Abstract
Background
Despite the widely known benefits of physical activity, people with disabilities are more likely to be inactive when compared to people without disabilities. Previous questionnaires that measure barriers physical activity for people with disabilities do not measure barriers from an ecological perspective.
Objective
The purpose of this study was to develop the Barriers to Physical Activity Questionnaire for People with Mobility Impairments (BPAQ-MI) that measures barriers using an ecological framework.
Methods
This study consisted of two phases. In Phase one, developed the content validity by (a) developing an item bank, (b) identifying missing items and combining items using a Delphi panel, and (c) refine item wording via cognitive interviews. In Phase two, people with mobility impairments took part in in-person interviews to establish test-retest reliability, internal consistency, and construct validity of the BPAQ-MI.
Results
Exploratory factor analysis revealed the BPAQ-MI was comprised of eight subscales or factors: health; beliefs and attitudes; family; friends; fitness center built environment; staff and policy; community built environment; and safety. The BPAQ-MI demonstrated very good test-retest reliability. Cronbach’s alpha ranged from 0.792 to 0.935. The BPAQ-MI showed significant negative correlations with exercise (minutes/week) and significant positive correlations between BPAQ-MI subscales and inactivity (hours/day).
Conclusions
The BPAQ-MI is the first questionnaire that places greater equity at measuring barriers to physical activity across the intrapersonal, interpersonal, organizational, and community domains. The BPAQ-MI has the potential to assist researchers in understanding the complex relationship between barriers and ultimately develop physical activity interventions that address these barriers.
Introduction
Despite the many health benefits of physical activity1, people with disabilities are more likely to be physically inactive (47.1% versus 26.1%)2 or have lower physical activity participation rates (14.7% vs. 34.8%)3 compared to people without disabilities. This disparity in physical activity may be explained by the relationship between individuals with disabilities and their environments.
Human ecological models have examined the interactions by structuring the individual and the environment into four domains of influence (Figure 1) that include: intrapersonal influences, which operate at the personal level and involves health, attitude, and impairment; interpersonal influences, which involves social relationships with family, friends, and professionals; organizational influences, which includes attributes of institutions within the community, such as programs and staff; and community influences, which involve community-at-large variables such as public transportation and the built and natural environment. 4,5
Figure 1.
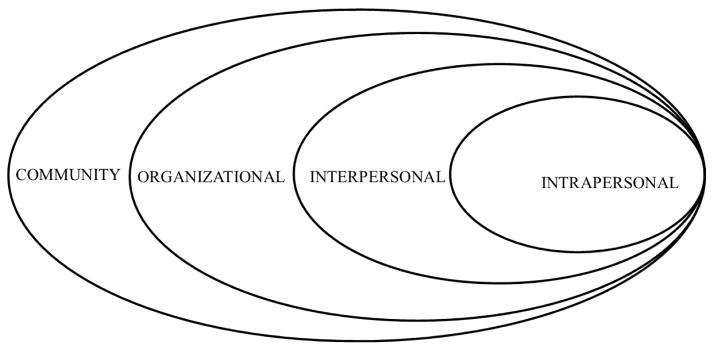
Ecological framework of health promotion
There are barriers to physical activity for people with mobility impairments across all four ecological domains. The most common barriers to physical activity include attitudes and beliefs towards physical activity held by people with mobility impairments, their friends, and their family members6–10, built environment features of fitness centers11–13, and community features such as safety and the built environment.14–17
Seven questionnaires have been used in the measurement of perceived barriers to physical activity for people with mobility impairments. All seven questionnaires had at least 51% of their items within one ecological domain.18–24 Two questionnaires measured barriers within all four ecological domains; 22,23 however the majority of items were within the intrapersonal domain.
The purpose of this manuscript is to describe the development and psychometric properties of a Barriers to Physical Activity Questionnaire for people with mobility impairments (BPAQ-MI) that places approximately equal weight across the four ecological domains.
Methods
There were two phases in this study. Phase I was used for content validity, item development, and item refinement, and Phase II was used for measuring criterion validity, internal consistency, and test-retest reliability. This study was approved by the Institutional Review Board from a large, metropolitan university. Informed written, consent was obtained from all participants.
Phase I: Content Validity
Phase Ia: Item Bank Development
An extensive review of several databases (e.g., MEDLINE and Cumulative Index to Nursing and Allied Health Literature) was conducted to identify both qualitative and quantitative studies that employed questionnaires to identify barriers to physical activity for people with diverse mobility disabilities (e.g. people with arthritis, cerebral palsy, or multiple sclerosis). In order to sample the widest possible range of barriers, both medical subject headings and natural language were used. In order to minimize bias to barrier identification, barriers were included in the item bank if they were identified from qualitative focus groups or interviews, quantitative surveys, or existing questionnaires measuring barriers to physical activity. Questionnaire items that measured multiple topics were split into separate items. For example “Lack of support from friends or family” was separated into two distinct questionnaire items: “Lack of support from friends” and “Lack of support from family.” 6,7,11,18,20,22,23,25–62 The authors have experience promoting physical activity, measuring physical activity barriers, and developing questionnaires. They conceptually categorized the items into the four ecological domains: intrapersonal, interpersonal, organizational, and community.
Phase Ib: Delphi
The Delphi technique was developed by the Rand Corporation in the 1950s and seeks convergence on a topic from a panel of experts.63–66 The Delphi technique is widely used for gathering information from experts of specific topics. For the purposes of this study, convergence pertained to identifying barriers to physical activity within each domain of the ecological model. The Delphi technique was selected because it allowed panelists to work independently of one another while providing constant feedback amongst panelists to generate new information and clarify old information from previous iterations.
Delphi panelists should be highly knowledge on a subject matter.63–66 The inclusion criteria for panelists in this study were that they had peer-reviewed journal articles on either physical activity promotion or measurement of physical activity barriers for people with disabilities. The authors partnered with potential panelists on other studies and programs. The authors reviewed the curriculum vitae for each potential panelist to judge their level of expertise based on the inclusion criteria. The potential panelists had at least ten years of experience at promoting physical activity or measuring barriers to physical activity for people with disabilities. A convenience sample of 15 potential panelists were emailed an information sheet explaining the study and how their expertise could develop a barriers to physical activity questionnaire. Potential panelists emailed the primary author any question they might have had. The potential panelists consented to being a Delphi panelist by responding via email.
While there is no consensus on how many iterations/rounds are needed, it has been generally accepted that three rounds is sufficient to gather enough information to reach consensus.64 In round one, panelists were emailed the item bank and asked to add items that were missing. New items were added without changing any wording. In round two, panelists emailed the updated item bank and asked to combine or remove redundant items. Panelists were asked to provide a reason for why they felt items ought to be combined. Finally, in round three, panelists were asked whether each item should be kept or removed. Items were combined or removed in rounds two and three if there was 70% agreement across panelists. Panelists had two weeks to respond for each round.
Phase Ic: Cognitive Interviews
Cognitive interviews were conducted with 10 individuals with mobility impairments, which is a typical number for that methodology.67,68 Participants were recruited from a convenience sample using flyers from a fitness center that is accessible to people with mobility impairments. Inclusion criteria for the cognitive interviews included: (1) be at least 18 years old; (2) live within Chicago city limits; and (3) have difficulty walking a quarter of a mile or climbing ten stairs without using a mobility aid (e.g., cane, walker, or wheelchair). If the participant self-identified as having a cognitive, sensory, or intellectual disability with no mobility impairments, they were excluded from participating. The cognitive interviews were conducted one-on-one in a private room. Participants were read each of the BPAQ-MI items and were asked for their responses. Participants were asked if they felt an item could be removed and to identify poorly worded or confusing questions. They were asked to provide justification for why they felt the item could be removed. If an item was poorly worded and they were asked to describe the item in their own words and how to reword the item to help with clarification. Information about sex and race was also collected. Participants were paid $50 for their participation.
Phase II: Field Testing
Recruitment
Participants (n=150) were recruited from a fitness center that is accessible to people with mobility impairments and an independent living center from an urban city environment. Participants were recruited using flyers that were posted at the different recruitment facilities, direct mailing, and via snowball recruiting. Inclusion criteria for field testing included: (1) be at least 18 years old; (2) live within Chicago city limits; and (3) have difficulty walking a quarter of a mile or climbing ten stairs without using a mobility aid (e.g., cane, walker, or wheelchair). If the participant self-identified as having a cognitive, sensory, or intellectual disability with no mobility impairments, they were excluded from participating. Interviews were scheduled for 30 minutes and were conducted one-on-one by the primary author in a private room.
Procedure
Participants took part in an in-person interview and completed the BPAQ-MI, Physical Activity and Disability Survey (PADS)69, and the following demographic data were collected: age, gender, race/ethnicity, education, income range, type of mobility impairments, use of a mobility device, self-reported height and weight. Participants were paid $20 for their participation.
The item stem structure of BPAQ-MI was “Thinking over the past three months, were there any times when you wanted to participate in physical activity but couldn’t or found it more difficult because [insert barrier]?” If the participant stated that they did not experience the barrier within the past three months, a score of zero was imputed for that particular item or group of items. If the participant answered “yes”, they were then asked, “In general when you encounter [insert barrier], how much of a barrier was [insert barrier] on a scale from one to five, with one being very small and five being very big?”
The PADS was selected over other physical activity questionnaires and objective physical activity measures because of its ability to measure type of physical activity frequency and duration of each type on a continuous scale, and was validated for a similar population of people with mobility impairments. The PADS measures seven types of physical activity: exercise; leisure time physical activity (LTPA); indoor and outdoor household activities; physical/occupational therapy (PT/OT); active transit; and physical inactivity (hours per day sleeping, watching television, or being on the computer). These seven types of physical activity helped establish criterion validity for the BPAQ-MI’s domains. The PADS has good internal consistency, test-retest, and interrater reliabilities. There were significant correlations between PADS subscales and absolute peak volume oxygen (VO2), relative peak VO2, maximum workload, and time to exhaustion.69
Statistical Analysis
Domain Identification
SPSS version 20.0 statistical software was used for all quantitative analyses.a Exploratory Factor Analysis (EFA) was performed to identify underlying constructs using principal axis factoring extraction and promax (oblique) factor rotation. Principal axis extraction was used to identify the fewest number of factors that could explain the variance of the questionnaire items. Because the ecological model depicts that the domains are related with one another, an oblique rotation was selected because the factors/domains were hypothesized to be correlated with one another. A preliminary EFA using principal axis factoring and varimax (orthogonal) rotation was also conducted to assess if the factors might have been uncorrelated. A minimum eigenvalue of 1.0 was employed and scree plots were used to limit the number of factors. The Kaiser-Guttman rule states that when a factor has an eigenvalue greater than 1.0, the factor accounts for more than the total variance in the items70. To be included, the factor must account for a minimum of five percent of the total item variance. Five percent was selected to assure practical significance in the extracted factors. For items to be included, items must load on selected factors with a minimum loading factor of at least 0.40 to assure strong correlation with other items on that factor. The items also had to be conceptually consistent within subscales.
Domain Scoring
BPAQ-MI domain scores were computed using weighted sums of the items. Coefficients from the factor score correlation matrix were used as the item weights. Domain scores were calculated by summing the products of each item score (0 to 5) with its respective item weight.
Criterion Validity
Criterion validity was assessed by examining the relationship of BPAQ-MI domain scores to physical activity levels calculated by PADS. This involved correlating domain scores with number of minutes per week of various physical activities and across demographic variables.
Internal Consistency
Internal consistency was represented by Cronbach’s alpha (α).71 The minimum, acceptable α score was 0.70. If the subscale had an α less than 0.70, individual items were examined to see if the α increased when that item was removed from the subscale. If α increased significantly when the item was removed, that item was removed from the analysis and α was calculated again.
Test-Retest Reliability
Thirty out of the 150 participants were randomly selected to complete the BPAQ-MI a second time within approximately seven to 14 days of their initial assessment to assess test-retest reliability. The rationale for the seven to 14 days was to have the time period be long enough to prevent participants from recalling their previous responses and short enough that their responses would not change.
Test-retest reliability was calculated using paired t-tests to measure the differences between factor scores at both time points. Domain scores with significant differences between the two time periods (p < 0.05) were deemed unreliable over time.
Results
Phase I: Content Validity
Phase Ia
The item bank was comprised of items from questionnaires that measured barriers to physical activity for people with disabilities as well as barriers described in qualitative studies. The initial version of the item bank was comprised of 112 uniquely-worded items across all four domains of the ecological framework.
Phase Ib
Eleven panelists consented to participate in the Delphi panel, four declined to participate because of other time commitments. Panelists had expertise with either: measuring barriers to physical activity and the accessibility of facilities for people with disabilities (n = 4) and promoting physical activity for people with disabilities in urban and rural environments (n = 4) and for older adults (n = 3). The panelists qualifications include: measuring the accessibility of fitness centers and communities, adapted physical activity, psycho social determinants of physical activity, and developing interventions that are implemented in urban and rural communities.
In round one of the Delphi, panelists added intrapersonal items that related to health and beliefs about physical activity and its effects, interpersonal items that pertained to health care professionals and personal care attendants, organizational items that pertained to the built environment, staff, equipment, and policy, and community items that pertained to crime, weather, and built environment.
In round two, 76 items were combined or deemed redundant with another item. Intrapersonal items that were combined pertained to enjoyability of physical activity, lack of time, medical/health problems, and lack of knowledge on how to be physically active. Interpersonal items that were combined pertained to the training and encouragement of family, friends, and healthcare providers. Organization items that were combined included distance to a fitness center, staff training, and lack of options. Community items that were combined pertained to accessibility of sidewalks, crime, and weather. No items were removed after round two.
In round three, the agreement for items that were included ranged from 0.73 to 1.0. The agreement for items that were removed ranged from 0.45 to 0.64. In the intrapersonal domain, items that were removed were related to the consequences of physical activity and the relationship between caloric intake and energy balance and physical activity. Items were removed regarding family and friends complaining about being physically active and discussion about physical activity in the interpersonal domain. The organizational domain items that were removed included: rudeness of other fitness center patrons, and the amount of disability knowledge held by the fitness center staff. One community domain item about stagnant water or puddles at the crosswalk or curb cut was removed.
Phase Ic
Cognitive interview participants (n=10) were predominantly female (70%) and African American (80%). The participants stated that many items were understandable, but wanted examples or additional words and phrases within parentheses, such as “(e.g. lack of muscle strength or endurance)”. Two items were removed because participants thought the barriers were accurately measured by other items. Another two items were removed because the participants stated that they could not effectively evaluate the other people’s skill at working with someone with a disability or the disability training they received. One item (lack of assistance from fitness center staff) was moved from interpersonal to the organizational domain. In order to speed up the amount of time it took to complete the BPAQ-MI, participants requested skip questions for three topics: having a professional caregiver (four items), living in a group home (two items), and going to a fitness center (28 items).
Phase II: Field Testing
Participant characteristics
Table 1 describes the participant demographics (n = 150). The majority of the study participants were African American (73.3%) and female (55.4%). The mean age of participants was 55.2 years old with a mean body mass index (BMI) of 30.4 kg/m2. The majority of participants (79.3%) used at least one mobility aid, while 38.0% used multiple mobility aids.
TABLE 1.
Participant Demographic Characteristics (n=150)
| % Total | |
|---|---|
| Age (years) | |
| 18–39 | 10.1 |
| 40–59 | 53.0 |
| 60+ | 36.9 |
| BMI (Kg/m2) | |
| Underweight (< 20) | 10.0 |
| Normal Weight (20–24.99) | 22.7 |
| Overweight (25–29.99) | 23.3 |
| Obese (≥ 30) | 44.0 |
| Education | |
| Less than high school | 14.0 |
| High school graduate | 24.7 |
| Some college | 35.3 |
| College graduate | 26.0 |
| Annual Income | |
| Less than $10,000 | 42.7 |
| $10,000 to less than $15,000 | 26.7 |
| More than $15,000 | 30.6 |
| Mobility impairments | |
| Arthritis | 30.0 |
| Stroke | 20.0 |
| Diabetes or heart disease | 19.3 |
| Pain | 18.7 |
| Pulmonary | 12.7 |
| Spinal Cord Injury | 10.0 |
| Neurological | 8.0 |
| Cerebral Palsy | 6.7 |
| Multiple Sclerosis | 6.0 |
| Lymphedema | 4.7 |
| Amputee | 4.0 |
| Mobility Aid | |
| Cane | 50.7 |
| Wheelchair | 36.7 |
| Walker | 30.0 |
| Brace | 12.7 |
| Prosthesis | 4.0 |
Table 2 depicts the amount of physical activity the participants engaged in per week. The majority of participants took part in some form of exercise (79.3%) with participation rates of other types of physical activity ranging from 7.3% (Transit) to 44.0% (Indoor household activities).
TABLE 2.
Physical Activity Overview
| Mean | SD | Min | Max | |
|---|---|---|---|---|
| PADS subscale scores | ||||
| Exercise (min/week) | 189.9 | 170.8 | 0.0 | 690.0 |
| LTPA (min/week) | 27.2 | 128.3 | 0.0 | 1440.0 |
| Indoor (min/week) | 76.7 | 118.8 | 0.0 | 575.0 |
| Outdoor (min/week) | 7.9 | 36.2 | 0.0 | 270.0 |
| PT/OT (min/week) | 15.2 | 41.0 | 0.0 | 240.0 |
| Transit (min/week) | 12.1 | 78.5 | 0.0 | 900.0 |
| Inactivity (hours/day) | 13.8 | 4.4 | 3.5 | 24.0 |
BPAQ-MI overview and psychometric properties
Domain Identification
A preliminary analysis using varimax rotation revealed that important items such as lack of transportation or depression did not load on any factors. Additionally some items loaded on both factors, such as feeling old or believing that physical activity could not help. A promax rotation was ultimately utilized based upon our use of the ecological framework and the preliminary analysis of the EFA using varimax rotation. The ecological framework depicts that the four domains are related with one-another.
The BPAQ-MI took approximately 15–20 minutes to complete. Eight subscales (two within each domain) were extracted from the EFA analysis. The extracted domains described personal health, attitudes/beliefs towards physical activity, friends, family, fitness center built environment, policy, programs, and staff, community built environment, and safety.
Table 3 summarizes the item distribution in BPAQ-MI across the ecological domains, and how the item pool changed after each round of the Delphi, cognitive interviews, and EFA. The item distribution after each phase of the study was: 112 (after phase 1a), 115 (after phase 1b), 111 (after 1c) and 63 (after phase 2).
Table 3.
Item Distribution Across Ecological Domains After Each Study Phase
| Lit Review | Delphi | Cognitive Interview | EFA | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Round 1 | Round 2 | Round 3 | ||||
| Intrapersonal | 37 | 60 | 40 | 34 | 31 | 15 |
| Interpersonal | 37 | 50 | 30 | 27 | 25 | 11 |
| Organizational | 18 | 47 | 31 | 27 | 28 | 21 |
| Community | 20 | 48 | 28 | 27 | 27 | 16 |
|
| ||||||
| Total items | 112 | 205 | 129 | 115 | 111 | 63 |
Domain Scores
Table 4 summarizes barrier scores across each ecological domain and the percentage of study participants who experienced each barrier to physical activity. The health subscale had the highest mean score indicating it was perceived as the greatest barrier to physical activity. The fitness center built environment had the lowest score indicating it was the perceived as a small barrier to physical activity.
Table 4.
BPAQ-MI overview (Domain means, Percentage of participants reporting item as a barrier, and Item weight for domain scoring)
| Mean | % reporting | Item weight | |
|---|---|---|---|
| Health | 2.14 | ||
| you get tired or fatigued | 77.9 | 0.233 | |
| you were in pain | 60.2 | 0.126 | |
| you believe physical activity requires too much work/effort/energy | 59.1 | 0.199 | |
| you didn’t have an appropriate fitness level to be physically active (e.g., lack of aerobic ability) | 57.5 | 0.162 | |
| you felt physical discomfort while being physically active | 56.4 | 0.126 | |
| you were afraid of getting injured while being physically active | 49.2 | 0.122 | |
| you were depressed | 38.1 | 0.081 | |
| Beliefs/Attitudes towards physical activity | 0.89 | ||
| you lack the motivation to be physically active | 43.1 | 0.062 | |
| you don’t have confidence in your ability to be physically active | 28.7 | 0.068 | |
| you were embarrassed about your appearance while being physically active | 28.7 | 0.089 | |
| you have not seen positive results from previous physical activity | 25.4 | 0.143 | |
| you feel you are too old to be physically active | 13.3 | 0.258 | |
| you didn’t think physical activity would help you | 12.2 | 0.127 | |
| being physically active is not enjoyable | 11.5 | 0.240 | |
| you don’t see a reason to be physically fit | 8.8 | 0.229 | |
| Friends | 0.61 | ||
| you did not have another person with a disability who was physically active to look up to | 29.8 | 0.068 | |
| your friends didn’t assist you to be physically active | 29.3 | 0.194 | |
| your friends are not physically active | 26.0 | 0.374 | |
| your friends don’t talk about being physically active | 25.4 | 0.126 | |
| your friends were not encouraging or supportive of your efforts to be physically active | 17.7 | 0.161 | |
| your friend’s priorities take precedence/priority over you being physically active | 16.6 | 0.094 | |
| Family | 0.81 | ||
| your family’s culture, beliefs, or morals did not place physical activity as a priority | 21.0 | 0.169 | |
| your family did not assist you to be physically active | 20.4 | 0.207 | |
| your family members are not physically active | 26.5 | 0.214 | |
| your family members were not encouraging or supportive of your efforts to be physically active | 14.9 | 0.194 | |
| your family did not think physical activity would be helpful to improve your health | 11.6 | 0.232 | |
| Fitness Center Built Environment (FC_BE) | 0.56 | ||
| lack of accessible exercise equipment at fitness center | 18.2 | 0.055 | |
| the walkways/aisles were too narrow or had obstacles | 14.9 | 0.038 | |
| lack of accessible door handles | 13.3 | 0.114 | |
| lack of accessible curb cuts at fitness center | 13.3 | 0.185 | |
| ground that you walk/roll on was not accessible | 10.5 | 0.208 | |
| lack of accessible ramps at fitness center | 9.9 | 0.121 | |
| lack of accessible bathrooms at fitness center | 9.4 | 0.158 | |
| lack of accessible showers/locker rooms | 9.4 | 0.055 | |
| lack of accessible elevators at fitness center | 8.8 | 0.104 | |
| lack of accessible parking at fitness center | 7.7 | 0.055 | |
| lack of access to indoor track for walking/wheeling | 6.0 | 0.034 | |
| Staff/Program /Policy | 0.99 | ||
| fitness center membership fees were too high | 37.0 | 0.145 | |
| your health insurance plan do not cover membership fees | 31.5 | 0.081 | |
| lack of inclusive marketing | 21.5 | 0.049 | |
| lack of accessible classes/programs at fitness center | 18.2 | 0.136 | |
| other fitness center members were mean or rude | 18.2 | 0.094 | |
| lack of accessible walking/rolling paths at parks | 16.0 | 0.195 | |
| lack of assistance from fitness center staff | 15.5 | 0.152 | |
| lack of accessible sport opportunities at fitness center | 15.5 | 0.103 | |
| signs showing where things are located were not accessible | 13.3 | 0.096 | |
| lack of interpretive services (e.g. sign language) | 12.2 | 0.111 | |
| Community Built Environment (C_BE) | 1.30 | ||
| lack of access to public restrooms | 47.0 | 0.042 | |
| uneven or crooked sidewalks | 39.2 | 0.007 | |
| the sidewalks have cracks, gaps, or are under construction | 38.1 | 0.117 | |
| lack of rest areas (e.g. benches) | 36.5 | 0.153 | |
| potholes in the street, driveways, or parking lot | 31.5 | 0.353 | |
| sidewalk’s cross slope is too steep/slanted | 28.7 | 0.089 | |
| the crosswalks lack traffic lights | 27.6 | 0.007 | |
| lack of accessible curb cuts in community | 26.5 | 0.200 | |
| lack of accessible transportation to fitness center | 26.0 | 0.092 | |
| sidewalks were not wide enough | 16.6 | 0.083 | |
| Safety | 1.10 | ||
| excessive crime or fear of crime in neighborhood | 42.0 | 0.078 | |
| the cars drive too fast | 40.9 | 0.227 | |
| excessive car traffic in my community | 37.0 | 0.207 | |
| the traffic lights or crosswalk signals change too quickly | 33.7 | 0.084 | |
| lack of adequate street lighting at night | 23.8 | 0.036 | |
| loose dogs in community | 17.1 | 0.083 |
Reliability
The BPAQ-MI demonstrated moderate to very good internal consistency (Table 5). Cronbach’s alpha ranged from 0.792 (Friends) to 0.935 (Fitness Center Built Environment). No items significantly increased Cronbach’s alpha when the item was removed.
Table 5.
BPAQ-MI Reliability: Internal Consistency
| α | |
|---|---|
| Intrapersonal | |
| Health | 0.857 |
| Beliefs/Attitudes | 0.826 |
| Interpersonal | |
| Friends | 0.792 |
| Family | 0.833 |
| Organizational | |
| FC_BE | 0.935 |
| Staff/Program /Policy | 0.904 |
| Community | |
| C_BE | 0.879 |
| Safety | 0.793 |
The mean number of days between the test and retest periods was 7, with a minimum of 4 and a maximum of 14. There was no significant difference in subscale scores between time periods, thusly the BPAQ-MI demonstrated good test-retest reliability.
Criterion Validity
Table 6 summarizes the correlation of the BPAQ-MI subscales across the physical activity types, age, and BMI. There were moderate, negative correlations between the BPAQ-MI subscales and exercise and moderate positive correlations between the BPAQ-MI subscales and inactivity and BMI. Participants who perceived more barriers reported lower physical activity levels, more time being inactive, and/or had a greater BMI.
Table 6.
Correlation between BPAQ-MI subscale scores and PADS scores
| Exercise | LTPA | Indoor | Outdoor | PT/OT | Transit | Inactivity | |
|---|---|---|---|---|---|---|---|
| Health | −0.241 ** | −0.128 | 0.020 | −0.052 | −0.017 | 0.003 | 0.186 * |
| Beliefs/Attitudes | −0.239 ** | −0.083 | 0.065 | −0.101 | −0.077 | 0.076 | 0.198 * |
| Friends | −0.224 ** | −0.085 | 0.125 | −0.075 | −0.023 | −0.003 | 0.141 |
| Family | −0.174 * | −0.104 | 0.049 | −0.080 | −0.163* | −0.007 | 0.152 # |
| FC_BE | −0.158 # | −0.026 | −0.024 | −0.085 | −0.041 | −0.026 | 0.107 |
| Staff/Program/Policy | −0.166 * | −0.079 | −0.009 | −0.123 | −0.089 | −0.044 | 0.141 # |
| C_BE | −0.142 # | −0.058 | 0.012 | −0.072 | −0.059 | −0.066 | −0.012 |
| Safety | −0.225 ** | −0.044 | 0.051 | −0.124 | −0.059 | −0.006 | 0.157 # |
p < 0.10,
p < 0.05,
p < 0.01
Discussion
When measuring barriers to physical activity for people with disabilities, it is important to have a questionnaire that is capable of barrier measurement within an ecological framework because people interact with their environments in complex ways. Previous questionnaires had at least 51% of their items within one ecological domain. For the BPAQ-MI, approximately equal weight was placed across the four ecological domains.
The BPAQ-MI builds upon previous questionnaires that measure barriers to physical activity to measure barriers across all four ecological domains. Table 7 compares the percentage of items of the BPAQ-MI and previous barrier questionnaires across the ecological domains. The BPAQ-MI has the most items and the greatest proportion of items across the four ecological domains. Because of the complex relationship between the person and their environment72, measurement tools must be capable of identifying the physical activity constructs within the domains of the ecological framework.
Table 7.
Distribution of Questionnaire Items by Ecological Domain
| Number of Items | Intrapersonal | Interpersonal | Organizational | Community | |
|---|---|---|---|---|---|
| BPAQ-MI | 63 | 23.8% | 17.5% | 33.3% | 25.4% |
| EBBS18 | 43 | 88.4% | 4.7% | 2.2% | 4.7% |
| PASSS19 | 20 | 0.0% | 100.0% | 0.0% | 0.0% |
| BHPAPD20 | 18 | 55.5% | 22.2% | 0.0% | 22.3% |
| BPADS6 | 40 | 87.5% | 5.0% | 5.0% | 2.5% |
| PARRQ22 | 23 | 56.5% | 8.7% | 17.4% | 17.4% |
| EBSP23 | 46 | 69.6% | 8.7% | 15.2% | 6.5% |
| FABS/M24 | 61 | 0.0% | 0.0% | 48.1% | 51.9% |
Because the BPAQ-MI places greater equity across the ecological domains, new and improved interventions can be developed to enhance physical activity. Previously, the majority of interventions have been developed to address barriers in one domain of the ecological framework at a time. Rimmer and colleagues did one such intervention with African American women with disabilities and saw an increase in exercise by only 26 minutes per week.73 While this intervention successfully increased physical activity for a subgroup of people with disabilities, most of the increase was associated with indoor household activity and leisure activity in indoor or outdoor recreational settings (a more enjoyable form of physical activity) did not change. Understanding barriers across multiple domains may help with developing targeted intervention approaches and ultimately enhance the effects of an intervention by increasing the quality and quantity of physical activity in multiple venues and settings in the community (vs. the home only).
Study Limitations
The limitations of this study included: (1) potential lack of generalizability of BPAQ-MI and (2) measuring self-reported physical activity.
The BPAQ-MI might not be generalizable to individuals with other impairments or demographic backgrounds. For example, items such as “lack of time” or the necessity of caregivers did not load onto any domain. These items could have been captured by other items or are specific to people with a different impairments (e.g. sensory or intellectual/developmental).37, 72 Some items might apply primarily to urban communities, such as excessive crime or cars. Rural communities might find that other barriers are more pertinent to their communities, for example lack of adequate lighting might be big barriers in a rural community but is not a barrier in an urban community like Chicago. Future studies should examine the factor structure of the BPAQ-MI for other populations (e.g. translate the BPAQ-MI for people who speak other languages, locations, or other types of impairment) to help minimize sample bias and improve the generalizability of the BPAQ-MI.
The other limitation was the use of self-report physical activity measures, such as the PADS. Self-report physical activity might have contributed to inflated levels of physical activity. The physical activity levels in this study were not consistent with previous studies that found people with disabilities were more likely to be inactive.2 The use of objective measures of physical activity like accelerometers has been utilized for specific impairments like people with Parkinson disorder, osteoarthritis, or Multiple Sclerosis74. The use of objective physical activity measures do not provide information regarding type of physical activity, such as exercise. The PADS was selected because it was validated on a population that most closely resembles people with mobility impairments.
In order to address these limitations, future studies should: (1) examine the psychometric properties of the BPAQ-MI among people without disabilities or with other disabilities and (2) assess the predictive and sensitivity of the BPAQ-MI by using objective physical activity measures. By assessing the psychometric properties of the BPAQ-MI among different groups, researchers will be able to better generalize the construct of barriers and whether separate barrier questionnaires are required for people with different impairments or if one questionnaire is sufficient. Further validation of the BPAQ-MI should measure the predictive and concurrent validity of the BPAQ-MI by via intervention studies address barriers within and across ecological domains.
Conclusions
The BPAQ-MI is the first comprehensive instrument that measures barriers across intrapersonal, interpersonal, organizational, and community domains. Future physical activity interventions could benefit from using the BPAQ-MI to capture barrier changes before, during and after an intervention and to monitor potential changes in barrier type and quantity with relation to higher or lower levels of physical activity participation.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to report. The study sponsor had no role in the study design, data collection, analysis, interpretation or writing of this report.
Suppliers
IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.
Financial Disclosure: The project described was supported by Grant Number P30AG022849 from the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. [Accessed February 21, 2014];The Benefits of Physical Activity. 2011 http://www.cdc.gov/physicalactivity/everyone/health/
- 2.Carroll DD, Courtney-Long EA, Stevens AC, et al. Vital Signs: Disability and Physical Activity — United States, 2009–2012. Morbidity and Mortality Weekly Report. 2014;63(18):407–413. [PMC free article] [PubMed] [Google Scholar]
- 3.Altman B, Bernstein A. Disability and health in the United States, 2001–2005. Hyattsville: National Center for Health Statistics; 2008. [Google Scholar]
- 4.McLeroy K, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Edu Behav. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 5.Sallis J, Owen N. Ecological Models of Health Behvaior. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: John WIley & Sons, Inc; 2002. pp. 462–484. [Google Scholar]
- 6.Rimmer J, Rubin S, Braddock D. Barriers to exercise in African American women with physical disabilities. Arch Phys Med Rehab. 2000;81:182–188. doi: 10.1016/s0003-9993(00)90138-2. [DOI] [PubMed] [Google Scholar]
- 7.Rimmer J, Wang E, Smith D. Barriers associated with exercise and community access for individuals with stroke. J Rehabil Res Dev. 2008;45:315–322. doi: 10.1682/jrrd.2007.02.0042. [DOI] [PubMed] [Google Scholar]
- 8.Kayes N, McPherson K, Schluter P, Taylor D, Leete M, Kolt G. Exploring the facilitators and barriers to engagement in physical activity for people with multiple sclerosis. Disabil Rehabil. 2011;33:1043–1053. doi: 10.3109/09638288.2010.520801. [DOI] [PubMed] [Google Scholar]
- 9.Kayes N, McPherson K, Taylor D, Schlüter P, Kolt G. Facilitators and barriers to engagement in physical activity for people with multiple sclerosis: a qualitative investigation. Disabil Rehabil. 2011;33:625–642. doi: 10.3109/09638288.2010.505992. [DOI] [PubMed] [Google Scholar]
- 10.Stephens C, Neil R, Smith P. The perceived benefits and barriers of sport in spinal cord injured individuals: a qualitative study. Disability and Rehabilitation. 2012;34(24):2061–2070. doi: 10.3109/09638288.2012.669020. [DOI] [PubMed] [Google Scholar]
- 11.Rimmer J, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: Barriers and facilitators. Am J Prev Med. 2004;26:419–425. doi: 10.1016/j.amepre.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Rimmer J, Riley B, Wang E, Rauworth A. Development and validation of AIMFREE: Accessibility instruments measuring fitness and recreation environments. Disabil Rehabil. 2004;26:1087–1095. doi: 10.1080/09638280410001711432. [DOI] [PubMed] [Google Scholar]
- 13.Arbour-Nicitopoulos KP, Ginis KAM. Universal Accessibility of “Accessible” Fitness and Recreational Facilities for Persons With Mobility Disabilities. Adapted Physical Activity Quarterly. 2011;28(1):1–15. doi: 10.1123/apaq.28.1.1. [DOI] [PubMed] [Google Scholar]
- 14.Rolfe D, Yoshida K, Renwick R, Bailey C. Negotiating participation: How women living with disabilities address barriers to exercise. Health Care Women Int. 2009;30:743–766. doi: 10.1080/07399330802484621. [DOI] [PubMed] [Google Scholar]
- 15.Humpel N, Owen N, Leslie E. Environmental factors associated with adults’ participation in physical activity: A review. Am J Prev Med. 2002;22:188–199. doi: 10.1016/s0749-3797(01)00426-3. [DOI] [PubMed] [Google Scholar]
- 16.Rosenberg DE, Huang DL, Simonovich SD, Belza B. Outdoor Built Environment Barriers and Facilitators to Activity among Midlife and Older Adults with Mobility Disabilities. The Gerontologist. 2013;53(2):268–279. doi: 10.1093/geront/gns119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirchner CE, Gerber EG, Smith BC. Designed to Deter: Community Barriers to Physical Activity for People with Visual or Motor Impairments. American Journal of Preventive Medicine. 2008;34(4):349–352. doi: 10.1016/j.amepre.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 18.Sechrist K, Walker S, Pender N. Development and psychometric evaluation of the exercise benefits/barriers scale. Res Nurs Health. 1987;10:357–365. doi: 10.1002/nur.4770100603. [DOI] [PubMed] [Google Scholar]
- 19.Sallis J, Grossman R, Pinski R, Patterson T, Nader P. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 20.Becker H, Stuifbergen A, Sands D. Development of a scale to measure barriers to health promotion activities among persons with disabilities. Am J Health Behav. 1991;5:449–454. doi: 10.4278/0890-1171-5.6.449. [DOI] [PubMed] [Google Scholar]
- 21.Rimmer J, Rubin S, Braddock D. Barriers to exercise in African American women with physical disabilities. Archives of Physical Medicine and Rehabilitation. 2000;81(2):182–188. doi: 10.1016/s0003-9993(00)90138-2. [DOI] [PubMed] [Google Scholar]
- 22.Zhu W, Timm G, Ainsworth B. Rasch calibration and optimal categorization of an instrument measuring women’s exercise. Res Q Exerc Sport. 2001;72:104–116. doi: 10.1080/02701367.2001.10608940. [DOI] [PubMed] [Google Scholar]
- 23.Kang M, Zhu W, Ragan BG, Frogley M. Exercise barrier severity and perseverance of active youth with physical disabilities. Rehabilitation Psychology. 2007;52(2):170–176. [Google Scholar]
- 24.Gray D, Hollingsworth H, Stark S, Morgan K. A subjective measure of environmental facilitators and barriers to participation for people with mobility limitations. Disabil Rehabil. 2008;30:434–457. doi: 10.1080/09638280701625377. [DOI] [PubMed] [Google Scholar]
- 25.Addy C, Wilson D, Kirtland K, Ainsworth B, Sharpe P, Kimsey D. Associations of perceived social and physical environmental supports with physical activity and walking behavior. Am J Public Health. 2004;94:440–443. doi: 10.2105/ajph.94.3.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ainsworth B, Wilcox S, Thompson W, Richter D, Henderson K. Personal, Social, and Physical Environment Correlates of Physical Activity in African-American Women in South Carolina. Am J Prev Med. 2003;25:23–29. doi: 10.1016/s0749-3797(03)00161-2. [DOI] [PubMed] [Google Scholar]
- 27.Bodde A, Seo D. A review of social and environmental barriers to physical activity for adults with intellectual disabilities. Disabil Health J. 2009;2:57–66. doi: 10.1016/j.dhjo.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 28.Booth M, Bauman A, Owen N. Perceived Barriers to Physical Activity Among Older Australians. J Aging Phys Act. 2002;10:271–280. [Google Scholar]
- 29.Bragg M, Tucker C, Kaye L, Desmond F. Motivators of and barriers to engaging in physical activity: Perspectives of low-income culturally diverse adolescents and adults. Am J Health Educ. 2009;40:146–154. doi: 10.1080/19325037.2009.10599089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brownson R, Baker E, Housemann R, Brennan L, Bacak S. Environmental and policy determinants of physical activity in the United States. Am J Public Health. 2001;91:1995–2003. doi: 10.2105/ajph.91.12.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Conn V. Older women’s beliefs about physical activity. Public Health Nursing. 1998;15(5):370–378. doi: 10.1111/j.1525-1446.1998.tb00362.x. [DOI] [PubMed] [Google Scholar]
- 32.Courneya KS, Friedenreich CM, Quinney HA, et al. A longitudinal study of exercise barriers in colorectal cancer survivors participating in a randomized control trial. Annals of Behavioral Medicine. 2005;29(2):147–153. doi: 10.1207/s15324796abm2902_9. [DOI] [PubMed] [Google Scholar]
- 33.Eyler A, Brownson R, Donatelle R, King A, Brown D, Sallis J. Physical activity social support and middle- and older-aged minority women: Results from a U.S. survey. Soc Sci Med. 1999;49:781–789. doi: 10.1016/s0277-9536(99)00137-9. [DOI] [PubMed] [Google Scholar]
- 34.Ford E, Merritt R, Heath G, et al. Physical activity behaviors in lower and higher socioeconomic status populations. Am J Epidemiol. 1991;133:1246–1256. doi: 10.1093/oxfordjournals.aje.a115836. [DOI] [PubMed] [Google Scholar]
- 35.Glasgow R, Eakin E, Fisher E, Bacak S, Brownson R. Physician advice and support for physical activity: Results from a national survey. Am J Prev Med. 2001;21:189–196. doi: 10.1016/s0749-3797(01)00350-6. [DOI] [PubMed] [Google Scholar]
- 36.Gray DB, Hollingsworth HH, Stark S, Morgan KA. A subjective measure of environmental facilitators and barriers to participation for people with mobility limitations. Disability and Rehabilitation. 2008;30(6):434–457. doi: 10.1080/09638280701625377. [DOI] [PubMed] [Google Scholar]
- 37.Grubbs L, Carter J. The Relationship of Perceived Benefits and Barriers to Reported Exercise Behaviors in College Undergraduates. Fam Community Health. 2002;25:76–84. doi: 10.1097/00003727-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Heller T, Ying G, Rimmer J, Marks B. Determinants of exercise in adults with cerebral palsy. Public Health Nurs. 2002;19:223–231. doi: 10.1046/j.0737-1209.2002.19311.x. [DOI] [PubMed] [Google Scholar]
- 39.Jones M, Nies MA. The relationship of perceived benefits of and barriers to reported exercise in older African American women. Public Health Nursing. 1996;13(2):151–158. doi: 10.1111/j.1525-1446.1996.tb00233.x. [DOI] [PubMed] [Google Scholar]
- 40.Kayes NM, McPherson KM, Schluter P, Taylor D, Leete M, Kolt GS. Exploring the facilitators and barriers to engagement in physical activity for people with multiple sclerosis. Disability and Rehabilitation. 2011;33(12):1043–1053. doi: 10.3109/09638288.2010.520801. [DOI] [PubMed] [Google Scholar]
- 41.Kayes NM, McPherson KM, Taylor D, Schlüter PJ, Kolt GS. Facilitators and barriers to engagement in physical activity for people with multiple sclerosis: A qualitative investigation. Disability and Rehabilitation. 2011;33(8):625–642. doi: 10.3109/09638288.2010.505992. [DOI] [PubMed] [Google Scholar]
- 42.Kerstin W, Gabriele B, Richard L. What promotes physical activity after spinal cord injury? An interview study from a patient perspective. Disability and Rehabilitation. 2006;28(8):481–488. doi: 10.1080/09638280500211932. [DOI] [PubMed] [Google Scholar]
- 43.Kinne S, Patrick DL, Maher EJ. Correlates of exercise maintenance among people with mobility impairments. Disability and Rehabilitation. 1999;21(1):15–22. doi: 10.1080/096382899298052. [DOI] [PubMed] [Google Scholar]
- 44.Kirchoff AC, Elliott L, Schlichting JA, Chin MH. Strategies for physical activity maintenance in African American women. American Journal of Health Behavior. 2008;32(5):517–524. doi: 10.5555/ajhb.2008.32.5.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leslie E, Owen N, Salmon J, Bauman A, Sallis JF, Lo SK. Insufficiently Active Australian College Students: Perceived Personal, Social, and Environmental Influences. Preventive Medicine. 1999;28(1):20–27. doi: 10.1006/pmed.1998.0375. [DOI] [PubMed] [Google Scholar]
- 46.Lim K, Taylor L. Factors associated with physical activity among older people: A population-based study. Prev Med. 2005;40:33–40. doi: 10.1016/j.ypmed.2004.04.046. [DOI] [PubMed] [Google Scholar]
- 47.Messent R, Cooke CB, Jonathon Long P. Primary and secondary barriers to physically active healthy lifestyles for adults with learning disabilities. Disability and Rehabilitation. 1999;21(9):409–419. doi: 10.1080/096382899297396. [DOI] [PubMed] [Google Scholar]
- 48.Meyers A, Anderson J, Miller D, Shipp K, Hoenig H. Barriers, facilitators, and access for wheelchair users: Substantive and methodologic lessons from a pilot study of environmental effects. Soc Sci Med. 2002;55:1435–1446. doi: 10.1016/s0277-9536(01)00269-6. [DOI] [PubMed] [Google Scholar]
- 49.Miller WC, Miller TA. Attitudes of overweight and normal weight adults regarding exercise at a health club. Journal of Nutrition Education and Behavior. 2010;42(1):2–9. doi: 10.1016/j.jneb.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 50.Myers RS, Roth DL. Perceived benefits of and barriers to exercise and stage of exercise adoption in young adults. Health Psychology. 1997;16(3):277–283. doi: 10.1037//0278-6133.16.3.277. [DOI] [PubMed] [Google Scholar]
- 51.Neuberger G, Kasal S, Smith K, Hassanein R, DeViney S. Determinants of exercise and aerobic fitness in outpatients with arthritis. Nurs Res. 1994;43:11–17. [PubMed] [Google Scholar]
- 52.Nies M, Vollman M, Cook T. African American Women’s Experiences with Physical Activity in their Daily Lives. Public Health Nurs. 1999;16:23–36. doi: 10.1046/j.1525-1446.1999.00023.x. [DOI] [PubMed] [Google Scholar]
- 53.Phillips M, Flemming N, Tsintzas K. An exploratory study of physical activity and perceived barriers to exercise in ambulant people with neuromuscular disease compared with unaffected controls. Clin Rehabil. 2009;23:746–755. doi: 10.1177/0269215509334838. [DOI] [PubMed] [Google Scholar]
- 54.Plotnikoff R, Brez S, Hotz S. Exercise behavior in a community sample with diabetes: Understanding the determinants of exercise behavioral change. Diabetes Educ. 2000;26:450–459. doi: 10.1177/014572170002600312. [DOI] [PubMed] [Google Scholar]
- 55.Rhodes R, Martin A, Taunton J, Rhodes E, Donnelly M, Elliot J. Factors Associated with Exercise Adherence Among Older Adults: An Individual Perspective. Sports Med. 1999;28:397–411. doi: 10.2165/00007256-199928060-00003. [DOI] [PubMed] [Google Scholar]
- 56.Scelza W, Kalpakjian C, Zemper E, Tate D. Perceived Barriers to Exercise in People with Spinal Cord Injury. Am J Phys Med Rehabil. 2005;84:576–583. doi: 10.1097/01.phm.0000171172.96290.67. [DOI] [PubMed] [Google Scholar]
- 57.Shaughnessy M, Resnick B, Macko R. Testing a model of post-stroke exercise behavior. Rehabil Nurs. 2006;31:15–21. doi: 10.1002/j.2048-7940.2006.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 58.Sherwood N, Jeffery R. The behavioral determinants of exercise: Implications for physical activity interventions. Annu Rev Nutr. 2000;20:21–44. doi: 10.1146/annurev.nutr.20.1.21. [DOI] [PubMed] [Google Scholar]
- 59.Ståhl T, Rütten A, Nutbeam D, et al. The importance of the social environment for physically active lifestyle -- results from an international study. Soc Sci Med. 2001;52:1–10. doi: 10.1016/s0277-9536(00)00116-7. [DOI] [PubMed] [Google Scholar]
- 60.Temple V, Walkley J. Perspectives of constraining and enabling factors for health promoting physical activity by adults with intellectual disability. J Intellect Dev Disabil. 2007;32:28–38. doi: 10.1080/13668250701194034. [DOI] [PubMed] [Google Scholar]
- 61.Trost S, Owen N, Bauman A, Sallis J, Brown W. Correlates of adults’ participation in physical activity: Review and update. Med Sci Sports Exerc. 2002;34:1996–2001. doi: 10.1097/00005768-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 62.Wilcox S, Der Ananian C, Abbott J, et al. Perceived exercise barriers, enablers, and benefits among exercising and nonexercising adults with arthritis: Results from a qualitative study. Arthritis Rheum. 2006;55:616–627. doi: 10.1002/art.22098. [DOI] [PubMed] [Google Scholar]
- 63.Helmer O. Analysis of the Future: The Delphi Method. Santa Monica, CA: Rand Corporation; 1967. [Google Scholar]
- 64.Hsu C-C, Sandford BA. The Delphi Technique: Making Sense of Consensus. Practical Assessment Research & Evaluation. 2007;12(10) [Google Scholar]
- 65.Sackman H. Delphi Assessment: Expert Opinion, Forecasting and Group Process. Santa Monica, CA: Rand Corporation; 1974. [Google Scholar]
- 66.Yousuf MI. Using Experts’ Opinions through Delphi Technique. Practical Assessment Research & Evaluation. 2007;12(4) [Google Scholar]
- 67.Haeger H, Lambert AD, Kinzie J, Gieser J. Using Cognitive Interviews to Improve Survey Instruments. Association for Institutional Research; New Orleans: 2012. [Google Scholar]
- 68.Willis G. Cognitive Interviews: A “How to” Guide. American Statistical Association; 1999. [Google Scholar]
- 69.Rimmer J, Riley B, Rubin S. A new measure for assessing the physical activity behaviors of persons with disabilities and chronic health conditions: The physical activity and disability survey. Am J Health Promot. 2001;16:34–45. doi: 10.4278/0890-1171-16.1.34. [DOI] [PubMed] [Google Scholar]
- 70.Pett M, Lackey N, Sullivan J. Making sense of factor analysis: The use of factor analysis fo instrument development in heath care research. Thousand Oaks, CA: Sage Publications Inc; 2003. [Google Scholar]
- 71.Crocker L, Algina J. Introduction to classical and modern test theory. Mason, OH: Cengage Learning; 2008. [Google Scholar]
- 72.Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 73.Rimmer J, Hsieh K, Graham B, Gerber B, Gray-Stanley J. Barrier Removal in Increasing Physical Activity Levels in Obese African American Women with Disabilities. J Womens Health. 2010;19:1869–1876. doi: 10.1089/jwh.2010.1941. [DOI] [PubMed] [Google Scholar]
- 74.Strath S. Accelerometer use with children, older adults, and adults with functional limitations. Medicine and Science in Sports and Exercise. 2012;44(1S):S77–S85. doi: 10.1249/MSS.0b013e3182399eb1. [DOI] [PMC free article] [PubMed] [Google Scholar]


