Abstract
Objectives
Cognitive and emotional deficits have been documented in youth with pediatric bipolar disorder (PBD); however, to date, a systematic evaluation of comprehension and memory for verbally presented information has not been conducted. The effect of emotion on comprehension and memory for verbally presented material also has not been examined. We examined whether youth with PBD have difficulty recalling the big picture (macrostructure) as well as the story details (microstructure).
Methods
A total of 35 youth with PBD and 25 healthy controls completed an Affective Story Task. A psychological processing model allowed for the examination of both the macrostructure and microstructure of language comprehension.
Results
Youth with PBD were capable of comprehending the gist of the stories and were not impaired by emotion when comprehending and remembering macrostructure. However, negative emotional material was found to proactively interfere with the encoding and recall of microstructure. Level of depression appeared to impact recall of microstructure, but not macrostructure.
Conclusions
Negatively valenced material may impair subsequent comprehension and memory for details among youth with PBD. This deficit could impact the daily functioning of these youth, as the perception of negative affect may derail aspects of successful comprehension and learning.
Keywords: bipolar disorder, cognition, comprehension, emotion, language
Children with pediatric bipolar disorder (PBD) exhibit deficits in executive function (1, 2) that, despite pharmacotherapy, continue to deteriorate over time (3). Within the broad domain of executive function, verbal memory impairments appear to be the most significant (largest effect size, d = 0.77) when comparing those with bipolar disorder to healthy controls (HC) (4). Additionally, even first-degree relatives of individuals with bipolar disorder show reductions in verbal memory and learning (5) and this deficit has been suggested as a useful cognitive endophenotype for bipolar disorder. However, to date, assessments of verbal memory and learning have relied upon testing that does not allow discrete analysis of the factors within verbal memory that affect function. One way of addressing this void is to examine not only total amount of material recalled (whether in lists of words, sentences, or longer connected discourse), but specifically what information is recalled or under what conditions. In addition, we are not aware of any studies that have examined the effect of emotion on verbal memory despite documentation of an interaction between cognition and emotion in PBD (6). This question is clinically relevant, as many psychosocial interventions such as Cognitive Behavior Therapy can be delivered in a primarily verbal manner. If a child with PBD cannot encode the information verbally delivered in therapy sessions or retrieve this information later, the effectiveness of the intervention will be limited.
Initial evidence of impairments in verbal memory in children with a diagnosis of PBD can be found in two key investigations that use word list and narrative recall. First, McClure and colleagues (2) examined list memorization using the California Verbal Learning Test for Children (CVLT-C) (7) as well as narrative recall (Memory for Stories) from the Test for Memory and Learning (TOMAL) (8). On the CVLT-C, youth are asked to recall a list of 15 orally presented words over five trials, with free recall after each trial. On the Memory for Stories subtest of the TOMAL a child is read three paragraph-length stories. After each story, as well as after a 30-minute delay, the child is asked to recall as much of the narrative as possible. An interference list is presented following the fifth recall trial. Short- and long-delayed free recall are assessed, followed by a delayed recognition test. McClure and colleagues (2) found that children with PBD performed more poorly than controls on short-term free recall, both short- and long-delay cued recall, and delayed narrative recall.
Another investigation (9) also used the CVLT-C to examine verbal declarative memory among children with PBD. As with the work of McClure and colleagues, children with PBD were found to recall and recognize significantly fewer words than HC. These findings added to evidence suggesting that children with PBD demonstrate poor encoding abilities, reduced memory capacities, or both (9). Together, these studies suggest a global impairment that may be better understood through a closer examination of the components. In other words, a fine-grained exploration of verbally presented information and recall may further illuminate the nature of the executive functioning deficits observed among youth with PBD.
We hypothesized that impairments in text comprehension [by this we refer to the underlying text base communicated through verbal speech or written word (10)] and memory among children with PBD is likely to stem from cognitive factors that are affected by emotional factors (11, 12). Among healthy adults, emotionally laden stories have been associated with increased recall relative to neutral stories (13-15). In contrast, adults with bipolar disorder have not shown enhanced recall of emotionally bound information in a procedure requiring patients to watch and subsequently recall stories depicted by slide shows (16). Our neuroimaging work has demonstrated that youth with PBD display reductions in brain activation, specifically in the dorsolateral prefrontal cortex, relative to controls during an executive task performed in the face of negative emotion (6). This suggests that children with PBD may have enhanced perception of negative emotions (6, 17) and poor frustration tolerance (18), which may impact text comprehension and memory.
Fueled by our clinical observations of the difficulty youth with PBD have in grasping verbal discourse, we designed a paradigm to further evaluate these difficulties. Our study was informed by research within cognitive psychology examining text comprehension, memory, and learning (19). Due to our study specific questions and concerns with the appropriateness of using standardized measures (length, emotion, gender of actor in story, etc.), we designed materials that included connected, but lengthy discourse. The use of such materials generally forces a bias away from rote recall (which is common in neuropsychological tests) and instead into comprehension of material.1 In addition, we sought to examine verbal memory in relation to emotion, in a way that would allow for the interaction between social and cognitive function and still allow characterization of the type as well as amount of information recalled suggesting an overall impairment in verbal memory but unclear is whether this deficit is due to problems at encoding or retrieval. We hypothesized that children with PBD would demonstrate a general deficit in recall relative to HC. We also hypothesized that emotional material, either positive or negative, would impair text comprehension and memory among youth with PBD. Additionally, given the structure of the materials created for this study, we can further hypothesize that children with PBD will show differential impairments in micro units (details) consistent with the work of McClure and colleagues (2) but intact recall of macro units (main ideas). Successful comprehension of macro units would help facilitate recall of details by allowing the listener to create as structure on which details can be added. This type of comprehension is assessed via a serial position effect of recall. Unlike in short term memory, one would predict an increase in recall of details later in the story because the story structure has already been established.
Methods
Subjects
All subjects were recruited through the outpatient Pediatric Mood Disorders Program, Institute for Juvenile Research, Chicago, IL, USA. This project was approved by the University of Illinois at Chicago Institutional Review Board. Parents and adolescents over age 15 gave written permission, and adolescents and children under 15 gave assent to participate in this trial. HC were recruited from the community via advertisements. Inclusion criteria for patients were: (i) a DSM-IV (20) diagnosis of bipolar I disorder (BD-I) or bipolar II disorder (BD-II) meeting current criteria for a mixed, manic or hypomanic episode, (i) being between the ages of 8 and 18, and (iii) being medication free or washed out of current ineffective pharmacotherapy regime prior to participation (3). Exclusion criteria for all subjects included: (i) active substance abuse measured through urine drug screen at baseline, (ii) serious medical problems, and (iii) the presence of another current DSM-IV Axis I diagnosis to reduce diagnostic confound. Subject groups were matched on age, gender, and estimated IQ as assessed by the Wechsler Abbreviated Scale of Intelligence (PBD: n = 35, females = 20; HC = 25, females = 14; mean age = 13.3 ± 3.1 years). A total of 103 subjects were screened to include 29 youth with BD-I and 6 subjects with BD-II. Of the 29 BD-I youth, 20 were in a mixed manic episode. A total of 32 potential healthy subjects were screened and 25 met the inclusion criteria for the HC group.
Assessment
All youth with PBD underwent a standard clinical assessment consisting of a diagnostic interview with the patient and family by a board-certified child psychiatrist or a doctoral-level nurse practitioner in child psychiatry. In addition, each child and the parent (or legal guardian) were interviewed by master's level research assistants using the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) (21). Clinical information from all sources was combined and further discussed to agree on the final diagnosis in a weekly consensus conference involving the research team. In addition, 10 diagnostic interviews were coded by all three research assistants and reviewed by MNP to establish inter-rater reliability. By Cohen's Kappa, reliability of diagnoses was 0.96 between the raters. The Young Mania Rating Scale (YMRS) (22) and the Child Depression Rating Scale-Revised (CDRS-R) (23) were also administered (see Table 1).
Table 1. Demographics.
| PBD Mean (SD) | Healthy controls Mean (SD) | t | p-value | |
|---|---|---|---|---|
| Intelligence quotient | 103.8 (16.0) | 110.5 (17.8) | 1.45 | 0.15 |
| WRAT | 104.7 (10.6) | 110.1 (14.3) | 1.57 | 0.12 |
| YMRS | 17.9 (10.2) | 1.8 (2.8) | -7.38 | 0.00 |
| CDRS-R | 48.9 (15.7) | 19.6 (2.6) | -8.33 | 0.00 |
| Frequency | Frequency | χ2 | p-value | |
| Socioeconomic status | Median 2 | Median 2 | 3.65 | 0.30 |
| Sex, female | 20 | 14 | 0.02 | 0.90 |
| Race, white | 71% | 43% | 10.04 | 0.04 |
PBD = pediatric bipolar disorder; WRAT = Wide Range Achievement Test; YMRS = Young Mania Rating Scale; CDRS-R = Child Depression Rating Scale-Revised.
The Affective Story Task
The Kintsch and van Dijk model (10)
This model guided our task construction and assumes that successful comprehension of connected discourse requires at least three key components including: (i) elements of meaning must be organized into a coherent whole, (ii) the full meaning of the text is condensed into the gist; and (iii) a new text is generated based on what was comprehended and remembered from the original text. The analysis of these principles can be applied to the recall of any text. We chose to focus on free recall rather than comprehension questions to allow for an examination of both the structure and content of the information retained. For example, poor recall could result from poor encoding or attention to minor detail (microstructure) or it could result from a lack of comprehension of the main ideas (macrostructure). Therefore, macrostructure of text comprehension is constituted by main idea units, broader themes, or schema of the text. These main ideas ought to be reproduced in serial position to reassemble the story. Further, successful encoding and recall of these main ideas facilitate memory for minor units (24, 25). These minor units, or microstructure of the text, are represented by individual propositions as well as relevant syntax to support the construction of the main idea units (10). If there is a failure to grasp the main ideas, text construction at the level of minor units is negatively affected.
Story construction
Positive, neutral, and negatively valenced stories (26) were created and matched on word length, semantic and syntactic complexity (i.e., details, dialogue, characters, events, text base), and semantic structure (see Supporting Information). The positive, neutral, and negative stories reflected content consistent with manic, euthymic, or depressed states. To ensure that the results were not a function of specific story content, three stories for each condition (positive, negative, neutral) were generated, with male and female versions in each story, for a total of 18 stories. Subjects received one story from each of the three conditions. The task was constructed to present a significantly higher number of propositional units after the introduction of emotional content as opposed to before the introduction to allow for a more stable measurement of recall subsequent to the introduction of emotional content. By propositional units, we refer to unit of text that includes both a predicate and one or more arguments (10). The stories were standardized in the timing and number of propositions. Further, we controlled for number of propositions following the introduction of emotional content to ensure that there were no significant differences between the positive and negative stories. For positive stories, the first introduction of emotion occurred, on average, at proposition 42 with 73 propositions after the introduction of emotion. For negative stories, the first introduction of emotion occurred, on average, at proposition 34 with 76 propositions after the introduction of emotion.
Randomized administration
The stories were read aloud to participants and the order of conditions was counterbalanced. Stories were gender specific; female subjects received the female story version and male subjects received the male story version. Participants were asked to recall each story after it was read, and responses were recorded and later transcribed.
Coding
Free recall was coded according to the criteria outlined by Kintsch and vanDijk (10). Stories were deconstructed into main idea units as well as micro units (relevant propositions). We coded the hierarchical structure of main idea units that appeared in serial position with associated minor ideas or propositions. The idea unit was coded in the range of 0 to 2, where 0 indicates the idea was missed, 1 indicates a portion of the component was grasped, and a 2 indicates that the exact idea was reconstructed. The gold standard for the reassembly of the text structure from the Affective Story Task and corresponding coding rules were constructed (DML) based on the rules established by Kintsch and vanDijk (10). The transcribed recall data was coded for total recall (total number of correct propositions), total proportion of main idea propositions (macrostructure), and total proportion of details (microstructure) (10). As an example, the name ‘Spot’ may appear three times in a paragraph that is heard, but saying it once is adequate to refer to this noun. Similarly, the word ‘Sunday’ may not be critical in the story but ‘morning’ or ‘Sunday morning’ would yield a score of 2 as it is relevant to the story. Inter-rater reliability was initially established at 0.84 to 0.90 on five stories and three subjects across three independent research assistants who were blind to participant diagnoses to establish inter-rater reliability in deconstructing the transcribed text into idea units. Disagreements were subsequently clarified within a consensus meeting with two raters (and with DML when agreement could not be reached) to reach 100% agreement based on predetermined criteria. To examine the impact of emotional valence on text comprehension and recall, the number of propositions administered prior to and after the introduction of emotional content were separated and analyzed independently for each of the emotional stories.
Statistical analyses
Data representing total recall of macro- and micro-level data were submitted to a mixed-design ANOVA with subject group (PBD and HC) as the between-subjects factor and story affect (positive, negative, neutral) as the within-subjects factor. In addition, to better characterize the effects of emotion on story recall, the data were submitted to a three-way ANOVA with recall position (before emotion, after emotion) and story affect (positive, negative) as within-subject factors, and subject group (PBD and HC) as the between-subjects factor. We subsequently reran our analyses controlling for CDRS-R and YMRS mood symptoms.
Results
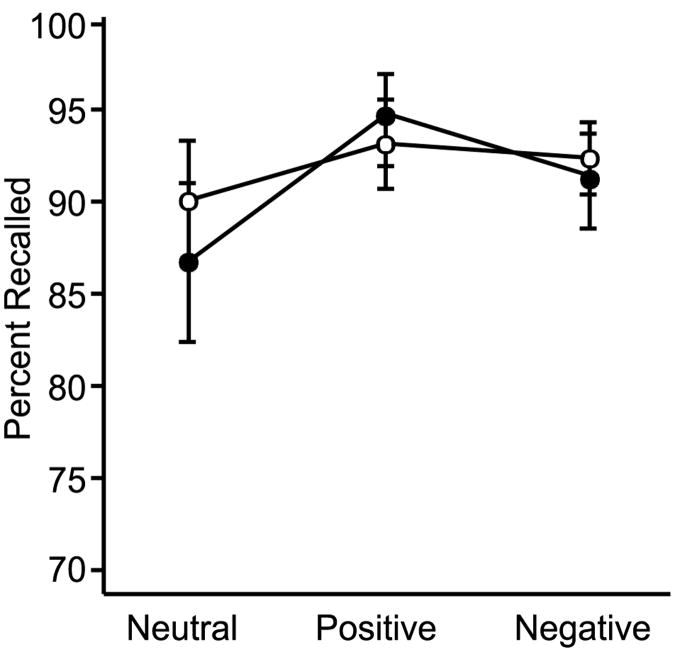
Recall of main ideas
Recall of main ideas is depicted in Figure 1. There was no interaction between emotion and subject group [F(2,116) = 0.36, p = 0.69, η2 = 0.006] nor were there main effects of emotion content [F(2,116) = 1.98, p = 0.14, η2 = 0.033] or subject group [F(1,58) = 0.15, p = 0.70, η2 = 0.003]. Including CDRS and YMRS scores as covariates did not change these findings.
Fig. 1.
Recall of main ideas from emotional stories.
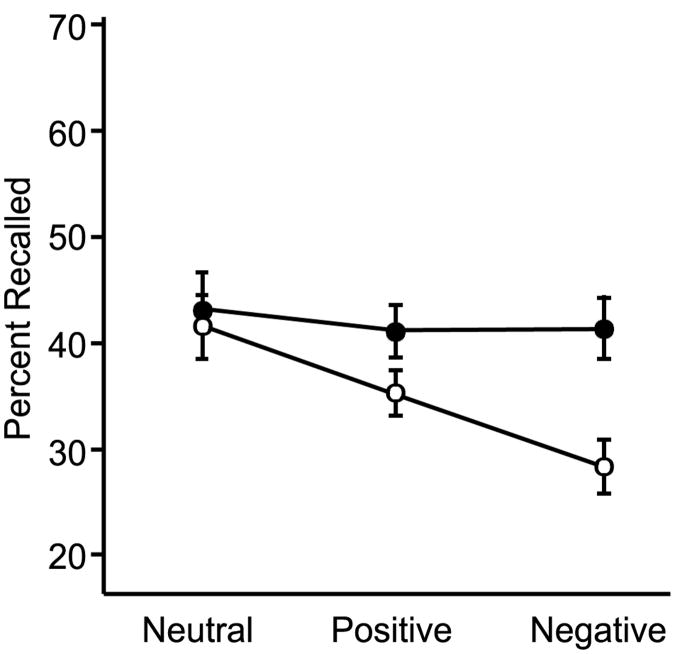
Recall of propositions (micro units)
There was an interaction between story affect and subject group [F(2,116) = 4.45, p = 0.02, η2 = 0.14] as well as a main effect of story affect [F(2,116) = 4.89, p = 0.011, η2 = 0.15]. There was no main effect of subject group [F(1,58) = 3.356, p = 0.072, η2 = 0.055]. As illustrated in Figure 2, there was significantly reduced recall in the PBD group for propositions in the negative stories [F(1,59) = 12.202, p = 0.001]. Including CDRS and YMRS scores as covariates eliminated these significant findings. However, when we controlled for mood symptoms, CDRS scores predicted recall for propositions in the negative stories [F(1,59) = 6.00, p = 0.02], whereas diagnostic group was no longer significant. No group effects on propositional recall were observed for either the neutral [F(1,59) = 0.04, p = 0.85] or positive stories [F(1,59) = 1.19, p = 0.28].
Fig. 2.
Recall of propositions from emotional stories.
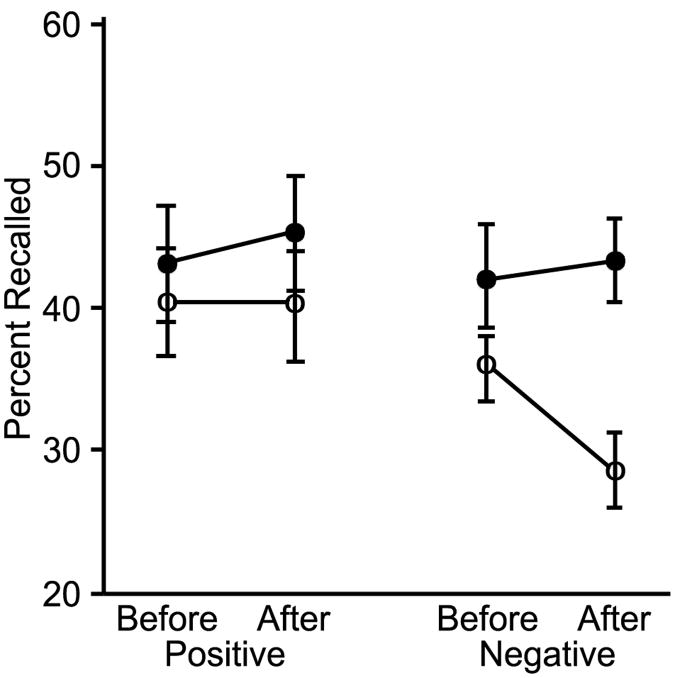
Location of emotion
The interaction between position of emotion by story affect by subject group was not significant [F(1,58) = 0.36, p = 0.55]. Similarly, the interactions between story affect and subject group [F(1,58) = 3.26, p = 0.08] as well as story affect and position relative to emotion [F(1,58) = 0.55, p = 0.46] were not statistically significant. There also was not a significant interaction between subject group and position of emotion [F(1,58) = 1.69, p = 0.20]. These results did not change when CDRS and YMRS scores were included as covariates.
Finally, we examined the effect of position and emotion within each diagnostic group separately. No differences were found among controls for content presented before or after negative (t = -0.36, df = 24, p = 0.75) or positive (t = -0.33, df = 24, p = 0.73) emotion. Within the PBD group there was not a significant difference between content recalled before versus after positive stimuli (t = 0.07, df = 34, p = 0.95). However, youth with PBD remembered less content after negative emotion (t = 2.88, df = 34, p = 0.01) as depicted in Figure 3.
Fig. 3.
Recall of propositions before and after the introduction of emotion.
Discussion
To our knowledge, this is the first study to present detailed data on text comprehension and memory among youth with PBD. It is also the first study to specifically examine the effects of emotion on text comprehension and memory among these youth. Our study yielded three noteworthy findings. First, the text base (main ideas) was found to be intact in PBD, meaning these youth were capable of comprehending the gist of the story. Second, recall of main ideas was not affected by emotional content, meaning youth with PBD were not impaired by emotion when comprehending and remembering the big picture. Third, post-hoc comparisons between patients and HC suggested that the greatest decrease in propositional recall or minor ideas occurred following the initial presentation of emotion in the negative stories. This suggests that negative emotional material acted as proactive interference in the encoding and recall of story details; thus, children with PBD may struggle to remember details in relation to a story after they have been exposed to negative emotion. The finding regarding microstructure appeared to be driven by low mood, as assessed by the CDRS-R. Somewhat surprisingly, positive emotion did not similarly impact encoding and recall.
In understanding these results in the context of the emerging literature, it is important to note the distinctions between list recall and free passage recall. In list learning, primacy and recency effects apply, wherein, information at the beginning and end of a list are remembered best. This type of information processing relies heavily on short-term memory abilities. In contrast, text comprehension and memory violate these primacy and recency rules. We found that the fundamental ability to recall main ideas is preserved among youth with PBD; however, the minor details or propositions used to support the main ideas are significantly impaired in PBD relative to HC in the presence of negative emotions. Clinically, this offers preliminary evidence that negatively valenced, or state congruent, material may impair subsequent comprehension and memory for details. This is directly relevant to the daily lives of children with PBD, in that the perception of affect may derail aspects of successful comprehension and learning.
Deficits in text comprehension and memory may stem from physiological abnormalities that have been documented among youth with PBD and include reports of decreased volume (27-31) and hyperactivity in the amygdala (6, 17, 32, 33). Animal studies have identified a pronounced synchronization between the amygdala and the hippocampus during the retrieval of negative memories (34). Informed by this work, it may be that PBD patients demonstrate a bias towards negative emotions, which may be partly explained by abnormal brain pathophysiology in PBD relative to HC (6, 17, 32, 33).
The current investigation is limited by several factors. First, to address the limited psychometric data on our novel task, we are currently collecting data to assess the reliability and validity. To discriminate the effects of attention-deficit hyperactivity disorder (ADHD) versus PBD, it will be critical to compare youth with ADHD versus youth with PBD versus youth with PBD and ADHD. Assessment of learning disorders would also be informative. This was an inclusive investigation into the effects of bipolar disorder on language comprehension. As the first study in this series, we included both BD-I and BD-II patients. Due to lack of power we cannot examine differences across subtypes in the current investigation, but look forward to doing this in the future. Last, although all children were free of medication at the time of the study, this does not mean previous lifetime exposure to medication could not be contributing to these results. Duration of lifetime medication exposure as well as the specific agent should be evaluated in future studies.
There are several strengths of the current study. It is a first attempt to analyze text comprehension and memory within a PBD sample. We used standardized stories and administered these in a randomized fashion to youth with PBD as well as HC who were demographically and intellectually matched. Language output was transcribed and coded by blind raters with established inter-rater reliability. Memory ability was not confounded with potential medication effects in the PBD group. Future work can examine language construction and recall in euthymic samples as well as replicate the current findings. Extended analyses in estimating time latency between listening, processing and production, prosody, as well as examination of the serial position effects of main and minor idea units will further inform this line of work. Furthermore, correlating these findings with neurocognitive abilities such as attention and working memory as well as with imaging studies may inform future research and the modification of empirically supported interventions.
Supplementary Material
Acknowledgments
MNP receives research support from NIMH and NICHD; and is on a speakers bureau for Janssen, AstraZeneca, and Bristol-Myer Squibbs. DML receives research support from NIA, NIMH, NINDS, CDMRP, TATRC, and the Department of the Army.
Footnotes
These stories are included in the Supporting Information.
The authors of this paper report no relevant commercial associations that might pose a conflict of interest in connection with this manuscript.
References
- 1.Doyle AE, Wilens TE, Kwon A, et al. Neuropsychological functioning in youth with bipolar disorder. Biol Psychiatry. 2005;58:540–548. doi: 10.1016/j.biopsych.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 2.McClure EB, Treland JE, Snow J, et al. Memory and learning in pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2005;44:461–469. doi: 10.1097/01.chi.0000156660.30953.91. [DOI] [PubMed] [Google Scholar]
- 3.Pavuluri MN, West A, Hill SK, Jindal K, Sweeney JA. Neurocognitive function in pediatric bipolar disorder: 3-year follow-up shows cognitive development lagging behind healthy youths. J Am Acad Child Adolesc Psychiatry. 2009;48:299–307. doi: 10.1097/CHI.0b013e318196b907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joseph MF, Frazier TW, Youngstrom EA, Soares JC. A quantitative and qualitative review of neurocognitive performance in pediatric bipolar disorder. J Child Adolesc Psychopharmacol. 2008;18:595–605. doi: 10.1089/cap.2008.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balanzá-Martinez N, Rubio C, Selva-Vera G, et al. Neurocognitive endophenotypes (endophenocognitypes) from studies of relatives of bipolar disorder subjects: a systematic review. Neurosci Biobehav Rev. 2008;8:1426–1438. doi: 10.1016/j.neubiorev.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 6.Pavuluri MN, O'Connor MM, Harral EM, Sweeney JA. An fMRI study of the interface between affective and cognitive neural circuitry in pediatric bipolar disorder. Psychiatry Res. 2008;162:244–255. doi: 10.1016/j.pscychresns.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Delis DC, Kramer JH, Kaplan E, Ober B. California Verbal Learning Test- Children's Version (CVLT-C) Manual. San Antonio: Psychological Corporation; 1994. [Google Scholar]
- 8.Reynolds CR, Bigler ED. Test of Memory and Learning Examiner's Manual. Austin: Pro-Ed; 1994. [Google Scholar]
- 9.Glahn DC, Bearden CE, Caetano S, et al. Declarative memory impairment in pediatric bipolar disorder. Bipolar Disord. 2005;7:546–554. doi: 10.1111/j.1399-5618.2005.00267.x. [DOI] [PubMed] [Google Scholar]
- 10.Kintsch W, van Dijk T. Toward a model of text comprehension and production. Psychol Rev. 1978;85:363–394. [Google Scholar]
- 11.Pavuluri MN, Schenkel LS, Aryal S, et al. Neurocognitive function in unmedicated manic and medicated euthymic pediatric bipolar patients. Am J Psychiatry. 2006;163:286–293. doi: 10.1176/appi.ajp.163.2.286. [DOI] [PubMed] [Google Scholar]
- 12.Schenkel LS, Pavuluri MN, Herbener ES, Harral EM, Sweeney JA. Facial emotion processing in acutely ill and euthymic patients with pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatr. 2007;46:1070–1079. doi: 10.1097/chi.0b013e3180600fd6. [DOI] [PubMed] [Google Scholar]
- 13.Burke A, Heuer F, Reisberg D. Remembering emotional events. Mem Cognit. 1992;20:277–290. doi: 10.3758/bf03199665. [DOI] [PubMed] [Google Scholar]
- 14.Heuer F, Reisberg D. Vivid memories of emotional events: the accuracy of remembered minutiae. Mem Cognit. 1990;18:496–506. doi: 10.3758/bf03198482. [DOI] [PubMed] [Google Scholar]
- 15.Cahill L, McGaugh JL. A novel demonstration of enhanced memory associated with emotional arousal. Conscious Cogn. 1995;4:410–421. doi: 10.1006/ccog.1995.1048. [DOI] [PubMed] [Google Scholar]
- 16.Kauer-Sant'Anna M, Yatham LN, Tramontina J, et al. Emotional memory in bipolar disorder. Br J Psychiatry. 2008;192:458–463. doi: 10.1192/bjp.bp.107.040295. [DOI] [PubMed] [Google Scholar]
- 17.Rich BA, Vinton DT, Roberson-Nay R, et al. Limbic hyperactivation during processing of neutral facial expressions in children with bipolar disorder. Proc Natl Acad Sci USA. 2006;103:8900–8905. doi: 10.1073/pnas.0603246103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rich BA, Schmajuk M, Perez-Edgar KE, Pine DS, Fox NA, Leibenluft E. The impact of reward, punishment, and frustration on attention in pediatric bipolar disorder. Biol Psychiatry. 2005;58:532–539. doi: 10.1016/j.biopsych.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 19.Kintsch W. The representation of knowledge in mind and machines. Int J Psychology. 1998;33:411–420. [Google Scholar]
- 20.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders IV. 4. Washington DC: American Psychiatric Association; 1994. [Google Scholar]
- 21.Geller B, Warner K, Williams M, Zimerman B. Prepubertal and young adolescent bipolarity versus ADHD: assessment and validity using the WASH-U-KSADS, CBCL, and TRF. J Affect Disord. 1998;51:93–100. doi: 10.1016/s0165-0327(98)00176-1. [DOI] [PubMed] [Google Scholar]
- 22.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 23.Posnanski EO, Grossman JA, Buchsbaum Y, Banegas M, Freeman L, Gibbons R. Preliminary studies of the reliability and validity of the children's depression rating scale. J Am Acad Child Adolesc Psychiatry. 1984;23:191–197. doi: 10.1097/00004583-198403000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Gernsbacher MA. Language comprehension as structure building. Hillsdale: Lawrence Erlbaum Associates; 1990. [Google Scholar]
- 25.Little DM, Prentice KJ, Darrow AW, Wingfield A. Listening to spoken text: adult age differences as revealed by self-paced listening. Exp Aging Res. 2005;31:313–330. doi: 10.1080/03610730590948203. [DOI] [PubMed] [Google Scholar]
- 26.Schenkel LS, Marlow-O'Connor M, Moss M, Sweeney JA, Pavuluri MN. Theory of mind and social inference in children and adolescents with bipolar disorder. Psychol Med. 2008;38:791–800. doi: 10.1017/S0033291707002541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DelBello MP, Zimmerman ME, Mills NP, Getz GE, Strakowski SM. Magnetic resonance imaging analysis of amygdala and other subcortical brain regions in adolescents with bipolar disorder. Bipolar Disord. 2004;6:43–52. doi: 10.1046/j.1399-5618.2003.00087.x. [DOI] [PubMed] [Google Scholar]
- 28.Blumberg HP, Kaufman J, Martin A, et al. Amygdala and hippocampal volumes in adolescents and adults with bipolar disorder. Arch Gen Psychiatry. 2003;60:1201–1208. doi: 10.1001/archpsyc.60.12.1201. [DOI] [PubMed] [Google Scholar]
- 29.Dickstein DP, Milham MP, Nugent AC, et al. Frontotemporal alterations in pediatric bipolar disorder: results of a voxel-based morphometry study. Arch Gen Psychiatry. 2005;62:734–741. doi: 10.1001/archpsyc.62.7.734. [DOI] [PubMed] [Google Scholar]
- 30.Chang K, Barnea-Goraly N, Karchemskiy A, et al. Cortical magnetic resonance imaging findings in familial pediatric bipolar disorder. Biol Psychiatry. 2005;58:197–203. doi: 10.1016/j.biopsych.2005.03.039. [DOI] [PubMed] [Google Scholar]
- 31.Chen BK, Sassi R, Axelson D, et al. Cross-sectional study of abnormal amygdala development in adolescents and young adults with bipolar disorder. Biol Psychiatry. 2004;56:399–405. doi: 10.1016/j.biopsych.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 32.Chang K, Adleman NE, Dienes K, Simeonova DI, Menon V, Reiss A. Anomalous prefrontal-subcortical activation in familial pediatric bipolar disorder: a functional magnetic resonance imaging investigation. Arch Gen Psychiatry. 2004;61:781–792. doi: 10.1001/archpsyc.61.8.781. [DOI] [PubMed] [Google Scholar]
- 33.Pavuluri MN, O'Connor MM, Harral E, Sweeney JA. Affective neural circuitry during facial emotion processing in pediatric bipolar disorder. Biol Psychiatry. 2007;62:158–167. doi: 10.1016/j.biopsych.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 34.Seidenbecher T, Laxmi TR, Stork O, Pape HC. Amygdalar and hippocampal theta rhythm synchronization during fear memory retrieval. Science. 2003;301:846–850. doi: 10.1126/science.1085818. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.