This qualitative study showed that multiple factors contribute to the challenge of cervical cancer screening and treatment in Tanzania and highlighted systematic developments aimed at expanding services. The themes that emerged from the results may help inform programs that plan to improve screening and treatment in Tanzania and potentially in other areas with high burdens of cervical cancer.
Keywords: Cervical cancer, Health services research, Service delivery, Screening and treatment
Abstract
Tanzania has the highest burden of cervical cancer in East Africa. This study aims to identify perceived barriers and facilitators that influence scale-up of regional and population-level cervical cancer screening and treatment programs in Tanzania. Convenience sampling was used to select participants for this qualitative study among 35 key informants. Twenty-eight stakeholders from public-sector health facilities, academia, government, and nongovernmental organizations completed in-depth interviews, and a seven-member municipal health management team participated in a focus group discussion. The investigation identified themes related to the infrastructure of health services for cervical cancer prevention, service delivery, political will, and sociocultural influences on screening and treatment. Decentralizing service delivery, improving access to screening and treatment, increasing the number of trained health workers, and garnering political will were perceived as key facilitators for enhancing and initiating screening and treatment services. In conclusion, participants perceived that system-level structural factors should be addressed to expand regional and population-level service delivery of screening and treatment.
Implications for Practice:
Tanzanian women have a high burden of cervical cancer. Understanding the perceived structural factors that may influence screening coverage for cervical cancer and availability of treatment may be beneficial for program scale-up. This study showed that multiple factors contribute to the challenge of cervical cancer screening and treatment in Tanzania. In addition, it highlighted systematic developments aimed at expanding services. This study is important because the themes that emerged from the results may help inform programs that plan to improve screening and treatment in Tanzania and potentially in other areas with high burdens of cervical cancer.
Introduction
In most nations in sub-Saharan Africa, cervical cancer remains the most common cancer among women [1]. Although progress has been made in cervical cancer prevention over the past 40 years, most African countries have not yet introduced comprehensive screening and treatment programs [2, 3]. Competing health needs, inadequate funding, social disadvantages, and low priority for cancer control and prevention vis-à-vis other health care programs are factors limiting programs at the population level [3–6]. Country-specific findings on program successes and challenges are necessary for development of initiatives aimed at increasing delivery of services in countries with limited screening coverage and high rates of cervical cancer [7]. For program development, country-specific findings provide insight into likely challenges that may be associated with implementation, facilitators of screening and treatment, lessons learned in service delivery, and sustainability of services [7–12].
In Africa, approximately 40% of new cases of cervical cancer occur in East Africa. Tanzanian women bear the highest burden of cervical cancer in this region, with age-adjusted standardized incidence rates of 50.6 cases per 100,000 [1]. In response to the high burden of cervical cancer, a variety of pilot projects, regional outreach clinics, and research studies on cervical cancer have been conducted in Tanzania [13]. In 2011, the Tanzania Ministry of Health and Social Welfare developed national guidelines for delivery of cervical cancer control and prevention. Tanzania is one of the few African countries participating in studies of human papillomavirus vaccine safety and immunogenicity [13, 14]. In 2010, more than 10,000 women were screened in an evaluation of the efficacy of visual inspection based “screen-and-treat” protocols for prevention of cervical cancer [15]. Visual inspection approaches (most prominently, visual inspection with acetic acid [VIA]) can be linked to immediate treatment of precancerous lesions with cryotherapy for eligible women. Despite challenges and limitations (e.g., underdetection and overtreatment) [16], VIA-based single-visit screen-and-treat approaches have been shown to be safe, accurate, and feasible for scaling up cervical cancer screening and treatment services in low-resource settings [17–19].
Notwithstanding the limited country-specific data on cervical cancer prevention programs in Tanzania and the East African region, it is important to understand the spectrum of challenges that influence enhancement of service delivery and expansion of screening coverage. Despite various demonstration projects and research initiatives for cervical cancer prevention, there has been limited examination in the literature of perceived structural and societal factors that constrain implementation of population-level programs and the facilitators that have led to participation in such large-scale programs. The purpose of this qualitative study was to fill in this gap in evidence by identifying perceived structural barriers and facilitators that may influence broadening of regional and population-level cervical cancer screening and treatment programs in Tanzania.
Methods
Study Design
This study consisted of face-to-face interviews and one focus group discussion. Qualitative forms of inquiry were selected to elicit data on participants’ knowledge, perceptions, and recommendations on cervical cancer screening and treatment in Tanzania. The institutional review board at the University of Alabama at Birmingham and the National Institute for Medical Research in Tanzania reviewed and approved the study protocol.
Participants
The total study sample was composed of 35 participants and key informants. In-depth interviews were conducted with 28 stakeholders from public-sector health facilities, academia, government, and nongovernmental organizations (NGOs). In addition, the community health management team and administrative clinicians (n = 7) from a municipal district in Dar es Salaam, Tanzania, participated in a single focus group discussion. To be eligible for the study, participants had to be stakeholders engaged in cervical cancer research, practice, or policy in Tanzania; had to provide verbal informed consent; and had to agree to have their responses audio-recorded and transcribed for analyses. Participants were recruited by telephone and through face-to-face contact using convenience sampling based on profession and location of employment (Dar es Salaam). Verbal informed consent and permission to audio-record the discussion were provided.
Of the 35 participants, 20 were women. Twelve participants who were physicians reported working in public-sector health clinics, and an equal number of physicians worked with the government. Six participants were senior-level researchers who worked in academia. Five others worked with nongovernmental organizations, including two physicians and three social scientists trained in public health. All participants resided in Dar es Salaam.
Procedures
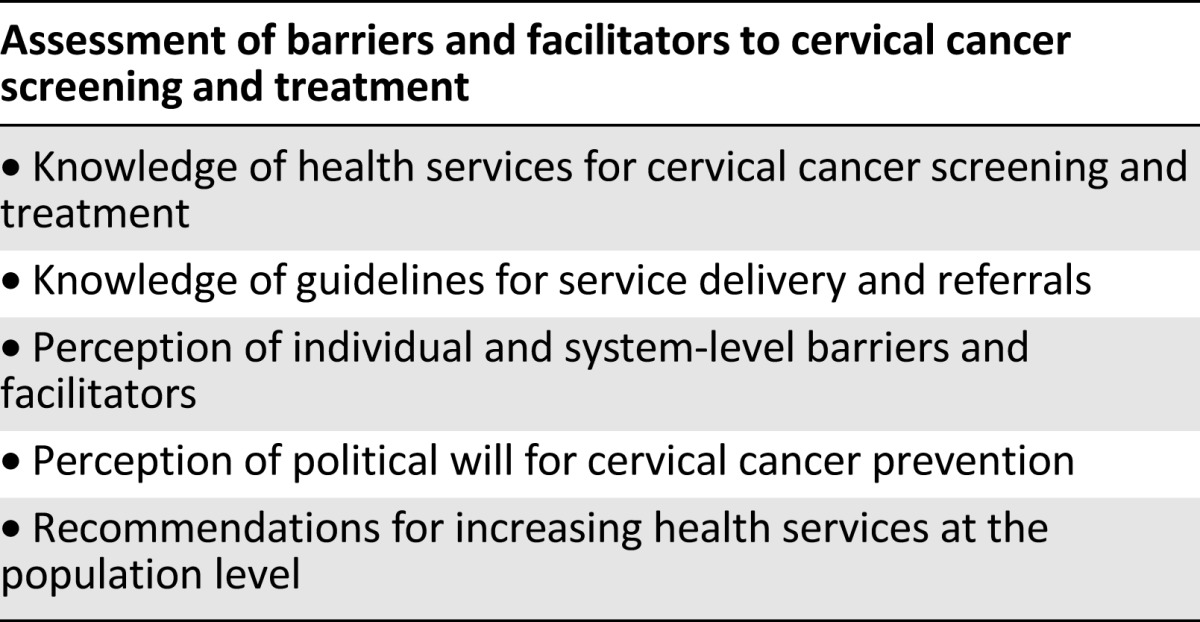
Open-ended questions were developed to elicit data on barriers and facilitators to cervical cancer screening and treatment, political will for cervical cancer prevention, knowledge of available health services in public-sector facilities for screening and treatment, and recommendations for population-level increases in delivery of services (Table 1). Interview questions were based on findings from cervical cancer research conducted in low-resource settings [7, 20–22]. The interviews lasted approximately 1 hour and 30 minutes, and the focus group discussion lasted about 1 hour. All interviews and the focus group discussion were conducted in English. Because anonymity was necessary for participants to give complete and unbiased responses, limited demographic data were obtained.
Table 1.
Topic guide
Data Analysis
Qualitative data were analyzed using framework analysis [23]. Framework analysis allows for familiarization with data, coding, thematic development, and interpretation of qualitative data. Familiarization is an iterative process that involves a detailed review of transcripts, data collection tools, and field notes. This iterative process was used to create themes that represent larger phenomena reflected through the data. Guided by this iterative process and the principles of reflexivity, data were analyzed using an inductive approach. Four cervical cancer researchers independently analyzed the data to establish intercoder reliability and to identify salient themes related to perceived barriers and facilitators that influence scale-up of cervical cancer screening and treatment in Tanzania. NVivo 8 qualitative software (QSR International, Melbourne, Australia, http://www.qsrinternational.com) [24] was used to organize the data to allow for in-depth analysis.
The multilevel social ecological model [25] provided a theoretical framework for analysis of the emerging themes. The social ecological model [25] argues that multiple contextual factors influence health behavior and health promotion and the systems that support systematic, structural change. The social ecological model [25] posits that there are five levels of influence: individual, intrapersonal, community, institutional, and policy levels. The model [26] is based on the idea that individual to policy levels of influence facilitate and limit health behavior and health promotion. The themes that emerged in this study relate to each level of influence included in the social ecological model.
Results
The analysis of data from the interviews and focus group discussion provided insight into system-level, structural factors that may constrain and facilitate cervical cancer screening and treatment in Tanzania. Four major themes emerged based on institutional and intrapersonal factors, including sociocultural and policy-level contextual factors, along with selected quotes from participants, as presented below.
Theme 1: Resource Allocation Will Facilitate Wider Screening Coverage and Implementation of Cervical Cancer Screening and Treatment
Nearly all participants perceived that limited financial and human resources were major barriers to increasing cervical cancer screening and treatment. Limited financial and human resources were perceived to constrain population-level health services for cervical cancer control and prevention efforts. Participants largely agreed with the following statements:
With increased screening, we must have more treatment facilities. It’s a question of human and financial resources. [Male interview participant, cancer prevention specialist]
The problem of financial resources is always there. If the program is not part of the main budget, there is no way to fit it in. [Male interview participant, oncologist]
Participants suggested, however, that building partnerships and leveraging existing reproductive health services were potential solutions for overcoming challenges of insufficient resources for scale-up of cervical cancer screening and treatment.
[We] need to figure out what partnerships are already working and see if we can work with what already exists. [Male interview participant, cancer prevention specialist]
Theme 2: Capacity Building Is Necessary for Increasing Screening and Treatment Programs
Capacity building at the regional and district levels of the health system was reported as a key facilitator for improving access to early detection and treatment across the country. Creating regional centers of expertise to expand the number of trained clinicians and health centers providing screening and treatment was considered to be an integral part of the long-term plan for improving health services. Participants suggested that decentralizing health services for cervical cancer prevention was the next step.
[We] need to designate institutions to do onsite cervical cancer screenings and provide trainings at health centers to build capacity at the regional and district levels. [Female focus group participant, physician at a district health center]
The ministry of health wants this test in all areas of Tanzania; therefore, we are training teams to go out and train others. [Male interview participant, senior physician from the Ministry of Health and Social Welfare]
To illustrate ongoing capacity building for cervical cancer prevention in each geographic zone and region, a participant briefly explained the structure of health services:
The country is divided into [several] regions with zones within them. We train a zone in one region and move to the next region so there is training in all regions, not just one. [Female interview participant, physician]
Participants argued that immediate improvements in the referral system were needed to treat cervical cancer at the district and regional levels. Participants suggested that creating regional services would improve access to care for women living farther away from the national hospital and cancer center in Dar es Salaam. Participants stated that improving regional and district services would likely decrease the demand on the referral system. Comments from two participants support this point:
We must make the referral system more efficient including decentralization of treatment from the [national level] to making regional districts with cancer care capacities. [Male interview participant, cancer prevention specialist]
We need to focus training on health center and dispensary workers at the [regional and district levels]. [Male interview participant, physician of obstetrics and gynecology]
Theme 3: Sociocultural Factors Influence Cervical Cancer Prevention, but Gaps in the Health System May Have Greater Influence on Scale-Up of Screening and Treatment
Participants reported that sociocultural factors influence acceptance of cervical cancer screening and treatment. Fatalism toward cancer diagnosis and treatment were perceived to influence people’s health seeking behaviors and attitudes toward prevention. In the first quote below, a participant discussed the influence of fatalism on health-seeking behavior. In addition, participants perceived that the religious beliefs, a proxy measure of sociocultural beliefs, of Tanzanian men and women shaped attitudes about cervical cancer and cancer in general. Despite the reported influence of sociocultural factors such as fatalism and religious beliefs, participants indicated that Tanzanian women would seek screening and treatment if there were interventions to create awareness.
People believe that anyone going [for treatment] will die. What they don’t realize is that most people who come [for treatment] have waited until the disease is late stage. [Male interview participant, senior health expert]
Religion is very important to most Tanzanians. If you can get to them through their religion, you have a better chance of success [with prevention]. [Female interview participant, technical advisor with a local NGO]
The gap is more in the health care system. The community is willing to uptake services. The major problem is the capacity to treat [women]. [Female focus group participant, physician with an NGO]
Theme 4: Political Will Exists for Cervical Cancer Screening and Treatment
Participants perceived that political will exists for cervical cancer screening and treatment. Participants from the ministry of health reported that the government is preparing to fund services for sustainability and integration of screening and treatment.
Currently, there is a lot of political [support] for cancer prevention. [Male interview participant, physician from the Ministry of Health and Social Welfare]
For sustainability, the government is working on a package and funding from the health basket with the intention to sustain program[s] initiated by foreign organizations. Once their time is over, the government will take over for the long term. [Male interview participant, senior physician from the Ministry of Health and Social Welfare]
Discussion
Through this study, we have identified four themes that represent the perceived system-level structural factors that may influence scale-up of cervical cancer screening and treatment in Tanzania. The themes emerging from our study are consistent with ongoing and phased developments in the field, which have been supported by responses given by our key stakeholders. This study complements the literature [10, 11, 27, 28] by highlighting the perceived system-level factors of key stakeholders in a country with a high burden of cervical cancer, using the social ecological model as a theoretical framework [24]. The framework provides a way to categorize the multiple factors that may both constrain and facilitate scale-up of population-level screening and treatment. Our thematic analysis enabled us to identify resource allocation, capacity building, sociocultural influence, and political will as prominent factors to consider in the scale-up of cervical cancer screening and treatment in Tanzania.
In the context of the theoretical framework proposed in the social ecological model, the respective themes in the study are relevant to individual, intrapersonal, institutional, community, and policy levels of influence. Theme 1 (resource allocation) relates to institutional factors that limit scale-up of screening and treatment. Theme 2 (capacity building) pertains to both institutional and policy-level factors that help determine how to strengthen the health system to provide population-level cervical cancer screening and treatment. Theme 3 (sociocultural influence) reflects the intrapersonal and cultural contexts within the community that have some influence on women’s health-seeking behaviors. Theme 4 (political will) is relevant to policy-level contextual factors that influence systematic changes through formal and informal government-supported initiatives.
Resource allocation and capacity building are fundamental components of successful screen-and-treat programs. One of the major perceived structural challenges in our study relates to the need for strengthening service delivery across the health system including in the district and tertiary referral centers. In our findings, key stakeholders argued that there was an immediate need for systematic approaches to improve access to screen-and-treat services for women living in all parts of the country. The responses of the key stakeholders are in accord with ongoing efforts to create system-level advances in the way Tanzania will deliver cervical cancer screen-and-treat services in the future. The development of the Tanzanian national guidelines for cervical cancer screening and treatment [14] is an example of a systematic effort to improve resource allocation and to build capacity for cervical cancer prevention on a large scale. Mwanahamuntu and colleagues [12] suggest that country ownership in the development of national guidelines was a key factor that helped sustain cervical cancer prevention programs over time in Zambia, where thousands of deaths have been prevented through comprehensive screening and treatment programs [28].
Our key stakeholders discussed the advantage of developing partnerships to improve capacity and resource allocation for screen-and-treat programs. In 2013, Tanzania was selected as a country partner in Pink Ribbon Red Ribbon, an innovative public-private partnership designed to improve cervical cancer prevention by leveraging the HIV/AIDS President’s Emergency Plan for AIDS Relief (PEPFAR) platform [29]. More specifically, the Pink Ribbon Red Ribbon partnership was developed to help countries in Africa and Latin America enhance the implementation of their national women’s cancer control programs [29]. This partnership represents a great opportunity to expand screening and treatment services across Tanzania and is the kind of partnership that was recommended by stakeholders in our study.
Political will for capacity building for screening and treatment was reported to influence the expansion and sustainability of health services. This aspect has been reported previously and is consistently accepted as a key factor influencing cervical cancer screening and treatment programs in low-resource settings [5, 30]. Our key stakeholders commented on ongoing activities that demonstrate a high level of political will for cervical cancer prevention in Tanzania, and they suggested that organizations will work to fund cancer prevention programs over the long term to promote sustainability. The support of First Lady Mama Salma Kikewte for the Pink Ribbon Red Ribbon partnership and the Medical Women Association of Tanzania breast and cervical cancer campaigns and her development of the Wanawake Na Maendeleo (WAMA) Foundation for women’s health and social well-being demonstrates the great extent of political will for cervical cancer prevention in Tanzania [31, 32].
Sociocultural factors have been reported to influence acceptance of cervical cancer screening and treatment in low-resource settings [20, 33, 34]. Chirwa et al. [33] found that folk myths and misconceptions about cervical cancer were prevalent in their community-based assessment of women’s knowledge and attitudes in Zambia. Folk myths were associated with poorer acceptance of screening in the Zambian study, and this finding is similar to those on sociocultural influence in other studies of health behavior [33, 34]. In our study, key stakeholders perceived that sociocultural factors including myths and misconceptions would influence screening behavior; however, key stakeholders believed that limited service delivery and perceptions about low resources for cervical cancer prevention would limit uptake of screening more than perceived sociocultural barriers related to folk myths. This finding is more striking compared with what has been reported in the literature on the influence of folk myths and misconceptions [33] and highlights the stakeholders’ perceived impact of material resources and social and economic factors on health behavior. White et al. [35] reported that both traditional cultural beliefs and newer biomedical information about cervical cancer acted as determinants of behavior among Zambian women participating in screening programs, and this is more similar to our findings.
Conclusion
Results from this study indicate that various factors contribute to the challenge of cervical cancer screening and treatment in Tanzania. The study also suggests that there are systematic developments aimed at improving cervical cancer prevention and control in Tanzania. Although the lack of comprehensive sociodemographic data of the participating stakeholders and convenience sampling preclude generalization of results, the sample represents key stakeholders who have been influential in improving screening and treatment programs. We believe the themes emerging from the results of this study may be used to inform programs that seek to expand cervical cancer screening and treatment in Tanzania.
Acknowledgments
We thank Dr. Innocent Semali for his guidance and expertise during the planning of this study and Stanford Mwasongwe for his help with data collection and organization. We are grateful to Rejoice and Hope Ministries International for funding this study. Dr. McCree thanks the University of Alabama at Birmingham Cancer Prevention and Control Training Program (R25 Grant CA47888) for supporting this research as part of her dissertation fellowship.
Footnotes
For Further Reading: Eva Johanna Kantelhardt, Ulrike Moelle, Matthias Begoihn et al. Cervical Cancer in Ethiopia: Survival of 1,059 Patients Who Received Oncologic Therapy. The Oncologist 2014;19:727–734.
Implications for Practice: This study analyzes 1,059 patients from Ethiopia with newly diagnosed cervical cancer who were treated by radiotherapy in the country’s only oncologic referral center. Overall survival after 2 years was considerably high (74%) compared with data from African cancer registries, underlining the usefulness of radiotherapy. The survival was still lower than that of patients from higher-resource settings, probably because of the lack of brachytherapy. Therefore, brachytherapy for cervical cancer patients should be of high priority. Patients with earlier stages of disease had better outcome compared with those with later stages. Awareness and early detection programs are needed in the Ethiopian setting.
Author Contributions
Conception/Design: Renicha McCree, Mary Rose Giattas, Nedra Lisovicz
Provision of study material or patients: Renicha McCree
Collection and/or assembly of data: Renicha McCree, Mary Rose Giattas, Nedra Lisovicz
Data analysis and interpretation: Renicha McCree, Nedra Lisovicz
Manuscript writing: Renicha McCree, Vikrant V. Sahasrabuddhe, Pauline E. Jolly, Michelle Y. Martin, Stuart Lawrence Usdan, Connie Kohler, Nedra Lisovicz
Final approval of manuscript: Renicha McCree, Vikrant V. Sahasrabuddhe, Pauline E. Jolly, Michelle Y. Martin, Stuart Lawrence Usdan, Connie Kohler, Nedra Lisovicz
Disclosures
The authors indicated no financial relationships.
References
- 1.GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012. Available at http://globocan.iarc.fr. Accessed November 8, 2014.
- 2.Gakidou E, Nordhagen S, Obermeyer Z. Coverage of cervical cancer screening in 57 countries: Low average levels and large inequalities. PLoS Med. 2008;5:e132. doi: 10.1371/journal.pmed.0050132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sitas F, Parkin DM, Chirenje M, et al. Part II: Cancer in indigenous Africans—causes and control. Lancet Oncol. 2008;9:786–795. doi: 10.1016/S1470-2045(08)70198-0. [DOI] [PubMed] [Google Scholar]
- 4.Schiffman M, Castle PE, Jeronimo J, et al. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907. doi: 10.1016/S0140-6736(07)61416-0. [DOI] [PubMed] [Google Scholar]
- 5.Tsu VD, Levin CE. Making the case for cervical cancer prevention: What about equity? Reprod Health Matters. 2008;16:104–112. doi: 10.1016/S0968-8080(08)32411-2. [DOI] [PubMed] [Google Scholar]
- 6.Huerta E, Grey N. Cancer control opportunities in low- and middle-income countries. CA Cancer J Clin. 2007;57:72–74. doi: 10.3322/canjclin.57.2.72. [DOI] [PubMed] [Google Scholar]
- 7.Bradley J, Barone M, Mahé C, et al. Delivering cervical cancer prevention services in low-resource settings. Int J Gynaecol Obstet. 2005;89(suppl 2):S21–S29. doi: 10.1016/j.ijgo.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 8.Moodley J, Kawonga M, Bradley J, et al. Challenges in implementing a cervical screening program in South Africa. Cancer Detect Prev. 2006;30:361–368. doi: 10.1016/j.cdp.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Mwanahamuntu MH, Sahasrabuddhe VV, Pfaendler KS, et al. Implementation of ‘see-and-treat’ cervical cancer prevention services linked to HIV care in Zambia. AIDS. 2009;23:N1–N5. doi: 10.1097/QAD.0b013e3283236e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parham GP, Mwanahamuntu MH, Sahasrabuddhe VV, et al. Implementation of cervical cancer prevention services for HIV-infected women in Zambia: Measuring program effectiveness. HIV Ther. 2010;4:703–722. doi: 10.2217/hiv.10.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pfaendler KS, Mwanahamuntu MH, Sahasrabuddhe VV, et al. Management of cryotherapy-ineligible women in a “screen-and-treat” cervical cancer prevention program targeting HIV-infected women in Zambia: Lessons from the field. Gynecol Oncol. 2008;110:402–407. doi: 10.1016/j.ygyno.2008.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mwanahamuntu MH, Sahasrabuddhe VV, Kapambwe S, et al. Advancing cervical cancer prevention initiatives in resource-constrained settings: Insights from the Cervical Cancer Prevention Program in Zambia. PLoS Med. 2011;8:e1001032. doi: 10.1371/journal.pmed.1001032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Louie KS, de Sanjose S, Mayaud P. Epidemiology and prevention of human papillomavirus and cervical cancer in sub-Saharan Africa: A comprehensive review. Trop Med Int Health. 2009;14:1287–1302. doi: 10.1111/j.1365-3156.2009.02372.x. [DOI] [PubMed] [Google Scholar]
- 14.Sherris J, Wittet S, Kleine A, et al. Evidence-based, alternative cervical cancer screening approaches in low-resource settings. Int Perspect Sex Reprod Health. 2009;35:147–154. doi: 10.1363/ifpp.35.147.09. [DOI] [PubMed] [Google Scholar]
- 15.Ngoma T, Muwonge R, Mwaiselage J, et al. Evaluation of cervical visual inspection screening in Dar es Salaam, Tanzania. Int J Gynaecol Obstet. 2010;109:100–104. doi: 10.1016/j.ijgo.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 16.Blumenthal PD, Lauterbach M, Sellors JW, et al. Training for cervical cancer prevention programs in low-resource settings: Focus on visual inspection with acetic acid and cryotherapy. Int J Gynaecol Obstet. 2005;89(suppl 2):S30–S37. doi: 10.1016/j.ijgo.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 17.Sauvaget C, Fayette J-M, Muwonge R, et al. Accuracy of visual inspection with acetic acid for cervical cancer screening. Int J Gynaecol Obstet. 2011;113:14–24. doi: 10.1016/j.ijgo.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 18.Chamot E, Kristensen S, Stringer JS, et al. Are treatments for cervical precancerous lesions in less-developed countries safe enough to promote scaling-up of cervical screening programs? A systematic review. BMC Womens Health. 2010;10:11. doi: 10.1186/1472-6874-10-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sankaranarayanan R, Gaffikin L, Jacob M, et al. A critical assessment of screening methods for cervical neoplasia. Int J Gynaecol Obstet. 2005;89(suppl 2):S4–S12. doi: 10.1016/j.ijgo.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 20.Bingham A, Bishop A, Coffey P, et al. Factors affecting utilization of cervical cancer prevention services in low-resource settings. Salud Publica Mex. 2003;45(suppl 3):S408–S416. doi: 10.1590/s0036-36342003000900015. [DOI] [PubMed] [Google Scholar]
- 21.Lisovicz N, Wynn T, Fouad M, et al. Cancer health disparities: What we have done. Am J Med Sci. 2008;335:254–259. doi: 10.1097/maj.0b013e31816a43ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chirenje ZM, Rusakaniko S, Kirumbi L, et al. Situation analysis for cervical cancer diagnosis and treatment in east, central and southern African countries. Bull World Health Organ. 2001;79:127–132. [PMC free article] [PubMed] [Google Scholar]
- 23.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess RG, editors. The Qualitative Researcher’s Companion. Thousand Oaks, CA: Sage Publications; 2002. pp. 173–194. [Google Scholar]
- 24.McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 25.Kawonga M, Fonn S. Achieving effective cervical screening coverage in South Africa through human resources and health systems development. Reprod Health Matters. 2008;16:32–40. doi: 10.1016/S0968-8080(08)32403-3. [DOI] [PubMed] [Google Scholar]
- 26.Denny L, Quinn M, Sankaranarayanan R. Chapter 8: Screening for cervical cancer in developing countries. Vaccine. 2006;24(suppl 3):S3/71–S3/77. doi: 10.1016/j.vaccine.2006.05.121. [DOI] [PubMed] [Google Scholar]
- 27.Perng P, Perng W, Ngoma T, et al. Promoters of and barriers to cervical cancer screening in a rural setting in Tanzania. Int J Gynaecol Obstet. 2013;123:221–225. doi: 10.1016/j.ijgo.2013.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sahasrabuddhe VV, Parham GP, Mwanahamuntu MH, et al. Cervical cancer prevention in low- and middle-income countries: Feasible, affordable, essential. Cancer Prev Res (Phila) 2012;5:11–17. doi: 10.1158/1940-6207.CAPR-11-0540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oluwole D, Kraemer J. Innovative public-private partnership: A diagonal approach to combating women’s cancers in Africa. Bull World Health Organ. 2013;91:691–696. doi: 10.2471/BLT.12.109777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pollack AE, Balkin MS, Denny L. Cervical cancer: A call for political will. Int J Gynaecol Obstet. 2006;94:333–342. doi: 10.1016/j.ijgo.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 31.Medical Women Association of Tanzania. Available at http://www.mewata.org. Accessed November 8, 2014.
- 32.WAMA Foundation. Available at http://www.wamafoundation.or.tz. Accessed November 8, 2014.
- 33.Chirwa S, Mwanahamuntu M, Kapambe S. Myths and misconceptions about cervical cancer among Zambian women: Rapid assessment by peer educators. Global Health Promot. 2010;17:47–50. doi: 10.1177/1757975910363938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dein S. Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncol. 2004;5:119–124. doi: 10.1016/S1470-2045(04)01386-5. [DOI] [PubMed] [Google Scholar]
- 35.White HL, Mulambia C, Sinkala M, et al. ‘Worse than HIV’ or ‘not as serious as other diseases’? Conceptualization of cervical cancer among newly screened women in Zambia. Soc Sci Med. 2012;74:1486–1493. doi: 10.1016/j.socscimed.2012.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]


