This study examined data from the 2010 China Chronic Disease and Risk Factor Surveillance System to profile cervical cancer screening behavior among women in China. The results indicate that screening programs need to be strengthened along with a more intense focus on specific demographic groups to make screening services available and accessible to all women, especially those who reside in rural areas and those with no health insurance.
Keywords: Cervical cancer, Papanicolaou test, Women, China, Epidemiology
Abstract
Introduction.
Cervical cancer is one of the most commonly diagnosed cancers among women in China. The World Health Organization (WHO) recommends routine screening for cervical cancer, and the WHO Global Monitoring Framework suggests that every nation monitors cervical cancer screening. However, little information is available on cervical cancer screening behavior among women in China.
Methods.
We used data from the 2010 China Chronic Disease and Risk Factor Surveillance System that included 51,989 women aged 18 years and older. We report the proportion of women who reported ever having had a Papanicolaou (Pap) test, stratified by sociodemographic characteristics and geographic region. Multivariable logistic regression modeling was performed to adjust for potential confounders.
Results.
Overall, 21% of 51,989 women reported having ever had a Pap test. The highest proportion was reported among women aged 30–39 years (30.1%, 95% confidence interval, 26.8%–33.4%). In all geographic regions, women in rural areas were consistently less likely than women in urban areas to report having had a Pap test. Among women who reported ever having a Pap test, 82% reported having the most recent test in the past 3 years. Factors associated with reporting ever having a test were being aged 30–49 years, higher education, being married, and having urban health insurance.
Conclusion.
Our results indicate that screening programs need to be strengthened along with a more intense focus on specific demographic groups. National cervical cancer screening guidelines and comprehensive implementation strategies are needed to make screening services available and accessible to all women.
Implications for Practice:
This study is the largest nationwide and population-based assessment of self-reported history of Pap test for cervical cancer screening in China. This article describes cervical cancer screening behavior among women and examines key demographic and geographic factors. Only one fifth of Chinese women reported having ever had a Pap test for cervical cancer screening. The results highlight the urgent need to develop national cervical cancer screening guidelines and strategies that make screening services widely available, accessible, and acceptable to all women, especially to those who reside in rural areas and those with no health insurance.
Introduction
Cervical cancer is one of the most commonly diagnosed cancers among women in China. The 2012 Chinese Cancer Registry reported an overall age-adjusted cervical cancer incidence rate of 8.98 per 100,000 and a mortality rate of 2.13 per 100,000 that was 48% higher in the rural than that in urban areas in all cancer registration areas after standardization using the world population. The increase in age-specific incidence rates started with the group aged 25 years and older and peaked at the age group of 35–45 years. The mortality was relatively low before 35 years of age, dramatically increased after 35 years of age, and peaked with the group aged 85 years and older [1].
The World Health Organization (WHO) recommends cancer screening when resources are available to reach a high proportion of the at-risk population and when management and treatment of abnormalities detected are available [2]. In 2013, the WHO Global Monitoring Framework suggested that all nations monitor cervical cancer screening. The framework recommends a metric that measures women aged 30 years and older who have been screened at least once during their lifetime [3].
Cervical cancer screening services are available in all provinces of China, but coverage is highly variable across regions. Better understanding of the current status of cervical cancer screening across China is needed to facilitate development of a comprehensive cervical cancer prevention strategy and national guidelines. In this study, we describe a self-reported history of a Pap test of the uterine cervix among women in China and examine key demographic and geographic factors associated with the reported history of Pap test.
Material and Methods
Study Population
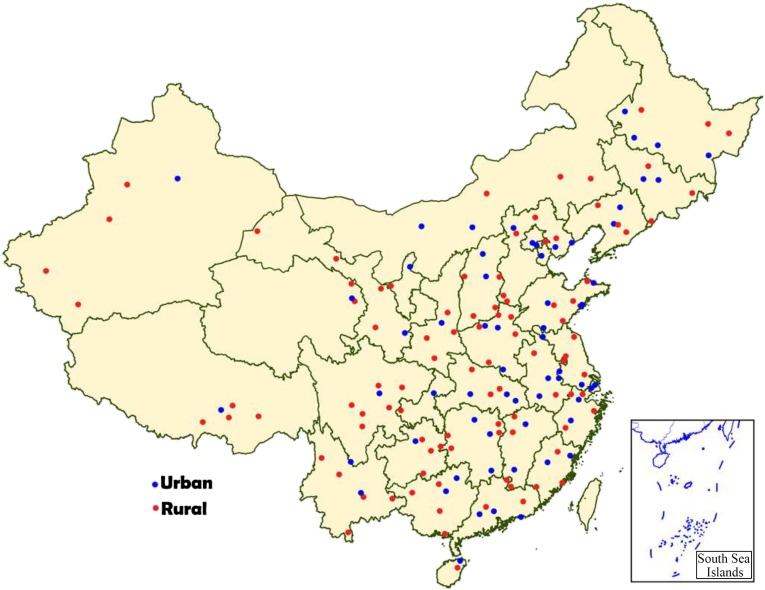
We obtained data from the 2010 China Chronic Disease and Risk Factor Surveillance (CCDRFS) System. CCDRFS is a nationwide survey using face-to-face interviews and physical measurements. It is conducted once every 3 years using a random sampling design based on the China National Disease Surveillance Points (DSP) system [4–6]. Briefly, the 2010 CCDRFS covered all 31 provinces, autonomous regions, and municipalities and included 162 counties with surveillance points; 63 counties were in urban areas and 99 counties in rural areas (Fig. 1). Multistage stratified cluster random sampling methods were used to sample households. In the first stage of sampling, four townships per county were randomly selected from each surveillance point using the method of probability proportion to size (PPS). PPS is a sampling procedure under which the probability of a unit being selected is proportional to the size of the ultimate unit, giving larger clusters a greater probability of selection and smaller clusters a lower probability. In the second stage, three villages or communities were sampled from each selected township by the PPS method. In the third sampling stage, a residential group (at least 50 households) from each village or community was selected, and finally, from those households, one permanent resident aged 18 years or older was selected using the Kish grid method [6, 7]. Permanent residents were defined as those who had lived in the surveillance counties or districts for at least 6 months.
Figure 1.
Location of 162 urban and rural study sites of the China National Disease Surveillance Points System, the 2010 China Chronic Disease and Risk Factor Surveillance.
At least three attempts were made to contact each selected resident. If the selected household could not be reached, a household with similar structure in terms of family size and socioeconomic status in the same village or community neighborhood was used as a replacement. Upon obtaining informed consent, a face-to-face interview using standardized questionnaires was carried out by trained interviewers.
A total of 98,712 participants (54% female, n = 53,513) were enrolled and interviewed from August to December in the 2010 CCDRFS. The overall household sample replacement rate was 9.3%. For this analysis, we included only women and excluded 1,524 women who did not respond to the Pap test question, resulting in a final analysis sample of 51,989 women aged 18 years or older. The survey protocol received Institutional Review Board approval from the Ethics Committee of the Chinese Center for Disease Control and Prevention. Informed consent was obtained from all study participants.
History of Pap Test for Cervical Cancer Screening
The proportion of women who reported a history of Pap test was determined by two questions under the questionnaire section “For Cervical Cancer Screening (Women Only)”: “Have you ever had a Pap test of the uterine cervix?” The response categories were yes, no, or don’t know. For those who answered yes, they were further queried “If you ever had a test, how many years ago was your last examination?”
Sociodemographic Factors
We examined the following demographic factors: age (18–29, 30–39, 40–49, 50–59, 60–69, or 70+ years), ethnicity (Han or other, which included Zhuang, Manchu, Hui, Miao, Uyghur, Yi, Tujia, Mongol, Korean, and Tibetan), years of education (fewer than 6, 6–11, or 12 or more), marital status (married, never married, or other, which included those living with partner, widowed, divorced, or married but not living with husband), occupation (employed, student/unemployed, or retired), and medical insurance (urban insurance, rural insurance, or no insurance). Urban insurance included a basic medical insurance system for urban employees, government payment for government employees, commercial insurance, supplementary insurance for urban residents, as well as specific insurance for serious diseases. Rural insurance included a basic medical insurance system for rural residents known as the New Rural Cooperative Medical System. Provinces, autonomous regions, and municipalities were categorized into geographic region (eastern, middle, or western region), and residence status (urban or rural) was according to the China National Bureau of Statistics. We also created a variable that combined geographic region and urban/rural residence.
Statistical Analysis
We used SAS (Version 9.2; SAS Institute, Inc., Cary, NC, http://sas.com/en_us/home.html) for statistical analysis and to adjust for the complex sampling design in these analyses. Prevalence estimates were adjusted to the population of sampled areas consistent with the CCDRFS complex sampling design, accounting for sampling stratification, primary sampling units, and clustering. We weighted all proportions to obtain results representative of DSP areas to account for the sampling scheme. Poststratification adjustments were made for age and gender using data from the 2009 National Sample Survey on Population Changes, as well as the Taylor series method for finite population correction to estimate standard errors.
We used descriptive statistics to examine demographic characteristics and cervical cancer screening behaviors. We calculated the proportion of women who reported ever having a Pap test, prevalence odds ratios (POR), and 95% confidence intervals (CIs) by sociodemographic and geographic region categories. We used logistic regression modeling to simultaneously adjust for covariates. We also examined factors associated with having a Pap test within the past 3 years. Statistical significance was defined to be a p value of <.05.
Results
Overall Characteristics of Survey Participants
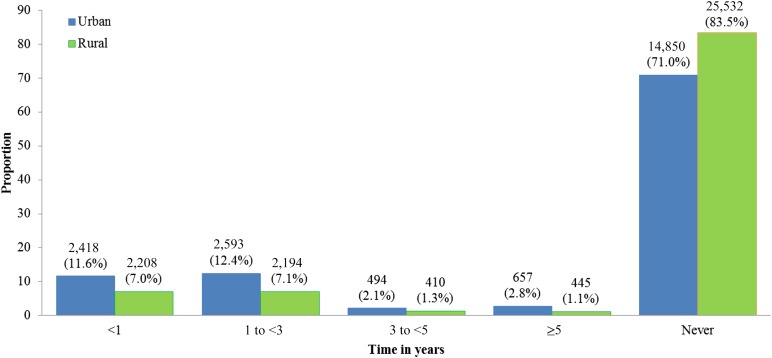
A total of 51,989 adult women 18 years and older (mean age, 46 years; standard deviation, 15; range, 18–107 years) participated and answered the question of Pap test for cervical cancer. Approximately 45.7% were women younger than 40 years of age, 68.6% were from rural areas, and 40.2% were from the eastern region (Table 1).
Table 1.
Number of subjects (N), proportion (%), and weighted proportion by sociodemographic characteristics (female participants, 2010 China Chronic Disease and Risk Factor Surveillance)
Prevalence of Pap Testing
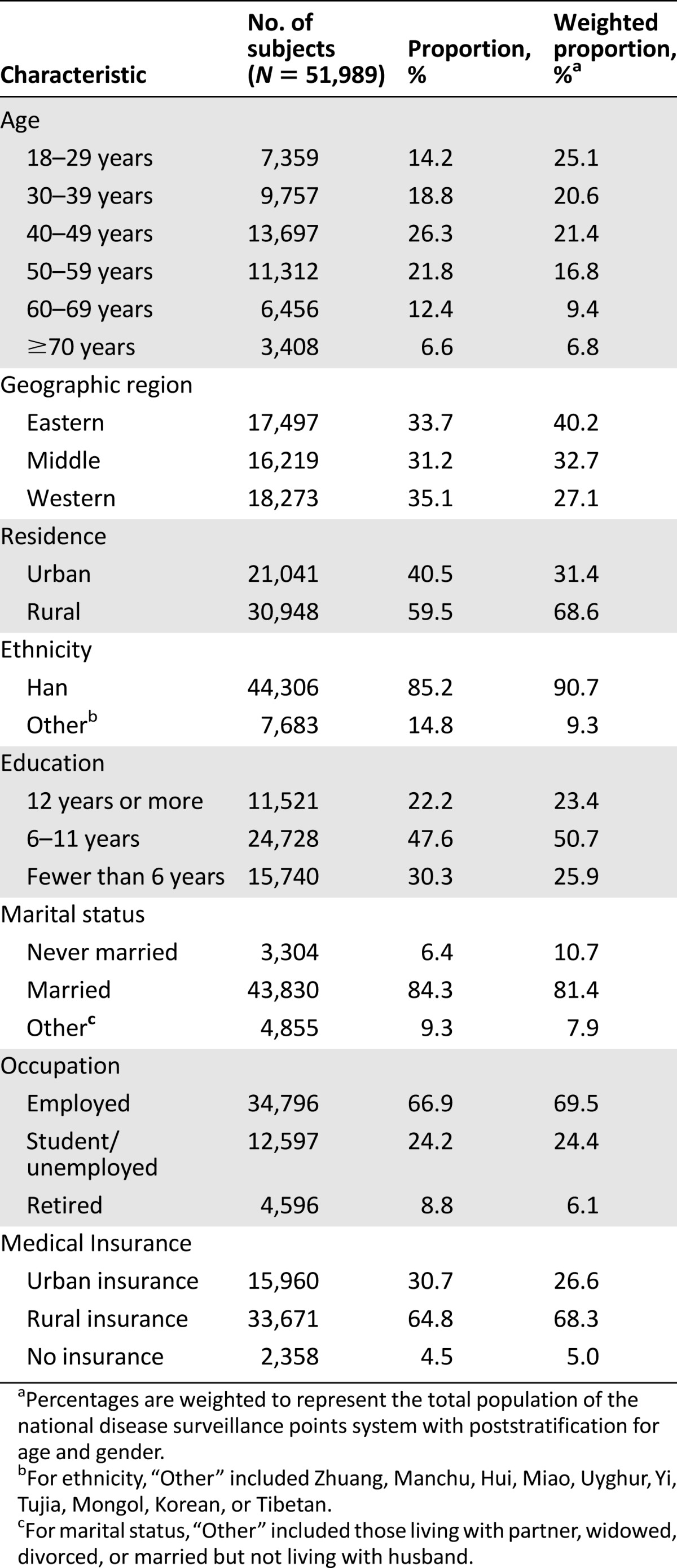
Overall, 20.7% (11,607 of 51,989, 95% CI 18.6%–22.8%) of women reported ever having had a Pap test. The highest proportion was reported by women aged 30–39 years (30.1%, 95% CI 26.8%–33.4%). Prevalence of reporting Pap test was highest among women in eastern China (23.9%), followed by women in the western (18.9%) and middle regions (18.3%). Compared with the eastern region, the adjusted POR (95% CI) was 0.86 (0.65–1.12) for women in the western region and 0.78 (0.57–1.07) for women in the middle region. The proportion of women who reported ever having had a Pap test was higher among women residing in urban areas (29.1%) compared with those in rural areas (16.9%); the adjusted POR was 0.76 with 95% CI 0.58–1.00, p = .048 (Table 2).
Table 2.
Number of subjects, number reported ever having Pap test, proportion (%), unadjusted POR, adjusted POR, 95% CI by sociodemographic characteristics (female participants, 2010 China Chronic Disease and Risk Factor Surveillance)
Compared with women with 12 or more years of education, women with 6–11 years of education (adjusted POR 0.73, 95% CI 0.65–0.83, p < .001) and women with fewer than 6 years of education (adjusted POR 0.49, 95% CI 0.41–0.60, p < .001) were significantly less likely to report a history of Pap test. When compared with women who reported being married, those who reported never being married were least likely to report a history of Pap test (adjusted POR 0.12, 95% CI 0.09–0.16, p < .001). Compared with women who reported having urban medical insurance, women with rural insurance coverage (adjusted POR 0.47, 95% CI 0.38–0.58, p < .001) and women who reported no insurance coverage (adjusted POR 0.55, 95% CI 0.46–0.67, p < .001) were significantly less likely to report a history of Pap test (Table 2).
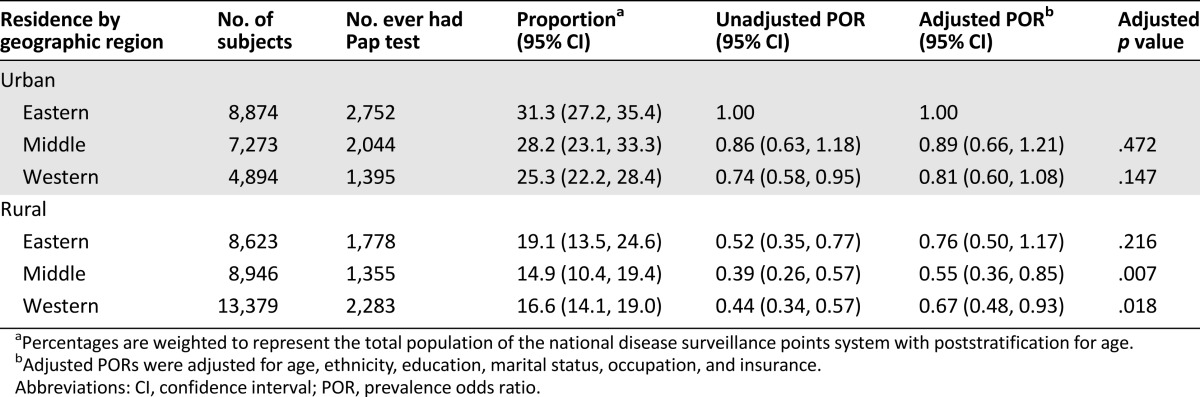
When geographic region was further examined by urban or rural residence (Table 3), we found that women residing in urban areas were more likely than those with rural residence to report a history of Pap test, regardless of geographic region. Compared with women with urban residence in the eastern region, Pap testing rates were significantly lower among women with rural residence in the middle (adjusted POR 0.55, 95% CI 0.36–0.85, p = .007) and western regions (adjusted POR 0.67, 95% CI 0.48–0.93, p = .018).
Table 3.
Number of subjects, number reported ever having Pap test, proportion (%), unadjusted POR, and adjusted POR, 95% CI by residence and geographic region (female participants, 2010 China Chronic Disease and Risk Factor Surveillance)
Further subgroup analyses stratified by urban and rural residence showed that women aged 50 years and older were significantly less likely to report ever having a test, regardless of urban or rural residence. In both areas, the proportions of women aged 40–49 years had the largest difference (urban 39.7%, 95% CI 36.1–43.3; rural 23.6%, 95% CI 19.6–27.6). Although women with fewer than 6 years of education were significantly less likely to report a history of Pap test in both urban and rural areas, reporting 6–11 years of education was associated with lower prevalence of Pap test only among women in urban areas. Similarly, reporting being a student or unemployed was associated with lower prevalence of reporting history of Pap test among women in the urban areas but not among women in rural areas. Compared with women with urban insurance, women with rural insurance and women without insurance were significantly less likely to report history of a Pap test in both urban and rural areas.
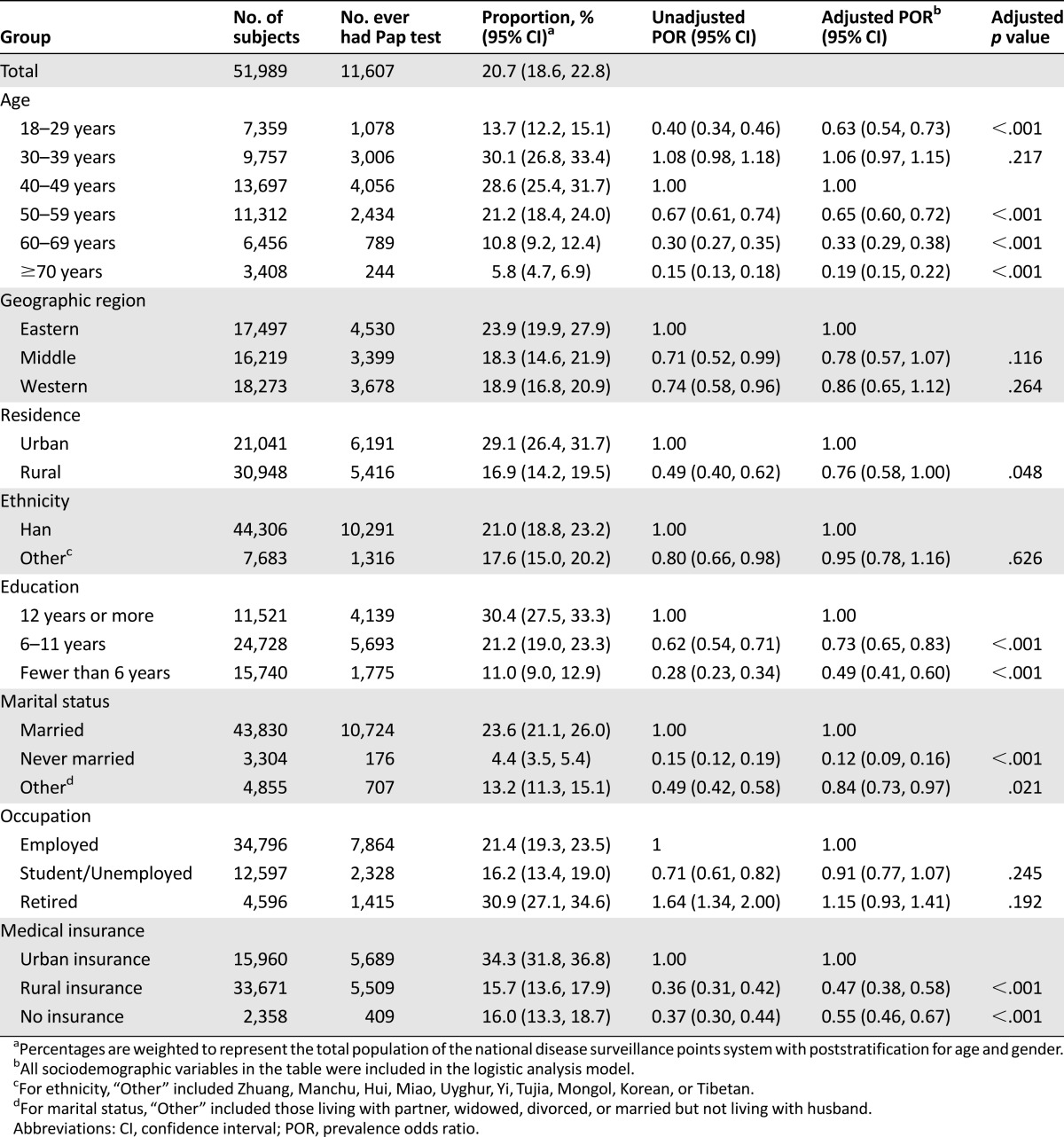
Most of women who reported ever having had a Pap test reported the duration since their last test. Most women reported having had the last Pap test within the past 5 years. Of those reporting the duration from their most recent screening, all the proportions in rural areas were lower than those in urban areas, respectively. Among women who had a Pap test within the past year (Fig. 2), a lower proportion of women in rural areas (7%) reported having had a Pap test compared with women in urban areas (11.6%).
Figure 2.
Prevalence and time since last Pap test by urban/rural status (2010 China Chronic Disease and Risk Factor Surveillance). The percentages are weighted to represent the total population of the national disease surveillance points system with poststratification for age and gender. A total of 188 screened subjects were excluded because of missing test time information on time since last Pap test.
Discussion
Only one fifth of Chinese women in the CCDRFS reported having ever had a Pap test for cervical cancer screening in our study. This is a worrisome finding given that cervical cancer is a common cancer in China with increasing incidence and younger age at diagnosis [8]. Consistent with other surveys around the world, we found that poor and uneducated women and those aged 50 years and older were less likely to report having had a Pap test. In China, the peak incidence of cervical cancer occurs among women ages 35–45 years of age [1], and our data show that the highest prevalence of reporting a Pap test is occurring the 10 years prior to this peak incidence as recommended by WHO/International Agency for Research on Cancer (IARC) [3].
In September 2012, the United Nations High Level Meeting on Non-Communicable Diseases (NCDs) made a political declaration on the importance of NCDs [9]. One of the voluntary global targets includes monitoring women 30 years and older who have been screened at least once in their lifetime. The IARC recommended that organized cytology screening for cervical cancer in developed countries, plus follow-up of individuals who had confirmed or suspicious diagnoses, would markedly reduce the incidence and mortality from cervical cancer among women aged 35–64 years [10]. The most recent WHO guidelines (2013) recommend that priority be given to maximizing coverage within the at-risk target age group and assuring complete follow-up of those women with abnormal screening test results, rather than maximizing the number of tests performed in a woman’s lifetime. Cervical cancer screening is recommended for every woman 30 years and older at least once in her lifetime, and women between 30 and 49 years old should be prioritized for screening [3]. Based on the WHO global monitoring framework, our study found less than a quarter of Chinese women aged 30 and older reported having been screened using the Pap test. Ensuring availability of screening services to maximize coverage throughout China and increasing screening participation among the high-risk age groups are critical priorities for cervical cancer prevention and screening in adult women.
WHO guidelines recommend the screening interval (frequency) should not be less than 5 years (and not less than 10 years if using with a human papillomavirus [HPV] test) [3]. For the general population, the newest evidence-based screening guidelines recommended starting screening with cytologic testing at age 21 and then every 3 years for women aged 21–29 years. Women aged 30 and older can be screened by cytologic and HPV cotesting every 5 years or cytology alone every 3 years [11]. However, our study indicated the proportion of women aged 30 years and older and having a Pap test in the last 3 years was less than 20% in China.
We found a significant difference in reporting history of Pap test between urban and rural areas. There are vast differences in sociocultural and economic development and in health care access across China [12]. Eastern China is generally more developed than middle China, and western China is the least developed, which may explain the higher screening rates in the east (23.9%). We also found that the proportion of women reporting a history of Pap test within rural areas was lower than those in urban areas in both the middle and western regions. Thus, any cervical cancer early detection program that can increase availability in rural areas in middle and western region in China could increase screening substantially.
In this analysis, we found that the prevalence of reporting Pap test use increased with increasing education level, consistent with previous studies [13–15]. Socioeconomic indicators predict health awareness, health care access, and affordability through economic, psychological, and social mediators [16, 17]. We also found that women with urban insurance tended to be more likely to report a history of Pap test compared with those with rural insurance or with no insurance. The successive the New Rural Cooperative Medical System (NRCMS), which had a low reimbursement level for outpatient services, was not initiated until 2002 [18]. In general, compared with the urban insurance system, NRCMS does not have standard reimbursement policies across different areas, and coverage rates for clinical preventive services and medicines are lower. In China, the shift to a market economy was accompanied by the disintegration of the rural communes in the 1980s, and the rural health insurance system based on the rural communes immediately became devoid [19]. Generally, outpatient costs (including examinations) are not covered, and only a part of inpatient hospital bills are compensated by the NRCMS. Few rural residents pay out-of-pocket for fees associated with screening test. However, most parts of outpatient and inpatient costs (including examinations) can be compensated by different kinds of urban insurances, although the reimbursement ratios are different in different provinces. Regular physical examinations are required for employees in many state organizations and companies (with the expense borne by the departments). Increasing the availability and participation of screening services in poor and rural areas is an important component of working toward increasing cervical cancer screening [20, 21].
Screening for precancerous lesions can be done in several ways including cervical cytology (Pap tests), visual inspection of the cervix with acetic acid (VIA), and testing for HPV DNA (self-collection, physician collection, or point-of-care test). Each of these methods has specific advantages, disadvantages, and health system requirements that countries should consider when planning screening programs [22]. Varied screening methods for cervical cancer have been explored in low- and middle-income countries where organized Pap test screening is neither affordable nor feasible [23, 24]. Currently, China does not have national screening guidelines or services for cervical cancer. Current screening in urban areas is opportunistic, and screening is less common in rural areas, where the burden is highest. In 2009, the Chinese Ministry of Finance, Ministry of Health, and the All China Women’s Federation jointly promoted the Free Examination Program among rural women, providing cervical and breast cancer screening in parts of selected areas, but not all. The technical solution of cervical cancer screening in the project concluded that most women should have Pap tests for cervical cancer every 3 years. For women with positive results of Pap test or VIA, colposcopy and biopsy are administered to confirm diagnosis, follow-up, and/or treatment. During 2009–2011, approximately 10 million women in rural areas were screened for cervical cancer using the Pap test or VIA in selected areas of China. However, there were approximately 350 million adult women who should have been screened in China [25]. As our study showed, the Pap test self-report rates were significantly lower among women with rural residence regardless of geographic region, suggesting that screening services must be made available to more women in rural areas. The Free Examination Program has been expanding to test 10 million rural women every year since 2012 [25]. The efficacy and effectiveness of such screening methods with good training and sustained quality assurance has been addressed by some randomized controlled trials in developing countries [26, 27].
In the latest WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention [28], experts recommend using the “screen-and-treat strategies.” New strategies for screening and treatment had to be considered to increase coverage in all countries and ultimately decrease cervical cancer incidence and mortality. Use of HPV screening and treatment strategy is superior to the VIA and treatment strategies and is better than that of cytology and colposcopy (with or without a biopsy) screening and treatment strategy. It is likely that a more sensitive and effective screening strategy for better prevention and early detection of cervical cancer could be implemented in China, including the concept that different tests may be more suitable for different areas. For the cervical cancer screening component, the Pap test or VIA (in relatively low-resource areas) are both provided. Recently, researchers found that HPV testing on self-collected cervical specimens may be a more effective means to screen for cervical cancer. This method may be effective in rural China, where there are shortages of cytopathologists and health care workers for screening by Pap test or VIA [29, 30]. A multicenter population-based study in China showed that HPV prevalence in the entire study population was 14.3%. Patterns of HPV prevalence differed by age, geographic region, and cytology findings. Researchers believed there was great potential for HPV vaccines, including types 16 and 18, to significantly decrease the cervical cancer burden in China [31].
Our study has many strengths. First, it is the largest nationwide and population-based assessment of self-reported history of Pap test for cervical cancer screening in China. The CCDRFS is the surveillance system that China plans to use to monitor the WHO global NCD framework indictors. Second, we included a nationwide sample of urban and rural areas selected from all 31 provinces, autonomous regions, and municipalities in China; this resulted in a nationwide study population. Third, the survey achieved a high response rate. Fourth, we were able to control for potential confounders in statistical analysis.
Our study has some limitations. First, to ensure adequate sample size, we used a replacement method when selected residents failed to take part in our survey. However, we used a strict replacement procedure, where only a household with a similar structure to the one originally sampled could be selected as a replacement. The overall sample replacement rate was 9.3%; therefore, we believe the impact of the replacement method on parameter estimations was minimal. A second limitation is that Pap test testing was self-reported and not obtained from actual medical records, and we assumed that the self-reported history of cytology testing was for cervical cancer screening and not for diagnosis of symptomatic disease. Another limitation is that the CCDRFS survey did not ask about history of VIA. The use of this cervical cancer screening method would have been more common in rural areas. This limitation may have partly accounted for the significantly lower likelihood of history of Pap test among women in rural areas if they received cervical cancer screening using VIA.
The key public health challenges for cervical cancer screening are ensuring availability of screening services, ensuring coverage, getting people to start screening, and linking them to follow-up and treatment. Geographic region by urban and rural residence, education level, and medical insurance status significantly influence the prevalence of self-reported Pap test in our study. Ensuring the availability and accessibility of high-quality cervical cancer screening services and designing promotional programs targeting rural women, those unemployed, and those without insurance are important components of a cervical cancer prevention and control program for adult Chinese women. In addition, educational interventions are needed to provide information and raise public awareness about the prevention of cervical cancer. Health care practitioners involved in cervical cancer screening program could be trained to take an active role in providing Chinese women with consistent and appropriate information about the importance of cervical screening to women’s health, as well as the risk factors associated with cervical cancer [32]. Successful strategies to increase participation in cervical cancer screening include organized programs with cost-reducing interventions (e.g., offering free tests and eliminating geographical barriers), a greater involvement of community health care workers, and tailored proactive communications that address barriers to screening [33]. However, suitable measures that are appropriate to the Chinese women at high risk need further exploration.
Conclusion
Our results highlight the urgent need to develop national cervical cancer screening guidelines and strategies that make screening services widely available, accessible, and acceptable to all women. Intensified efforts are needed to reach specific risk groups who reside in rural areas and those with no health insurance coverage.
Acknowledgments
This study was funded by the National Health and Family Planning Commission of the People’s Republic of China. We thank all study participants for taking part in this study. We are grateful to all staff members of the provincial and local health administrative departments and the provincial and county Centers for Disease Control and Prevention and the more than 2,000 field interviewers for their support and hard work. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author Contributions
Conception/Design: Baohua Wang, Minfu He, Ann Chao, Linhong Wang
Provision of study material or patients: Limin Wang
Collection and/or assembly of data: Baohua Wang, Limin Wang, Linhong Wang
Data analysis and interpretation: Baohua Wang, Minfu He, Ann Chao, Michael M. Engelgau, Mona Saraiya, Linhong Wang
Manuscript writing: Baohua Wang, Minfu He, Ann Chao, Mona Saraiya, Linhong Wang
Final approval of manuscript: Baohua Wang, Minfu He, Ann Chao, Michael M. Engelgau, Mona Saraiya, Limin Wang, Linhong Wang
Disclosures
The authors indicated no financial relationships.
References
- 1.He J, Chen WQ. 2012 Chinese Cancer Registry Annual Report. Beijing, China. Beijing, People’s Republic of China: Military Medical Science Press; 2012. [Google Scholar]
- 2.World Health Organization . National Cancer Control Programmes: Policies and Managerial Guidelines. 2nd ed. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 3.World Health Organization (WHO) WHO Guidance Note: Comprehensive Cervical Cancer Prevention and Control: A Healthier Future for Girls and Women. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 4.Yang G, Hu J, Rao KQ, et al. Mortality registration and surveillance in China: History, current situation and challenges. Popul Health Metr. 2005;3:3. doi: 10.1186/1478-7954-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou MG, Jiang Y, Huang ZJ, et al. Adjustment and representativeness evaluation of national disease surveillance points system [in Chinese] Dis Surveill. 2010;25:239–244. [Google Scholar]
- 6.National Center for Chronic and Noncommunicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention . Report on Chronic Disease and Risk Factor Surveillance in China 2010 [in Chinese] Beijing, People’s Republic of China: Military Medical Science Press; 2012. [Google Scholar]
- 7.Wang BH, He MF, Wang LM, et al. Breast cancer screening among adult women in China, 2010. Prev Chronic Dis. 2013;10:130136. doi: 10.5888/pcd10.130136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao EF, Bao L, Li C, et al. Changes in epidemiology and clinical characteristics of cervical cancer over the past 50 years [in Chinese] J First Mil Med Univ. 2005;25:605–609. [PubMed] [Google Scholar]
- 9.World Health Organization (WHO). United Nations High-Level Meeting on Noncommunicable Disease Prevention and Control. Available at http://www.who.int/nmh/events/un_ncd_summit2011/en/. Accessed January 6, 2014.
- 10.International Agency for Research on Cancer (IARC) Cervix Cancer Screening. Vol 10. Lyon, France: IARC Press; 2005. [Google Scholar]
- 11.Jin XW, Lipold L, McKenzie M, et al. Cervical cancer screening: What’s new and what’s coming? Cleve Clin J Med. 2013;80:153–160. doi: 10.3949/ccjm.80a.12092. [DOI] [PubMed] [Google Scholar]
- 12.Chen YC, Tang SC, Le H, et al. Compare health development of rural areas in different districts of China: About social economy and inhabitant’s health condition [in Chinese] Chinese Health Economics. 2006;25:37–38. [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC) Cancer screening: United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:41–45. [PubMed] [Google Scholar]
- 14.Lee M, Chang HS, Park EC, et al. Factors associated with participation of Korean women in cervical cancer screening examination by age group. Asian Pac J Cancer Prev. 2011;12:1457–1462. [PubMed] [Google Scholar]
- 15.Lin SJ. Factors influencing the uptake of screening services for breast and cervical cancer in Taiwan. J R Soc Promot Health. 2008;128:327–334. doi: 10.1177/1466424007092802. [DOI] [PubMed] [Google Scholar]
- 16.Ulijaszek SJ. Socio-economic status, forms of capital and obesity. J Gastrointest Cancer. 2012;43:3–7. doi: 10.1007/s12029-012-9366-5. [DOI] [PubMed] [Google Scholar]
- 17.Kottke TE, Isham GJ. Measuring health care access and quality to improve health in populations. Prev Chronic Dis. 2010;7:A73. [PMC free article] [PubMed] [Google Scholar]
- 18.Feng X, Tang S, Bloom G, et al. Cooperative medical schemes in contemporary rural China. Soc Sci Med. 1995;41:1111–1118. doi: 10.1016/0277-9536(94)00417-r. [DOI] [PubMed] [Google Scholar]
- 19.Yu B, Meng Q, Collins C, et al. How does the New Cooperative Medical Scheme influence health service utilization?: A study in two provinces in rural China. BMC Health Serv Res. 2010;10:116. doi: 10.1186/1472-6963-10-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qian D, Pong RW, Yin A, et al. Determinants of health care demand in poor, rural China: The case of Gansu Province. Health Policy Plan. 2009;24:324–334. doi: 10.1093/heapol/czp016. [DOI] [PubMed] [Google Scholar]
- 21.Tang S, Meng Q, Chen L, et al. Tackling the challenges to health equity in China. Lancet. 2008;372:1493–1501. doi: 10.1016/S0140-6736(08)61364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saslow D, Runowicz CD, Solomon D, et al. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. CA Cancer J Clin. 2002;52:342–362. doi: 10.3322/canjclin.52.6.342. [DOI] [PubMed] [Google Scholar]
- 23.Gaffikin L, Blumenthal PD, Emerson M, et al. Safety, acceptability, and feasibility of a single-visit approach to cervical-cancer prevention in rural Thailand: A demonstration project. Lancet. 2003;361:814–820. doi: 10.1016/s0140-6736(03)12707-9. [DOI] [PubMed] [Google Scholar]
- 24.Denny L, Kuhn L, De Souza M, et al. Screen-and-treat approaches for cervical cancer prevention in low-resource settings: A randomized controlled trial. JAMA. 2005;294:2173–2181. doi: 10.1001/jama.294.17.2173. [DOI] [PubMed] [Google Scholar]
- 25.National Health and Family Planning Commission of the People’s Republic of China. The Technical Solution of Cervical Cancer Screening for Chinese Rural Women 2009 [in Chinese]. Available at http://www.nhfpc.gov.cn/fys/s3581/200909/ 53c0839f88f74bb0966d8c75d7304d2c.shtml. Accessed January 6, 2014.
- 26.Sankaranarayanan R, Nene BM, Dinshaw KA, et al. A cluster randomized controlled trial of visual, cytology and human papillomavirus screening for cancer of the cervix in rural India. Int J Cancer. 2005;116:617–623. doi: 10.1002/ijc.21050. [DOI] [PubMed] [Google Scholar]
- 27.Sankaranarayanan R, Esmy PO, Rajkumar R, et al. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India: A cluster-randomised trial. Lancet. 2007;370:398–406. doi: 10.1016/S0140-6736(07)61195-7. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization (WHO). WHO Guidelines for Screening and Treatment of Precancerous Lesions for Cervical Cancer Prevention 2013. Available at http://www.who.int/reproductivehealth/topics/cancers/en/index.html. Accessed January 9, 2015. [PubMed]
- 29.Zhao FH, Lewkowitz AK, Chen F, et al. Pooled analysis of a self-sampling HPV DNA test as a cervical cancer primary screening method. J Natl Cancer Inst. 2012;104:178–188. doi: 10.1093/jnci/djr532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao FH, Tiggelaar SM, Hu SY, et al. A multi-center survey of age of sexual debut and sexual behavior in Chinese women: Suggestions for optimal age of human papillomavirus vaccination in China. Cancer Epidemiol. 2012;36:384–390. doi: 10.1016/j.canep.2012.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu EQ, Liu B, Cui JF, et al. Prevalence of type-specific human papillomavirus and pap results in Chinese women: A multi-center, population-based cross-sectional study. Cancer Causes Control. 2013;24:795–803. doi: 10.1007/s10552-013-0162-8. [DOI] [PubMed] [Google Scholar]
- 32.Gu C, Chan CW, Twinn S. How sexual history and knowledge of cervical cancer and screening influence Chinese women’s screening behavior in mainland China. Cancer Nurs. 2010;33:445–453. doi: 10.1097/NCC.0b013e3181e456dc. [DOI] [PubMed] [Google Scholar]
- 33.Spadea T, Bellini S, Kunst A, et al. The impact of interventions to improve attendance in female cancer screening among lower socioeconomic groups: A review. Prev Med. 2010;50:159–164. doi: 10.1016/j.ypmed.2010.01.007. [DOI] [PubMed] [Google Scholar]