Abstract
The aim of this study is to systematically review the literature that explored the association between smoking and suicidal risk among those with serious mental illness and to estimate the risk of suicidal behaviors attributable to smoking among this patient group. Multiple databases (CINAHL, PsycINFO, EMBASE, Informit Health Collection and the Cochrane Library databases) were searched from 1 January 1975 through 15 January 2014, along with references from relevant articles for observational studies that ascertained the association between smoking and suicidal behaviors among patients with psychotic disorders conducted in adult patients. Thirteen studies involving 6813 patients with severe mental illness were included. We found that smoking was significantly associated with suicidality in psychosis with an Odds Ratio of 2.12 (95% CI 1.67–2.7). Smoking is associated with suicidal risk amongst individuals with a severe mental illness; however, it is still unclear whether this represents a true risk factor or a confounder or a mediator via mechanisms, hitherto unknown, needs to be studied further.
Introduction
Although there are differences in smoking rates and anti-smoking campaigns between different countries, it would be safe to surmise that smoking awareness is overall higher than it has been in the past; despite this, people continue to smoke. People with mental illness are more likely to smoke than the general population. According to large epidemiological studies the prevalence of smoking is about 2–3 fold higher in those with a mental illness [1]. The risk of smoking is particularly high in those with severe mental illnesses such as schizophrenia, bipolar disorders and depression [2–8]. Individuals with these disorders also smoke, on average, more cigarettes than the general population [9, 10] and are less likely to quit [11]. An elevated risk for smoking has also been reported in those with alcohol or substance use and anxiety disorders [12, 13].
Research undertaken to understand why people with psychosis smoke has focused mainly on the “self-medication hypothesis”. According to this hypothesis smoking alleviates negative mood states, reduces positive symptoms, enhances cognitive functioning and reduces medication-induced side effects [14–17]. Others contend that this association is best explained by a “shared diathesis” between tobacco and mental illness, and provide evidence for how smoking predates psychosis [18].
A number of studies have focused on the association between smoking and increased suicidal risk [19–21]. Some such studies have specifically addressed this issue in mentally ill cohorts [22–24]. Interestingly, while studies in general population samples have found an association between smoking and an increased risk of suicide, as evidenced by a recent meta-analysis [25], studies done in mentally ill have yielded conflicting results. For example, while Tanskanen et al [22] and Kessler et al [26] have shown a positive association between smoking and suicidality among patients with mental illness, our study [27] failed to demonstrate an increased suicidal risk in smokers with a psychotic disorder, particularly after adjusting for confounding factors such as depression.
To interrogate these inconsistencies, we conducted a systematic-review and meta-analysis of observational studies to determine the effect of smoking on risk of suicide or suicidal behaviour in people with psychotic disorders. Our apriori hypothesis was that smoking is associated with an increased risk (current or lifetime) of suicidality (suicide ideation, suicide attempts, or completed suicides) in people with a psychotic disorder.
Materials and Methods
We have followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [28] in reporting this systematic review (detailed in S1 PRISMA Checklist). Studies were identified by searching six electronic databases and checking reference lists of relevant articles. Results were limited to articles published in the English language between 1 January 1975 and 15 January 2014. Database searches were carried out by an experienced medical research librarian (HW) with an initial search strategy applied to Medline (EBSCOhost) and adapted for CINAHL (EBSCOhost), PsycINFO (EBSCOhost), EMBASE (Embase.com), Informit Health Collection and the Cochrane Library. All searches were last updated on 15 January 2014. All potentially eligible studies were considered for review.
The search strategy for Medline (EBSCOhost) used a combination of MeSH Terms and title keywords as directed by our research question. Accordlngly, we were interested in studying the association between smoking [(MH "Smoking") OR (MH "Tobacco") OR (MH "Tobacco Use Cessation") OR (MH "Smoking Cessation") OR (MH "Tobacco Use Disorder") OR (MH "Nicotine") OR TI smoking OR TI cigarette* OR TI nicotine OR TI tobacco] and all suicidal behaviors [(MH "Suicide") OR (MH "Suicidal Ideation") OR (MH "Suicide, Attempted") OR (MH "Self-Injurious Behaviour") OR (MH "Self Mutilation") OR TI suicid* OR TI self-harm* OR TI DSH OR TI self-mutilat* OR TI self-injur*] and patients with severe mental illness [(MH "Mental Disorders") OR (MH "Anxiety Disorders+") OR (MH "Eating Disorders+") OR (MH "Mood Disorders+") OR (MH "Schizophrenia and Disorders with Psychotic Features+") OR (MH "Personality Disorders+") OR TI mental OR TI psychiatric OR TI psychosis OR TI psychotic OR TI schiz* OR TI mood disorder* OR TI affective disorder* OR TI bipolar OR TI depression OR TI depressive disorder* OR TI personality disorder* OR TI eating disorder* OR TI anorexia OR TI bulimia]
We used a broader search strategy that included mental illnesses other than psychosis as some studies include multiple diagnoses and we were keen to screen their appropriateness for the study. Similarly we wanted to include all forms of suicidal behaviors that had previously been associated with smoking. Previous systematic reviews on suicidal behaviors have used a similar approach [29, 30].
Other searches followed a similar format with adaptations appropriate to the individual database; thesaurus and subject headings used i.e. CINAHL Headings and EMTREE Terms. The additional search strategies are set out in the Appendix.
Study Selection
Studies were considered eligible and included if they fulfilled the following criteria:
Observational studies
Included adults (above the age of 18 years),
Performed in patients with a psychotic disorder; for the purpose of this review, we included the following diagnostic categories: schizophrenia, schizoaffective disorder, first episode psychosis, delusional disorder, bipolar disorder and psychotic depression.
Studies that specifically looked for or reported an association between cigarette smoking and suicidality; we included studies that reported suicidal risk, suicide attempt, suicidal ideation and/or completed suicide.
Data Extraction and Quality Assessment
AS and SG independently reviewed study titles and abstracts for potential inclusion in the systematic review. Studies that satisfied the inclusion criteria were retrieved for full-text evaluation. Studies selected for detailed analysis by these two authors had an agreement value (Κ) of .88; a third investigator (DC) resolved disagreements.
We developed a 19-item data-extraction sheet, based on the STROBE statement [31], that would yield a maximum of 23 points based on the type of study, clarity of aims, objectives and hypothesis, internal validity, external validity and statistical validity. This is detailed in S2 Table. While this would naturally award higher points for cohort studies, we also factored in negative markings where cohort studies did not discuss drop-out rates or fixed time periods of assessments. Further, we adjusted the final score by subtracting one point when studies did not score across all categories. Where two studies had the same adjusted scores, the final rating also took into consideration the type of study and the sample size. We also extracted quantitative data including characteristics of the sample, number of events and unadjusted and adjusted risk estimates. Where the study did not provide specific information, publication’s authors were contacted by e-mail for extra information.
Meta-analysis
The included studies employed a range of outcome measures to examine the association between smoking and suicidality. Some reported the exact number of suicidal behaviours (i.e., suicide ideation, suicide attempts, or completed suicides) in people with a psychotic disorder, while others reported odds ratios. We used odds ratios with 95% confidence intervals as the main outcome measure. To calculate the pooled odds ratio, we used R, version 3.0.2 (R foundation for Statistical Computing, Vienna, Austria) with the ‘metafor’ package [32]. Due to differences in study design, sample characteristics, and outcome measures, we expected considerable heterogeneity amongst the studies. Therefore, we calculated the pooled odds ratio using a random-effects model with the DerSimionian-Laird estimator [33].
To examine heterogeneity, we calculated the I2 statistic and its 95% confidence intervals. A value of 0% indicated no observed heterogeneity, and larger values show increasing heterogeneity, with 25% considered low, 50% moderate, and 75% high heterogeneity [34]. We tested for heterogeneity using the Q statistic, with p<0.10 indicating significant heterogeneity.
Subgroup analyses were conducted using the mixed-effects models function of the ‘metafor’ package [32]. For this method, studies within groups are pooled with the random-effects model, while tests for significant differences between subgroups are conducted with the fixed-effects model.
Publication bias was assessed using funnel plots and the trim-and-fill procedure [34], which yields an estimate of the effect size after publication bias has been taken into account. We also conducted Egger’s regression test [35] to quantify the bias captured by the funnel plot and tested whether it was significant. All results were considered significant at p<0.05.
Results
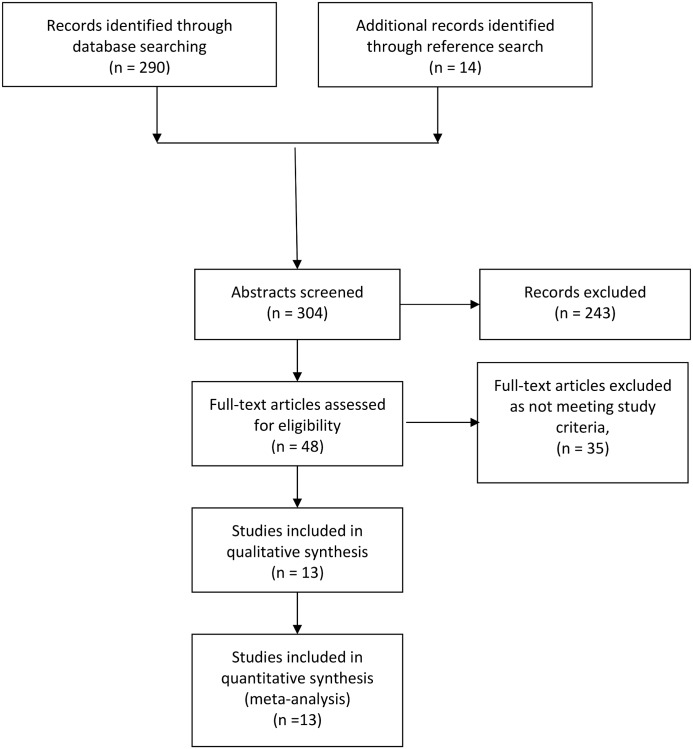
Fig 1 details the search-strategy flow-chart. We identified a total of 13 studies [6; 23; 27; 36–45] meeting our predefined criteria. Seven were cross-sectional, two case-control and four were cohort studies. While two studies [27; 37] employed a broad definition for psychotic illnesses and included patients with schizophrenia, schizoaffective disorders, bipolar disorders and psychotic depression, other studies focused solely on either schizophrenia (and/or schizoaffective disorder) or bipolar disorder. Only one study [38] ascertained completed suicides as the outcome of interest. Other studies focused on suicide attempts and/or suicidal intent. The studies are summarised in S1 Table.
Fig 1. Flow-diagram for screening of articles.
S3 Table summarizes the qualitative assessments for the studies. Five studies [6; 23; 27; 40; 42] reported a clear hypothesis. The study of Ostacher et al [39] received the highest rating. Five studies [6; 38; 39; 42; 45] rated poorly on internal validity rating, thereby questioning their final conclusions. Three studies [23; 38; 42] did not describe the final adjusted odds ratio.
We aimed to study whether smoking is associated with an increased risk (current or lifetime) of suicidality (suicide ideation, suicide attempts, or completed suicides) in people with a psychotic disorder. Six studies [6; 36. 39; 43; 37; 45] reported suicide attempt, while the rest studied both suicidal ideation and suicidal attempts. Of the studies that reported rates of suicidal attempts, all except one [36] reported lifetime rates. Altamura et al (2003) reported current rates.
Meta-analysis
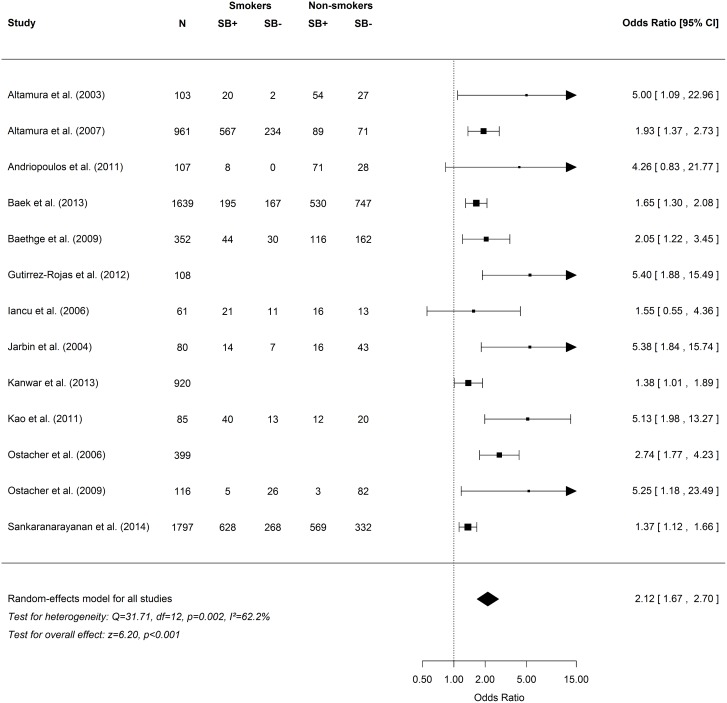
As shown in Fig 2, the overall odds ratio for the association between cigarette smoking and suicidality in psychosis was 2.12 (95% CI = 1.67–2.70, p<0.001). Heterogeneity was moderate and significant (I2 = 62.2%, 95% CI = 28.5–93.0, p = 0.002). Exclusion of three potential outliers (27; 37; 44) significantly reduced heterogeneity (I2 = 25.0%, 95% CI = 0.0–81.0, p = 0.213) and had a small effect on the overall odds ratio (2.74, 95% CI = 2.07–3.62, p<0.001).
Fig 2. Frequency table and forest plot for suicidal behaviors in psychosis meta-analysis.
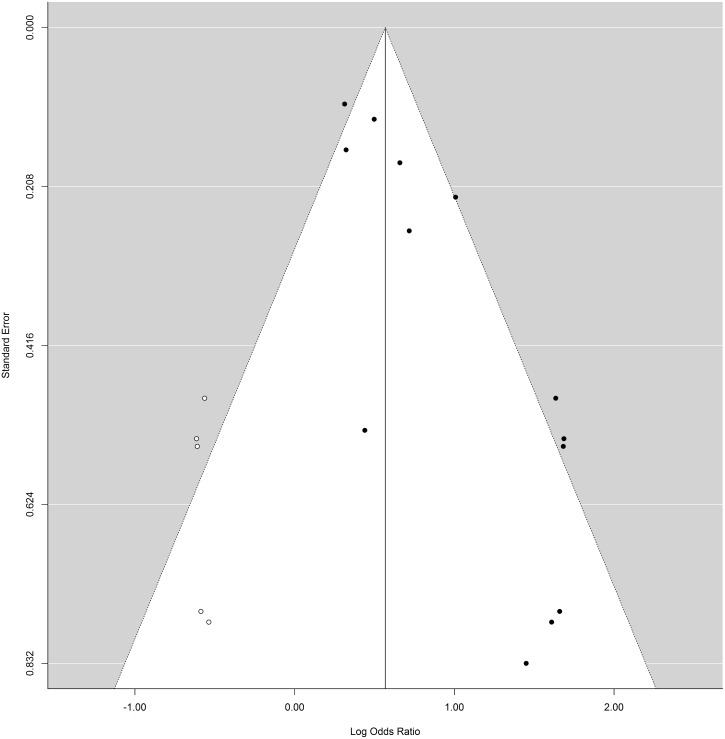
After adjustment for publication bias with the trim-and-fill procedure, the overall odds ratio was reduced to 1.76 (95%CI = 1.37–2.26, p<0.001; the number of filled studies was 5). Egger’s regression test for funnel plot asymmetry also indicated significant publication bias (z = 4.65, p<0.001). Given this small reduction in the overall odds ratio, which remained significant, the impact of publication bias is likely modest [46]. A funnel plot with the imputed studies is presented in Fig 3.
Fig 3. Trim-and-fill plot.
Subgroup analyses
The subgroup analyses are presented in Table 1, which shows that the odds ratio did not differ between suicidal behavior type (suicide attempt and. suicide attempt/suicidal ideation) (p = 0.421). The odds ratio did not differ in relation to diagnostic group (schizophrenia/schizoaffective disorder, bipolar disorder, and broad psychosis) (p = 0.851) or study design (case-control, cohort, and cross-sectional) (p = 0.243).
Table 1. Meta-analyses results for random-effects and mixed-effects models.
| Effect Size | Heterogeneity | p | |||
|---|---|---|---|---|---|
| OR | (95% CI) | I2 | (95% CI) | ||
| Random-effect models | |||||
| Unadjusted | 2.12 | (1.67–2.70)*** | 62.2% | (28.5–93.0)** | |
| Outliers removed | 2.74 | (2.07–3.62)*** | 25.0% | (0.0–81.1) | |
| Adjusted for publication bias | 1.76 | (1.37–2.26)*** | 25.0% | (0.0–81.0)*** | |
| Suicidal Behaviours | 0.421 | ||||
| Attempts | 2.63 | (1.66–4.16)*** | 67.7% | (12.1–95.3)*** | |
| Attempts/Ideation | 1.84 | (1.40–2.42)*** | 54.7% | (0.0–97.1) ** | |
| Sample | 0.851 | ||||
| Schizophrenia/Schizoaffective Disorder | 2.12 | (1.40–3.19)*** | 52.1% | (0.0–95.2) + | |
| Bipolar Disorder | 2.12 | (1.32–3.42)** | 59.7% | (0.0–99.6) + | |
| Broad Psychosis | 2.44 | (0.65–9.18) | 83.4% | (16.8–99.9)* | |
| Design | 0.243 | ||||
| Case-control | 2.09 | (0.85–5.18) | 5.1% a | ||
| Cohort | 2.76 | (2.03–3.76)*** | 0.8% | (0.0–90.1) | |
| Cross-sectional | 1.77 | (1.37–2.29)*** | 67.4% | (31.0–98.8)** | |
a Unable to calculate confidence interval for I2 (k = 2).
+ p<0.10
* p<0.05
** p<0.01
*** p<0.001
Discussion
While smoking has been associated with suicidal behaviours in the general population, studies limited to those with a mental illness have shown conflicting results. We undertook a systematic review and meta-analysis to study the strength of association reported in observational studies conducted in people with a psychotic illness. We found that smoking was significantly associated with suicidal behaviours among people with severe mental illness. Accordingly, the pooled odds ratio for the association was 2.12. We did not find differences in the odds ratio across study design (i.e., case-control, cohort, and cross-sectional) or diagnosis (i.e., schizophrenia/schizoaffective disorder, bipolar disorder, and broadly defined psychosis). This strongly implies that there is a significant association between smoking and suicidal behaviors in people with severe mental illness thereby proving our hypothesis right.
Smoking is highly prevalent among people with severe mental illness; for example, a meta-analysis based on 9 studies from 6 countries [11] demonstrated that patients with schizophrenia have a higher prevalence of ever smoking compared to the general population. Smoking has also been shown to be associated with suicidal risk in a previous meta-analysis [25]. It is therefore conceivable that smoking is associated with suicidal behaviours among patients with severe mental illness. Such an association was first described nearly four decades ago [19] although it was downplayed as an “artefact” [47].
From a clinical point, what is more important though is to explain this association; for example, is smoking a predictor or an independent risk factor or a mediator or in fact a confounder. Hughes [48] reviewed the association between smoking and suicide and proposed three potential explanatory hypotheses: (i) smoking is a non-causal marker; (ii) smoking is a psychological or physical toxin; and (iii) smokers are self-medicating a suicide risk.
If indeed smoking was “suicidogenic”, we need to understand the possible mechanisms. One approach therefore would be to tease out the effects of smoking that might contribute to suicidal behaviors in those with mental illness. Previous research indicates that smoking might increase the risk of mental illness [49–53] possibly through its action on brain nerurotransmitters such as serotonin [54] or Monoamine Oxidase [55]. It is also possible that smoking and mental illness shares common vulnerability factors [56–58].
Such individuals with a predisposition might begin to smoke as a form of coping strategy [59]; for example, patients with severe mental illnesses have significant problem solving difficulties, particularly in the social context [60–66]. It is likely that smoking leads to some initial gains, such as improved attention, behavioural arousal and enhanced problem-solving [67–68]; however chronic smoking can lead to neurocognitive deficits such as impairments in cognitive flexibility. Cognitive inflexibility is defined as the inability to change decision-making in response to feedback from the environment [69]. Such individuals have difficulty in finding effective solutions to problems during times of stress, which leads to hopelessness and suicidal ideation and/or tend to brood or in other words, have difficulty disengaging from negative ruminations [70]. The diathesis–stress–hopelessness model of suicidality [71–72] identifies hopelessness as a key mechanism through which cognitive inflexibility results in suicidal ideation [73–74].
From a biological point of view, chronic smoking is associated with neurobiological changes such as orbito-frontal cortical (OFC) thinning [75–76] and/or biochemical changes such as lower serotonin [77–78]. These changes are significant because lesion studies have demonstrated that emotion recognition and other social cognitive abilities depend critically on the orbitofrontal cortex [79–81] while suicidal behaviours, aggression, impulsivity and smoking have all been linked to a reduced central serotonin or “low serotonin syndrome” [82]. These changes affect the individual’s decision making capacity, impulse control, judgment, planning and reasoning skills, and hence serve to increase the risk of suicidal behaviours [54].
In summary, it is plausible therefore that patients with severe mental illness (or a vulnerability thereto) starts smoking either because they share common heritable factors or as a coping strategy to manage certain distress (e.g. negative affect). However chronic smoking is associated with biological and neurocognitive changes that in turn predispose the individual to contemplate suicide and/or engage in such behaviors because of increased impulsivity and/or poor problem solving abilities.
Study Limitations
The results of our study must be interpreted within the context of some limitations. Firstly, we only chose literature published in English and this is likely to cause selection bias. Secondly, there was significant heterogeneity across studies. However, removal of potential outliers reduced heterogeneity to non-significance but had only a small effect on the overall odds ratio. In a similar vein, although there was evidence of publication bias, smoking was still significantly associated with suicidality in patients with severe mental illness after adjusting for this bias.
Our finding of a significant association between smoking and suicidality in those with severe mental illness is not in keeping with findings from previous systematic reviews on suicidal risk factors in severe mental illness [83–88]. Interestingly, while Hor and Taylor [89] reported a weak association between smoking and suicide, they did not elaborate on this. It is likely that the earlier reviews included studies that adjusted for smoking and therefore did not find a significant association. Leistikow [90] had warned against “over-adjusting” as smoking may independently be associated with and contribute to other suicide risk factors that the authors adjust for, including adverse life situations and stress.
Finally, although we were keen on studying all suicidal behaviors including completed suicide, we could identify only one study [44] that described completed suicide as an outcome of interest. Thus we did not have the capacity to study completed suicide and have only reported on suicidal behaviors. While suicidal behaviours are doubtlessly an important “predictor” of future suicide, the predictive capabilities are limited as suicide is rare. For example, the association between suicidal ideation and completed suicide is weak [91].
Conclusions
Smoking is moderately associated [92] with suicidal behaviors in patients with psychotic disorders as is evidenced by results of our meta-analysis. What is less well known is how smoking is associated with suicidality in this patient group. There is however potential to test the effectiveness of smoking intervention in reducing suicidality in this patient group. Future research should therefore focus on the impact of smoking cessation on suicidal behaviours in those with psychotic disorders. Further, it would also be useful to test some of these theories in clinical research to build on the evidence base. Examples include studying neurocognitive functioning in smokers who attempt suicide and in particular looking for any correlation to neuroimaging findings. This can, however, be difficult to undertake considering there are multiple potential confounders. Ideally one would need a long-term prospective study that describes all variables of interest and can adjust for association between and interaction of changes in smoking status, mental status, and suicidality over time.
Supporting Information
(DOC)
(DOC)
(DOC)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was approved funding by the Hamad Medical Corporation Medical Research Centre (Research Proposal # 14486/14) to cover publication charges. None of the authors received any financial benefits, incentives or salary from the funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness. JAMA. 2000; 284: 2606–2610. [DOI] [PubMed] [Google Scholar]
- 2. Beratis S, Katrivanou A, Gourzis P. Factors affecting smoking in schizophrenia. Compr Psychiatry. 2001; 42: 393–402. [DOI] [PubMed] [Google Scholar]
- 3. de Leon J, Becona E, Gurpegui M, Gonzalez-Pinto A, Diaz FJ. The association between high nicotine dependence and severe mental illness may be consistent across countries. J Clin Psychiatry. 2002; 63: 812–6. [DOI] [PubMed] [Google Scholar]
- 4. Wilhelm K, Mitchell P, Slade T, Brownhill S, Andrews G. Prevalence and correlates of DSM-IV major depression in an Australian national survey. J Affect Disord. 2003; 75: 155–62. [DOI] [PubMed] [Google Scholar]
- 5. Waxmonsky JA, Thomas MR, Miklowitz DJ, Allen MH, Wisniewski SR, Zhng H, et al. Prevalence and correlates of tobacco use in bipolar disorder: data from the first 2000 participants in the Systematic Treatment Enhancement Program. Gen Hosp Psychiatry. 2005; 27: 321–328 [DOI] [PubMed] [Google Scholar]
- 6. Ostacher MJ, Nierenberg AA, Perlis RH, Fidelman P, Borrelli DJ, Tran TB, et al. The relationship between smoking and suicidal behavior, comorbidity, and course of illness in bipolar disorder. J Clin Psychiatry. 2006; 67: 1907–11. [DOI] [PubMed] [Google Scholar]
- 7. McClave AK, McKnight-Eily LR, Davis SP, Dube SR. Smoking characteristics of adults with selected lifetime mental illness: results from the 2007 National Health Interview Survey. Am J Public Health. 2010; 100: 2464–72. 10.2105/AJPH.2009.188136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cooper J, Mancuso SG, Borland R, Slade T, Galletly C, Castle D. Tobacco smoking among people living with a psychotic illness: the second Australian Survey of Psychosis. Aust NZ J Psychiatry. 2012; 46: 851–63 [DOI] [PubMed] [Google Scholar]
- 9. Araya R, Gaete J, Rojas G, Fritsch R, Lewis G. Smoking and common mental disorders: a population-based survey in Santiago, Chile. Soc Psychiatry Psychiatr Epidemiol. 2007; 42: 874–80. [DOI] [PubMed] [Google Scholar]
- 10. Xian H, Scherrer JF, Eisen SA, Lyons MJ, Tsuang M, True WR, et al. Nicotine dependence subtypes: Association with smoking history, diagnostic criteria and psychiatric disorders in 5440 regular smokers from the Vietnam era twin registry. Addict Behav. 2007; 32: 137–47. [DOI] [PubMed] [Google Scholar]
- 11. de Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res. 2005; 76: 135–157. [DOI] [PubMed] [Google Scholar]
- 12. Cuijpers P, Smit F, ten Have M, de Graaf R. Smoking is associated with first-ever incidence of mental disorders: A prospective population-based study. Addiction. 2007; 102: 1303–1309. [DOI] [PubMed] [Google Scholar]
- 13. Morissette SB, Tull MT, Gulliver SB, Kamholz BW, Zimering RT. Anxiety, anxiety disorders, tobacco use, and nicotine: A critical review of interrelationships. Psychol Bull. 2007; 133: 245–272. [DOI] [PubMed] [Google Scholar]
- 14. Goff DC, Henderson DC, Amico E. Cigarette smoking in schizophrenia: relationship to psychopathology and medication side effects. Am J Psychiatry. 1992; 149: 1189–1194. [DOI] [PubMed] [Google Scholar]
- 15. Levin ED, Wilson W, Rose JE, McEvoy J. Nicotine–haloperidol interactions and cognitive performance in schizophrenics. Neuropsychopharmacology. 1996; 15: 429–436 [DOI] [PubMed] [Google Scholar]
- 16. Lyon ER. A review of the effects of nicotine on schizophrenia and antipsychotic medications. Psychiatr Serv. 1999; 50: 1346–1350. [DOI] [PubMed] [Google Scholar]
- 17. Kumari V, Postma P. Nicotine use in schizophrenia: the self medication hypotheses. Neurosci Biobehav Rev. 2005; 29: 1021–1034. [DOI] [PubMed] [Google Scholar]
- 18. Myles N, Newall HD, Curtis J, Nielssen O, Shiers D, Large M. Tobacco use before, at, and after first-episode psychosis: A systematic meta-analysis. J Clin Psychiatry 2012; 73: 468–475. 10.4088/JCP.11r07222 [DOI] [PubMed] [Google Scholar]
- 19. Doll R, Peto R. Mortality in relation to smoking: 20 years' observations on male British doctors. Br Med J. 1976; 2: 1525–1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tanskanen A, Tuomilehto J, Viinamäki H, Vartiainen E, Lehtonen J, Puska P. Smoking and the risk of suicide. Acta Psychiatr Scand. 2000; 101: 243–245. [PubMed] [Google Scholar]
- 21. Iwasaki M, Akechi T, Uchitomi Y, Tsugane S. Cigarette smoking and completed suicide among middle-aged men, a population-based cohort study in Japan. Ann Epidemiol. 2005; 15: 286–292. [DOI] [PubMed] [Google Scholar]
- 22. Tanskanen A, Viinamaki H, Hintikka J, Koivumaa-Haonkanen HT, Lehtonen J. Smoking and suicidality among psychiatric patients. Am J Psychiatry. 1998; 155: 129–30. [DOI] [PubMed] [Google Scholar]
- 23. Iancu I, Sapir AP, Shaked G, Poreh A, Dannon PN, Chelben J, et al. Increased suicidal risk among smoking schizophrenia patients. Clin Neuropharmacol. 2006; 9: 230–237. [DOI] [PubMed] [Google Scholar]
- 24. Goldstein BI, Birmaher B, Axelson DA, Goldstein TR, Esposito-Smythers C, Strober MA, et al. Significance of Cigarette smoking among youth with Bipolar Disorder. Am J Addict. 2008; 17: 364–371. 10.1080/10550490802266151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Li D, Yang X, Ge Z, Hao Y, Wang Q, Liu F, et al. Cigarette smoking and risk of completed suicide: a meta-analysis of prospective cohort studies. J Psychiatr Res. 2012; 46: 1257–1266. 10.1016/j.jpsychires.2012.03.013 [DOI] [PubMed] [Google Scholar]
- 26. Kessler RC, Berglund PA, Borges G, Castilla-Puentes C, Glantz MD, Jaeger SA, et al. Smoking and suicidal behaviors in the National Comorbidity Survey, Replication. J Nerv Ment Dis. 2007; 195: 369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sankaranarayanan A, Mancuso S, Castle D. Smoking and suicidality in patients with a psychotic disorder. Psychiatry Res. 2014; 215: 634–40. 10.1016/j.psychres.2013.12.032 [DOI] [PubMed] [Google Scholar]
- 28. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4: 1 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fassberg MM, van Orden KA, Duberstein P, Erlangsen A, Lapiette S, Bodner E, et al. A systematic review of social factors and suicidal behavior in older adulthood. Int J Environ Res Public Health. 2012; 9: 722–745. 10.3390/ijerph9030722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Malik S, Kanwar A, Sim LA, Prokop LJ, Wang Z, Benkhadra K, et al. The association between sleep disturbances and suicidal behaviors in patients with psychiatric diagnoses: a systematic review and meta-analysis. Syst Rev. 2014; 3: 18 10.1186/2046-4053-3-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. von Elm E, Altman DG, Egger M, Pocock AJ, Gotzsche PC, Vandenbroucke JP, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007; 335: 806–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Viechtbauer W. Conducting Meta-Analysis. J Stat Softw. 2010; 36: 1–48. [Google Scholar]
- 33. DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986; 7: 177–88. [DOI] [PubMed] [Google Scholar]
- 34. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327: 557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315: 629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Altamura AC, Bassetti R, Bignotti S, Pioli R, Mundo E. Clinical variables related to suicide attempts in schizophrenic patients: a retrospective study Schizophr Res. 2003; 60: 47–55. [DOI] [PubMed] [Google Scholar]
- 37. Jarbin H, Von Knorring AL. Suicide and suicide attempts in adolescent onset psychotic disorders. Nord J Psychiatry. 2004; 58: 115–123. [DOI] [PubMed] [Google Scholar]
- 38. Altamura AC, Mundo E, Bassetti R, Green A, Lindenmayer JP, Alphs L, et al. Transcultural differences in suicide attempters: Analysis on a high-risk population of patients with schizophrenia or schizoaffective disorder. Schizophr Res. 2007; 89: 140–146. [DOI] [PubMed] [Google Scholar]
- 39. Baethge C, Tondo L, Lepri B, Baldessarini RJ. Coffee and cigarette use: association with suicidal acts in 352 Sardinian bipolar disorder patients. Bipolar Disord. 2009; 11: 494–503. 10.1111/j.1399-5618.2009.00727.x [DOI] [PubMed] [Google Scholar]
- 40. Ostacher MJ, LeBeaua RT, Perlisa RH, Nierenberg AA, Lund HG, Moshier SJ, et al. Cigarette smoking is associated with suicidality in bipolar disorder. Bipolar Disord. 2009; 11: 766–771. 10.1111/j.1399-5618.2009.00744.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Andriopoulos I, Ellul J, Skokou M, Beratis S. Suicidality in the “prodromal” phase of schizophrenia. Compr Psychiatry. 2011; 52: 479–485. 10.1016/j.comppsych.2010.10.011 [DOI] [PubMed] [Google Scholar]
- 42. Kao YC, Liu YP, Cheng TH, Chou MK. Cigarette smoking in outpatients with chronic schizophrenia in Taiwan: Relationships to socio-demographic and clinical characteristics. Psychiatry Res. 2011; 190: 193–199. 10.1016/j.psychres.2011.05.016 [DOI] [PubMed] [Google Scholar]
- 43. Gutie´ rrez L, Gurpegui M, Soto F, Martı´nez-Ortega JM, Jurado L. High nicotine dependence is a factor in the risk of suicide in bipolar disorder patients. Int Clin Psychopharmacol. 2012; 28 (e-Supplement): A e18–19. [Google Scholar]
- 44. Baek JH, Eisner LR, Nierenberg AA. Smoking and suicidality in subjects with bipolar disorder: results from the national epidemiologic survey on alcohol and related conditions (NESARC). Depress Anxiety. 2013; 30: 982–90. 10.1002/da.22107 [DOI] [PubMed] [Google Scholar]
- 45. Kanwar J, Okusaga O, Giegling I, Konte B, Vaswani D, Sleemi A, et al. In patients with schizophrenia, non-fatal suicidal self-directed violence is positively associated with present but not past smoking. Schizophr Res. 2013; 149: 194–195. 10.1016/j.schres.2013.06.010 [DOI] [PubMed] [Google Scholar]
- 46. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis Sussex. United Kingdom: Hoboken: John Wiley & Sons, Ltd; 2009. [Google Scholar]
- 47. Smith GD, Phillips AN, Neaton JD. Smoking as “independent” risk factor for suicide: illustration of an artefact from observational epidemiology? Lancet. 1992; 340: 709–12. [PubMed] [Google Scholar]
- 48. Hughes JR. Smoking and suicide: a brief overview. Drug Alcohol Depend. 2008; 98: 169–178. 10.1016/j.drugalcdep.2008.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wu LT, Anthony JC. Tobacco smoking and depressed mood in late childhood and early adolescence. Am J Public Health. 1999; 89: 1837–1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Goodman E, Capitman J. Depressive symptoms and cigarette smoking among teens. Paediatrics. 2000; 106: 748–755. [DOI] [PubMed] [Google Scholar]
- 51. Upadhyaya HP, Deas D, Brady KT, Kruesi M. Cigarette smoking and psychiatric comorbidity in children and adolescents. J Am Acad Child and Adolesc Psychiatry. 2002; 41: 1294–305. [DOI] [PubMed] [Google Scholar]
- 52. Isensee B, Wittchen HU, Stein MB, Hofler M, Lieb R. Smoking increases the risk of panic: findings from a prospective community study. Arch Gen Psychiatry. 2003; 60: 692–700. [DOI] [PubMed] [Google Scholar]
- 53. Klungsoyr O, Nygard JF, Sorensen T, Sandanger I. Cigarette smoking and incidence of first depressive episode: an 11-year, population-based follow-up study. Am J Epidemiol. 2006; 163: 421–432. [DOI] [PubMed] [Google Scholar]
- 54. Malone KM, Waternaux C, Haas GL, Cooper TB, Li S, Mann JJ. Cigarette smoking, suicidal behavior, and serotonin function in major psychiatric disorders. Am J Psychiatry. 2003; 160: 773–779 [DOI] [PubMed] [Google Scholar]
- 55. Whitfield JB, Pang D, Bucholz KK, Madden PA, Heath AC, Statham DJ, et al. Monoamine oxidase: associations with alcohol dependence, smoking and other measures of psychopathology. Psychol Med. 2000; 30: 443–454. [DOI] [PubMed] [Google Scholar]
- 56. Gilbert DG, Gilbert BO. Personality, psychopathology, and nicotine response as mediators of the genetics of smoking. Behav Genet. 1995; 5: 33–147. [DOI] [PubMed] [Google Scholar]
- 57. Kendler KS, Neale MC, MacLean CJ, Heath AC, Eaves LJ, Kessler RC. Smoking and major depression. A causal analysis. Arch Gen Psychiatry. 1993; 50: 36–43. [DOI] [PubMed] [Google Scholar]
- 58. Goodwin RD, Fergusson DM, Horwood LJ. Association between anxiety disorders and substance use disorders among young persons: results of a 21-year longitudinal study. J Psychiatr Res. 2004; 38: 295–304. [DOI] [PubMed] [Google Scholar]
- 59. Berlin I, Covey LS. Pre-cessation depressive mood predicts failure to quit smoking: The role of coping and personality traits. Addiction. 2006; 101: 1814–1821. [DOI] [PubMed] [Google Scholar]
- 60. Bellack AS, Sayers M, Mueser KT, Bennett M. Evaulation of social problem solving in schizophrenia. J Abnorm Psychol. 1994; 103: 371–378. [DOI] [PubMed] [Google Scholar]
- 61. Haaga DAF, Fine JA, Roscow Terrill D, Stewart BL, Beck AT. Social problem-solving deficits, dependency and depressive symptoms. Cognit Ther Res. 1995; 19: 147–158. [Google Scholar]
- 62. Morris RG, Rushe T, Woodruffe PW, Murray RM. Problem solving in schizophrenia: a specific deficit in planning ability. Schizophr Res. 1995; 14: 235–246. [DOI] [PubMed] [Google Scholar]
- 63. D'Zurilla TJ, Chang EC, Nottingham EJ 4th, Faccinni L. Social problem-solving deficits and hopelessness, depression, and suicidal risk in college students and psychiatric inpatients. J Clin Psychol. 1998; 54: 1091–1107. [DOI] [PubMed] [Google Scholar]
- 64. Getz GE, Shear PK, Strakowski SM. Facial affect recognition deficits in bipolar disorder. J Int Neuropsychol Soc. 2003; 9: 623–632. [DOI] [PubMed] [Google Scholar]
- 65. Chan RCK, Chen EYH, Cheung EFC, Chen RYL, Cheung HK. Problem-solving ability in chronic schizophrenia: a comparison study of patients with traumatic brain injury. Eur Arch Psychiatry Clin Neurosci. 2004; 254: 236–241. [DOI] [PubMed] [Google Scholar]
- 66. McClure EB, Treland JE, Snow J, Schmajuk M, Dickstein DP, Towbin KE, et al. Deficits in social cognition and response flexibility in pediatric bipolar disorder. Am J Psychiatry. 2005; 162: 1644–1651. [DOI] [PubMed] [Google Scholar]
- 67. Henningfield JE. Behavioural pharmacology of cigarette smoking In: Thompson T, Dews PB, Barrett JE, editors. Advances in Behavioural Pharmacology. New York: Academic Press: 1984. pp. 131–210. [Google Scholar]
- 68. Kassel JD. Smoking and attention: A review and reformulation of the stimulus-filter hypothesis. Clin Psychol Rev. 1997; 17: 451–478. [DOI] [PubMed] [Google Scholar]
- 69. Lezak MD, Howieson DB, Bigler ED, Tranel D. Neuropsychological Assessment. 5th edition New York: Oxford University Press; 2012. [Google Scholar]
- 70. Davis RN, Nolen-Hoeksema S. Cognitive inflexibility among ruminators and nonruminators. Cognit Ther Res. 2000; 24: 699–711. [Google Scholar]
- 71. Schotte DE, Clum GA. Suicide ideation in a college population: a test of a model. J Consult Cin Psychol. 1982; 50: 690–696. [DOI] [PubMed] [Google Scholar]
- 72. Schotte DE, Clum GA. Problem-solving skills in suicidal psychiatric patients. J Consul Clin Psychol. 1987; 55: 49–54. [DOI] [PubMed] [Google Scholar]
- 73. Pollock LR, Williams JM. Problem solving in suicide attempters. Psychol Med. 2004; 34: 163–167. [DOI] [PubMed] [Google Scholar]
- 74. Gibbs LM, Dombrovski AY, Morse J, Siegle GJ, Houck PR, Szanto K. When the solution is part of the problem: problem solving in elderly suicide attempters. Int J Geriatr Psychiatry. 2009; 24: 1396–404. 10.1002/gps.2276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Loftipour S, Ferguson E, Leonard G, Perron M, Pike B, Richer L, et al. Orbitofrontal cortex and drug use during adolescence: role of prenatal exposure to maternal smoking and BDNF genotype. Arch Gen Psychiatry. 2009; 66: 1244–52. 10.1001/archgenpsychiatry.2009.124 [DOI] [PubMed] [Google Scholar]
- 76. Kühn S, Schubert F, Gallinat J. Reduced Thickness of Medial Orbitofrontal Cortex in Smokers. Biol Psychiatry. 2010; 68: 1061–1065. 10.1016/j.biopsych.2010.08.004 [DOI] [PubMed] [Google Scholar]
- 77. Stanley M, Mann JJ. Increased serotonin-2 binding sites in frontal cortex of suicide victims. Lancet. 1983; 1: 214–216. [DOI] [PubMed] [Google Scholar]
- 78. Benwell ME, Balfour DJ, Anderson JM. Smoking-associated changes in the serotonergic systems of discrete regions of human brain. Psychopharmacology. 1990; 102: 68–72. [DOI] [PubMed] [Google Scholar]
- 79. Stuss DT, Gallup GG Jr, Alexander MP. The frontal lobes are necessary for ‘theory of mind’. Brain. 2001; 124: 279–286. [DOI] [PubMed] [Google Scholar]
- 80. Shamay-Tsoory SG, Tibi-Elhanany Y, Aharon-Peretz J. The ventromedial prefrontal cortex is involved in understanding affective but not cognitive theory of mind stories. Soc Neurosci. 2006; 1: 149–66. 10.1080/17470910600985589 [DOI] [PubMed] [Google Scholar]
- 81. Heberlein AS, Padon AA, Gillihan SJ, Farah MJ, Fellows LK. Ventromedial frontal lobe plays a critical role in facial emotion recognition. J Cogn Neurosci. 2008; 20: 721–733. [DOI] [PubMed] [Google Scholar]
- 82. Linnoila VMI, Virkkunen M. Aggression, suicidality, and serotonin. J Clin Psychiatry. 1992; 53: 46–51 [PubMed] [Google Scholar]
- 83. Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005; 87: 9–20. 10.1192/bjp.187.1.9 [DOI] [PubMed] [Google Scholar]
- 84. Hawton K, Sutton L, Haw C, Sinclair J, Harriss L. Suicide and attempted suicide in bipolar disorder: a systematic review of risk factors. J Clin Psychiatry. 2005; 66: 693–704. [DOI] [PubMed] [Google Scholar]
- 85. Haw C, Hawton K. Schizophrenia and Deliberate Self Harm: A Systematic Review of Risk Factors. Suicide Life-Threat Behav. 2005; 35: 50–62. [DOI] [PubMed] [Google Scholar]
- 86. Palmer BA, Pankratz VS Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry. 2005; 62: 247–253. [DOI] [PubMed] [Google Scholar]
- 87. Hawton K, Casanas I, Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013; 147: 17–28. 10.1016/j.jad.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 88. Costa Lda S, Alencar AP, Nascimento NPJ, dos Santos Mdo S, da Silva CG, Pinheiro Sde F, et al. Risk factors for suicide in bipolar disorder: a systematic review. J Affect Disord. 2015; 170: 237–54. 10.1016/j.jad.2014.09.003 [DOI] [PubMed] [Google Scholar]
- 89. Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010; 24: 81–90. 10.1177/1359786810385490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Leistikow B. Commentary: Questionable premises, overadjustment, and a smoking/suicide association in younger adult men. Int J Epidemiol. 2003; 32: 1005–6. [DOI] [PubMed] [Google Scholar]
- 91. Large MM, Nielssen O. Suicidal Ideation and Later Suicide. Am J Psychiatry. 2012; 169: 662. [DOI] [PubMed] [Google Scholar]
- 92. Rosenthal JA. Quality descriptors of strength association and effect size. J Soc Serv Res 1996; 21: 37–59. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.