Abstract
This study examines trends in adolescent substance use disorders (SUDs) and treatment utilization in the US using data from the National Household Survey on Drug Use and Health (NSDUH) and data from the National Survey of Substance Abuse Treatment Services (N-SSATS). Results indicate an overall decrease in the percent of adolescents meeting past year criteria for an alcohol or illicit drug disorder between 2003 and 2010, but the percent of adolescents meeting criteria who had not received any treatment in the past year was substantial and has remained stable since 2003. In 2010, less than 30% of facilities participating in the N-SSATS survey indicated that they offered special programming for adolescents, reflecting an overall decrease since 2003.
Keywords: substance use disorders, adolescents, adolescent substance abuse treatment
Introduction
Early initiation of alcohol or drug use is often associated with the development of substance use disorders (SUDs; Anthony & Petronis, 1995; Grant & Dawson, 1997; Hingson, Heeren, & Edwards, 2008; Hingson & Zha, 2009; Winters & Lee, 2008), defined as meeting diagnostic criteria for abuse or dependence on alcohol, illicit drugs, or alcohol or illicit drugs. Recent findings from the 2009 National Household Survey on Drug Use and Health (NSDUH) indicate that approximately 7% of adolescents in the US met DSM-IV criteria for an alcohol or illicit drug disorder in the past year (SAMHSA, 2010b), representing over 1.7 million youth age 12-17 (SAMHSA, 2010a). Preventing or delaying substance use initiation is critical for mitigating the development of SUDs. However, for many adolescents (ages 12-17) who already meet criteria, services are needed to treat the disorder and related health and social consequences (Brook, Richter, & Rubenstone, 2000; Daudin et al., 2010; Green, Doherty, Stuart, & Ensminger, 2010; Hingson, et al., 2008; Hingson & Zha, 2009; Newcomb, 1997). Unfortunately, many adolescents who need substance abuse treatment never receive it (SAMHSA, 2010b).
When SUDs in adolescents go untreated, they can raise the risk of several adverse consequences, including escalation in the severity of the disorder (e.g., transition from abuse to dependence), motor vehicle accidents, violent events, and high risk sexual behavior (Chung & Martin, 2011; Steinberg, 2004; Weinberg, Rahdert, Colliver, & Glantz, 1998). Moreover, high levels of substance use are associated with the three leading causes of death among youth: accidents, homicide and suicide (Clark & Winters, 2002). Other studies have shown that the persistence of SUDs can also be associated with either the aggravation of or the development of other childhood or adolescent disorders, such as major depressive disorders, anxiety disorders, conduct disorders and ADHD (Kaminer & Bukstein, 2008).
Although it is widely accepted that adolescent–specific treatment is needed, many substance abuse treatment providers do not offer adolescent-specific programs. Data from the 2003 National Survey of Substance Abuse Treatment Services (N-SSATS) indicated that while 52% of facilities admitted adolescent clients , only 32% of all facilities offered “programs or groups” for adolescents (SAMHSA, 2004), a proxy for adolescent-specific treatment. In other words, less than one-in-three substance abuse treatment providers offer services that may be appropriate for this age group.
While these “point-in-time” data are discouraging, an examination of trends might suggest that there has been improvement or suggest factors that might be related to it. Unfortunately, we lack comprehensive information regarding trends in the need for, use of, and availability of substance abuse treatment for adolescents, so we know little about whether the adolescent treatment system is currently improving, worsening, or static. For example, the NSDUH provides national estimates on the use of alcohol and various drugs and receipt of treatment for substance use and can be used to estimate the overall gap between those who need treatment and those who receive it, but the most recent report highlighting trends in need for and use of substance abuse treatment for adolescents using this data or any other national data set examined trends up to 2008 (Ilgen et al 2011; SAMHSA, 2008). The N-SSATS data has been previously used to examine the availability of substance abuse treatment for adolescents (Mark et al., 2006; Olmstead & Sindelar, 2004; SAMHSA, 2004), but these studies did not examine trends nor could we find any published reports examining trends in the need for/use of substance abuse treatment and the availability of it using both the NSDUH and the N-SSATS data.
To fill this gap in the literature, the current study had two purposes. First, we examined trends between 2003-2010 in the prevalence of past year SUDs and treatment received in the past year among adolescents in the US using NSDUH data. Second, for the corresponding time period, we documented trends in the provision of adolescent treatment in the US using N-SSATS data. Our analyses begin in 2003 due to differences in how questions about services for special populations, like adolescents, were asked in the N-SSATS survey prior to 2003.
Methods
This study involves the analysis of publicly available datasets downloaded from the Inter-university Consortium for Political and Social Research (ICPSR) website. Data were used in accordance to terms and conditions of a standard Restricted Data Use Agreement and the study was approved by the Treatment Research Institute Institutional Review Board.
The National Survey of Drug Use and Health (NSDUH)
Data on the prevalence of SUDs among adolescents were derived from the National Household Survey on Drug Use and Health (NSDUH), an annual, nationwide survey involving interviews with approximately 70,000 randomly selected non-institutionalized individuals in the US ages 12 and older collected and prepared for release by the Research Triangle Institute. Since 2003, response rates for screener have been at 89% or higher and for the computer-assisted portion of the survey at 74% or higher. In the NSDUH survey, adolescent and adult respondents are asked about the use alcohol and illicit drugs (including nonmedical prescription drug use) and treatment received for problems with these substances. If respondents report using a substance in the past year (and on more than five days in the past year for alcohol and marijuana) they are asked questions that correspond to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for past year disorders.
The National Survey of Substance Abuse Treatment Services (N-SSATS)
The National Survey of Substance Abuse Treatment Services (N-SSATS) collects information annually from all known facilities in the U.S., both public and private, that provide substance abuse treatment. As such, it provides a mechanism for quantifying the character and composition of the US substance abuse treatment delivery system from year to year. Data are collected by Mathematica Policy Research and prepared for release by Synectics for Management Decisions, Inc. The N-SSATS survey collects data about facilities, not individual clients. Data is collected by mail, phone, and web-based questionnaire. Response rates among eligible facilities are generally high, ranging from 93% to 97% since 2003. In contrast to the NSDUH survey, the N-SSATS is largely a point-prevalence survey, providing information on the substance abuse treatment system and its clients on a particular reference date (March 31st) in the data collection year. Data are routinely collected on topics such as the types of services offered and number of clients (total and under age 18) served on the reference date.
Measures
We used the NSDUH data to examine trends in the need for and receipt of substance abuse treatment. We tracked trends in the percent of US adolescents meeting past-year DSM-IV criteria for an alcohol, illicit drug (e.g., marijuana, hallucinogens, inhalants, cocaine, or heroin, or nonmedical use of psychotherapeutics, such as tranquilizers, pain relievers, sedatives, or stimulants), or alcohol or illicit drug disorder (abuse or dependence). We also tracked trends in the receipt of treatment (for alcohol, drugs, and for alcohol or drugs) in the past year at any facility and at specialty facilities. In the NSDUH, treatment refers to treatment or counseling provided at any location designed to help reduce or stop substance use and includes detoxification and any other treatment for medical problems associated with substance use. Specialty treatment is defined in the NSDUH as treatment received at any of the following types of facilities: hospitals (inpatient only), drug or alcohol rehabilitation facilities (inpatient or outpatient), or mental health centers. It does not include treatment at an emergency room, private doctor's office, self-help group, prison or jail, or hospital as an outpatient. Receipt of treatment at any facility in the past year includes receipt of specialty treatment or treatment received in any of these other settings1. We also examined the percent of adolescents with SUDs who did not receive treatment at any location (specialty or otherwise).
The N-SSATS survey asks about the type and nature of services provided by the facility being surveyed as well as estimates of the number of clients (including those under 18) served on the reference date of the survey. With respect to services for adolescents, survey respondents are queried to determine whether their facility accepts adolescents and if so, whether it offers specially designed programming or groups for adolescents. In our analyses, we recoded logical skips resulting from facilities not accepting adolescents as “No” to offering a special program or group for adolescents . The N-SSATS survey also asks respondents to provide counts for clients receiving different types of services (i.e., hospital, residential, and outpatient) on a particular reference date each year and to indicate how many of those clients served were under 18. The public use datasets contain a variable that represents the total number of clients under 18 served by each responding facility on the reference day for that year. We used this variable to designate programs that served anyone under 18 and programs that served 10 or more individuals under 18. The cutoff of 10 has been used in prior studies (Mark et al., 2006) because serving 10 or more adolescents would increase the chances that a facility would have developed specialized treatment services for adolescents.
Statistical Methods
Descriptive epidemiologic techniques (Bowling, 1997; Rothman, 1986) were used to generate yearly estimates for various parameters in the NSDUH and N-SSATS data from 2003 to 2010. All NSDUH estimates were weighted. The person-level analysis weight is the product of 15 weight components. Each weight component accounts for either a selection probability at a selection stage or an adjustment factor adjusting for nonresponse, coverage, or extreme weights. Estimates for each year were produced using a weighted cross tabulation commands (e.g., svy: tab) in Stata (StataCorp, 2009) using Taylor-series linearization to compute variances; strata with single sampling units treated as certainty units. We tested differences from year to year (e.g., percent in 2003 versus the percent in 2004) and from 2003 to the most recent year (e.g., 2010). Analysis of the N-SSATS data proceeded in a similar way, however, our analyses were not weighted. Chi-Square analyses were used to test differences in parameter estimates from year to year (e.g., percent in 2003 versus the percent in 2004) and from 2003 to the most recent year (e.g., 2010).
Results
Trends in Adolescent SUDs
Table 1 displays trends in the past-year prevalence of SUDs among 12-17 year olds from 2003-2010. In any year between 2003 and 2010, anywhere from 7-9% of adolescents in the US met criteria for an alcohol or illicit drug disorder. During this time period, there was a statistically significant decline in the percent of adolescents with any substance use disorder (9.0% v. 7.3%) and any alcohol disorder (6.0% v. 4.6%). As a group, illicit drug use disorders dropped significantly between 2004 and 2005, with significant declines in heroin and psychotherapeutic disorders in these years. While there was no statistically significant decline in the prevalence of illicit drug use disorders as a whole between 2003 and 2010, some drug disorders (e.g., cocaine, sedative, and stimulant disorders) did decrease during this time period.
Table 1.
Trends in Percent of Adolescents (Youth Ages 12-17) with Past Year Substance Use Disorders* (NSDUH)
| 2003 |
2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
2010 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Alcohol or Illicit Drug | 9.0 | [8.5-9.6] | 9.0 | [8.5-9.6] | 8.0 | [7.6-8.6] a | 8.2 | [7.6-8.7] | 7.8 | [7.3-8.3] | 7.8 | [7.2-8.3] | 7.1 | [6.6-7.6] | 7.3 | [6.9-7.9] b |
| Alcohol | 6.0 | [5.5-6.4] | 6.0 | [5.6-6.5] | 5.6 | [5.2-6.1] | 5.5 | [5.1-5.9] | 5.4 | [5.0-5.9] | 5.0 | [4.6-5.5] | 4.6 | [4.2-5.0] | 4.6 | [4.2-5.0] b |
| Illicit Drugs | 5.2 | [4.8-5.6] | 5.5 | [5.1-6.0] | 4.6 | [4.2-5.0] a | 4.7 | [4.3-5.1] | 4.4 | [4.0-4.8] | 4.7 | [4.3-5.1] | 4.3 | [4.0-4.8] | 4.7 | [4.3-5.1] |
| Marijuana | 3.9 | [3.6-4.3] | 3.9 | [3.5-4.3] | 3.5 | [3.1-3.8] | 3.5 | [3.1-3.9] | 3.1 | [2.8-3.5] | 3.4 | [3.1-3.8] | 3.4 | [3.1-3.8] | 3.6 | [3.2-3.9] |
| Hallucinogens | 0.4 | [0.3-0.6] | 0.5 | [0.4-0.7] | 0.5 | [0.4-0.6] | 0.4 | [0.3-0.6] | 0.5 | [0.4-0.6] | 0.4 | [0.3-0.5] | 0.5 | [0.4-0.7] | 0.5 | [0.4-0.7] |
| Inhalants | 0.4 | [0.3-0.5] | 0.6 | [0.4-0.8] | 0.4 | [0.3-0.6] | 0.4 | [0.3-0.5] | 0.4 | [0.3-0.5] | 0.4 | [0.3-0.5] | 0.4 | [0.3-0.6] | 0.4 | [0.3-0.5] |
| Cocaine | 0.3 | [0.2-0.4] | 0.4 | [0.3-0.5] | 0.4 | [0.3-0.5] | 0.3 | [0.2-0.4] | 0.4 | [0.3-0.5] | 0.4 | [0.3-0.5] | 0.2 | [0.1-0.3] a | 0.1 | [0.1-0.2] b |
| Heroin | 0.1 | [0.0-0.1] | 0.1 | [0.0-0.2] | 0.0 | [0.0-0.1] a | 0.0 | [0.0-0.1] | 0.0 | [0.0-0.1] | 0.1 | [0.0-0.1] | 0.1 | [0.0-0.2] | 0.0 | [0.0-0.1] a |
| Psychotherapeutics | 1.4 | [1.2-1.7] | 1.7 | [1.4-2.0] | 1.3 | [1.1-1.6] a | 1.4 | [1.2-1.7] | 1.3 | [1.1-1.6] | 1.3 | [1.1-1.5] | 1.0 | [0.9-1.2] | 1.2 | [1.0-1.4] |
| Tranquilizers | 0.4 | [0.3-0.5] | 0.3 | [0.2-0.4] | 0.3 | [0.2-0.4] | 0.3 | [0.2-0.4] | 0.3 | [0.2-0.4] | 0.3 | [0.2-0.3] | 0.2 | [0.1-0.3] | 0.3 | [0.2-0.4] |
| Pain Relievers | 1.1 | [0.9-1.3] | 1.4 | [1.2-1.6] | 1.1 | [0.9-1.4] | 1.1 | [0.9-1.3] | 1.0 | [0.8-1.2] | 1.0 | [0.8-1.1] | 0.8 | [0.7-1.0] | 0.9 | [0.8-1.1] |
| Sedatives | 0.2 | [0.1-0.3] | 0.1 | [0.1-0.2] | 0.1 | [0.1-0.2] | 0.1 | [0.0-0.1] | 0.1 | [0.1-0.2] | 0.1 | [0.1-0.2] | 0.1 | [0.0-0.1] | 0.0 | [0.0-0.1] b |
| Stimulants | 0.4 | [0.3-0.5] | 0.4 | [0.3-0.5] | 0.3 | [0.2-0.4] | 0.4 | [0.3-0.5] | 0.3 | [0.2-0.5] | 0.3 | [0.2-0.4] | 0.2 | [0.1-0.3] | 0.2 | [0.2-0.3] b |
Abuse or dependence
Signficantly different (p<0.05) from prior year.
Significant difference (p<0.05) between 2003 and 2010.
Trends in Substance Abuse Treatment Utilization
Table 2 shows the percent of adolescents in the US who reported receiving treatment in the past year for any substance as well as for alcohol and for illicit drugs at any location and at specialty facilities (e.g., a hospital as an inpatient, inpatient/outpatient rehabilitation facility, or mental health center). Less than 2% of adolescents in the US in any given year between 2003 and 2010 received any treatment in the past year for alcohol or illicit drugs at any location. No significant differences from year to year were observed on any of these measures. However, there was an overall drop in the percent of adolescents receiving treatment for alcohol use at specialty locations between 2003 and 2010 (0.4% v. 0.2%). In general, treatment utilization has been low and relatively stable during the majority of the last decade.
Table 2.
Trends in Percent of Adolescents (Youth Ages 12-17) Receiving Treatment (NSDUH)
| 2003 |
2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
2010 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Alcohol or Illicit Drugs | ||||||||||||||||
| Received Any Treatment (Any Location) | 1.4 | [1.2-1.7] | 1.6 | [1.4-1.9] | 1.4 | [1.2-1.6] | 1.4 | [1.2-1.6] | 1.4 | [1.2-1.7] | 1.4 | [1.2-1.6] | 1.2 | [1.0-1.5] | 1.2 | [1.0-1.4] |
| Received Any Treatment (Specialty Location) | 0.7 | [0.5-0.8] | 0.7 | [0.6-0.9] | 0.7 | [0.6-0.9] | 0.7 | [0.6-0.9] | 0.6 | [0.5-0.8] | 0.6 | [0.5-0.8] | 0.6 | [0.5-0.8] | 0.5 | [0.4-0.7] |
| Alcohol | ||||||||||||||||
| Received Treatment for Alcohol (Any Location) | 0.8 | [0.7-1.0] | 0.9 | [0.8-1.1] | 0.9 | [0.7-1.1] | 0.8 | [0.6-0.9] | 0.8 | [0.7-1.0] | 0.8 | [0.6-1.0] | 0.8 | [0.6-1.0] | 0.6 | [0.5-0.8] |
| Received Treatment for Alcohol (Specialty Location) | 0.4 | [0.3-0.5] | 0.5 | [0.4-0.6] | 0.5 | [0.4-0.6] | 0.4 | [0.3-0.5] | 0.4 | [0.3-0.5] | 0.3 | [0.3-0.5] | 0.4 | [0.3-0.5] | 0.2 | [0.2-0.4] a |
| Illicit Drugs | ||||||||||||||||
| Received Treatment for Illicit Drugs (Any Location) | 0.9 | [0.8-1.1] | 1.1 | [0.9-1.3] | 1.0 | [0.8-1.2] | 1.0 | [0.8-1.2] | 1.0 | [0.8-1.2] | 0.9 | [0.7-1.1] | 0.9 | [0.7-1.1] | 0.9 | [0.7-1.1] |
| Received Treatment for Illicit Drugs (Specialty Location) | 0.5 | [0.3-0.6] | 0.5 | [0.4-0.7] | 0.6 | [0.4-0.7] | 0.5 | [0.4-0.7] | 0.5 | [0.4-0.6] | 0.5 | [0.4-0.6] | 0.5 | [0.4-0.6] | 0.4 | [0.3-0.5] |
NOTES: Respondents were not asked questions in treatment module if they did not endorse any lifetime substance use; treatment refers to treatment or counseling designed to help reduce or stop substance use and includes detox and any other treatment for medical problems associated with substance use.
Significant difference (p<0.05) between 2003 and 2010.
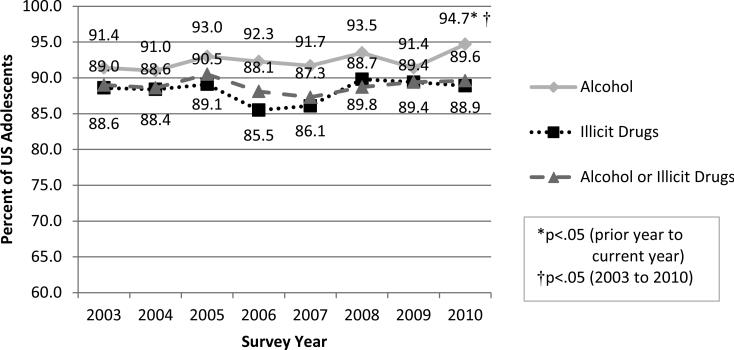
Figure 1 displays trends in the gap between adolescents who needed treatment and those who received it—denoted as the percent of adolescents with these disorders who did not receive treatment for them at any location. As can be seen, the gap is very large and has remained relatively stable since 2003. Between the years 2003 and 2010 close to 90% of adolescents with an alcohol or illicit drug disorder did not receive treatment at any location in the preceding year. In all years between 2003 and 2010, unmet need was greatest for alcohol disorders. In fact, unmet need grew significantly between 2003 and 2010 from 91.4% to 94.7%.
Figure 1.
Trends in Percent of Adolescents with Past-Year Disorders Who Did NOT Receive Treatment at Any Location in the Past Year
Trends in Adolescent Treatment Availability
Table 3 presents trends related to the availability of treatment for adolescents. Regardless of how adolescent treatment availability is defined (i.e., serving at least one adolescent on the reference date or providing special programing for adolescents) less than 36% of substance abuse treatment programs in the US in any year between 2003 and 2010 provided services to adolescents. From 2003-2010, there was an overall decrease in the percent of facilities reporting that they offered special programming for adolescents (32.0% v. 28.7%). Although there was no overall decrease in the percent of facilities that reporting serving at least one adolescent on the reference date between 2003 and 2010, there was a decrease in the percent of facilities that reported servicing 10 or more adolescents on the reference date (18.4% v. 17.1%).
Table 3.
Trends in Percent of US Treatment Facilities with Adolescent Treatment Capacity (N-SSATS)
| 2003 (N=13,623) |
2004 (N=13,454) |
2005 (N=13,371) |
2006 (N=13,771) |
2007 (N= 13,648) |
2008 (N=13,688) |
2009 (N=13,513) |
2010 (N=13,339) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Special Programming for Adolescents | 4,359 | 32.0 | 4,164 | 31.0 | 4,299 | 32.2 a | 4,353 | 31.6 | 4,259 | 31.2 | 4,116 | 30.1 a | 3,948 | 29.2 | 3,831 | 28.7 b |
| >1 Client Under 18 on Reference Date | 4,755 | 34.9 | 4,721 | 35.1 | 4,711 | 35.2 | 4,736 | 34.4 | 4,601 | 33.7 | 4,569 | 33.4 | 4,499 | 33.3 | 4,515 | 33.9 |
| ≥10 Clients Under 18 on Reference Date | 2,500 | 18.4 | 2,448 | 18.2 | 2,431 | 18.2 | 2,429 | 17.6 | 2,356 | 17.3 | 2,335 | 17.1 | 2,309 | 17.1 | 2,280 | 17.1 b |
NOTE: Sample sizes for each year represent the number of facilities surveyed. Valid precentages are presented for facilities providing special programming for adolescent clients (e.g., responses of DK or refused were coded as missing). Missing data on this item was minimal, representing less than 1% of facilities surveyed each year.
Signficantly different (p<0.05) from prior year.
Significant difference (p<0.05) between 2003 and 2010.
Discussion
This study sought to examine trends in the need for and use of adolescent substance abuse treatment as well as the availability of treatment programs in the US to address these needs. Analysis of the NSDUH data indicates an overall decrease since 2003 in the percent of adolescents meeting DSM-IV criteria for an alcohol or illicit drug use disorder. However, since 2003, past year treatment utilization has been low, and as was found in the 1983-2008 analysis of the Monitoring the Future utilization data (Ilgen et al., 2011), has remained largely unchanged. Given the large number of participants in the NSDUH study, and hence, the more than adequate statistical power to detect differences from year to year, the fact that few differences emerged is both striking and unfortunate. Even more worrisome is that the percent of adolescents with an alcohol or illicit drug disorder who do not receive treatment is substantial--nearly 9 out of 10 adolescents meeting criteria for a past-year alcohol or illicit drug disorder did not receive treatment at any facility (specialty or otherwise) for it in the past year—a figure that has also remained relatively stable since 2003. Furthermore, analysis of the N-SSATS data reveal that there has been an overall decrease in the percent of substance abuse treatment facilities that reported providing specialized programming for adolescents.
These findings indicate that much more work needs to be done to provide services to adolescents with SUDs. Adolescence is a critical period, and research suggests that failure to accomplish certain developmental tasks during this period can have cascading and lasting effects across the life course (Lynne-Landsman, Bradshaw, & Ialongo, 2010; Marti, Stice, & Springer, 2010; Morissette, Maranda, & Lessard, 2006; Schulenberg, Bryant, & O'Malley, 2004; Schuster, O'Malley, Bachman, Johnston, & Schulenberg, 2001; Sťaff et al., 2010; Windle & Wiesner, 2004). Substance abuse treatment during this critical period could serve as an important turning point for adolescents with SUDs, providing them with the adaptive resources to navigate a more favorable adult trajectory (Hser, Longshore, & Anglin, 2007; Masten et al., 2004). Future work examining trends in the proportion of SUD youth receiving treatment (using the NSDUH or other national data sets) within subgroups of the population (by region, race/ethnicity, and income) might be useful for developing strategies and policies to improve service delivery.
According to the Behavioral Model of Health Service Use, whether or not individuals who need services receive them depends on a variety of individual- and larger systems-level factors as well (Aday & Andersen, 1974; Andersen & Newman, 1973; Andersen, 1995). Strategies to increase service utilization among adolescents must address both of these factors. Individual-level factors (e.g., predisposing, enabling, and need characteristics) generally refer to characteristics of individuals as well as to beliefs about illness and treatment and perceived need for it. Perhaps because they are easier to assess, most explanations for low service utilization tend to focus on these factors. For example, using NSDUH data combined across 2005-2009, Hedden and Gfroerer (2011) found that only 12.4% of adults who needed treatment for an alcohol or drug disorder perceived a need for treatment. However, these individual-level factors are less straightforward to target among adolescents because they are not yet autonomous individuals, and characteristics of their parents may be as important in predicting service use as the characteristics of the youth in need of treatment. For instance, in a study looking at agreement between adolescents and parents on perceived need for mental health services, Williams and colleagues (2011) found that concordance between adolescents and parents was poor and that fewer parents perceived a need for treatment than the adolescents themselves.
Systems-level factors generally refer to available treatment resources (i.e., the labor and capital devoted to the system) and the organization of those resources (i.e., the manner in which personnel and facilities are coordinated and controlled in the process of providing services) (Andersen & Newman, 1973). Our analyses indicate that less than a third of substance abuse treatment facilities in the US offer special programming for adolescents. Limited system quantity is further compromised by limited system quality (Meyers & McLellan, 2005). Studies have found that many facilities serving adolescents lack components considered essential to effective adolescent substance abuse (Knudsen, 2009; Mark, et al., 2006). Improving the quality of what is currently available in the specialty care substance abuse treatment sector—that is by providing evidence-based and empirically supported treatment and by professionalizing the workforce--could go a long way not only to improving treatment out comes but also to increasing desirability and perceived effectiveness of treatment.
Screening and Brief Intervention (SBI; Babor & Higgins-Biddle, 2000) techniques hold great promise to increase individual awareness of need and motivation for treatment as well as to expand the scope and reach of the substance abuse treatment system. SBI techniques have been developed, implemented, and tested in a variety of medical settings (trauma units, general practitioner offices, prenatal care settings, and college health settings) for both alcohol and drug use. In general, studies of these programs for adult problem drinkers find that even a few minutes of feedback, information, and advice given by a general practitioner can lead excessive drinkers to reduce their alcohol consumption patterns to sensible limits (Beich, Thorsen, & Rollnick, 2003). Similar techniques developed for adult illicit drug users in medical settings have also shown promising results (Madras et al., 2009). Although preliminary research suggests that brief advice from a primary care provider can significantly decrease substance use among adolescents (Harris et al., 2012; Knight et al., 2005), much more work is needed in this area. Further, research on SBI techniques needs to be conducted in other venues where adolescents are found: high schools, child welfare programs, and juvenile justice settings. More research is also needed to determine whether SBI techniques do indeed increase the capacity of the substance abuse treatment system in ways that other efforts, such as the introduction of office-based treatment of opioid dependence with buprenorphine (Arfken, Johanson, di Menza, & Schuster, 2010) and California's Prop 36 (Hser et al., 2007), have had success in doing.
Strengths and Limitations
To our knowledge, this study is the first to examine both trends in adolescent SUDs and trends in percent of facilities providing services to adolescents in the US. While this is an important contribution to the literature on treatment for adolescents with SUDs, it is not without limitations. It is important to keep in mind that our estimates of the number of adolescents needing treatment are based on those who met criteria for past year disorder, which we defined as meeting DSM IV criteria for alcohol or illicit drug abuse or dependence. Discussions about the development of criteria for DSM V, have focused on eliminating the distinction between diagnostic syndromes for abuse and dependence as well as changing certain criteria for reaching the diagnostic threshold for SUDs (Winters, Martin, & Chung, 2011). However, preliminary analyses of how these changes might affect estimates of the prevalence of SUDs among adolescent in the US have shown that overall rates remain largely the same regardless of criteria used, but that concordance between criteria vary by gender (Case, He, & Merikangas, 2011). Future work is needed to replicate our work once DSM V criteria have been finalized and implemented with the NSDUH data. It is also important to note that our work highlights trends but does not specifically examine factors that may explain differences in the proportion of adolescents with SUDs receiving treatment. Future studies examining regional, urban vs suburban vs rural, racial and ethnic group, and income differences in the proportion of SUD youth receiving treatment may be useful in developing strategies to increase service use among this population.
Another limitation of our study is the lack of data on the capacity of the substance abuse treatment system. Although the N-SSATS provides the most comprehensive mechanism for quantifying the dynamic character and composition of the US substance abuse treatment delivery system, it is a voluntary survey, and there is no adjustment for the approximately 4 percent facility non-response. As a point-prevalence survey, it provides information on the substance abuse treatment system and its clients on a particular reference date; client counts reported do not represent annual totals. And although the N-SSATS does include a question on annual admissions, it does not include a question on annual adolescent admissions and there is no reliable way to determine the total number of treatment slots (residential and hospital bed as well as outpatient slots) available to adolescent on the reference date.
Summary and Implications
SUDs among adolescents are associated with a multitude of adverse consequences. Our analyses of the NSDUH data suggest that only one in ten adolescents with alcohol or illicit drug disorder receive treatment; a trend that has remained stable since 2003. Analyses of the N-SSATS data point to clear deficits in the substance abuse treatment system's ability to address the needs of adolescents with SUDs. In 2010, less than 29% of facilities participating in the N-SSATS survey indicated that they offered special programming for adolescents, reflecting an overall decrease since 2003 when approximately 32% of facilities offered these services. Efforts to increase adolescent substance abuse treatment utilization must target individual- , family-, and systems-level factors. Improving the quality of existing adolescent substance abuse treatment programs as well as expanding the purview of the adolescent substance abuse treatment into other service sectors such as medical, educational, juvenile justice, and child welfare systems through the use of SBI techniques could enhance and extend to the nation's ability to address the needs of adolescents with SUDs.
Acknowledgments
This research was supported by the National Institute of Drug Abuse (P50-DA02784). In addition to our funders we would like to acknowledge the assistance of staff at the Interuniversity Consortium for Political and Social Research (ICPSR) Substance Abuse and Mental Health Data Archive (SAMHDA) as well as Cathie E. Alderks, PhD, Brady Case, MD, A. Thomas McLellan, PhD and Lois Benishek, PhD. An earlier version of this manuscript was presented at the 2011 Addiction Health Services Research conference in Fairfax, VA.
Footnotes
Although the NSDUH does not sample individuals who are currently detained/incarcerated, it does ask respondents about treatment that could have been received in jail/prison. These forms of treatment are included in our estimates of the percent of youth with SUDs who received any treatment in the past year.
REFERENCES
- Aday LA, Andersen R. A framework for the study of access to medical care. Health Services Research. 1974;9(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Memorial Fund Quarterly: Health and Society. 1973;51(1):95–124. [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Anthony JC, Petronis KR. Early-onset drug use and risk of later drug problems. Drug and Alcohol Dependence. 1995;40(1):9–15. doi: 10.1016/0376-8716(95)01194-3. [DOI] [PubMed] [Google Scholar]
- Arfken CL, Johanson C-E, di Menza S, Schuster CR. Expanding treatment capacity for opioid dependence with office-based treatment with buprenorphine: National surveys of physicians. Journal of Substance Abuse Treatment. 2010;39(2):96–104. doi: 10.1016/j.jsat.2010.05.004. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC. Alcohol screening and brief intervention: Dissemination strategies for medical practice and public health. Addiction. 2000;95(5):677–686. doi: 10.1046/j.1360-0443.2000.9556773.x. [DOI] [PubMed] [Google Scholar]
- Beich A, Thorsen T, Rollnick S. Screening in brief intervention trials targeting excessive drinkers in general practice: Systematic review and meta-analysis. BMJ: British Medical Journal. 2003;327(7414):536–542. doi: 10.1136/bmj.327.7414.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A. Research methods in health: investigating health and health services. Open University Press; 1997. [Google Scholar]
- Brook JS, Richter L, Rubenstone E. Consequences of adolescent drug use on psychiatric disorders in early adulthood. Annals of Medicine. 2000;32(6):401–407. doi: 10.3109/07853890008995947. [DOI] [PubMed] [Google Scholar]
- Case BG, He J, Merikangas KR. Comparison of DSM-IV and proposed DSM-V substance use disorder criteria in US adolescents.. Paper presented at the 73rd Annual Meeting of the College on the Problems of Drug Dependence.2011. [Google Scholar]
- Chung T, Martin CS. Prevalence and clinical course of adolescent substance use and substance use disorders. In: Kaminer Y, Winters KC, editors. Clinical manual of adolescent substance abuse treatment. American Psychiatric Publishing, Inc.; Arlington, VA: 2011. pp. 2011–2023. [Google Scholar]
- Clark DB, Winters KC. Measuring risks and outcomes in substance use disorders prevention research. Journal of Consulting and Clinical Psychology. Special Issue: Impact of childhood psychopathology interventions on subsequent substance abuse. 2002;70(6):1207–1223. doi: 10.1037//0022-006x.70.6.1207. [DOI] [PubMed] [Google Scholar]
- Daudin M, Cohen D, Edel Y, Bonnet N, Bodeau N, Consoli A, et al. Psychosocial and clinical correlates of substance use disorder in an adolescent inpatient psychiatric population. Journal of the Canadian Academy of Child and Adolescent Psychiatry / Journal de l'Académie canadienne de psychiatrie de l'enfant et de l'adolescent. 2010;19(4):264–273. [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National longitudinal alcohol epidemiologic survey. Journal of Substance Abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Green KM, Doherty EE, Stuart EA, Ensminger ME. Does heavy adolescent marijuana use lead to criminal involvement in adulthood? Evidence from a multiwave longitudinal study of urban African Americans. Drug and Alcohol Dependence. 2010;112(1-2):117–125. doi: 10.1016/j.drugalcdep.2010.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris SK, Csemy L, Sherritt L, Starostova O, Van Hook S, Johnson J, et al. Computer-facilitated substance use screening and brief advice for teens in primary care: an international trial. Pediatrics. 2012;129(6):1072–1082. doi: 10.1542/peds.2011-1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedden SL, Gfroerer JC. Correlates of perceiving a need for treatment among adults with substance use disorder: Results from a National Survey. Addictive Behaviors. 2011;36(12):1213–1222. doi: 10.1016/j.addbeh.2011.07.026. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Edwards EM. Age at drinking onset, alcohol dependence, and their relation to drug use and dependence, driving under the influence of drugs, and motor-vehicle crash involvement because of drugs. Journal of Studies on Alcohol and Drugs. 2008;69(2):192–201. doi: 10.15288/jsad.2008.69.192. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Zha W. Age of drinking onset, alcohol use disorders, frequent heavy drinking, and unintentionally injuring oneself and others after drinking. Pediatrics. 2009;123(6):1477–1484. doi: 10.1542/peds.2008-2176. [DOI] [PubMed] [Google Scholar]
- Hser Y-I, Longshore D, Anglin MD. The life course perspective on drug use: A conceptual framework for understanding drug use trajectories. Evaluation Review. 2007;31(6):515–547. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- Hser Y-I, Teruya C, Brown AH, Huang D, Evans E, Anglin MD. Impact of California's proposition 36 on the drug treatment system: Treatment capacity and displacement. American Journal of Public Health. 2007;97(1):104–109. doi: 10.2105/AJPH.2005.069336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen MA, Schulenberg J, Kloska DD, Czyz E, Johnston L, O'Malley P. Prevalence and characteristics of substance abuse treatment utilization by US adolescents: National data from 1987 to 2008. Addictive Behaviors. 2011;36(12):1349–1352. doi: 10.1016/j.addbeh.2011.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminer Y, Bukstein OG. Adolescent substance abuse: Psychiatric comorbidity and high-risk behaviors. Routledge/Taylor & Francis Group, 501; New York, NY, US: 2008. [Google Scholar]
- Knight JR, Sherritt L, Van Hook S, Gates EC, Levy S, Chang G. Motivational interviewing for adolescent substance use: A pilot study. Journal of Adolescent Health. 2005;37(2):167–169. doi: 10.1016/j.jadohealth.2004.08.020. [DOI] [PubMed] [Google Scholar]
- Knudsen HK. Adolescent-only substance abuse treatment: Availability and adoption of components of quality. Journal of Substance Abuse Treatment. 2009;36(2):195–204. doi: 10.1016/j.jsat.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynne-Landsman SD, Bradshaw CP, Ialongo NS. Testing a developmental cascade model of adolescent substance use trajectories and young adult adjustment. Development and Psychopathology. Special Issue: Developmental cascades: Part. 2010;222(4):933–948. doi: 10.1017/S0954579410000556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug and Alcohol Dependence. 2009;99(1-3):280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark TL, Song X, Vandivort R, Duffy S, Butler J, Coffey R, et al. Characterizing substance abuse programs that treat adolescents. Journal of Substance Abuse Treatment. 2006;31(1):59–65. doi: 10.1016/j.jsat.2006.03.017. [DOI] [PubMed] [Google Scholar]
- Marti CN, Stice E, Springer DW. Substance use and abuse trajectories across adolescence: A latent trajectory analysis of a community-recruited sample of girls. Journal of Adolescence. 2010;33(3):449–461. doi: 10.1016/j.adolescence.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Burt KB, Roisman GI, Obradović J, Long JD, Tellegen A. Resources and resilience in the transition to adulthood: Continuity and change. Development and Psychopathology. Special Issue: Transition from Adolescence to Adulthood. 2004;16(4):1071–1094. doi: 10.1017/s0954579404040143. [DOI] [PubMed] [Google Scholar]
- Meyers K, McLellan AT. The American Treatment System for Adolescent Substance Abuse: Formidable Challenges, Fundamental Revisions, and Mechanisms for Improvements. In: Evans DL, Foa EB, Gur RE, Hendin H, O'Brien CP, Seligman ME, Walsh T, editors. Treating and preventing adolescent mental health disorders: What we know and what we don't know: A research agenda for improving the mental health of our youth. Oxford University Press; New York, NY: 2005. pp. 2561–2578. [Google Scholar]
- Morissette P, Maranda M-F, Lessard D. Young Substance Abusers and Precarious Employment: Trajectories and Anchoring Dynamics. Canadian Journal of Counselling. 2006;40(3):175–191. [Google Scholar]
- Newcomb MD. Psychosocial predictors and consequences of drug use: A developmental perspective within a prospective study. Journal of Addictive Diseases. 1997;16(1):51–89. doi: 10.1300/J069v16n01_05. [DOI] [PubMed] [Google Scholar]
- Olmstead T, Sindelar JL. To what extent are key services offered in treatment programs for special populations? Journal of Substance Abuse Treatment. 2004;27(1):9–15. doi: 10.1016/j.jsat.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Rothman KJ. Modern Epidemiology. Little Brown and Company; Boston: 1986. [Google Scholar]
- SAMHSA . The NSDUH Report: Trends in Substance Use, Dependence or Abuse, and Treatment among Adolescents: 2002 to 2007. Office of Applied Statistics; Rockville, MD: 2008. [Google Scholar]
- SAMHSA . National Survey of Substance Abuse Treatment Services (N-SSATS): 2003. Data on Substance Abuse Treatment Facilities. Office of Applied Statistics; Rockville, MD: 2004. DHHS Publication No. SMA 04-3966. [Google Scholar]
- SAMHSA . National Survey on Drug Use and Health, 2009 [Data file]. Inter-university Consortium for Political and Social Research [Distributor]; 2010a. [Google Scholar]
- SAMHSA . Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. Office of Applied Statistics; Rockville, MD: 2010b. NSDUH Series H-38A, HHS Publication No. SMA 10-4586. [Google Scholar]
- Schulenberg JE, Bryant AL, O'Malley PM. Taking hold of some kind of life: How developmental tasks relate to trajectories of well-being during the transition to adulthood. Development and Psychopathology. Special Issue: Transition from Adolescence to Adulthood. 2004;16(4):1119–1140. doi: 10.1017/s0954579404040167. [DOI] [PubMed] [Google Scholar]
- Schuster C, O'Malley PM, Bachman JG, Johnston LD, Schulenberg J. Adolescent marijuana use and adult occupational attainment: A longitudinal study from age 18 to 28. Substance Use & Misuse. 2001;36(8):997–1014. doi: 10.1081/ja-100104486. [DOI] [PubMed] [Google Scholar]
- Sťaff J, Schulenberg JE, Maslowsky J, Bachman JG, O'Malley PM, Maggs JL, et al. Substance use changes and social role transitions: Proximal developmental effects on ongoing trajectories from late adolescence through early adulthood. Development and Psychopathology. Special Issue: Developmental cascades: Part 2. 2010;22(4):917–932. doi: 10.1017/S0954579410000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . Stata Statistical Software: Release 11. StataCorp LP; College Station, TX: 2009. [Google Scholar]
- Steinberg L. Dahl, Ronald E.; Spear, Linda Patia (2004) xii. New York Academy of Sciences; New York, NY, US: 2004. Risk taking in adolescence: What changes, and why? pp. 51–58.pp. 472 pp. Adolescent brain development: Vulnerabilities and opportunities. [DOI] [PubMed] [Google Scholar]
- Weinberg NZ, Rahdert E, Colliver JD, Glantz MD. Adolescent substance abuse: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37(3):252–261. doi: 10.1097/00004583-199803000-00009. [DOI] [PubMed] [Google Scholar]
- Williams CD, Lindsey M, Joe S. Parent–adolescent concordance on perceived need for mental health services and its impact on service use. Children and Youth Services Review. 2011;33(11):2253–2260. doi: 10.1016/j.childyouth.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M, Wiesner M. Trajectories of marijuana use from adolescence to young adulthood: Predictors and outcomes. Development and Psychopathology. Special Issue: Transition from Adolescence to Adulthood. 2004;16(4):1007–1027. doi: 10.1017/s0954579404040118. [DOI] [PubMed] [Google Scholar]
- Winters KC, Lee C-YS. Likelihood of developing an alcohol and cannabis use disorder during youth: Association with recent use and age. Drug and Alcohol Dependence. 2008;92(1-3):239–247. doi: 10.1016/j.drugalcdep.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Martin CS, Chung T. Substance use disorders in DSM-V when applied to adolescents. Addiction. 2011;106(5):882–884. doi: 10.1111/j.1360-0443.2010.03334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]