Abstract
Background
Little is known about the sexual health behaviors of Deaf American Sign Language (ASL) users.
Objective
We sought to characterize the self-reported sexual behaviors of Deaf individuals.
Methods
Responses from 282 Deaf participants aged 18–64 from the greater Rochester, NY area who participated in the 2008 Deaf Health were analyzed. These data were compared with weighted data from a general population comparison group (N=1890). We looked at four sexual health-related outcomes: abstinence within the past year; number of sexual partners within the last year; condom use at last intercourse; and ever tested for HIV. We performed descriptive analyses, including stratification by gender, age, income, marital status, and educational level.
Results
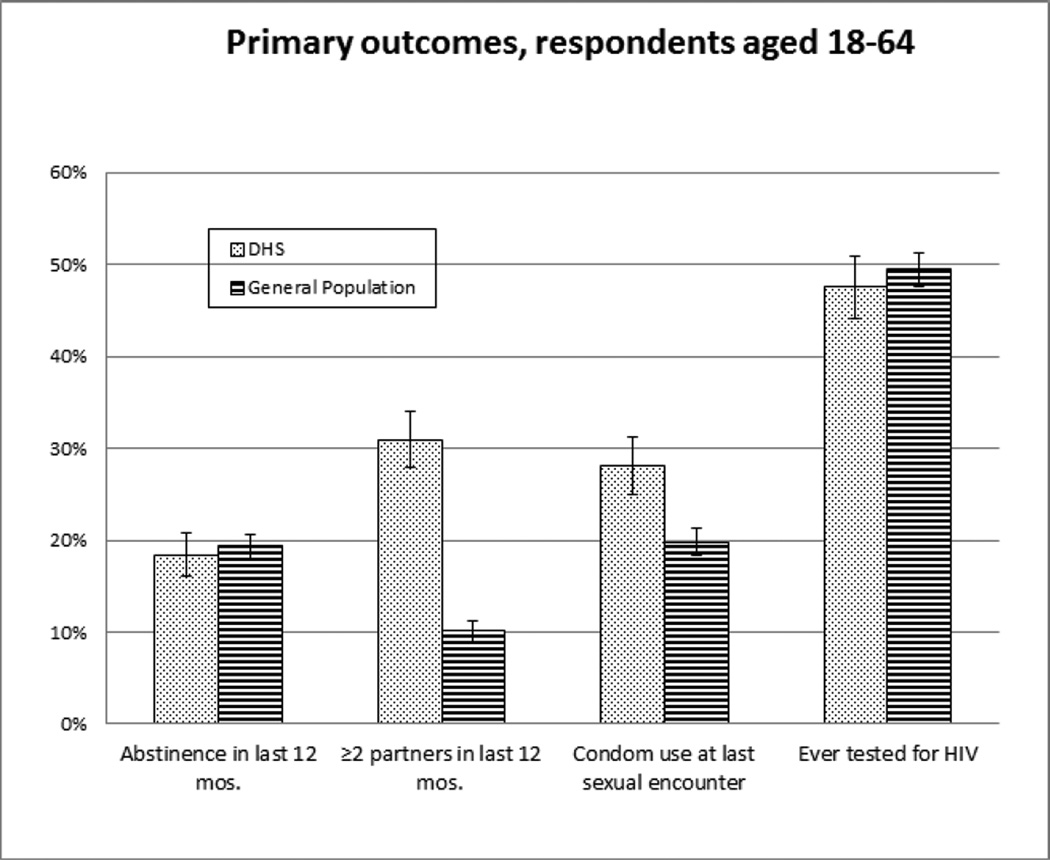
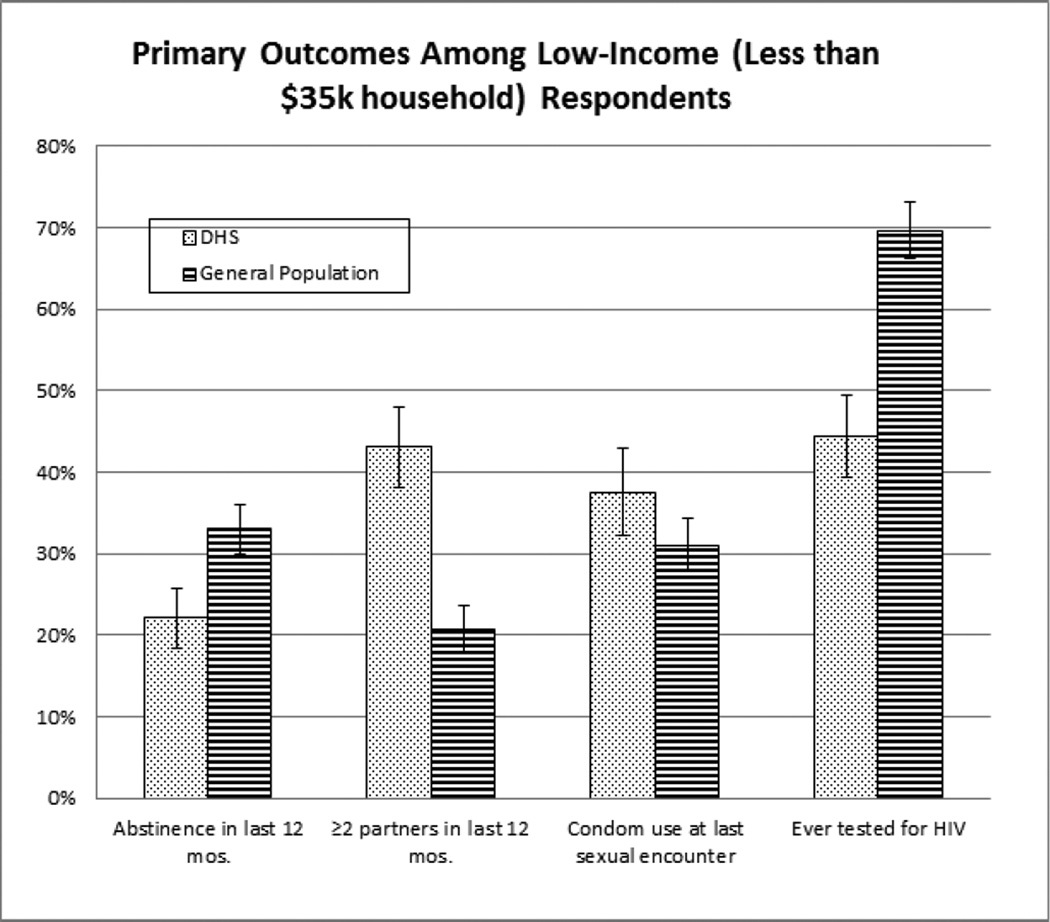
Deaf respondents were more likely than the general population respondents to self-report two or more sexual partners in the past year (30.9% vs 10.1%) but self-reported higher condom use at last intercourse (28.0% vs 19.8%). HIV testing rates were similar between groups (47.5% vs 49.4%) but lower for certain Deaf groups: Deaf women (46.0% vs. 58.1%), lower-income Deaf (44.4% vs. 69.7%) and among less educated Deaf (31.3% vs. 57.7%) than among respondents from corresponding general population groups.
Conclusion
Deaf respondents self-reported higher numbers of sexual partners over the past year compared to the general population. Condom use was higher among Deaf participants. HIV was similar between groups, though HIV testing was significantly lower among lower-income, less well-educated, and female Deaf respondents. Deaf individuals have a sexual health risk profile that is distinct from that of the general population.
Keywords: Deaf health, sexual behavior, STI, HIV, condom use
Introduction
Members of American Deaf communities who communicate primarily in American Sign Language (ASL) view being deaf and using ASL as defining features of their cultural identity. (1) Deaf ASL users may struggle with healthcare marginalization as a result of language, communication, and cultural barriers. (2–5) The marginalization results in significant health disparities and knowledge gaps for this population in a variety of health topics, including sexual health, cancer, preventive health and cardiovascular disease. (6–12) The impact of these gaps appears to result in poorer prevention health care outcomes among Deaf individuals with discordant communication with their health care providers. (6)
There is a lack of accessible high-quality sexual health information in ASL, (9, 13) which may increase the risk for misinformation among members in the Deaf community. (14) Little data has been collected on sexual health behaviors of Deaf individuals. Previous studies have suggested greater prevalence of misunderstandings about HIV and sexually transmitted infections (STIs) among Deaf adults and college students (8, 11), and limited understanding of effective techniques for HIV/STI prevention among Deaf high school students (15, 16) compared with hearing peers. Surveys of Deaf college students found low prevalence of consistent condom usage (34–50%) and an overreliance on withdrawal as a form of contraception. (17, 18) Deaf individuals also face higher risks of child sexual abuse and intimate partner violence (IPV) than is seen in the general population (19–21), which may increase the risk of sexually transmitted infections. Substance use, including alcohol use, may be higher among Deaf adolescents and adults. (22, 23)
We sought to better characterize behaviors relating to the sexual health of Deaf individuals, as self-reported via the innovative survey tool described below.
Methods
The Deaf Health Survey (DHS) is a computer-administered ASL adaptation of CDC’s Behavioral Risk Factor Surveillance System (BRFSS). (24, 25) The DHS was developed through a community-based participatory research (CBPR) process with the Rochester NY Deaf community, and contains 98 items developed through rigorous translations and back-translations between English and ASL. (5, 24, 26) The survey was administered in 2008 to a sample of 339 Deaf adults in the Rochester, NY metropolitan statistical area (MSA). Respondents were recruited at community events, via community organizations, and via emails and posters.
We performed descriptive analyses using data from DHS participants who reported they were between the ages of 18 and 64. To provide comparison with the general population in the Rochester, NY area, respondents from the 2006 Adult Health Survey (AHS) were used. The AHS is a telephone-based BRFSS that was also conducted in Rochester/Monroe County, NY. The AHS data is calibrated post-collection to match Monroe County census data with regards to age, race, sex, and area of residence. Since the AHS did not ask sexual health related questions to respondents aged 65 and older, no DHS respondents aged 65 and older were included in the analysis.
Using these datasets, we looked at four outcome variables: 1) abstinence in the last year; 2) two or more sexual partners within the last year, 3) condom use at last intercourse, 4) and HIV testing (ever). The last three outcomes looked only at respondents who self-reported one or more partners in the previous 12 months, as these outcomes are pertinent only to a sexually active population. We stratified by age, sex, income, education, and marital status. Due to the smaller Deaf sample, the following relationship categories were grouped together to allow for analyses of the 4 listed outcomes. First, persons who reported that they were an unmarried couple were grouped with those who reported being married. Second, persons who reported themselves to be in non-committed relationships (divorced, separated, widowed, single) were similarly grouped together. The AHS utilized complex sampling procedures designed to attain a sample representative of the population, as projected from census data. (27) The DHS utilized a simple sampling technique and could not be weighted due to a lack of existing knowledge or standardized collection of local or national Deaf population demographics. As a result, datasets from DHS and AHS could not be combined.
To test if differences between the two samples were significant, we performed two-sample proportion Z-tests. Differences were considered significant if p-values for two-tailed tests were less than 0.05. Missing values are noted when they represent greater than 5% of the total responses, and are discussed further in the results and discussion sections. All analyses with the AHS were performed with survey weights contained within the dataset, as the AHS utilizes complex sampling and analysis using survey weights is advised. Analyses were done on STATA version 12 (StataCorp. 2011, College Station, TX).
Results
We analyzed data from a total of 282 adult respondents of the Deaf Health Survey, and 1890 adult respondents of the 2006 Monroe County Adult Health Survey. Demographic characteristics are shown in Table 1. Deaf DHS respondents were more likely to be college educated yet had lower median household incomes; they were less likely to be married and more likely to be divorced. There were no differences with respect to gender and age between the two samples of respondents. Missing values represented less than 5% of the total responses in each category except: condom use in the DHS sample, multiple partners in the AHS sample, and household income from both datasets.
Table 1.
Self-Reported Demographic Characteristics
| Deaf Health Survey (N=282) |
Adult Health Survey (N=1890) |
||
|---|---|---|---|
| Gender | N (%) | N (weighted %) | |
| Female | 155 (55.0) | 1228 (51.0) | |
| Male | 127 (45.0) | 662 (49.0) | |
| Age | |||
| 18–34 | 60 (21.3) | 432 (35.7) | |
| 35–64 | 222 (78.7) | 1458 (64.3) | |
| Mean age | 44.6 | 40.5 | |
| Race | |||
| White | 239 (85.7) | 1,448 (80.5) | |
| Black/African-American | 14 (5.0) | 294 (13.3) | |
| Asian or Pacific Islander | 6 (2.1) | 32 (3.0) | |
| American Indian or Alaska Native | 2 (0.7) | 21 (0.7) | |
| Other/multiple selected/missing | 18 (6.5) | 60 (2.6) | |
| Marital Status | |||
| Married | 140 (50.2) | 898 (53.6) | |
| Divorced | 42 (15.1) | 287 (8.9) | |
| Widowed | 1 (0.4) | 68 (1.9) | |
| Separated | 10 (3.6) | 76 (2.2) | |
| Never been Married | 72 (25.8) | 456 (27.1) | |
| Member of an Unmarried Couple | 14 (5.0) | 105 (6.3) | |
| Education | |||
| high school or less | 42 (15.1) | 612 (29.9) | |
| some college or higher | 236 (84.9) | 1276 (70.1) | |
| Annual Household income | |||
| $35,000 or less | 131 (46.5) | 660 (26.8) | |
| more than $35,000 | 131 (46.5) | 1062 (64.4) | |
| Missing/no response | 20 (7.0) | 168 (8.9) | |
Abstinence in the last year was similar between the groups: 18.4% among DHS respondents and 19.3% among AHS respondents (Table 2 and Figure 1). Abstinence was reported less frequently among Deaf respondents with lower income, and among Deaf respondents who were single, divorced, or separated. It was more frequent among Deaf respondents who were married or part of an unmarried couple.
Table 2.
Self-Reported Sexual Health Behaviors of Total Samples and Stratified by Key Demographic Variables
| Deaf Health Survey (N=282)† | Adult Health Survey (N=1890)† |
P-value | |||||
|---|---|---|---|---|---|---|---|
| Total Sample | N (%) | 95% CI | N (%) | 95% CI | |||
| Abstinence in last 12 months | 52 (18.4) | (13.9, 23.0) | 417 (19.3) | (16.6, 22.1) | 0.74 | ||
| *≥2 partners in last 12 mos. | 71 (30.9) | (24.9, 36.9) | 158 (10.1) | (7.9, 12.3) | <0.01 | ||
| *Condom use at last sexual encounter | 58 (28.0) | (21.9, 34.2) | 265 (19.8) | (16.8, 22.8) | 0.02 | ||
| Ever tested for HIV | 104 (47.5) | (40.8, 54.2) | 705 (49.4) | (45.9, 52.9) | 0.61 | ||
| Gender | |||||||
| Female | |||||||
| Abstinence in last 12 months | 35 (22.6) | (15.9, 29.2) | 297 (19.7) | (16.8, 22.6) | 0.43 | ||
| *≥2partners in last 12 mos. | 29 (24.2) | (16.9, 31.9) | 82 (9.1) | (6.3, 11.9) | <0.01 | ||
| Condom use at last sexual encounter | 25 (23.4) | (15.2, 31.5) | 161 (18.2) | (14.7, 21.7) | 0.25 | ||
| *Ever tested for HIV | 52 (46.0) | (36.7, 55.3) | 486 (58.1) | (53.9, 62.2) | 0.02 | ||
| Male | |||||||
| Abstinence in last 12 months | 17 (13.4) | (7.4, 19.4) | 120 (19.0) | (14.3, 23.7) | 0.15 | ||
| *≥2 partners in last 12 mos. | 42 (38.2) | (30.0, 47.4) | 76 (11.1) | (7.7, 14.5) | <0.01 | ||
| *Condom use at last sexual encounter | 33 (33.0) | (23.6, 42.4) | 104 (21.4) | (16.6, 26.3) | 0.03 | ||
| Ever tested for HIV | 52 (49.1) | (39.4, 58.7) | 219 (40.8) | (35.3, 46.2) | 0.35 | ||
| Age | |||||||
| 18–34 | |||||||
| Abstinence in last 12 months | 8 (13.3) | (4.5, 22.2) | 64 (22.0) | (15.8, 28.2) | 0.11 | ||
| *≥2 partners in last 12 mos. | 21 (40.4) | (26.6, 54.2) | 69 (17.6) | (12.3, 22.9) | <0.01 | ||
| Condom use at last sexual encounter | 26 (50.0) | (35.9, 64.1) | 119 (35.8) | (28.9, 42.7) | 0.07 | ||
| Ever tested for HIV | 27 (56.3) | (41.7, 70.8) | 249 (59.9) | (52.6, 67.2) | 0.65 | ||
| 35–64 | |||||||
| Abstinence in last 12 months | 44 (19.8) | (14.5, 25.1) | 353 (17.8) | (15.5, 20.1) | 0.49 | ||
| *≥2 partners in last 12 mos. | 50 (28.1) | (21.4, 34.8) | 89 (6.0) | (4.4, 7.6) | <0.01 | ||
| *Condom use at last sexual encounter | 32 (20.7) | (14.2, 27.1) | 146 (11.1) | (9.0, 13.3) | 0.01 | ||
| Ever tested for HIV | 77 (45.0) | (37.5, 52.6) | 456 (43.7) | (40.0, 47.4) | 0.75 | ||
| Income | |||||||
| Less than $35,000 | |||||||
| *Abstinence in last 12 months | 29 (22.1) | (14.9, 29.3) | 232 (33.0) | (27.0, 39.0) | 0.02 | ||
| *≥2 partners in last 12 mos. | 44 (43.1) | (33.3, 52.9) | 86 (20.7) | (14.9, 26.6) | <0.01 | ||
| Condom use at last sexual encounter | 32 (37.6) | (27.1, 48.2) | 124 (31.0) | (24.6, 37.5) | 0.29 | ||
| *Ever tested for HIV | 44 (44.4) | (34.5, 54.4) | 276 (69.7) | (63.0, 76.5) | <0.01 | ||
| More than $35,000 | |||||||
| Abstinence in last 12 months | 21 (16.0) | (9.7, 22.4) | 149 (12.9) | (10.0, 15.9) | 0.38 | ||
| *≥2 partners in last 12 mos. | 20 (18.2) | (10.9, 25.5) | 62 (7.0) | (4.8, 9.3) | <0.01 | ||
| Condom use at last sexual encounter | 22 (20.4) | (12.7, 28.1) | 122 (15.9) | (12.5, 19.4) | 0.30 | ||
| Ever tested for HIV | 56 (52.8) | (43.2, 62.5) | 392 (44.2) | (40.0, 48.4) | 0.10 | ||
| Education | |||||||
| High school or less | |||||||
| Abstinence in last 12 months | 9 (21.4) | (8.5, 34.4) | 167 (25.6) | (19.8, 31.4) | 0.55 | ||
| *≥2 partners in last 12 mos. | 16 (48.5) | (30.5, 66.5) | 60 (13.9) | (9.2, 18.7) | <0.01 | ||
| Condom use at last sexual encounter | 5 (17.9) | (2.7, 33.0) | 89 (21.7) | (16.0, 27.4) | 0.63 | ||
| *Ever tested for HIV | 10 (31.3) | (14.3, 48.2) | 245 (57.7) | (50.9, 64.4) | <0.01 | ||
| Some college or higher | |||||||
| Abstinence in last 12 months | 43 (18.2) | (13.3, 23.2) | 248 (16.6) | (13.6, 19.6) | 0.58 | ||
| *≥2 partners in last 12 mos. | 52 (26.9) | (20.6, 33.3) | 98 (8.7) | (6.3, 11.0) | <0.01 | ||
| *Condom use at last sexual encounter | 52 (29.6) | (22.7, 36.3) | 176 (19.1) | (15.6, 22.6) | 0.01 | ||
| Ever tested for HIV | 93 (50.5) | (43.3, 57.8) | 460 (46.3) | (42.3, 50.3) | 0.32 | ||
| Marital status | |||||||
| Married or part of an unmarried couple | |||||||
| *Abstinence in last 12 months | 20 (13.0) | (7.6, 18.4) | 53 (5.4) | (3.7, 7.1) | <0.01 | ||
| *≥2 partners in last 12 mos. | 21 (15.7) | (9.4, 21.9) | 27 (2.4) | (1.3, 3.5) | <0.01 | ||
| *Condom use at last sexual encounter | 26 (21.3) | (13.9, 28.7) | 94 (9.2) | (7.0, 11.4) | <0.01 | ||
| Ever tested for HIV | 55 (43.0) | (34.3, 51.7) | 415 (46.6) | (42.7, 50.6) | 0.45 | ||
| Single, divorced, or separated | |||||||
| *Abstinence in last 12 months | 32 (25.6) | (17.8, 33.4) | 364 (40.6) | (35.0, 46.1) | <0.01 | ||
| *≥2 partners in last 12 mos. | 48 (51.6) | (41.3, 62.0) | 131 (28.8) | (22.5, 35.1) | <0.01 | ||
| Condom use at last sexual encounter | 32 (38.6) | (27.9, 49.2) | 171 (45.4) | (38.2, 52.6) | 0.29 | ||
| Ever tested for HIV | 48 (53.9) | (43.4, 64.5) | 290 (56.1) | (48.8, 63.4) | 0.74 | ||
Denotes 95% confidence of significant difference between proportions
Total N for condom use and HIV testing analyses includes only sexually active respondents. For DHS: N=230; for AHS: N=1358.
Confidence intervals are reported by percentage, not number of respondents.
Figure 1.
The four primary study outcomes for Deaf Health Survey respondents and general population (Monroe County) respondents. Total DHS N=282, Monroe County N=1890. Error bars denote +/− one SD.
The other three study outcomes focused on the survey populations who reported sexual activity within the last year. Among respondents who did report sexual activity in the last year (N=230 for DHS, N=1358 for AHS), Deaf individuals were significantly more likely to report two or more sexual partners in the past year (30.9%, 95% CI 24.9, 36.9) when compared with the general population (10.1%, 95% CI 7.9, 12.3) (Table 2 and Figure 1). Condom use at last intercourse was significantly different between the two groups, with Deaf individuals reporting higher rates of condom use at last sexual encounter (28.0% vs 19.8%). Ever having HIV testing between Deaf and the general population did not significantly differ (Table 2 and Figure 1).
Among female respondents, those who were Deaf reported significantly lower levels of HIV testing versus their hearing counterparts (46.0% vs 58.1%). The same finding applied to lower income and lower education respondents, with Deaf people reporting significantly lower rates of HIV testing. Deaf respondents who were male, married, or more educated were more likely to report condom use at last sexual intercourse than their general population counterparts.
Discussion
This is the first known study comparing sexual behaviors of Deaf respondents with the general population. Deaf respondents appear more likely to engage in sexual activity with multiple partners (two or more partners in the past year) when compared with the general population. A higher number of reported sexual partners places individuals at higher risk for sexually transmitted diseases. It is possible that Deaf individuals may underestimate the risk associated with more sexual partners. This may be due to limited access to high-quality sexual health information in ASL. Deaf individuals struggle with lower health literacy and knowledge when compared with the general population. (7, 14, 28)
In the general population, sexual health knowledge is not the only determinant of sexual behavior. (29, 30) Having more sexual partners, whether serially or concurrently, may be a more socially acceptable or socially expected behavior within the Deaf community than the general US population. Consistent with this idea is our finding that a lower percentage of Deaf respondents in our analysis reported they were married or within a committed couple, and a higher percentage were divorced. Longer-term partnerships may be less of a feature of Deaf life than among the general population, although there is no previous data to corroborate this notion. Although the partnership categories that we used for our analyses combined different types of relationships -- married or in an unmarried couple vs single, divorced, separated, widowed – the finding of higher levels of multiple partners among Deaf respondents held true when examining individual groups for which sufficient responses were available. For example, married Deaf respondents reported higher levels of multiple partners than married general population respondents (13.9% vs 1.7%), and never married Deaf respondents did likewise (51.9 vs 31.9).
Another possible cause of the disparity in self-reported partnership numbers may be differing reporting tendencies. Social desirability bias is the tendency of respondents to answer in a way that will be viewed favorably by others, (31) and is especially relevant to sexual health research. (32) As a distinct culture, the Deaf community may have different expectations on behaviors, affecting respondents’ reporting of their sexual behaviors. Deaf respondents may thus be more likely to honestly report sexual behaviors than the general population. It is worth noting that there were no missing responses to the question regarding number of sexual partners posed to DHS respondents, but 115 missing responses (approximately 6%) to this question for the AHS.
Anecdotally, the Deaf community appears to be have a higher prevalence of gay, lesbian, bisexual, and transgender sexual orientations. (33) It is unclear how this may affect sexual patterns in the Deaf community as well as the proportion of respondents reporting being married. The data collection preceded the passage of the Marriage Equality Act. This was passed and recognized in the state of New York on July, 2011. The DHS does not contain information regarding sexual orientation.
The increased risk due to higher numbers of partners reported by Deaf respondents may be at least in part mitigated by a somewhat higher condom use. The general population as well as four subgroups of Deaf respondents-- females, those who were older, those more highly educated, and those who were married-- were more likely to report condom use at last sexual encounter than their general population counterparts. This may indicate a relative preference towards condoms over other contraceptive methods within these groups, as compared to the general population. This observation differs somewhat from literature suggesting lower condom use among Deaf college students. (17, 18) The trend towards higher levels of condom use was an encouraging finding yet the rate was still relatively low given that the Deaf community is less likely to be monogamous. However, it is difficult to generalize these findings, given that condom use at last sexual encounter may not represent consistent condom use; that this finding was not observed in all demographic groups; and that our data is limited by missing observations in this data category.
Deaf respondents with lower education and annual household incomes reported lower rates of HIV testing. Although sample sizes for these groups were small (N=40 for education high school or less, N=131 for annual income $35,000 or less), these findings achieved statistical significance. Both low socioeconomic status and low education have been implicated in poorer health outcomes in HIV/AIDS and STIs, for the general public as well as for minority groups. (34, 35) These individuals struggle with additional socioeconomic barriers that may further impede health care access and lack the skills and knowledge necessary to navigate health systems effectively. (36)
There is limited availability of sexual health information in ASL. Further public announcements and outreach programs need to ensure their messages are available in ASL through the use of video-based blogs (vlogs) and ASL-fluent community educators. Clinicians should use ASL interpreters to facilitate health communication. Our findings indicate that members of the Deaf community may be at risk for STIs based on the self-reported number of sexual partners in the past year. Lower income and less educated Deaf individuals may be at particular high risk and should be a group of concern for health care providers and systems. Health care practitioners and public health officials should be aware of these risk factors when interacting with Deaf patients, and designing culturally and linguistically appropriate programs aimed towards promoting improved sexual health in Deaf communities.
Limitations
The findings of our study represent data from a limited geographic area (greater Rochester, New York area) with a sizeable Deaf community with strong community-based organizations. The Rochester area may also have more accessible healthcare systems for Deaf individuals. Thus, findings may not be generalizable to other Deaf communities where resources may be less available. The DHS and AHS data are both self-reported. Desirability bias is long known to affect sexual health studies, and differing social expectations may lead to significantly different self-reporting. (37) It is unclear if Deaf and the general population differ with social norms in regards to sexual behavior.
The DHS also differed from the AHS in their methods of recruitment and data collection. DHS participants were recruited at Deaf community events and other social functions; the AHS was a random telephone survey. The AHS consisted of weighted data. The DHS is not weighted due to the lack of knowledge on the population’s demographics. Further, the baseline characteristics of DHS respondents differ from the general population (AHS) respondents in some ways. Notably, the DHS contains fewer married respondents. This may have implications for the respondents’ self-reported sexual behavior.
Finally, the problem of missing data is difficult to counter, especially in sexual health research. The question concerning condom use over the last year had a low response in the DHS survey due to a problem in the data collection stage, with survey administrators not posing this question to all of the respondents it was intended for. There were 23 missing observations, which was 10.0% of all sexually active adults. The question regarding number of partners, when posed to the AHS sample, had 6.1% missing responses in the raw sample, and 4.7% missing when examining weighted data. Questions about income had high rates of missing observations in both the DHS and AHS, with 7.0% of DHS responses and 8.9% of AHS responses missing. Our study is similar to any sexual health data set in this regard, with added limitation that self-report may be different between the Deaf and non-Deaf communities, as mentioned above.
Conclusion
This is the first known population-based study evaluating sexual health behaviors among Deaf ASL users in the Rochester NY area. Our analyses indicate that Deaf individuals may have more sexual partners than individuals within the general population. Deaf respondents with lower education levels and lower annual income may have less access to HIV testing than their counterparts in the general population. More research is needed to learn about the sexual health behaviors in Deaf communities and how to best promote healthy sexual practices in higher risk Deaf groups, including lower educated and lower income individuals. Understanding the higher than expected condom usage reported by Deaf respondents can inform interventions with Deaf communities and potentially other populations that remain marginalized from a health care perspective.
Figure 2.
Primary outcomes among DHS and general population respondents who also reported annual household income less than $35,000. DHS N=131, General population N=660. Error bars signify +/− one SD.
Acknowledgments
The authors are grateful for the assistance and support from the National Center for Deaf Health Research and the Deaf Health Community Committee, as well as from the Monroe County Department of Health.
This research was supported by Cooperative Agreement Numbers U48 DP001910 and U48 DP000031 from the US Centers for Disease Control and Prevention (CDC) Prevention Research Centers Program. Dr. McKee is currently supported by grant K01 HL103140 from the National Heart, Lung, and Blood Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors have no further financial disclosures.
The findings reported in this paper were previously presented at the Summit on the Science of Eliminating Health Disparities, December 2012.
Bibliography
- 1.Padden C, Humphries T. Inside deaf culture. Cambridge, Mass: Harvard University Press; 2005. p. 208. [Google Scholar]
- 2.McKee M, Schlehofer D, Thew D. Ethical issues in conducting research with deaf populations. American journal of public health. 2013 Dec;103(12):2174–2178. doi: 10.2105/AJPH.2013.301343. PubMed PMID: 24134363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnett S, McKee M, Smith SR, Pearson TA. Deaf sign language users, health inequities, and public health: opportunity for social justice. Preventing chronic disease. 2011 Mar;8(2):A45. PubMed PMID: 21324259. Pubmed Central PMCID: 3073438. [PMC free article] [PubMed] [Google Scholar]
- 4.Hauser PC, O'Hearn A, McKee M, Steider A, Thew D. Deaf epistemology: Deafhood and Deafness. American annals of the deaf. 2010 Winter;154(5):486–492. doi: 10.1353/aad.0.0120. discussion 93-6. PubMed PMID: 20415284. [DOI] [PubMed] [Google Scholar]
- 5.McKee M, Thew D, Starr M, Kushalnagar P, Reid JT, Graybill P, et al. Engaging the Deaf American sign language community: lessons from a community-based participatory research center. Progress in community health partnerships : research, education, and action. 2012 Fall;6(3):321–329. doi: 10.1353/cpr.2012.0037. PubMed PMID: 22982845. Pubmed Central PMCID: 3576694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McKee MM, Barnett SL, Block RC, Pearson TA. Impact of communication on preventive services among deaf American Sign Language users. American journal of preventive medicine. 2011 Jul;41(1):75–79. doi: 10.1016/j.amepre.2011.03.004. PubMed PMID: 21665066. Pubmed Central PMCID: 3117257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Margellos-Anast H, Estarziau M, Kaufman G. Cardiovascular disease knowledge among culturally Deaf patients in Chicago. Preventive medicine. 2006 Mar;42(3):235–239. doi: 10.1016/j.ypmed.2005.12.012. PubMed PMID: 16460789. [DOI] [PubMed] [Google Scholar]
- 8.Heuttel KL, Rothstein WG. HIV/AIDS knowledge and information sources among deaf and hearing college students. American annals of the deaf. 2001 Jul;146(3):280–286. doi: 10.1353/aad.2012.0067. PubMed PMID: 11523204. [DOI] [PubMed] [Google Scholar]
- 9.Peinkofer JR. HIV education for the deaf, a vulnerable minority. Public health reports. 1994 May-Jun;109(3):390–396. PubMed PMID: 8190862. Pubmed Central PMCID: 1403503. [PMC free article] [PubMed] [Google Scholar]
- 10.Wollin J, Elder R. Mammograms and Pap smears for Australian deaf women. Cancer nursing. 2003 Oct;26(5):405–409. doi: 10.1097/00002820-200310000-00010. PubMed PMID: 14710803. [DOI] [PubMed] [Google Scholar]
- 11.Woodroffe T, Gorenflo DW, Meador HE, Zazove P. Knowledge and attitudes about AIDS among deaf and hard of hearing persons. AIDS care. 1998 Jun;10(3):377–386. doi: 10.1080/09540129850124154. PubMed PMID: 9828980. [DOI] [PubMed] [Google Scholar]
- 12.Tamaskar P, Malia T, Stern C, Gorenflo D, Meador H, Zazove P. Preventive attitudes and beliefs of deaf and hard-of-hearing individuals. Archives of family medicine. 2000 Jun;9(6):518–525. doi: 10.1001/archfami.9.6.518. discussion 26. PubMed PMID: 10862214. [DOI] [PubMed] [Google Scholar]
- 13.Winningham A, Gore-Felton C, Galletly C, Seal D, Thornton M. Lessons learned from more than two decades of HIV/AIDS prevention efforts: implications for people who are deaf or hard of hearing. American annals of the deaf. 2008 Spring;153(1):48–54. doi: 10.1353/aad.0.0002. PubMed PMID: 18619068. Pubmed Central PMCID: 2728086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McKee M, Schlehofer D, Cuculick J, Starr M, Smith S, Chin NP. Perceptions of cardiovascular health in an underserved community of deaf adults using American Sign Language. Disability and health journal. 2011 Jul;4(3):192–197. doi: 10.1016/j.dhjo.2011.04.001. PubMed PMID: 21723526. Pubmed Central PMCID: 3378999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baker-Duncan N, Dancer J, Gentry B, Highly P, Gibson B. Deaf adolescents' knowledge of AIDS. Grade and gender effects. American annals of the deaf. 1997 Dec;142(5):368–372. doi: 10.1353/aad.2012.0344. PubMed PMID: 9439032. [DOI] [PubMed] [Google Scholar]
- 16.Goldstein MF, Eckhardt EA, Joyner-Creamer P, Berry R, Paradise H, Cleland CM. What do deaf high school students know about HIV? AIDS education and prevention : official publication of the International Society for AIDS Education. 2010 Dec;22(6):523–537. doi: 10.1521/aeap.2010.22.6.523. PubMed PMID: 21204628. [DOI] [PubMed] [Google Scholar]
- 17.Doyle A. AIDS Knowledge, Attitudes, and Behaviors among Deaf College Students: A preliminary study. Sexuality and Disability. 1995;13(12):107–134. [Google Scholar]
- 18.Joseph JM, Sawyer R, Desmond S. Sexual knowledge, behavior and sources of information among deaf and hard of hearing college students. American annals of the deaf. 1995 Oct;140(4):338–345. doi: 10.1353/aad.2012.0379. PubMed PMID: 8849663. [DOI] [PubMed] [Google Scholar]
- 19.Sebald AM. Child abuse and deafness: an overview. American annals of the deaf. 2008 Fall;153(4):376–383. doi: 10.1353/aad.0.0059. PubMed PMID: 19146074. [DOI] [PubMed] [Google Scholar]
- 20.Anderson ML, Leigh IW, Samar VJ. Intimate Partner Violence Against Deaf Women: A review. Aggression and Violent Behavior. 2011 May;16(3):200–206. 2011. [Google Scholar]
- 21.Sobsey D, Doe T. Patterns of Sexual Abuse and Assault. Sexuality and Disability. 1991;9(3):243–259. [Google Scholar]
- 22.Rendon ME. Deaf culture and alcohol and substance abuse. Journal of substance abuse treatment. 1992;9(2):103–110. doi: 10.1016/0740-5472(92)90076-z. PubMed PMID: 1512798. [DOI] [PubMed] [Google Scholar]
- 23.Lipton D, Golstein M. Measuring Substance Abuse among the Deaf. Journal of Drug Issues. 1997;27(4):733–754. [Google Scholar]
- 24.Barnett S, Klein JD, Pollard RQ, Jr, Samar V, Schlehofer D, Starr M, et al. Community participatory research with deaf sign language users to identify health inequities. American journal of public health. 2011 Dec;101(12):2235–2238. doi: 10.2105/AJPH.2011.300247. PubMed PMID: 22021296. Pubmed Central PMCID: 3222424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.About BRFSS. [cited 2014 April, 15];2013 Available from: http://www.cdc.gov/brfss/about/index.htm.
- 26.Graybill P, Aggas J, Dean RK, Demers S, Finigan EG, Pollard RQ., Jr A Community-Participatory Approach to Adapting Survey Items for Deaf Individuals and American Sign Language. Field Methods. 2010;22(4):429–448. [Google Scholar]
- 27.Smarr KL, Keefer AL. Patient outcomes in rheumatology, 2011: a review of measures. Measures of depression and depressive symptoms. Arthritis Care & Research (2151464X) 2011;63(11):S454–S466. doi: 10.1002/acr.20556. PubMed PMID: 2011384213. Language: English. Entry Date: 20120217. Revision Date: 20120217. Publication Type: journal article. [DOI] [PubMed] [Google Scholar]
- 28.Bat-Chava Y, Martin D, Kosciw JG. Barriers to HIV/AIDS knowledge and prevention among deaf and hard of hearing people. AIDS care. 2005 Jul;17(5):623–634. doi: 10.1080/09540120412331291751. PubMed PMID: 16036248. [DOI] [PubMed] [Google Scholar]
- 29.Donovan B, Ross MW. Preventing HIV: determinants of sexual behaviour. Lancet. 2000 May;27355(9218):1897–1901. doi: 10.1016/S0140-6736(00)02302-3. PubMed PMID: 10866459. [DOI] [PubMed] [Google Scholar]
- 30.King R. Sexual Behavioural Change for HIV: Where have theories taken us? Geneva: UNAIDS; 1999. 1999. Report No. [Google Scholar]
- 31.Rosenthal R, Persinger GW, Fode KL. Experimenter bias, anxiety, and social desirability. Perceptual and motor skills. 1962 Aug;15:73–74. doi: 10.2466/pms.1962.15.1.73. PubMed PMID: 14494067. [DOI] [PubMed] [Google Scholar]
- 32.Ghanem KG, Hutton HE, Zenilman JM, Zimba R, Erbelding EJ. Audio computer assisted self interview and face to face interview modes in assessing response bias among STD clinic patients. Sexually transmitted infections. 2005 Oct;81(5):421–425. doi: 10.1136/sti.2004.013193. PubMed PMID: 16199744. Pubmed Central PMCID: 1745029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKee M, Hauser PC. Gay and Lesbian Medical Association Conference. Denver, CO: 2013. Sep 15, Addressing Deaf and Hard of Hearing LGBT Individuals' Health Care Needs: A Communication and Cultural Primer. [Google Scholar]
- 34.Dean HD, Fenton KA. Addressing social determinants of health in the prevention and control of HIV/AIDS, viral hepatitis, sexually transmitted infections, and tuberculosis. Public health reports. 2010 Jul-Aug;125(Suppl 4):1–5. doi: 10.1177/00333549101250S401. PubMed PMID: 20629250. Pubmed Central PMCID: 2882967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Joint United Nations Programme on HIV/AIDS. Geneva: UNAIDS; 2007. UNAIDS practical guidelines for intensifying HIV prevention : towards universal access; p. iv.p. 61. [Google Scholar]
- 36.McKee MM, McKee K, Winters P, Sutter E, Pearson T. Higher educational attainment but not higher income is protective for cardiovascular risk in Deaf American Sign Language (ASL) users. Disability and health journal. 2014 Jan;7(1):49–55. doi: 10.1016/j.dhjo.2013.07.001. PubMed PMID: 24411507. Pubmed Central PMCID: 3893794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fenton KA, Johnson AM, McManus S, Erens B. Measuring sexual behaviour: methodological challenges in survey research. Sexually transmitted infections. 2001 Apr;77(2):84–92. doi: 10.1136/sti.77.2.84. PubMed PMID: 11287683. Pubmed Central PMCID: 1744273. [DOI] [PMC free article] [PubMed] [Google Scholar]