Abstract
Objectives
This study examined warfarin usage for elderly Medicare beneficiaries with atrial fibrillation (AF) who suffered traumatic brain injury (TBI), hip fracture, or torso injuries.
Design and Participants
Using the 5% Chronic Condition Data Warehouse administrative claims data, this study included Fee-for-Service Medicare beneficiaries who had a single injury hospitalization (TBI, hip fracture, or major torso injury) between 1/1/2007 and 12/31/2009, with complete Medicare Parts A, B (no Medicare Advantage) and D coverage 6 months before injury, and who were aged 66 years or older and diagnosed with AF at least one year before injury.
Results
About 45% of the AF patients were using warfarin before TBI or torso injury, and 35% before hip fracture. After injury, there was a dramatic and persistent decrease in warfarin use in TBI and torso injury groups (30% for TBI and 37% for torso injury at 12 months after injury). Warfarin usage in hip fracture patients also dropped after injury but returned to pre-injury level within 4 months.
Conclusions
TBI and torso injury lead to significant decreases in warfarin usage in elderly AF patients. Further research is needed to understand reasons for the pattern and to develop evidence-based management strategies in the post-acute setting.
Keywords: Stroke, Warfarin, Traumatic injury
Introduction
Atrial fibrillation (AF) disproportionately affects older adults and the number of elderly AF patients is projected to increase as the population continues to age.1 Untreated AF patients have a five-fold increased risk of ischemic stroke compared with those treated with anticoagulant medication 2. Warfarin is a potent and widely used anticoagulant for preventing ischemic stroke among high-risk patients 3,4. Traumatic injury in older adults is associated with an increased risk of bleeding and thromboembolic events 5,6. Consequently, balancing risks and benefits of resuming warfarin after traumatic injury in older patients is a significant challenge.
There is no consensus on whether and when to resume warfarin in elderly patients with AF who experience traumatic injury. Warfarin may be contraindicated soon after traumatic injury owing to an abrupt increase in risk of bleeding. However, it is crucial to re-institute warfarin as soon as the risk of thrombotic events starts to outweigh the risk of bleeding. The decision to resume warfarin is complicated by the fact that the risk of bleeding and thrombosis differ among patients with different injury types, and among patients with different pre-injury risk strata. Several studies have evaluated the ever-changing balance of bleeding and thrombotic risk after spontaneous intracranial bleeding or surgery and have made varying recommendations for optimal warfarin resumption time 7–11. It is unclear whether research findings from these studies of intracranial bleeding or surgery are applicable to patients with traumatic injury.
Although under-utilization of warfarin among AF patients has been well-documented 12,13 and some single-center studies in acute hospital settings suggested that increased risk of fall, inability to tolerate warfarin, and established contraindications may all contribute to the low usage of warfarin among elderly patients 14,15, there is a paucity of research examining the long-term management of warfarin after traumatic injury. Related studies have focused upon warfarin reversal immediately following injury or on venous thromboembolism prophylaxis during injury hospitalization 16–19. To our knowledge, past research studies have not investigated how often patients with traumatic injury resume warfarin after in the community setting (after discharge from the hospital or skilled care facility) or whether certain groups of patients are more likely to resume warfarin therapy after traumatic injury.
The objectives of this study were to examine warfarin usage patterns among elderly AF patients who suffered traumatic brain injury (TBI), hip fracture, or torso injury with internal organ or blood vessel damage, and to determine factors associated with warfarin usage before and after injury in a national sample of Medicare beneficiaries.
Methods
The University of Maryland, Baltimore investigational review board (IRB) reviewed and approved the study protocol.
Definition of injury cohorts
The study sample in this retrospective cohort study was drawn from the 5% sample of Chronic Condition Data Warehouse (CCW) Medicare administrative claims database. Medicare is the national health insurance program that covers people aged 65 years and older in the United States. Patients can receive Medicare benefit of Part A (which covers hospital care), Part B (which covers outpatient care) and/or Part D (prescription drug coverage). In 2009, about 23% of beneficiaries chose to receive their Medicare benefits through a Medicare Advantage plan instead of the traditional Medicare program. The CCW database provides a 5% random sample of the remaining Fee-for-Service beneficiaries, of whom slightly fewer than half received prescription drug coverage.
The study sample included Medicare beneficiaries who had a single hospitalization for an injury event between 1/1/2007 and 12/31/2009 that was a TBI, hip fracture, or a torso injury with internal organ or blood vessel damage (henceforth referred to as ‘major torso injury’). The International Classification of Diseases, 9th version, Clinical Modification (ICD-9-CM) codes used to identify the injury-related hospitalizations are in the attached Appendix. For patients who had multiple hospitalizations for a single injury within a short period of time, succeeding injury-related hospitalizations occurring within 30 days of each other were treated as non-independent injury events and combined into a single event. Other inclusion criteria were: complete Medicare Part A, B and D coverage during the 6 months before injury, age 66 or older at the time of injury, and diagnosed with AF at least one year before injury. Patients who had evidence of Medicare Advantage coverage during the study period were excluded because their claims data were not captured in the CCW database. Patients followed up for less than one year before their injury were also excluded. The maximum follow-up time after injury was 3 years.
Definition of warfarin usage
Each patient’s follow-up time was divided into 30-day periods before injury hospitalization admission and after hospital discharge. The first and the last periods did not always include a full length of 30 days (e.g. the patient died or was lost to follow-up). In this manuscript, the 30-day periods are referred to as ‘months’. The month preceding hospitalization of a patient for traumatic injury was treated as the ‘baseline’ period. Warfarin usage during months when the patients were covered under Medicare Part D was evaluated by determining the number of days with warfarin coverage based on prescription refills. For a month to be categorized as ‘having warfarin usage,’ warfarin should have been available to the patient for at least one day in the month according to prescription refill dates and dispensed days’ supply.
Definition of covariates
Age at the time of injury, sex, race, and chronic disease conditions associated with an increased risk of thrombotic events or bleeding were included as covariates. Chronic disease conditions already defined and constructed by CCW were retained in the analysis 20: heart failure, stroke or transient ischemic attack (TIA), chronic kidney disease, and nine other domains of chronic condition (Alzheimer disease, and related disorders; cataract; chronic obstructive pulmonary disease; diabetes; glaucoma; depression; osteoporosis; rheumatoid arthritis; occurrence of any type of cancer). In addition, new disease flags were constructed for the following conditions by searching all patient claims from 2006 and 2009: valvular heart disease or valve replacement, atrial flutter, chronic liver disease, coagulation defect (congenital coagulation defects and thrombocytopenia), and alcohol abuse. The ICD-9-CM and CPT (Current Procedural Terminology) codes used to construct the new disease flags are included in appendix 1.
Statistical analysis
Differences in baseline characteristics across the three injury groups (TBI, hip fracture, and major torso injury) were compared using one-way ANOVA for continuous variables, and Chi-square test for categorical variables. Factors associated with higher warfarin usage at the time of injury among the total study sample were identified using Chi-square test.
Logistic generalized estimating equations (GEE) were used to model usage of warfarin while accounting for within-patient correlation. Time (after injury vs. before injury), injury type, and the interaction of the two were included in the model as the main independent variables. The analysis included age, sex and race, and comorbid conditions that were significantly associated with warfarin usage in univariate analysis to adjust for potential confounding. Hypothesizing that injury type may be a significant modifier of the effect of injury on warfarin usage, the odds ratio of warfarin usage (after vs. before injury) in each injury group were estimated by interpreting the interaction between time and injury type. To account for different durations of follow-up between patients, the analysis was limited to data from one year before and after traumatic injury for each individual. A sensitivity analysis was performed using data from all available follow-up for each individual. Statistical significance was defined as p 0.05. All analyses were performed using SAS 9.2 (SAS institute Inc., Cary, NC).
Results
Patient characteristics at the time of injury
A total of 4622 patients were included in the study – 1470 with TBI, 2527 with hip fracture and 625 with major torso injury (Table 1). Patients with hip fracture were slightly older than patients with other types of traumatic injury. Individuals in the study cohort were predominantly white (91.5%, 94.9% and 89.8% for TBI, hip fracture and torso injury respectively). The majority of TBI and hip fracture patients were female in the hip fracture (78%) and TBI (68%). The sex distribution was more balanced in the major torso injury group where 43.4% were female.
Table 1.
Patient characteristics at the time of injury by injury group
| Characteristics | TBI N=1470 | Hip Fracture N=2527 | Major Torso N=625 | P value |
|---|---|---|---|---|
|
|
|
|
||
| Mean age at injury, years | 83.3±7.4 | 85.0±6.8 | 82.1±7.2 | <0.001 |
|
|
|
|
||
| Race | ||||
|
|
|
|
||
| White | 1345(91.5) | 2397(94.9) | 561(89.8) | <0.001 |
|
|
|
|||
| Black | 49(3.3) | 58(2.3) | 42(6.7) | |
|
|
|
|||
| Other | 76(5.2) | 72(2.9) | 22(3.5) | |
|
|
|
|
||
| Sex, female | 1000(68.0) | 1974(78.1) | 271(43.4) | <0.001 |
|
|
|
|
||
| Comorbid conditions-possible indications | ||||
|
|
|
|
||
| Valvular heart disease/valve replacement a | 201(13.7) | 313(12.4) | 90(14.4) | 0.289 |
|
|
|
|
||
| Atrial flutter a | 78(5.3) | 131(5.2) | 51(8.2) | 0.012 |
|
|
|
|
||
| Heart failure | 983(66.9) | 1674(66.2) | 445(71.2) | 0.060 |
|
|
|
|
||
| Stroke or TIA | 347(23.6) | 422(16.7) | 131(21.0) | <0.001 |
|
|
|
|
||
| Comorbid conditions-possible contraindications | ||||
|
|
|
|
||
| Chronic liver disease a | 60(4.1) | 78(3.1) | 29(4.6) | 0.089 |
|
|
|
|
||
| Chronic kidney disease | 433(29.5) | 720(28.5) | 236(37.8) | <0.001 |
|
|
|
|
||
| Coagulation defect a | 79(5.4) | 90(3.6) | 24(3.8) | 0.020 |
|
|
|
|
||
| Alcohol abuse a | 32(2.2) | 29(1.2) | 10(1.6) | 0.038 |
|
|
|
|
||
| Counts of other CCW chronic conditions b | 2.6±1.5 | 2.6±1.5 | 2.6±1.5 | 0.825 |
|
|
|
|
||
| In-hospital mortality | 157(10.7) | 99(3.9) | 35(5.6) | <0.001 |
- Abbreviations: TIA, transient ischemic attack; TBI, traumatic brain injury; CCW: Chronic Conditions Data Warehouse
- P value obtained from analysis of variance (ANOVA) test (continuous variable) or Chi-square test (categorical variable), by comparing three injury groups with respect to patient characteristics.
- a Disease conditions not defined by CCW, ICD codes provided in appendix
-
b We counted the total number of several other comobid conditions defined by CCW (maximum=9) to represent general chronic disease burden:
- Alzheimer disease, and related disorders
- Cataract
- Chronic obstructive pulmonary disease
- Diabetes
- Glaucoma
- Depression
- Osteoporosis
- Rheumatoid arthritis
- Occurrence of any type of cancer listed(Endometrial cancer, female breast cancer, colorectal cancer, lung cancer, or prostate cancer)
About two-thirds of the injury patients had a history of heart failure at the time of injury (66.9%, 66.2% and 71.2% in the TBI, hip fracture and major torso injury group, respectively). TBI patients had the highest prevalence of history of stroke or TIA (23.6%) among the three groups, while the highest prevalence of atrial flutter (8.2%), valvular disease or valve replacement (14.4%) was observed in major torso injury patients. At the time of injury, only a small number of patients had conditions associated with increased bleeding risk (e.g., chronic liver disease and coagulation defect). The only exception was chronic kidney disease, with prevalence of 29.5%, 28.5% and 37.8% in TBI, hip fracture and torso injury groups, respectively.
Warfarin usage before and after injury
Unadjusted analysis
Fewer than half of the patients were using warfarin before traumatic injury (Figure 1). Warfarin usage was less prevalent before traumatic injury among patients who had hip fracture compared with patients who had TBI or major torso injury. Warfarin usage declined among patients with all three types of traumatic injury but was greater in magnitude with TBI compared with the other two types of injury. 17%, 24%, and 24% of the patients continued to use warfarin in the 1st, 2nd, and 3rd month after TBI, respectively. By 12 months after TBI, warfarin usage increased to 30% of patients but remained significantly lower than pre-injury levels. A similar trend in warfarin usage was observed among those with torso injuries. Hip fracture patients had a very low prevalence of warfarin usage (36%) before injury. In contrast with TBI and major torso injury, post-injury warfarin usage returned to pre-injury levels within 12 months.
Figure 1.
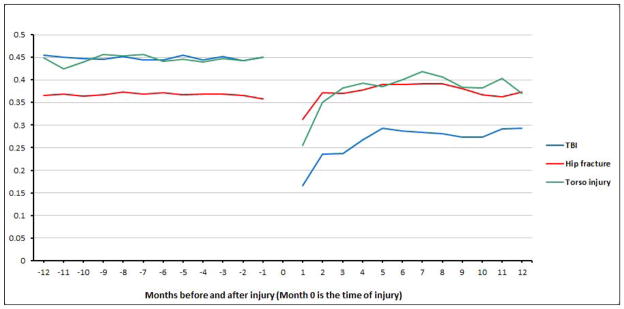
Proportion of atrial fibrillation patients with warfarin usage in 30-day periods during the 12 months before and the 12 months after injury, by injury type
Analysis adjusting for covariates
We first investigated the association between potential risk factors and warfarin usage at baseline. Younger age, white race, valvular heart disease or valve replacement, atrial flutter, heart failure, and stroke or TIA were significantly associated with higher warfarin usage in the month before injury (p<0.001) (Table 2). Patients who had comorbid conditions that may contribute to an increased bleeding risk were less likely to receive warfarin but the associations were not significant. Increased number of comorbid conditions was also associated with lower warfarin usage (p=0.02).
Table 2.
Warfarin usage among patient subgroups (30 days before injury), by patient characteristics (total n=4622)
| Subgroups | % used warfarin | P value | |
|---|---|---|---|
| Age at injury, yrs | 66–70 | 51.3 | <0.001 |
| 70<–75 | 45.5 | ||
| 75<–80 | 43.3 | ||
| 80<–85 | 43.4 | ||
| 85<–older | 34.2 | ||
| Race | White | 40.5 | 0.001 |
| Black | 29.5 | ||
| Other | 30.0 | ||
| Sex | Male | 41.8 | 0.059 |
| Female | 38.9 | ||
| Comorbid conditions-possible indications | |||
| Valvular heart disease/valve replacement | Y | 54.6 | <0.001 |
| N | 37.5 | ||
| Atrial flutter | Y | 50.0 | <0.001 |
| N | 39.1 | ||
| Heart failure | Y | 42.5 | <0.001 |
| N | 34.1 | ||
| Stroke or TIA | Y | 44.8 | <0.001 |
| N | 38.5 | ||
| Comorbid conditions-possible contraindications | |||
| Chronic liver disease | Y | 35.3 | 0.235 |
| N | 39.9 | ||
| Chronic kidney disease | Y | 38.2 | 0.168 |
| N | 40.4 | ||
| Coagulation defect | Y | 38.3 | 0.684 |
| N | 39.8 | ||
| Alcohol abuse | Y | 32.4 | 0.202 |
| N | 39.9 | ||
| Counts of other CCW chronic conditions | 0–1 | 42.1 | 0.021 |
| 2 | 41.7 | ||
| 3 | 39.3 | ||
| 4 | 35.3 | ||
| 5 and above | 37.3 | ||
- Abbreviations: TIA, transient ischemic attack; TBI, traumatic brain injury; CCW: Chronic Conditions Data Warehouse; Y, yes; N, No
- P value obtained from Chi-square test
In a multivariable regression model adjusting for all covariates within one year pre- and post- injury (Table 3), the interaction term between injury types and time (before injury vs. after injury) was statistically significant (p<0.001). Before injury, TBI and major torso injury patients had higher warfarin usage than hip fracture patients (p<0.001). After injury, decreased warfarin usage was observed in all three injury groups compared with pre-injury estimates. However, TBI patients had the biggest decrease of the three groups, with an odds ratio (OR) of warfarin usage (after vs. before injury) of 0.41(95% confidence interval (CI): 0.36 to 0.46, p<0.001), followed by major torso injury (OR=0.69, 95%CI: 0. 60 to 0.80, p<0.001).
Table 3.
Results of mutivariable GEE model, odds ratios of warfarin usage within 30-day periods within 1 year pre- and post- injury (no. of patients=4622)
| Comparison | Odds ratio of warfarin usage (95%CI) | P value |
|---|---|---|
| TBI | ||
| After injury vs. before injury | 0.41(0.36 to 0.46) | <0.001 |
| Hip fracture | ||
| After injury vs. before injury | 0.93(0.87 to 1.00) | 0.051 |
| Major torso | ||
| After injury vs. before injury | 0.69(0.60 to 0.80) | <0.001 |
| Age at injury | ||
| (Five years increase) | 0.84(0.80 to 0.87) | <0.001 |
| Race | ||
| White vs. other | 1.53(1.06 to 2.23) | 0.025 |
| Black vs. other | 0.62(0.35 to 1.10) | 0.101 |
| Sex | ||
| Male vs. female | 0.96(0.84 to 1.11) | 0.592 |
| Comorbid conditions (yes vs. no) | ||
| Valvular heart disease/valve replacement | 1.03(0.91 to 1.17) | 0.597 |
| Atrial flutter | 1.29(1.09 to 1.52) | 0.003 |
| Heart failure | 1.17(1.07 to 1.28) | 0.001 |
| Stroke or TIA | 0.98(0.87 to 1.09) | 0.683 |
| Chronic liver disease or alcohol abuse | 0.82(0.70 to 0.96) | 0.012 |
| Chronic kidney disease | 0.97(0.87 to 1.09) | 0.609 |
| Coagulation defect | 1.19(1.00 to 1.42) | 0.056 |
| No. of other CCW chronic conditions (each additional condition) | 1.01(0.98 to 1.04) | 0.628 |
- Abbreviations: TIA, transient ischemic attack; TBI, traumatic brain injury; CCW: Chronic Conditions Data Warehouse; GEE, generilzed estimating equations
- We combined chronic liver disease with alchohol abuse, two similar disease condition categories with extremely small number of patients.
- In multivariable regression model, we tested for the statistical significance of interaction terms between time (after injury vs. before injury) and injury type, age, sex, race and other confounders. The only statistically significant interaction was time*injury type.
Among hip fracture patients, the decrease in warfarin usage after injury was small but statistically significant. However, by 4 months post-hip fracture, the prevalence of warfarin usage had increased and was no longer statistically different from the pre-injury level. Sensitivity analysis which included the entire follow-up months in the multivariable regression model gave very similar effect estimates.
Discussion
Traumatic injury in elderly patients with AF poses a significant challenge of balancing the risk of hemorrhage against the benefit of preventing thromboembolism. Prior to this study, little was known about how traumatic injury event affects management of warfarin among elderly patients with a strong indication of warfarin (e.g., atrial fibrillation). This study confirmed previous findings about under-utilization of warfarin among high-risk patients 12,13,21. Additionally, this study also demonstrated that traumatic injury is associated with a sharp and sustained decline in warfarin usage among patients with AF.
Our findings reinforce the previously documented underutilization of warfarin among high stroke risk elderly patients 12,13,21 and suggest a potentially large scope for improvement of warfarin management. A considerable proportion of AF patients in our study sample were not receiving warfarin before their injury despite having no known contraindication for anticoagulation. The prevalence of chronic conditions that might be considered as contraindications for warfarin was relatively low in our study sample, and associations between these chronic conditions and warfarin usage were not statistically significant. The incidence of other acute disease events such as major bleeding which may prevent initiation or halt usage of warfarin was also low in our study sample and is unlikely to explain under-utilization of warfarin for elderly patients with AF. At the time of injury, fewer than 10% of patients had a history of upper GI bleeding and fewer than 5% had a history of hemorrhagic stroke. We suspect that the under-utilization of warfarin may be attributed to a fear of prescribing an oral anticoagulation medication to fragile elderly patients who are at high risk for falls 22, as physicians may overestimate the risk of hemorrhage and stroke in this population 23.
The three injury types included in our analysis differ with respect to mechanisms and outcomes of injury and require different healthcare management strategies24. Pre-injury warfarin usage was very different among patients who experienced TBI, hip fracture, and major torso injury. Pre-injury warfarin usage in patients who experienced hip fracture was much lower than that in patients who experienced TBI or major torso injury. A possible explanation is that hip fracture patients are predominantly female; previous research has shown that women tend to have lower warfarin usage than men 25. Other factors may also have precluded the use of warfarin for patients who experienced hip fracture, such as a greater predisposition to gait dysfunctions or osteoporosis.
In our study, TBI patients had a sharp and sustained decline in warfarin usage after injury. The decline in warfarin usage was sustained event at 12 months among patients with TBI but returned to pre-injury levels among patients who experienced hip fracture. We hypothesize that TBI provokes a high level of concern for bleeding events, thereby leading to the observed decline in warfarin usage. TBI related intracranial bleeding is generally considered to have more drastic consequences than bleeding in some other contexts. Further, patients with hip fracture may be perceived to be at a lower risk of bleeding than TBI once the fracture is surgically treated. In our study sample, hip fracture patients also had the lowest hospital mortality among the three groups, indicating that hip fracture is the least severe injury.
A steep decline in the prevalence of warfarin usage was also found among the group of torso injury patients who were at a high risk of thrombotic event before injury. However, compared with TBI patients, the magnitude of sustained decreased warfarin usage was much smaller in major torso injury patients. There seemed to be less concern for bleeding events after the patient recovers from a major torso injury.
Our study has limitations. The data we used only provided information on warfarin usage during months with Medicare Part D coverage and not during care provided in the hospital or other nursing facility (when prescriptions are covered under Part A). We do no expect that lack of data on warfarin usage during care provided within healthcare facilities introduced bias into our findings because our goal was to describe warfarin usage in the community setting (after discharge from healthcare facilities following traumatic injury). We did not account for certain potential confounders such as the functional status of patients, supplemental insurance, or socioeconomic factors, which may be related to warfarin usage.
We also did not explicitly examine the usage of alternatives to warfarin that may have been used for anticoagulation therapy for patients in our study sample. Warfarin is the predominantly used vitamin K antagonist in the United States. Other orally administered anticoagulants have been approved only recently and were not available to patients in our study sample (dabigatran: October, 2010; rivaroxaban: July, 2011; apixaban: December, 2012). We were unable to assess usage aspirin because it is available without a prescription. Finally, we did not evaluate other antiplatelet agents such as clopidogrel as alternatives to warfarin because we considered that antiplatelet therapy alone is not an ideal substitute for anticoagulation therapy with warfarin for long-term stroke prevention.
There are several strengths to our study. Our study is the first to examine the impact of an acute injury event on chronic medication management of warfarin and to identify patterns of warfarin usage before and after injury. We used a large, nationally representative sample to study warfarin usage among an under-studied older adult population who experienced traumatic injury and who are vulnerable for bleeding events. Our findings provide national estimates of warfarin usage among elderly Medicare patients who suffered traumatic injury. Our study participants represent patients with multiple chronic diseases seen in ‘real-world’ clinical settings. We were able to examine the impact of injury on the prevalence of warfarin usage while adjusting for multiple risk factors and contraindications. Warfarin management in this population with multimorbidity requires a careful balance of the competing bleeding and thrombotic risks. Our findings establish the low levels of warfarin usage among elderly patients with AF following traumatic injury.
Conclusion
We found that the prevalence of warfarin use in the elderly atrial fibrillation patient decreased after traumatic injury. The decline in warfarin usage among patients who experienced TBI or major torso injury was sustained months after injury. Practitioners should be alerted to the low prevalence of warfarin usage in this high-risk population and its potential impact on patient outcomes. Further research is needed to understand reasons for the decline in warfarin usage after traumatic injury, to evaluate risks and benefits of prescribing warfarin for elderly injury patients, and to develop evidence-based management strategies in the post-acute setting.
Acknowledgments
The authors thank the Pharmaceutical Research Computing Center, Department of Pharmaceutical Health Services Research, University of Maryland School of Pharmacy, for its support in data storage, management, and analytic file processing for this study.
This research is supported by NIH R21: Long-term anticoagulation therapy after traumatic brain injury in older adults. Project number: 5R21AG042768-02
Footnotes
Author Contributions: Dr. Xinggang Liu, Dr. Ilene Zuckerman and Dr. Gail Rattinger were involved in the acquisition of data. All authors were involved in study concept and design, and the analysis and interpretation of data, and preparation of manuscript.
Disclosure: Dr. Baumgarten, Dr. Ilene Zuckerman, Dr. Langenberg, Dr. Gordon Smith, Dr. Xinggang Liu, Dr. Jennifer Albrecht , Dr. Stephen Gottlieb and Dr. Steven Gambert and/or their institution received grant fund support from National Institute on Aging which funded this work; Dr. Gail Rattinger was a consultant of the National Institute on Aging grant (NIH R21, 5R21AG042768-02)
References
- 1.Go AS. The epidemiology of atrial fibrillation in elderly persons: the tip of the iceberg. The American journal of geriatric cardiology. 2005 Mar-Apr;14(2):56–61. doi: 10.1111/j.1076-7460.2005.02278.x. [DOI] [PubMed] [Google Scholar]
- 2.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991 Aug;22(8):983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 3.Birman-Deych E, Radford MJ, Nilasena DS, Gage BF. Use and effectiveness of warfarin in Medicare beneficiaries with atrial fibrillation. Stroke. 2006 Apr;37(4):1070–1074. doi: 10.1161/01.STR.0000208294.46968.a4. [DOI] [PubMed] [Google Scholar]
- 4.Hart RG, Benavente O, McBride R, Pearce LA. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis. Annals of internal medicine. 1999 Oct 5;131(7):492–501. doi: 10.7326/0003-4819-131-7-199910050-00003. [DOI] [PubMed] [Google Scholar]
- 5.Karni A, Holtzman R, Bass T, et al. Traumatic head injury in the anticoagulated elderly patient: a lethal combination. Am Surg. 2001 Nov;67(11):1098–1100. [PubMed] [Google Scholar]
- 6.Meldon SW, Reilly M, Drew BL, Mancuso C, Fallon W., Jr Trauma in the very elderly: a community-based study of outcomes at trauma and nontrauma centers. J Trauma. 2002 Jan;52(1):79–84. doi: 10.1097/00005373-200201000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Majeed A, Kim YK, Roberts RS, Holmstrom M, Schulman S. Optimal timing of resumption of warfarin after intracranial hemorrhage. Stroke. 2010 Dec;41(12):2860–2866. doi: 10.1161/STROKEAHA.110.593087. [DOI] [PubMed] [Google Scholar]
- 8.Morgenstern LB, Hemphill JC, 3rd, Anderson C, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010 Sep;41(9):2108–2129. doi: 10.1161/STR.0b013e3181ec611b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Romualdi E, Micieli E, Ageno W, Squizzato A. Oral anticoagulant therapy in patients with mechanical heart valve and intracranial haemorrhage. A systematic review. Thromb Haemost. 2009 Feb;101(2):290–297. [PubMed] [Google Scholar]
- 10.You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e531S–575S. doi: 10.1378/chest.11-2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Armstrong MJ, Gronseth G, Anderson DC, et al. Summary of evidence-based guideline: periprocedural management of antithrombotic medications in patients with ischemic cerebrovascular disease: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013 May 28;80(22):2065–2069. doi: 10.1212/WNL.0b013e318294b32d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT. Why do patients with atrial fibrillation not receive warfarin? Arch Intern Med. 2000 Jan 10;160(1):41–46. doi: 10.1001/archinte.160.1.41. [DOI] [PubMed] [Google Scholar]
- 13.Fang MC, Stafford RS, Ruskin JN, Singer DE. National trends in antiarrhythmic and antithrombotic medication use in atrial fibrillation. Arch Intern Med. 2004 Jan 12;164(1):55–60. doi: 10.1001/archinte.164.1.55. [DOI] [PubMed] [Google Scholar]
- 14.Hylek EM, D'Antonio J, Evans-Molina C, Shea C, Henault LE, Regan S. Translating the results of randomized trials into clinical practice: the challenge of warfarin candidacy among hospitalized elderly patients with atrial fibrillation. Stroke. 2006 Apr;37(4):1075–1080. doi: 10.1161/01.STR.0000209239.71702.ce. [DOI] [PubMed] [Google Scholar]
- 15.Waldo AL, Becker RC, Tapson VF, Colgan KJ. Hospitalized patients with atrial fibrillation and a high risk of stroke are not being provided with adequate anticoagulation. J Am Coll Cardiol. 2005 Nov 1;46(9):1729–1736. doi: 10.1016/j.jacc.2005.06.077. [DOI] [PubMed] [Google Scholar]
- 16.Carlile M, Nicewander D, Yablon SA, et al. Prophylaxis for venous thromboembolism during rehabilitation for traumatic brain injury: a multicenter observational study. J Trauma. 2010 Apr;68(4):916–923. doi: 10.1097/TA.0b013e3181b16d2d. [DOI] [PubMed] [Google Scholar]
- 17.Levy AS, Salottolo K, Bar-Or R, et al. Pharmacologic thromboprophylaxis is a risk factor for hemorrhage progression in a subset of patients with traumatic brain injury. J Trauma. 2010 Apr;68(4):886–894. doi: 10.1097/TA.0b013e3181d27dd5. [DOI] [PubMed] [Google Scholar]
- 18.Phelan HA, Wolf SE, Norwood SH, et al. A randomized, double-blinded, placebo-controlled pilot trial of anticoagulation in low-risk traumatic brain injury: The Delayed Versus Early Enoxaparin Prophylaxis I (DEEP I) study. The journal of trauma and acute care surgery. 2012 Dec;73(6):1434–1441. doi: 10.1097/TA.0b013e31825ac49e. [DOI] [PubMed] [Google Scholar]
- 19.Zielinski MD, Smoot DL, Stubbs JR, Jenkins DH, Park MS, Zietlow SP. The development and feasibility of a remote damage control resuscitation prehospital plasma transfusion protocol for warfarin reversal for patients with traumatic brain injury. Transfusion. 2013 Jan;53( Suppl 1):59S–64S. doi: 10.1111/trf.12037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. [Accessed November the 1st, 2013, 2013];Chronic Conditions Data Warehouse: Condition Categories. 2013 https://www.ccwdata.org/web/guest/condition-categories.
- 21.Garwood CL, Corbett TL. Use of anticoagulation in elderly patients with atrial fibrillation who are at risk for falls. Ann Pharmacother. 2008 Apr;42(4):523–532. doi: 10.1345/aph.1K498. [DOI] [PubMed] [Google Scholar]
- 22.Man-Son-Hing M, Nichol G, Lau A, Laupacis A. Choosing antithrombotic therapy for elderly patients with atrial fibrillation who are at risk for falls. Arch Intern Med. 1999 Apr 12;159(7):677–685. doi: 10.1001/archinte.159.7.677. [DOI] [PubMed] [Google Scholar]
- 23.Choudhry NK, Anderson GM, Laupacis A, Ross-Degnan D, Normand SL, Soumerai SB. Impact of adverse events on prescribing warfarin in patients with atrial fibrillation: matched pair analysis. Bmj. 2006 Jan 21;332(7534):141–145. doi: 10.1136/bmj.38698.709572.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferrera PC, Bartfield JM, D'Andrea CC. Outcomes of admitted geriatric trauma victims. Am J Emerg Med. 2000 Sep;18(5):575–580. doi: 10.1053/ajem.2000.9266. [DOI] [PubMed] [Google Scholar]
- 25.Raji MA, Lowery M, Lin YL, Kuo YF, Baillargeon J, Goodwin JS. National utilization patterns of warfarin use in older patients with atrial fibrillation: a population-based study of Medicare Part D beneficiaries. Ann Pharmacother. Jan;47(1):35–42. doi: 10.1345/aph.1R515. [DOI] [PMC free article] [PubMed] [Google Scholar]


