Abstract
Background
Malignant melanoma involving the gastrointestinal (GI) tract may be primary or metastatic. Small bowel is the commonest site of GI metastases from cutaneous malignant melanoma, metastatic lesion in the gallbladder is extremely rare.
Case presentation
This case report describes the presentation of metastatic melanoma in duodenum and gallbladder. A 45-year-old man has presented melena with intermittent abdominal pain. On physical examination we found a small lesion between the fourth and fifth toes, associated with inguinal lymph node. An Abdominal ultrasound revealed diffuse duodenal thickening. Upper endoscopy was performed and discovered an ulcerative lesion in the second part of the duodenum. The biopsy with immunohistochemical stains was in favor of a duodenal location of melanoma. Computed tomography (CT) revealed many circumferential thickening of ileal loops associated with a nodular lesion in the anterior wall of the gallbladder. The patient was treated by palliative chemotherapy.
Discussion
Malignant melanoma of the GI tract may be primary or secondary. The small bowel is the most affected, but it’s rare in the gallbladder. The clinical presentation can mimic the other intestinal tumors, and the diagnosis is based on imaging; CT scan and GI endoscopy have a key role on the diagnosis, and the treatment depends on the location and the number of lesions.
Conclusions
Metastases of melanoma in the GI tract are uncommon, the diagnosis must be suspected in any patient with a history of melanoma with digestive signs.
Keywords: Melanoma, metastases, duodenum, gallbladder
Introduction
Gastrointestinal (GI) malignant melanoma is an unusual clinical entity. Patients often present the similar clinical symptoms like other common tumors in this site, and there are no specific radiological features. It may be primary or metastatic (1,2).
Cutaneous melanoma, whose incidence is increasing, is the most common cause of metastasis in the GI tract (3-8). Metastasis to the GI tract is often seen in the small intestine, followed by the colon, stomach, and rectum, but it’s rare in the esophagus and in the gallbladder (9-12).
We describe a case of a 45-year-old male with duodenal and gallbladder metastasis of malignant melanoma.
Case presentation
We report a case of a 45-year-old man, without medical history, who presents intermittent abdominal pain associated with melena for the past five months.
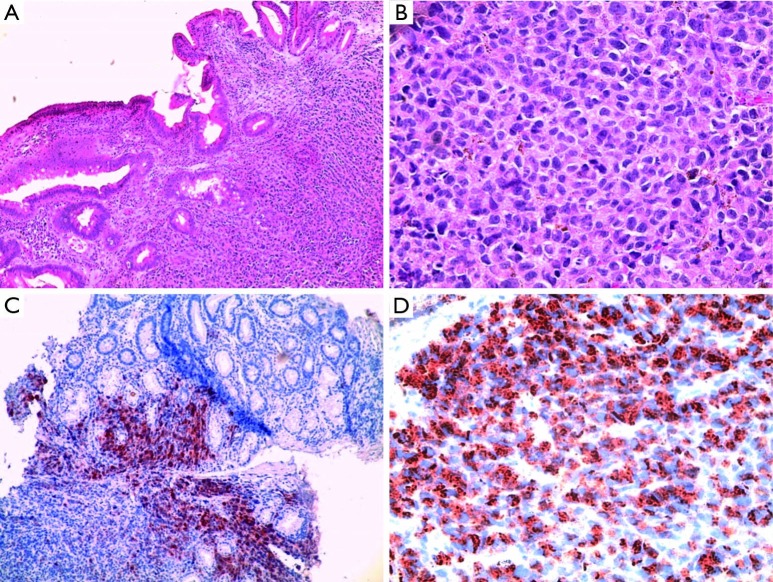
On physical examination we found a small submillimeter lesion between the fourth and fifth toes, associated with ipsilateral inguinal lymph node measuring 40 mm × 35 mm. Biopsy of these lesions confirmed diagnosis of melanoma with many sites of involution (Figure 1).
Figure 1.
Histological examination of primary skin lesion (hemalun-erythrosin-safran, HES). (A) Dermal node of melanoma (×50); (B) epidermal partial regression of melanoma (×100).
An abdominal ultrasound revealed diffuse duodenal thickening, with deep abdominal lymph nodes.
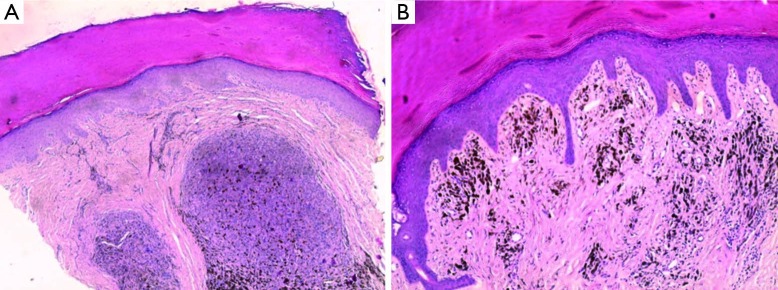
A gastroduodenoscopy was performed and discovered an ulcerative lesion in the second part of the duodenum (Figure 2). Biopsy with immunohistochemical stains was in favor of a duodenal location of melanoma. Indeed, S100 protein, HMB-45 antibodies, and Melan A staining were strongly positive, thus confirming a diagnosis of duodenal melanoma (Figure 3).
Figure 2.

Upper gastrointestinal endoscopy showing an ulcerative and necrotic lesion.
Figure 3.
Histological examination of the duodenal lesion (hematoxylin-eosin) with immunohistochemical stains. (A) Duodenal round cells proliferation (×40); (B) details of cells (×400); (C) the tumor cells were positive for Melan-A in cytoplasm (×100); (D) the tumor cells were positive for HMB45 in cytoplasm (×400).
An abdominal computed tomography (CT) scan has found many circumferential thickening of ileal loops with the presence of peri-intestinal, peri-renal and inguinal lumph nodes, associated with a nodular lesion in the anterior wall of the gallbladder (Figure 4).
Figure 4.
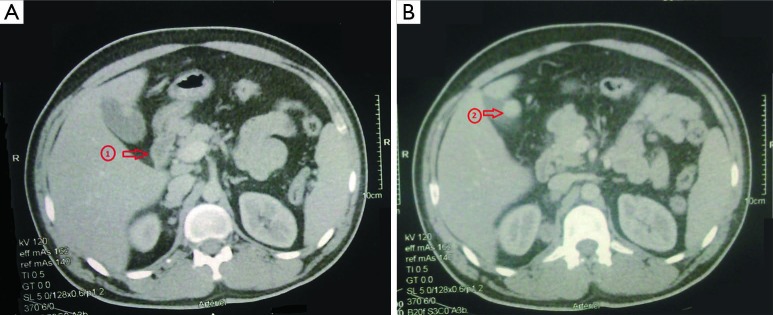
Computed tomography scan of the abdomen reveals a circumferential thickening of the duodenum (red arrow in A) and gallbladder location of melanoma (red arrow in B).
The case was discussed in multidisciplinary concertation meeting, and we decided to treat the patient by palliative chemotherapy. Our patient received a regimen of palliative chemotherapy based on dacarbazine (DTIC). The assessment after three cycles was in favor of stable disease.
Discussion
Melanoma is a malignant tumor which develops from melanocytes, a pigmented, dendritic like cells, present mainly in the skin, eyes, meninges, and GI mucosa, from the mouth to the anal canal (13). Over 90% of melanoma cases are observed on the skin (14). Melanoma is a relatively rare tumor comprising 1-3% of all tumors and exhibits an unusual tendency to metastasize to the GI tract (12,15).
The incidence of melanoma is increasing in Europe and the United States, and the mortality related to unresectable or metastatic melanoma remains high. Globally, 132,000 new cases of melanoma are diagnosed and an estimated 48,000 persons die from advanced melanoma each year (16).
Malignant melanoma of the GI tract may be primary or secondary (14). Metastases are not uncommon, the small bowel is the most affected, followed by the stomach, large bowel, but it’s rare in esophagus and in the gallbladder. It can appear in a few years after treatment of primary melanoma. These lesions are often clinically occult and are diagnosed in 1-9% of cases (7,8). From 1963 to 2000, Wagner et al. reported the review of six cases of primary malignant melanoma of common bile duct (17).
It is difficult to differentiate primary intestinal melanoma from metastatic melanoma, because primary lesion tends to regress and disappear. In addition, melanoma can mimic other neoplasia and may create a major diagnostic challenge when it’s located in intra-abdominal area (18,19).
Almost all GI melanoma are metastatic from cutaneous, ocular, or anal primary melanomas (20). However, melanoma can arise de novo from certain areas of the GI system (21) and may sometimes be hidden by a rectal polyp (22). In total 2-4% of patients with melanoma will be diagnosed with GI metastasis during the course of their disease (20).
The post-mortem examination of patients with melanoma reveals an invasion of the digestive tract in 50% to 60% cases (7,8). However, an ante-mortem diagnosis of metastasis on the digestive tract is only in 1-9% of cases.
The clinical presentation is like other intestinal tumors, they may be accompanied by abdominal pain, upper or lower GI tract bleeding, anemia, weight loss, intestinal obstruction, perforation or intussusceptions. The classic presentation is intestinal intussusceptions which causes obstruction, and may require urgent surgical intervention (14).
A Belgian series, concerning only ten patients, shows that metastases in the GI tract are often unique and always visible on morphological examinations (8).
The diagnosis based on imaging, routine barium examinations, CT scan of the abdomen, ultrasound and PET imaging are used to locate sites of metastasis. The CT scan has 60-70% sensibility in detection of metastasis. In ultrasounds examination, these lesions present as one or more submucosal nodes, with hyperechoic central ulceration (14,23).
The GI endoscopy should be the procedure of choice to diagnose malignant melanoma of GI tract. We can describe three types of malignant melanoma at the endoscopy: the ulcerated melanoma resulting from mucosal fold, sub-mucosal masses with ulceration and tumoral lesions with necrosis and melanosis. However, neoplasia may be completely amelanotic with variable cytological appearance.
Immunohistochemical stains are needed to confirm diagnosis of malignant melanoma; the S100 sensitivity varies between 33-100%, HMB-45 antibodies has sensitivity between 80-97%, but the specificity is high (100%) (24).
Management of GI malignant melanoma depends on the location and number of the lesion. The optimum treatment for malignant melanoma is an extensive and curative surgery, if possible, because other therapeutics methods including adjuvant radiotherapy, chemotherapy and immunotherapy cannot offer definite treatment outcome. The time of diagnosis and the presence of metastases are the most important prognostic factors (25,26).
In case of single lesion, surgical treatment offers an efficient relief of symptoms and, in rare cases, a relatively extended survival (8).
The discovery of BRAF, NRAS, PTEN and KIT alterations in melanoma has allowed the emergence of various rational therapeutic approaches. Indeed, the management of unresectable or metastatic melanoma will be based on anticancer drugs targeting BRAF or c-kit.
Prognosis of malignant melanoma of GI tract is very poor because of difficult to diagnosis. The median overall survival time in patients with metastatic melanoma is 7.5 months, with a 5 years survival of 6%. Patients with malignant melanoma in the GI tract have a duration of survival at 12.5 months with a 5-year survival of 14% (14,27).
Conclusions
Metastases of melanoma in the GI tract are uncommon, and should be suspected in patient with a history of melanoma with symptoms of the digestive system. The presence of these signs should carry out morphological examinations including upper endoscopy with biopsy.
Any treatment decisions should be done in a multidisciplinary meeting, in case of unresectable or metastatic melanoma, only palliative treatment can be considered.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Schuchter LM, Green R, Fraker D. Primary and metastatic diseases in malignant melanoma of the gastrointestinal tract. Curr Opin Oncol 2000;12:181-5. [DOI] [PubMed] [Google Scholar]
- 2.Canhoto M, Barbeiroa S, Arrojaa B, et al. Multiple gastric metastases of malignant melanoma. GE J Port Gastrenterol 2013;20:279-81. [Google Scholar]
- 3.McDermott VG, Low VH, Keogan MT, et al. Malignant melanoma metastatic to the gastrointestinal tract. AJR Am J Roentgenol 1996;166:809-13. [DOI] [PubMed] [Google Scholar]
- 4.Petrelli NJ. Retrospective reviews can be learning experiences. Ann Surg Oncol 1999;6:127-8. [DOI] [PubMed] [Google Scholar]
- 5.Gutman H, Hess KR, Kokotsakis JA, et al. Surgery for abdominal metastases of cutaneous melanoma. World J Surg 2001;25:750-8. [DOI] [PubMed] [Google Scholar]
- 6.Agrawal S, Yao TJ, Coit DG. Surgery for melanoma metastatic to the gastrointestinal tract. Ann Surg Oncol 1999;6:336-44. [DOI] [PubMed] [Google Scholar]
- 7.Berger AC, Buell JF, Venzon D, et al. Management of symptomatic malignant melanoma of the gastrointestinal tract. Ann Surg Oncol 1999;6:155-60. [DOI] [PubMed] [Google Scholar]
- 8.Dequanter D, Sales F, Legendre H, et al. Surgical resection for gastrointestinal metastatic melanoma. Ann Chir 2004;129:278-81. [DOI] [PubMed] [Google Scholar]
- 9.Elsayed AM, Albahra M, Nzeako UC, et al. Malignant melanomas in the small intestine: a study of 103 patients. Am J Gastroenterol 1996;91:1001-6. [PubMed] [Google Scholar]
- 10.Houissa F, Bouzaidi S, Mouelhi L, et al. Diffuse primary malignant melanoma of the upper gastrointestinal tract. Gastroenterol Clin Biol 2010;34:85-7. [DOI] [PubMed] [Google Scholar]
- 11.Korkolis DP, Apostolaki K, Gontikakis E, et al. Primary malignant melanoma of the duodenum: aggressive management and long-term survival of an unusual oncologic entity. South Med J 2008;101:836-9. [DOI] [PubMed] [Google Scholar]
- 12.Li H, Fan Q, Wang Z, et al. Primary malignant melanoma of the duodenum without visible melanin pigment: a mimicker of lymphoma or carcinoma. Diagn Pathol 2012;7:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blecker D, Abraham S, Furth EE, et al. Melanoma in the gastrointestinal tract. Am J Gastroenterol 1999;94:3427-33. [DOI] [PubMed] [Google Scholar]
- 14.Darouichi M. Intussusception on multiple metastases of malignant melanoma. J Radiol 2011;92:437-40. [DOI] [PubMed] [Google Scholar]
- 15.Reintgen DS, Thompson W, Garbutt J, et al. Radiologic, endoscopic, and surgical considerations of melanoma metastatic to the gastrointestinal tract. Surgery 1984;95:635-9. [PubMed] [Google Scholar]
- 16.Robert C, Long GV, Brady B, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 2015;372:320-30. [DOI] [PubMed] [Google Scholar]
- 17.Wagner MS, Shoup M, Pickleman J, et al. Primary malignant melanoma of the common bile duct: a case report and review of the literature. Arch Pathol Lab Med 2000;124:419-22. [DOI] [PubMed] [Google Scholar]
- 18.Gabali AM, Priebe P, Ganesan S. Primary melanoma of small intestine masquerading as gastrointestinal stromal tumor: a case report and literature review. Am Surg 2008;74:318-21. [PubMed] [Google Scholar]
- 19.Katsanos KH, Tsianos VE, Tsianos EV. Metastatic melanoma in stomach and large bowel. Ann Gastroenterol 2010;23:322-4. [Google Scholar]
- 20.Schuchter LM, Green R, Fraker D. Primary and metastatic diseases in malignant melanoma of the gastrointestinal tract. Curr Opin Oncol 2000;12:181-5. [DOI] [PubMed] [Google Scholar]
- 21.Blecker D, Abraham S, Furth EE, et al. Melanoma in the gastrointestinal tract. Am J Gastroenterol 1999;94:3427-33. [DOI] [PubMed] [Google Scholar]
- 22.Lens M, Bataille V, Krivokapic Z. Melanoma of the small intestine. Lancet Oncol 2009;10:516-21. [DOI] [PubMed] [Google Scholar]
- 23.Damian DL, Fulham MJ, Thompson E, et al. Positron emission tomography in the detection and management of metastatic melanoma. Melanoma Res 1996;6:325-9. [DOI] [PubMed] [Google Scholar]
- 24.Clemmensen OJ, Fenger C. Melanocytes in the anal canal epithelium. Histopathology 1991;18:237-41. [DOI] [PubMed] [Google Scholar]
- 25.Atmatzidis KS, Pavlidis TE, Papaziogas BT, et al. Primary malignant melanoma of the small intestine: report of a case. Surg Today 2002;32:831-3. [DOI] [PubMed] [Google Scholar]
- 26.Wade TP, Goodwin MN, Countryman DM, et al. Small bowel melanoma: extended survival with surgical management. Eur J Surg Oncol 1995;21:90-1. [DOI] [PubMed] [Google Scholar]
- 27.Patel JK, Didolkar MS, Pickren JW, et al. Metastatic pattern of malignant melanoma. A study of 216 autopsy cases. Am J Surg 1978;135:807-10. [DOI] [PubMed] [Google Scholar]