Abstract
The purpose of study is to analyze the feasibility, utility, and advantage of using alternate methods of anesthesia in patients undergoing surgeries for minor anorectal ailments. A total of 60 cases with proctoscopic findings of low fistula in ano, fissure in ano, hemorrhoids grade II and grade III, were operated between October 2005 and April 2007. Patients were randomized and divided into two groups of 30 each. Group A underwent surgeries under local anesthesia while group B under spinal anesthesia. There was no significant difference in operating time and patient satisfaction score. Postoperative urinary retention was significantly higher in group B—30 % patients in group B versus 6.7 % in group A. Hospital stay was significantly decreased in group A, with 93.3 % patients discharged on day 1 as compared to 70 % in group B (P = 0.02). Surgeries under local anesthesia were beneficial in terms of hospital stay and postoperative complications like urinary retention. No significant difference in patient satisfaction was observed. Hence, compared to spinal anesthesia, local anesthesia is a safe and advantageous technique in performing minor anorectal surgeries.
Keywords: Anorectal, Hemorrhoids, Minor anorectal surgery, Local anesthesia
Introduction
Anorectal surgeries constitute one of the most frequent surgeries performed by the surgeons. Although usually considered minor surgeries, the associated morbidity of these procedures can be quite debilitating. Traditionally these surgeries have been conducted under spinal anesthesia. It entails numerous postoperative issues such as long postoperative hospital stay, urinary retention, hypotension, and postspinal headache which are best avoided in the geriatric age groups and the patients suffering from co morbid conditions. (Figs. 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, and 12; Tables 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 and 14)
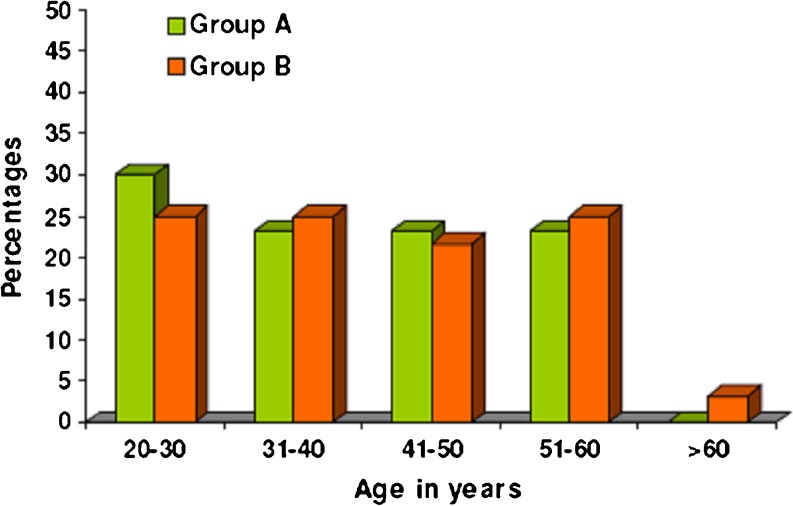
Fig. 1.
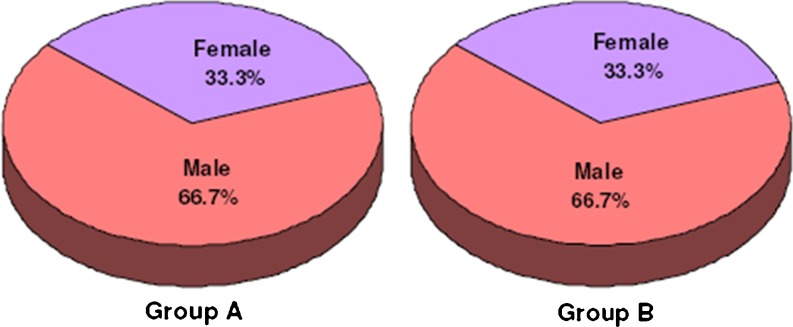
Fig. 2.
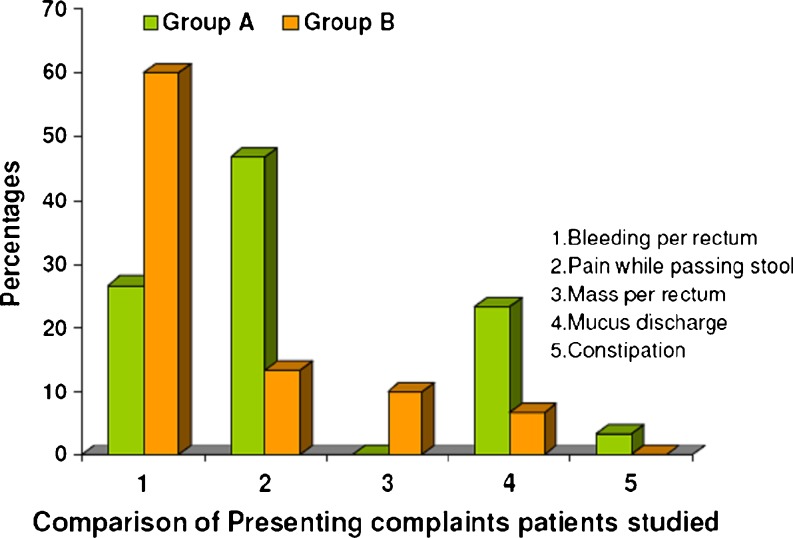
Fig. 3.
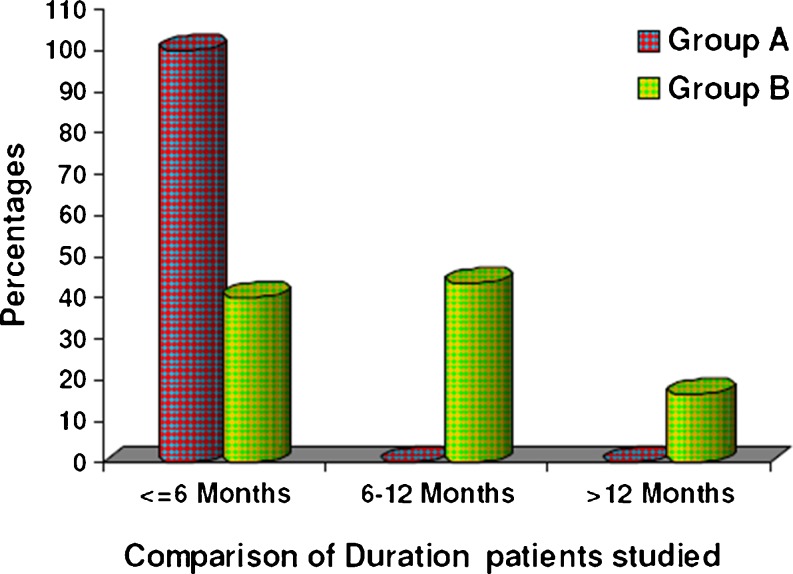
Fig. 4.
Fig. 5.
Fig. 6.
Fig. 7.
Fig. 8.
Fig. 9.
Fig. 10.
Fig. 11.
Fig. 12.
Table 1.
Results
| Results | ||||||
|---|---|---|---|---|---|---|
| Age in years | Group A | Group B | Combined | |||
| No | % | No | % | No | % | |
| 20–30 | 9 | 30.0 | 6 | 20.0 | 15 | 25.0 |
| 31–40 | 7 | 23.3 | 8 | 26.7 | 15 | 25.0 |
| 41–50 | 7 | 23.3 | 6 | 20.0 | 13 | 21.7 |
| 51–60 | 7 | 23.3 | 8 | 26.7 | 15 | 25.0 |
| >60 | – | – | 2 | 6.7 | 2 | 3.3 |
| Total | 30 | 100.0 | 30 | 100.0 | 60 | 100.0 |
| Mean±SD | 39.53±11.71 | 43.17±12.70 | 41.35±12.25 | |||
Table 2.
Comparison of gender of patients studied
| Gender | Group A | Group B | Combined | |||
|---|---|---|---|---|---|---|
| No | % | No | % | No | % | |
| Male | 20 | 66.7 | 20. | 66.7 | 40 | 66.7 |
| Female | 10 | 33.3 | 10 | 33.3 | 20 | 33.3 |
| Total | 30 | 100.0 | 30 | 100.0 | 60 | 100.0 |
Table 3.
Comparison of presenting complaints patients studied
| Presenting complaints | Group A (n = 30) | Group B (n = 30) | ||
|---|---|---|---|---|
| No | % | No | % | |
| Bleeding per rectum | 8 | 26.7 | 18 | 60.0 |
| Pain while passing stool | 14. | 46.7 | 4 | 13.3 |
| Mass per rectum | – | – | 3 | 10.0 |
| Mucus Discharge | 7 | 23.3 | 2 | 6.7 |
| Constipation | 1 | 3.3 | – | – |
Table 4.
Comparison of duration patients studied
| Duration | Group A (n = 30) | Group B (n = 30) | ||
|---|---|---|---|---|
| No | % | No | % | |
| ≤6 months | 30 | 100.0 | 12 | 40.0 |
| 6–12 months | – | – | 13 | 43.3 |
| >12 months | – | – | 5 | 16.7 |
Table 5.
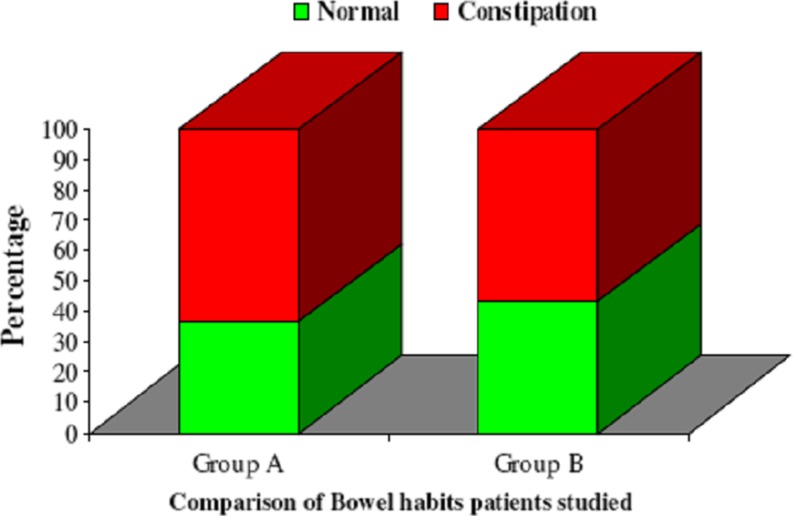
Comparison of bowel habits patients studied
| Bowel habits | Group A (n = 30) | Group B (n = 30) | ||
|---|---|---|---|---|
| No | % | No | % | |
| Normal | 11 | 36.7 | 13 | 43.3 |
| Constipation | 19 | 63.3 | 17 | 56.7 |
Table 6.
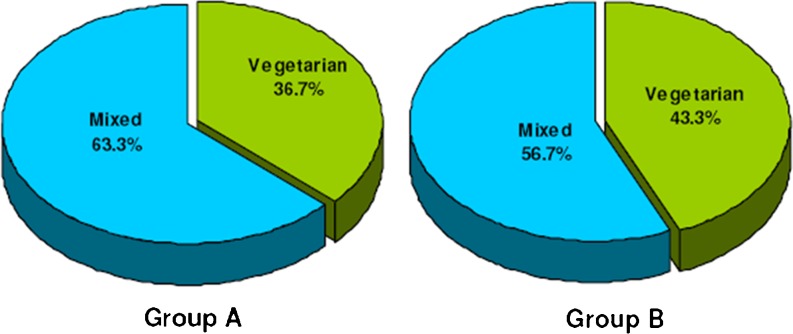
Comparison of diet patients studied
| Diet | Group A (n = 30) | Group B (n = 30) | ||
|---|---|---|---|---|
| No | % | No | % | |
| Vegetarian | 11 | 36.7 | 13 | 43.3 |
| Mixed | 19 | 63.3 | 17 | 56.7 |
Table 7.
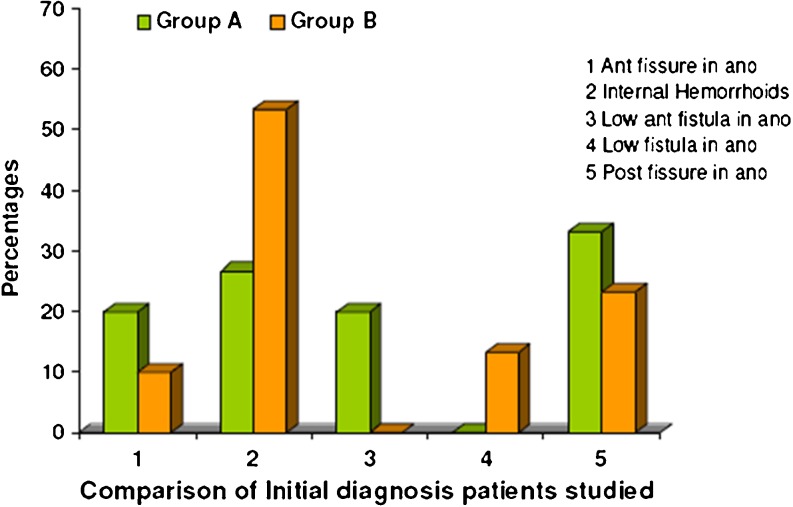
Comparison of initial diagnosis patients studied
| Initial diagnosis | Group A(n = 30) | Group B (n = 30) | ||
|---|---|---|---|---|
| No | % | No | % | |
| Ant fissure in ano | 6 | 20.0 | 3 | 10.0 |
| Internal Hemorrhoids | 8 | 26.7 | 16 | 53.3 |
| Low ant fistula in ano | 6 | 20.0 | – | – |
| Low fistula in ano | – | – | 4 | 13.3 |
| Post fissure in ano | 10 | 33.3 | 7 | 23.3 |
Table 8.
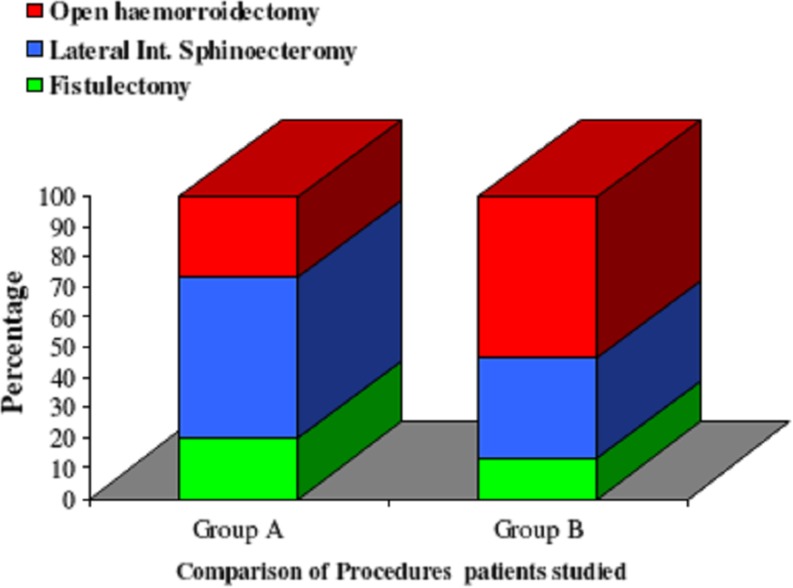
Comparison of procedures patients studied
| Procedures | Group A (n = 30) | Group B (n = 30) | ||
|---|---|---|---|---|
| No | % | No | % | |
| Fistulectomy | 6 | 20.0 | 4 | 13.3 |
| Lateral Int Sphincoecteromy | 16 | 53.3 | 10 | 33.3 |
| Open haemorroidectomy | 8 | 26.7 | 16 | 53.3 |
Table 9.
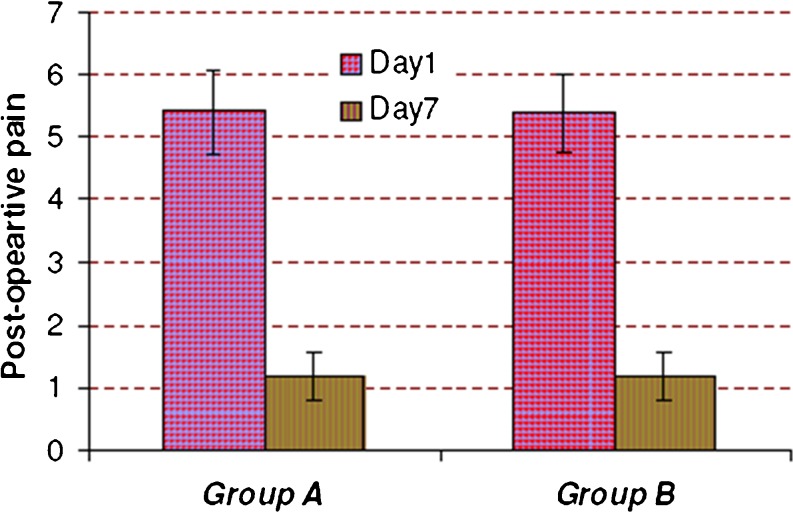
Comparison of postoperative pain in two groups of patients
| Post-operative pain | Group A | Group B | P value |
|---|---|---|---|
| Day 1 | 5.40 ± 0.68 | 5.37 ± 0.62 | 0.841 |
| Day 7 | 1.17 ± 0.38 | 1.17 ± 0.38 | 0.999 |
| P value | <0.001** | <0.001** | – |
Table 10.
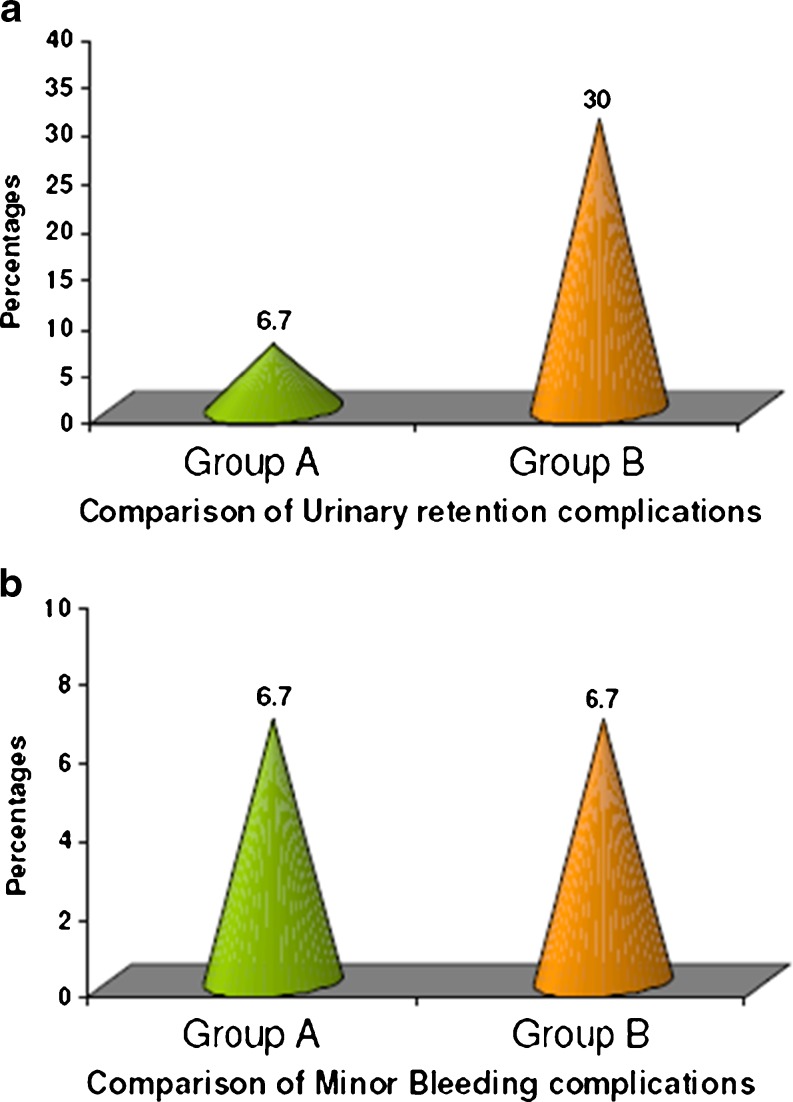
Comparison of post operative complications
| Post-op complications | Group A (n = 30) | Group B (n = 30) | P value | ||
|---|---|---|---|---|---|
| No | % | No | % | ||
| Fecal urgency and incontinence | – | – | – | – | – |
| Urinary Retention | 2 | 6.7 | 9 | 30.0 | 0.020* |
| Minor Bleeding | 2 | 6.7 | 2 | 6.7 | 1.000 |
| Mortality | – | – | – | – | – |
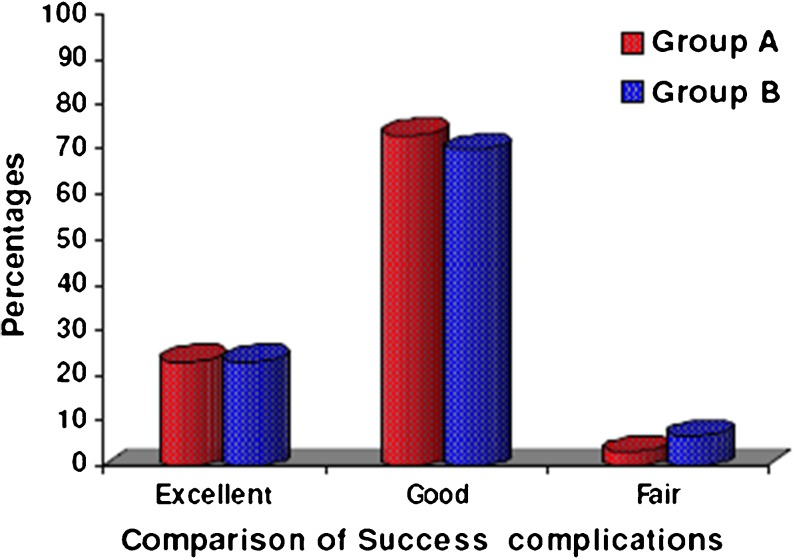
Table 11.
Comparison of success rates
| Success | Group A | Group B | P value | ||
|---|---|---|---|---|---|
| No | % | No | % | ||
| Excellent | 7 | 23.3 | 7 | 23.3 | 1.000 |
| Good | 22 | 73.3 | 21 | 70.0 | 0.774 |
| Fair | 1 | 3.3 | 2 | 6.7 | 1.000 |
Table 12.
Complications at 3 months and 6 month follow up
| Follow up status | Group A | Group B |
|---|---|---|
| At 3 months | Nil | Nil |
| At 6 months | Nil | Nil |
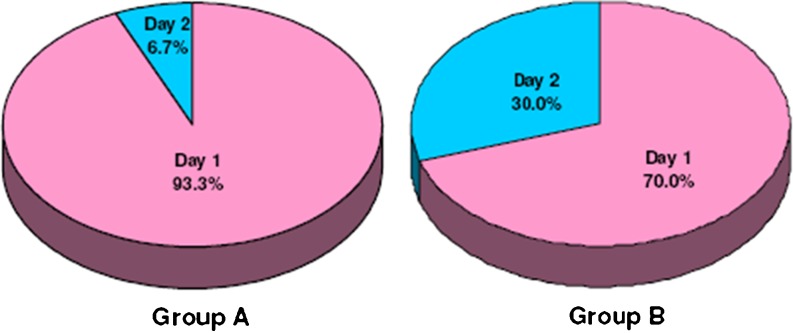
Table 13.
Comparison of discharge
| Discharge | Group A (n = 30) | Group B (n = 30) |
|---|---|---|
| Day 1 | 28(93.3 %) | 21 (70.0 %) |
| Day 2 | 2 (6.7 %) | 9(30.0 %) |
| Inference | Discharge at day 2 is significantly more in Group B with P = 0.020* | |
Table 14.
Comparison of patient satisfaction
| Patient satisfaction | Group A (n = 30) | Group B (n = 30) |
|---|---|---|
| Range | 9–10 | 9–10 |
| Mean ± SD | 9.33 ± 0.48 | 9.36±0.47 |
| Inference | Patient satisfaction is statistically similar between two groups with P = 0.828 | |
Until recently surgeons were hesitant to perform anal and rectal procedures in an ambulatory setting because of fear of postoperative pain and retention of urine. This attitude has slowly changed. Due to increase in experience and confidence, more than 90 % of anorectal surgeries can be done successfully on an ambulatory basis [1]. Hence, the current trend is toward conducting these surgeries under the local anesthesia. This study was aimed at comparing the advantages and disadvantages of conducting minor anorectal surgeries under local anesthesia versus spinal anesthesia.
Objectives of Study
To assess the complications with anorectal surgeries conducted under local anesthesia.
To assess the average duration of hospital stay and cost-effectiveness after anorectal surgeries under local anesthesia.
Materials and Methods
A total of 60 cases with symptoms of bleeding per rectum, mass per rectum, pain in the anal region and constipation and proctoscopic findings of low fistula in ano, fissure in ano, hemorrhoids grade II and grade III, admitted to the surgical ward of M.S. Ramaiah Teaching Hospital Bangalore, between October 2005 and April 2007, were randomized and divided into two groups of 30 patients each—group A and group B. Group A patients included random set of 30 patients who underwent minor anorectal surgeries under local anesthesia. Group B patients included random set of 30 patients who underwent minor anorectal surgeries under spinal anesthesia.
Type of Anesthesia
The procedure was performed with the patient in jack-knife/lithotomy position. Patients were monitored with a pulse oximeter. Preoperatively bowel preparation, antibiotics were given. Local anesthesia (pudendal and perianal block using 2 % lignocaine or 0.5 % bupivacaine) was injected with a 25 G needle, infiltrating the skin, intersphincteric space, internal anal sphincter, and submucosa on the left and right sides, as well as the bed of the fissure in group A and spinal anesthesia in group B. Spinal anesthesia was given using bupivacaine at L2-L3 space. Postoperative period was monitored carefully. All the patients in both the groups received IV tramadol hydrochloride two doses and then oral tramadol hydrochloride twice a day for 5 days. Details regarding patients’ complaints, duration of incapacity to work, and the complications were recorded.
The patients were advised to come for follow-up at 1 week, 3 months, and 6 months. They were advised to come earlier in case they noticed any complications. The results are tabulated mainly stressing on following points such as age and sex distribution, probable causative factor, degree of hemorrhoids, low anal fistula, and fissure in ano complications in each technique.
Results
There was no significant difference in operating time. Urinary retention was significantly higher in the group receiving spinal anesthesia (group B). About 30 % patients in group B and 6.7 % in group A had postoperative retention. The mean patient satisfaction score was 9.31 (0= poor satisfaction, 10= excellent satisfaction). Hospital stay was significantly decreased in group A (P = 0.02). About 93.3 % patients in this group were discharged on day 1, whereas 70 % patients in group B were discharged on day 1. There was no mortality, incontinence, fecal urgency, or persistent pain.
Discussion
Minor anorectal ailments such as hemorrhoids, fissure in ano and fistula in ano conventional hemorrhoidectomy involve excision of the prolapsed hemorrhoids and are usually associated with severe pain [2]. There is a wide variation in practice regarding the hospital stay following conventional hemorrhoidectomy. This depends on economic constraints, the culture of the population, and the home environment of patients. Hospital stay following conventional hemorrhoidectomy can range from a few hours after the operation to a mean stay of more than 6 days [3]. Despite ambulatory surgery for conventional hemorrhoidectomy being practiced in some centers, many patients prefer to be admitted to hospital if possible [3]. This possibly reflects concern regarding the management of severe pain, the need for wound care, and the fear of complications following hemorrhoidectomy.
The control of posthemorrhoidectomy pain has always been the main concern for the surgeon, and tremendous efforts have been made to reduce the pain in order to render hemorrhoidectomy possible as an ambulatory procedure. There have been attempts to modify the surgical technique, such as using diathermy [4], a harmonic scalpel [5], or Ligasure [6] (Valleylab, Boulder, US) for the excision of hemorrhoids. Surgical or medical means to reduce the sphincter muscle spasm have also been tried to reduce postoperative pain [7–9]. Different forms of analgesia and anesthesia have also been used [10, 11]. Furthermore, postoperative antibiotics to reduce infection have been shown to be effective in reducing postoperative pain.
Despite these approaches, the primary cause of pain—the trauma to the pain-sensitive perianal skin and the anal epithelium during excision of hemorrhoids—is still present and pain reduction is usually limited. Hemorrhoids are now regarded as cushions of fibrous and vascular tissue at the anal canal that become symptomatic when prolapse occurs [12].
The absence of a wound and subsequent potential infection at the perianal area helps to reduce postoperative pain following a stapled hemorrhoidectomy [13]. Moreover, wound care is not necessary, as the staple line is inside the rectum.
In this study the mean age of patients was 45.97 ± 16.46 years of which male patients constituted 65.7 % of the study and female patients constituted 34.3 %. Mean duration of symptoms was 11.4 %. The main presenting complaint in this was bleeding per rectum which constituted 65.7 % and the least presenting was mass per rectum which constituted 22.9 %. The patients in this study consumed mixed diet and constituted 82.9 % and 57.1 % presented with constipation. The patients in this study had grade II 40 %, grade III 57 %, and grade IV 2.9 %, respectively. Majority of patients had internal hemorrhoids (77.8 %), and combination of internal and external hemorrhoids was 11 %.
In this series, there were two cases of minor bleeding and urinary retention. These patients were conservatively treated without blood transfusion or further surgery. They were kept for observation and discharged on the next day. Complications following stapled hemorrhoidectomy are mostly urological. Urinary retention is one of the most important reasons for hospital stay and re-admission following hemorrhoidectomy [13, 14]. Urinary retention occurred in 5.7 % of patients in this series and no difference was noted between day-surgery and in-patient groups. This rate is relatively low when compared with other series involving conventional hemorrhoidectomy. Zaheer et al reported urinary retention in 16 % of patients following anorectal surgery and 34 % of patients following hemorrhoidectomy. These authors suggested that there was a correlation between urinary retention and the degree of pain. In this study the postoperative pain on day 1 ranges from 4/10 to 7/10. These results are similar with the study of Law et al. Complications and analgesic requirements are similar to the study conducted by Amosi et al. In this study subjective success was excellent in 25.7 % and good in 68.6 %. In this study, 94.3 % of patient had been discharged on the same day and 2 (5.7 %) patients on the second day. Subjective success following surgery was excellent in 25.7 %, good in 68.6 %, and average in 5.7 %. These patients were followed up for 12 months and no complications were noted.
Conclusion
This study was aimed to analyze the feasibility and utility of using the alternate method of anesthesia in patients undergoing surgeries for minor anorectal ailments. The results of this study were in accord with the previous studies. The use of local anesthesia in these surgeries was found to be beneficial in terms of hospital stay [1, 15] and postoperative complications such as urinary retention [1]. The technique had no significant difference in postoperative pain, perioperative complications, and patient satisfaction. Hence, it can be concluded that local anesthesia is a safe and advantageous technique in performing minor anorectal surgeries.
Summary
Minor anorectal disease constitutes quite large percentage of cases in the surgical outpatient department (OPD). This study helps to know the effectiveness of local anesthesia for daycare surgery [15]. It is a randomized comparative study. A total of 60 patients randomly selected into group A (local anesthesia) and group B (spinal anesthesia) underwent minor anorectal surgeries. Patients’ detailed history, physical examination, operative details, postoperative complications, length of hospital stay, pain scores, analgesic requirements, and patient satisfaction scores were collected. There were 20 female and 40 male patients in the study. The mean age was 39.53 and 43.17 years in group A and group B, respectively. The main presenting symptom was bleeding in 26.7 % and 60 %, mucous discharge in 23.3 % and 6.7 %, and pain 46.7 % and 13.3 % in group A and group B, respectively. Out of the study group, 60 % patients were on nonvegetarian diet, which shows a significant increase in patients with low-fiber diet. This is further emphasized by the fact that 60 % of the patients suffer from constipation. There was no significant difference in the operating time. Urinary retention was significantly higher in the group receiving spinal anesthesia (group B); 30 % patients in group B and 6.7 % in group A had postoperative retention. The postoperative pain score was measured by a scale from 0 to 10 (0= no pain, 10= severe pain). The mean patient satisfaction score was 9.31 (0= poor satisfaction, 10= excellent satisfaction). Data about the number of doses of oral/parenteral analgesics were recorded. Patient subjective success was assessed. Hospital stay was significantly decreased in group A (P = 0.02). In group A 93.3 % patients were discharged on day 1, whereas 70 % of group B were discharged on day 1.
There was no mortality, incontinence, fecal urgency, and persistent pain. The current study was aimed to analyze the feasibility and utility of using alternate method of anesthesia in patients undergoing surgeries for minor anorectal ailments. The results of this study were in accord with the previous studies. The use of local anesthesia in these surgeries was found to be beneficial in terms of hospital stay and postoperative complications such as urinary retention [1, 15]. The technique had no significant difference in postoperative pain, perioperative complications, and patient satisfaction. Hence, it can be concluded that local anesthesia is a safe and advantageous technique in performing minor anorectal surgeries.
Contributor Information
Srikant V. Kulkarni, Email: shrikulkarni58@gmail.com
Prateek Agarwal, Phone: +91-948-0491966, Email: prateek.agl@gmail.com.
References
- 1.Griffin JF (1989) Anaesthesia for ambulatory anorectal surgery. Current Surgical Therapy-3. Philidelphia: B C Decker Inc, London.
- 2.Corman M. Colon and rectal surgery. 4. USA: Lippincott-Raven, Publications; 1998. [Google Scholar]
- 3.Gordon PH, Gordon PH, Nivatvongs S. Principles and practice of surgery for the colon, rectum and anus. 2. London: Quality Medical Publishing Publications; 1999. [Google Scholar]
- 4.Jackson CC, Robertson E. Etiology of hemorrhoids. Dis Colon Rectum. 1965;8:185–189. doi: 10.1007/BF02617086. [DOI] [PubMed] [Google Scholar]
- 5.Rangabhashyam N, Manohar V. Etiopathogenesis of hemorrhoids in Madras. Indian J Surg. 1978;40(6):305. [Google Scholar]
- 6.Haas PA, Fox TA, Jr, Haas GP. The pathogenesis of hemorrhoids. Dis Colon Rectum. 1984;27:442–450. doi: 10.1007/BF02555533. [DOI] [PubMed] [Google Scholar]
- 7.Keighley MRB, Williams NS. Surgery of the anus, rectum and colon. London: WB Saunders Co. Ltd; 1993. [Google Scholar]
- 8.Jacobs OM, Rubrick MP, Onstad GR. The relationship of hemorrhoids to portal hypertension. Dis Colon Rectum. 1980;23:567. doi: 10.1007/BF02988998. [DOI] [PubMed] [Google Scholar]
- 9.Hancock BO, Smith K. The internal sphincter & Lord’s procedure for hemorrhoids. Br J Surg. 1975;62:833–836. doi: 10.1002/bjs.1800621021. [DOI] [PubMed] [Google Scholar]
- 10.Dodi G, Pirone E, Cavallari F. Sclerotherapy & elastic band ligation of hemorrhoids. Ann Ital Chir. 1995;66(6):769–773. [PubMed] [Google Scholar]
- 11.Park AG. The surgical treatment of hemorrhoids. Br J Surg. 1956;180:337–351. doi: 10.1002/bjs.18004318002. [DOI] [PubMed] [Google Scholar]
- 12.Pescatori M. Closed hemorrhoidectomy. Ann Ital Chir. 1995;66(6):787–790. [PubMed] [Google Scholar]
- 13.Medwell SJ, Friend WG. Outpatient anorectal surgery. Dis Colon Rectum. 1979;22:480–482. doi: 10.1007/BF02586936. [DOI] [PubMed] [Google Scholar]
- 14.Houston GD, Russel SR. Thrombosed external hemorrhoids: outcome after conservative or surgical management. Dis Colon Rectum. 2004;47:1493–1498. doi: 10.1007/s10350-004-0607-y. [DOI] [PubMed] [Google Scholar]
- 15.Hoff SD, Bailey HR, Butts DR, Max E, Smith KW, Zamora LF, Skakun GB. Ambulatory surgical haemorrhoidectomy—a solution to postoperative urinary retention? Dis Colon Rectum. 1994;37:1242–1244. doi: 10.1007/BF02257789. [DOI] [PubMed] [Google Scholar]