Abstract
Background
Nasopharyngeal carcinoma (NPC) has known as a highly distinct kind of head and neck cancer. This distinction has been due to its clinical presentation, epidemiology, outcome, and treatment. There have not been any reports of epidemiological analysis of NPC in Iran. This study has evaluated the incidence rates and trends of nasopharyngeal carcinoma in the Iranian population during 2004 to 2009.
Methods
The data have collected from the Iranian national cancer data system registry. All the cases of nasopharyngeal carcinoma (with the topography code 11 and histology of carcinoma) have retrieved and analyzed from an overall cancer database during a 6-year period. The data have analyzed by using the SPSS, version 16.
Results
To determine the current incidence of NPC in Iran, we have examined the NPC cases from 2004 to 2009. A total of 1431 cases (981 male and 450 female NPC patients) have analyzed epidemiologically in this study. The mean age of the patients was 47.1 years. The incidence was 0.33 per 100000 persons. The overall incidence rate have increased annually (p<0.05). The incidence of NPC gradually increased with age. Prefectures that bordering the Caspian Sea have proved to have a higher incidence than the other studied areas.
Conclusion
Our study has indicated an increasing trend in the incidence of nasopharyngeal carcinoma. Therefore; attempts should be precipitated for prevention.
Keywords: Incidence, Nasopharyngeal carcinoma, NPC, Trend
Introduction
Nasopharyngeal carcinoma has proved to be the most common type of nasopharyngeal cancer which arising from the epithelial cells that line the nasopharynx. Nasopharyngeal carcinoma (NPC) is a unique malignant cancer in the head and neck area. Its demographic, clinical and geographic characteristics are distinct from those of other head and neck epithelial malignancies [1]. NPC is endemic in certain geographic regions of the world and has unique biological features which make it intimately associated with the Epstein - Barr virus (EBV); its genome can thus be identified in 80% of cases worldwide [2]. However, different ethnic populations characterize NPC with major variations [3]. NPC is rarely found in most regions, especially in Europe and North America (as reported, the incidence is below 1/100 000) [4, 5]. In contrast, it is of a high incidence in some areas in Southern China, especially in the Cantonese region around Guangzhou, where approximately 25 per 100,000 people catch the disease [6]. Taiwan, Vietnam and the Philippines are considered as other areas of high incidence. Also, an incidence of mediocre rate is observed among Arab populations living in Northern Africa, and Saudi Arabia, Caribbean residents, as well as the Eskimo population in Alaska and Greenland [7, 8]. In North Africa, the incidence is nearly 5to7 per 100000 [9]. As for Iran, there have been no reports of epidemiological analysis of NPC yet. Therefore, this paper will focus on the demographic patterns of NPC in Iran from 2004 to 2009.
Materials and Methods
The data on registrations of NPC for the years 2004-2009 have obtained from the Iranian cancer data system registry using the International Classification of Diseases (ICD) codes appropriate for the time period of diagnosis. The Iranian cancer data system registry has been a national registry that aimed to record all incident cases of cancer in the Iranian population. Cases of NPC (marked with topography code 11 and histology of carcinoma) have retrieved and analyzed from the country’s overall cancer database. The information about the selected population (i.e. overall personal specifications such as age groups, gender, and provinces of residence) has obtained from the Statistical Center of Iran.
To estimate the trends in the incidence rates, these registries' data have pooled together. The ages have categorized into eight age groups (≤4; 5-14; 15-24; 25-34; 35-44; 45-54; 55-64; 65≤). Data have analyzed using SPSS, version 16. Chi-square test has employed to compare the scores of each of the measures and some of the parameters. A p-value of less than 0.05 has considered statistically significant. The ethical approval for the study has granted by the Research Ethics Committee of Tracheal Research Center of Masih Daneshvari hospital.
Results
The investigated items have included the total number of NPC patients, the number of male and female patients, the annual number of male and female patients, the mean age at diagnosis of NPC, the mean age in the province, the incidence of NPC per 100000 persons, the age-specific incidence of NPC per 1000000 persons among the male and female patients, the trends of incidence, the trends of incidence in males and females, and the incidence in the provinces of Iran (Figure 3, 6). From2004 to2009, 1431patients have identified with histologically proven nasopharyngeal carcinoma according to the WHO classification. The male patients have accounted for 981 cases and the females for 450. Nasopharyngeal carcinoma has occurred more frequently among males than females. The annual numbers of male and female patients have shown in figure 1.The mean age of all the cases at the time of diagnosis was 47.1±17.9 years. The lowest mean age at diagnosis was in Semnan (36.9), and highest in Lorestan (56.4). Figure 2 has shown the mean age in the provinces.
Figure 3.
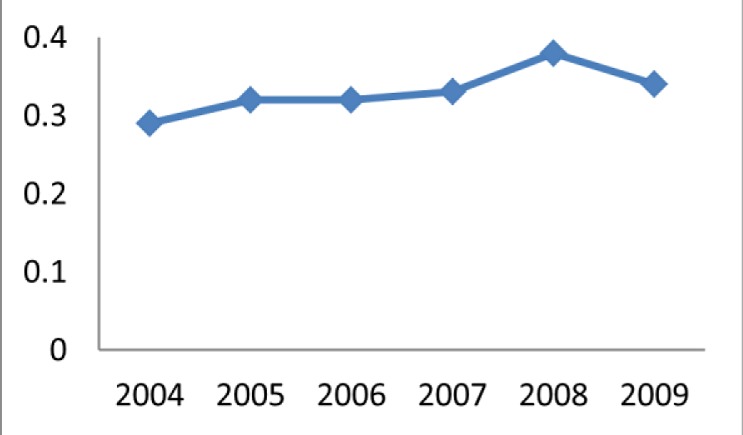
NPC incidence trend during the period 2004-2009
Figure 6.
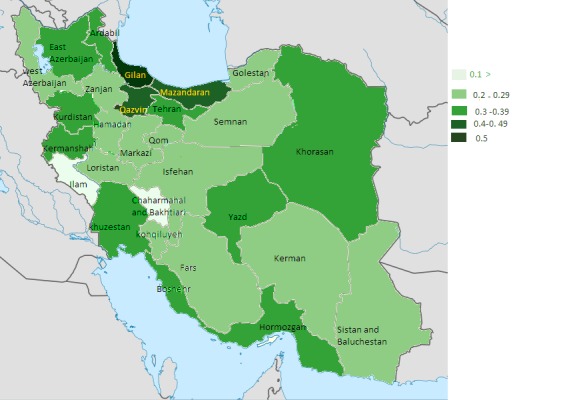
Map of NPC incidence in provinces of Iran.
Figure 1.
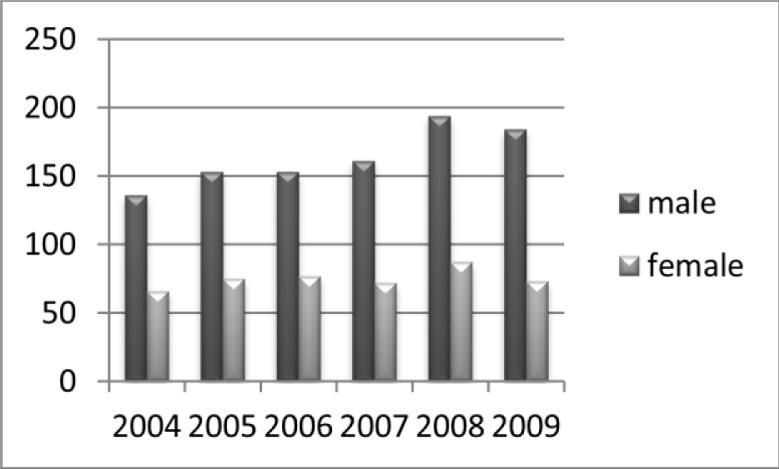
Number of patients per year (2004-2009)
Figure 2.
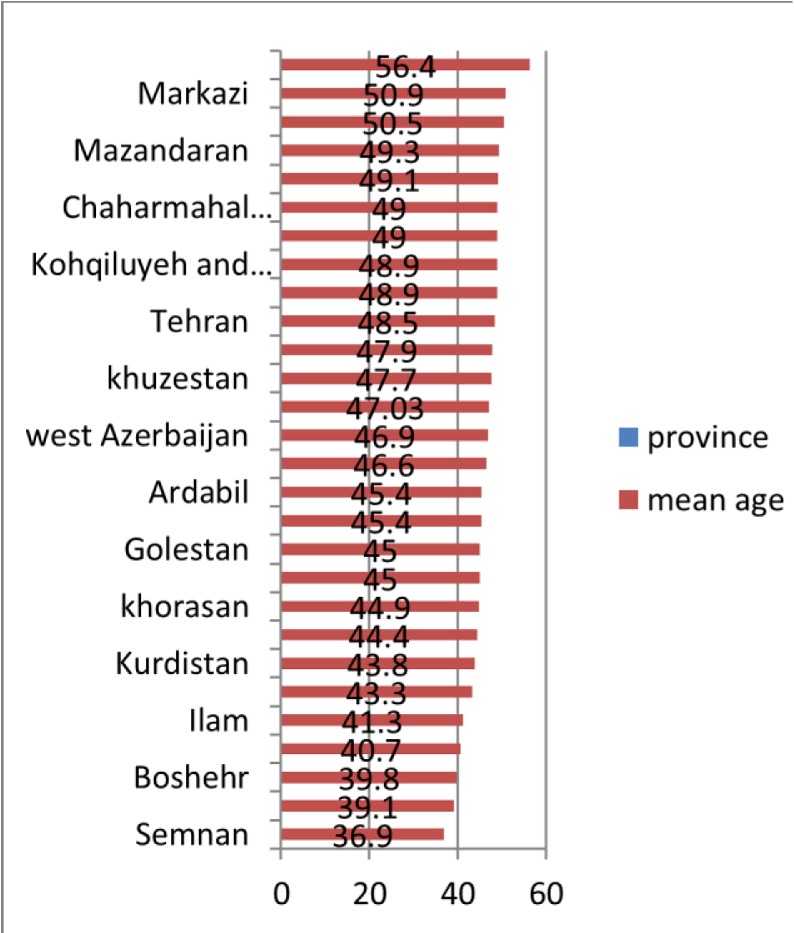
Mean age in provinces of Iran
The incidence rate was 0.33 per 100000. For the males and the females, the incidence rates were 0.45 per 100,000 and 0.21 per 100,000 respectively. We have also detected an increase in the incidence during this 6-year period; the overall incidence rates has increased annually (p<0.05). Using the chi-square test, the p-value for the trend of carcinoma was 0.021. For the males and the females, the trend p values were 0.006 and 0.958 respectively (increasing in the overall incidence rates in the males). The age-specific incidence has compared for both sexes. In general, it was relatively low in persons under 35 years of age but increased in males over 35 years, peaking in the 55-64 age groups in males. In females, the incidence has increased with age, peaking over 55 years of age. For persons over 45, NPC age-specific incidence was twice as high in males as in females (Figure 4). The age-specific incidence of NPC in Gilan (0.5 per 100000) was generally higher than that in the other areas. Next to Gilan, there were Qazvin and Mazandaran with higher rates than the other provinces. The lowest incidence has found in the provinces of Ilam and Chaharmahal. The details about the incidence in the provinces have presented in figure 5 and the map. A comparative review of the three provinces with the highest rates of incidence of carcinoma has shown an increasing trend in Mazandaran (p=0.037).
Figure 4.
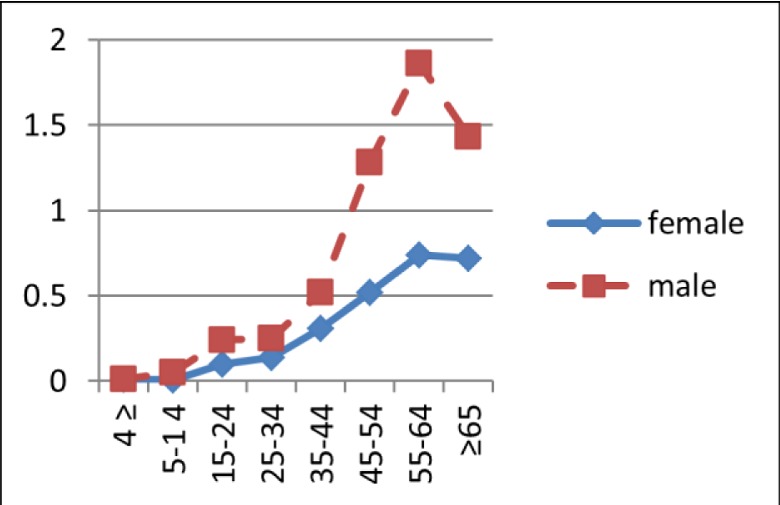
Age-specific incidence of nasopharyngeal carcinoma in males and females.
Figure 5.
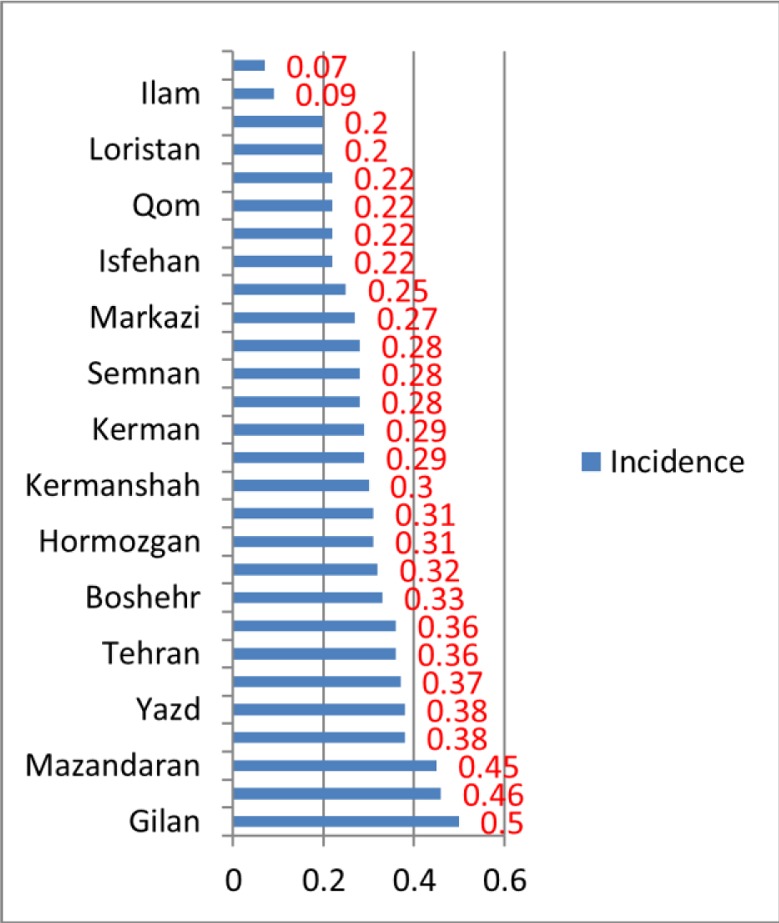
Incidence per 1000000 persons in provinces of Iran.
Discussion
The patterns that turn out of the analysis of NPC have provided a better understanding of its epidemiology and, thus, serve as a useful guide for authorities to come up with effective decisions and policies as to control the disease in Iran. The country has located in the Middle East area. In literature, a medium incidence has seen in some parts of this area [10], but Most Middle East countries have reported higher incidence rates than Iran [11]. The lower incidence of NPC in Iran compared with most Middle East countries might reflect differences in the prevalence of risk factors, such as diet, genetic predisposition, lifestyle or environment.
However, this study has demonstrated a considerable increase in NPC incidence rates in Iran from 2004 to 2009, particularly among males. Our findings were in contrast to those obtained in certain countries, where the trends analyses have shown the rates stable (as in Singapore) [10] or decreased (as in Hong Kong) [12]. Perhaps changes in lifestyle might influence the trend of NPC. Anyway, it is to be borne in mind that precision of recording cancers has improved gradually over the time. This, in turn, contributes to the rise of incidence rates.
Distributions of age-specific rates of NPC have shown distinct features across different populations. In the case of most low-risk populations, NPC incidence increases monotonically with age, which is like the age distributions in most epithelial cancers. Contrastively, among high-risk Southern Chinese of both sexes, the incidence of the disease has risen with age until it has come up to its peak between 45 and 54 years. Then the trend has started to decline at older ages [10]. In a Chinese study in 2009, NPC age-incidence relationship has investigated with the result that the incidence was relatively low in people under 30, but it has dramatically risen in those over 30 years of age, arising on to a peak in the 60-64 age group in males and urban areas, in 80-84 age group in rural areas, and in 70-74 age group in females [13]. Several studies from populations at low to moderate risks for NPC (American blacks and whites, Malaysian, Kadazans, and Indians) have shown a minor peak in incidence among adolescents and young adults (early teens to early twenties) [10, 14-16].
In our study, similar to high-risk areas, the incidence has increased with age; the peak occurred between 55 and 64 years of age and thereafter decreased. This increase has most pronounced in males. However, there was not any peak among adolescents and young adults in our study. In China, for persons over 30, NPC age-specific incidence was more than twice greater in males than in females, although there were slight differences among those under 30 years of age [13]. In our study, for persons over 45, NPC age-specific incidence was more than twice greater in males than in females, but there were differences in all ages (except≤4). The major etiological factors have proposed for NPC pathogenesis has include genetic susceptibility, environmental factors and EBV infection [16, 17]. Consumption of preserved foods, including salted fish, has been implicated in its etiology [18]. In low-incidence regions, NPC has been related to alcohol and tobacco smoking [19, 20]. Cancer incidence rates were the highest in Gilan (0.5 per 100,000) and then in Qazvin and Mazandaran. Gilan and Mazandaran are adjacent to the Caspian Sea, and fish consumption (including salted fish) in these two areas is higher. Moreover, migration from the adjacent provinces (especially Gilan to Qazvin) is relatively high. However, due to the high incidence in these three adjacent provinces and increase of incidence in Mazandaran, a common risk factor might be involved. However, it should be noted that precision in recording cancer cases may vary from province to province. This variation can have an impact on the obtained results.
Conclusion
Finally, it has proposed that some research be conducted on the causes of higher incidence in areas adjacent to the Caspian Sea as well as the role of possible factors in this regard, including genetic, dietary, and environmental factors such as EBV.
Acknowledgments
We have thanked the Research Committee of Tracheal Research Center of Masih daneshvari hospital; we have also thanked Dr Rozita Jafari for her collaboration during the data analysis.
Footnotes
Conflicts of Interest
There would be none to mention.
Authors' Contribution
Ali Safavi designed the study; Nasim Rad contributed to literature review and wrote the paper. Samira Chaibakhsh contributed to the data entry, analyzed the data. Jahangir Ghorbani analyzed the data and writing-up process. Rashid Ramezani contributed to the study design and analysis. All authors read and approved the final manuscript.
REFERENCES
- 1.Liu FF, Frappier L, Kim J, O'Sullivan B, Hui A, Bastianutto C. East-West Symposium on nasopharyngeal cancer. Int J Radiat Oncol Biol Phys. 2007;67(3):703–8. doi: 10.1016/j.ijrobp.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 2.Raab-Traub N. Epstein- Barr virus in the pathogenesis of NPC. Semin Cancer Biol. 2002;12(6):431–41. doi: 10.1016/s1044579x0200086x. [DOI] [PubMed] [Google Scholar]
- 3.Takeshita H, Furukawa M, Fujieda S, Shoujaku H, Ookura T, Sakaguchi M, et al. Epidemiological research into nasopharyngeal carcinoma in the Chubu region of Japan . Auris Nasus Larynx. 1999;26(3):277–86. doi: 10.1016/s0385-8146(98)00080-7. [DOI] [PubMed] [Google Scholar]
- 4.Sun LM, Epplein M, Li CI, Vaughan TL, Weiss NS. Trends in the incidence rates of nasopharyngeal carcinoma among Chinese Americans living in Los Angeles County and the San Francisco metropolitan area, 1992-2002. Am J Epidemiol. . 2005;162(12):1174–8. doi: 10.1093/aje/kwi345. [DOI] [PubMed] [Google Scholar]
- 5.Turkoz FP, Celenkoglu G, Dogu GG, Kalender ME, Coskun U, Alkis N, et al. Risk factors of nasopharyngeal carcinoma in Turkey-an epidemiological survey of the Anatolian Society of Medical Oncology. Asian Pac J Cancer Prev. . 2011;12(11):3017–21. [PubMed] [Google Scholar]
- 6.Wang Y, Zhang Y, Ma S. Racial differences in nasopharyngeal carcinoma in the United States. Cancer Epidemiol. 2013;37(6):793–802. doi: 10.1016/j.canep.2013.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spano JP, Busson P, Atlan D, Bourhis J, Pignon JP, Esteban C, et al. Nasopharyngeal carcinomas: an update. Eur J Cancer. 2003;39(15):2121–35. doi: 10.1016/s0959-8049(03)00367-8. [DOI] [PubMed] [Google Scholar]
- 8.Adham M, Kurniawan AN, Muhtadi AI, Roezin A, Hermani B, Gondhowiardjo S, et al. Nasopharyngeal carcinoma in Indonesia: epidemiology, incidence, signs, and symptoms at presentation. Chin J Cancer. . 2012;31(4):185–96. doi: 10.5732/cjc.011.10328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hila L, Farah F, Ayari H, Ferjaoui M, Dehria W, Ben Jilani S. Epidemiological study, immunohistochemistry and in situ hybridization studies of nasopharyngeal carcinomas: A Tunisian report. Pathol Biol (Paris). 2009;57(5):427–9. doi: 10.1016/j.patbio.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 10.Yu MC, Yuan JM. Epidemiology of nasopharyngeal carcinoma. Semin Cancer Biol . 2002;12(6):421–9. doi: 10.1016/s1044579x02000858. [DOI] [PubMed] [Google Scholar]
- 11.Chang ET, Adami HO. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2006;15(10):1765–77. doi: 10.1158/1055-9965.EPI-06-0353. [DOI] [PubMed] [Google Scholar]
- 12.Lee AW, Foo W, Mang O, Sze WM, Chappell R, Lau WH, et al. Changing epidemiology of nasopharyngeal carcinoma in Hong Kong over a 20-year period (1980-99): an encouraging reduction in both incidence and mortality. Int J Cancer. . 2003;103(5):680–5. doi: 10.1002/ijc.10894. [DOI] [PubMed] [Google Scholar]
- 13.Xu ZJ, Zheng RS, Zhang SW, Zou XN, Chen WQ. Nasopharyngeal carcinoma incidence and mortality in China in 2009. Chin J Cancer. 2013;32(8):453–60. doi: 10.5732/cjc.013.10118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeyakumar A, Brickman TM, Jeyakumar A, Doerr T. Review of nasopharyngeal carcinoma. Ear Nose Throat J. . 2006;85(3):168–84. [PubMed] [Google Scholar]
- 15.Brennan B. Nasopharyngeal carcinoma. Orphanet J Rare Dis. . 2006;1:23. doi: 10.1186/1750-1172-1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abdullah NE, Adam AA, Khalifa EH, El Hassan LA, Ibrahim ME, Hamad KM, et al. Nasopharyngeal cancer in Sudan: epidemiology, clinical and histological characteristics. Clin Med Insights Ear Nose Throat. . 2011;4:5–11. doi: 10.4137/CMENT.S5825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jia WH, Huang QH, Liao J, Ye W, Shugart YY, Liu Q, et al. Trends in incidence and mortality of nasopharyngeal carcinoma over a 20-25 year period (1978/1983-2002) in Sihui and Cangwu counties in southern China. BMC Cancer. . 2006;6:178. doi: 10.1186/1471-2407-6-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsao SW, Yip YL, Tsang CM, Pang PS, Lau VM, Zhang G, et al. Etiological factors of nasopharyngeal carcinoma. Oral Oncol. 2014;50(5):330–8. doi: 10.1016/j.oraloncology.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Polesel J, Franceschi S, Talamini R, Negri E, Barzan L, Montella M, et al. Tobacco smoking, alcohol drinking, and the risk of different histological types of nasopharyngeal cancer in a low-risk population. Oral Oncol. . 2011;47(6):541–5. doi: 10.1016/j.oraloncology.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 20.Xue WQ, Qin HD, Ruan HL, Shugart YY, Jia WH. Quantitative association of tobacco smoking with the risk of nasopharyngeal carcinoma: a comprehensive meta-analysis of studies conducted between 1979 and 2011. Am J Epidemiol. . 2013;178(3):325–38. doi: 10.1093/aje/kws479. [DOI] [PMC free article] [PubMed] [Google Scholar]


