Abstract
Loss-of-function mutations in the X-linked gene Methyl-CpG-binding protein 2 (MECP2) cause a devastating pediatric neurological disorder called Rett syndrome. In males, these mutations typically result in severe neonatal encephalopathy and early lethality. On the other hand, owing to expression of the normal allele in ∼50% of cells, females do not suffer encephalopathy but instead develop Rett syndrome. Typically females with Rett syndrome exhibit a delayed onset of neurologic dysfunction that manifests around the child's first birthday and progresses over the next few years. Features of this disorder include loss of acquired language and motor skills, intellectual impairment and hand stereotypies. The developmental regression observed in patients with Rett syndrome arises from altered neuronal function and is not the result of neurodegeneration. Maintenance of an appropriate level of MeCP2 appears integral to the function of healthy neurons as patients with increased levels of MeCP2, owing to duplication of the Xq28 region encompassing the MECP2 locus, also present with intellectual disability and progressive neurologic symptoms. Despite major efforts over the past two decades to elucidate the molecular functions of MeCP2, the mechanisms underlying the delayed appearance of symptoms remain unclear. In this review, we will highlight recent findings that have expanded our knowledge of MeCP2's functions, and we will discuss how epigenetic regulation, chromatin organization and circuit dynamics may contribute to the postnatal onset of Rett syndrome.
Introduction
Rett syndrome (RTT; OMIM Entry 312750) is a postnatal neurodevelopmental disorder that results in profound intellectual and motor disability and affects ∼1 in 10 000 live female births (1,2). The vast majority of RTT cases result from mutations in Methyl-CpG-binding protein 2 (MECP2), which is located within Xq28 and encodes an epigenetic regulator that is highly expressed in the nervous system (3). Approximately 99% of reported cases of classical RTT are sporadic, and 95% of cases are caused by de novo, loss-of-function mutations in MECP2; however, a handful of cases are familial and display an X-linked dominant inheritance pattern (3,4). Classical RTT is infrequently observed in males because a deleterious mutation in the only copy of MECP2 typically results in severe neonatal encephalopathy and early lethality (5). RTT is characterized by a period of ostensibly normal development during the first 6–18 months of life; after this time period, patients with RTT undergo a developmental regression marked by loss of acquired language abilities, a slowing of both head and brain growth, impaired motor skills and loss of purposeful hand movements (6). Following this regressive stage, a period of stabilization or even partial recovery of certain skills ensues; after this plateau period, however, comes a later phase of motor deterioration (6). Patients with RTT also exhibit a wide array of phenotypes including abnormal breathing patterns, autistic features, seizures and autonomic nervous system dysfunction (7). The clinical picture produced by a MECP2 mutation can be influenced considerably by favorable X-inactivation patterns as well as the degree of MeCP2 dysfunction conferred by the specific mutation. Hypomorphic alleles typically produce mild or partial phenotypes in females, and they typically cause psychiatric disorders and intellectual disability without neonatal lethality in males (8–18). Notably, enhanced MeCP2 function caused by duplications of the MECP2 locus also results in neurologic impairment; individuals with MECP2 duplication syndrome present with early-onset infantile hypotonia, delayed cognitive and motor development, severe intellectual disability, epilepsy and progressive spasticity during childhood (19–21). The similarities between these two neurological disorders highlight the importance of having MeCP2 at the appropriate level for proper neuronal function.
Histologically, the brains of RTT patients have smaller, more closely packed neurons with decreased dendritic complexity; despite these changes in connectivity and cell morphology, there is no evidence of neurodegeneration or gross malformations (22,23). Efforts to unravel the biological functions of MeCP2 have benefitted from the generation of numerous mouse models with disease-causing Mecp2 mutations that reproduce many aspects of RTT, including altered dendritic branching and decreased brain weight (24–28). MeCP2 is expressed in the majority of cell types within the body, is highly expressed within the central nervous system, and its expression increases during neuronal maturation (29–32). The extensive expression of MeCP2 throughout the brain helps explain the breadth of symptoms seen in RTT. Similar to findings in human patients, mouse models also exhibit a broad spectrum of symptom severity and phenotypes. Female mice heterozygous for a Mecp2-null allele show a delayed onset of behavioral deficits around 4 months of age or older (24,33,34). Male mice with a Mecp2-null allele are more severely affected than heterozygous females, with overt symptoms observable at 3–4 weeks of age and death occurring at ∼8–10 weeks of age (24,33). Consistent with patient data, male mice with hypomorphic alleles have milder phenotypes and variable increases in longevity depending on the specific mutation (25,35–37).
One of the most intriguing and, as of yet, incompletely understood features of RTT is the period of seemingly normal early development prior to the onset of progressive neurologic dysfunction. This belated appearance of symptoms has been recapitulated in mouse models and begs the following question: how does altered MeCP2 function lead to delayed disease manifestation? In this review, we will discuss the pathophysiological mechanisms that might account for this postnatal onset of neurological dysfunction by examining recent advances in our understanding of MeCP2 function at the molecular, nuclear and network levels. First, we will consider the epigenetic mechanisms that might contribute to the timing of symptom appearance by discussing the dynamic interaction of MeCP2 with alternatively methylated forms of DNA. Then, we will move to the nuclear level to look at the chromatin-organizing abilities of MeCP2 and the progressive chromatin architectural changes observed in mouse models. Finally, we will discuss the ramifications of the molecular and nuclear changes on neuronal network function.
Impaired epigenetic transcriptional regulation
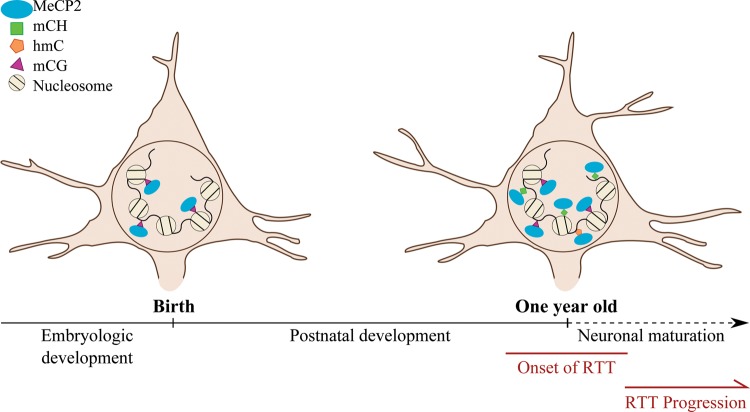
Originally characterized as having a high affinity for methylated cytosines that are followed by a guanine nucleotide (mCG) (38), recently MeCP2 has also been found to bind two alternatively methylated forms of DNA: methylated cytosine followed by a nucleotide other than guanine (mCH, where H = A, C or T) and hydroxymethylcytosine (hmC) (39,40). Both mCH and hmC are enriched in human and mouse brain samples, and, in contrast to most methylated CpG dinucleotides, these marks accumulate postnatally during neuronal maturation (40–42). Coinciding with these changes in the DNA methylation landscape of neuronal chromatin is a surge in MeCP2 expression, which also correlates with the maturation of neurons (29). In general, mCH appears to be a repressive mark that acts to inhibit gene expression (40,42), whereas the presence of hmC within gene bodies has been associated with active gene expression in neurons (39,42). However, it is important to note that the impact of DNA methylation on transcription is context dependent, as methylation has been shown to either inhibit or promote gene expression depending on the location of the mark (43). Given the timing of the concurrent increase in both MeCP2 and its methylated DNA substrate, as well as the role of these marks in transcriptional regulation, it is possible that binding of MeCP2 at mCH and hmC regulates gene expression in mature neurons (Fig 1). Consistent with this idea is the finding that overt symptoms of RTT typically appear around the end of the first year of life. This timing coincides with increased synaptogenesis, metabolic activity and maturation of the neuronal circuitry (44,45), as well as correlates with the period during which mCH accumulates most rapidly in the frontal cortex in humans (42). Notably, many of the genes whose transcriptional profiles are altered in mouse models of RTT are enriched for mCH (46,47), and mice that overexpress MeCP2 show enhanced MeCP2 binding at mCH in the genes that are misregulated (47). Impaired binding of MeCP2 to hmC has also been implicated as a contributor to the symptoms of RTT. One of the most common missense mutations, Arg133Cys (11), has been shown to specifically affect MeCP2 binding to hmC in vitro (39). However, adult knockout of MeCP2 has demonstrated that the timing of symptom onset does not track precisely with the loss of MeCP2; rather, the change in the behavioral phenotype of the mice emerges a few weeks after the change in MeCP2 protein levels (48,49). If MeCP2 binding at these marks directly mediated the behavioral impairment observed in the adult knockout, we would anticipate that symptoms appear as MeCP2 protein levels declined. Given the delay between changes in MeCP2 levels and behavioral findings, it is likely that binding to mCH and hmC is only one component of the process that results in the delayed onset of RTT symptoms, and that loss of MeCP2 may initiate a series of events that eventually lead to disease presentation.
Figure 1.
Model of MeCP2 binding at alternative DNA methylation sites during neuronal development. Schematic diagram showing accumulation of hmC and mCH marks on chromatin coincides with increased MeCP2 expression during neuronal maturation. Lack of MeCP2 binding at these marks may lead to the onset of RTT symptoms.
Altered chromatin architecture
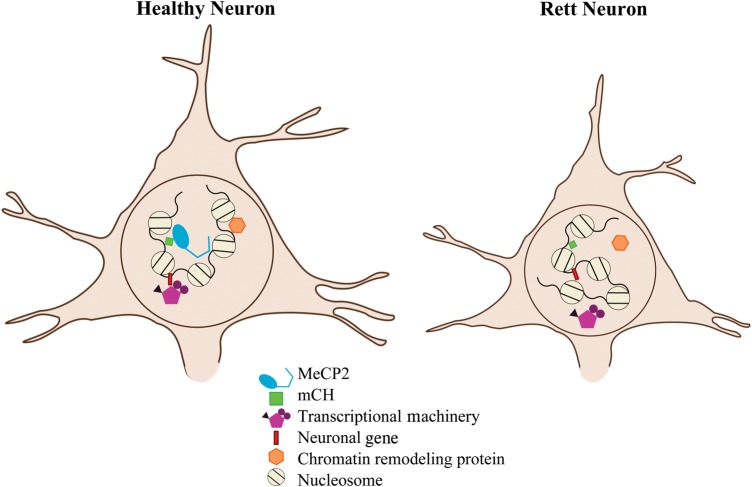
At the nuclear level, a contributing factor to the delayed appearance of RTT symptoms may be the time it takes for the chromatin organization to change upon the loss or restoration of MeCP2. Specifically, it is possible that alterations in chromatin architecture could affect gene transcription, leading to neuronal dysfunction and symptom onset. The interaction of MeCP2 with chromatin has been found to extend beyond its ability to bind methylated DNA using its methyl-CpG-binding domain (MBD). The protein sequence of MeCP2 contains three basic clusters that bear homology to the high-mobility group AT hook family of chromatin-associated proteins (35). Using these basic residues, known as AT hooks because of their high affinity for AT-rich DNA sequences, MeCP2 is able to compact chromatin and influence the higher-order structure of the DNA (35,36,50). In doing so, MeCP2 appears to be able to impact the ability of other nuclear proteins to interact with the chromatin, such as the chromatin remodeling protein alpha thalassemia/mental retardation syndrome X-linked (ATRX), which has been shown to lose its normal localization at heterochromatic foci in MeCP2-null mice (35,51). MeCP2-null mice, as well as early truncating mutations (Arg270X and Gly273X) that disrupt one or more of these AT hooks, but leave the putative ATRX interaction domain of MeCP2 intact (51), also show a gradual loss of ATRX from the heterochromatin, indicating that the mislocalization of ATRX is not due to a loss of direct interaction with MeCP2 (35). Both truncated mutants display altered chromatin states, and the loss of ATRX from heterochromatin is cell autonomous and correlates with disease onset and progression (35). Taken together, these discoveries suggest that the gradual onset of chromatin disorganization, as visualized by delayed ATRX mislocalization, may be one of the contributing factors to the delayed onset of RTT symptoms as well as disease progression (Fig. 2). Consistent with the idea that the basic clusters are important for MeCP2 function, five of the six most common MeCP2 mutations cataloged in the IRSA MECP2 Variation Database (Arg168X, Arg255X, Arg270X, Arg294X and Arg306Cys) (52) either lack a portion of these basic residues or show impaired function of the residues. However, it is important to note that the chromatin-organizing capabilities of these basic clusters are likely dependent on MeCP2 first binding to methylated DNA via its MBD, as mutations that specifically disrupt MBD function cause loss of MeCP2 from the chromatin (36,53,54). Consequently, any mutation that disrupts binding to methylated DNA (including mCH or hmC) is also predicted to impair MeCP2 binding via its basic residues.
Figure 2.
Model of how chromatin organization may differ between healthy neurons and Rett neurons. The absence of MeCP2 could cause altered chromatin architecture that impairs the activities of other nuclear proteins, including transcription-regulating and chromatin-remodeling proteins, resulting in the appearance of RTT symptoms.
Neuronal circuit dysfunction
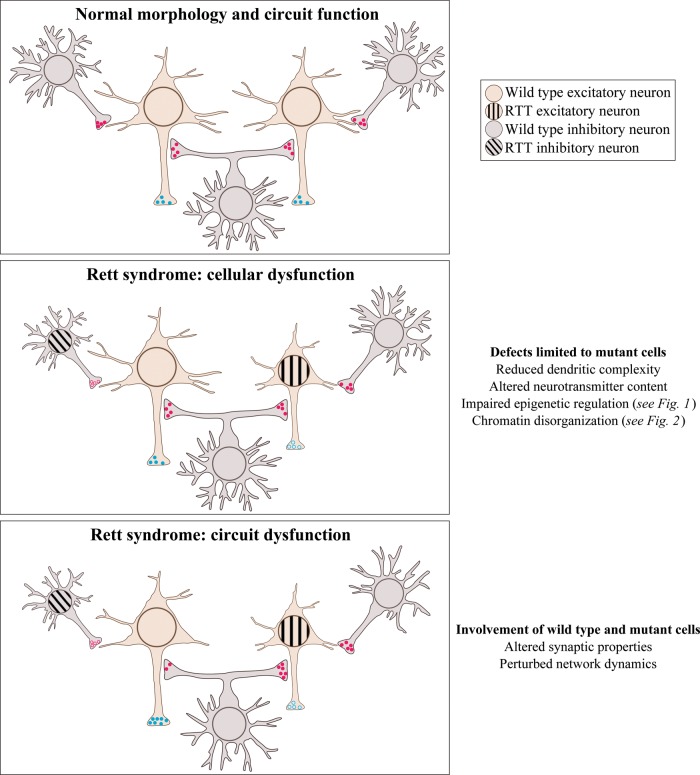
The third aspect in the discussion of the timing of RTT onset pertains to the impact of MeCP2 dysfunction at the level of the neuronal circuit. The progressive molecular and nuclear changes that accrue in MeCP2-deficient neurons can reasonably be expected to impair neuronal function (Fig. 3 middle panel) and ultimately culminate in altered neuronal network dynamics (Fig. 3 bottom panel). As a result, the time required for a neuronal circuit to manifest dysfunction can also contribute to the delayed onset of RTT symptoms. Altered connectivity has been suggested by the diminished dendritic arborization of cortical neurons (23) and by the altered neurotransmitter profiles observed in patients, such as decreased aminergic metabolites (55) and reduced tyrosine hydroxylase staining in the substantia nigra and hypothalamus (56). Electroencephalogram (EEG) recordings from patients have demonstrated changes in cortical circuit activity, including cortical hyperexcitability that is consistent with a decrease in inhibitory synaptic control (7,57). Interestingly, EEG abnormalities are typically not observed during the pre-regression (pre-symptomatic) stage of RTT; rather, the development of aberrant cortical activity patterns appears to coincide with the regressive stage of RTT (7). This finding supports the theory that atypical network properties may directly lead to the appearance of symptoms. Furthermore, this finding also indicates that circuit dysfunction develops over time. Consistent with this idea is the discovery that female mice heterozygous for a Mecp2-null allele have deficits in hippocampal long-term potentiation, which do not arise until the mice are symptomatic (58).
Figure 3.
Model of the cellular and circuit changes that occur in Rett syndrome. Schematic diagram showing a normal circuit (top panel) and two time points in the disease course: (1) (middle panel) cell-autonomous changes arise only in mutant neurons and impair their functioning. These changes include altered neurotransmitter content, decreased dendritic complexity, impaired epigenetic regulation and changes in chromatin architecture; (2) (bottom panel) over time, both the wild-type and mutant neurons are affected, causing overt circuit dysfunction and manifestation of symptoms.
Network hyperexcitability has also been implicated in the generation of specific symptoms, including seizures (59,60) and breathing abnormalities (61,62). Furthermore, pharmacologic interventions that directly decrease the synaptic excitability of respiratory cells within the nucleus tractus solitarius (nTS) of the brainstem have demonstrated improvement in the breathing parameters of MeCP2-null mice (63,64). Changes in neuronal firing and circuit dynamics have been demonstrated in both RTT patients and mouse models, and this altered connectivity appears to produce at least a portion of the symptoms associated with RTT. Moreover, perturbations in neuronal networks may also explain the variability in disease progression observed with different MeCP2 alleles. Specifically, individuals with hypomorphic alleles, such as the Ala140Val mutation, have a less severe phenotype and typically develop symptoms more slowly (8,17,65). Because MeCP2 retains some activity with hypomorphic mutations, we would expect that network dysfunction would occur more gradually, which is consistent with the clinical picture of individuals with these types of mutations.
Mouse models of RTT recapitulate other synaptic morphological and physiological features of this disorder, including increased cell packing density, decreased brain weight and reduced dendritic branching (25,30,66,67). EEG abnormalities and altered synaptic plasticity have also been described in numerous mouse models (27,28,58,59,68–72). Furthermore, many of the electrophysiological findings in RTT mouse models reveal an imbalance between excitation and inhibition in neuronal circuits. Selective loss of MeCP2 expression in either GABAergic or glutamatergic cortical neurons can alter circuit function and result in the appearance of specific RTT-associated phenotypes (59,69,73–75). Along these same lines, the characteristic progression of neurologic symptoms seen in RTT patients (76) hints at the possibility that certain neuronal subtypes and networks are more vulnerable to the loss of MeCP2. As a result, symptoms derived from the dysfunction of these more susceptible neuronal circuits would be predicted to manifest earlier in the course of disease.
Future Perspectives
The delayed presentation of symptoms is a striking feature of Rett syndrome, and recent research has provided insight into the potential mechanisms leading to postponed disease onset. At the molecular and nuclear levels, MeCP2 binding to alternatively methylated DNA and chromatin remodeling have been implicated as contributing factors in the timing of symptom presentation. However, it remains unclear whether these processes are impaired in all cases of RTT or only in patients with specific MECP2 mutations. To better understand these functions of MeCP2, it will be important to establish whether the specific loss or gain of MeCP2 binding at mCH/hmC can reproduce or rescue all symptoms of RTT, respectively. In addition, a thorough evaluation of the three-dimensional structure of the chromatin in mouse models bearing different MeCP2 mutations would help illuminate the role of disordered chromatin in RTT. Finally, the symptoms of RTT can also be viewed in light of the underlying circuit dysfunction that produces them. A critical next step for understanding these neuronal network changes will be elucidation of the precise series of molecular and nuclear events that culminate in aberrant circuit dynamics.
Funding
This work was supported by the National Institute of Health (grant number R01NS057819 to H.Y.Z.); the Howard Hughes Medical Institute (to H.Y.Z.); the McNair Medical Institute MD-PhD Student Scholars Program (to A.E.P.); and Baylor Research Advocates for Student Scientists (to A.E.P.).
Acknowledgements
The authors wish to dedicate this review to the memory of Professor Bengt Hagberg (1923–2015), whose astute observations and exemplary clinical work led Huda Zoghbi to recognize Rett syndrome and pursue its genetic cause. The authors also thank members of the Zoghbi lab, especially Kerstin Ure, Aya Ishida, Laura Lavery, and Laura Lombardi for discussions and input on the manuscript.
Conflict of Interest statement. H.Y.Z. is one of the co-holders of U.S. Patent 6,709,817 Method of Screening Rett Syndrome by Detecting a Mutation in MECP2, 23 March 2004.
References
- 1.Laurvick C.L., de Klerk N., Bower C., Christodoulou J., Ravine D., Ellaway C., Williamson S., Leonard H. (2006) Rett syndrome in Australia: a review of the epidemiology. J. Pediatr., 148, 347–352. [DOI] [PubMed] [Google Scholar]
- 2.Hagberg B. (1985) Rett's syndrome: prevalence and impact on progressive severe mental retardation in girls. Acta Paediatr. Scand., 74, 405–408. [DOI] [PubMed] [Google Scholar]
- 3.Amir R.E., Van den Veyver I.B., Wan M., Tran C.Q., Francke U., Zoghbi H.Y. (1999) Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nat. Genet., 23, 185–188. [DOI] [PubMed] [Google Scholar]
- 4.Bienvenu T., Carrié A., de Roux N., Vinet M.C., Jonveaux P., Couvert P., Villard L., Arzimanoglou A., Beldjord C., Fontes M. et al. (2000) MECP2 mutations account for most cases of typical forms of Rett syndrome. Hum. Mol. Genet., 9, 1377–1384. [DOI] [PubMed] [Google Scholar]
- 5.Schanen N.C., Kurczynski T.W., Brunelle D., Woodcock M.M., Dure L.S., Percy A.K. (1998) Neonatal encephalopathy in two boys in families with recurrent Rett syndrome. J. Child Neurol., 13, 229–231. [DOI] [PubMed] [Google Scholar]
- 6.Neul J.L., Kaufmann W.E., Glaze D.G., Christodoulou J., Clarke A.J., Bahi-Buisson N., Leonard H., Bailey M.E.S., Schanen N.C., Zappella M. et al. (2010) Rett syndrome: revised diagnostic criteria and nomenclature. Ann. Neurol., 68, 944–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glaze D.G. (2005) Neurophysiology of Rett syndrome. J. Child Neurol., 20, 740–746. [DOI] [PubMed] [Google Scholar]
- 8.Orrico A., Lam C., Galli L., Dotti M.T., Hayek G., Tong S.F., Poon P.M., Zappella M., Federico A., Sorrentino V. (2000) MECP2 mutation in male patients with non-specific X-linked mental retardation. FEBS Lett., 481, 285–288. [DOI] [PubMed] [Google Scholar]
- 9.Imessaoudene B., Bonnefont J.P., Royer G., Cormier-Daire V., Lyonnet S., Lyon G., Munnich A., Amiel J. (2001) MECP2 mutation in non-fatal, non-progressive encephalopathy in a male. J. Med. Genet., 38, 171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meloni I., Bruttini M., Longo I., Mari F., Rizzolio F., D'Adamo P., Denvriendt K., Fryns J.P., Toniolo D., Renieri A. (2000) A mutation in the Rett syndrome gene, MECP2, causes X-linked mental retardation and progressive spasticity in males. Am. J. Hum. Genet., 67, 982–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fabio R.A., Colombo B., Russo S., Cogliati F., Masciadri M., Foglia S., Antonietti A., Tavian D. (2014) Recent insights into genotype-phenotype relationships in patients with Rett syndrome using a fine grain scale. Res. Dev. Disabil., 35, 2976–2986. [DOI] [PubMed] [Google Scholar]
- 12.Urbanowicz A., Downs J., Girdler S., Ciccone N., Leonard H. (2015) Aspects of speech-language abilities are influenced by MECP2 mutation type in girls with Rett syndrome. Am. J. Med. Genet. A, 167, 354–362. [DOI] [PubMed] [Google Scholar]
- 13.Neul J., Fang P., Barrish J., Lane J. (2008) Specific mutations in methyl-CpG-binding protein 2 confer different severity in Rett syndrome. Neurology, 70, 1313–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen D., Lazar G., Couvert P., Desportes V., Lippe D., Mazet P., Héron D. (2002) MECP2 mutation in a boy with language disorder and schizophrenia. Am. J. Psychiatry, 159, 148–149. [DOI] [PubMed] [Google Scholar]
- 15.Inui K., Akagi M., Ono J., Tsukamoto H., Shimono K., Mano T., Imai K., Yamada M., Muramatsu T., Sakai N. et al. (2001) Mutational analysis of MECP2 in Japanese patients with atypical Rett syndrome. Brain Dev., 23, 212–215. [DOI] [PubMed] [Google Scholar]
- 16.Moog U., Van Roozendaal K., Smeets E., Tserpelis D., Devriendt K., Van Buggenhout G., Frijns J.-P., Schrander-Stumpel C. (2006) MECP2 mutations are an infrequent cause of mental retardation associated with neurological problems in male patients. Brain Dev., 28, 305–310. [DOI] [PubMed] [Google Scholar]
- 17.Winnepenninckx B., Errijgers V., Hayez-Delatte F., Reyniers E., Frank Kooy R. (2002) Identification of a family with nonspecific mental retardation (MRX79) with the A140V mutation in the MECP2 gene: is there a need for routine screening? Hum. Mutat., 20, 249–252. [DOI] [PubMed] [Google Scholar]
- 18.Klauck S.M., Lindsay S., Beyer K.S., Splitt M., Burn J., Poustka A. (2002) A mutation hot spot for nonspecific X-linked mental retardation in the MECP2 gene causes the PPM-X syndrome. Am. J. Hum. Genet., 70, 1034–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Esch H., Bauters M., Ignatius J., Jansen M., Raynaud M., Hollanders K., Lugtenberg D., Bienvenu T., Jensen L.R., Gecz J. et al. (2005) Duplication of the MECP2 region is a frequent cause of severe mental retardation and progressive neurological symptoms in males. Am. J. Hum. Genet., 77, 442–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramocki M.B., Tavyev Y.J., Peters S.U. (2010) The MECP2 duplication syndrome. Am. J. Med. Genet. Part A, 152, 1079– 1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Esch H. (2012) MECP2 duplication syndrome. Mol. Syndromol., 2, 128–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Armstrong D., Dunn J.K., Antalffy B., Trivedi R. (1995) Selective dendritic alterations in the cortex of Rett syndrome. J. Neuropathol. Exp. Neurol., 54, 195–201. [DOI] [PubMed] [Google Scholar]
- 23.Bauman M.L., Kemper T.L., Arin D.M. (1995) Pervasive neuroanatomic abnormalities of the brain in three cases of Rett's syndrome. Neurology, 45, 1581–1586. [DOI] [PubMed] [Google Scholar]
- 24.Guy J., Hendrich B., Holmes M., Martin J.E., Bird A. (2001) A mouse Mecp2-null mutation causes neurological symptoms that mimic Rett syndrome. Nat. Genet., 27, 322–326. [DOI] [PubMed] [Google Scholar]
- 25.Jentarra G.M., Olfers S.L., Rice S.G., Srivastava N., Homanics G.E., Blue M., Naidu S., Narayanan V. (2010) Abnormalities of cell packing density and dendritic complexity in the MeCP2 A140 V mouse model of Rett syndrome/X-linked mental retardation. BMC Neurosci., 11, 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou Z., Hong E.J., Cohen S., Zhao W.-N., Ho H.-Y.H., Schmidt L., Chen W.G., Lin Y., Savner E., Griffith E.C. et al. (2006) Brain-specific phosphorylation of MeCP2 regulates activity-dependent Bdnf transcription, dendritic growth, and spine maturation. Neuron, 52, 255–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dani V.S., Chang Q., Maffei A., Turrigiano G.G., Jaenisch R., Nelson S.B. (2005) Reduced cortical activity due to a shift in the balance between excitation and inhibition in a mouse model of Rett syndrome. Proc. Natl Acad. Sci., 102, 12560–12565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moretti P., Levenson J.M., Battaglia F., Atkinson R., Teague R., Antalffy B., Armstrong D., Arancio O., Sweatt J.D., Zoghbi H.Y. (2006) Learning and memory and synaptic plasticity are impaired in a mouse model of Rett syndrome. J. Neurosci., 26, 319–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shahbazian M.D., Antalffy B., Armstrong D.L., Zoghbi H.Y. (2002) Insight into Rett syndrome: MeCP2 levels display tissue- and cell-specific differences and correlate with neuronal maturation. Hum. Mol. Genet., 11, 115–124. [DOI] [PubMed] [Google Scholar]
- 30.Kishi N., Macklis J.D. (2004) MECP2 is progressively expressed in post-migratory neurons and is involved in neuronal maturation rather than cell fate decisions. Mol. Cell. Neurosci., 27, 306–321. [DOI] [PubMed] [Google Scholar]
- 31.Song C., Feodorova Y., Guy J., Peichl L., Jost K.L., Kimura H., Cardoso M.C., Bird A., Leonhardt H., Joffe B. et al. (2014) DNA methylation reader MECP2: cell type- and differentiation stage-specific protein distribution. Epigenetics Chromatin, 7, 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Skene P.J., Illingworth R.S., Webb S., Kerr A.R.W., James K.D., Turner D.J., Andrews R., Bird A.P. (2010) Neuronal MeCP2 is expressed at near histone-octamer levels and globally alters the chromatin state. Mol. Cell, 37, 457–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Santos M., Silva-Fernandes A., Oliveira P., Sousa N., Maciel P. (2007) Evidence for abnormal early development in a mouse model of Rett syndrome. Genes. Brain. Behav., 6, 277–286. [DOI] [PubMed] [Google Scholar]
- 34.Samaco R.C., McGraw C.M., Ward C.S., Sun Y., Neul J.L., Zoghbi H.Y. (2013) Female Mecp2(+/-) mice display robust behavioral deficits on two different genetic backgrounds providing a framework for pre-clinical studies. Hum. Mol. Genet., 22, 96–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baker S.A., Chen L., Wilkins A.D., Yu P., Lichtarge O., Zoghbi H.Y. (2013) An AT-hook domain in MeCP2 determines the clinical course of Rett syndrome and related disorders. Cell, 152, 984–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heckman L.D., Chahrour M.H., Zoghbi H.Y. (2014) Rett-causing mutations reveal two domains critical for MeCP2 function and for toxicity in MECP2 duplication syndrome mice. eLife, 3, e02676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lyst M.J., Ekiert R., Ebert D.H., Merusi C., Nowak J., Selfridge J., Guy J., Kastan N.R., Robinson N.D., de Lima Alves F. et al. (2013) Rett syndrome mutations abolish the interaction of MeCP2 with the NCoR/SMRT co-repressor. Nat. Neurosci., 16, 898–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lewis J.D., Meehan R.R., Henzel W.J., Maurer-Fogy I., Jeppesen P., Klein F., Bird A. (1992) Purification, sequence, and cellular localization of a novel chromosomal protein that binds to methylated DNA. Cell, 69, 905–914. [DOI] [PubMed] [Google Scholar]
- 39.Mellén M., Ayata P., Dewell S., Kriaucionis S., Heintz N. (2012) MeCP2 binds to 5hmC enriched within active genes and accessible chromatin in the nervous system. Cell, 151, 1417–1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guo J.U., Su Y., Shin J.J.H., Li H., Xie B., Zhong C., Hu S., Le T., Fan G., Zhu H. et al. (2014) Distribution, recognition and regulation of non-CpG methylation in the adult mammalian brain. Nat. Neurosci., 17, 215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Szulwach K.E., Li X., Li Y., Song C.-X., Wu H., Dai Q., Irier H., Upadhyay A.K., Gearing M., Levey A.I. et al. (2011) 5-hmC–mediated epigenetic dynamics during postnatal neurodevelopment and aging. Nat. Neurosci., 14, 1607–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lister R., Mukamel E.A., Nery J.R., Urich M., Puddifoot C.A., Johnson N.D., Lucero J., Huang Y., Dwork A.J., Schultz M.D. et al. (2013) Global epigenomic reconfiguration during mammalian brain development. Science, 341, 1237905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jones P.A. (2012) Functions of DNA methylation: islands, start sites, gene bodies and beyond. Nat. Rev. Genet., 13, 484–492. [DOI] [PubMed] [Google Scholar]
- 44.Chugani H.T. (1998) A critical period of brain development: Studies of cerebral glucose utilization with PET. Prev. Med., 27, 184–188. [DOI] [PubMed] [Google Scholar]
- 45.Huttenlocher P.R., Dabholkar A.S. (1997) Regional differences in synaptogenesis in human cerebral cortex. J. Comp. Neurol., 387, 167–178. [DOI] [PubMed] [Google Scholar]
- 46.Gabel H.W., Kinde B., Stroud H., Gilbert C.S., Harmin D.A., Kastan N.R., Hemberg M., Ebert D.H., Greenberg M.E. (2015) Disruption of DNA-methylation-dependent long gene repression in Rett syndrome. Nature, 522, 89–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen L., Chen K., Lavery L.A., Baker S.A., Shaw C.A., Li W., Zoghbi H.Y. (2015) MeCP2 binds to non-CG methylated DNA as neurons mature, influencing transcription and the timing of onset for Rett syndrome. Proc. Natl Acad. Sci., 112, 5509–5514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McGraw C.M., Samaco R.C., Zoghbi H.Y. (2011) Adult neural function requires MeCP2. Science, 333, 186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cheval H., Guy J., Merusi C., De Sousa D., Selfridge J., Bird A. (2012) Postnatal inactivation reveals enhanced requirement for MeCP2 at distinct age windows. Hum. Mol. Genet., 21, 3806–3814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nikitina T., Shi X., Ghosh R.P., Horowitz-Scherer R.A., Hansen J.C., Woodcock C.L. (2007) Multiple modes of interaction between the methylated DNA binding protein MeCP2 and chromatin. Mol. Cell. Biol., 27, 864–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nan X., Hou J., Maclean A., Nasir J., Lafuente M.J., Shu X., Kriaucionis S., Bird A. (2007) Interaction between chromatin proteins MECP2 and ATRX is disrupted by mutations that cause inherited mental retardation. Proc. Natl Acad. Sci., 104, 2709–2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Christodoulou J., Grimm A., Maher T., Bennetts B. (2003) Rett BASE: The IRSA MECP2 variation database-a new mutation database in evolution. Hum. Mutat., 21, 466–472. [DOI] [PubMed] [Google Scholar]
- 53.Hansen J.C., Ghosh R.P., Woodcock C.L. (2010) Binding of the Rett syndrome protein, MeCP2, to methylated and unmethylated DNA and chromatin. IUBMB Life, 62, 732–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Casas-Delucchi C.S., Becker A., Bolius J.J., Cristina Cardoso M. (2012) Targeted manipulation of heterochromatin rescues MeCP2 Rett mutants and re-establishes higher order chromatin organization. Nucl. Acids Res., 40, e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Samaco R.C., Mandel-Brehm C., Chao H.-T., Ward C.S., Fyffe-Maricich S.L., Ren J., Hyland K., Thaller C., Maricich S.M., Humphreys P. et al. (2009) Loss of MeCP2 in aminergic neurons causes cell-autonomous defects in neurotransmitter synthesis and specific behavioral abnormalities. Proc. Natl Acad. Sci., 106, 21966–21971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jellinger K., Armstrong D., Zoghbi H.Y., Percy A.K. (1988) Neuropathology of Rett syndrome. Acta Neuropathol., 76, 142–158. [DOI] [PubMed] [Google Scholar]
- 57.Yoshikawa H., Kaga M., Suzuki H., Sakuragawa N., Arima M. (1991) Giant somatosensory evoked potentials in the Rett syndrome. Brain Dev., 13, 36–39. [DOI] [PubMed] [Google Scholar]
- 58.Guy J., Gan J., Selfridge J., Cobb S., Bird A. (2007) Reversal of neurological defects in a mouse model of Rett syndrome. Science, 315, 1143–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang W., Peterson M., Beyer B., Frankel W.N., Zhang Z. (2014) Loss of MeCP2 from forebrain excitatory neurons leads to cortical hyperexcitation and seizures. J. Neurosci., 34, 2754–2763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McLeod F., Ganley R., Williams L., Selfridge J., Bird A., Cobb S.R. (2013) Reduced seizure threshold and altered network oscillatory properties in a mouse model of Rett syndrome. Neuroscience, 231, 195–205. [DOI] [PubMed] [Google Scholar]
- 61.Kline D.D., Ogier M., Kunze D.L., Katz D.M. (2010) Exogenous brain-derived neurotrophic factor rescues synaptic dysfunction in Mecp2-null mice. J. Neurosci., 30, 5303–5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kron M., Howell C.J., Adams I.T., Ransbottom M., Christian D., Ogier M., Katz D.M. (2012) Brain activity mapping in Mecp2 mutant mice reveals functional deficits in forebrain circuits, including key nodes in the default mode network, that are reversed with ketamine treatment. J. Neurosci., 32, 13860–13872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schmid D.A., Yang T., Ogier M., Adams I., Mirakhur Y., Wang Q., Massa S.M., Longo F.M., Katz D.M. (2012) A TrkB small molecule partial agonist rescues TrkB phosphorylation deficits and improves respiratory function in a mouse model of Rett syndrome. J. Neurosci., 32, 1803–1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kron M., Lang M., Adams I.T., Sceniak M., Longo F., Katz D.M. (2014) A BDNF loop-domain mimetic acutely reverses spontaneous apneas and respiratory abnormalities during behavioral arousal in a mouse model of Rett syndrome. Dis. Model. Mech., 7, 1047–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Couvert P., Bienvenu T., Aquaviva C., Poirier K., Moraine C., Gendrot C., Verloes A., Andrès C., Le Fevre A.C., Souville I. et al. (2001) MECP2 is highly mutated in X-linked mental retardation. Hum. Mol. Genet., 10, 941–946. [DOI] [PubMed] [Google Scholar]
- 66.Chen R.Z., Akbarian S., Tudor M., Jaenisch R. (2001) Deficiency of methyl-CpG binding protein-2 in CNS neurons results in a Rett-like phenotype in mice. Nat. Genet., 27, 327–331. [DOI] [PubMed] [Google Scholar]
- 67.Stearns N.A., Schaevitz L.R., Bowling H., Nag N., Berger U.V., Berger-Sweeney J. (2007) Behavioral and anatomical abnormalities in Mecp2 mutant mice: a model for Rett syndrome. Neuroscience, 146, 907–921. [DOI] [PubMed] [Google Scholar]
- 68.Pelka G.J. (2006) Mecp2 deficiency is associated with learning and cognitive deficits and altered gene activity in the hippocampal region of mice. Brain, 129, 887–898. [DOI] [PubMed] [Google Scholar]
- 69.Chao H.-T., Chen H., Samaco R.C., Xue M., Chahrour M., Yoo J., Neul J.L., Gong S., Lu H.-C., Heintz N. et al. (2010) Dysfunction in GABA signalling mediates autism-like stereotypies and Rett syndrome phenotypes. Nature, 468, 263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Asaka Y., Jugloff D.G.M., Zhang L., Eubanks J.H., Fitzsimonds R.M. (2006) Hippocampal synaptic plasticity is impaired in the Mecp2-null mouse model of Rett syndrome. Neurobiol. Dis., 21, 217–227. [DOI] [PubMed] [Google Scholar]
- 71.Chao H.-T., Zoghbi H.Y., Rosenmund C. (2007) MeCP2 controls excitatory synaptic strength by regulating glutamatergic synapse number. Neuron, 56, 58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Calfa G., Li W., Rutherford J.M., Pozzo-Miller L. (2015) Excitation/inhibition imbalance and impaired synaptic inhibition in hippocampal area CA3 of Mecp2 knockout mice. Hippocampus, 25, 159–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Castro J., Garcia R.I., Kwok S., Banerjee A., Petravicz J., Woodson J., Mellios N., Tropea D., Sur M. (2014) Functional recovery with recombinant human IGF1 treatment in a mouse model of Rett Syndrome. Proc. Natl Acad. Sci., 111, 9941–9946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gogolla N., Takesian A.E., Feng G., Fagiolini M., Hensch T.K. (2014) Sensory integration in mouse insular cortex reflects GABA circuit maturation. Neuron, 83, 894–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.He L.J., Liu N., Cheng T.L., Chen X.J., Li Y.D., Shu Y.S., Qiu Z.L., Zhang X.H. (2014) Conditional deletion of Mecp2 in parvalbumin-expressing GABAergic cells results in the absence of critical period plasticity. Nat. Commun., 5, 5036. [DOI] [PubMed] [Google Scholar]
- 76.Chahrour M., Zoghbi H.Y. (2007) The story of Rett syndrome: from clinic to neurobiology. Neuron, 56, 422–437. [DOI] [PubMed] [Google Scholar]