Abstract
The incidence of Gastroesophageal reflux disease (GERD) has increased remarkably worldwide. This study focuses on the background features of these patients and evaluates the two GERD sub types; none erosive (NERD) and erosive (ERD). In a case-control study, patients with reflux symptoms who had obtained a total score of 8-18 of the GERD questionnaire were included. Control group consisted of their families with lower scores and no reflux presentations. All demographic features were recorded. Then upper GI endoscopy performed and the cases divided into two sub groups: NERD and ERD. In the next step, all demographic data analyzed for these two subgroups. The data were analyzed using the SPSS software version 21. A number of 210 subjects included in each group (210 patients with GERD and 210 control group) with normal statistical distribution of age and gender. There was a significant relationship between GERD and BMI (P=0.001), eating fatty foods (P=0.0001), lying after meal (P=0.0001), drinking beverages with meal (0.0001), eating spicy food (0.006) and NSAIDs use (P=0.0001). Then the cases divided into two subgroups; NERD (n=146) and ERD (n=64). There were a significant relationship with eating salty-smoky food (P=0.005) and eating spicy food (P=0.011). The difference of BMI between NERD and ERD was remarkable but was not statistically significant. Our results showed that obesity is an important risk factor for GERD. Other possible risk factors such as NSAIDs use and certain foods and wrong habits like lying after meal should be addressed in future longitudinal surveys.
Keywords: Gastroesophageal reflux disease, life style, severity
Introduction
Gastroesophageal reflux disease (GERD) is defined as the presence of acid reflux related symptoms, including heartburn and regurgitation, or esophageal mucosal damage, caused by the abnormal reflux of gastric contents into the esophagus [1]. The incidence of GERD has increased remarkably worldwide over the past decades, with prevalence rates of 10%-25% in population-based studies [2,3]. This may be related to increased fat consumption in the diet, and the expanding proportion of obese individuals [4]. Various risk factors were shown to be associated with gastroesophageal reflux symptoms, including body weight, genetic factors, pregnancy, nutrition, alcohol consumption, smoking habits and intake of non-steroidal anti-inflammatory drugs and sleeping position [5]. Non erosive reflux disease (NERD), defined as the presence of acid-reflux-related symptoms without esophageal mucosal breaks, and erosive reflux disease (ERD), the progression of NERD to erosive esophagitis, are the two main presentations of GERD [1,6]. The clinical characteristics of patients with NERD that they are less likely to smoke or have an esophageal hiatal hernia, and more likely to be female, underweight, and have Helicobacter pylori infection differ from those of ERD patients. Also, esophageal mucosal sensitivity in NERD patients tends to be higher than those with ERD [7]. Over the years, several issues have been emerged regarding the definition, history and treatment of GERD. This study focuses on the background features of these patients and evaluates them. The results can show which life habits may be considered as risk factors and changing our life styles may decreases the GERD incidence.
Patients and methods
In this case-control survey, a total of 210 subjects with GERD symptoms, i.e. heartburn and acid regurgitation, referred to Razi hospital gastroenterology clinic in Rasht (a city in north of Iran), were enrolled. “Heart burn” defined as a burning sensation at the retrosternal area and “Acid regurgitation” defined as bitter or sour liquid rushing up to the mouth. The patients were given the GERD Q Questionnaire (Astra Zeneca) [8] for evaluating the disease and the individuals who obtained the total score of 8 to 18 underwent upper GI endoscopy between January 2013 to 2015. Sampling method was easy and available. The control group consisted of patient’s family who did not have digestive problems, completed the GERD questionnaire related to reflux and did not obtain the proper score. This study was approved by the Guilan University of Medical Science ethical committee. The written informed consent was obtained from all participants.
Exclusion criteria
Patients with a history of GI surgery, Barrett’s esophagus, esophageal motility disorder, duodenal ulcer, benign gastric ulcer or gastroduodenal cancer were excluded. In this study, Patients with systemic disease requiring chronic medication such as hypertension, diabetes mellitus and Asthma were not involved. Also, subjects who took histamine type II receptor blocker or PPI within 4 month were excluded.
Variables
For each patient a check list was completed including age, sex, height, weight, waist circumference, hip circumference, coffee, tea and alcohol consumption, cigarettes, eating habits and the medical history. The Body Mass Index (BMI) was obtained by using a digital SECA scale with an accuracy of 0.5 kg. The classification of BMI was considered as: normal (Less than 25 kg/m2), overweight (25-30 kg/m2) and obese (above 30 kg/m2). Waist to hip ratio was calculated by dividing the waist to hip circumstance. Waist size is obtained by the lower margin of the latest palpable rib and upper part of iliac crest. Hip circumstance is obtained by measuring the widest part of the hip circumstance. Abdominal obesity is defined as the ratio of waist circumstance to hip circumstance above 0.9 for male and above 0.85 for female. To prevent bias, measurements were performed by a single person. At the next step, upper GI endoscopy performed for all patients in the case group and based on the visual findings during the process, they were divided into two subgroups: NERD and ERD. Then all the variables analyzed between these two subgroups.
Statistical analysis
All data were statistically analyzed using SPSS software package for windows v. 21.0 (SPSS Inc., Chicago, IL, USA). Percentage and frequency were used in order to report the results of the qualitative data and standard deviation and the mean were used in order to report the quantitative data. Chi-square, Fisher exact test and independent T test were used to compare variable. P<0.05 is considered statistically significant.
Results
The case group of 210 patients with mean age of 45.5 ± 14.5 years old was included 91 males and 119 females. The control group of 210 individuals with mean age of 45.4 ± 14.4 years old, was included 89 males and 121 females. In both cases above, the statistical distribution of age and gender was normal.
The average of smoking in the both groups was 5 cigarettes per day; 24 smokers in the case group and 29 smokers in the control group. Also, the mean amount of alcohol in the case and control groups was 100 ml per month; 5 subjects in case group and 12 individuals in control group. There were no significant differences of smoking and alcohol consumption between the two study groups.
In the case group, there were 11.4% Illiterate cases, 78.6% with collage education and 10% with higher education degree. In the control group, there were 3.8% Illiterate cases, 83.8% with collage education and 12.4% with higher education degree. The difference of education level between the two groups was statistically significant (P=0.02).
Waist to hip ratio (WHR) and BMI were calculated for each individual. The results showed higher scores of BMI in the case group rather than the control group (P=0.001). Although the results of WHR in the case group were higher than the control group, this contrast was not statistically significant (Table 1).
Table 1.
BMI and WHR between the two study groups
| Measurements | Case (%) N=210 | Control (%) N=210 | P value | |
|---|---|---|---|---|
| BMI | <24 | 61 (29) | 122 (58.1) | 0.001 |
| 25-30 | 102 (48.6) | 67 (32) | ||
| 30< | 47 (22.4) | 21 (9.9) | ||
| Waist to hip ratio (WHR) | Normal | 50 (23.8) | 86 (41) | 0.087 |
| Abdominal obesity in male (0.9<) | 60 (28.6) | 43 (20.5) | ||
| Abdominal obesity in female (0.85<) | 100 (47.6) | 81 (38.5) | ||
Table 2 shows the demographic characteristics of the two study group individuals. As the table shows, there were a significant relationship between GERD andeating fatty foods (P=0.0001), lying immediately after meal (P=0.0001), Drinking beverages with the meal (0.0001), eating spicy food (0.006) and NSAIDs consumption (P=0.0001).
Table 2.
Demographic features of the two study group participations
| Demographic features | Case (%) N=210 | Control (%) N=210 | P-value | |
|---|---|---|---|---|
| Drug histories | ||||
| NSAIDs* | No | 177 (84.3) | 200 (95.2) | 0.0001 |
| Yes | 33 (15.7) | 10 (4.8) | ||
| OCP* | No | 200 (95.2) | 198 (94.3) | NS |
| Yes | 10 (4.8) | 12 (5.7) | ||
| Aspirin* | No | 198 (94.3) | 202 (96.2) | NS |
| Yes | 12 (5.7) | 8 (3.8) | ||
| Dietary/drinking habits | ||||
| Eating fatty food | Monthly | 55 (26.2) | 52 (24.7) | 0.0001 |
| Weekly | 97 (46.2) | 152 (72.4) | ||
| Daily | 33 (15.7) | 3 (1.45) | ||
| None | 25 (11.9) | 3 (1.45) | ||
| Eating smoky and salty food | Monthly | 80 (38.1) | 90 (42.85) | NS |
| Weekly | 11 (5.24) | 12 (5.7) | ||
| None | 119 (56.66) | 108 (51.45) | ||
| Eating spicy food | Monthly | 71 (33.8) | 96 (45.7) | 0.006 |
| Weekly | 41 (19.5) | 21 (10) | ||
| None | 98 (46.7) | 93 (44.3) | ||
| Drinking soda or other beverages with the meal | Monthly | 100 (47.64) | 166 (79.19) | 0.0001 |
| Weekly | 14 (6.66) | 8 (3.81) | ||
| None | 96 (45.7) | 36 (17) | ||
| Drinking tea | <3 cups daily | 140 (66.66) | 143 (68.16) | NS |
| >3 cups daily | 61 (29.5) | 56 (26.6) | ||
| None | 9 (3.84) | 11 (5.24) | ||
| Drinking coffee | <2 cups monthly | 12 (5.75) | 17 (8) | NS |
| >2 cups monthly | 1 (0.48) | 0 (0) | ||
| None | 197 (93.95) | 193 (92) | ||
| Lying immediately after meal | No | 92 (43.8) | 197 (93.8) | 0.0001 |
| Yes | 118 (56.2) | 13 (6.2) | ||
Consumption during previous 3 month.
Sixty-four patients with ERD and the other cases with NERD (n=146) were diagnosed Using upper GI endoscopy. At the next step we evaluated the demographic features between these two subgroups. There were no significant differences based on age, gender, education and drug consumption (NSAIDs, OCP, Aspirin) between these two subgroups. There were a statistically significant relationship with consumption of salty-smoky food (P=0.005) and spicy food (P=0.011) (Table 3).
Table 3.
Comparison of demographic features between ERD and NERD patients
| Dietary/drinking habits | ERD (%) N=64 | NERD (%) N=146 | P value | |
|---|---|---|---|---|
| Eating salty-smoky food | Monthly | 26 (40.6) | 54 (37) | 0.005 |
| Weekly | 8 (12.5) | 3 (2.05) | ||
| None | 30 (46.9) | 89 (60.95) | ||
| Eating spicy food | Monthly | 24 (37.5) | 47 (32.2) | 0.011 |
| Weekly | 19 (30) | 22 (15.07) | ||
| None | 21 (32.5) | 77 (52.73) | ||
The abdominal obesity in male (WHR>0.9) appeared in 17 of ERD and 43 of NERD cases. Also, 24 females with ERD and 76 females with NERD showed abdominal obesity with WHR more than 0.85. There was no significant relationship between NERD and ERD cases based on WHR. Figure 1 shows the BMI differences between the two main groups and the two subgroups. it is obvious that patients have a higher level of BMI rather than the control group.
Figure 1.
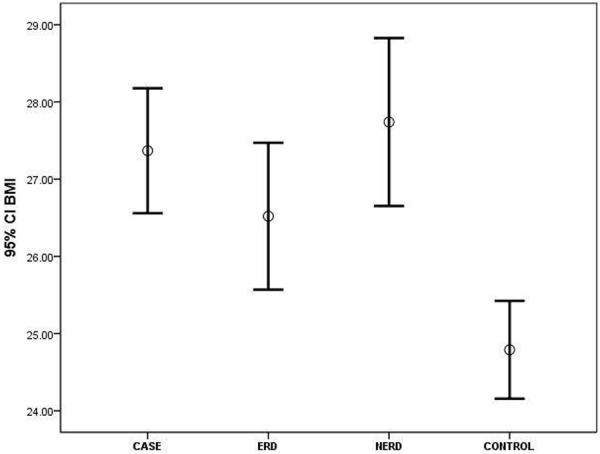
BMI distribution between all participations.
Discussion
Nowadays, the prevalence of GERD and obesity is increasing worldwide. Considering the effect of GERD on different aspects of patients’ life, our knowledge about it is so important and can help in leading new community health strategies [9,10]. In this study, the risk of GERD in patients with higher BMI scores (30<) and lower educational levels, is higher. There are other studies which support these findings. Based on Mansour-Ghenaei et al survey [10], there is a significant statistical relationship between the prevalence of GERD and higher scores of BMI. Also Murray et al [11] showed the importance of education specially the knowledge of people about digestive diseases, the pattern and the risk factors of GERD.
The results of some studies point to the fact that higher scores of BMI increase the likelihood of suffering from severe GERD presentations. Klauser et al and Wajed et al studies [12,13] mentioned that the prevalence of GERD is more common in obese patients with heartburn, acid reflux and dysphagia. Obese people experience this state, three times more than general population. Also, Murray et al [11] showed a direct relationship between overweight or obesity with the frequency and severity of heartburn and regurgitation. The results of such studies confirm our findings. Although we did not find a statistical relationship between higher scores of BMI and severity of GERD (erosive lesions), but it was so clear that ERD is more common in obese cases.
Blondeau et al [14] suggested a direct relationship between the incidence of GERD and BMI and WHR. This state is observed in both patients receiving and not receiving proton pump inhibitors. Also, we found no statistical relationship between WHR and ERD or NERD incidence. The analysis of WHR in other previous conducted studies was not found. This score may be used as an appropriate index to determine obesity, but it is not a strong option to indicate the risk of GERD.
In a study conducted by Nocon et al [15], environmental factors such as food, alcohol and smoking, have been introduced as the main risk factors in the prevalence and severity of GERD. Mansour-Ghenaei et al [10] showed a significant statistical relationship between the prevalence of GERD and smoking. Also, in another study published by Locke et al [16] dealt with evaluating the risk factors accompanying with the symptoms of GERD, smoking and alcohol consumption were significantly related to the frequency of GERD symptoms. In contrast, our survey showed no significant differences of smoking and alcohol consumption between patients and controls or NERD and ERD subgroups.
Same as others survey [10,12,17,18], evaluation of dietary habits and drug history in our study showed a direct relationship between GERD and consumption of NSAIDs, eating fatty and spicy foods, drinking beverages with the meal and lying after eating. Also, this study stated that there is a significant statistical relationship between ERD and eating spicy and salty-smoky foods.
Lying after meal is an Asian habit which can lead to lower esophagus sphincter weakening and acid or food regurgitation. This study showed that this wrong habit increases the risk of GERD.
PH of many beverages such as soda is 2.5-3.5, so they cause an acidic environment in the stomach. In the total path of digestive system, only the stomach can withstand such acidic state. But other parts of digestive system like mouth, throat and esophagus are very sensitive and vulnerable to the lower levels of PH. Phosphoric acid in such drinks influence on the stomach by competing with hydrochloric acid. In such circumstances, the stomach is inefficient and the remaining food causes indigestion and bloating. So we can say that patients with GERD must avoid drinking beverages with the meal, especially soda.
The spread of western food culture among the Asians is increasing the prevalence of GERD [19]. since GERD is one of the main risk factors in the field of gastric cancer, prevention of eating foods with high levels of nitrate (like salty-smoky foods which are so common in Iranian food habits), spicy foods (like Indian foods) and all kind of fast foods (Western foods) should be considered as an important task in health programs and the ministry of health should invest more in the field of food culture and place it on its long-term plans.
In conclusion, this case-control study confirms that obesity is an important risk factor for GERD. Other possible risk factors such as consumption of NSAIDs and certain foods and wrong habits like lying after meal should be addressed in future longitudinal surveys.
Acknowledgements
We thank Dr. Zahra Haghparast Ghadim Limudahi and Dr. Ehsan Kazemnejhad Leili for critical reading of the manuscript and for the insightful suggestions. This manuscript is a part of internist thesis.
Disclosure of conflict of interest
None.
References
- 1.Badillo R, Francis D. Diagnosis and treatment of gastroesophageal reflux disease. World J Gastrointest Pharmacol Ther. 2014;5:105–112. doi: 10.4292/wjgpt.v5.i3.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu YW, Tseng PH, Lee YC, Wang SY, Chiu HM, Tu CH, Wang HP, Lin JT, Wu MS, Yang WS. Association of esophageal inflammation, obesity and gastroesophageal reflux disease: from FDG PET/CT perspective. PLoS One. 2014;9:e92001. doi: 10.1371/journal.pone.0092001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Islami F, Pourshams A, Nasseri-Moghaddam S, Khademi H, Poutschi H, Khoshnia M, Norouzi A, Amiriani T, Sohrabpour AA, Aliasgari A. Gastroesophageal Reflux Disease and overall and Cause-specific Mortality: A Prospective Study of 50000 Individuals. Middle East J Dig Dis. 2014;6:65–80. [PMC free article] [PubMed] [Google Scholar]
- 4.Liakakos T, Karamanolis G, Patapis P, Misiakos EP. Gastroesophageal reflux disease: medical or surgical treatment? Gastroenterol Res Pract. 2009;2009:371580. doi: 10.1155/2009/371580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahadeva S, Raman M, Ford A, Follows M, Axon A, Goh KL, Moayyedi P. Gastro-oesophageal reflux is more prevalent in Western dyspeptics: a prospective comparison of British and South-East Asian patients with dyspepsia. Aliment Pharmacol Ther. 2005;21:1483–1490. doi: 10.1111/j.1365-2036.2005.02455.x. [DOI] [PubMed] [Google Scholar]
- 6.Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007;41:131–137. doi: 10.1097/01.mcg.0000225631.07039.6d. [DOI] [PubMed] [Google Scholar]
- 7.Sugimoto M, Nishino M, Kodaira C, Yamade M, Uotani T, Ikuma M, Umemura K, Furuta T. Characteristics of non-erosive gastroesophageal reflux disease refractory to proton pump inhibitor therapy. World J Gastroenterol. 2011;17:1858–1865. doi: 10.3748/wjg.v17.i14.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jonasson C, Wernersson B, Hoff DA, Hatlebakk JG. Validation of the Gerd Q questionnaire for the diagnosis of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2013;37:564–572. doi: 10.1111/apt.12204. [DOI] [PubMed] [Google Scholar]
- 9.Wienbeck M, Babnert J. Epidemiology of reflux disease and reflux esophagitis. Scand J Gastroenterol Suppl. 1989;24:7–13. doi: 10.3109/00365528909091032. [DOI] [PubMed] [Google Scholar]
- 10.Mansour-Ghanaei F, Joukar F, Atshani SM, Chagharvand S, Souti F. The epidemiology of gastroesophageal reflux disease: a survey on the prevalence and the associated factors in a random sample of the general population in the Northern part of Iran. Int J Mol Epidemiol Genet. 2013;4:175–182. [PMC free article] [PubMed] [Google Scholar]
- 11.Murray L, Johnston B, Lane A, Harvey I, Donovan J, Nair P, Harvey R. Relationship between body mass and gastro-oesophageal reflux symptoms: The Bristol Helicobacter Project. Int J Epidemiol. 2003;32:645–650. doi: 10.1093/ije/dyg108. [DOI] [PubMed] [Google Scholar]
- 12.Klauser A, Schindlbeck N, Müller-Lissner S. Symptoms in gastro-oesophageal reflux disease. Lancet. 1990;335:205–208. doi: 10.1016/0140-6736(90)90287-f. [DOI] [PubMed] [Google Scholar]
- 13.Wajed SA, Streets CG, Bremner CG, DeMeester TR. Elevated body mass disrupts the barrier to gastroesophageal reflux. Arch Surg. 2001;136:1014–1019. doi: 10.1001/archsurg.136.9.1014. [DOI] [PubMed] [Google Scholar]
- 14.Blondeau K, Boecxstaens V, Van Oudenhove L, Farre R, Boeckxstaens G, Tack J. Increasing body weight enhances prevalence and proximal extent of reflux in GERD patients ‘on’ and ‘off’ PPI therapy. Neurogastroenterol Motil. 2011;23:724–e327. doi: 10.1111/j.1365-2982.2011.01720.x. [DOI] [PubMed] [Google Scholar]
- 15.Nocon M, Labenz J, Willich S. Lifestyle factors and symptoms of gastro-oesophageal reflux-a population-based study. Aliment Pharmacol Ther. 2006;23:169–174. doi: 10.1111/j.1365-2036.2006.02727.x. [DOI] [PubMed] [Google Scholar]
- 16.Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Risk factors associated with symptoms of gastroesophageal reflux. Am J Med. 1999;106:642–649. doi: 10.1016/s0002-9343(99)00121-7. [DOI] [PubMed] [Google Scholar]
- 17.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 18.Bashashati M, Hejazi RA, Andrews CN, Storr MA. Gastroesophageal reflux symptoms not responding to proton pump inhibitor: GERD, NERD, NARD, esophageal hypersensitivity or dyspepsia? Can J Gastroenterol Hepatol. 2014;28:335–341. doi: 10.1155/2014/904707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jung HK. Epidemiology of gastroesophageal reflux disease in Asia: a systematic review. J Neurogastroenterol Motil. 2011;17:14–27. doi: 10.5056/jnm.2011.17.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]


