Abstract
IMPORTANCE
Dialysis facilities in the United States are required to educate patients with end-stage renal disease about all treatment options, including kidney transplantation. Patients receiving dialysis typically require a referral for kidney transplant evaluation at a transplant center from a dialysis facility to start the transplantation process, but the proportion of patients referred for transplantation is unknown.
OBJECTIVE
To describe variation in dialysis facility–level referral for kidney transplant evaluation and factors associated with referral among patients initiating dialysis in Georgia, the US state with the lowest kidney transplantation rates.
DESIGN, SETTING, AND PARTICIPANTS
Examination of United States Renal Data System data from a cohort of 15 279 incident, adult (18–69 years) patients with end-stage renal disease from 308 Georgia dialysis facilities from January 2005 to September 2011, followed up through September 2012, linked to kidney transplant referral data collected from adult transplant centers in Georgia in the same period.
MAIN OUTCOMES AND MEASURES
Referral for kidney transplant evaluation within 1 year of starting dialysis at any of the 3 Georgia transplant centers was the primary outcome; placement on the deceased donor waiting list was also examined.
RESULTS
The median within-facility percentage of patients referred within 1 year of starting dialysis was 24.4% (interquartile range, 16.7%–33.3%) and varied from 0% to 75.0%. Facilities in the lowest tertile of referral (<19.2%) were more likely to treat patients living in high-poverty neighborhoods (absolute difference, 21.8% [95% CI, 14.1%–29.4%]), had a higher patient to social worker ratio (difference, 22.5 [95% CI, 9.7–35.2]), and were more likely nonprofit (difference, 17.6% [95% CI, 7.7%–27.4%]) compared with facilities in the highest tertile of referral (>31.3%). In multivariable, multilevel analyses, factors associated with lower referral for transplantation, such as older age, white race, and nonprofit facility status, were not always consistent with the factors associated with lower waitlisting.
CONCLUSIONS AND RELEVANCE
In Georgia overall, a limited proportion of patients treated with dialysis were referred for kidney transplant evaluation between 2005 and 2011, but there was substantial variability in referral among facilities. Variables associated with referral were not always associated with waitlisting, suggesting that different factors may account for disparities in referral.
For most of the more than 600 000 patients in the United States with end-stage renal disease (ESRD),1 kidney transplantation represents the optimal treatment, providing longer survival, better quality of life, and substantial cost savings compared with dialysis.2 Despite these benefits, kidney transplantation is not available to all patients with ESRD, owing to the paucity of available organs, as well as longstanding racial/ethnic, socioeconomic, sex, age, and geographic disparities in access to kidney transplantation.3–6
The traditional framework for examining steps to receiving a kidney transplant in the United States starts with placement on the national deceased donor waiting list (waitlisting),7 since regional and national surveillance data do not report patient activities prior to waitlisting. However, a focus on earlier steps of the transplantation process, such as referral from a dialysis facility to the transplant center—without which the required medical evaluation, waitlisting, and, ultimately, transplantation cannot occur—may better inform intervention efforts to improve equity in early access to transplantation.5 Although significant variation in kidney transplantation rates exists across US dialysis facilities,8 the contribution of heterogeneity in transplant referral by dialysis facility clinicians vs other patient, facility, or neighborhood factors remains unknown.
In the United States, rates of kidney transplantation are the lowest in the Southeast and, in particular, Georgia.9 Partnering with the community-based Southeastern Kidney Transplant Coalition, which includes ESRD Network 6, patients, transplant centers, social workers, clinicians, patient advocacy groups, and others, we collected kidney transplantation referral data from all Georgia transplant centers as part of our Reducing Disparities in Access to Kidney Transplantation (RaDIANT) Community Study.10 The purpose of this study is to describe dialysis facility–level referral for kidney transplant evaluation in Georgia and the patient- and facility-level factors associated with referral and access to the national deceased donor waiting list.
Methods
Data Sources
Patient-level data were collected from all transplant referral forms between January 1, 2005, and December 31, 2012, received by all 3 adult transplant centers in Georgia: Emory Transplant Center (Atlanta), Georgia Regents Kidney and Pancreas Transplant Program (Augusta), and Piedmont Transplant Institute (Atlanta). Each transplant center sent referral data securely to ESRD Network 6, which served as the data coordinating center.
To ensure complete patient follow-up and to identify a cohort of non referred patients receiving dialysis in Georgia during the same period, we linked referral data to the 2014 United States Renal Data System (USRDS) Standard Analytic Files, which included data on all patients with ESRD from January 1, 2005, through September 20, 2012. The USRDS is a national surveillance data system that aggregates demographic, diagnosis, treatment, and facility information on nearly 2.5 million patients with ESRD from various data sources, including the Medical Evidence Report (CMS-2728), which is completed for all patients with ESRD at the start of treatment, as well as United Network for Organ Sharing files on waitlisting and transplantation.
Data on characteristics of the patients’ residential neighborhoods, as defined by patient 5-digit zip code tabulation area, were obtained from the 2007–2011 American Community Survey (http://www.census.gov/programs-surveys/acs/) and linked by patient zip code at start of dialysis to USRDS. Facility characteristics were obtained from the annual USRDS facility survey data.
This study was approved by the institutional review boards at Emory University, Georgia Regents University, and Piedmont Hospital. Collection of referral data was retrospective, and participant consent was waived.
Study Population
Patients referred to a Georgia transplant center from January 1, 2005, to December 31, 2012, were included in the study. A cohort of both referrals and non referrals within the study period was created; first, we identified a cohort of incident patients with ESRD initiating treatment on or after January 1, 2005, in a Georgia dialysis facility using the USRDS and excluded patients if they were younger than 18 years or 70 years or older or if they were waitlisted prior to starting dialysis. The referral data were then merged with USRDS records. We classified matching patients from the referral data as referred, and the remaining patients in the referral data who were not matched to the incident USRDS cohort of interest were excluded. Patients who started dialysis after September 30, 2011 (to ensure 1 year of follow-up for referral outcomes), were excluded for primary analysis.
Study Variables Outcomes
Outcomes
The primary outcome examined was referral for kidney transplant evaluation to 1 of the 3 transplant centers in Georgia within 1 year of starting dialysis among patients younger than 70 years. Since all dialysis facilities are required to educate patients about transplantation within the first 60 days of starting dialysis, we considered referral within the first year of dialysis as a proxy for access to appropriate care. Referral was defined as the date on which the transplant center received a referral form, primarily from a dialysis facility or referring health professional.
As a secondary outcome, we also examined whether a patient was placed on the national deceased donor waiting list (waitlisted) at any US transplant center within 1 year of referral for transplant evaluation. In addition, we examined crude data on the total number of patients receiving a transplant.
Patient- and Facility-Level Characteristics
Patient characteristics included demographic and clinical data reported by clinicians on the CMS-2728 form at the time of first dialysis treatment, including race/ethnicity, age at incident ESRD, sex, cause of ESRD, as well as other clinical characteristics potentially related to medical eligibility for transplantation, including body mass index greater than 35 (calculated as weight in kilograms divided by height in meters squared), tobacco use, cancer, and comorbidities. Proxies for socioeconomic status included pre-ESRD nephrology care and health insurance at first dialysis treatment, as well as aggregate residential zip code–level data on the percentages of black residents, high school dropouts (residents aged ≥25 years without a high school degree or equivalent), and poor households (living below 100% of the federal poverty threshold).
We assigned each patient to the dialysis facility in which they started treatment, since decisions regarding ESRD treatment are expected to occur within 3 months after starting dialysis for most patients. Facility-level characteristics examined included for-profit status, hospital-based vs freestanding facility, and the ratio of patients to social workers within a facility. We categorized the proportion of patients referred within 1 year over the entire study period at each facility into tertiles and examined whether characteristics varied by tertile.
Statistical Analyses
Demographic and clinical characteristics of the study population were examined using χ2 or t tests. Because the outcomes were binary and correlated (within facilities), a multivariable generalized linear mixed model was used. An intraclass correlation was estimated as a measure of proportion of total variance in patient referral attributable to facility-level clustering. Details regarding the multilevel model can be found in the eAppendix in the Supplement. Covariates that were statistically significant in bivariate analyses (P < .05) were included in multilevel analyses. Because the missing pattern was arbitrary, we used a fully conditional specification method to obtain multiple imputed data sets (n = 5) and used likelihood-based methods for inference.
In sensitivity analyses, we considered outcomes of whether patients treated with dialysis were ever referred for kidney transplantation during the entire study period (yes/no) and time to referral (censoring at date of death, waitlisting at any US transplant center, receipt of a living donor transplant, or study end [September 30, 2012)]).
SAS version 9.4 (SAS Institute Inc) and Stata version 13.1 (StataCorp) were used for analyses. All P values were 2-sided and considered statistically significant at the P < .05 level.
Results
Study Population
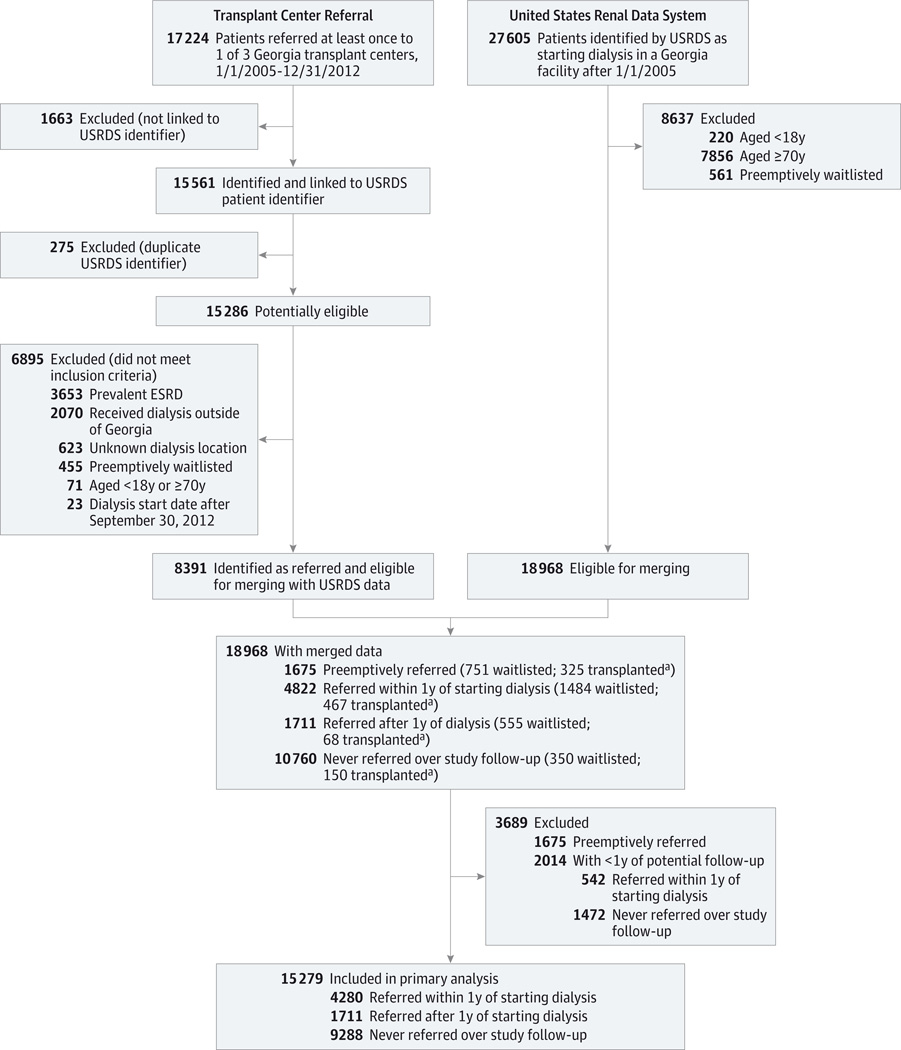
A total of 17 224 patients were referred to Georgia transplant centers over 8 years (January 1, 2005, through December 31, 2012); 15 561 of these (90.3%) were successfully identified and linked to a USRDS patient identifier, 275 of which were duplicates, leaving 15 286 patients with at least 1 referral (Figure 1). A cohort of 27 605 incident patients with ESRD initiating treatment on or after January 1, 2005, in a Georgia dialysis facility using the USRDS were identified, and patients younger than 18 years (n = 220) or 70 years or older (n = 7856) or who were waitlisted prior to starting dialysis (n = 561) were excluded (Figure 1). Of the 15 286 patients with a first referral, 8391 were identified in USRDS on merging and classified as referred. The remaining 6895 referred patients who were not matched to the incident USRDS cohort of interest were excluded because they were prevalent patients with ESRD (n = 3653 with start dates prior to January 1, 2005), their start date was after September 30, 2012 (n = 23), their dialysis treatment occurred in a facility outside of Georgia (n = 2070) or the location of the dialysis facility was unknown (n = 623), they were younger than 18 years or 70 years or older (n = 71), or they were preemptively waitlisted (n = 455). Last, in the merged data (Figure 1), 1675 were excluded because they were referred prior to the start of dialysis; waitlisting and transplantation among these patients, as well as included patients who were referred within a year of dialysis start, referred after 1 year, and never referred are also shown (Figure 1).
Figure 1.
Study Inclusion Criteria for Incident Patients With ESRD in Georgia: 2005–2011
a Among the 1675 preemptively referred, 30 received transplants outside Georgia and 128 received living donor transplants; among the 4822 referred within 1 year of starting dialysis, 51 received transplants outside Georgia and 171 received living donor transplants; among the 1711 referred after 1 year of starting dialysis, 14 received transplants outside Georgia and 23 received living donor transplants; among the 10 760 never referred, 55 received transplants outside Georgia and 39 received living donor transplants.
A total of 15 279 patients at 308 Georgia dialysis facilities were included in primary analyses. Patients excluded because of preemptive referral or preemptive transplantation were more likely young, white, and insured, and had fewer co-morbidities, compared with the study population. A more complete description of excluded patients is available in the eAppendix in the Supplement.
Facility Referral and Characteristics
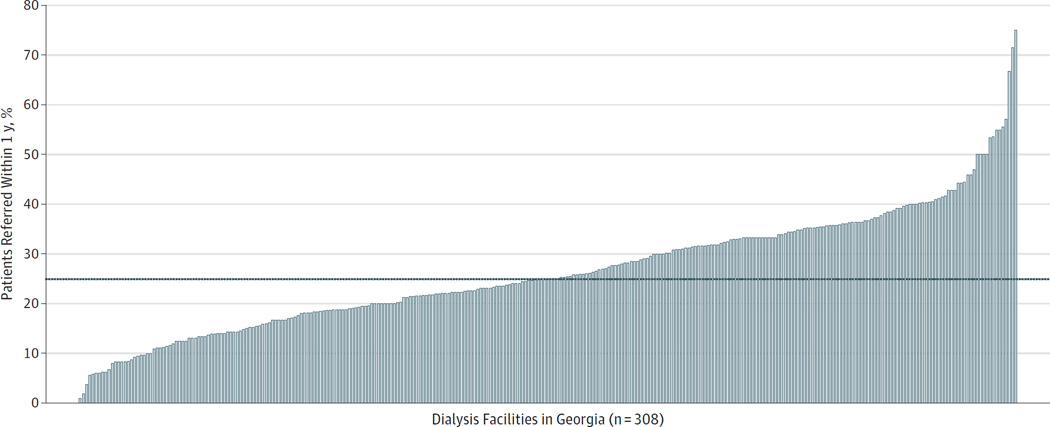
The median within-facility cumulative percentage of patients aged 18 through 69 years referred within 1 year of starting dialysis at 308 Georgia dialysis facilities was 24.4% (interquartile range, 16.7%–33.3%). There were 15 facilities (4.9%) that referred zero patients within 1 year of starting dialysis; the maximum referral in a year was 75.0% (Figure 2). The variance of the facility random effect was significantly different from zero (σ2u = 0.35 [SE, 0.04]). After accounting for patient mix, 7.5% of the total variation in referral was explained by facility-level clustering.
Figure 2.
Percentages of Patients With End-Stage Renal Disease Referred for Kidney Transplantation Within 1 Year of Starting Dialysis Among Georgia Dialysis Facilities: 2005–2011
Dotted line indicates median (24.4%).
The proportions of patients referred within 1 year over the entire study period at each facility were categorized into tertiles (low, 0.0%–19.2%; moderate, 19.3%–31.2%; and high, 31.3%–75.0%). Facilities with the lowest likelihood of referral for transplantion within 1 year of starting dialysis (tertile 3) were more likely to be nonprofit (difference, 17.6% [95% CI, 7.7% −27.4%]), to be hospital-based (vs freestanding; difference, 9.0% [95% CI, 2.8%–15.2%]), to have more patients (difference, 8.6 [95% CI, −4.4 to 21.6), to treat patients living in high-poverty neighborhoods (difference, 21.8% [95% CI, 14.1%−29.4%]), and to have a higher patient to social worker ratio (difference, 22.5 [95% CI, 9.7–35.2]) compared with facilities with the highest referral (tertile 1) (Table 1).
Table 1.
Characteristics of Dialysis Facilities With Lowest, Middle, and Highest Referral for Kidney Transplantation Within 1 Year in Georgia: 2005–2011
| Characteristic | Dialysis Facility Characteristics No. (%) |
Tertile of Transplant Referral, Median (Range) | PValuea | ||
|---|---|---|---|---|---|
| Lowest 13.1 (0–19.2) |
Middle 24.4 (19.3–31.2) |
Highest 36.4 (31.3–75.0) |
|||
| Facilities, No. | 308 | 103 | 103 | 102 | |
| Total No. of patients | 15 279 | 5125 | 5954 | 4200 | |
| Facility Incident Patient-Level Characteristics | |||||
| Age, mean (95% CI), y | 53.4 (53.0–53.8) | 53.8 (53.1–54.5) | 53.5 (53.0–54.0) | 53.0 (52.1–53.9) | .27 |
| Men, mean % (95% CI) | 53.6 (52.1–55.1) | 54.1 (51.1–57.1) | 54.3 (52.3–56.3) | 52.4 (49.5–55.3) | .53 |
| Race/ethnicity, mean % (95% CI) | |||||
| White, non-Hispanic | 34.6 (31.8–37.5) | 37.0 (31.5–42.6) | 32.0 (27.4–36.5) | 34.9 (30.1–39.6) | .36 |
| White, Hispanic | 1.8 (1.4–2.1) | 1.9 (1.2–2.6) | 1.7 (1.1–2.3) | 1.8 (1.1–2.4) | .93 |
| Black, non-Hispanic | 61.9 (58.9–64.9) | 60.3 (54.6–66.0) | 65.0 (60.3–69.8) | 60.2 (55.1–65.3) | .33 |
| Black | 1.7 (1.3–2.2) | 0.8 (0.5–1.1) | 1.3 (0.7–1.9) | 3.1 (2.0–4.3) | <.001 |
| Attributed cause of ESRD, mean % (95% CI)b | |||||
| Diabetes | 46.9 (45.1–48.8) | 48.2 (44.7–51.6) | 46.3 (43.6–48.9) | 46.4 (42.7–50.1) | .67 |
| Hypertension | 34.0 (31.9–36.1) | 32.6 (28.9–36.3) | 35.1 (32.0–38.1) | 34.3 (30.3–38.4) | .63 |
| Glomerulonephritis | 4.8 (4.1–5.4) | 4.3 (3.3–5.3) | 5.3 (4.1–6.4) | 4.7 (3.6–5.8) | .45 |
| Other | 14.3 (13.1–15.5) | 14.9 (12.9–17.0) | 13.4 (11.5–15.3) | 14.5 (12.3–16.7) | .57 |
| Patient 2incident year, No. of incident patients, mean (95% CI) | |||||
| 2005 | 7.2 (6.1–8.3) | 8.1 (5.3–10.9) | 8.5 (7.0–10.0) | 4.9 (3.7–6.2) | .02 |
| 2006 | 7.5 (6.3–8.7) | 8.2 (5.2–11.2) | 8.7 (7.2–10.2) | 5.5 (4.3–6.7) | .07 |
| 2007 | 7.2 (6.2–8.2) | 7.4 (4.9–9.8) | 8.4 (7.1–9.8) | 5.8 (4.6–7.0) | .10 |
| 2008 | 7.3 (6.3–8.2) | 7.5 (5.2–9.8) | 8.2 (6.9–9.6) | 6.0 (4.8–7.3) | .19 |
| 2009 | 7.6 (6.8–8.3) | 7.3 (6.0–8.6) | 8.9 (7.5–10.3) | 6.5 (5.3–7.7) | .03 |
| 2010 | 7.3 (6.5–8.0) | 6.3 (5.1–7.5) | 8.6 (7.2–10.1) | 6.9 (5.7–8.0) | .03 |
| 2011 | 5.7 (5.1–6.2) | 5.0 (4.1–5.9) | 6.4 (5.4–7.4) | 5.6 (4.8–6.4) | .09 |
| Facility % of Incident Patient Clinical and Laboratory Measures, Mean % (95% CI) | |||||
| BMI ≥35b,c | 24.1 (23.0–25.3) | 23.5 (21.3–25.6) | 25.0 (23.1–27.0) | 23.9 (21.9–25.9) | .54 |
| Congestive heart failure | 25.3 (23.7–26.9) | 27.6 (24.6–30.7) | 26.4 (23.9–28.8) | 21.8 (19.2–24.5) | .008 |
| Atherosclerotic heart disease | 10.8 (9.5–12.2) | 10.8 (8.6–13.0) | 12.4 (9.7–15.2) | 9.3 (7.1–11.4) | .18 |
| Other cardiac disease | 12.6 (11.4–13.9) | 12.8 (10.7–14.9) | 13.1 (11.2–15.1) | 12.0 (9.5–14.4) | .74 |
| Cerebrovascular disease (stroke) | 8.2 (7.4–9.0) | 9.2 (7.9–10.5) | 8.7 (7.4–10.0) | 6.6 (5.1–8.1) | .02 |
| Peripheral vascular disease | 9.6 (8.4–10.8) | 10.7 (8.9–12.4) | 10.4 (8.0–12.7) | 7.8 (5.5–10.0) | .12 |
| Hypertension | 86.4 (84.8–87.9) | 84.2 (80.7–87.8) | 88.1 (86.6–89.6) | 86.8 (84.2–89.4) | .13 |
| Diabetes | 54.5 (52.8–56.3) | 54.2 (50.7–57.7) | 57.0 (54.8–59.2) | 52.4 (49.2–55.7) | .10 |
| Chronic obstructive pulmonary disease | 6.4 (5.6–7.2) | 8.2 (6.5–9.9) | 6.7 (5.4–8.0) | 4.4 (3.4–5.4) | .001 |
| Tobacco useb | 9.5 (8.6–10.4) | 11.0 (9.3–12.6) | 10.2 (8.7–11.7) | 7.2 (57–8.7) | .002 |
| Cancer | 4.5 (4.0–5.0) | 5.0 (4.0–6.0) | 4.5 (3.7–5.3) | 4.0 (3.3–4.8) | .29 |
| Facility % of Incident Patient Socioeconomic Characteristics, Mean % (95% CI) | |||||
| Pre-ESRD nephrology careb | 60.7 (58.4–63.0) | 61.4 (57.3–65.6) | 61.0 (57.5–64.5) | 59.6 (55.3–64.0) | .81 |
| Primary health insurance provider | |||||
| Medicare | 36.7 (35.1–38.4) | 39.2 (36.1–42.3) | 38.6 (36.4–40.8) | 32.4 (29.3–35.4) | .001 |
| Medicaid | 26.2 (24.5–27.8) | 29.8 (26.7–33.0) | 27.9 (25.4–30.4) | 20.7 (18.1–23.3) | <.001 |
| Employer group | 30.1 (28.1–32.0) | 21.9 (18.9–25.0) | 29.7 (26.9–32.5) | 38.6 (34.9–42.3) | <.001 |
| Other coverage | 9.5 (8.3–10.7) | 10.2 (7.8–12.5) | 8.9 (6.9–10.9) | 9.4 (7.6–11.2) | .69 |
| No coverage | 17.5 (16.3–18.8) | 18.3 (15.8–20.8) | 17.2 (15.4–19.0) | 17.1 (15.0–19.2) | .69 |
| Facility % of Incident Patient Neighborhood (Zip Code) Characteristics, Mean % (95% CI) | |||||
| Neighborhood poverty (% of zip code residents below poverty) | |||||
| 0%-19.9% below poverty | 55.5 (52.3–58.8) | 45.9 (40.3–51.4) | 53.2 (47.9–58.5) | 67.7 (62.4–72.9) | <.001 |
| ≥20% below poverty | 44.5 (41.2–47.7) | 54.1 (48.6–59.7) | 46.8 (41.5–52.1) | 32.3 (27.1–37.6) | <.001 |
| Average % black, mean (95% CI) | 39.3 (37.1–41.5) | 36.2 (32.4–40.0) | 41.2 (37.4–45.0) | 40.5 (36.5–44.6) | .15 |
| Average % high school graduates, mean (95% CI) | 81.4 (80.8–82.0) | 78.8 (77.8–79.8) | 81.2 (80.3–82.1) | 84.3 (83.5–85.2) | <.001 |
| Dialysis Facility Characteristics, No. (%) | |||||
| Profit statusb | |||||
| For-profit | 261 (86.4) | 74 (75.5) | 93 (90.3) | 94 (93.1) | .001 |
| Nonprofit | 41 (13.6) | 24 (24.5) | 10 (9.7) | 7 (6.9) | |
| Type of facilityb | |||||
| Freestanding | 290 (95.4) | 90 (90.0) | 100 (97.1) | 100 (99.0) | .006 |
| Hospital-based | 14 (4.6) | 10 (10.0) | 3 (2.9) | 1 (1.0) | |
| Facility size (No. of patients) | |||||
| ≤25 | 118 (38.8) | 36 (36.0) | 29 (28.2) | 53 (53.9) | .01 |
| 26–54 | 85 (28.0) | 29 (29.0) | 29 (28.2) | 27 (26.7) | |
| 55–78 | 54 (17.7) | 20 (20.0) | 23 (22.3) | 11 (10.9) | |
| >79 | 47 (15.5) | 15 (15.0) | 22 (21.4) | 10 (9.9) | |
| Patient to social worker ratiod | |||||
| Mean (95% CI) | 55.9 (50.3–61.5) | 61.2 (51.5–71.0) | 67.5 (57.1–78.0) | 38.8 (30.5–47.1) | <.001 |
| Quartile, No. (%) | |||||
| <39:1 (quartile 1) | 114 (39.5) | 31 (32.6) | 32 (32.7) | 51 (53.1) | .001 |
| 40:1–74:1 (quartile 2) | 71 (24.6) | 27 (28.4) | 19 (19.4) | 25 (26.0) | |
| 75:1–102:1 (quartile 3) | 56 (19.4) | 21 (22.1) | 21 (21.4) | 14 (14.6) | |
| >102:1 (quartile 4) | 48 (16.6) | 16 (16.8) | 26 (26.5) | 6 (6.3) | |
Abbreviations: BMI, body mass index; ESRD, end-stage renal disease.
Across tertiles of referral, by analysis of variance or χ2 test.
A total of 4 facilities (1.3%) were missing information on BMI and tobacco use; 7 facilities (2.2%) were missing information on pre-ESRD nephrology care; 3 facilities (1.0%) were missing information on primary cause of ESRD; 6 facilities were missing information on for-profit status; and 4 facilities were missing information on hospital-based vs freestanding status.
Calculated as weight in kilograms divided by height in meters squared.
Number of patients for every 1 social worker. Calculated only among those facilities that have social workers. Overall, n = 5 facilities did not have a social worker (n = 4 for facilities in the lowest tertile of referral; n = 1 for those in the intermediate tertile; and n = 0 for those in the highest tertile).
Patient Referral and Characteristics
Among 15 279 patients aged 18 through 69 years initiating dialysis in 308 Georgia facilities from 2005 to 2011, a total of 4280 patients (28.0%) were referred to a Georgia kidney transplant center within 1 year of starting dialysis, and 39.2% were referred at any time during follow-up. Referral increased over the study period, from 22.0% of incident patients with ESRD in 2005 to 34.2% of patients in 2011 overall, with referral patterns among each tertile showing a consistent upward trend (P < .001 for trend for each tertile) (eTable 1 in the Supplement).
Compared with patients referred within a year, patients not referred within 1 year of starting dialysis were significantly older (difference, 5.7 years [95% CI, 5.3–6.1 years]) and more likely white (absolute difference, 5.0% [95% CI, 3.4%–6.6%]) and female (difference, 3.8% [95% CI, 2.1%–5.6%]). Patients not referred had higher reported tobacco use (difference, 3.7% [95% CI, 2.7% 4.7%]), more comorbidities (eg, diabetes; difference, 3.9% [95% CI, 2.1% – 5.6%]), lower utilization of pre-ESRD nephrology care (difference, 3.5% [95% CI, 1.7%–5.3%]), and were more likely to have Medicaid (difference, 8.8% [95% CI, 7.3%–10.2%]) or Medicare (difference, 9.9% [95% CI, 8.6%–11.3%]) insurance and to live in high-poverty neighborhoods (difference, 8.7% [95% CI, 6.9%–10.5%]) vs those referred within a year. Those not referred were more likely to receive treatment at dialysis facilities that were nonprofit (difference, 7.4% [95% CI, 6.1%–8.6%]), had larger facility size (overall difference, 13.1 patients [95% CI, 9.9–16.2 patients]), and had higher patient to social worker ratios (difference, 4.4 [95% CI, 2.7–6.1]), compared with those referred within 1 year (Table 2).
Table 2.
Characteristics of Patients With End-Stage Renal Disease Referred for Kidney Transplantation Within 1 Year of Starting Dialysis vs Not Referred Within 1Year in Georgia: 2005–2011
| Characteristic | No. (%) |
P Valuea |
||
|---|---|---|---|---|
| Study Population (n = 15 279) |
Transplant Within 1 Year | |||
| Referred (n = 4280 [28.0%]) |
Not Referred (n = 10999 [72.0%]) |
|||
| Patient-Level Characteristics at Start of Dialysis | ||||
| Age, mean (95% CI), y | 53.2 (53.0–53.4) | 49.1 (48.7–49.4) | 54.8 (54.6–54.8) | <.001 |
| Age category, y | ||||
| 18–29 | 690 (4.5) | 334 (7.8) | 356 (3.2) | <.001 |
| 30–39 | 1462 (9.6) | 644 (15.0) | 818 (7.4) | |
| 40–49 | 2873 (18.8) | 1004 (23.5) | 1869 (17.0) | |
| 50–59 | 4763 (31.2) | 1348 (31.5) | 3415 (31.1) | |
| 60–69 | 5491 (35.9) | 950 (22.2) | 4541 (41.3) | |
| Sex | ||||
| Male | 8381 (54.9) | 2465 (57.6) | 5916 (53.8) | <.001 |
| Female | 6898 (45.1) | 1815 (42.4) | 5083 (46.2) | |
| Race/ethnicity | ||||
| White, non-Hispanic | 4662 (30.5) | 1156 (27.0) | 3506 (31.9) | <.001 |
| White, Hispanic | 352 (2.3) | 104 (2.4) | 248 (2.3) | |
| Black, non-Hispanic | 9992 (65.4) | 2906 (67.9) | 7086 (64.4) | |
| Other race/ethnicity | 273 (1.8) | 114 (2.7) | 159 (1.4) | |
| Attributed cause of ESRD | ||||
| Diabetes | 6810 (44.6) | 1829 (42.7) | 4981 (45.3) | <.001 |
| Hypertension | 5253 (34.4) | 1570 (36.7) | 3683 (33.5) | |
| Glomerulonephritis | 734 (4.8) | 296 (6.9) | 438 (4.0) | |
| Other | 2482 (16.2) | 585 (13.7) | 1897 (17.2) | |
| Patient incident year | ||||
| 2005 | 2216 (14.5) | 487 (11.4) | 1729 (15.7) | <.001 |
| 2006 | 2303 (15.1) | 618 (14.4) | 1685 (15.3) | |
| 2007 | 2217 (14.5) | 574 (13.4) | 1643 (14.9) | |
| 2008 | 2237 (14.6) | 596 (13.9) | 1641 (14.9) | |
| 2009 | 2328 (15.2) | 691 (16.1) | 1637 (14.9) | |
| 2010 | 2237 (14.6) | 723 (16.9) | 1514 (13.8) | |
| 2011 | 1741 (11.4) | 591 (13.8) | 1150 (10.5) | |
| Clinical and Laboratory Measures at Start of Dialysis | ||||
| BMI >35b | 3532 (23.1) | 959 (22.4) | 2573 (23.4) | .19 |
| Congestive heart failure | 4096 (26.8) | 853 (19.9) | 3243 (29.5) | <.001 |
| Atherosclerotic heart disease | 1754 (11.5) | 331 (7.7) | 1423 (12.9) | <.001 |
| Other cardiac disease | 2007 (13.1) | 410 (9.6) | 1597 (14.5) | <.001 |
| Cerebrovascular disease (stroke) | 1362 (8.9) | 230 (5.4) | 1132 (10.3) | <.001 |
| Peripheral vascular disease | 1482 (9.7) | 265 (6.2) | 1217 (11.1) | <.001 |
| Hypertension | 13 438 (88.0) | 3854 (90.0) | 9584 (87.1) | <.001 |
| Diabetes | 8344 (54.6) | 2218 (51.8) | 6126 (55.7) | <.001 |
| Chronic obstructive pulmonary disease | 1023 (6.7) | 136 (3.2) | 887 (8.1) | <.001 |
| Tobacco use | 1559 (10.2) | 325 (7.6) | 1234 (11.2) | <.001 |
| Cancer | 714 (4.7) | 85 (2.0) | 629 (5.7) | <.001 |
| Socioeconomic Characteristics at Start of Dialysis | ||||
| Pre-ESRD nephrology carec | ||||
| Yes | 7865 (60.0) | 2362 (62.4) | 5503 (58.9) | <.001 |
| No | 5254 (40.0) | 1421 (37.6) | 3833 (41.1) | |
| Primary health insurance providerc | ||||
| Medicare | 3266 (21.4) | 609 (14.2) | 2657 (24.2) | <.001 |
| Medicaid | 3870 (25.3) | 814 (19.0) | 3056 (27.8) | |
| Employer group | 4267 (27.9) | 1742 (40.7) | 2525 (23.0) | |
| Other coverage | 693 (4.5) | 191 (4.5) | 502 (4.6) | |
| No coverage | 3132 (20.5) | 920 (21.5) | 2212 (20.1) | |
| Neighborhood (Zip Code) Characteristicsc | ||||
| Neighborhood poverty (% of zip code below poverty) | ||||
| 0%–19% (Low) | 7027 (47.5) | 1714 (41.2) | 5313 (49.9) | <.001 |
| >20% (High) | 7779 (52.5) | 2447 (58.8) | 5332 (50.1) | |
| Average % black, mean (95% CI) | 42.0 (41.6–42.5) | 41.9 (41.1–42.7) | 42.1 (41.5–42.6) | .79 |
| Average % high school graduates, mean (95% CI) | 81.3 (81.2–81.5) | 82.4 (82.2–82.7) | 80.9 (80.7–81.0) | <.001 |
| Dialysis Facility Characteristics | ||||
| For-profitc | 12 417 (82.1) | 3725 (87.3) | 8692 (80.0) | <.001 |
| Freestandingc | 13 949 (91.4) | 4073 (95.2) | 9876 (89.9) | <.001 |
| Facility size (No. of patients)c | ||||
| <25 | 3315 (21.7) | 1098 (25.7) | 2217 (20.2) | <.001 |
| 26–54 | 4224 (27.7) | 1062 (24.8) | 3162 (28.8) | |
| 55–78 | 3837 (25.1) | 1028 (24.0) | 2809 (25.6) | |
| >79 | 3894 (25.5) | 1091 (25.5) | 2803 (25.5) | |
| Patient to social worker ratiod | ||||
| Mean (95% CI) | 72.8 (72.0–73.5) | 69.6 (68.1–71.1) | 74.0 (73.1–74.9) | <.001 |
| Quartile, No. (%) | ||||
| <39:1 (quartile 1) | 3429 (23.2) | 1103 (26.8) | 2326 (21.8) | <.001 |
| 40:1–74:1 (quartile 2) | 3994 (27.0) | 1081 (26.2) | 2913 (27.3) | |
| 75:1–102:1 (quartile 3) | 3602 (24.3) | 905 (21.9) | 2697 (25.3) | |
| >102:1 (quartile 4) | 3772 (25.5) | 1035 (27.4) | 2737 (25.6) | |
Abbreviations: BMI, body mass index; ESRD, end-stage renal disease.
Across categories of patients referred or not referred for transplantation within 1 year, by analysis of variance or χ2 test.
Calculated as weight in kilograms divided by height in meters squared.
A total of 14.1% of patients were missing data on pre-ESRD nephrology care; 0.3% were missing insurance information; 3.1% were missing neighborhood characteristics from Census data; 0.9% were missing facility profit status; less than 0.1% were missing facility type; 0.2% were missing facility size information.
Number of patients for every 1 social worker. Calculated only among those facilities that have social workers.
Patient Waitlisting and Characteristics
Characteristics of those waitlisted within 1 year of referral vs not are shown in Table 3. Patients who received a living donor transplant but who were never waitlisted were considered waitlisted (n = 3). Among those referred within 1 year (n = 4280 patients with ESRD), a total of 918 patients (21.5%) were subsequently waitlisted within 1 year of referral.
Table 3.
Characteristics of Patients With End-Stage Renal Disease Who Were Waitlisted or Received a Kidney Transplant Within 1 Year of Referral in Georgia Among Those Referred for Transplantation Within 1 Year of Starting Dialysis: 2005–2011
| Characteristic | No. (%) | P Valuea | ||
|---|---|---|---|---|
| Patients Referred Within 1 Year of ESRD (n = 4280) |
Within 1 Year of Referral, Among Referred Patients |
|||
| Waitlisted or Received Transplant (n = 918) |
Not Waitlisted (n = 3362) |
|||
| Patient-level Characteristics at Start of Dialysis | ||||
| Age, mean (95% CI), y | 49.1 (48.7–49.4) | 48.0 (47.2–48.9) | 49.3 (48.9–49.7) | .15 |
| Age category, y | ||||
| 18–29 | 334 (7.8) | 96 (10.5) | 238 (7.1) | .01 |
| 30–39 | 644 (15.1) | 143 (15.6) | 501 (14.9) | |
| 40–49 | 1004 (23.5) | 210 (22.9) | 794 (23.6) | |
| 50–59 | 1348 (31.5) | 270 (29.4) | 1078 (32.1) | |
| 60–69 | 950 (22.2) | 199 (21.7) | 751 (22.3) | |
| Sex | ||||
| Male | 2465 (57.6) | 551 (60.0) | 1914 (56.9) | .09 |
| Female | 1815 (42.4) | 367 (40.0) | 1448 (43.1) | |
| Race/ethnicity | ||||
| White, non-Hispanic | 1156 (27.0) | 291 (31.7) | 865 (25.7) | <.001 |
| White, Hispanic | 104 (2.4) | 28 (3.1) | 76 (2.3) | |
| Black, non-Hispanic | 2906 (67.9) | 561 (61.1) | 2345 (69.8) | |
| Other race/ethnicity | 114 (2.7) | 38 (4.1) | 76 (2.3) | |
| Attributed cause of ESRD | ||||
| Diabetes | 1829 (42.7) | 314 (34.2) | 1515 (45.1) | <.001 |
| Hypertension | 1570 (36.7) | 328 (35.7) | 1242 (36.9) | |
| Glomerulonephritis | 296 (6.9) | 103 (11.2) | 193 (5.7) | |
| Other | 585 (13.7) | 173 (18.9) | 412 (12.3) | |
| Patient incident year | ||||
| 2005 | 487 (11.4) | 99 (10.8) | 388 (11.5) | .27 |
| 2006 | 618 (14.4) | 117 (12.8) | 501 (14.9) | |
| 2007 | 574 (13.4) | 121 (13.2) | 453 (13.5) | |
| 2008 | 596 (13.9) | 138 (15.0) | 458 (13.6) | |
| 2009 | 691 (16.1) | 167 (18.2) | 524 (15.6) | |
| 2010 | 723 (16.9) | 158 (17.2) | 565 (16.8) | |
| 2011 | 591 (13.8) | 118 (12.9) | 473 (14.1) | |
| Clinical and Laboratory Measures at Start of Dialysis | ||||
| BMI >35b | 959 (22.4) | 138 (15.0) | 821 (24.4) | <.001 |
| Congestive heart failure | 853 (19.9) | 123 (13.4) | 730 (21.7) | <.001 |
| Atherosclerotic heart disease | 331 (7.7) | 59 (6.4) | 272 (8.1) | .10 |
| Other cardiac disease | 410 (9.6) | 67 (7.3) | 343 (10.2) | .008 |
| Cerebrovascular disease (stroke) | 230 (5.4) | 33 (3.6) | 197 (5.9) | .007 |
| Peripheral vascular disease | 265 (6.2) | 25 (2.7) | 240 (7.1) | <.001 |
| Hypertension | 3854 (90.1) | 801 (87.3) | 3053 (90.8) | .001 |
| Diabetes | 2218 (51.8) | 394 (42.9) | 1824 (54.3) | <.001 |
| Chronic obstructive pulmonary disease | 136 (3.2) | 9 (1.0) | 127 (3.8) | <.001 |
| Tobacco use | 325 (7.6) | 50 (5.5) | 275 (8.2) | .006 |
| Cancer | 85 (2.0) | 14 (1.5) | 71 (2.1) | .26 |
| Socioeconomic Characteristics at Start of Dialysis | ||||
| Pre-ESRD nephrology carec | ||||
| Yes | 2362 (55.2) | 527 (64.1) | 1835 (62.0) | .26 |
| No | 1421 (33.2) | 295 (35.9) | 1126 (38.0) | |
| Primary health insurance providerc | ||||
| Medicare | 609 (14.2) | 89 (9.7) | 520 (15.5) | <.001 |
| Medicaid | 814 (19.0) | 100 (10.9) | 714 (21.3) | |
| Employer group | 1742 (40.7) | 483 (52.6) | 1259 (37.5) | |
| Other coverage | 191 (4.5) | 63 (6.9) | 128 (3.8) | |
| No coverage | 920 (21.5) | 183 (19.9) | 737 (22.0) | |
| Neighborhood (Zip Code) Characteristicsc | ||||
| Neighborhood poverty (% zip code Below poverty) | ||||
| 0%–19% (Low) | 1714 (41.2) | 324 (36.1) | 1390 (42.6) | <.001 |
| >20% (High) | 2447 (58.8) | 574 (63.9) | 1873 (57.4) | |
| Average % black, mean (SD) | 41.9 (41.1–42.7) | 37.0 (35.3–38.7) | 43.2 (42.3–44.2) | <.001 |
| Average % high school graduates, mean (SD) | 82.4 (82.2–82.7) | 83.4 (82.8–83.9) | 82.2 (81.9–82.4) | <.001 |
| Dialysis Facility Characteristics | ||||
| For-profitc | 3725 (87.3) | 817 (89.3) | 2908 (86.8) | .05 |
| Freestanding facilityc | 4073 (95.2) | 889 (96.8) | 3184 (94.7) | .008 |
| Facility size (No. of patients)c | ||||
| <25 | 1098 (25.7) | 252 (27.5) | 846 (25.2) | .06 |
| 26–54 | 1062 (24.8) | 222 (24.2) | 840 (25.0) | |
| 55–78 | 1028 (24.0) | 193 (21.0) | 835 (24.8) | |
| >79 | 1091 (25.5) | 251 (27.3) | 840 (25.0) | |
| Patient to social worker ratiod | ||||
| Mean (SD) | 69.6 (68.1–71.1) | 68.2 (65.0–71.4) | 70.0 (68.3–71.7) | .49 |
| Quartile, No. (%) | ||||
| <39:1 (quartile 1) | 1103 (26.8) | 259 (28.7) | 844 (26.2) | .40 |
| 40:1–74:1 (quartile 2) | 1081 (26.2) | 221 (24.5) | 860 (26.7) | |
| 75:1–102:1 (quartile 3) | 905 (21.9) | 197 (21.8) | 708 (22.0) | |
| >102:1 (quartile 4) | 1035 (27.4) | 225 (24.9) | 810 (25.1) | |
Abbreviations: BMI, body mass index; ESRD, end-stage renal disease.
Across categories of waitlisted or transplanted within 1 year vs not waitlisted or transplanted within 1 year, among those referred, by analysis of variance or χ2 test.
Calculated as weight in kilograms divided by height in meters squared.
A total of 11.6% of patients were missing data on pre-ESRD nephrology care; <0.1% were missing insurance information; 2.8% were missing neighborhood characteristics from Census data; 0.4% were missing facility profit status; less than 0.1% were missing facility type; <0.1% were missing facility size information.
Number of patients for every 1 social worker. Calculated only among those facilities that have social workers.
Factors Associated With Patient Referral for Kidney Transplantation Within 1 Year of Starting Dialysis
In adjusted models (17.6% of patients with imputed covariate data), older age (60–69 vs 18–29 years; odds ratio [OR], 0.19 [95% CI: 0.15–0.23]), female sex (OR, 0.89 [95% CI, 0.83–0.96]), other cause of ESRD (vs hypertension) (OR, 0.66 [95% CI, 0.58–0.74]), Medicaid (vs Medicare) insurance (OR, 0.85 [95% CI, 0.73–0.98]), higher neighborhood poverty (per 5% increase; OR, 0.94 [95% CI, 0.91–0.96]), and generally more comorbidities were all associated with lower likelihood of patient referral within 1 year of starting dialysis in multilevel analyses (Table 4). In contrast, patients who were black (vs white) (OR, 1.22 [95% CI, 1.10–1.35]), had employer (vs Medicare) insurance (OR, 2.12 [95% CI, 1.89–2.38]), pre-ESRD nephrology care (OR, 1.27 [95% CI, 1.16–1.40]), and were treated at for-profit dialysis facilities (OR, 1.51 [95% CI, 1.20–1.91]) were more likely to be referred within a year of starting dialysis than their counterparts.
Table 4.
Association of Patient- and Dialysis Facility-level Factors With Referral for Kidney Transplantation in Georgia Within 1 Year of Starting Dialysis, and Waitlisting Within 1Year of Referral: 2005–2011
| Covariate | Odds Ratio (95% CI) | |
|---|---|---|
| Referral Within 1 Year of ESRD (n = 15 279) |
Waitlisting or Transplant Receipt Within 1 Year of Referral, Among Patients Referred Within 1 Year of ESRD (n = 4280) |
|
| Patient-Level Characteristics | ||
| Age, y | ||
| 18–29 | 1 [Reference] | 1 [Reference] |
| 30–39 | 0.77 (0.62–0.94) | 0.82 (0.58–1.15) |
| 40–49 | 0.48 (0.40–0.58) | 0.77 (0.56–1.10) |
| 50–59 | 0.35 (0.28–0.42) | 0.73 (0.53–1.00) |
| 60–69 | 0.19 (0.15–0.23) | 0.83 (0.57–1.20) |
| Female vs male | 0.89 (0.83–0.96) | 0.93 (0.78–1.09) |
| Race/ethnicity | ||
| Non-Hispanic white | 1 [Reference] | 1 [Reference] |
| Hispanic white | 0.94 (0.66–1.34) | 1.12 (0.70–1.78) |
| Non-Hispanic black | 1.22 (1.10–1.35) | 0.77 (0.64–0.93) |
| Other | 1.95 (1.47–2.58) | 1.35 (0.86–2.13) |
| ESRD cause | ||
| Hypertension | 1 [Reference] | 1 [Reference] |
| Diabetes | 1.00 (0.89–1.13) | 0.90 (0.70–1.15) |
| Glomerulonephritis | 1.20 (1.00–1.44) | 1.67 (1.27–2.19) |
| Other | 0.66 (0.58–0.74) | 1.46 (1.14–1.86) |
| Year of incident ESRD | ||
| 2005 | 1 [Reference] | 1 [Reference] |
| 2006 | 1.36 (1.14–1.62) | 0.95 (0.69–1.30) |
| 2007 | 1.29 (1.11–1.51) | 1.12 (0.81–1.56) |
| 2008 | 1.38 (1.18–1.61) | 1.28 (0.92–1.78) |
| 2009 | 1.59 (1.34–1.87) | 1.44 (1.06–1.94) |
| 2010 | 1.80 (1.52–2.13) | 1.18 (0.86–1.62) |
| 2011 | 1.97 (1.65–2.35) | 1.11 (0.80–1.53) |
| Clinical and Laboratory Measures (Yes vs No) | ||
| Congestive heart failure | 0.78 (0.71–0.86) | 0.75 (0.60–0.93) |
| Atherosclerotic heart disease | 0.88 (0.76–1.02) | 1.08 (0.77–1.51) |
| Other cardiac disease | 0.83 (0.74–0.93) | 0.82 (0.61–1.11) |
| Cerebrovascular disease (stroke) | 0.67 (0.57–0.80) | 0.84 (0.57–1.24) |
| Peripheral vascular disease | 0.79 (0.68–0.93) | 0.45 (0.29–0.70) |
| Hypertension | 1.35 (1.19–1.54) | 0.81 (0.62–1.04) |
| Diabetes | 0.98 (0.89–1.08) | 0.86 (0.70–1.05) |
| Chronic obstructive pulmonary disease | 0.62 (0.50–0.76) | 0.30 (0.16–0.58) |
| Tobacco use | 0.78 (0.67–0.91) | 0.73 (0.53–1.01) |
| Cancer | 0.39 (0.31–0.50) | 0.68 (0.36–1.30) |
| Socioeconomic Characteristics | ||
| Pre-ESRD nephrology care: yes vs no | 1.27 (1.16–1.40) | 1.14 (0.96–1.36) |
| Health insurance | ||
| Medicare | 1 [Reference] | 1 [Reference] |
| Medicaid | 0.85 (0.73–0.98) | 0.87 (0.62–1.22) |
| Employer group | 2.12 (1.89–2.38) | 2.10 (1.58–2.77) |
| Other coverage | 1.35 (1.10–1.65) | 2.72 (1.80–4.09) |
| No coverage | 1.10 (0.96–1.25) | 1.36 (0.98–1.87) |
| Neighborhood Characteristics | ||
| Neighborhood poverty (per 5% increase) | 0.94 (0.91–0.96) | 0.92 (0.87–0.97) |
| Dialysis Facility Characteristics | ||
| Patient to social worker ratio | ||
| 0–39:1 | 1 [Reference] | 1 [Reference] |
| 40:1–74:1 | 0.89 (0.72–1.09) | 0.84 (0.64–1.09) |
| 75:1–102:1 | 0.73 (0.58–0.91) | 0.96 (0.72–1.28) |
| ≥102:1 | 0.89 (0.67–1.19) | 0.94 (0.72–1.23) |
| For-profit vs nonprofit | 1.51 (1.20–1.91) | 1.09 (0.83–1.44) |
Abbreviation: ESRD, end-stage renal disease.
Factors Associated With Patient Waitlisting With in 1 Year of Referral
In contrast to referral, sex and age were not significantly associated with waitlisting, and black (vs white) patients had lower odds of waitlisting within 1 year of referral (OR, 0.77 [95% CI, 0.64–0.93]) (Table 4). Dialysis facility characteristics, including patient to social worker ratio and for-profit status, were not associated with waitlisting.
Transplantation
There were a total of 685 living (36.6%) or deceased (63.4%) donor transplants among the 15 279 individuals (3.1% of all patients with ESRD) during the study follow-up. A total of 467 (10.9%) were among those referred within 1 year of ESRD (Figure 1).
Sensitivity Analyses
Demographic, clinical, socioeconomic, and dialysis facility characteristics were similar among patients who were ever referred for transplantation vs those referred within 1 year (Table 2 in the Supplement). Hazard ratios from time-to-referral and time-to waitlisting analyses, which were similar to odds ratios obtained from the main analyses, are shown in eTable 3 and eTable 4 in the Supplement.
Discussion
We found that only 28.0% of all patients with incident ESRD aged 18 through 69 years in Georgia were referred for transplantation within 1 year of starting dialysis, and referral varied significantly across the 308 dialysis facilities, from 0% to 75.0%. Furthermore, factors associated with lower referral for transplantation, such as white race, older age, and nonprofit facility status, were not necessarily the same as those associated with lower waitlisting. Results of this study suggest that referral for transplantation among Georgia dialysis facilities is not uniform and that national surveillance data measuring waitlisting and transplantation, but not referral, may be inadequate to assess and intervene on disparities in access to kidney transplantation.
Although the proportion of patients who should be referred for kidney transplantation within 1 year of ESRD is unknown, 28% is likely low. Ineligibility due to medical contra indications is estimated to be less than 15% in the few single-center studies that have been conducted.11,12 However, determination of eligibility for transplantation is complex and varies across transplant centers. Although active drug or alcohol abuse, untreated psychiatric conditions, active cancer, systemic infection, and non adherence are common exclusion criteria for transplant surgery,13 none are permanent conditions that necessarily preclude transplant referral.
National guidelines recommend that, if there is any uncertainty about eligibility, the patient should be referred for transplantation.14 However, nephrologists and dialysis facility staff may be unsure of which patients to refer,15 which may lead to significant facility-level variation in referral, as observed in our study. Dialysis professionals may need more guidance about what constitutes an appropriate vs inappropriate referral to ensure that appropriate candidates are referred for transplantation.16 It is also possible that, despite Centers for Medicare & Medicaid Services (CMS) requirements that facilities must educate their patients about transplantation and track patients’ referrals for transplantation,17 the level of detail facility staff present to patients on treatment options is likely variable. This is supported by findings that less than 50% of nephrologists have a detailed discussion about transplantation with their patients18 and only 33% of patients are informed of transplant options at the time of dialysis start.19 This variability in dialysis facility–level referral may be contributing to the observed inequities in access to kidney transplantation.9
Nationally, roughly 23% of patients younger than 70 years in a dialysis facility are waitlisted, and 3.4% receive transplants annually.8 Variation in both waitlisting20 and transplantation rates8 among dialysis facilities has been reported even after adjustment for patient factors, with lower transplantation rates among facilities with for-profit status,8,21 higher proportions of black patients8 and patients with limited access to health care,8,20 and fewer staff.8 However, waitlisting and kidney transplantation outcomes among dialysis facilities may not be the ideal quality performance metric for facilities. Lower facility-level transplantation rates may not be attributable to lower waitlisting rates; Ashby et al22 found that, in general, states with lower waitlisting rates had higher transplantation rates. Many factors beyond the dialysis facility may be associated with placement on the deceased donor waiting list, such as whether the patient started or completed the transplant evaluation, was interested in transplantation, or was medically eligible for transplantation.
The need to examine multiple transplant steps is well illustrated by our study, in which we found that factors associated with referral for transplantation were not always the same as those factors associated with waitlisting. For example, we observed racial disparities in waitlisting, as has been reported previously in the United States5,23 and in the Southeast24 and Georgia.25 Without referral data we might have concluded that observed racial disparities in access to waitlisting were attributable to disparities in referral by a dialysis facility. However, we found that black patients had an OR of 1.22 for referral compared with white patients but an OR of 0.77 for waitlisting. Thus, the reasons for racial disparities in waitlisting may be attributable to racial differences in preferences for kidney transplantation,26 starting or completing the evaluation,25 medical eligibility for transplantation,25,27 or referral prior to starting dialysis.28,29 Patients excluded from our study because of referral or transplantation prior to starting dialysis were more likely white and insured. An examination of all patients with kidney disease may find different results.
In addition, we observed that, as age increased, referral for transplantation decreased—but, among those referred, age was not a significant predictor of waitlisting within a year. This may reflect a difference in the perception of the dialysis facility vs transplant center that older age is a contraindication to transplantation. Consistent with prior literature,6,30,31 for both referral and waitlisting, Medicaid, no access to pre-ESRD nephrology care, and higher neighborhood poverty were associated with reduced access to transplantation.
Similarly, several studies have found that for-profit facilities, which may have a financial motivation to keep patients on dialysis, have lower transplantation rates8,19,21 and fewer staff32 compared with nonprofit facilities. In our study, we found that patients receiving dialysis in for-profit facilities had an OR of 1.51 for referral for transplantation within a year but an equal chance of waitlisting compared with patients in nonprofit facilities. The reasons for this are unclear; it is possible that large, for-profit dialysis chains have responded to the criticism of low transplantation rates by increasing referrals; the reasons for why referrals have not translated into higher waitlisting among patients with ESRD in Georgia should be explored in future research.
These findings may have implications for health policy makers, researchers, clinicians, and patients. Low facility-level referral for transplantation, as well as the variability in referral across Georgia facilities, suggests that standardized guidelines are needed for the content and duration of a patient-clinician educational discussion regarding treatment options at start of dialysis. Socioeconomic status factors were significant barriers to both referral and waitlisting in this study; national policies, such as Medicaid expansion, could help to alleviate disparities.9,33 The collection of national transplant referral surveillance data by CMS among all of the more than 5000 US dialysis facilities is needed to identify poorly performing facilities on which to focus quality improvement interventions. A CMS Technical Expert Panel recommended the collection of these data nearly a decade ago,34 yet there is still no national benchmark for transplant referral in the United States. Researchers should continue to develop, test, and implement ragmatic interventions to improve knowledge of transplantation among both clinicians and patients. In Georgia, such interventions could focus on those dialysis facilities with the lowest proportions of patients with ESRD referred for kidney transplantation.10 Efforts should not stop at referral; because we found that factors associated with referral and waitlisting may differ, it is important to highlight possible discrepancies between dialysis facilities’ perceptions of appropriate referrals and the reality of which patients are actually waitlisted and undergo transplantation in practice.
Our study has several strengths, including the collaboration of all transplant centers in Georgia to contribute data for what is to our knowledge the largest regional study of dialysis facility–level referral for kidney transplantation. The use of multilevel modeling techniques and sensitivity analyses ensured the robustness of findings.
However, there are limitations to our study interpretations. Our study was conducted in Georgia, and results may not be generalizable to other states. However, our data emphasize the importance of measuring referral for transplantation to capture its variability both within and between regions. Second, our data source does not capture facility referrals outside of Georgia; however, in a 2012 survey of Georgia dialysis facilities,10 only 1 facility referred patients to transplant centers exclusively outside of Georgia. We linked referral data to the USRDS registry to capture waitlisting and transplant outcomes at any US transplant center. However, the small number of transplants precluded multivariable and stratified analyses of transplantation as an outcome. While the US-RDS registry includes some patient comorbidities, there are likely many unmeasured and unknown factors that influence a patient’s eligibility for transplantation that may vary across dialysis facilities. Although the use of a random-effects model provides estimates of an overall effect while allowing baseline referral to vary at each facility, it is unlikely this approach completely accounts for facility-level variation in patient eligibility. Last, variability in transplant center evaluation could influence the rate of waitlisting and is unaccounted for in our study. Future regional or national studies could examine how transplant center factors influence waitlisting.
Conclusions
In Georgia overall, a limited proportion of patients treated with dialysis were referred for kidney transplant evaluation between 2005 and 2011, but there was substantial variability in referral among facilities. Variables associated with referral were not always associated with waitlisting, suggesting that different factors may account for disparities in referral.
Supplementary Material
Acknowledgments
Funding/Support: This work was supported by National Institute on Minority Health and Health Disparities grant R24MD008077.
Role of the Funder/Sponsor: The study funder/ sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Additional Contributions: We thank the Southeastern Kidney Council and all of the members of the Southeastern Kidney Transplant Coalition for their significant assistance with this work.
Footnotes
Author Contributions: Dr Patzer had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Patzer, Krisher, Gibney, Mulloy, Pastan.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Patzer, Plantinga, Gander, Pastan.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Patzer, Plantinga, Paul, Gander.
Obtained funding: Patzer, Pastan.
Administrative, technical, or material support: Patzer, Gander, Krisher, Sauls, Gibney, Mulloy, Pastan.
Study supervision: Patzer, Krisher, Sauls, Gibney, Mulloy, Pastan.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Pastan reported being a minority shareholder in Fresenius Dialysis (College Park, Georgia). No other disclosures were reported.
Disclaimer: The data reported here have been supplied by the United States Renal Data Service. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as official policy or interpretation of the US government. The collection of transplant referral data from the 3 Georgia transplant centers reported here was performed in part under contract HHSM-500-2013-NW006C. The content of this article does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US government. The authors assume full responsibility for the accuracy and completeness of the ideas presented.
REFERENCES
- 1.US Renal Data System (USRDS) Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2014. USRDS 2014 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. [Google Scholar]
- 2.Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11(10):2093–2109. doi: 10.1111/j.1600-6143.2011.03686.x. [DOI] [PubMed] [Google Scholar]
- 3.Arce CM, Goldstein BA, Mitani AA, Lenihan CR, Winkelmayer WC. Differences in access to kidney transplantation between Hispanic and non-Hispanic whites by geographic location in the United States. Clin J Am Soc Nephrol. 2013;8(12):2149–2157. doi: 10.2215/CJN.01560213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garg PP, Furth SL, Fivush BA, Powe NR. Impact of gender on access to the renal transplant waiting list for pediatric and adult patients. J Am Soc Nephrol. 2000;11(5):958–964. doi: 10.1681/ASN.V115958. [DOI] [PubMed] [Google Scholar]
- 5.Alexander GC, Sehgal AR. Barriers to cadaveric renal transplantation among blacks, women, and the poor. JAMA. 1998;280(13):1148–1152. doi: 10.1001/jama.280.13.1148. [DOI] [PubMed] [Google Scholar]
- 6.Patzer RE, McClellan WM. Influence of race, ethnicity and socioeconomic status on kidney disease. Nat Rev Nephrol. 2012;8(9):533–541. doi: 10.1038/nrneph.2012.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ladin K, Rodrigue JR, Hanto DW. Framing disparities along the continuum of care from chronic kidney disease to transplantation: barriers and interventions. Am J Transplant. 2009;9(4):669–674. doi: 10.1111/j.1600-6143.2009.02561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patzer RE, Plantinga L, Krisher J, Pastan SO. Dialysis facility and network factors associated with low kidney transplantation rates among United States dialysis facilities. Am J Transplant. 2014;14(7):1562–1572. doi: 10.1111/ajt.12749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patzer RE, Pastan SO. Kidney transplant access in the Southeast: view from the bottom. Am J Transplant. 2014;14(7):1499–1505. doi: 10.1111/ajt.12748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patzer RE, Gander J, Sauls L, et al. Southeastern Kidney Transplant Coalition The RaDIANT community study protocol: community-based participatory research for reducing disparities in access to kidney transplantation. BMC Nephrol. 2014;15(1):171. doi: 10.1186/1471-2369-15-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kianda MN, Wissing KM, Broeders NE, et al. Ineligibility for renal transplantation: prevalence, causes and survival in a consecutive cohort of 445 patients. Clin Transplant. 2011;25(4):576–583. doi: 10.1111/j.1399-0012.2010.01317.x. [DOI] [PubMed] [Google Scholar]
- 12.Weng FL, Joffe MM, Feldman HI, Mange KC. Rates of completion of the medical evaluation for renal transplantation. Am J Kidney Dis. 2005;46(4):734–745. doi: 10.1053/j.ajkd.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Bunnapradist S, Danovitch GM. Evaluation of adult kidney transplant candidates. In: Danovitch GM, editor. Handbook of Kidney Transplantation. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. pp. 77–126. [Google Scholar]
- 14.Organ Procurement and Transplantation Network (OPTN) Minority Affairs Committee. [Access date March 10, 2015];Educational Guidance on Patient Referral to Kidney Transplantation. 2014 OPTN website. http://optn.transplant.hrsa.gov/ContentDocuments/Guidance_Kidney_Transplant_Referral.pdf.
- 15.Ayanian JZ, Cleary PD, Keogh JH, Noonan SJ, David-Kasdan JA, Epstein AM. Physicians’ beliefs about racial differences in referral for renal transplantation. Am J Kidney Dis. 2004;43(2):350–357. doi: 10.1053/j.ajkd.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 16.Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation— clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343(21):1537–1544. doi: 10.1056/NEJM200011233432106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services (CMS) [Accessed July 9, 2015];Conditions for Coverage for End-Stage Renal Disease Facilities. 2008 CMS website. https://www.cms.gov/Regulations-and-Guidance/Legislation/CFCsAndCoPs/downloads/ESRDfinalrule0415.pdf. [PubMed]
- 18.Balhara KS, Kucirka LM, Jaar BG, Segev DL. Disparities in provision of transplant education by profit status of the dialysis center. Am J Transplant. 2012;12(11):3104–3110. doi: 10.1111/j.1600-6143.2012.04207.x. [DOI] [PubMed] [Google Scholar]
- 19.Kucirka LM, Grams ME, Balhara KS, Jaar BG, Segev DL. Disparities in provision of transplant information affect access to kidney transplantation. Am J Transplant. 2012;12(2):351–357. doi: 10.1111/j.1600-6143.2011.03865.x. [DOI] [PubMed] [Google Scholar]
- 20.Alexander GC, Sehgal AR. Transplant Task Force of The Renal Network, Inc Variation in access to kidney transplantation across dialysis facilities: using process of care measures for quality improvement. Am J Kidney Dis. 2002;40(4):824–831. doi: 10.1053/ajkd.2002.35695. [DOI] [PubMed] [Google Scholar]
- 21.Garg PP, Frick KD, Diener-West M, Powe NR. Effect of the ownership of dialysis facilities on patients’ survival and referral for transplantation. N Engl J Med. 1999;341(22):1653–1660. doi: 10.1056/NEJM199911253412205. [DOI] [PubMed] [Google Scholar]
- 22.Ashby VB, Kalbfleisch JD, Wolfe RA, Lin MJ, Port FK, Leichtman AB. Geographic variability in access to primary kidney transplantation in the United States, 1996–2005. Am J Transplant. 2007;7(5, pt 2):1412–1423. doi: 10.1111/j.1600-6143.2007.01785.x. [DOI] [PubMed] [Google Scholar]
- 23.Saunders MR, Cagney KA, Ross LF, Alexander GC. Neighborhood poverty, racial composition and renal transplant waitlist. Am J Transplant. 2010;10(8):1912–1917. doi: 10.1111/j.1600-6143.2010.03206.x. [DOI] [PubMed] [Google Scholar]
- 24.Patzer RE, Amaral S, Wasse H, Volkova N, Kleinbaum D, McClellan WM. Neighborhood poverty and racial disparities in kidney transplant waitlisting. J Am Soc Nephrol. 2009;20(6):1333–1340. doi: 10.1681/ASN.2008030335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patzer RE, Perryman JP, Schrager JD, et al. The role of race and poverty on steps to kidney transplantation in the Southeastern United States. Am J Transplant. 2012;12(2):358–368. doi: 10.1111/j.1600-6143.2011.03927.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341(22):1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 27.Waterman AD, Peipert JD, Hyland SS, McCabe MS, Schenk EA, Liu J. Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clin J Am Soc Nephrol. 2013;8(6):995–1002. doi: 10.2215/CJN.08880812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keith D, Ashby VB, Port FK, Leichtman AB. Insurance type and minority status associated with large disparities in prelisting dialysis among candidates for kidney transplantation. Clin J Am Soc Nephrol. 2008;3(2):463–470. doi: 10.2215/CJN.02220507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kasiske BL, Snyder JJ, Matas AJ, Ellison MD, Gill JS, Kausz AT. Preemptive kidney transplantation: the advantage and the advantaged. J Am Soc Nephrol. 2002;13(5):1358–1364. doi: 10.1097/01.asn.0000013295.11876.c9. [DOI] [PubMed] [Google Scholar]
- 30.Kasiske BL, London W, Ellison MD. Race and socioeconomic factors influencing early placement on the kidney transplant waiting list. J Am Soc Nephrol. 1998;9(11):2142–2147. doi: 10.1681/ASN.V9112142. [DOI] [PubMed] [Google Scholar]
- 31.Perneger TV, Whelton PK, Klag MJ. Race and end-stage renal disease: socioeconomic status and access to health care as mediating factors. Arch Intern Med. 1995;155(11):1201–1208. [PubMed] [Google Scholar]
- 32.Yoder LA, Xin W, Norris KC, Yan G. Patient care staffing levels, facility characteristics in U.S hemodialysis facilities. Am J Kidney Dis. 2013;62(6):1130–1140. doi: 10.1053/j.ajkd.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Srinivas TR. Kidney transplant access in the Southeastern United States: the need for a top-down transformation. Am J Transplant. 2014;14(7):1506–1511. doi: 10.1111/ajt.12747. [DOI] [PubMed] [Google Scholar]
- 34.Sehgal AR, Leon J, Stark S Renal Network. [Accessed February 2, 2015];ESRD Special Study: Developing Dialysis Facility–Specific Kidney Transplant Referral Clinical Performance Measures. 2005 Jun 30; Renal Network website. http://www.therenalnetwork.org/qi/resources/TransTEPfinalrpt805.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.