The association between financial distress and quality of life in patients with advanced cancer treated at a comprehensive cancer center were compared with that of patients treated at a general hospital, as was the frequency of financial distress and its correlates. Financial distress occurred very frequently in both groups, but the median intensity of financial distress among patients treated at the general public hospital was significantly greater than that of patients treated at the cancer center.
Keywords: Financial distress, Advanced cancer, Quality of life
Abstract
Objective.
There are limited data on the effects of financial distress (FD) on overall suffering and quality of life (QOL) of patients with advanced cancer (AdCa). In this cross-sectional study, we examined the frequency of FD and its correlates in AdCa.
Patients and Methods.
We interviewed 149 patients, 77 at a comprehensive cancer center (CCC) and 72 at a general public hospital (GPH). AdCa completed a self-rated FD (subjective experience of distress attributed to financial problems) numeric rating scale (0 = best, 10 = worst) and validated questionnaires assessing symptoms (Edmonton Symptom Assessment System [ESAS]), psychosocial distress (Hospital Anxiety and Depression Scale [HADS]), and QOL (Functional Assessment of Cancer Therapy-General [FACT-G]).
Results.
The patients’ median age was 60 years (95% confidence interval [CI]: 58.6–61.5 years); 74 (50%) were female; 48 of 77 at CCC (62%) versus 13 of 72 at GPH (18%) were white; 21 of 77 (27%) versus 32 of 72 (38%) at CCC and GPH, respectively, were black; and 7 of 77 (9%) versus 27 of 72 (38%) at CCC and GPH, respectively, were Hispanic (p < .0001). FD was present in 65 of 75 at CCC (86%; 95% CI: 76%–93%) versus 65 of 72 at GPH (90%; 95% CI: 81%–96%; p = .45). The median intensity of FD at CCC and GPH was 4 (interquartile range [IQR]: 1–7) versus 8 (IQR: 3–10), respectively (p = .0003). FD was reported as more severe than physical distress, distress about physical functioning, social/family distress, and emotional distress by 45 (30%), 46 (31%), 64 (43%), and 55 (37%) AdCa, respectively (all significantly worse for patients at GPH) (p < .05). AdCa reported that FD was affecting their general well-being (0 = not at all, 10 = very much) with a median score of 5 (IQR: 1–8). FD correlated (Spearman correlation) with FACT-G (r = −0.23, p = .0057); HADS-anxiety (r = .27, p = .0014), ESAS-anxiety (r = .2, p = .0151), and ESAS-depression (r = .18, p = .0336).
Conclusion.
FD was very frequent in both groups, but median intensity was double among GPH patients. More than 30% of AdCa rated FD to be more severe than physical, family, and emotional distress. More research is needed to better characterize FD and its correlates in AdCa and possible interventions.
Implications for Practice:
Financial distress is an important and common factor contributing to the suffering of advanced cancer patients and their caregivers. It should be suspected in patients with persistent, refractory symptom expression. Early identification, measurement, and documentation will allow clinical teams to develop interventions to improve financial distress and its impact on quality of life of advanced cancer patients.
Introduction
Twenty-five percent to 50% of all cancer patients report significant levels of distress, and it is frequently not assessed nor detected by health professionals [1]. Advanced cancer has an adverse effect in virtually all dimensions of patients’ lives, including physical, psychosocial, spiritual, familial, and role function. Cancer’s least-explored effects include its impact on personal finances and the contribution of financial distress to the overall quality of life. Financial issues have been found to be the second most frequent source of distress identified by cancer patients in a community cancer center context (22%) [1].
A substantial proportion of cancer patients and their families might experience adverse financial events during the trajectory of the illness [2]. Factors that influence these events include increased direct out-of-pocket expenses related to cancer diagnosis [2], and costs associated with purchasing new clothes because of weight fluctuations, changes in diet and nutritional supplements needed during treatment, home- or childcare [3, 4], and increased utility bills and loss of income secondary to decline functional status [2, 4], among others. In view of continuously increasing health-care costs, the frequency of health care-related financial problems will likely to continue to rise [5]. Patients with advanced cancer may be particularly susceptible to financial distress, given the increased costs of recently developed diagnostic procedures and therapies (e.g., targeted therapies); increased survival, which expands the time frame of expenditures; and the difficulties in generating and/or increasing income in the context of a severely debilitating disease. Many cancer patients make a wide range of financial adjustments to cope with out-of-pocket costs and changes in income they experience postdiagnosis [6]. The extent of financial adjustments needed varies, but extreme measures such as house repossessions [7] and home refinancing [8] have been reported in both the U.S. and the U.K. Forgoing treatment and rationing of medications because of cost have also been reported [9–12]. Insured patients undergoing cancer treatment and seeking copayment assistance can experience a considerable subjective financial burden, and they may alter their care because of high out-of-pocket expenses [13].
The relative contributions of adverse financial events to overall distress in patients with advanced cancer are not well understood. The severity of financial distress in patients with advanced cancer and the relationship between financial distress and physical, psychosocial, spiritual, or family distress and overall quality of life have not been well characterized in the literature. One study showed an inverse association between increased financial difficulties and quality of life [14].
For this study, financial distress was defined as the distress attributed by the patient to the financial burden within the past month. Financial burden, for this study, was defined as the percentage of total family income spent on direct out-of-pocket expenditures in health care during the last month, without considering health insurance [8, 15, 16].
The assessment of the impact of financial distress on overall suffering and quality of life in patients with advanced cancer and the identification of possible associations and explanations is of paramount importance. Unfortunately, patient financial distress is not systematically assessed, and, therefore, opportunities are missed to relieve and prevent financial suffering.
The primary objective of our study was to determine the association between financial distress and quality of life in patients with advanced cancer in a comprehensive cancer center and a general public hospital. The secondary objectives were to characterize the frequency and intensity of financial distress in patients with advanced cancer and determine the association between financial distress, cancer-related symptom burdens, patient characteristics, socioeconomic status, quality of life, and subjective class identification.
Patients and Methods
This was a cross-sectional survey of 149 patients in the outpatient Supportive Care Center at a comprehensive cancer center (CCC) and at a general public hospital (GPH) (supportive care clinic and general oncology clinic) in Texas. The patients completed the survey at the time of their initial consultation or follow-up visit. No compensation was provided to participate in the study. The study was approved by the institutional review board of The University of Texas MD Anderson Cancer Center.
Patients older than 18 years with advanced breast, colon, lung, or prostate cancer, and with normal cognition were included. Advanced cancer was defined as one of the following: recurrent disease, had received more than two lines of chemotherapy, locally advanced disease, metastatic disease, or refractory disease. Informed consent was obtained for those patients interested in participation.
We collected demographics and clinical information from each patient, including symptom burden according to the Edmonton Symptom Assessment System (ESAS); Hospital Anxiety Depression Scale (HADS); the Functional Assessment of Cancer Therapy and Functional Assessment of Chronic Illness Therapy-General (FACT-G), to assess quality of life and spirituality; Socioeconomic Status Instrument (SESI); and the Multidimensional Scale of Perceived Social Support (MSPSS). For this investigation, we defined financial distress as the subjective experience of distress attributed by the patient to financial problems on a numeric rating scale, with 0 being best or not present and 10 being worst.
Survey Instruments
We used the following validated survey instruments. ESAS measures the occurrence of 10 symptoms in the 24 hours preceding the taking of the questionnaire: pain, fatigue, nausea, depression, anxiety, drowsiness, shortness of breath, appetite, sleep, and feeling of well-being. This questionnaire has been validated in cancer populations [17]. For this study, we added an item assessing spiritual pain.
The Socioeconomic Status Instrument is a 13-item scale with 9 items documented directly by patients and 3 documented by the research personnel. It has been validated in cancer patients, showing good validity and reliability (overall Cronbach α coefficient was 0.78) [18].
The Hospital Anxiety Depression Scale is a 14-item scale with separate subscales for anxiety and depression validated in cancer patients for depression and anxiety assessment [19]. It can be administered or used as a self-assessment tool. A score of 16 or higher is suggestive of a severe case of anxiety or depression [20].
FACT-G (version 4) is a widely used measure of quality of life and constitutes the core of the Functional Assessment of Chronic Illness Therapy. FACT-G comprises 27 questions that assess well-being in four domains: physical symptoms, participation in and enjoyment of normal daily activities, social support and communication, and mood and emotional response to illness—the physical, functional, social/family, and emotional domains, respectively. The scores for the individual domains are summed to obtain a total quality-of-life score. Both the total score and the individual subscale scores have good internal reliability (α = 0.72–0.85), and the instrument has been validated in cancer patients [21].
The 12-item MSPSS measures perceived adequacy of social support from family, friends, and a significant other. Ratings are made on a seven-point Likert scale ranging from “very strongly disagree” to “very strongly agree.” Although MSPSS was initially tested in a narrow undergraduate-student population, several further studies found that the MSPSS is psychometrically sound in diverse populations and has good internal reliability, test-retest reliability, and strong factorial validity. Cronbach α for the MSPSS has been reported to be 0.93. The α coefficients for the family, friends, and significant-other subscales have been reported to be 0.91, 0.89, and 0.91, respectively. Comparable coefficients have been obtained for race/sex subgroups [22–24].
The patients were also asked to rate from “strongly agree” to “strongly disagree” statements related to the impact of financial distress on their physical distress, physical functioning, social/family distress, spiritual distress, and emotional distress. The statements were considered positive when the patient responded “strongly agree, agree or somewhat agree.”
We also conducted an exploratory measurement and analysis of different subjective terms to determine the association between those patient-reported terms and financial distress. The questions the patients were asked to rate from 0 (absent) to 10 (worst possible) the following terms: “subjective financial burden,” “financial concerns,” “financial difficulties,” and “financial worries.” At the time of this study, there was no validated tool for the determination of financial distress or another term from the perspective of the patients.
Statistical Considerations and Analysis
A sample of 149 patients was necessary to allow detection of Pearson’s correlation between financial distress and quality of life as small as 0.232 with 80% power and a 5% type I error rate. We quantified the frequency and intensity of financial distress and determined 95% confidence intervals. We also estimated the Pearson’s correlation between financial distress and other variables for both the CCC subgroup and the GPH subgroup. The association between financial distress and quality of life was assessed by calculating the Spearman correlation for the two measures and then testing the correlation against the null hypothesis. All tests were two-sided, and p values less than .05 were considered statistically significant. Analyses were performed using SAS software version 9.2 (SAS Institute Inc., Cary, NC, http://www.sas.com).
Results
Patient characteristics are listed in Table 1. The median age was 60 years (95% confidence interval [CI]: 58.6–61.5 years). Seventy-four of the 149 patients (50%) were female. Seventy-eight patients (52%) were married. The distribution of race/ethnicity differed significantly (Fisher’s exact test, p < .0001) between the CCC and GPH patients: 62% of the 77 patients at the CCC and 18% of the 72 patients at the GPH were white; 27% and 38% were black, respectively; and 9% and 38% were Hispanic, respectively.
Table 1.
Advanced cancer patients’ characteristics
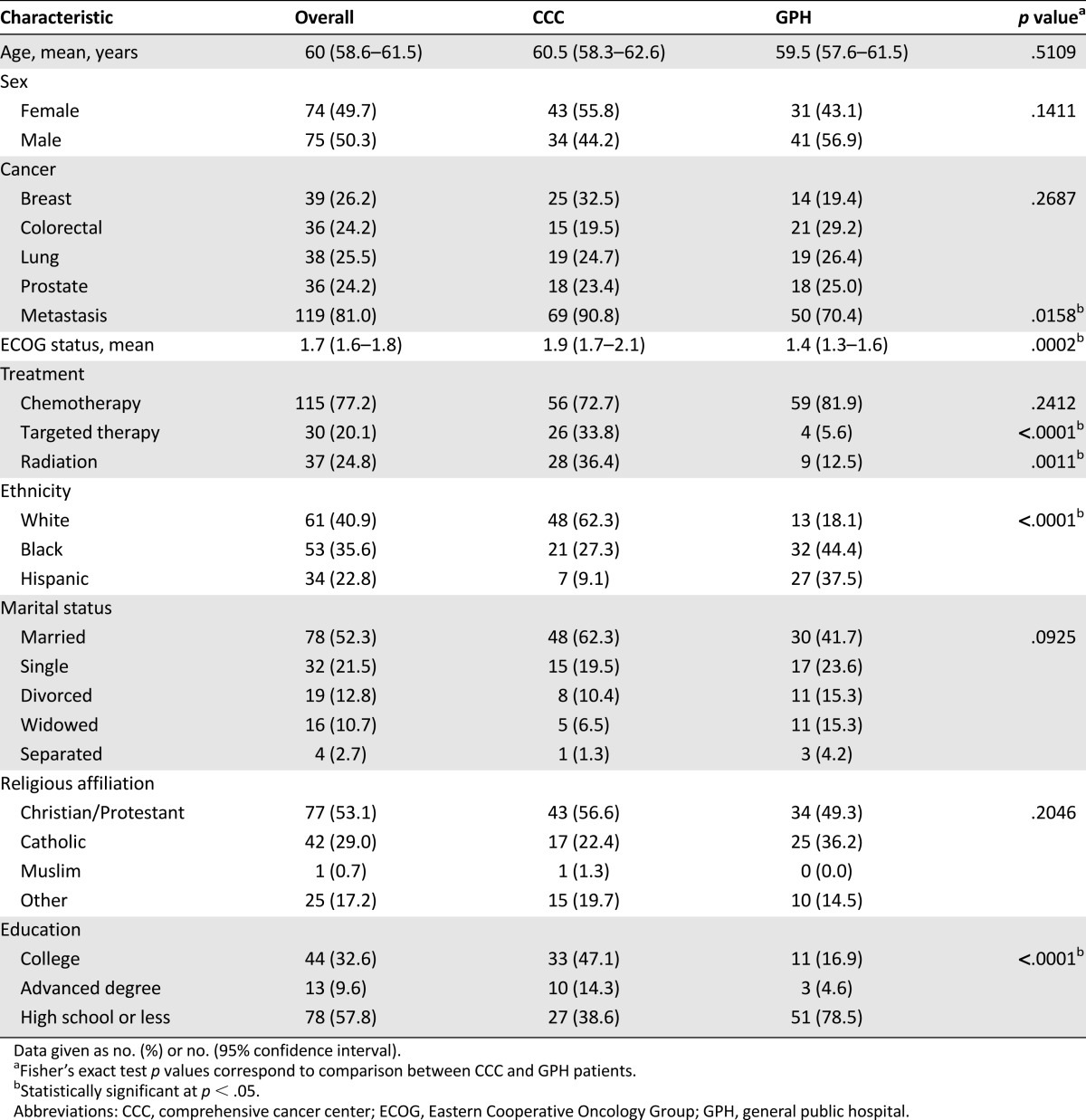
Education levels differed significantly (Fisher’s exact test, p < .0001) between the CCC and GPH patients: 58% and 19%, respectively, had a college education or an advanced degree. The median monthly income was $3,000 (interquartile range [IQR]: $1,400–$7,000) for CCC patients and $940 (IQR: $350–$1,300) for GPH patients (p = .0017). Of the total 149 patients, 51% self-reported as being middle class before cancer diagnosis and 39% self-reported as being middle class at the time of the study (p < .0001).
Financial distress was present in 65 of 75 patients at CCC (86%; 95% confidence interval: 76%–93%) versus 65 of 72 patients at GPH (90%; 95% confidence interval: 81%–96%; p = .45). The median intensity score of financial distress (FD) at CCC and GPH was 4 (IQR: 1–7) versus 8 (3–10), respectively (p = .0003).
Table 2 lists the data on the impact of financial distress relative to the impact of physical distress, distress in physical functioning, social/family distress, and emotional distress. Financial distress was reported as “strongly agree,” “agree,” or “somewhat agree” significantly more often for GPH patients than for CCC patients for the following outcomes: social/family distress (Fisher’s exact test, p = .0085) and emotional distress (Fisher’s exact test, p = .0411). We found that advanced cancer patients reported that the presence of financial distress was significantly associated with general well-being (0 = not at all, 10 = very much) with a median score of 5 (IQR: 1–8).
Table 2.
Perception of the impact of financial distress on other clinical problems among advanced cancer patients
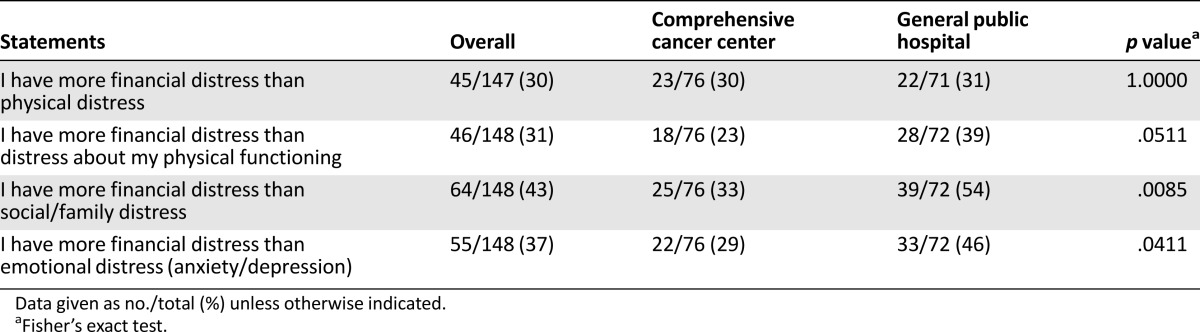
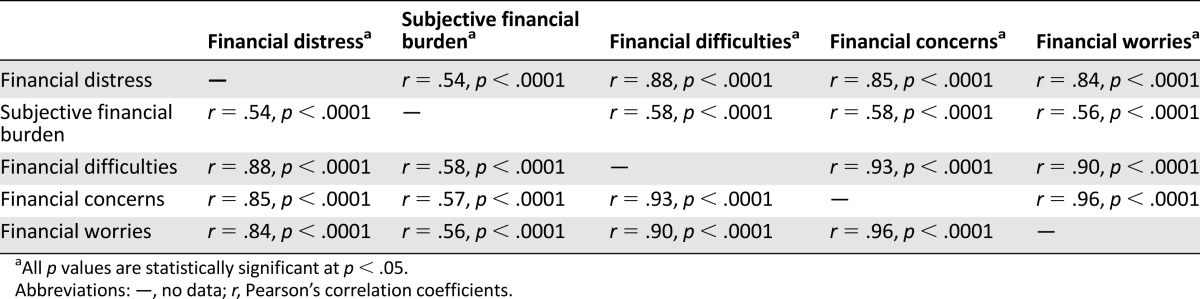
Table 3 lists Spearman coefficients of correlation between financial distress and quality of life (FACT-G, r = −0.23, p = .005), anxiety (Hospital Anxiety and Depression Scale, r = .27, p = .001; ESAS-anxiety, r = .20, p = .01), depression (ESAS-depression; r = .18, p = .03), subjective financial burden (r = −0.53, p < .0001), total social support (MSPSS, r = −0.17, p = .04), and annual household income (Socioeconomic Status Instrument, r = −0.45, p < .0001). Multivariate analysis showed independent correlation between financial distress and ESAS-anxiety for the CCC group (r = .63, p = .04), and for FACT-G and ESAS-appetite for the GPH group (r = −0.10, p = .002; and r = −41, p = .03, respectively). Table 4 shows the associations between patient-reported financial distress and other subjective terms, including subjective financial burden (r = .54, p < .0001); self-rated financial difficulties (r = .88, p < .0001); self-rated financial concerns (r = .85, p < .0001); and self-rated financial worries (r = .84, p < .0001).
Table 3.
Correlation between financial distress and clinical and economic variables
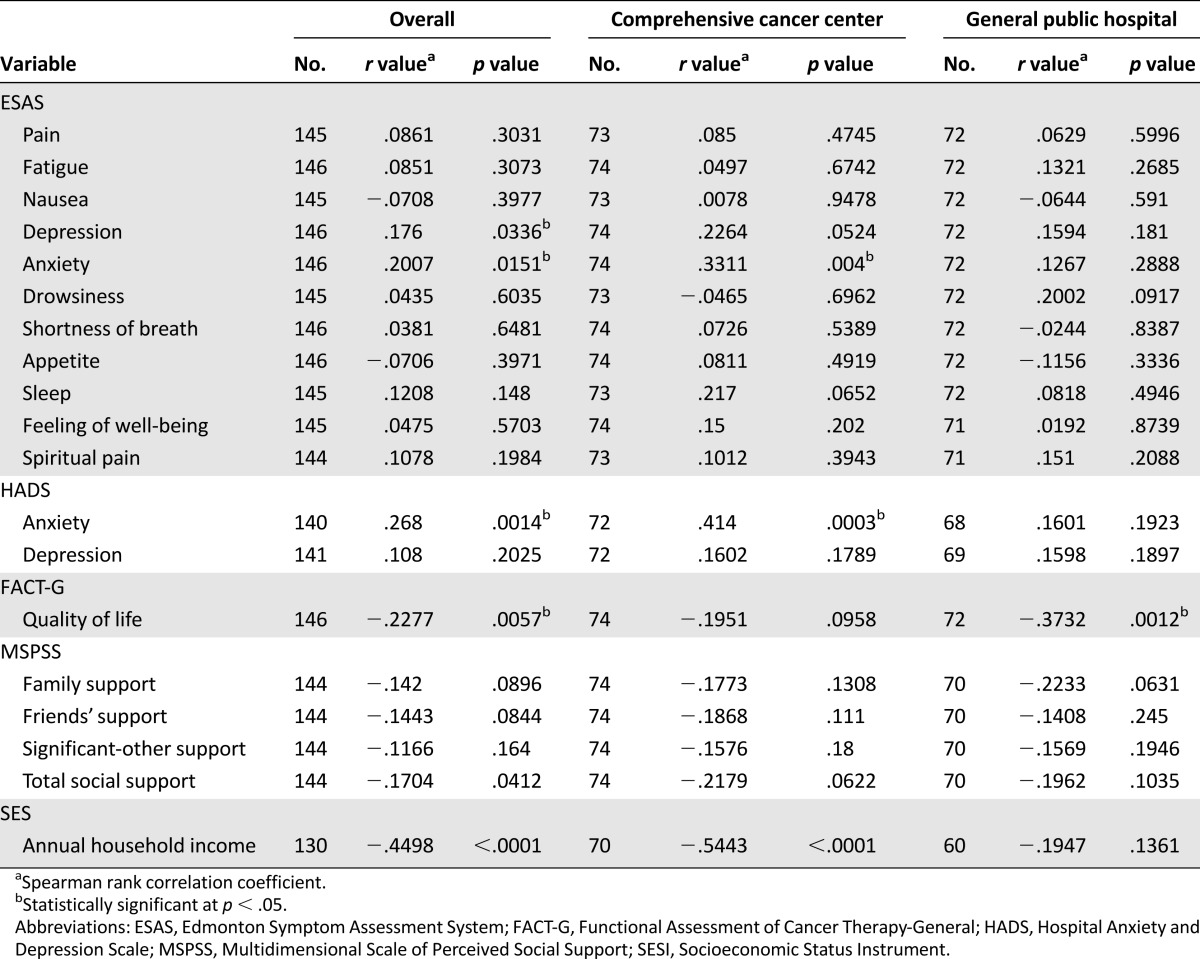
Table 4.
Associations between patient-reported financial distress and other subjective terms.
Discussion
The main purpose of our study was to measure the frequency and severity of subjective perception of financial distress among patients with advanced cancer who were referred to a palliative care service. Financial distress is rarely reported or even measured in clinical care, especially in patients with advanced and terminal illness with severe burden and distress secondary to symptoms and treatments. Financial distress can affect many facets of life, including patients’ financial well-being and general quality of life. Our findings showed that a high proportion of our advanced cancer patients said they had high frequency and intensity of financial distress; these were significantly associated with anxiety, depression, and quality of life. These elements are part of a phenomenon that has been named financial toxicity [25]. Self-reported financial distress or subjective financial burden has been previously reported in patients with cancer. Chino et al. reported that 47% of patients with cancer diagnosis expressed significant/catastrophic, self-reported financial burden and worse general satisfaction with their medical care [26]. Sharp et al. [27] used National Cancer Registry Ireland data to show that cancer-related financial stress and strain were consistently associated with increased risk for adverse psychological outcomes. For example, the risk for depression was three times higher in patients reporting high levels of cancer-related financial stress and strain.
In agreement with the previously reported finding that the effect of social support was strongest at high levels of financial stress [28], we found that social support was negatively associated with the presence of financial distress. It is possible that the presence of social support makes patients hopeful that they will receive care from their loved ones even in the presence of financial difficulties.
The finding that many patients perceived financial distress as being more severe than physical, emotional, and spiritual distress is concerning, since the vast majority of the instruments aimed at determining symptom distress and quality of life do not include a financial distress item. Our findings suggest that measuring the impact of financial distress as one of component of quality of life, together with physical, emotional, and spiritual distress, is important. Another important point is that clinicians should explore more in detail the presence of financial distress in patients who consistently report a high level of physical, spiritual, and emotional distress.
Our population perceived that financial distress was more severe than physical distress, distress about physical functioning, social/family distress, and emotional distress. Others have reported that financial distress can be associated with nonadherence to prescribed medications [29] and poor overall patient satisfaction [26].
Comparing different studies on the effects of financial distress can be difficult when different terms are used to refer to the same concept. The lack of a common definition of financial distress is a challenge. Nevertheless, our finding that the self-rated variables financial difficulties, financial concerns, and financial worries were all significantly correlated with financial distress indicates that these variables likely measured the same concept. This finding is reassuring because it implies that patients interpret these terms in a concordance fashion, but more research is needed to better define the best way to evaluate subjective perception of financial distress.
In contrast to the lack of a common definition of financial distress, there is some concordance in the literature on the definition of objective financial burden as the ratio of total out-of-pocket spending on health-care services and premiums to total family income [8, 15, 16]. Recent literature has highlighted some limitations of the use of objective definitions of financial burden [30]. This has been specifically addressed in the context of establishing a relationship between financial burden and mental health issues; some authors argue that subjective factors such as feelings of subjective deprivation or subjective social class identification predict psychological well-being independently of objective financial burden. This relationship is probably explained by the lower self-esteem and the lower sense of control over life that people who experience this subjective feeling have [30, 31]. Not all patients experience the same objective and subjective financial burden; certain subgroups of the population are at higher risk for paying more out of pocket. In a study of patients receiving chemotherapy for colorectal cancer, younger patients and those with lower household income were predisposed to experience greater financial burden [32]. In addition, other sociodemographic characteristics, including type of insurance, race, marital status, education, geographic location, and comorbidity, all contribute to higher out-of-pocket expenses [32, 33]. Another factor is the place where the health care is delivered, either public or private settings [33]. Further research is needed to evaluate these aspects in patients with advanced cancer and other chronic illnesses.
Some tools, such as the Comprehensive Score for Financial Toxicity [34], and strategies to correctly assess these domains will help us better understand what is happening to our patients and identify possible interventions to ease their suffering and improve their quality of life. The content validity and internal consistency of this tool were reported in a study of 155 advanced cancer patients. More research needs to be done to validate it in larger samples and other settings. Our study had been completed already by the time this tool was published.
This study is not without limitations. Because we used a cross-sectional study design, the causal relationships between financial distress and other factors related cannot be considered. More research is needed to address the possible causality and fluctuations in intensity and frequency during the trajectory of the illness. Also, we cannot generalize our results, since only two institutions were involved; further studies would need to be developed at a higher scale, including private and public hospitals.
Our results strongly support that financial distress should be regularly measured in all patients with advanced illness attending to supportive/palliative care services. Expressive supportive counseling for financial distress as a component of overall emotional distress and psycho-educational interventions to help patients address financial problems should be part of health-care strategies among supportive and palliative care teams. The regular measurement and documentation of financial distress will allow clinical teams to test interventions aimed at reducing the overall impact of financial distress on quality of life.
Conclusion
In summary, financial distress was very common in both hospital groups, but the severity of financial distress in GPH patients was double the severity of financial distress in CCC patients. Financial distress was associated with anxiety, depression, and poor quality of life. More than 30% of the patients rated financial distress as more severe than physical, family, and emotional distress. Additional research is needed to confirm these associations and to develop effective interventions for cancer patients who experience financial distress.
Acknowledgments
Eduardo Bruera is supported, in part, by the National Institutes of Health (Grants R01NR010162-01A1, R01CA122292-01, and R01CA124481-01).
Author Contributions
Conception/Design: Marvin Delgado-Guay, Jeanette Ferrer, Alyssa G. Rieber, Wadih Rhondali, Gary Chisholm, Janet Williams, Susan Frisbee-Hume, Eduardo Bruera
Provision of study material or patients: Marvin Delgado-Guay, Jeanette Ferrer, Alyssa G. Rieber, Wadih Rhondali, Supakarn Tayjasanant, Jewel Ochoa, Hilda Cantu, Susan Frisbee-Hume, Eduardo Bruera
Collection and/or assembly of data: Marvin Delgado-Guay, Jewel Ochoa, Hilda Cantu, Janet Williams, Eduardo Bruera
Data analysis and interpretation: Marvin Delgado-Guay, Supakarn Tayjasanant, Gary Chisholm, Janet Williams, Susan Frisbee-Hume, Eduardo Bruera
Manuscript writing: Marvin Delgado-Guay, Jeanette Ferrer, Alyssa G. Rieber, Supakarn Tayjasanant, Gary Chisholm, Eduardo Bruera
Final approval of manuscript: Marvin Delgado-Guay, Jeanette Ferrer, Alyssa G. Rieber, Wadih Rhondali, Supakarn Tayjasanant, Jewel Ochoa, Hilda Cantu, Gary Chisholm, Janet Williams, Susan Frisbee-Hume, Eduardo Bruera
Disclosures
Alyssa G. Rieber: Steris Corporation (E [spouse]). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.Kendall J, Glaze K, Oakland S, et al. What do 1281 distress screeners tell us about cancer patients in a community cancer center? Psychooncology. 2011;20:594–600. doi: 10.1002/pon.1907. [DOI] [PubMed] [Google Scholar]
- 2.Stommel M, Given CW, Given BA. The cost of cancer home care to families. Cancer. 1993;71:1867–1874. doi: 10.1002/1097-0142(19930301)71:5<1867::aid-cncr2820710525>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 3.Brooks J, Wilson K, Amir Z. Additional financial costs borne by cancer patients: A narrative review. Eur J Oncol Nurs. 2011;15:302–310. doi: 10.1016/j.ejon.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Longo CJ, Deber R, Fitch M, et al. An examination of cancer patients’ monthly ‘out-of-pocket’ costs in Ontario, Canada. Eur J Cancer Care (Engl) 2007;16:500–507. doi: 10.1111/j.1365-2354.2007.00783.x. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham PJ. The growing financial burden of health care: national and state trends, 2001-2006. Health Aff (Millwood) 2010;29:1037–1044. doi: 10.1377/hlthaff.2009.0493. [DOI] [PubMed] [Google Scholar]
- 6.Timmons A, Gooberman-Hill R, Sharp L. “It’s at a time in your life when you are most vulnerable”: A qualitative exploration of the financial impact of a cancer diagnosis and implications for financial protection in health. PLoS One. 2013;8:e77549. doi: 10.1371/journal.pone.0077549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amir Z, Wilson K, Hennings J, et al. The meaning of cancer: Implications for family finances and consequent impact on lifestyle, activities, roles and relationships. Psychooncology. 2012;11:1167–1174. doi: 10.1002/pon.2021. [DOI] [PubMed] [Google Scholar]
- 8.Shankaran V, Jolly S, Blough D, et al. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: A population-based exploratory analysis. J Clin Oncol. 2012;30:1608–1614. doi: 10.1200/JCO.2011.37.9511. [DOI] [PubMed] [Google Scholar]
- 9.Bradley S, Sherwood PR, Donovan HS, et al. I could lose everything: Understanding the cost of a brain tumor. J Neurooncol. 2007;85:329–338. doi: 10.1007/s11060-007-9425-0. [DOI] [PubMed] [Google Scholar]
- 10.Mathews M, Buehler S, West R. Perceptions of health care providers concerning patient and health care provider strategies to limit out-of-pocket costs for cancer care. Curr Oncol. 2009;16:3–8. doi: 10.3747/co.v16i4.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Markman M, Luce R. Impact of the cost of cancer treatment: An Internet-based survey. J Oncol Pract. 2010;6:69–73. doi: 10.1200/JOP.091074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weaver KE, Rowland JH, Alfano CM, et al. Parental cancer and the family: A population-based estimate of the number of US cancer survivors residing with their minor children. Cancer. 2010;116:4395–4401. doi: 10.1002/cncr.25368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: A pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. The Oncologist. 2013;18:381–390. doi: 10.1634/theoncologist.2012-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta D, Lis CG, Grutsch JF. Perceived cancer-related financial difficulty: Implications for patient satisfaction with quality of life in advanced cancer. Support Care Cancer. 2007;15:1051–1056. doi: 10.1007/s00520-007-0214-2. [DOI] [PubMed] [Google Scholar]
- 15.Banthin JS, Cunningham P, Bernard DM. Financial burden of health care, 2001-2004. Health Aff (Millwood) 2008;27:188–195. doi: 10.1377/hlthaff.27.1.188. [DOI] [PubMed] [Google Scholar]
- 16.Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients’ families. JAMA. 1994;272:1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 17.Bruera E, Kuehn N, Miller MJ, et al. The Edmonton Symptom Assessment System (ESAS): A simple method for the assessment of palliative care patients. J Palliat Care. 1991;7:6–9. [PubMed] [Google Scholar]
- 18.Cyrus-David M. The validity and reliability of the Socioeconomic Status Instrument for assessing prostate cancer patients. Cancer Epidemiol. 2010;34:382–387. doi: 10.1016/j.canep.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 19.Lloyd-Williams M, Spiller J, Ward J. Which depression screening tools should be used in palliative care? Palliat Med. 2003;17:40–43. doi: 10.1191/0269216303pm664oa. [DOI] [PubMed] [Google Scholar]
- 20.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 21.Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: Properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79. doi: 10.1186/1477-7525-1-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Canty-Mitchell J, Zimet GD. Psychometric properties of the Multidimensional Scale of Perceived Social Support in urban adolescents. Am J Community Psychol. 2000;28:391–400. doi: 10.1023/A:1005109522457. [DOI] [PubMed] [Google Scholar]
- 23.Zimet GD, Dahlem NW, Zimet SG, et al. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52:30–41. [Google Scholar]
- 24.Zimet GD, Powell SS, Farley GK, et al. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 25.Ubel PA, Abernethy AP, Zafar SY. Full disclosure—out-of-pocket costs as side effects. N Engl J Med. 2013;369:1484–1486. doi: 10.1056/NEJMp1306826. [DOI] [PubMed] [Google Scholar]
- 26.Chino F, Peppercorn J, Taylor DH, Jr, et al. Self-reported financial burden and satisfaction with care among patients with cancer. The Oncologist. 2014;19:414–420. doi: 10.1634/theoncologist.2013-0374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sharp L, Carsin A-E, Timmons A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psychooncology. 2013;22:745–755. doi: 10.1002/pon.3055. [DOI] [PubMed] [Google Scholar]
- 28.Aslund C, Larm P, Starrin B, et al. The buffering effect of tangible social support on financial stress: Influence on psychological well-being and psychosomatic symptoms in a large sample of the adult general population. Int J Equity Health. 2014;13(1):85. doi: 10.1186/s12939-014-0085-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zullig LL, Peppercorn JM, Schrag D, et al. Financial distress, use of cost-coping strategies, and adherence to prescription medication among patients with cancer. J Oncol Pract. 2013;9:60s–63s. doi: 10.1200/JOP.2013.000971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Emanuel EJ, Fairclough DL, Slutsman J, et al. Understanding economic and other burdens of terminal illness: The experience of patients and their caregivers. Ann Intern Med. 2000;132:451–459. doi: 10.7326/0003-4819-132-6-200003210-00005. [DOI] [PubMed] [Google Scholar]
- 31.Bradshaw M, Ellison CG. Financial hardship and psychological distress: Exploring the buffering effects of religion. Soc Sci Med. 2010;71:196–204. doi: 10.1016/j.socscimed.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Selenko E, Batinic B. Beyond debt. A moderator analysis of the relationship between perceived financial strain and mental health. Soc Sci Med. 2011;73:1725–1732. doi: 10.1016/j.socscimed.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 33.Gibson PJ, Koepsell TD, Diehr P, et al. Increasing response rates for mailed surveys of Medicaid clients and other low-income populations. Am J Epidemiol. 1999;149:1057–1062. doi: 10.1093/oxfordjournals.aje.a009751. [DOI] [PubMed] [Google Scholar]
- 34.de Souza JA, Yap BJ, Hlubocky FJ, et al. The development of a financial toxicity patient-reported outcome in cancer: The COST measure. Cancer. 2014;120:3245–3253. doi: 10.1002/cncr.28814. [DOI] [PubMed] [Google Scholar]


