Abstract
Objective. To identify sleep patterns and frequency of daytime sleepiness and to assess the association between sleep duration and academic performance among student pharmacists.
Methods. A cross-sectional design was used. An anonymous self-administered paper questionnaire was administered to first-year through third-year students at a pharmacy school.
Results. Questionnaires were completed by 364 student pharmacists (79.4% response rate and 93.8% cooperation rate). More than half of student pharmacists obtained less than 7 hours of sleep at night during a typical school week (54.7%) and a large majority on the night prior to an examination (81.7%). Almost half (47.8%) felt daytime sleepiness almost every day. Longer sleep duration the night prior to an examination was associated with higher course grades and semester grade point averages (GPAs).
Conclusion. A majority of student pharmacists had suboptimal durations of sleep, defined as fewer than 7 hours. Adequate sleep the night prior to an examination was positively associated with student course grades and semester GPAs.
Keywords: sleep, academic performance, students, pharmacy, grade
INTRODUCTION
Adequate sleep optimally impacts mental functioning and therefore impacts students’ performance on examinations and ultimately grades received.1-5 The pattern of sleep one experiences in a 24-hour period directly correlates with physical health, mood, and mental functioning.6,7 Suboptimal sleep is a national problem, with more than a quarter of the US adult population not obtaining the recommended 7 hours of sleep each night.4 Increasing public knowledge of the positive effects of adequate sleep and increasing the proportion of adults who obtain sufficient amounts of sleep to improve health, wellness, productivity, quality of life, and public safety is a national health objective reflected in Healthy People 2020.8
Cognitive performance is susceptible to inadequate sleep durations, defined as fewer than 7 hours a day for adults.1,8 Inadequate sleep decreases general alertness and impairs attention, resulting in slowed cognitive processing. Lack of adequate sleep also interferes with the function of brain structures critical to cognitive processes. The most notably impacted structure is the prefrontal cortex, which executes higher brain functions including language, working memory, logical reasoning, and creativity.1 Yoo et al demonstrated that a single night of shortened sleep duration resulted in decreased memory encoding, which led to less knowledge retention, an effect suggesting the hippocampus was affected.3
Studies assessing the impact of sleep on academic performance focus primarily on teens, adolescents, and undergraduate students. Few studies have explored sleep habits in populations of students who are pursing health care degrees. Those studies that have, found sleep complaints were common in medical students and poor sleep habits were correlated with changes in academic performance.9,10 However, studies that provide knowledge about sleep habits among student pharmacists have yet to be conducted in the United States. Research is needed to provide student pharmacists with tangible evidence they can use to make daily decisions regarding their sleep as it relates to their academic success.
Ours was an exploratory study of sleep patterns and their association with academic performance at one pharmacy school. Specific study objectives were to identify sleep patterns among student pharmacists and the frequency of daytime sleepiness during the school week and to assess the association between sleep duration and academic performance among these students.
METHODS
An anonymous, voluntary, self-administered paper questionnaire was administered to student pharmacists at Auburn University’s Harrison School of Pharmacy. This public institution has a main campus and a satellite campus located about 225 miles from the main campus. The approximate enrollment of student pharmacists was 600 at the time of the study, with 13% of the students attending on the satellite campus. The study sample included all current, professional first-year (P1), second-year (P2), and third-year (P3) student pharmacists on both campuses. Students in their fourth professional year were excluded because the majority of these students were completing their advanced pharmacy practice experiences, which required them to be at clinical practice sites across Alabama during the time the survey was administered.
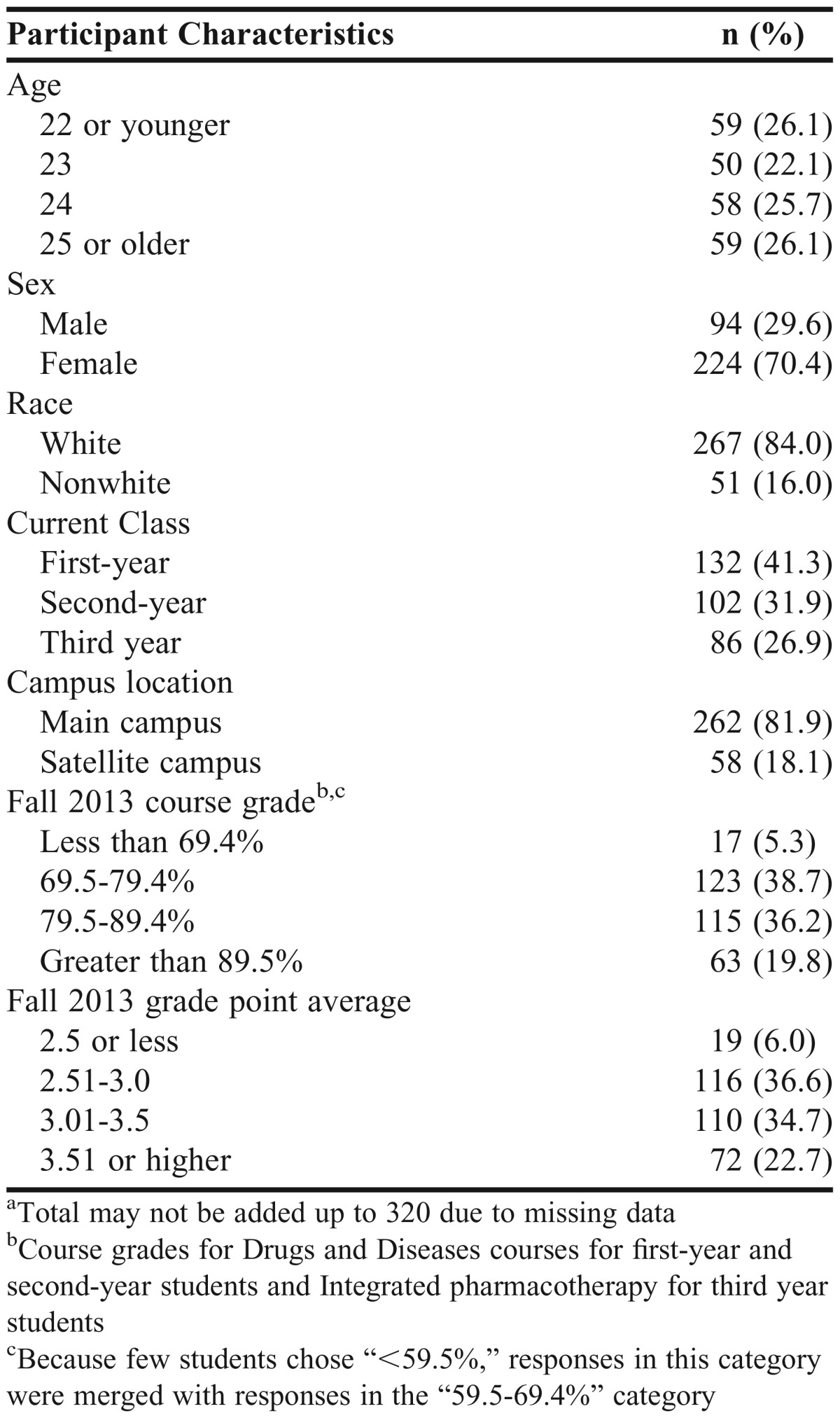
The questionnaire was composed of 3 sections: student characteristics, sleep patterns during a typical school week and the night before an examination, and frequency of daytime sleepiness. Student characteristics pertained to student demographic variables and measures of academic performance. Student demographics included age, sex, race, current professional year (P1, P2, or P3), and campus location. Academic performance was measured by the self-reported grade received during fall semester 2013 for one specific course for each corresponding professional year and by the self-reported GPA for the fall 2013 semester. Both were measured as categorical data with 5 response categories for the course grade measure and 4 response categories for the GPA measure (Table 1). The Drugs and Diseases I and III courses were chosen for P1 and P2 cohorts, respectively. The Integrated Pharmacotherapy course was chosen for the P3 cohort. These courses were chosen because their credit hours and coursework rigor were higher than any other courses taken in the same semester, meaning more students typically had difficulty with these courses compared to other courses. In addition, these courses were chosen as they occured at the roughly the same time of day each semester and would not be influenced by the time of day during which students are most productive Questions in the next 2 sections, related to sleep patterns and daytime sleepiness, were based on the Sleep and Daytime Habits Questionnaire, an instrument that investigates sleep habits and sleep problems in medical students.10 The questionnaire is not a validated instrument, but was adapted from the validated Basic Nordic Sleep Questionnaire.10 In our study, 10 questions were adapted from the Sleep and Daytime Habits Questionnaire. The questions used language specific to the academic coursework and phraseology common to this particular pharmacy school so participants could more easily comprehend them and more accurately respond. Sleep patterns during a typical school week of the fall 2013 and spring 2014 semesters were measured by the following participant-reported factors: (1) time to go to bed; (2) number of hours slept at night; (3) time to wake up; and (4) occurrence of naps. Participants also reported on sleep patterns the night before an examination with slightly different factors: (1) time to go to bed; (2) number of hours slept at night; (3) wake up time earlier than typical nights; and (4) go to bed time later than typical nights. Lastly, frequency of daytime sleepiness was measured by self-reported sleepiness when waking, throughout the day, during study time, and during class time. Data related to sleep patterns and frequency of daytime sleepiness were collected as categorical data, except for the sleep duration which was collected as continuous data. This cross-sectional study received approval by the authors’ institutional review board (IRB).
Table 1.
Characteristics and Academic Achievements of Pharmacy Students Who Participated in a Survey of Sleep Habits (N=320)a
A pilot test of the questionnaire was administered to a group of 16 P1-P3 students. Students’ responses and feedback were used to assess the questionnaire on its question clarity, format, and length. Additionally, students were polled for their thoughts on peer willingness to complete the questionnaire. Feedback collected from the pilot group was assessed and adjustments on question wording and response choices were incorporated into a revision of the questionnaire. The pilot study was conducted to ensure face validity, however no further steps to validate the questionnaire were performed. Students who participated in the pilot test were not excluded from the main study, as participants in the pilot were anonymous, as were those in the main study.
The questionnaire was self-administered in class during a 1-hour weekly professional seminar in February 2014. On the day of survey administration, the seminar topic was related to the importance of sleep on cognitive functions; however, students were not informed of the seminar topic or that a study would be conducted prior the seminar. At the beginning of the seminar, packets were distributed to all students in attendance. Each packet contained the questionnaire, an IRB approval letter, and an opaque envelope. The study’s benefits, potential risks, and participant rights were then explained. Students were allowed 15 minutes to complete the survey, and an attendance count was taken to assess response rate and cooperation rate. The surveys were returned in the opaque envelopes in order to maintain anonymity. All envelopes were collected immediately before the speaker began the seminar session.
Exclusion criteria consisted of students who were repeating coursework for any reason and/or taking at least one prescription medication for a sleep disorder (eg, insomnia or narcolepsy). The rationale for such exclusion was to eliminate confounders that could potentially impact academic success and/or sleep patterns. Data quality control strategies were also implemented to ensure data accuracy. Multiple, related questions, such as duration of sleep and time students went to bed and woke up, allowed researchers to validate data accuracy.
Data was analyzed using SPSS for Mac, v21 (SPSS Inc., Cary, NC) and SAS 9.3 (SAS Institute, Inc., Cary, NC). Using the 2011 Standard Definitions published by the American Association for Public Opinion Research as guidance, the overall response rate (the number of complete surveys divided by the number of complete surveys (eligible cases) plus the number of nonsurveys—those who refused to participate plus those who were not present at the seminar) and cooperation rate (the number of complete surveys divided by the number of complete surveys (eligible cases) plus the number of nonparticipating eligible students who were present in the seminar) were calculated. Descriptive statistics were used to describe participant characteristics, sleep patterns during a typical school week and the night before an examination, and frequency of daytime sleepiness. Chi-square tests were conducted to assess unadjusted associations between student demographics and academic performance (course grades and semester GPA), as well as unadjusted associations between frequency of daytime sleepiness and hours of sleep (6 hours or less vs 7 hours or more). Next, unadjusted associations between sleep duration and academic performance were assessed using analysis of variance (ANOVA). If a significant unadjusted association was found between a demographic variable and academic performance, analysis of covariance was used to assess the adjusted association between sleep duration and academic performance while controlling for the effect of the demographic variable(s) (covariates). An a priori alpha value was set at 0.05.
RESULTS
Of the 447 potential participants among P1-P3 students, 385 attended the professional seminar at both the main and the satellite campuses on the day the survey was conducted. A total of 364 student pharmacists returned completed questionnaires with minimal data missing. Of these, 44 student pharmacists met the above-exclusion criteria and were excluded from response and cooperation rates calculation and subsequent data analyses. The overall response rate and cooperation rate were 79.4% (320/403) and 93.8% (320/341), respectively. No data was collected from students who were absent or refused to participate.
Student demographics and their academic performance can be found in Table 1. The largest percentage of respondents were 22 or younger (26.1%) or 25 and older (26.1%), female (70.4%), white (84.0%), and in their first professional year (41.3%). In terms of academic performance, the largest proportion earned a final course grade of 69.5-79.4% in the specified course for the fall 2013 semester (38.7%) and had a fall 2013 semester GPA between 2.51-3.00 (36.6%). None of the student demographics except for the current professional year variable were associated with the course grades (chi-square (df)=41.7 (6), p<0.0001).
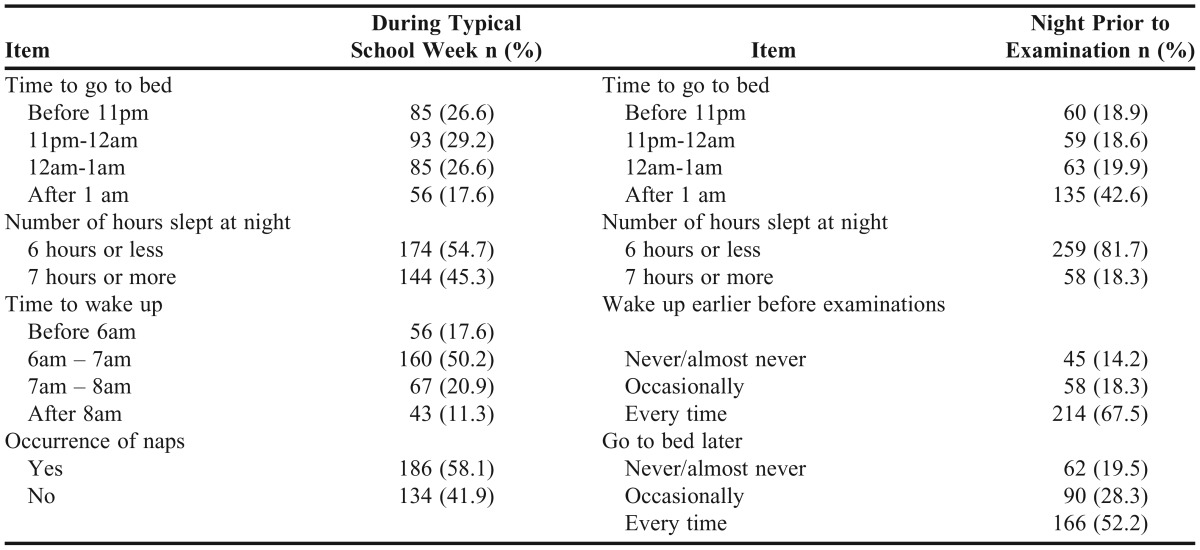
Table 2 identifies sleeping patterns among student pharmacists. Hours of sleep were classified into 2 categories: 6 hours of sleep or less and 7 hours of sleep or more. More than half of respondents reported obtaining 6 hours of sleep or less at night during a typical school week (54.7%) and a majority on the night prior to an examination (81.7%). The average sleep duration was 6.34 (SD=1.16) hours at night during a typical school week and 5.01 (1.63) hours the night prior to examinations (results not shown in table). More than half of the respondents (58.1%) took naps during the day. Also, more than half the respondents reported waking up earlier (67.5%) and going to bed later (52.2%) on nights prior to examinations.
Table 2.
Sleep Patterns During Typical School Week and on Night Prior to an Examination (N=320)
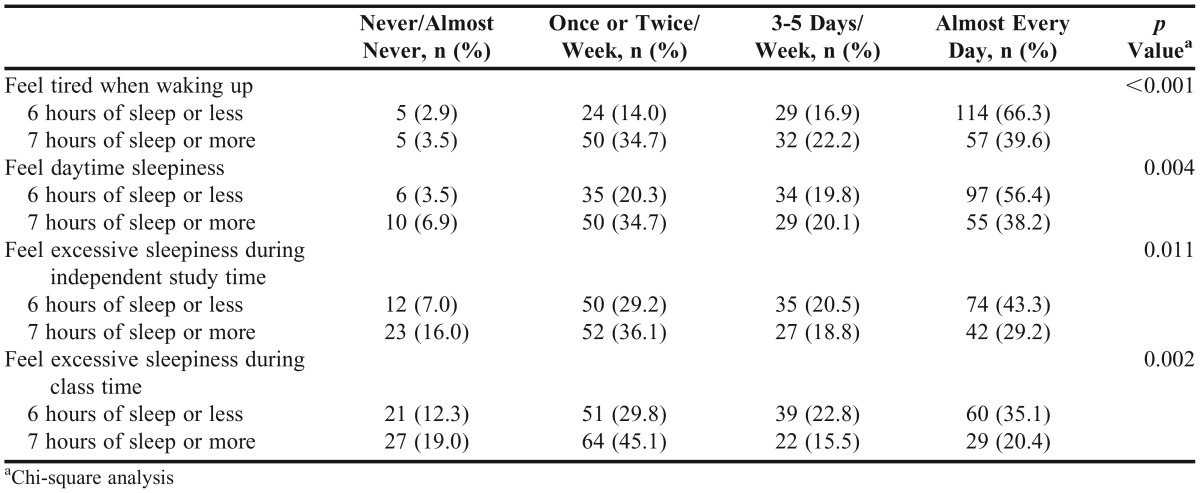
Regarding the frequency of sleepiness during a typical school week (Table 3), more than half of the respondents (54.4%) reported feeling tired when waking up almost every day. Associations between hours slept (6 hours of sleep or less vs 7 hours of sleep or more) and frequency of sleepiness were found: students who slept 6 hours or less tended to report a greater incidence of sleepiness compared to the other group who obtained more sleep.
Table 3.
Comparison of Frequency of Sleepiness During a Typical School Week between Group with 6 Hours of Sleep or Less and Group with 7 hours of Sleep or More (N=320)
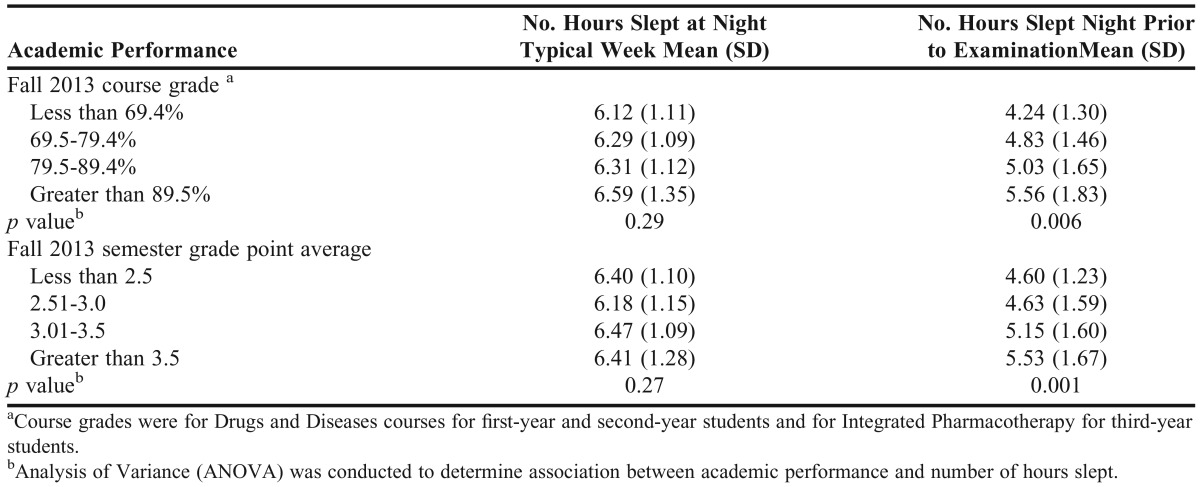
Unadjusted associations between academic performance and duration of sleep are displayed in Table 4. The associations between student academic performance and sleep duration at night during a typical school week were not significant. However, significant associations were found between final course grade and sleep duration the night prior to an examination (F (df)=4.29 (3), p=0.006) and between semester GPA and sleep duration the night prior to an examination (F (df)=5.38 (3), p=0.001). After controlling for current professional year, sleep duration the night prior to an examination was still significantly associated with course grade (p=0.0001). The adjusted coefficient of sleep duration on course grade was 0.11, which meant increasing sleep by one hour was associated with an increase of 11% on course grade.
Table 4.
Associations between Academic Performance and Sleep Duration (N=320)
DISCUSSION
Obtaining more than 7 hours of sleep per day for adults is essential for optimum health and well-being.11 Inadequate sleep is a public health problem, and getting adequate sleep was deemed critical enough to be an objective by Healthy People 2020 to improve national health.8 The majority of student pharmacists in this study slept less than the recommended duration for adequate sleep. Specifically, student pharmacists had an average sleep duration of a little over 6 hours on a typical school night. They had even greater sleep deficits the night prior to an examination, with an average sleep duration of 5 hours. The consequences of sleep inadequacies among the majority of participants included excessive sleepiness almost every day, tiredness upon waking, and excessive sleepiness during study time and class time.
Duration of sleep the night prior to an examination was associated with academic performance as measured by course grades and semester GPA. This finding is consistent with Medeiros et al’s research among medical students that found students who reported sleeping for longer durations obtained higher scores on examinations, as well as Veldi et al’s study that found sleep behaviors to be associated with academic progression.9,10 Moreover, congruent findings of decreased sleep duration associated with poor examination performance were found in Gruber et al’s study on children’s performance on IQ measures and Perez-Lloret et al’s study on adolescents’ performance on mathematics and literature coursework.12-13
The causal relationship between sleep duration (cause) and academic performance (outcome) cannot be established because of the nature of the cross-sectional study. One may argue that students who performed well in class slept longer the night prior to an examination because they were more prepared, hence did not feel they needed additional time to study. Even though this speculation is reasonable, we hypothesized that longer sleep duration would lead to better academic performance based on the scientific foundation related to the effect of sleep on cognitive performance. Sleep has an integral role in learning and memory consolidation. Sleep is necessary to form synapses between dendritic branches that allow for memory formation of learned information, thus enabling students to recall information more rapidly and for more prolonged time periods.14,15 In addition, neurophysiologic and imaging studies show that sleep works to ensure adequate function of the prefrontal cortex, which executes higher brain functions including language, working memory, logical reasoning, and creativity.1,2,15 Belenky et al’s experimental study examining differences in cognitive function following sleep restriction of 3, 7, 5, or 9 hours a night showed decline in speed and accuracy of information proportional to amount of sleep restriction.2 Thus our findings are consistent with established scientific foundation and would suggest the extra hour of sleep provides an advantage for higher academic performance on examinations among student pharmacists.
Sleep deficits among student pharmacists warrant attention from faculty members and school administrators. In addition to daytime fatigue and poor academic performance, previous research showed that sleep deficits led to sleep-related complications including diabetes, cardiovascular disease, and decreased cognitive function and well-being.16-18 Student pharmacists should be educated on the importance of obtaining adequate sleep prior to an examination—especially that even one hour of additional sleep could be beneficial to their course grade and overall GPA than an extra hour of studying. Providing such information to student pharmacists would increase student awareness of the advantages of additional sleep and give them the opportunity to make informed decisions regarding their academic performance and their health. This information could be provided during first-year student pharmacist orientation and could include findings of this study and tips for establishing healthy sleep hygiene, such as refraining from eating large meals near bed time and avoiding reading or watching TV in bed.19 In addition, increased awareness of beneficial sleep behaviors could lead students to establish sleep habits that extend into their professional pharmacy careers.
This study has several limitations. First, there may have been differences in sleep behaviors, subjective sleepiness, and grades received among questionnaire respondents, students who refused to participate, and students absent from the seminar. There was a potential for recall error as we asked participants to recall sleep behaviors and grades received over the period of 6 months. Furthermore, while piloted among a small sample of the study population, the questionnaire was not validated, thus limiting the applicability of its results. In addition, this study was only conducted at a single institution, which makes it difficult to generalize results to student pharmacists at other institutions. Causality between sleep duration and academic performance could not be established because of the cross-sectional design of this study. Another limitation is lack of thorough analysis of daytime naps; so, it is unknown if students with shorter nighttime sleep durations were compensating with daytime naps, which could potentially provide benefits to cognitive function.20 Lastly, several confounders were not accounted for that could have affected academic performance. For example, sleep quality was not captured in this study. Sleep quality, in addition to sleep quantity, is impactful on academic performance.21 Other confounders that could impact cognitive function and academic success include students’ intellectual ability, achievement motivation, personality, emotional health, presence of stressors, learning style, studying skills, time management strategies, diet, exercise, and caffeine use.4,5,22
Future research could enhance generalizability and provide further understanding of the effect of student pharmacists’ sleep duration and patterns. For example, a similar study could be conducted at other schools in different regions or with different enrollment sizes. An experimental study that investigates the effect of sleep on academic performance would be ideal (eg, including the use of polysomnography in order to provide a more objective measure of sleep quality), however such a study could not easily be conducted. An observational study with rigorous methods could also be considered. For example, to remove recall bias, students’ sleep hours could be recorded using diaries, and students’ grades could be obtained with permission from student records.
CONCLUSION
A majority of student pharmacists chronically obtain less than the recommended 7 hours of sleep each night, with particularly insufficient sleep duration on nights prior to examinations. Higher course grades and semester GPAs are associated with longer duration of sleep on nights prior to examinations. Schools of pharmacy should seek to increase awareness among students on the potential impact their sleep habits have on academic performance.
ACKNOWLEDGMENTS
Preliminary results of this study were presented at the Alabama Public Health Association Conference in Birmingham, AL, in April 2014 as well as the Alabama Society of Health-System Pharmacists Summer Meeting in Pensacola, FL in June 2014.
Appendix A.
Survey of Sleep Habits among Pharmacy Students
Part 1. Tell us about yourself by checking (✔) the best response.
-
1. Your current class:
○P1 ○P2 ○P3
2. What is your age at your last birthday?
-
3. Sex:
○Male ○Female
-
4. Race:
○White/Caucasian ○Black/African American ○Asian or Pacific Islander ○Hispanic/Latino ○Indian ○Native American
-
5. At any time during your pharmacy school career, have you repeated any courses? This does not include remediation.
○Yes ○No
-
6. Do you take prescription medication for a sleep disorder such as insomnia or narcolepsy?
○Yes ○No
Part 2. The following questions are about your sleep during weekdays of a typical school week of the Fall 2013-Spring 2014 semesters. Check (✔) the best response.
-
1. When do you go to bed?
○Before 8:00pm ○8:00-9:00pm ○9:00-10:00pm ○10:00-11:00pm
○11:00pm-12:00am ○12:00-1:00am ○1:00-2:00am ○After 2:00am
-
2. What time do you typically wake up and begin activities of your day?
○Before 3:00am ○3:00-4:00am ○4:00-5:00am ○5:00-6:00am
○6:00-7:00am ○7:00-8:00am ○8:00-9:00am ○9:00-10:00am
○10:00-11:00am ○After 11:00am
-
3. How many hours of sleep do you typically obtain at night?
○≤1 ○2 ○3 ○4 ○5 ○6 ○7 ○8 ○9 ○10 ○>10
-
4. How many daytime naps do you take in a typical school week (Monday-Friday)?
○0 ○1 ○2 ○3 ○4 ○5 ○6 ○7 ○ >7
Part 3. The following questions are about your sleep around a DAD examination (current P1, P2) or IP Phase Final Examination (current P3) of the fall 2013 through spring 2014 semesters. Check (✔) the best response.
-
1. Do you go to bed later than usual the night before DAD exams or IP phase final examinations?
○Never or almost never ○Occasionally ○Every time
-
2. Do you wake up earlier than usual the morning before DAD examinations or IP phase final examinations?
○Never or almost never ○Occasionally ○Every time
-
3. When do you typically go to bed before DAD examinations or an IP phase final examinations?
○Before 8:00pm ○8:00-9:00pm ○9:00-10:00pm ○10:00-11:00pm
○11:00pm-12:00am ○12:00-1:00am ○1:00-2:00am ○After 2:00am
-
4. During the night before DAD examinations or IP phase final examinations, how many hours of sleep do you typically obtain?
○≤1 ○2 ○3 ○4 ○5 ○6 ○7 ○8 ○9 ○10 ○>10
Part 4. Please check (✔) the appropriate response.
-
1. How often during the school week (Monday- Friday):
-
a. Do you feel tired when waking up?
○Never/almost never ○Once/twice a week
○3-5 days a week ○Almost every day
-
b. Do you feel daytime sleepiness?
○Never/almost never ○Once/twice a week
○3-5 days a week ○Almost every day
-
c. Do you feel excessive sleepiness during independent study time?
○Never/almost never ○Once/twice a week
○3-5 days a week ○Almost every day
-
d. Do you feel excessive sleepiness during class time?
○Never/almost never ○Once/twice a week
○3-5 days a week ○Almost every day
-
-
2. What was your overall fall 2013 semester GPA?
○<2.5 ○2.51-3.0 ○3.01-3.5 ○>3.5
-
3. What was the final letter grade you received in the fall 2013 DAD I course (P1), DAD III course (P2) or IP Phase II course (P3)?
○<59.5% ○59.5-69.4% ○69.5-79.4% ○79.5-89.4% ○>89.5%
REFERENCES
- 1.Alhola P, Polo-Kantola P. Sleep deprivation: impact on cognitive performance. Neuropsychiatr Dis Treat. 2007;3(5):553–567. [PMC free article] [PubMed] [Google Scholar]
- 2.Belenky G, Wesenten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12(1):1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 3.Yoo SS, Hu PT, Gujar N, Jolesz FA, Walker MP. A deficit in the ability to form new human memories without sleep. Nat Neurosci. 2007;10(3):385–392. doi: 10.1038/nn1851. [DOI] [PubMed] [Google Scholar]
- 4.Hillman CH, Erickson KI, Kramer AF. Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci. 2008;9(1):58–65. doi: 10.1038/nrn2298. [DOI] [PubMed] [Google Scholar]
- 5.McEwen BS. Protective and damaging effects of stress mediators. NEJM. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 6.Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10(5):323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Ferrie JE, Shipley MJ, Akbaraly TN, Marmot MG, Kivimaki M, Singh-Manoux A. Change in sleep duration and cognitive function: findings from the Whitehall II Study. Sleep. 2011;34(5):565–573. doi: 10.1093/sleep/34.5.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Healthy People. 2020, Office of Disease Health and Promotion, U.S. Department of Health and Human Services. Sleep health. http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=38. Accessed April 21, 2014.
- 9.Medeiros ALD, Mendes DBF, Lima PF, Araujo JF. The relationships between sleep-wake cycle and academic performance in medical students. Biol Rhythm Res. 2001;32(2):263–270. [Google Scholar]
- 10.Veldi M, Aluoja A, Vasar V. Sleep quality and more common sleep-related problems in medical students. Sleep Med. 2005;6(3):269–275. doi: 10.1016/j.sleep.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gruber R, Laviolette R, Deluca P, Monson E, Cornish K, Carrier J. Short sleep duration is associated with poor performance on IQ measures in healthy school-age children. Sleep Med. 2010;11(3):289–294. doi: 10.1016/j.sleep.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Perez-Lloret S, Videla AJ, Richaudeau A, et al. A multi-step pathway connecting short sleep duration to daytime somnolence, reduced attention, and poor academic performance: an exploratory cross-sectional study in teenagers. J Clin Sleep Med. 2013;9(5):469–473. doi: 10.5664/jcsm.2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang G, Lai CS, Cichon J, Ma L, Li W, Gan WB. Sleep promotes branch-specific formation of dendritic spines after learning. Science. 2014;344(6188):1173–1178. doi: 10.1126/science.1249098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2005;25(1):117–129. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- 16.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. The Lancet. 1999;354(9188):1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 17.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47(5):833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 18.Kamdar BB, Kaplan KA, Kezirian EJ, Dement WC. The impact of extended sleep on daytime alertness, vigilance, and mood. Sleep Med. 2004;5(5):441–448. doi: 10.1016/j.sleep.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Sleep and sleep disorders: sleep hygiene tips. http://www.cdc.gov/sleep/about_sleep/sleep_hygiene.htm. Accessed September 28, 2014.
- 20.Ficca G, Axelsson J, Mollicone DJ, Muto V, Vitiello MV. Naps, cognition and performance. Sleep Med Rev. 2010;14(4):249–258. doi: 10.1016/j.smrv.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Ahrberg K, Dresler M, Niedermaier S, Steiger A, Genzel L. The interaction between sleep quality and academic performance. J Psychiatr Res. 2012;46(12):1618–1622. doi: 10.1016/j.jpsychires.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 22.Busato VV, Prins FJ, Elshout JJ, Hamaker C. Intellectual ability, learning style, personality, achievement motivation and academic success of psychology students in higher education. Pers Individ Dif. 2000;29(6):1057–1068. [Google Scholar]


