Abstract
While a number of factors have been linked with excessive anxiety (e.g., parenting, child temperament), the impact of stressful life events remains under-studied. Moreover, much of this literature has examined bivariate associations rather than testing more complex theoretical models. The current study extends the literature on life events and child anxiety by testing a theory-driven meditational model. Specifically, one child factor (child cognitions/locus of control), two parent factors (parent psychopathology and parenting stress), and two parent-child relationship factors (parent-child dysfunctional interaction and parenting style) were examined as mediators in the relationship between stressful life events and severity of child anxiety. One hundred and thirty anxious parents and their nonanxious, high-risk children (ages ranged from 7 to 13 years) participated in this study. Results indicated that levels of parenting stress, parental anxious rearing, and dysfunctional parent-child interaction mediated the association between stressful life events and severity of anxiety symptoms. Child cognition and parent psychopathology factors failed to emerge as mediators. Findings provide support for more complex theoretical models linking life events and child anxiety and suggest potential targets of intervention.
Keywords: stressful life events, parent stress, child anxiety
Introduction
Epidemiologic studies have estimated that greater than 20% of individuals meet criteria for an anxiety disorder by the age of 26 and that receiving a diagnosis of any anxiety disorder during childhood or adolescence predicts impairments in physical, financial, and interpersonal functioning in young adulthood [1]. Moreover, pediatric anxiety disorders predict adult anxiety, depressive and substance use disorders [2]. As such, understanding factors that contribute to the development of pediatric anxiety disorders will inform both their treatment and prevention. Numerous factors have been linked with the development of pediatric anxiety disorders including parental psychopathology [3, 4], parenting behaviors (e.g., overcontrol, rejection, negativity, lack of warmth) [5], parent-child attachment [6], family environment (including level of cohesion and conflict) [7], child temperament [8], child’s cognitive bias [9], and the occurrence of stressful life events [10, 11].
Of these contributing factors, stressful or negative life events (as opposed to severe traumatic events) have received little empirical attention in the study of pediatric anxiety disorders despite evidence that they are common and can have detrimental impacts on a child’s mental health and overall functioning [12, 13]. Extant studies that have examined the link between non-traumatic stressful life events (e.g., parent divorce, loss of a grandparent, relocation) and anxiety disorders or symptoms have found that children diagnosed with an anxiety disorder are more likely to have experienced a stressful life event in the recent past than non-anxious children [10, 14–16]. Likewise, families reporting increasing numbers of stressful life events also report higher levels of both parent and child anxiety symptoms [11]. Related work has examined the effect of specific types of life events such as arrival of a step-parent [11], divorce [17], and teasing [18] on childhood anxiety symptoms. In general, the presence of the life event has been associated with higher anxiety symptoms.
While this literature has served to identify stressful life events as an important correlate of child anxiety, one major limitation of these studies is the reliance on bivariate associations. This type of analysis provides very little information regarding the likely complex associations that exist between these constructs. As such, the focus of this study was on testing a more complex theoretical model, which attempts to identify potential mechanisms that may account for the association between stressful life events and higher anxiety. Toward this end, the current study focuses on exploring the contribution of several potential mediating variables, which have been previously identified within the literature as being significantly associated with symptoms of child anxiety. These variables fell within three broad domains, including: 1) parent factors (parental psychopathology and parenting stress); 2) child factors (distorted cognition/locus of control); and 3) parent-child relational factors (parenting and parent-child relationship dysfunction). A brief review of the literature on these potential mediators follows.
Parent Factors
A variety of parent and family factors have been associated with child anxiety [19]. Notwithstanding the effects of life events, children of parents with psychiatric disorders, compared to those without a psychiatric disorder, are at particularly high risk for development of anxiety, [20] and greater risk with greater severity of parental impairment [21]. However, the mechanism of this increased risk and the nature of the pathway towards the child’s development of anxiety appears to be complex, with heritability explaining only a third of the variance in anxiety symptoms [7]. Environmentally, anxious parents may communicate increased threat, either verbally or through modeling of anxious behavior, as they may be less equipped to model adaptive coping in the context of stressful life events [22]. Additionally, though it is more frequently studied in the context of externalizing behaviors, parenting stress (i.e., a parent’s perception of child-rearing competence, conflict with his or her spouse or partner regarding parenting, and stressors associated with the restrictions placed on other life roles as the result of being a parent) has also been found to be a significant mediator between stressful life events (such as child health or parent health problems, death of family member, family conflict, and financial problems) and child adjustment (including internalizing symptoms and social inhibition) [23] and has independently been associated with development of anxiety disorders in adolescents [24, 25]. Thus, we speculate that negative life events will exacerbate parental symptoms of psychopathology and stress, which in turn will lead to an increase in child anxiety symptoms.
Child Factors
Maladaptive cognitions have long been linked to the etiology and maintenance of anxiety [26] and are a primary target of evidence-based therapies for anxiety. Perceived control is one cognitive factor through which both adult and child cognitions are understood. Perceived control (also referred to as locus of control; LOC) and particularly an external locus of control, which refers to the tendency to expect that outcomes are the result of external forces rather than one’s own behavior or competence, has been linked to both parent and child anxiety [27]; and an external LOC in childhood has been associated with risk for a number of adverse physical and mental health outcomes in adulthood [28]. Experimentally, external LOC has predicted the development of increased anxiety in the setting of a stressful event, for example a high-stakes school test [29]. In this model, we speculate that negative life events may increase a child’s external LOC, which in turn will lead to higher anxiety.
Parenting and Parent-Child Relationship Factors
As noted above several parenting behaviors (e.g., over protection, rejection and control) and aspects of the parent-child relationship have been linked to higher anxiety in children (30, 7) Mechanistically, overprotective or controlling parenting (i.e., not allowing a child to do as many things as other children) may limit the opportunities for a child to develop coping skills and encourages an avoidant coping style which increases anxiety, and which may be particularly relevant when a child is confronted with a stressor [31, 32], while an anxious rearing style (characterized by excessive worry and concern about children’s safety and well-being) may exacerbate the perceived threat of a stressful life event to the child (33). Similarly, a negative or dysfunctional parent-child relationship (in which parent feels dissatisfaction with the child or with the parent-child relationship) may also undermine children’s perceived competence to cope with adversity (34, 35). Conversely, warm, nurturing parenting and a positive parent-child relationship may buffer the effect of a stressful life event (i.e., peer victimization) on child anxiety in children with a fearful temperament [36]. Thus, negative life events may impact parenting behaviors and the parent-child relationship, either by increasing or decreasing the use of anxiety – promoting behaviors, which in turn will affect levels of child anxiety. These models were tested in the present study.
Current Study
The current study explored theory-driven child and parent meditators that may account for the association between negative life events and child anxiety symptoms. These models were examined within a high-risk sample (i.e., offspring of anxious parents), as it has been well documented that children of parents with an anxiety disorder are at a particularly high risk for developing anxiety [38]. Using data drawn from a larger study on offspring of anxious parents [20], the current study examined two parent factors (parent psychopathology and parenting stress), one child factor (distorted cognition/LOC), and two parent-child relationship factors (parenting behaviors and parent-child dysfunctional interactions) as possible mediators. Based on prior studies we hypothesized that each of the above constructs would mediate the relationship between stressful life events and child anxiety.
Method
Participants
Participants included 130 children between the ages of 7 and 13 years (M=8.82, SD=1.75) and slightly over half were female (n=72, 55.4%). See Table 1 for full sample demographics. Study design excluded children meeting DSM-IV criteria for an anxiety disorder at baseline; thus, none of the children included in this sample were rated by independent evaluators as exhibiting clinically significant symptoms of anxiety at the time of inclusion (see Methods for a description of the diagnostic evaluations). The children included in this sample were primarily European American (n=110, 84.6%), and from two parent families (n=115, 88.5% were married) with high-income backgrounds (n=101, 77.7% earning over $80,000 or more per year). All parents met DSM-IV diagnostic criteria for a current and primary anxiety disorder, and over half (n=73; 54%) met criteria for a secondary diagnosis; the most common primary diagnosis in this sample was generalized anxiety disorder (GAD; n=89; 68.5%), followed by social phobia (n=16; 12.3%), panic disorder with agoraphobia (n=11; 8.5%), obsessive compulsive disorder (n=7; 5.4%), panic disorder without agoraphobia (n=5; 3.8%), and specific phobia (n=2; 1.5%). Inter-rater agreement for parental diagnoses on a random 25% of video-recorded administrations of the Anxiety Disorders Interview Schedule-Client Version was 97%.
Table 1.
Sample Demographics
| Parent | Child | |
|---|---|---|
| Age | M=40.78 (SD=5.1) | M=8.82 (SD=1.7) |
| Ethnicity: | ||
| European American | n=110; 84.62% | |
| African American | n=9; 6.92% | |
| Other ethnicity | n=11; 8.46% | |
| Marital Status: | ||
| Married | n=116; 89.23% | |
| Divorced | n=9; 6.92% | |
| Separated/Never married | n=5; 3.85% | |
| Level of Education: | ||
| Did not complete college | n=16; 12.31% | |
| College degree | n=52; 40% | |
| Advanced degree | n=61; 46.92% | |
| No response | n=1; 0.77% | |
| Family Income: | ||
| Under $50,000 | n=6; 4.62% | |
| $49,999 – 80,000 | n=22; 16.92% | |
| Over $80,000 | n=101; 77.69% | |
| No Response | n=1; 0.77% | |
Procedure
Families were recruited as part of a larger study examining the impact of a prevention program for children of parents with anxiety disorders [20]. Interested families contacted study staff by phone and completed a phone screen. Families who met preliminary inclusion and exclusion criteria completed an in person evaluation, which included all measures described below. Parents provided written informed consent for their participation in the study, as well as their child’s participation. All children provided informed assent. The study was approved and conducted in compliance with Institutional Review Board guidelines. Children who required assistance with completing study questionnaires were aided by a trained research assistant without their parents present. Trained independent evaluators (IEs) administered the semi-structured diagnostic interviews to parents and children. All data was collected prior to participation in the intervention.
Measures
Stressful Life Events
Coddington Life Events Scale (LES)
The LES is a 35-item measure completed by the parent that assesses children’s exposure to a range of stressful life events within the past 6 months and their lifetime [39]. It is the most widely used life events scale for school age children and has acceptable psychometric properties [39]. Given that the current study sought to explore the impact of stressful life events on the likelihood of the child to exhibit symptoms of anxiety, parental valence ratings of how good (i.e., how pleasant or how happy it made the child) or how bad (i.e., how sad, angry, or scared it made the child) each event was for the child were used to create a frequency count of stressful life events for each parent-child dyad. Life events rated by the parent as either “bad” or “neither good nor bad” for the child were summed together to create a composite stressful life event variable. One hundred and one parents reported at least one stressful life event as having had either a bad or neither good nor bad impact on their child (range=11, M=2.73, SD=2.16). See Table 2 for a summary of the life events reported by the current sample.
Table 2.
Stressful life events and the frequency of occurrence within the current sample
| Life Event | Frequency | Percent of Sample |
|---|---|---|
| Death of a grandparent | 39 | 30% |
| Mother beginning to work | 37 | 28.46% |
| Increase in number of arguments between parents/guardians | 26 | 20% |
| Change in parent’s income | 26 | 20% |
| A close friend moved away | 24 | 18.46% |
| Increase in number of arguments between you and your child | 22 | 16.92% |
| Beginning another school year | 20 | 15.38% |
| Loss of a job by a parent/guardian | 20 | 15.38% |
| Fighting with or problems with friends | 19 | 14.62% |
| Change in father’s job requiring increased absence from home | 15 | 11.54% |
| Serious illness requiring hospitalization of parent/guardian | 14 | 10.77% |
| Move to a new home or neighborhood | 13 | 10% |
| Marital separation of parents/guardian | 12 | 9.23% |
| Brother or sister leaving home | 11 | 8.46% |
| Serious illness requiring hospitalization of brother or sister | 10 | 7.69% |
| Birth of a brother or sister | 10 | 7.69% |
| Divorce of parents/guardian | 10 | 7.69% |
| Move to new school district | 6 | 4.62% |
| Serious illness requiring that he/she stay in hospital | 5 | 3.85% |
| Marriage of parent/guardian to stepparent | 4 | 3.08% |
| Having a visible deformity | 3 | 2.31% |
| Change in your acceptance by peers | 2 | 1.54% |
| Death of a brother or sister | 2 | 1.54% |
| Death of a parent/guardian | 1 | 0.77% |
| Jail sentence of parent/guardian | 1 | 0.77% |
| Decrease in number of arguments between you and your parents/guardians | 1 | 0.77% |
| Decrease in number of arguments between parents/guardians | 1 | 0.77% |
| Addition of third adult to family (i.e., grandparent, etc.) | 1 | 0.77% |
| Suspension from school | 1 | 0.77% |
| Failure of a grade in school | 1 | 0.77% |
| Death of a close friend | 1 | 0.77% |
| Discovering that he/she was adopted | 1 | 0.77% |
Child Symptomatology
Anxiety Disorders Interview Schedule for DSM-IV, Child and Parent Versions (ADIS-IV-C/P)
The ADIS-IV-C/P is a semi-structured interview, which provides the direct assessment of a broad range of anxiety, mood, and externalizing behavior disorders in youth, and screens for the presence of several additional disorders including developmental, psychotic, and somatoform disorders [40]. Interviews are conducted by independent evaluators (IEs) with both child and parent separately. IEs completed training on administering the interview and have achieved acceptable diagnostic reliability. The IE generates an impairment rating for each diagnosis using the Clinician Severity Rating (CSR, range = 0 – 8; > 4 required to assign a diagnosis). Discrepancies in parent and child report are reconciled in accordance with the procedural guidelines specified by Silverman and Albano’s Clinician Manual [40]. Given that none of the children enrolled in the study met criteria for an anxiety diagnosis, CSR scores for each of the anxiety disorders were summed to create one composite score of anxiety impairment. The ADIS-IV-C/P has good test-retest reliability (r=0.98 for the parent interview and r=0.93 for the child interview) [41] and good inter-rater reliability (e.g., k=0.76 for the child interview and k=0.67 for the parent interview) [42, 43].
Parent Psychopathology
Brief Symptom Inventory (BSI)
This 55-item measure is completed by the parent and provides an efficient dimensional measure of parental psychopathology [44]. The BSI measures nine dimensions of symptoms: somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Both convergent and construct validity with other measures of psychopathology have been demonstrated for this scale [45]. Research on the BSI has been conducted with ethnically diverse samples and demonstrated acceptable reliability and validity [46]. For the purposes of this study, the global severity index was used and strong internal consistency was achieved within this sample (Cronbach’s alpha = .95).
Parenting Stress
Parenting Stress Index-Short Form (PSI)
The short form of the PSI is comprised of 36 items, which are rated by the parent on a 5-point Likert scale (i.e., 1 = “strongly disagree” and 5 = “strongly agree”), with higher scores indicating greater degrees of distress [47, 48]. The short form of the PSI consists of three subscales: parenting stress, difficult child, and parent-child dysfunctional interaction. Higher scores indicate greater levels of distress in that domain. For the purposes of this study, the parenting stress subscale was chosen from this measure as an indicator of the parent’s level of distress resulting from the demands of raising a child. Some example items from this subscale include: “I feel myself giving up more of my life to meet my children’s needs than I ever expected.” “I feel alone and without friends.” Cronbach’s alpha in the current sample was .88 for the total parenting stress subscale.
Distorted Cognitions
Perceived Control Scale (PCS)
The PCS, completed by children, contains 24 items and is designed to assess a child’s perceptions with regard to their ability to control outcomes across several domains of functioning (academic, social, and behavioral) [49]. Children are asked to read each statement and rate it on a 4-point Likert scale (i.e., “very false” = 1, “sort of false” = 2, “sort of true” = 3, and “very true” = 4) in terms of how much that statement is representative of how they think. The PCS has high internal consistency among clinical samples of children (Cronbach’s alpha ≥.88) [50, 51]. For the purposes of this study, the total control subscale was used and Cronbach’s alpha for this scale was .86. Higher scores represent greater internal LOC.
Parent-Child Dysfunctional Interaction
For purposes of this study, the parent-child dysfunctional interaction subscale from the PSI (see description above under Parenting Stress) was used as an indicator of the parent’s degree of dissatisfaction about interactions with their child and their acceptance of their child. Some example items from this subscale include: “Sometimes I feel my child doesn’t like me and doesn’t want to be close to me.” “My child is not able to do as much as I expected.” Cronbach’s alpha in the current sample was .80 for the parent-child dysfunctional interaction subscale.
Parenting Behavior
Egna Minnen Betraffande Uppfostran (EMBU)
The EMBU (Swedish for “My memories of upbringing”) completed by both parents and children consists of 40 items designed to assess perceptions of parental rearing behaviors [52]. The child-report version is designed to assess the child’s perception of their parent’s behavior and the parent-report is designed to assess the parent’s perception of their own parenting behavior. Scores from the EMBU yield four subscales, which are comprised of 10 items each: overprotection/control, emotional warmth, rejection, and anxious rearing. Items are rated on a 4-point Likert scale (i.e., 1 = “No”, 2 = “Yes, but seldom”, 3 = “Yes, often”, 4 = “Yes, most of the time”). Parental rejection, overcontrol, and parental anxious rearing have demonstrated positive correlation with anxiety symptoms in children and adolescents [53, 54]. In terms of the current sample, internal consistencies for the four subscales of the child version were generally acceptable (Cronbach’s alphas on the child version ranged from .63 to .73). Internal consistency of the overprotection subscale on the parent version was poor for this sample (Cronbach’s alpha = .51), thus this subscale was omitted from all analyses. Internal consistencies for the three remaining subscales fell within acceptable range (Cronbach’s alphas ranging from .66 to .74).
Statistical Analysis Plan
All data were analyzed using SPSS, Version 20 [55]. To test for mediation, the degree of indirect effects for the variables of interest (i.e., parent psychiatric symptoms, parenting stress, child distorted cognition/LOC, parenting behavior, and parent-child dysfunctional interaction) was examined with regard to the relationship between the independent variable (IV; stressful life events) and the dependent variable (DV; CSR scores). That is, the total effect of the IV on the DV is calculated from the direct effect (c) of the IV on the DV, as well as the indirect effect (c’) of the IV on the DV through the mediator variable. Separate regression models were constructed examining parent factors (parent psychiatric symptoms and parenting stress), child factors (distorted cognition/LOC), and parent-child factors (parenting behavior and parent-child dysfunctional interaction).
Results
Descriptive Analyses
Means and bivariate correlations for all variables are presented in Table 3. Both the independent (total number of stressful life events) and dependent variables (ADIS-IV C/P CSR scores) were examined for significant correlations with the demographic variables (child age, child gender, child race, marital status, and family income). The total number of stressful life events was significantly positively correlated with ADIS-IV C/P CSR scores (r2=0.14, p=0.02) and child age (r2=0.45, p<0.001). Further, total number of stressful life events was significantly negatively correlated with family income (r2=−0.15, p<0.01). Children from divorced families reported the highest frequency of stressful life events (M=7.54; SD=2.67), followed by single families (M=4.69; SD=1.32), married families (M=3.85; SD=1.85), and separated families (M=2.00).
Table 3.
Descriptive statistics and two-tailed bivariate Pearson correlations for all variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child Age | - | .334** | .187* | −.016 | −.097 | .033 | −.106 | −.180* | .052 | .078 | −.194* | .083 | .087 | .190* | .062 |
| 2. Parent Age | - | −.006 | −.079 | .066 | −.076 | −.306** | −.187* | .048 | −.029 | −.224* | −.100 | −.071 | −.042 | .173 | |
| 3. Stressful Life Events (IV) | - | .018 | .041 | .156 | .195 | .032 | −.034 | .064 | .055 | .198* | .160 | .119 | −.011 | ||
| 4. Anxiety Severity (DV; ADIS-C CSR) | - | −.033 | .242* | .272** | .145 | .030 | −.061 | .279** | .098 | .165 | .170 | −.078 | |||
| 5. Parent-Report Emotional Warmth (EMBU-P) | - | −.266** | .113 | .049 | .224* | −.137 | .066 | .151 | −.370** | −.336** | .192 | ||||
| 6. Parent-Report Rejection (EMBU-P) | - | .113 | −.131 | −.251* | .127 | −.124 | .185 | .473** | .342** | −.226* | |||||
| 7. Parent-Report Anxious Rearing (EMBU-P) | - | .240* | −.030 | .093 | .308** | .305** | .099 | −.048 | −.038 | ||||||
| 8. Child- Report Overcontrol (EMBU-C) | - | .366** | .176 | .587** | .082 | −.076 | −.096 | .050 | |||||||
| 9. Child-Report Emotional Warmth (EMBU-C) | - | −.200* | .192* | −.104 | −.260** | −.216* | .361** | ||||||||
| 10. Child-Report Rejection (EMBU-C) | - | .241** | .056 | .226* | .077 | −.249** | |||||||||
| 11. Child-Report Anxious Rearing (EMBU-C) | - | −.027 | −.136 | −.100 | .056 | ||||||||||
| 12. Parent Psychopathology (BSI) | - | .409** | .279** | −.098 | |||||||||||
| 13. Total Parent Stress (PSI) | - | .809** | −.292** | ||||||||||||
| 14. Parent-Child Dysfunctional Interaction (PSI) | - | −.316** | |||||||||||||
| 15. Child Distorted Cognition (PCS) | - | ||||||||||||||
| Mean | 8.82 | 40.78 | 4.43 | 8.02 | 35.48 | 15.52 | 23.45 | 33.14 | 25.06 | 14.00 | 24.38 | 1.02 | 80.42 | 21.47 | 62.64 |
| SD | 1.75 | 5.08 | 2.38 | 4.34 | 2.91 | 2.83 | 4.21 | 4.29 | 4.49 | 3.43 | 4.85 | 0.60 | 16.72 | 7.03 | 7.79 |
| Range | 6.00 | 26.00 | 10.00 | 25.00 | 14.00 | 14.00 | 20.00 | 20.00 | 23.00 | 15.00 | 25.00 | 3.16 | 108.00 | 41.00 | 37.00 |
Notes:
p < 0.05
p < 0.01
IV Independent Variable; DV Dependent Variable; ADIS-C CSR Anxiety Disorders Interview Schedule for DSM-IV, Child Version Clinician Severity Rating; EMBU-P Egna Minnen Betraffande Uppfostran, Parent Version; BSI Brief Symptom Inventory; PSI Parenting Stress Index – Short Form; PCS Perceived Control Scale
Hypothesis Testing
First, a regression equation was constructed with total number of stressful life events entered as the independent variable and ADIS-IV C/P CSR scores entered as the dependent variable. To statistically control for their effects on the relationships examined in this model, child age, child gender, marital status, and family income were entered into Block 1 of the model as covariates. For each of the models, multicollinearity was evaluated in terms of contribution to the overall model using variance inflation factor (VIF; values > 10 are considered problematic) and tolerance (values less than .1 are considered problematic) values. All VIFs and tolerance values fell within acceptable limits. Results of testing the overall model indicated that stressful life events and covariates, predicted a significant proportion of the variance in child anxiety symptoms (r2=0.29; F(5, 316)=5.72, p <.001) and stressful life events uniquely predicted ADIS-IV C/P CSR scores after controlling for child age, child gender, marital status, and family income (β=0.44; t=3.61, p<0.001). See figure 1 for an illustration of the results from hypothesis testing.
Figure 1.
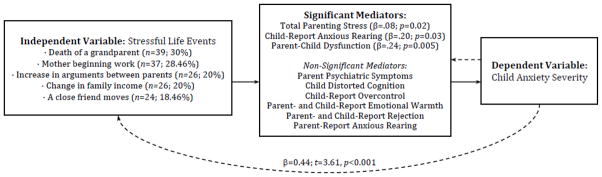
Mediation model of the association between stressful life events and child anxiety severity (r2=0.29; F(5, 316)=5.72, p <.001]. Covariates considered in the model include: child age, child gender, marital status, and family income.
Parent Factors
Next, a regression model was constructed using the SPSS PROCESS macro with bootstrapping [56] in order to test two parent factors (parent psychiatric symptoms and parenting stress) as mediators of this association. This model tested for the direct effects of stressful life events on ADIS- IV C/P CSRs. Indirect effects through parent psychiatric symptoms (BSI) and total parenting stress (PSI) were then calculated in order to demonstrate that a mediation relationship exists [57]. Child age, child gender, marital status, and family income were included in the model as covariates. The overall model predicted a significant portion of the variance in ADIS- IV C/P CSR scores (r2=0.29; F(3, 90)=2.71, p=0.05). Further, total parenting stress (PSI) was found to fully mediate the relationship between stressful life events and anxiety symptom severity ratings (β=.08; r2=0.37; F(5, 88)=2.74, p=0.02). In terms of parent psychiatric symptoms, this variable failed to emerge as a mediator in the association between stressful life events and anxiety severity; however, bivariate correlations revealed a positive association between stressful life events parent psychiatric symptoms (r2=0.36, p<0.001).
Child Factors
A second regression model was constructed to test one child factor (child distorted cognition/LOC) as a mediator of the association between stressful life events and ADIS-IV C/P CSRs. This model tested for the direct effects of stressful life events on ADIS-IV C/P CSRs. Indirect effects through child’s distorted cognition/LOC (PCS) were then calculated. Child age, child gender, marital status, and family income were included in the model as covariates. Results indicated that the overall model failed to reach statistical significance in predicting ADIS-IV C/P CSR scores after controlling for child age, child gender, marital status, and family income (r2=0.20; F(6, 90)=0.61, p=0.72).
Parent-Child Factors
A third regression model was constructed to test the two parent-child factors (parenting behavior and parent-child dysfunctional interaction) as mediators of the association between stressful life events and ADIS-IV C/P CSRs. This model tested for the direct effects of stressful life events on ADIS-IV-C/P CSRs. Indirect effects through parenting behavior (EMBU scales) and parent-child dysfunction (PSI) were then calculated. Responses from both parent and child on the EMBU were considered within the model with the exception of parent-reported overprotection, which was excluded owing to poor internal consistency of the items included in this subscale (see discussion in Measures section). Child age, child gender, marital status, and family income were included in the model as covariates. The overall model predicted a significant portion of the variance in ADIS-IV C/P CSR scores (r2=0.39; F(11, 62)=3.08, p=0.002). More specifically, the individual factors of child-reported (but not parent reported) anxious rearing (β=.20; r2=0.16; F(5, 70)=2.72, p=0.03) and parent-child dysfunction (β=.24; r2=0.21; F(5, 70)=3.71, p=0.005) were found to fully mediate the relationship between stressful life events and anxiety severity. All other subscales of both parent- and child-reported parenting behaviors failed to reach statistical significance as mediators of the association between stressful life events and anxiety severity.
Discussion
Stressful life events during childhood are common and have been found to contribute to excessive anxiety. The mechanisms of this association, however, are not well understood. As such, this study sought to explore various parent and child factors that may mediate the relationship between stressful life events and symptoms of anxiety during childhood. The factors chosen for the present study were identified in previous work as having a significant association with child anxiety and included: 1) parent factors (i.e., psychopathology and distress associated with parenting); 2) child factors (i.e., distorted cognition/LOC); and 3) parent-child relationship factors (i.e., parenting behaviors and parent-child dysfunctional interaction). The current study specifically examined this mediational model within a sample of parents who have been diagnosed with an anxiety disorder, as their offspring are at an elevated risk for developing anxiety disorders themselves [22].
Parent Factors
We hypothesized that levels of parental mental health symptoms and parenting stress would mediate the relationship between stressful life events and child anxiety. Contrary to our hypothesis, level of parent symptomatology did not emerge as a significant mediator. This is partially in line with a recent longitudinal study of the development of child depressive symptoms in which the effect of life events on child symptoms (in this case depressive symptoms) was more pronounced when there was not a family history of mood or anxiety disorder [58]. The authors of this study suggested that there may be separate pathways to depression onset in children; one driven primarily by stress (in this case, life events) and another driven more by familial risk. Although the current sample was composed solely of families with familial risk (i.e., diagnosed parent anxiety disorders), our findings could suggest that the association between life events and child anxiety is primarily “stress mediated” and independent of the parent’s level of psychopathology (which may reflect a genetic vulnerability that exists regardless of the occurrence of stressful life events). Conversely, in the sample, parenting stress was found to mediate the effect of stressful life events on child anxiety levels. This suggests that the occurrence of external stressful life events such as school problems, illness of a family member, or arguments between family members may directly increase parents’ sense of parenting incompetence, conflict, or frustration which may in turn increase child anxiety symptoms. This explanation is also consistent with a “stress mediated” pathway, such that stress responses, independent of parental psychopathology, are transmitted from parent to child.
Child Factors
Contrary to our hypothesis, in this sample, a child’s sense of perceived control over events and outcomes in their life did not mediate the relation between stressful life events and child anxiety, nor was it directly associated with level of anxiety symptoms or number of stressful life events. One potential explanation for this finding is the measure of perceived control used in the current study was not anxiety-specific; anxiety-specific attributions of control have been found to be better predictors of anxiety symptoms [59]. In addition, it is possible that the life events most frequently reported by the current sample (i.e.; death of grandparent) were ones in which an internal LOC was less relevant. Finally, the impact of cognitive development and maturation should be considered. It is possible that LOC was less relevant in our sample age range than it may be in older children or adolescents (in which LOC is more frequently studied), as cognitive development appears to have a significant role in differential expression of anxiety symptoms by age [60].
Parent-Child Relationship Factors
Our results supported child-reported anxious rearing style and parent reported dysfunctional parent-child interaction as mediating the relationship between stressful life events and child anxiety measures. Neither parental overcontrol (as reported by the child) warmth, nor rejection (as reported by both parent and child) emerged as significant mediators of this relationship.
The significance of anxious rearing (characterized by excessive worry and concern about children’s safety and well-being) as a mediator is consistent with past studies in which children as young as 15 to 20 months have been noted to exhibit fearful and avoidant responses in the setting of maternal anxious modeling [61]. It is likely that a parent who demonstrates significant worry and concern about a child’s well-being might increase that behavior in the setting of a stressor that could affect the child’s well-being, which may in turn increase the child’s level of anxiety.
Parent-child dysfunctional interaction (as measured by the subscale on the PSI which assesses the parent’s level of dissatisfaction about interactions with his/her child and their acceptance of the child) was also found to be a significant mediator of the life events-child anxiety relationship, suggesting that stressful life events may increase a parent’s level of dissatisfaction with the child or parent-child relationship, and that this dissatisfaction may increase a child’s level of anxiety. Prior studies in the setting of family focused interventions for depression have suggested that parents who are sensitive to and accepting of difficult emotions in their children may promote the development of the child’s emotion regulation and coping skills and be more likely to be viewed as a source of support during times of stress for the child [62]. Our findings suggest that similar targets (e.g. parent acceptance of the child) are relevant to preventive interventions for anxiety as well.
Taken together, these findings have clinical applications and suggest that in the setting of stressful life events (which occur frequently in both clinical and nonclinical samples), for school-age children, interventions which target the parent’s level of parenting distress (e.g. resources or groups for parent support), parental expectations of and satisfaction with the parent-child relationship (e.g. psychoeducation regarding expectations of child behaviors and abilities at different ages) and parenting behavior (particularly anxious rearing style) may be particularly helpful in reducing child anxiety or preventing increase in anxiety levels. For those treating an anxious parent, it may be important to periodically ask about stressful life events in the family, stress and behaviors related to parenting, and satisfaction with the parent-child relationship in order to identify children who may be at higher risk for developing clinically significant anxiety symptoms. Conversely, since the current findings did not find that child cognitions, at least perceived control, significantly mediated the relation between stressful life events and child anxiety symptoms, that interventions for children experiencing such events, stand-alone child and cognition-focused interventions (i.e., Cognitive Behavioral Therapy) may not be as helpful or sufficient.
Limitations
The current study is not without limitations. This study was cross-sectional in nature, thus causality cannot be assumed. Additional prospective studies are warranted to more clearly delineate the causal links between these variables and the child and parent factors that may mediate the effect of stressful life events on symptoms of child anxiety. The sample included in this study was predominantly European American and of relatively high socioeconomic status with two biological parents and, therefore, the results may not be generalizable to other settings or patient populations. Prior studies have suggested that individuals with lower socioeconomic status are more likely to experience stressful life events, and that the relationship between socioeconomic status and a number of mental health outcomes may be mediated by the experience of these stressful life events [66]. The presence of parental anxiety disorders may have had a significant impact on parent report of measures (including the Life Events Scale, and Parent Child Dysfunctional Interaction). Including the child’s report of the salience of life events and the quality of parent child interaction would have added an additional perspective to the study, as these may be distinct from the parents’ perception. While we were able to use child observation of parenting behaviors, we did not have a similar measure of child perception of dysfunctional interaction. It should be noted that the children included in this study, by definition, were not diagnosed with an anxiety disorder and, therefore, did not exhibit clinically significant symptoms of anxiety. As such, this study considered severity ratings of sub-clinical anxiety symptoms, which may have restricted statistical power and partially account for the lack of significant associations among several of the variables considered. The current study examined total number of life events rather than specific types of life events due to the limited range of events within specific domains and global rather than domain specific anxiety symptoms. However, prior studies have supported the correlation of specific types of life events with the onset of particular anxiety disorders; for instance, the arrival of a step-parent has been linked with symptoms of generalized anxiety disorder [11], separation from caregivers and marital discord has been linked with symptoms of separation anxiety [67], and episodes of teasing during childhood have been linked with symptoms of social phobia during adolescence [68]. Additionally, we did not have data on the timing of life events aside from whether they occurred within the 6 months prior to the study or ever. Having more specific information on the timing of events would have likely have added significant value to our findings, as it the timing of exposure to stressful life events (particularly early ones) likely has important effect on later expression of symptoms (69) While it was possible to draw some conclusions with regard to associations among the variables and child age, the restricted age range of children in the study included does not allow us to generalize either to preschool or adolescent age children. On the other hand, it is possible that an even more restricted age range may have produced more robust or developmentally specific findings as our sample spanned ages 7–13. Finally, a limited number of mediators were examined in the current study—other potential mediators and moderators such as child or family’s social support or parent-child attachment require further examination. Despite these limitations, the current study provides a significant contribution to the literature by exploring several potential mediators on the relationship between stressful life events and child anxiety.
Summary
Anxiety disorders are among the most prevalent mental health disorders occurring during childhood [2, 4]. Moreover, children of anxious parents are at a particularly high risk for developing an anxiety disorder themselves, [38]. While numerous factors have been linked with excessive anxiety, the impact of stressful life events remains under-studied [10–11, 38]. Most extant studies, which examined the relation between life events and childhood symptoms of anxiety, have used two variable correlational designs [13]. The present study examined several potential child and parent factors as mediators in the relationship between stressful life events and severity of child anxiety within a sample of high-risk children.
Findings indicated that child cognitions did not mediate the relationship between number of stressful life events and the extent of anxiety symptoms. In terms of the parent factors, total parenting stress mediated the relationship between stressful life events and severity of child anxiety, but parent psychopathology did not. With respect to the parent-child interaction, anxious rearing style and parent-child dysfunctional interaction mediated the relationship between stressful life events and severity of anxiety symptoms. Taken together, these findings extend our understanding about the mechanisms by which life events affects child anxiety levels and suggest that interventions targeting parenting stress and parent-child relationship quality in high-risk, school-aged children (e.g., who have a family history of anxiety or who have experienced a number of stressful life events) may be beneficial.
References
- 1.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch Gen Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32:483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eley T, Bolton D, O’Conner T, Perrin S, Smith P, Plomin R. A twin study of anxiety-related behaviours in pre-school children. J Child Psychol Psychiatry. 2003;44:945–960. doi: 10.1111/1469-7610.00179. [DOI] [PubMed] [Google Scholar]
- 4.Hettema JM, Neale MC, Kendler KS. A review and meta-analysis of the genetic epidemiology of anxiety disorders. Am J Psychiatry. 2001;158:1568–1578. doi: 10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- 5.Wood JJ, McLeod BD, Sigman M, Hwang WC, Chu BC. Parenting and childhood anxiety: Theory, empirical findings, and future directions. J Child Psychol Psychiatry. 2003;44:134–151. doi: 10.1111/1469-7610.00106. [DOI] [PubMed] [Google Scholar]
- 6.Colonnesi C, Draijer EM, Jan JM, Stams G, Van der Bruggen CO, Bögels SM, et al. The relation between insecure attachment and child anxiety: A meta-analytic review. J Clin Child Adolesc Psychol. 2011;40:630–645. doi: 10.1080/15374416.2011.581623. [DOI] [PubMed] [Google Scholar]
- 7.Drake KL, Ginsburg GS. Family factors in the development, treatment, and prevention of childhood anxiety disorders. Clin Child Fam Psychol Rev. 2012;15:144–162. doi: 10.1007/s10567-011-0109-0. [DOI] [PubMed] [Google Scholar]
- 8.Hudson JL, Dodd HF, Lyneham HJ, Bovopoulous N. Temperament and family environment in the development of anxiety disorder: Two-year follow-up. J Am Acad Child Adolesc Psychiatry. 2011;50:1255–1264. doi: 10.1016/j.jaac.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 9.Affrunti NW, Ginsburg GS. Exploring parental predictors of child anxiety: The mediating role of child interpretation bias. Child Youth Care Forum. 2012;41:517–527. doi: 10.1007/s10566-012-9186-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dougherty LR, Tolep MR, Bufferd SJ, Olino TM, Dyson M, Traditi J, et al. Preschool anxiety disorders: Comprehensive assessment of clinical, demographic, temperamental, familial, and life stress correlates. J Clin Child Adolesc Psychol. 2013;42:577–589. doi: 10.1080/15374416.2012.759225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grover RL, Ginsburg GS, Ialongo N. Childhood predictors of anxiety symptoms: A longitudinal study. Child Psychiatry Hum Dev. 2005;36:133–153. doi: 10.1007/s10578-005-3491-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim KJ, Conger RD, Elder GH, Lorenz FO. Reciprocal influences between stressful life events and adolescent internalizing and externalizing problems. Child Dev. 2003;74:127–143. doi: 10.1111/1467-8624.00525. [DOI] [PubMed] [Google Scholar]
- 13.McLaughlin KA, Greif Green J, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry. 2012;69:1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luby JL, Belden AC, Spitznagel E. Risk factors for preschool depression: The mediating role of early stressful life events. J Child Psychol Psychiatry. 2006;47:1292–1298. doi: 10.1111/j.1469-7610.2006.01672.x. [DOI] [PubMed] [Google Scholar]
- 15.Tiet QQ, Bird HR, Hoven CW, Moore R, Wu P, Wicks J, et al. Relationship between specific adverse life events and psychiatry disorders. J Abnorm Child Psychol. 2001;29:153–164. doi: 10.1023/a:1005288130494. [DOI] [PubMed] [Google Scholar]
- 16.Gothelf D, Aharonovsky O, Horesh N, Carty T, Apter A. Life events and personality factors in children and adolescents with obsessive-compulsive disorder and other anxiety disorders. Compr Psychiatry. 2004;45:192–198. doi: 10.1016/j.comppsych.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Lansford JE, Malone PS, Castellino DR, Dodge KA, Pettit GS, Cates JE. Trajectories of internalizing, externalizing, and grades for children who have and have not experienced their parents’ divorce or separation. J Fam Psychol. 2006;20:292–301. doi: 10.1037/0893-3200.20.2.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCabe RE, Antony MM, Summerfeldt LJ, Liss A, Swinson RP. Preliminary examination of the relationship between anxiety disorders in adults and self-reported history of teasing or bullying experiences. Cogn Behav Ther. 2002;32:187–193. doi: 10.1080/16506070310005051. [DOI] [PubMed] [Google Scholar]
- 19.Wei C, Kendall PC. Parental Involvement: Contribution to childhood anxiety and its treatment. Clin Child Fam Psychol Rev. 2014 doi: 10.1007/s10567-014-0170-6. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Ginsburg GS, Drake KL, Tein JY, Teetsel R, Riddle MA. Preventing the Onset of Anxiety Disorders in Offspring of Anxious Parents: A Randomized Controlled Trial of a Family-based Intervention. American Journal of Psychiatry. doi: 10.1176/appi.ajp.2015.14091178. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schreier A, Wittchen HU, Höfler M, Lieb R. Anxiety disorders in mothers and their children: Prospective longitudinal community study. Br J Psychiatry. 2008;192:308–309. doi: 10.1192/bjp.bp.106.033589. [DOI] [PubMed] [Google Scholar]
- 22.Burstein M, Ginsburg GS. The effect of parental modeling of anxious behaviors and cognitions in school-aged children: An experimental pilot study. Behav Res Ther. 2010;48:506–515. doi: 10.1016/j.brat.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ostberg M, Hagekull B. Parenting stress and external stressors as predictors of maternal ratings of child adjustment. Scand J Psychol. 2013;54:213–221. doi: 10.1111/sjop.12045. [DOI] [PubMed] [Google Scholar]
- 24.van Oort FVA, Verhulst FC, Ormel J, Huizink AC. Prospective community study of family stress and anxiety in (pre)adolescents: The TRAILS study. Eur Child Adolesc Psychiatry. 2010;19:483–491. doi: 10.1007/s00787-009-0058-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams NL, Shahar G, Riskind JH, Joiner TE. The looming maladaptive style predicts shared variance in anxiety disorder symptoms: Further support for a cognitive model of vulnerability to anxiety. J Anxiety Disord. 2005;19:157–175. doi: 10.1016/j.janxdis.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 26.Becker KD, Ginsburg GS, Domingues J, Tien JY. Maternal control behavior and locus of control: Examining mechanisms in the relation between maternal anxiety disorders and anxiety symptomatology in children. J Abnorm Child Pyschol. 2010;38:533–543. doi: 10.1007/s10802-010-9388-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gale CR, Batty DG, Deary IJ. Locus of control at age 10 years and health outcomes and behaviors at age 30 years: The 1970 British Cohort Study. Psychosom Med. 2008;70:397–403. doi: 10.1097/PSY.0b013e31816a719e. [DOI] [PubMed] [Google Scholar]
- 28.Li HCW, Chung OKJ. The relationship between children’s locus of control and their anticipatory anxiety. Public Health Nurs. 2009;26:153–160. doi: 10.1111/j.1525-1446.2009.00766.x. [DOI] [PubMed] [Google Scholar]
- 29.Edwards SL, Rapee RM, Kennedy S. Prediction of anxiety symptoms in preschool-aged children: Examination of maternal and paternal perspectives. J Child Psychol Psychiatry. 2010;51:313–321. doi: 10.1111/j.1469-7610.2009.02160.x. [DOI] [PubMed] [Google Scholar]
- 30.Lieb R, Wittchen HU, Höfler M, Fuetsch M, Stein MB, Merikangas KR. Parental psychopathology, parenting styles, and the risk of social phobia in offspring: A prospective-longitudinal community study. Arch Gen Psychiatry. 2000;57:859–866. doi: 10.1001/archpsyc.57.9.859. [DOI] [PubMed] [Google Scholar]
- 31.de Wilde A, Rapee RM. Do controlling maternal behaviors increase state anxiety in children’s responses to a social threat? A pilot study. J Behav Ther Exp Psychiatry. 2008;39:526–537. doi: 10.1016/j.jbtep.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 32.Burstein M, Ginsburg GS. The effect of parental modeling of anxious behaviors and cognitions in school-aged children: An experimental pilot study. Behav Res Ther. 2010;48:506–515. doi: 10.1016/j.brat.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Waters AM, Zimmer-Gembeck MJ, Farrell LJ. The relationships of child and parent factors with children’s anxiety symptoms: Parental anxious rearing as a mediator. Journal of Anxiety Disorders. 2012;26(7):737–45. doi: 10.1016/j.janxdis.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 34.Hudson JL, Rapee RM. Parent-child interactions and anxiety disorders: An observational study. Behav Res Ther. 2001;39:1411–1427. doi: 10.1016/s0005-7967(00)00107-8. [DOI] [PubMed] [Google Scholar]
- 35.Bögels SM, Brechman-Toussaint ML. Family issues in child anxiety: Attachment, family functioning, parental rearing, and beliefs. Clin Psychol Rev. 2006;26:834–856. doi: 10.1016/j.cpr.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 36.Affrunti NW, Geronimi EM, Woodruff-Borden J. Temperament, peer victimization, and nurturing parenting in child anxiety: A moderated mediation. Child Psychiatry Hum Dev. 2014;45:483–492. doi: 10.1007/s10578-013-0418-2. [DOI] [PubMed] [Google Scholar]
- 37.Taboas WR, McKay D, Whiteside SP, Storch EA. Parental involvement in youth anxiety treatment: Conceptual bases, controversies, and recommendations for intervention. J Anxiety Disord. 2014 doi: 10.1016/j.janxdis.2014.12.005. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 38.Vasey MW, Dadds MR. The developmental psychopathology of anxiety. New York, NY US: Oxford University Press; 2001. [Google Scholar]
- 39.Coddington RD. The significance of life events as etiologic factors in the diseases of children: II-A study of a normal population. J Psychosom Res. 1972;16:205–213. doi: 10.1016/0022-3999(72)90045-1. [DOI] [PubMed] [Google Scholar]
- 40.Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV – Child and Parent Versions. San Antonio, TX: Physiological Corporation; 1996. [Google Scholar]
- 41.Silverman WK, Nelles WB. The Anxiety Disorders Interview Schedule for Children. J Am Acad Child Adolesc Psychiatry. 1988;27:772–778. doi: 10.1097/00004583-198811000-00019. [DOI] [PubMed] [Google Scholar]
- 42.Silverman WK, Eisen AR. Age differences in the reliability of parent and child reports of child anxious symptomatology using a structured interview. J Am Acad Child Adolesc Psychiatry. 1992;31:117–124. doi: 10.1097/00004583-199201000-00018. [DOI] [PubMed] [Google Scholar]
- 43.Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. J Am Acad Child Adolesc Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- 44.Derogatis LR, Melisaratos N. The Brief Symptoms Inventory: An introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 45.Boulet J, Boss M. Reliability and validity of the Brief Symptom Inventory. J Consult Clin Psychol. 1991;3:433–437. [Google Scholar]
- 46.Hemmings M, Reimann JO, Madrigal D, Velasquez RJ. Predictors of scores on the Brief Symptom Inventory for ethnically diverse female clients. Psychol Rep. 1998;83:800–802. doi: 10.2466/pr0.1998.83.3.800. [DOI] [PubMed] [Google Scholar]
- 47.Abidin RR. Parenting Stress Index Manual. 3. Lutz, FL: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- 48.Reitman D, Currier RO, Stickle TR. A critical evaluation of the Parenting Stress Index-Short Form (PSI-SF) in a head start population. J Clin Child Adolesc Psychol. 2002;31:384–392. doi: 10.1207/S15374424JCCP3103_10. [DOI] [PubMed] [Google Scholar]
- 49.Weisz JR, Southam-Gerow MA, Sweeney L. The Perceived Control Scale for Children. Los Angeles: University of California, Los Angeles; 1998. [Google Scholar]
- 50.Margaro MM, Weisz JR. Perceived control mediates the relation between parental rejection and youth depression. J Abnorm Child Psychol. 2006;34:867–876. doi: 10.1007/s10802-006-9072-5. [DOI] [PubMed] [Google Scholar]
- 51.Weisz JR, Francis SE, Bearman SK. Assessing secondary control and its association with youth depression symptoms. J Abnorm Child Psychol. 2010;38:883–893. doi: 10.1007/s10802-010-9440-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Perris C, Jacobsson L, Lindström H, Von Knorring L, Perris H. Development of a new inventory for assessing memories of parental rearing behaviour. Acta Psychiatr Scand. 1980;61:265–274. doi: 10.1111/j.1600-0447.1980.tb00581.x. [DOI] [PubMed] [Google Scholar]
- 53.Castro J, Toro J, van der Ende J, Arrindell WA. Exploring the feasibility of assessing perceived rearing styles in Spanish children with the EMBU. Int J Soc Psychiatry. 1993;39:47–57. doi: 10.1177/002076409303900105. [DOI] [PubMed] [Google Scholar]
- 54.Penelo E, Viladrich C, Domenech JM. Adolescents’ perceptions of parental behavior: Psychometric properties of the short Egna Minnen Beträffande Uppfostran-Adolescent version (S-EMBU-A) in a clinical sample. Compr Psychiatry. 2012;53:87–94. doi: 10.1016/j.comppsych.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 55.IBM Corp. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp; 2011. [Google Scholar]
- 56.Hayes AF. Introduction to mediation, moderation, and conditional process analysis. The Guilford Press; New York: 2013. [Google Scholar]
- 57.Baron RM, Kenny DA. The moderator-mediatory variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 58.Bufferd SJ, Doughterty LR, Olino TM, Dyson MW, Laptook RS, Carlson GA, et al. Predictors of the onset of depression in young children: A multi-method, multi-informant longitudinal study from ages 3 to 6. J Child Psychol Psychiatry. 2014;55:1279–1287. doi: 10.1111/jcpp.12252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ginsburg GS, Lambert S, Drake K. Attributions of control, anxiety sensitivity, and panic symptoms among adolescents. Cog Ther Res. 2004;28:745–763. [Google Scholar]
- 60.Broeren S, Muris P. The relationship between cognitive development and anxiety phenomena in children. J Child Fam Stud. 2009;18:702–709. doi: 10.1007/s10826-009-9276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gerull FC, Rapee RM. Mother knows best: Effects of maternal modeling on the acquisition of fear and avoidance behaviors in toddlers. Behav Res Ther. 2002;40:279–287. doi: 10.1016/s0005-7967(01)00013-4. [DOI] [PubMed] [Google Scholar]
- 62.Watson KH, Dubmar JP, Thigpen J, Reising MM, Hudson K, McKee L, Forehand R, Compas BE. Observed Parental Responsiveness/Warmth and Children’s Coping: Cross-Sectional and Prospective Relations in a Family Depression Preventive Intervention. J Fam Psychol. 2014;28(3):278–86. doi: 10.1037/a0036672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brown AM, Whiteside SP. Relations among perceived parental rearing behaviors, attachment style, and worry in anxious children. J Anxiety Disord. 2008;22:263–272. doi: 10.1016/j.janxdis.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 64.Muris P. Parental Rearing Behaviors and Worry of Normal Adolescents. Psychol Rep. 2002;91(2):428–30. doi: 10.2466/pr0.2002.91.2.428. [DOI] [PubMed] [Google Scholar]
- 65.Drake KL, Ginsburg GS. Parenting practices of anxious and non-anxious mothers: A multi-method, multi-informant approach. Child Fam Behav Ther. 2011;33:299–321. doi: 10.1080/07317107.2011.623101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Businelle MS, Mills BA, Chartier KG, Kendzor DE, Reingle JM, Shuval K. Do stressful events account for the link between socioeconomic status and mental health? J Public Health. 2013;36:205–212. doi: 10.1093/pubmed/fdt060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Peleg-Popko O, Dar R. Marital quality, family patterns, and children’s fears and social anxiety. Contemp Fam Ther. 2001;23:465–487. [Google Scholar]
- 68.Boersm GJ, Bale TL, Casanello P, Lara HE, Lucion AB, Suchecki D, Tamashiro KL. Long-term impact of early life events on physiology and behavior. J Neuroendocrinol. 2014;26(9):587–602. doi: 10.1111/jne.12153. [DOI] [PubMed] [Google Scholar]


