae | Cordia curassavica (Jacq.) Roem. & Schult. | Black sage, blister bush | Leaves (yellow); decoction | Oral | Womb infection | 1 | |
| 40231 | Cactaceae | Nopalea cochenillifera (L.) Salm-Dyck | Ratchet | Succulent leaves; grate, hot or cold infusion | Oral | Cooling/cleanser | 9 |
| 40230 | Cactaceae | Rhipsalis baccifera (J.S.Muell.) Stearn | Old man beard | Stem and leaves; infusion or decoction | Oral | Diabetes | 3 |
| 40240 | Caprifoliaceae | Sambucus canadensis L. | Serrio | Leaves and flowers, decoction or crush and drink juice (add olive oil with/without salt) | Oral | Fever | 1 |
| Caprifoliaceae | Sambucus canadensis L. | Serrio | Leaves and flowers, decoction or crush and drink juice (add olive oil with/without salt) | Oral | Common cold & cough | 20 | |
| Caprifoliaceae | Sambucus canadensis L. | Serrio | Leaves and flowers, decoction or crush and drink juice (add olive oil with/without salt) | Oral | Asthma | 2 | |
| 40238 (40239) | Caricaceae | Carica papaya L. | Pawpaw | Fruit (young); grated for infusion or decoction | Oral | High blood pressure | 9 |
| Caricaceae | Carica papaya L. | Pawpaw | Leaves; chew and swallow juice | Oral | Diabetes | 2 | |
| Caricaceae | Carica papaya L. | Pawpaw | Roots of male plant; infusion | Oral | Stoppage of water | 1 | |
| Caricaceae | Carica papaya L. | Pawpaw | Roots of male plant; decoction | Oral | Kidney stones | 2 | |
| 40235 | Commelinaceae | Commelina erecta L. | Watergrass | Stem and leaves; infusion or decoction | Oral | Cooling/cleanser | 6 |
| Commelinaceae | Commelina erecta L. | Watergrass | Stem and leaves; infusion or decoction | Oral | Stoppage of water | 2 | |
| 40233 | Convolvulaceae | Cuscuta campestris Yunck. | Love vine | Vine (stem and leaves); infusion or decoction | Oral | Cooling/cleanser | 3 |
| Convolvulaceae | Cuscuta campestris Yunck. | Love vine | Vine (stem and leaves); infusion or decoction | Oral | Kidney stones | 1 | |
| 40232 | Crassulaceae | Bryophyllum pinnatum (Lam.) Oken | Wonder-of-the-world | Leaves, infusion or heat leaves and squeeze juice | Oral | Common cold & cough | 8 |
| Crassulaceae | Bryophyllum pinnatum (Lam.) Oken | Wonder-of-the-world | Leaves, infusion or heat leaves and squeeze juice | Oral | Cooling/cleanser | 2 | |
| Crassulaceae | Bryophyllum pinnatum (Lam.) Oken | Wonder-of-the-world | Leaves, infusion or heat leaves and squeeze juice | Oral | High blood pressure | 2 | |
| Crassulaceae | Bryophyllum pinnatum (Lam.) Oken | Wonder-of-the-world | Leaves, infusion or heat leaves and squeeze juice | Oral | Diabetes | 5 | |
| Crassulaceae | Bryophyllum pinnatum (Lam.) Oken | Wonder-of-the-world | Leaves, infusion or heat leaves and squeeze juice | Oral | Asthma | 2 | |
| Crassulaceae | Bryophyllum pinnatum (Lam.) Oken | Wonder-of-the-world | Leaves, infusion or heat leaves and squeeze juice | Oral | Kidney stones | 1 | |
| 40231 | Cucurbitaceae | Momordica charantia L. | Caraille | Vine (stem and leaves), decoction | Oral | Fever | 2 |
| Cucurbitaceae | Momordica charantia L. | Caraille | Vine (stem and leaves), decoction | Oral | Common cold & cough | 2 | |
| Cucurbitaceae | Momordica charantia L. | Caraille | Vine (stem and leaves), decoction | Oral | Cooling/cleanser | 21 | |
| Cucurbitaceae | Momordica charantia L. | Caraille | Vine (stem and leaves), decoction | Oral | High blood pressure | 4 | |
| Cucurbitaceae | Momordica charantia L. | Caraille | Vine (stem and leaves), decoction | Oral | Diabetes | 7 | |
| Cucurbitaceae | Momordica charantia L. | Caraille | Vine (stem and leaves), decoction | Oral | Womb infection | 7 | |
| Cucurbitaceae | Momordica charantia L. | Caraille | Vine (stem and leaves), decoction | Oral | Afterbirth | 1 | |
| 40267 | Euphorbiaceae | Euphorbia thymifolia L. | Female malomay | Vine (stem and leaves); infusion | Oral | High blood pressure | 1 |
| 40268 | Euphorbiaceae | Euphorbia hirta L. | Malomay | Leaves; infusion | Oral | Kidney stones | 1 |
| Euphorbiaceae | Euphorbia hirta L. | Malomay | Leaves; infusion | Oral | Womb infection | 1 | |
| 40273 | Euphorbiaceae | Euphorbia oerstediana (Klotzsch & Garcke) Boiss. | Kidney bush | Leaves, stem, seeds; decoction | Oral | Kidney stones | 2 |
| 40272 | Euphorbiaceae | Jatropha gossypiifolia L. var. elegans (Pohl) Müll.Arg | Red physic nut, wild cassava | Leaves; decoction or apply leaves to body | Topical | Common cold & cough | 1 |
| Euphorbiaceae | Jatropha gossypiifolia L. var. elegans (Pohl) Müll.Arg | Red physic nut, wild cassava | Leaves; decoction or apply leaves to body | Oral | Cooling/cleanser | 1 | |
| Euphorbiaceae | Jatropha gossypiifolia L. var. elegans (Pohl) Müll.Arg | Red physic nut, wild cassava | Leaves; decoction or apply leaves to body | Oral | Womb infection | 1 | |
| 40234 | Gentianaceae | Enicostema verticillatum (L.) Engl. ex Gilg. | Kainnine | Leaves, chew and swallow juice | Oral | Fever | 1 |
| 40277 | Lamiaceae | Hyptis suaveolens (L.) Poit. | African mint, jungle mint, matram, hyssop | Leaves, infusion or crush and inhaled | Oral, Inhalation | Fever | 1 |
| Lamiaceae | Hyptis suaveolens (L.) Poit. | African mint, jungle mint, matram, hyssop | Leaves, infusion or crush and inhaled | Oral | Common cold & cough | 3 | |
| Lamiaceae | Hyptis suaveolens (L.) Poit. | African mint, jungle mint, matram, hyssop | Leaves, infusion or crush and inhaled | Oral | Cooling/cleanser | 1 | |
| 40274 | Lamiaceae | Leonotis nepetifolia (L.) R.Br. | Shandilay | Leaves, infusion or decoction or pound and squeeze juice (add salt) | Oral | Fever | 1 |
| Lamiaceae | Leonotis nepetifolia (L.) R.Br. | Shandilay | Leaves, infusion or decoction or pound and squeeze juice (add salt) | Oral | Common cold & cough | 85 | |
| Lamiaceae | Leonotis nepetifolia (L.) R.Br. | Shandilay | Leaves, infusion or decoction or pound and squeeze juice (add salt) | Oral | Cooling/cleanser | 1 | |
| Lamiaceae | Leonotis nepetifolia (L.) R.Br. | Shandilay | Leaves, infusion or decoction or pound and squeeze juice (add salt) | Oral | Diabetes | 1 | |
| Lamiaceae | Leonotis nepetifolia (L.) R.Br. | Shandilay | Leaves, infusion or decoction or pound and squeeze juice (add salt) | Oral | Asthma | 1 | |
| 40276 | Lamiaceae | Ocimum gratissimum L. | Aroubaba | Leaves and stem, decoction | Oral | Fever | 1 |
| Lamiaceae | Ocimum gratissimum L. | Aroubaba | Leaves and stem, decoction | Oral | Common cold & cough | 2 | |
| 40275 | Lamiaceae | Ocimum micranthum Willd. | Jumbie basil | Stem and leaves, infusion or decoction | Cooling/cleanser | 2 | |
| 40278 | Lauraceae | Persea americana Mill. | Avocado | Leaves; decoction | Oral | High blood pressure | 2 |
| 40317 | Leguminosae | Abrus precatorius L. | Jumbie bead | Vine (stem and leaves); infusion or decoction | Oral | Common cold & cough | 4 |
| 40318 | Leguminosae | Brownea coccinea Jacq. ssp. capitella (Jacq.) D.Velázquez & G.Agostini, | Cooper hook | Flowers; infusion | Oral | Womb infection | 1 |
| 40319 | Leguminosae | Cajanus cajan (L.) Millsp. | Pigeon peas | Leaves; decoction added to bath water | Topical | Common cold & cough | 1 |
| Leguminosae | Cajanus cajan (L.) Millsp. | Pigeon peas | Leaves; decoction added to bath water | Oral | High blood pressure | 1 | |
| 40320 | Leguminosae | Entada polystachya (L.) DC. | Mayok shapel | Bark and roots; infusion | Oral | Cooling/cleanser | 3 |
| Leguminosae | Entada polystachya (L.) DC. | Mayok shapel | Bark and roots; infusion | Oral | Stoppage of water | 1 | |
| Leguminosae | Entada polystachya (L.) DC. | Mayok shapel | Bark and roots; infusion | Oral | Womb infection | 1 | |
| 40315 | Leguminosae | Flemingia strobilifera (L.) W.T.Aiton | Mosquito bush, wild hops | Whole plant (with roots); decoction | Oral | Stoppage of water | 2 |
| Leguminosae | Flemingia strobilifera (L.) W.T.Aiton | Mosquito bush, wild hops | Whole plant (with roots); decoction | Oral | Kidney stones | 3 | |
| 40316 | Leguminosae | Mimosa pudica L. | Timarie, shame bush, sensitive plant, Mary-Mary- close- your- door | Whole plant; decoction | Oral | Common cold & cough | 1 |
| Leguminosae | Mimosa pudica L. | Timarie, shame bush, sensitive plant, Mary-Mary- close- your- door | Whole plant; decoction | Oral | Diabetes | 1 | |
| Leguminosae | Mimosa pudica L. | Timarie, shame bush, sensitive plant, Mary-Mary- close- your- door | Roots; decoction | Oral | Stoppage of water | 4 | |
| Leguminosae | Mimosa pudica L. | Timarie, shame bush, sensitive plant, Mary-Mary- close- your- door | Roots; decoction | Oral | Kidney stones | 6 | |
| Leguminosae | Mimosa pudica L. | Timarie, shame bush, sensitive plant, Mary-Mary- close- your- door | Roots; decoction | Oral | Womb infection | 3 | |
| 40304 (36911) | Leguminosae | Senna alata (L.) Roxb. | Wild senna, ringworm bush | Leaves; infusion or decoction | Oral | Cooling/cleanser | 26 |
| Leguminosae | Senna alata (L.) Roxb. | Wild senna, ringworm bush | Seeds; roasted, grounded and infusion | Oral | Asthma | 1 | |
| Leguminosae | Senna alata (L.) Roxb. | Wild senna, ringworm bush | Leaves and flowers; infusion or decoction | Oral | Womb infection | 3 | |
| 40314 | Leguminosae | Senna bacillaris (L.f.) H.S.Irwin & Barneby | Christmas bush | Leaves and stem; decoction | Oral | Kidney stones | 1 |
| 40312 | Leguminosae | Senna occidentalis (L.) Link | Wild coffee | Seeds; roasted, grounded and infusion | Oral | Common cold & cough | 1 |
| Leguminosae | Senna occidentalis (L.) Link | Wild coffee | Roots; decoction | Oral | Cooling/cleanser | 1 | |
| Leguminosae | Senna occidentalis (L.) Link | Wild coffee | Roots; decoction | Oral | Asthma | 1 | |
| Leguminosae | Senna occidentalis (L.) Link | Wild coffee | Roots; decoction | Oral | Womb infection | 1 | |
| Leguminosae | Senna occidentalis (L.) Link | Wild coffee | Roots; decoction | Oral | Afterbirth | 8 | |
| 40313 | Leguminosae | Tamarindus indica L. | Tambran | Fruit (with seeds) and leaves; infusion | Oral | High blood pressure | 11 |
| Leguminosae | Tamarindus indica L. | Tambran | Bark; decoction | Oral | Diabetes | 1 | |
| Leguminosae | Tamarindus indica L. | Tambran | Bark; decoction | Oral | Asthma | 1 | |
| 40280 | Loranthaceae | Phthirusa stelis (L.) Kuijt | Birdvine | Vine (stem and leaves); decoction | Oral | Stoppage of water | 1 |
| 40310 | Malvaceae | Hibiscus rosa-sinensis L. | Double hibiscus, Arrahoo | Flowers, infusion or decoction | Oral | Common cold & cough | 10 |
| Malvaceae | Hibiscus rosa-sinensis L. | Double hibiscus, Arrahoo | Flowers, infusion or decoction | Oral | Cooling/cleanser | 1 | |
| Malvaceae | Hibiscus rosa-sinensis L. | Double hibiscus, Arrahoo | Flowers, infusion or decoction | Oral | Diabetes | 1 | |
| Malvaceae | Hibiscus rosa-sinensis L. | Double hibiscus, Arrahoo | Flowers, infusion or decoction | Oral | Stoppage of water | 1 | |
| Malvaceae | Hibiscus rosa-sinensis L. | Double hibiscus, Arrahoo | Flowers, infusion or decoction | Oral | Womb infection | 1 | |
| 40311 | Malvaceae | Urena sinuata L. | Kuzen mahoe | Stem and leaves; infusion or decoction | Oral | Cooling/cleanser | 2 |
| Malvaceae | Urena sinuata L. | Kuzen mahoe | Stem and leaves; infusion or decoction | Oral | Kidney stones | 1 | |
| 40309 | Meliaceae | Azadirachta indica A.Juss. | Neem | Leaves; decoction | Oral | Cooling/cleanser | 1 |
| Meliaceae | Azadirachta indica A.Juss. | Neem | Leaves; chew and swallow juice | Oral | Diabetes | 7 | |
| 40308 | Meliaceae | Carapa guianensis Aubl. | Carapa, crappo | Seed (oil extracted) | Oral | Common cold & cough | 1 |
| Meliaceae | Carapa guianensis Aubl. | Carapa, crappo | Seed (oil extracted) | Oral | Asthma | 1 | |
| 40306 | Menispermaceae | Cissampelos pareira L. | Grave yard bush, Cat ears, patacon | Vine (stem and leaves); infusion or decoction | Oral | Common cold & cough | 3 |
| Menispermaceae | Cissampelos pareira L. | Grave yard bush, Cat ears, patacon | Vine (stem and leaves); infusion or decoction | Oral | Asthma | 1 | |
| 40307 | Moraceae | Artocarpus altilis (Parkinson) Fosberg | Breadfruit | Yellow leaves; infusion or decoction | Oral | High blood pressure | 11 |
| 40303 | Moraceae | Morus alba L. | Pressure bush | Leaves; infusion or decoction | Oral | High blood pressure | 8 |
| 40302 | Myoporaceae | Bontia daphnoides L. | Olive bush | Leaves; infusion or decoction | Oral | Common cold & cough | 1 |
| Myoporaceae | Bontia daphnoides L. | Olive bush | Leaves; infusion or decoction | Oral | Cooling/cleanser | 6 | |
| Myoporaceae | Bontia daphnoides L. | Olive bush | Leaves; infusion or decoction | Oral | High blood pressure | 2 | |
| Myoporaceae | Bontia daphnoides L. | Olive bush | Leaves; infusion or decoction | Oral | Diabetes | 2 | |
| Myoporaceae | Bontia daphnoides L. | Olive bush | Leaves; infusion or decoction | Oral | Kidney stones | 5 | |
| Myoporaceae | Bontia daphnoides L. | Olive bush | Leaves; infusion or decoction | Oral | Womb infection | 1 | |
| 40301 | Myrtaceae | Pimenta racemosa (Mill.) J.W.Moore | Bay leaf, bay rum | Leaves, decoction | Oral | Fever | 1 |
| Myrtaceae | Pimenta racemosa (Mill.) J.W.Moore | Bay leaf, bay rum | Leaves, decoction | Oral | Common cold & cough | 1 | |
| Myrtaceae | Pimenta racemosa (Mill.) J.W.Moore | Bay leaf, bay rum | Leaves, decoction | Oral | Cooling/cleanser | 3 | |
| Myrtaceae | Pimenta racemosa (Mill.) J.W.Moore | Bay leaf, bay rum | Leaves, decoction | Oral | High blood pressure | 1 | |
| 40269 | Phyllanthaceae | Phyllanthus amarus Schumach. & Thonn. | Seed-under-leaf, Guen amber faye | Whole plant(stem, leaves and roots) | Oral | Diabetes | 6 |
| 40271 | Phyllanthaceae | Phyllanthus urinaria L. | Seed-under-leaf | Whole plant (stem, leaves and roots); decoction | Oral | Womb infection | 2 |
| Phyllanthaceae | Phyllanthus urinaria L. | Seed-under-leaf | Whole plant (stem, leaves and roots); decoction | Oral | Stoppage of water | 1 | |
| Phyllanthaceae | Phyllanthus urinaria L. | Seed-under-leaf | Whole plant (stem, leaves and roots); decoction | Oral | High blood pressure | 2 | |
| 40270 | Phyllanthaceae | Phyllantus sp. | Seed-under-leaf | Whole plant (stem, leaves and roots): infusion or decoction | Oral | Cooling | 1 |
| Phyllanthaceae | Phyllantus sp. | Seed-under-leaf | Whole plant (stem, leaves and roots): infusion or decoction | Oral | Stoppage of water | 1 | |
| Phyllanthaceae | Phyllantus sp. | Seed-under-leaf | Whole plant (stem, leaves and roots): infusion or decoction | Oral | Kidney stones | 3 | |
| 40298 | Phytolaccaceae | Microtea debilis Sw. | Alantoki | Leaves; decoction | Oral | Common cold & cough | 3 |
| Phytolaccaceae | Microtea debilis Sw. | Alantoki | Whole plant (leaves, stem and roots) | Oral | Asthma | 1 | |
| 40297 | Phytolaccaceae | Petiveria alliacea L. | Gully root | Roots; crushed and infused or soak in alcohol | Oral | Common cold & cough | 1 |
| 40300 | Passifloraceae | Passiflora edulis Sims | Passion fruit | Leaves; decoction | Oral | High blood pressure | 1 |
| 40299 | Passifloraceae | Passiflora quadrangularis L. | Barbadine | Leaves; infusion or decoction | Oral | High blood pressure | 9 |
| 40296 | Piperaceae | Peperomia pellucida (L.) Kunth | Shining bush | Whole plant; infusion or decoction | Oral | Common cold & cough | 2 |
| Piperaceae | Peperomia pellucida (L.) Kunth | Shining bush | Whole plant; infusion or decoction | Oral | Cooling/cleanser | 15 | |
| Piperaceae | Peperomia pellucida (L.) Kunth | Shining bush | Whole plant; infusion or decoction | Oral | Stoppage of water | 1 | |
| 40295 | Piperaceae | Piper marginatum Jacq. | Lanie bois | Leaves; decoction | Oral | Womb infection | 1 |
| 40292 | Piperaceae | Piper tuberculatum Jacq. | Candle bush | Leaves; decoction | Oral | Diabetes | 1 |
| 40293 | Plantaginaceae | Plantago major L. | Plante | Leaves; infusion | Oral | High blood pressure | 1 |
| 40265 | Poaceae (Gramineae) | Cymbopogon citratus (DC.) Stapf | Fevergrass | Leaves and roots, decoction | Oral | Fever | 46 |
| Poaceae (Gramineae) | Cymbopogon citratus (DC.) Stapf | Fevergrass | Leaves and roots, decoction | Oral | Common cold & cough | 1 | |
| Poaceae (Gramineae) | Cymbopogon citratus (DC.) Stapf | Fevergrass | Leaves and roots, decoction | Oral | Cooling/cleanser | 3 | |
| 40266 | Poaceae (Gramineae) | Pennisetum purpureum Schumach. | Wild cane, cane riviere | Stem; crush in cold infusion | Oral | Cooling/cleanser | 1 |
| Poaceae (Gramineae) | Pennisetum purpureum Schumach. | Wild cane, cane riviere | Stem; crush in cold infusion | Oral | Stoppage of water | 1 | |
| 40294 | Polygonaceae | Antigonon leptopus Hooker & Arn. | Coralita | Vine (stem and leaves) | Oral | Diabetes | 1 |
| 40288 | Rubiaceae | Genipa americana L. | Monkey apple | Fruit; decoction | Oral | Diabetes | 1 |
| 40291 | Rubiaceae | Morinda citrifolia L. | Noni, pain bush | Fruit; juice of ripened fruit | Oral | Cooling/cleanser | 1 |
| Rubiaceae | Morinda citrifolia L. | Noni, pain bush | Fruit; juice of ripened fruit | Oral | Diabetes | 1 | |
| 40289 | Rubiaceae | Spermacoce verticillata L. | White top, Fowl foot grass | Leaves; pound and boil | Oral | High blood pressure | 1 |
| Rubiaceae | Spermacoce verticillata L. | White top, Fowl foot grass | Leaves; pound and boil | Oral | Diabetes | 1 | |
| 40290 | Rutaceae | Citrus x aurantifolia (Christm. & Panzer) Swingle | Lime | Leaves (young), decoction | Oral | Fever | 1 |
| Rutaceae | Citrus x aurantifolia (Christm. & Panzer) Swingle | Juice of fruit | Oral | Common cold & cough | 4 | ||
| Rutaceae | Citrus x aurantifolia (Christm. & Panzer) Swingle | Leaves (young), decoction | Oral | Cooling/cleanser | 1 | ||
| 40287 | Rutaceae | Citrus x limon (L.) Osbeck, | Rough lemon | Juice of fruit, mixture with alcohol or coconut oil | Oral | Fever | 1 |
| Rutaceae | Citrus x limon (L.) Osbeck | Rough lemon | Juice of fruit, mixture with alcohol or coconut oil | Oral | Common cold & cough | 1 | |
| Rutaceae | Citrus x limon (L.) Osbeck | Rough lemon | Juice of fruit, mixture with alcohol or coconut oil | Oral | Cooling/cleanser | 4 | |
| Rutaceae | Citrus x limon (L.) Osbeck | Rough lemon | Juice of fruit, mixture with alcohol or coconut oil | Oral | High blood pressure | 1 | |
| Rutaceae | Citrus x limon (L.) Osbeck | Rough lemon | Juice or skin (grated with molasses) | Oral | Stoppage of water | 2 | |
| Rutaceae | Citrus x limon (L.) Osbeck | Rough lemon | Juice of fruit (with olive oil) | Oral | Kidney stones | 9 | |
| Rutaceae | Citrus x limon (L.) Osbeck | Rough lemon | Juice of fruit (with olive oil) | Oral | Womb infection | 1 | |
| 40237 | Urticaceae | Cecropia peltata L. | Bois cano | Dried leaves, infusion or decoction | Oral | Fever | 1 |
| Urticaceae | Cecropia peltata L. | Bois cano | Dried leaves, infusion or decoction | Oral | Common cold & cough | 9 | |
| Urticaceae | Cecropia peltata L. | Bois cano | Dried leaves, infusion or decoction | Oral | High blood pressure | 8 | |
| Urticaceae | Cecropia peltata L. | Bois cano | Dried leaves, infusion or decoction | Oral | Diabetes | 1 | |
| Urticaceae | Cecropia peltata L. | Bois cano | Dried leaves, infusion or decoction | Oral | Stoppage of water | 1 | |
| 40285 | Verbenaceae | Lantana camara L. | Kayakeet | Leaves, infusion or decoction | Oral | Fever | 1 |
| Verbenaceae | Lantana camara L. | Kayakeet | Leaves, infusion or decoction | Oral | Common cold & cough | 14 | |
| Verbenaceae | Lantana camara L. | Kayakeet | Leaves, infusion or decoction | Oral | Cooling/cleanser | 1 | |
| 40284 | Verbenaceae | Lippia alba (Mill.) N.E.Br. | Santa Maria | Leaves, decoction | Oral | Fever | 2 |
| Verbenaceae | Lippia alba (Mill.) N.E.Br. | Santa Maria | Leaves, decoction | Oral | Common cold & cough | 5 | |
| Verbenaceae | Lippia alba (Mill.) N.E.Br. | Santa Maria | Leaves, decoction | Oral | Diabetes | 1 | |
| 40305 | Verbenaceae | Stachytarpheta jamaicensis (L.) Vahl | Vervine | Leaves, infusion or decoction | Oral | Common cold & cough | 1 |
| Verbenaceae | Stachytarpheta jamaicensis (L.) Vahl | Vervine | Leaves, infusion or decoction | Oral | Cooling/cleanser | 36 | |
| Verbenaceae | Stachytarpheta jamaicensis (L.) Vahl | Vervine | Leaves, infusion or decoction | Oral | High blood pressure | 1 | |
| 40286 | Vitaceae | Cissus verticillata (L.) Vahl | Snake bush | Leaves, decoction | Oral | Common cold & cough | 1 |
| 40279 | Xanthorrhoeaceae | Aloe vera (L.) Burm.f. | Aloes | Leaves, extract gel and eat | Oral | Fever | 1 |
| Xanthorrhoeaceae | Aloe vera (L.) Burm.f. | Aloes | Leaves, extract gel and eat | Oral | Common cold & cough | 1 | |
| Xanthorrhoeaceae | Aloe vera (L.) Burm.f. | Aloes | Leaves, extract gel and eat | Oral | Cooling/cleanser | 8 | |
| Xanthorrhoeaceae | Aloe vera (L.) Burm.f. | Aloes | Leaves, extract gel and eat | Oral | Womb infection | 2 | |
| Xanthorrhoeaceae | Aloe vera (L.) Burm.f. | Aloes | Leaves, extract gel and eat | Oral | Afterbirth | 1 | |
| 40281 | Zingiberaceae | Cheilocostus speciosus (J.Koenig) C.D.Specht | Cane Riviere | Stem; Cut in pieces and boiled | Oral | Cooling/cleanser | 1 |
| Zingiberaceae | Cheilocostus speciosus (J.Koenig) C.D.Specht | Cane Riviere | Stem; Cut in pieces and boiled | Oral | Diabetes | 1 | |
| 40282 | Zingiberaceae | Curcuma longa L. | Saffron, hardi | Stem; pounded and make decoction | Oral | Cooling/cleanser | 1 |
| Zingiberaceae | Curcuma longa L. | Saffron, hardi | Stem; pounded and make decoction | Oral | Womb infection | 3 | |
| Zingiberaceae | Curcuma longa L. | Saffron, hardi | Stem; pounded and make decoction | Oral | Afterbirth | 17 | |
| 40283 | Zingiberaceae | Zingiber officinale Roscoe | Ginger | Rhizomes, crushed and decoction made | Oral | Common cold & cough | 2 |
Table 2.
Top five most commonly cited plants
| Family | Species | Local names | Condition treated | No. of citations |
|---|---|---|---|---|
| Lamiaceae | Leonotis nepetifolia (L.) R.Br. | Shandilay | Fever | 1 |
| Cough & common cold | 85 | |||
| “cooling/cleanser” | 1 | |||
| Diabetes | 1 | |||
| Asthma | 1 | |||
| Asteraceae | Neurolaena lobata (L.) R.Br. ex Cass. | Zebapique | Fever | 30 |
| Cough & common cold | 43 | |||
| Diabetes | 2 | |||
| “Womb infection” | 2 | |||
| Poaceae | Cymbopogon citratus (DC.) Stapf | Lemon grass | Fever | 46 |
| Cough & common cold | 1 | |||
| “cooling/cleanser” | 3 | |||
| Verbenaceae | Stachytarpheta jamaicensis (L.) Vahl | Vervine | Cough & common cold | 1 |
| “cooling/cleanser” | 36 | |||
| High blood pressure | 1 | |||
| Cucurbitaceae | Momordica charantia L. | Caraille | Fever | 2 |
| Cough & common cold | 2 | |||
| “cooling/cleanser” | 21 | |||
| High blood pressure | 4 | |||
| Diabetes | 7 | |||
| “Womb infection” | 7 | |||
| “afterbirth” | 1 |
Fig. 2.
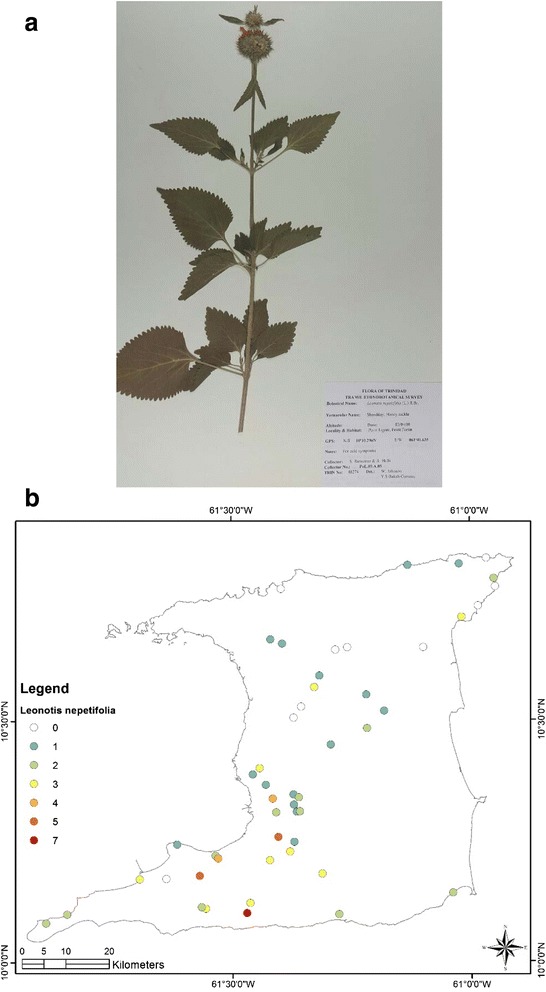
a (Top): Photograph of a voucher specimen of Leonotis nepetifolia (L.).R.Br. Used for cough/common cold. b (Bottom): Map of sites where Leonotis nepetifolia (L.) .R. Br Br. samples were collected. Used for cough/common cold
Fig. 3.
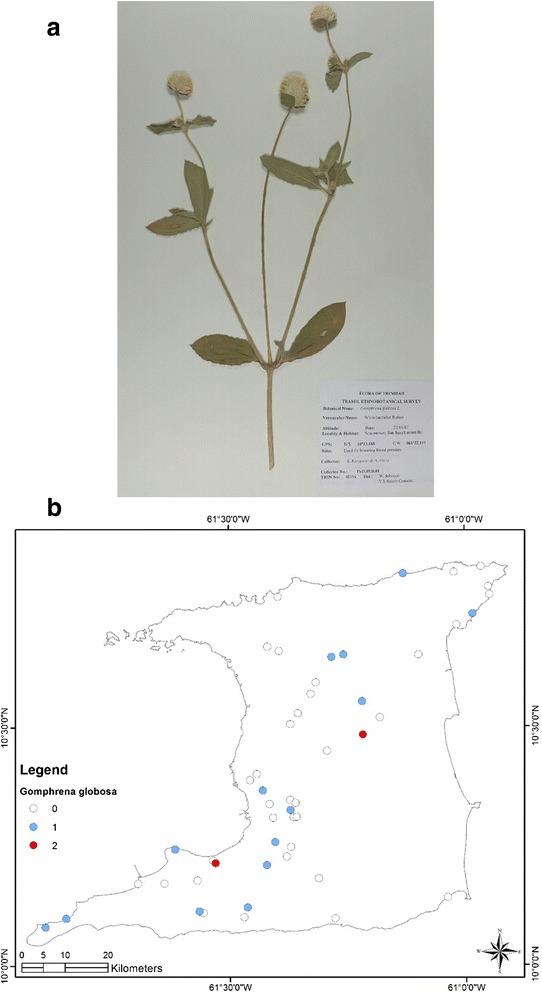
a (Top): Photograph of a voucher specimen for Gomphrena globosa L. Used for “stoppage of water”. b (Bottom): Map of sites where Gomphrena globosa L. was collected. Used for “stoppage of water”
Fig. 4.
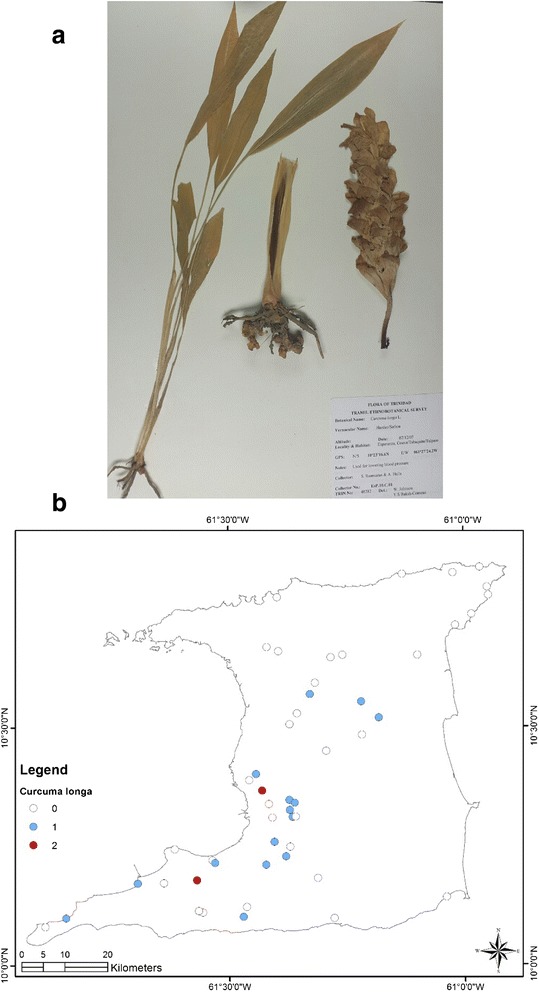
a (Top): Photograph of a voucher specimen for Curcuma longa L. Used for “afterbirth”. b (Bottom): Map of sites where Curcuma longa L. was collected. Used for “afterbirth”
Fig. 5.
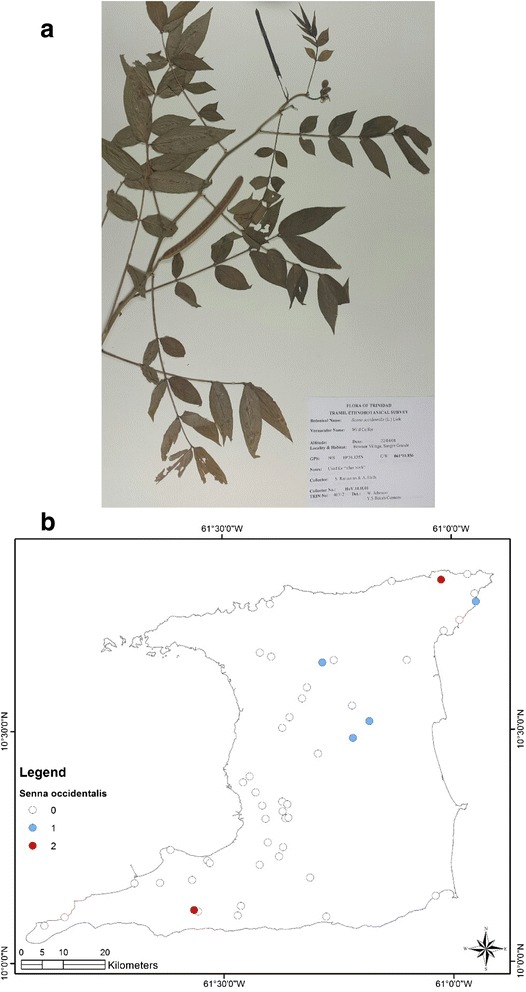
a (Top): Photograph of a voucher specimen for Senna occidentalis (L.) Link Link. Used for “afterbirth”. b (Bottom): Map of sites where Senna occidentalis (L.) Link. was collected. Used for “afterbirth”
Fig. 6.
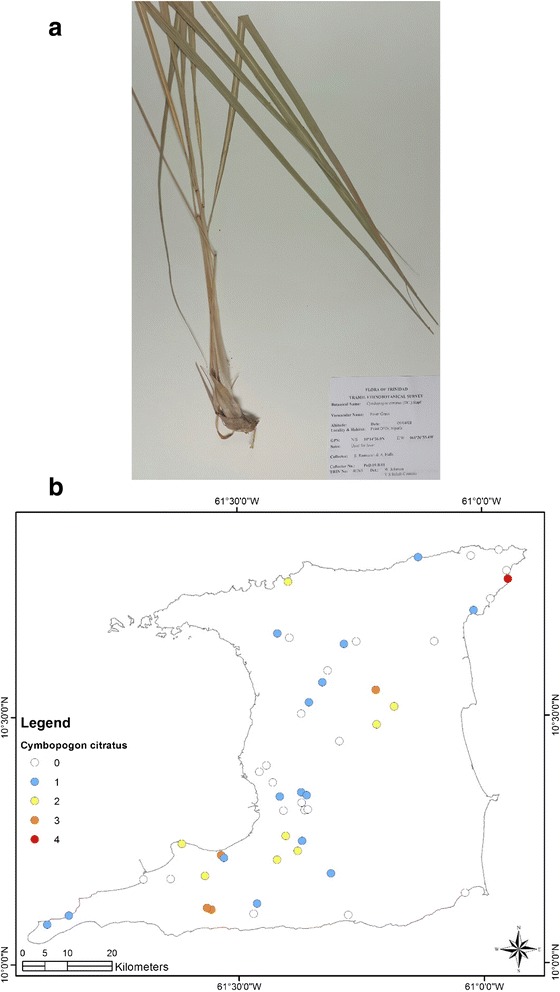
a (Top): Photograph of a voucher specimen for Cymbopogon citratus (DC.) Stapf Stapf. Used for fever. b (Bottom): Map of sites where Cymbopogon citratus (DC.) Stapf. was collected. Used for fever
Fig. 7.
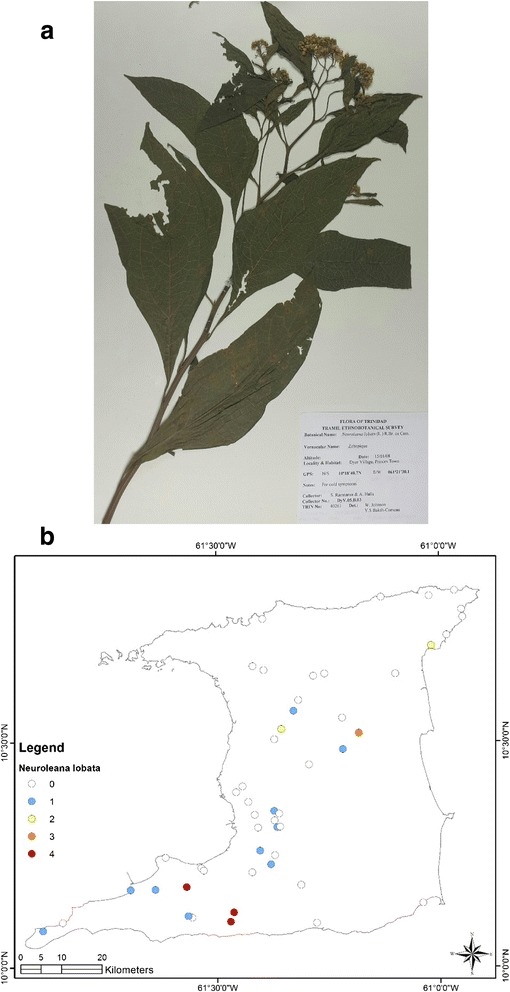
a (Top): Photograph of a voucher specimen for Neurolaena lobata (L.)R. Br. ex. Cass. Used for fever. b (Bottom): Map of sites where Neurolaena lobata (L.)R. Br. ex. Cass. was collected. Used for fever
Fig. 8.
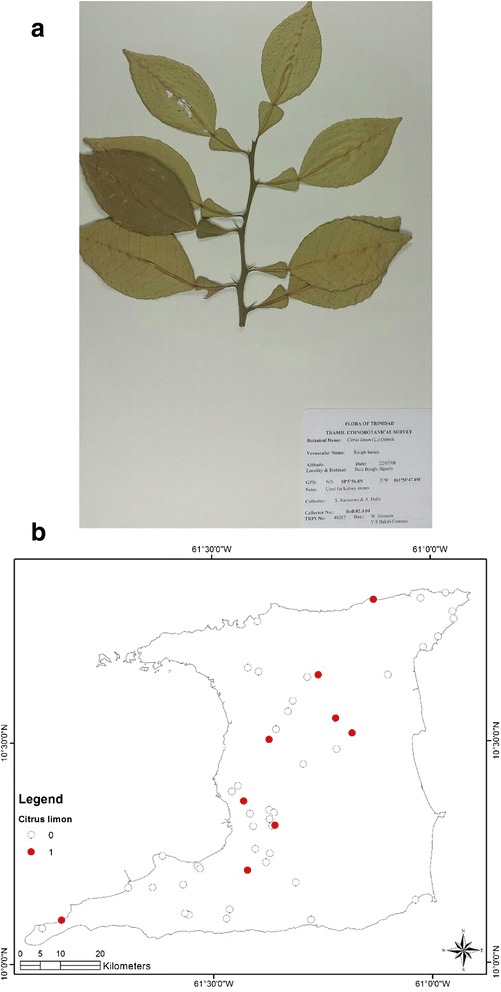
a (Top): Photograph of a voucher specimen for Citrus limon (L.) Osbeck. Used for kidney stones. b (Bottom): Map of sites where Citrus limon (L.) Osbeck. was collected. Used for kidney stones
Herbal remedies for ailments affecting the upper respiratory tract
A total of 279 persons identified herbal remedies for the treatment and management of cough/common cold. While 37 different plant species were identified, Leonotis nepetifolia turned out to be the most common with 85 citations out of 279 or 30.5 % thus applying the TRAMIL criteria it is a plant with popular use for the treatment of cough/common cold. The remedy was prepared as an aqueous infusion or decoction using fresh leaves, or the juice extracted by pounding the leaves and a teaspoon full mixed with a pinch of salt and taken orally. It was recommended that the remedy be taken for up to three days until symptomatic relief.
Only 13 respondents indicated the use of herbal remedies prepared from 11 different plant species in the treatment of asthmatic symptoms. However, the most commonly used plants were Sambucus canadensis and Bryophyllum pinnatum (2 each out of 13 citations; 15.4 %), which did not reach popular use level according to TRAMIL.
Herbal remedies for ailments affecting the genitourinary tract
Four common ailments that affected the genitourinary tract were “stoppage of water”, “womb infection”, kidney stones and “afterbirth”. “Stoppage-of-water” refers to the condition commonly known as urinary retention. This condition may arise from neurological complications or due to obstructive causes, the most common being benign prostatic hypertrophy in men and uterine fibroids in women. In our survey, 39 persons indicated the use of 17 different plant species for the treatment of “stoppage-of-water”. The most common plant used was Gomphrena globosa (17 out of 39 citations, 43.6 %) and had popular use according to TRAMIL. The remedy was made using a few flowers of the plants to make an aqueous infusion or decoction.
Sexually transmitted infections, such as Chlamydia and gonorrhea, are the most common causes of uterine or “womb” infection. Uterine infections are also more likely to occur following childbirth. In our survey, 43 persons cited the use of herbal remedies for “womb infection” with plants from 24 species; Momordica charantia was the most commonly cited plant with seven persons indicating its use (or 16.3 % of respondents). The remedy is made using a handful of leaves, attached to the vine, to make a decoction which is consumed for up to three days until the infection clears. However, none of the plants cited for use in the treatment of “womb infection” reached popular use status according to TRAMIL.
A total of 46 persons indicated the use of herbal remedies from 15 different plant species for the treatment of kidney stones. The juice of the fruit of Citrus limon was cited by 9 persons (or 19.6 %) for the treatment of kidney stones and reached popular use according to TRAMIL.
The natural expulsion of the placenta following childbirth is referred to as the “afterbirth”. However, there is a prevailing cultural belief in Trinidad that in some women the whole “afterbirth” may not be fully expelled; a similar belief held by many cultures throughout the developing world [18–21]. Therefore, herbal remedies are used to ensure the complete expulsion of the placenta and blood clots in the few days following childbirth. Postnatal vaginal bleeding and discharge containing blood clots and uterine tissue (also called lochia) occurs naturally for a few weeks following childbirth, and this may have been traditionally interpreted to mean that the whole placenta was not delivered following childbirth.
In our survey, 38 respondents cited the use of herbal remedies made from eight different plant species for the treatment of “afterbirth”. These remedies were usually taken within one week of childbirth. The most commonly used plants were Curcuma longa (17 out of 38 citations, or 44.7 %) and Senna occidentalis (8 out of 38 citations, 21.1 %) and both reached popular use status according to TRAMIL criterion. For Curcuma longa the herbal remedy was prepared using the rhizome or underground stem of the plant to make either a decoction or by pounding and extracting the juice for oral consumption. The roots of Senna occidentalis are used to make a decoction for oral administration.
Herbal remedies for chronic diseases
Diabetes mellitus and hypertension were the two common chronic diseases identified in the survey. For diabetes, there were 67 citations with plants being derived from 30 different species; Catharanthus roseus, Momordica charantia and Azadirachta indica were the most commonly cited plants for the treatment of diabetes, and were cited equally by 7 persons (10.5 % each). However, none of these plants reached significant use by TRAMIL standards.
There were 100 citations for hypertension treatment from 28 different plant species. The most commonly used plants for the treatment of hypertension were Artocarpus altilis (11 citations, or 11.0 %) and Tamarindus indica (11 citations, or 11.0 %). The yellow leaves of Artocarpus altilis were used to make either an infusion or decoction and an infusion or decoction was made using the fruit and leaves of Tamarindus indica. The remedies for diabetes and hypertension were used irregularly for symptomatic control of high blood pressure.
Herbal remedies used for ‘cooling/cleanser” and treatment of fever
The humoral medicine concept, with the “hot-cold” dichotomy, is probably one of the oldest universally held traditional beliefs of health and disease, which has been infused into traditional cultures in Latin America and the Caribbean [22, 23]. This classical humoral concept was used to describe good health as the maintenance of equilibrium between ‘hot’ and ‘cold’ elements in the body. A disruption in this balance would result in excessively ‘hot’ or excessively ‘cold’ diseases [24]. Diseases ascribed to excessive heat were treated with ‘cold’ remedies while “cold” diseases were treated with ‘hot’ remedies [25]. It was suggested by Lans [9] that in the Trinidadian context of “hot-cold” system, traditional herbal preparations were administered in accordance with the correlation between cause and effect, with “cooling/cleanser”being used as both treatment for “hot” conditions, as well as prophylaxis to bring the body "back into balance".
Although the “hot-cold” concept of disease has long been abandoned by mainstream Western biomedical science, it remains relevant in the folkloric concept of health and disease throughout the Americas. In our survey we found a large percentage of respondents indicated the use of herbal remedies for “cooling”. Most likely the use of traditional herbal remedies as “cooling/cleanser to treat certain “hot” ailments persists in present-day Trinidad as a relic of this historical “hot-cold” dichotomy of disease. In Trinidad, as in the Americas, “hot” aliments refer to conditions such as fever, constipation, rash and skin ailments, and general malaise.
We found that 38 different plant species were used as “cooling/cleanser” by 194 persons in the survey. For most of the remedies a few fresh leaves were used to make either an infusion or decoction which was consumed for a few days up to one week. Five plants accounted for a significant 59 % of the citations: Stachytarpheta jamaicensis (36 citations or 18.0 %), Senna alata (26 citations or 13.0 %), Momordica charantia (21 citations or 10.5 %), Tournefortia hirsutissima (20 citations or 10.0 %) and Peperomia pellucida (15 citations or 7.5 %). However, none of these plants reached popular use status according to TRAMIL requirement.
There were 98 citations for the treatment of fever with 21 plant species being identified. Two plants, Cymbopogon citratus (30 out of 98 citations, 30.6 %) and Neurolaena lobata (46 out of 98 citations, 46.9 %) accounted for most of the citations. Most of the herbal remedies for fever were made using a few leaves of the plant to prepare either an infusion or decoction, which was consumed for a few days until the fever subsided.
Discussion
To our knowledge this is the first systematic ethnobotanical study done in Trinidad to determine the extent of traditional use of medicinal plants throughout several rural communities on the island. This study is significant in that it covered fifty remote communities with a sufficiently large sample size to assess the distribution of medicinal plant use for common ailments. We used the validated TRAMIL survey instrument which allowed us to determine herbal ‘home remedies’ use among these rural communities. Although we limited the number of ailments, for practical considerations, we were able to gather a wealth of information on several plants, including methods of preparation and mode and frequency of administration.
There were notable differences between our findings and that obtained in earlier surveys. Almost 40 years ago, Wong [6] identified 186 different medicinal plants from his interviews with 70 villagers at a remote community for a wide range of ailments, but only 52 of these plants had similar traditional use compared to our survey; and none were used for kidney stones or asthma. In the more extensive survey by Seaforth and colleagues across 18 rural communities [8], although 78 plants were identified, only 28 of these plants had similar traditional use compared to our survey; and none were used for kidney stones, “stoppage-of-water” or “afterbirth”. The more recent survey by Lans cited 24 plants used for “cooling/cleanser” [9], but just 11 of these plants had similar use compared to our survey.
The surveys by Clement and colleagues [10–12] focused on the complementary use of herbal remedies in patients with chronic diseases attending modern primary public healthcare facilities. Although some commonly cited plants such as Leonotis nepetifolia, Zingiber officinale, Cymbopogon citratus and Aloe vera were also found in our survey, the use of herbal remedies for culture-bound health issues such as “afterbirth”, “stoppage-of-water” and “womb infection” was notably absent. In our setting, this observation partly supports our initial assumption that there are rural–urban differences in retention of traditional knowledge and use of herbal remedies.
Although medico-cultural concepts such as “stoppage-of-water”, “womb infection” and “afterbirth” could be explained by modern medicine, and conventional therapies are available for treatment, people in remote communities may still prefer to rely on generations-old traditions as their preferred mode of treatment. The cultural interpretation of these aliments and conditions may differ from that proposed by modern medicine, and generations of anecdotal evidence would be having a significant impact on the continuation of these rural traditions.
It would be problematic to conceptualize the use of “cooling/cleanser” as prophylaxis in modern medicine, as the “hot-cold” dichotomy of health and disease has long been abandoned. But, surprisingly, “cooling” was among the most popular indications for medicinal plant use in rural Trinidad. The maintenance and restoration of the “hot-cold” balance in the body seems to resonate among rural communities across the developing world, and point to similarities in the origin of cultural beliefs regarding health and disease.
A major objective of our survey was to determine whether relevant pharmacological evidence existed that would support the traditional use of medicinal plants with significant (popular) use in our setting. A preliminary review of the literature shows that there was very sparse clinical evidence. However, we provide in the rest of this discussion the limited evidence from studies conducted in cell cultures (in vitro), isolated tissues (ex vivo) and laboratory animals (in vivo) which may lend support to their traditional use.
Leonotis nepetifolia was the most commonly cited plant being used to treat an array of conditions, including fever, common cold/cough, “cooling”, diabetes and asthma; and, the literature is sparse regarding its biological activity. In an ex vivo model the aqueous extract of the leaves of L. nepetifolia produced relaxation of pre-contracted guinea-pig tracheal rings but only at relatively high concentrations of 1000 μg/mL and this may lend support for its traditional use in the treatment of asthma [26].
Neurolaena lobata was the second most commonly cited plant in our survey, and was used to treat fever, the common cold/cough, diabetes and “womb infection”. The infusion, made from the leaves, is very bitter-tasting and is commonly used throughout the Caribbean and Latin America for fever, colds, malaria, ‘painful belly pains’, painful menstruation and even diabetes [27]. Toxicity studies in mice have demonstrated safety in an animal model at aqueous oral doses up to 5,000 mg/kg [28].
The literature provides pre-clinical evidence to support the biological activity for several extracts of Neurolaena lobata against infectious organisms, including protozoa, malaria parasite, fungi and filarial worms. The aqueous and lipophilic extracts, and isolated sesquiterpene lactones were active in vitro against Plasmodium falciparium (the parasite responsible for malaria) [29]. The methanol extract significantly reduced parasitemias in Plasmodium berghei-infected mice and was active against both chloroquine-susceptible and resistant P. falciparum strains [30]. Crude, hexane and ethanol extracts significantly inhibited both trypomastigote and epimastigote developmental forms of Trypanosoma cruzi [31, 32]. Extracts, fractions and isolated sesquiterpenes lactones significantly inhibited parasite growth of Leishmania mexicana, L. cruzi and L. vaginalis [33]. The ethanol extract exhibited a significant macrofilaricidal effect against Brugia pahangi (a lymphatic dwelling filiarial worm) in a concentration- and time-dependent manner [34]. Bioassay-guided fractionation of N. lobata demonstrated its weak to moderately active antifungal activity [35]. Additionally, the leaf extracts possessed anti-inflammatory properties in an in vitro LPS-stimulated monocyte model [36, 37] and analgesic properties in in vivo models for pain [28]. However, there is no clinical data to support the use of this plant for any of the traditional uses in Trinidad.
Cymbopogon citratus was the most frequently cited plant for fever, and was used to a lesser extent for the treatment of common cold/cough and as “cooling”. The essential oils of Cymbopogon citratus demonstrated significant analgesic and anti-inflammatory properties [38]. Other pre-clinical studies show that the aqueous extract and the essential oils of C. citratus possess considerable anti-inflammatory properties [39–42]. Although Carlini and colleagues [42] reported that an aqueous extract of C. citratus was not effective in reducing body temperature in hyperthermic mice at a dose 40 times higher than that normally used in traditional preparations, a more recent study by a group led by Ghenou [43] showed that the essential oils demonstrated strong antipyretic effects similar to a conventional analgesic agent.
Curcuma longa was the most commonly cited herb in our survey for the treatment of “afterbirth”. Although thousands of papers have been published regarding the biological properties of Curcuma longa, and its purified constituent curcumin, very little is reported regarding its use or efficacy to support its use in the postpartum period. A single study by Itthipanichong and colleagues [44] showed that curcuminoids produced a dose-dependent relaxation of oxytocin-induced contractions in isolated rat uterus. However, this ex vivo study does not support the traditional use of C. longa where it would be expected that it would cause an increase in uterine contraction to expel remnants of the “afterbirth”. However, several in vitro studies show that C. longa extracts and curcuminoids possess potent antibacterial, antifungal and antiviral properties [45] which may be beneficial during the postpartum period when there is an increased likelihood of genitourinary infections.
Our review of the literature revealed there are no reports regarding the effects of Senna occidentalis extracts on the uterus that could be extrapolated to its usefulness in the postnatal period. Furthermore, there is limited pre-clinical evidence regarding the antimicrobial activity of S. occidentalis [46]. Similarly, there were no reports regarding whether extracts of Spondias mombin had any effect on uterine contractility; however, there were reports that plant extracts possessed wide spectrum antibacterial properties in vitro [47, 48]. Although the literature does not provide evidence for the use of these plants as spasmogenic agents to expel the “afterbirth”, it may be possible that their use may be inadvertently providing antimicrobial coverage as uterine infections are common following childbirth.
The juice of Citrus limon was most commonly used in the management of kidney stones and several clinical studies have supported the use of lemonade to reduce the recurrence of calcium oxalate kidney stones by increasing urinary citrate levels [49–52]. Although Gomphrena globosa was the most commonly used plant for “stoppage-of-water” or urinary retention and kidney stones there were no pre-clinical or clinical reports in the literature to support any of these traditional uses.
Although the literature shows limited pre-clinical evidence to demonstrate pharmacological activities for some of the plants cited in our survey, this must be taken cautiously, as this level of evidence does not represent the reality in the traditional use setting. Firstly, the pre-clinical evidence comes from studies utilizing solvent extracts, fractions, or isolated compounds which are not the modality traditionally used. Secondly, the concentrations of putative components in these solvent extracts, fractions or isolated compounds used in pre-clinical experiments may be significantly higher than that which could be attained following oral administration, thus making the extrapolations to the clinical setting unjustified. However, there are a few promising examples, such as Senna (an FDA-approved non-prescription laxative) which has been clinically proven to be efficacious. A similar approach is needed to determine the clinical efficacy of other herbal remedies.
However, the identification of these medicinal plants provides a platform from which further pre-clinical and clinical studies could be formulated to determine the efficacy and safety of herbal preparations. These research efforts may provide alternative and/or complementary approaches for healthcare provision in the Caribbean and beyond.
Conclusion
We were able to achieve our objectives and identify medicinal plants used for the most common ailments across a wide cross-section of rural communities in Trinidad. These findings add to the body of work previously done on the island, and should provide a platform for more focused surveys in the future. Our survey showed significant retention of traditional knowledge of medicinal plants in rural Trinidad. More interestingly, a large remnant of medico-cultural concepts such as “cooling/cleanser”, “afterbirth”, “stoppage-of-water” and “womb infection” persist in the rural population. Although the scientific literature show that some of the cited plants possessed antimicrobial, anti-inflammatory and related pharmacological activities in laboratory studies, these results must be taken with caution until clinical trials are conducted to establish safety and efficacy.
Acknowledgements
The authors wish to express their gratitude for the funding received from the Trinidad and Tobago Health Sciences Initiative under the auspices of the University of Trinidad and Tobago. We are thankful to our field researchers Mr. P. Mark, Ms. Alicia Halls and Mr. Steve Ramsaran for the professional manner in which they conducted the interviews, collected plant specimens and data input. Ms. Sharon Laurent for data entry and analysis. Mr. Winston Johnson, research technician, at the National Herbarium of Trinidad and Tobago for initially identifying the specimens by their scientific names. We also thank Mr. Terry Sampson for photographing the voucher specimens for significant plants and Mr. Hamish Asmath for the construction of GPS maps for sites visited and significant plants.
Appendix 1
TRAMIL sample survey questionnaire
Treatments used for: (local name of the problem)
Illness description (in basic English):
First treatments (the last time the problem has come out in the family):
___ traditional medicinal plants
___ healer or witch doctor
___ medical officer
Description and way of preparation of the remedy:
How did you take the remedy, in what quantity and how many times?:
Where did you find the plants?
___ yard
___ not at home
Have you already used this remedy?
___ Yes
___ No
Which results have you obtained?
What precautions should be observed during treatment?
(contraindications & side effects)
And for the children?
(contraindications and directions for use)
Available at: http://www.tramil.net/english/TramilModelo.html
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YC was involved in the initial design of the study, and training of the field researchers. He also spearheaded data analysis and drafting of the manuscript. YB-C contributed to guiding the botanical field survey, the identification of the plants in the herbarium and editing the manuscript. CS contributed to the data analysis, literature searches and reading and approving the manuscript. All authors read and approved the final manuscript.
Contributor Information
Y. N. Clement, Phone: 1-868-663-8613, Email: Yuri.Clement@sta.uwi.edu
Y. S. Baksh-Comeau, Email: yasmin.baksh-comeau@sta.uwi.edu
C. E. Seaforth, Email: ceseaforth@gmail.com
References
- 1.Trinidad and Tobago 2011 Population and Housing Census Report [http://cso.planning.gov.tt/sites/default/files/content/images/census/TRINIDAD%20AND%20TOBAGO%202011%20Demographic%20Report.pdf]. Accessed 15 March 2015.
- 2.Ahmad N. Soils of the Caribbean. Jamaica: Ian Randle Publishers; 2011. [Google Scholar]
- 3.Trinidad and Tobago Diversity. [http://www.biodiversity.gov.tt/home/trinidad-a-tobago-biodiversity.html]. Accessed 15 March 2015.
- 4.Simpson GE. Folk medicine in Trinidad. J Am Folk. 1962;75(298):326–40. doi: 10.2307/538368. [DOI] [Google Scholar]
- 5.Mischel F. Faith healing and medical practice in the southern Caribbean. Southwest J Anthropol. 1959;15:407–17. [Google Scholar]
- 6.Wong W. Some folk medicinal plants from Trinidad. Econ Bot. 1976;30:103–42. doi: 10.1007/BF02862958. [DOI] [Google Scholar]
- 7.Clement Y. Herbal medicine practices in the Caribbean. In: Sutherland P, Moodley P, Chevannes B, editors. Caribbean Healing Traditions – Implications for health and mental health. New York: Routledge, Taylor & Francis; 2014. pp. 52–61. [Google Scholar]
- 8.Seaforth CE, Adams CD, Sylvester Y. A guide to the medicinal plants of Trinidad & Tobago. London: Commonwealth Secretariat; 1983. [Google Scholar]
- 9.Lans C. Ethnomedicines used in Trinidad and Tobago for urinary problems and diabetes mellitus. J Ethnobio Ethnomed. 2006;2:45. doi: 10.1186/1746-4269-2-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clement YN, Williams AF, Aranda D, Chase R, Watson N, Mohammed R, et al. Medicinal herb use among asthmatic patients attending a specialty care facility in Trinidad. BMC Complement Altern Med. 2005;5:3. doi: 10.1186/1472-6882-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clement YN, Morton-Gittens J, Basdeo L, Blades A, Francis MJ, Gomes N, et al. Perceived efficacy of herbal remedies by users accessing primary healthcare in Trinidad. BMC Complement Altern Med. 2007;7:4. doi: 10.1186/1472-6882-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clement YN. Herbal self-medication at primary health care facilities in Trinidad. J Altern Complement Med. 2009;15(1):6–7. doi: 10.1089/acm.2008.0295. [DOI] [PubMed] [Google Scholar]
- 13.Pardo-de-Santayana M, Pieroni A, Puri RK, editors. Ethnobotany in the New Europe: People Health and Wild Pland Resources. New York: Berghahn Books; 2013. [Google Scholar]
- 14.Chew-Chung WA. Many paths to health: A study of 2,000 rural and urban Taiwan families. Am J Chin Med. 1980;8:313. doi: 10.1142/S0192415X8000030X. [DOI] [PubMed] [Google Scholar]
- 15.Adams J, Sibbritt D, Broom A, Loxton D, Pirotta M, Humphreys J, et al. A comparison of complementary and alternative medicine users and use across geographical areas: A national survey of 1,427 women. BMC Complement Altern Med. 2011;11:85. doi: 10.1186/1472-6882-11-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robineau L, Saejarto DD. TRAMIL: a research project on the medicinal resources of the Caribbean. In: Balick MJ, Elizabetski E, Laird SA, editors. Medicinal Resources of the Tropical Forest (Biodiversity and its importance to Human Health) New York: Columbia University Press; 1986. pp. 317–25. [Google Scholar]
- 17.Elections and Boundaries Commission, Government of Trinidad and Tobago [http://www.ebctt.com/index.php]. Accessed 15 March 2015.
- 18.van Andel T, de Boer HJ, Barnes J, Vandebroek I. Medicinal plants used for menstrual disorders in Latin America, the Caribbean, sub-Saharan Africa, south and Southeast Asia and their uterine properties: A review. J Ethnopharmacol. 2014;155:992–1000. doi: 10.1016/j.jep.2014.06.049. [DOI] [PubMed] [Google Scholar]
- 19.de Boer HJ, Cotingting C. Medicinal plants for women’s healthcare in southeast Asia: A meta-analysis of their traditional use, chemical constituents, and pharmacology. J Ethnopharmacol. 2014;151:747–67. doi: 10.1016/j.jep.2013.11.030. [DOI] [PubMed] [Google Scholar]
- 20.Zumsteg IS, Weckerle CS. Bakera, a herbal steam bath for postnatal care in Minahasa (Indonesia): Documentation of the plants used and assessment of the method. J Ethnopharmacol. 2007;111:641–50. doi: 10.1016/j.jep.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 21.Kaingu CK, Oduma JA, Kanui TI. Practices of traditional birth attendants in Machakos district, Kenya. J Ethnophramacol. 2011;137:495–502. doi: 10.1016/j.jep.2011.05.044. [DOI] [PubMed] [Google Scholar]
- 22.Foster GM. Humoral traces in United States folk medicine. Med Anthropol Newsl. 1979;10(2):17–20. doi: 10.1525/maq.1979.10.2.02a00130. [DOI] [Google Scholar]
- 23.Foster GM. The validating role of humoral theory in traditional Spanish-American therapeutics. Am Anthropol. 1988;15(1):120–35. [Google Scholar]
- 24.Jackson WA. A short guide to humoral medicine. TiPs. 2001;22(9):487–9. doi: 10.1016/s0165-6147(00)01804-6. [DOI] [PubMed] [Google Scholar]
- 25.Schoental R. Herbal medicines and disease. J Trop Ped. 1957;2(4):208. doi: 10.1093/oxfordjournals.tropej.a057439. [DOI] [PubMed] [Google Scholar]
- 26.Calixto JB, Yunes RA, Rae GA. Effect of crude extracts from Leonotis nepetaefolia (Labiatae) on rat and guinea-pig smooth muscle and rat cardiac muscle. J Pharm Pharmacol. 1991;43(8):529–34. doi: 10.1111/j.2042-7158.1991.tb03531.x. [DOI] [PubMed] [Google Scholar]
- 27.Hawthorne WD, Jules D, Marcelle G. Caribbean Spice Islands Plants. Oxford: Oxford Forestry Institute; 2004. [Google Scholar]
- 28.Gracioso JS, Paulo MQ, Hiruma Lima CA, Souza Brito AR. Antinociceptive effect in mice of a hydroalcoholic extract of Neurolaena lobata (L.) R. Br. and its organic fractions. J Pharm Pharmacol. 1998;50(12):1425–9. doi: 10.1111/j.2042-7158.1998.tb03370.x. [DOI] [PubMed] [Google Scholar]
- 29.François G, Passreiter CM, Woerdenbag HJ, Van Looveren M. Antiplasmodial activities and cytotoxic effects of aqueous extracts and sesquiterpene lactones from Neurolaena lobata. Planta Med. 1996;62(2):126–9. doi: 10.1055/s-2006-957833. [DOI] [PubMed] [Google Scholar]
- 30.Franssen FF, Smeijsters LJ, Berger I, Medinilla Aldana BE. In vivo and in vitro antiplasmodial activities of some plants traditionally used in Guatemala against malaria. Antimicrob Agents Chemother. 1997;41(7):1500–3. doi: 10.1128/aac.41.7.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berger I, Barrientos AC, Cáceres A, Hernández M, Rastrelli L, Passreiter CM, et al. Plants used in Guatemala for the treatment of protozoal infections: II. Activity of extracts and fractions of five Guatemalan plants against Trypanosoma cruzi. J Ethnopharmacol. 1998;62(2):107–15. doi: 10.1016/S0378-8741(98)00011-7. [DOI] [PubMed] [Google Scholar]
- 32.Cáceres A, López B, González S, Berger I, Tada I, Maki J. Plants used in Guatemala for the treatment of protozoal infections. I. Screening of activity to bacteria, fungi and American trypanosomes of 13 native plants. J Ethnopharmacol. 1998;62(3):195–202. doi: 10.1016/S0378-8741(98)00140-8. [DOI] [PubMed] [Google Scholar]
- 33.Berger I, Passreiter CM, Cáceres A, Kubelka W. Antiprotozoal activity of Neurolaena lobata. Phytother Res. 2001;15(4):327–30. doi: 10.1002/ptr.782. [DOI] [PubMed] [Google Scholar]
- 34.Fujimaki Y, Kamachi T, Yanagi T, Cáceres A, Maki J, Aoki Y. Macrofilaricidal and microfilaricidal effects of Neurolaena lobata, a Guatemalan medicinal plant, on Brugia pahangi. J Helminthol. 2005;79(1):23–8. doi: 10.1079/JOH2004262. [DOI] [PubMed] [Google Scholar]
- 35.Lentz DL, Clark AM, Hufford CD, Meurer-Grimes B, Passreiter CM, Cordero J, et al. Antimicrobial properties of Honduran medicinal plants. J Ethnopharmacol. 1998;63(3):253–63. doi: 10.1016/S0378-8741(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 36.Lajter I, Vasas A, Béni Z, Forgo P, Binder M, Bochkov V, et al. Sesquiterpenes from Neurolaena lobata and their antiproliferative and anti-inflammatory activities. J Nat Prod. 2014;77(3):576–82. doi: 10.1021/np400834c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Walshe-Roussel B, Choueiri C, Saleem A, Asim M, Caal F, Cal V, et al. Potent anti-inflammatory activity of sesquiterpene lactones from Neurolaena lobata (L.) R. Br. ex Cass., a Q'eqchi' Maya traditional medicine. Phytochemistry. 2013;92:122–7. doi: 10.1016/j.phytochem.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 38.Brito RG, Guimarães AG, Quintans JS, Santos MR, De Sousa DP, Badaue-Passos D, Jr, et al. Citronellol, a monoterpene alcohol, reduces nociceptive and inflammatory activities in rodents. J Nat Med. 2012;66(4):637–44. doi: 10.1007/s11418-012-0632-4. [DOI] [PubMed] [Google Scholar]
- 39.Sforcin JM, Amaral JT, Fernández A, Jr, Sousa JP, Bastos JK. Lemongrass effects on IL-1beta and IL-6 production by macrophages. Nat Prod Res. 2009;23(12):1151–9. doi: 10.1080/14786410902800681. [DOI] [PubMed] [Google Scholar]
- 40.Figueirinha A, Cruz MT, Francisco V, Lopes MC, Batista MT. Anti-inflammatory activity of Cymbopogon citratus leaf infusion in lipopolysaccharide-stimulated dendritic cells: contribution of the polyphenols. J Med Food. 2010;13(3):681–90. doi: 10.1089/jmf.2009.0115. [DOI] [PubMed] [Google Scholar]
- 41.Mitoshi M, Kuriyama I, Nakayama H, Miyazato H, Sugimoto K, Kobayashi Y, et al. Suppression of allergic and inflammatory responses by essential oils derived from herbal plants and citrus fruits. Int J Mol Med. 2014;33(6):1643–51. doi: 10.3892/ijmm.2014.1720. [DOI] [PubMed] [Google Scholar]
- 42.Carlini EA, de DP CJ, Silva-Filho AR, da Silveira-Filho NG, Frochtengarten ML, Bueno OF. Pharmacology of lemongrass (Cymbopogon citratus Stapf). I. Effects of teas prepared from the leaves on laboratory animals. J Ethnopharmacol. 1986;17(1):37–64. doi: 10.1016/0378-8741(86)90072-3. [DOI] [PubMed] [Google Scholar]
- 43.Ghenou JD, Ahounou JF, Akakpo HB, Laleye A, Yayi E, Gbaguidi F, et al. Phytochemical composition of Cymbopogon citratus and Eucalyptus citriodora essential oils and their anti-inflammatory and analgesic properties on Wistar rats. Mol Biol Rep. 2013;40(2):1127–34. doi: 10.1007/s11033-012-2155-1. [DOI] [PubMed] [Google Scholar]
- 44.Itthipanichpong C, Ruangrungsi N, Kemsri W, Sawasdipanich A. Antispasmodic effects of curcuminoids on isolated guinea-pig ileum and rat uterus. J Med Assoc Thai. 2003;86(Suppl 2):299–309. [PubMed] [Google Scholar]
- 45.Moghadamtousi SZ, Kadir HA, Hassandarvish P, Tajik H, Abubakar S, Zandi K. A review on antibacterial, antiviral, and antifungal activity of curcumin. Biomed Res Int. 2014;2014:186864. doi: 10.1155/2014/186864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Samy RP, Ignacimuthu S. Antibacterial activity of some folklore medicinal plants used by tribals in Western Ghats of India. J Ethnopharmacol. 2000;69(1):63–71. doi: 10.1016/S0378-8741(98)00156-1. [DOI] [PubMed] [Google Scholar]
- 47.Abo KA, Ogunleye VO, Ashidi JS. Antimicrobial potential of Spondias mombin, Croton zambesicus and Zygotritonia crocea. Phytother Res. 1999;13(6):494–7. doi: 10.1002/(SICI)1099-1573(199909)13:6<494::AID-PTR490>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 48.Corthout J, Pieters L, Claeys M, Geerts S, Vanden Berghe D, Vlietinck A. Antibacterial and molluscicidal phenolic acids from Spondias mombin. Planta Med. 1994;60(5):460–3. doi: 10.1055/s-2006-959532. [DOI] [PubMed] [Google Scholar]
- 49.Tosukhowong P, Yachantha C, Sasivongsbhakdi T, Ratchanon S, Chaisawasdi S, Boonla C, et al. Citraturic, alkalinizing and antioxidative effects of limeade-based regimen in nephrolithiasis patients. Urol Res. 2008;36(3-4):149–55. doi: 10.1007/s00240-008-0141-9. [DOI] [PubMed] [Google Scholar]
- 50.Penniston KL, Steele TH, Nakada SY. Lemonade therapy increases urinary citrate and urine volumes in patients with recurrent calcium oxalate stone formation. Urology. 2007;70(5):856–60. doi: 10.1016/j.urology.2007.06.1115. [DOI] [PubMed] [Google Scholar]
- 51.Kang DE, Sur RL, Haleblian GE, Fitzsimons NJ, Borawski KM, Preminger GM. Long-term lemonade based dietary manipulation in patients with hypocitraturic nephrolithiasis. J Urol. 2007;177(4):1358–62. doi: 10.1016/j.juro.2006.11.058. [DOI] [PubMed] [Google Scholar]
- 52.Seltzer MA, Low RK, McDonald M, Shami GS, Stoller ML. Dietary manipulation with lemonade to treat hypocitraturic calcium nephrolithiasis. J Urol. 1996;156(3):907–9. doi: 10.1016/S0022-5347(01)65659-3. [DOI] [PubMed] [Google Scholar]


