Abstract
A 68-year-old woman was referred to our hospital for a lung nodule identified on chest radiography. Computed tomography (CT) showed a 10-mm calcified nodule in the left thoracic cavity. On follow-up CT, the nodule was found in a different location within the left thoracic cavity. Thoracoscopy was performed under local anesthesia, removing a pearl-like pleural stone. Thoracolithiasis was therefore diagnosed without any complications. To the best of our knowledge, this is the first report on thoracoscopy under local anesthesia for the diagnosis of thoracolithiasis. When thoracolithiasis is suspected, thoracoscopy under local anesthesia is minimally invasive and useful, and could be considered as an option for definite diagnosis.
Keywords: Intrathoracic calculus, local anesthesia, lung nodule, thoracolithiasis, thoracoscopy
Introduction
Thoracolithiasis, also known as intrathoracic calculus, is a rare disease with a frequency less than 0.1% (11 of 12,835 individuals) [1]. To the best of our knowledge, only 25 cases have been reported in the literature. Exploratory thoracotomy or thoracoscopy under general anesthesia is usually necessary for the definitive diagnosis of thoracolithiasis. This is the first report to describe thoracolithiasis diagnosed by thoracoscopy under local anesthesia.
Case Report
A 68-year-old woman was referred to our hospital after a pulmonary nodule was found on a routine chest radiograph during a health checkup. She had been healthy and no noteworthy findings were apparent on physical examination or blood tests. Chest radiograph showed a well-defined nodule of 10 mm in diameter in the left lower lung field (Fig. 1A). Chest computed tomography (CT) revealed a well-defined subpleural nodule of 10 mm in diameter in the left thoracic cavity (Fig. 1B). The patient was carefully observed for 6 months. On follow-up CT, the nodule was found in a different location within the left thoracic cavity (Fig. 1C).
Figure 1.
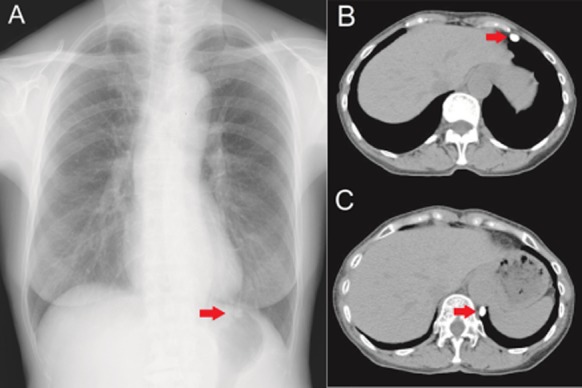
(A) Chest radiograph shows a well-defined oval nodule (arrow) in the left lower lung field. (B) Chest computed tomography (CT) at the initial visit shows a well-defined, oval, calcified mass (arrow) on the ventral side of the left thoracic cavity. (C) Follow-up CT shows migration of the calcified mass (arrow) on the dorsal side of the left thoracic cavity.
The homogeneously calcified nodule had not changed in size or appearance, but migration of the nodule was recognized on follow-up CT. We suspected that the nodule represented thoracolithiasis, which was not attached to the pleura. Because the nodule seemed likely to be easily approached by semi-rigid thoracoscope, thoracoscopy under local anesthesia was performed for definitive diagnosis. A pearl-like calcified nodule was readily removed using basket-type grasping forceps. The extracted material was 10 × 10 mm in size, with a milky white, glossy surface (Fig. 2). The cross-section showed a rough surface with yellowish brown coloration. Pathological examination revealed adipose and fatty necrotic tissue surrounded by hyalinized fibrous tissue. No epithelial component was evident. Thoracolithiasis was diagnosed and the patient was discharged 2 days after the thoracoscopic procedure without any complications.
Figure 2.
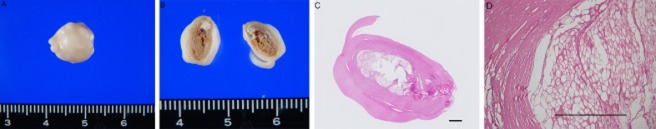
(A) Extirpated material, 10 × 10 mm in size. The surface appears milky white and glossy. (B) Cross-section of the material shows a rough surface, yellowish brown in color. (C, D) Histological examination indicates adipose and fatty necrotic tissue surrounded by hyalinized fibrous tissue (hematoxylin and eosin stain). Scale bar = 1 mm.
Discussion
Thoracolithiasis is a rare condition in which one or more free bodies with or without calcification exist in the thoracic cavity without any previous trauma, intervention, or pleurisy [2]. Most cases have been found incidentally on X-ray, CT, or at the time of surgery. The incidence in the general population is quite low (<0.01%) and nodules range in size from 5 to 15 mm (mean, 8 mm) [1].
The exact etiology of thoracolithiasis remains unclear, and various explanations have been proposed. These include pericardial or pleural fat necrosis [3], pericardial or pleural fat tearing off in the pleural cavity [2], old tuberculous foci, or an aggregation of macrophages phagocytosing dust [4] that becomes round and polished after a long period surrounded by structures that move continuously with breathing. Most pleural stones have been described on the left side (75%), supporting the necrotic pericardial fat theory [5]. We speculated that the stone in the present case could have been formed by necrotic pericardial fat because the stone consisted of adipose and fatty necrotic tissue surrounded by hyalinized fibrous tissue without an epithelial component, and because initial chest CT showed the nodule at the boundary of the pericardial fat and diaphragm.
Almost all patients with thoracolithiasis are asymptomatic, and non-specific symptoms such as cough and sputum correlate poorly with thoracolithiasis. Transthoracic or endobronchial biopsy is sometimes performed for definitive diagnosis, but often fails to obtain a diagnosis because it is difficult to get a specimen. Definitive diagnosis usually requires surgical removal of the stone irrespective of the distinctive radiological findings. In the recent literature, video-assisted thoracic surgery (VATS) has been used as a minimally invasive surgery for diagnostic and therapeutic purposes [5].
Thoracoscopy under local anesthesia has recently been established as an indispensable technique for the diagnosis and treatment of respiratory diseases. Although VATS is usually performed under general anesthesia by thoracic surgeons, thoracoscopy under local anesthesia could be performed by chest physicians if the target is limited to pleural diseases and the thoracic cavity. Thoracoscopy under local anesthesia would represent a less invasive surgery than VATS under general anesthesia.
In this case, we strongly suspected thoracolithiasis because of the radiological findings and migration of the nodule. Because the nodule was located in the peripheral portion of the lung and it migrated, we thought that thoracoscopy under local anesthesia might be sufficient for its removal.
In conclusion, we encountered a case of thoracolithiasis in which thoracoscopy under local anesthesia proved minimally invasive and useful. When thoracolithiasis is suspected, particularly with appearance of the lesion at different locations on CT due to mobility, thoracoscopy under local anesthesia represents a valid option for definitive diagnosis.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
References
- Kinoshita F, Saida Y, Okajima Y, et al. Thoracolithiasis: 11 cases with a calcified intrapleural loose body. J. Thorac. Imaging. 2010;25:64–67. doi: 10.1097/RTI.0b013e3181a4ba03. [DOI] [PubMed] [Google Scholar]
- Kosaka S, Kondo N, Sakaguchi H, et al. Thoracolithiasis. Jpn. J. Thorac. Cardiovasc. Surg. 2000;48:318–321. doi: 10.1007/BF03218148. [DOI] [PubMed] [Google Scholar]
- Pineda V, Caceres J, Andreu J, et al. Epipericardial fat necrosis: radiologic diagnosis and follow-up. AJR Am. J. Roentgenol. 2005;185:1234–1236. doi: 10.2214/AJR.04.1310. [DOI] [PubMed] [Google Scholar]
- Iwasaki T, Nakagawa K, Katsura H, et al. Surgically removed thoracolithiasis: report of two cases. Ann. Thorac. Cardiovasc. Surg. 2006;12:279–282. [PubMed] [Google Scholar]
- Bolca C, Trahan S. Frechette E. Intrapleural thoracolithiasis: a rare intrathoracic pearl-like lesion. Thorac. Cardiovasc. Surg. 2011;59:445–446. doi: 10.1055/s-0030-1270757. [DOI] [PubMed] [Google Scholar]


