Abstract
AIM: To investigate the effects and mechanisms of melatonin on immunological liver injury in mice.
METHODS: A model of liver injury was induced by tail vein injection of Bacillus Calmette Guerin (BCG) and lipopolysaccharide (LPS) in mice. Kupffer cells and hepatocytes were isolated and cultured according to a modified two-step collagenase perfusion technique. Levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST) and nitric oxide (NO), content of malondiadehyde (MDA), activity of superoxide dismutase (SOD), were measured by biochemical methods. Tumor necrosis factor-α (TNF-α) activity was determined by RIA. Interleukin (IL)-1 activity was measured by thymocyte proliferation bioassay. Hepatic tissue sections were stained with hematoxylin and eosin and examined under a light microscope.
RESULTS: Immunological liver injury induced by BCG+LPS was successfully duplicated. Serum transaminase (ALT, AST) activities were significantly decreased by melatonin (0.25, 1.0, 4.0 mg/kg bm). Meanwhile, MDA content was decreased and SOD in liver homogenates was upregulated. Furthermore, pro-inflammatory mediators (TNF-α, IL-1, NO) in serum and liver homogenates were significantly reduced by melatonin. Histological examination demonstrated that melatonin could attenuate the area and extent of necrosis, reduce the immigration of inflammatory cells. In in vitro experiment, TNF-α was inhibited at the concentrations of 10-8-10-6 mol/L of melatonin, while IL-1 production of Kupffer cells induced by LPS (5 μg/mL) was decreased only at the concentration of 10-6 mol/L of melatonin, but no effect on NO production was observed. Immunological liver injury model in vitro was established by incubating hepatocytes with BCG- and LPS-induced Kupffer cells. Activities of ALT, TNF-α, IL-1, and MDA in supernatant were significantly increased. Melatonin had little effect on the level of ALT, but reduced the content of TNF-α and MDA at concentrations of 10-7-10-5 mol/L and decreased the content of IL-1 at concentrations of 10-6-10-5 mol/L.
CONCLUSION: Melatonin could significantly protect liver injury in mice, which was related to free radical scavenging, increased SOD activity and pro-inflammatory mediators.
INTRODUCTION
Viral infection, alcoholic or drug toxicity, or any other factors that cause damage to hepatocytes elicit an inflammatory reaction in the liver. The damaged hepatocytes, their membrane components, metabolites of toxic agents, and infiltrating inflammatory cells are the activators of Kupffer cells. Kupffer cells, the resident macrophages in the sinusoids of the liver, play significant roles in immunomodulation, phagocytosis, and biochemical attack[1,2]. It has been reported that Kupffer cells to be activated are considered the key evidence in the pathophysiology of many animal models of hepatic injury[3-8]. Activated Kupffer cells contribute to the onset of liver injury by producing and releasing cytotoxic agents such as pro-inflammatory cytokines including tumor necrosis factor alpha (TNF-α)[9,10], interleukin-1 (IL-1)[9], interleukin-6 (IL-6) and active oxygen[11], nitric oxide (NO)[8] which damage sinusoidal endothelial cells and hepatocytes. Previous studies have shown that elimination of Kupffer cells by gadolinium chloride[5] and TNF-α antibodies are effective on reducing hepatic damage in vivo.
Ferluga et al[13] first reported the P. acnes-primed LPS-induced hepatic shock model in mice in 1978[12], and three years later Ferluga also reported that LPS injection subsequent to the priming of Bacillus Calmette-Guerin (BCG) provoked the same hepatic injury in mice. Since then, many investigators have tried to explain the mechanism of the above two similar models[14,15]. It is known that P. acnes or BCG priming and LPS challenge in mice cause massive liver injury, which consists of priming and eliciting phases. P. acnes or BCG priming induces mononuclear cell infiltration into the liver lobules and granuloma formation[16]. The subsequent LPS injection elicits acute and massive hepatic injury, with a concomitant release of various cytokines and active free radicals[17-21]. Thus, in immunological liver injury model induced by BCG and LPS, hepatocyte damage is presumably caused by immunological mechanisms. Pro-inflammatory cytokines and active free radicals produced by activated Kupffer cells play an important role in the progress of the resulted liver injury. This experimental immunological liver injury has frequently been used as a model for testing and developing new drugs[12,13,22-24].
The hormone melatonin (N-acetyl-5-methoxytryptamine) is synthesized by pineal gland. Melatonin participates in many important physiological functions, including anti-inflammation[25] and immunoregulation[26,27], as well as acting as a broad spectrum antioxidant[28-30]. In addition, melatonin protects against liver injury induced by endotoxin shock[31,32] and ischemia/reperfusion[33,34] in rats through its antioxidant action. The purpose of this study was to investigate whether exogenous melatonin would protect against BCG- and LPS-induced immunological liver injury in mice via antioxidative and immunoregulatory mechanisms. Meanwhile, the direct effect of melatonin on isolated Kupffer cells or co-cultured Kupffer cells and hepatocytes in vitro was studied.
MATERIALS AND METHODS
Materials
Melatonin, purchased from Sigma Chemical Co. (St Louis, Mo, USA), was dissolved in 9 g/L saline with absolute ethanol (</=0.1 mL/L) and stored at -20 °C. 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetra-zolium bromide (MTT), RPMI 1640, Hepes buffer, collagenase IV, Pronase E, DNase, Nycodenz and LPS from Escherichia coli were obtained from Sigma Chemical Co (St Louis, Mo, USA). Commercial kits used for determining lipid peroxidation and superoxide dismutase (SOD) activity were obtained from the Jiancheng Institute of Biotechnology (Nanjing, China). Other chemicals used in these experiments were of analytical grade from commercial sources.
Animals
Male Sprague-Dawley (SD) rats (300 ± 20 g), C57BL/6J mice (18 ± 2 g) and m ale Kunming mice (20 ± 2 g), obtained from the Animal Department of Anhui Medical University, were maintained on a 12 h light/dark cycle from 6AM to 6PM in a controlled environment (20 ± 1 °C). Animals were housed in plastic cages with free access to food and water. All experimental protocols described in this study were approved by the Ethics Review Committee for Animal Experimentation of Institute of Clinical Pharmacology, Anhui Medical University.
Establishment of immunological liver injury model[8,13]
A 2.5 mg dose of BCG (viable bacilli) suspended in 0.2 mL saline was injected via the tail vein into each animal, and 10 d later, 7.5 µg LPS dissolved in 0.2 mL saline was injected. Mice were anesthetized with ether, then sacrificed by cervical dislocation 16 h after LPS injection and trunk blood was collected into heparinized tubes (50 U/mL) and centrifuged (1500 r/min, 10 min, 4 °C). Serum was aspirated and stored at -70 °C until assayed as described below. The liver was also removed and stored at -70 °C until required.
Drug treatment
In vivo experiment, the animals were equally divided into 5 groups randomly, including normal, model control and melatonin groups (3 different doses). Mice in melatonin groups were received daily doses of 0.25, 1.0 or 4.0 mg/kg bm of melatonin using an 18-gauge stainless steel animal feeding needle for 10 d prior to LPS injection. Mice in normal and model control group were only fed the same volume of vehicle.
In in vitro experiment, after Kupffer cells were isolated from normal rat, the cells were divided into 7 groups randomly, including control cells, cells added with LPS (5 µg/mL) alone, cells added with LPS (5 µg/mL) simultaneously with melatonin (5 different concentrations including 10-9, 10-8, 10-7, 10-6, 10-5 mol/L). Every group had triplicate wells and the experiment above was repeated twice.
In another in vitro experiment, after Kupffer cells were isolated from BCG priming rat and hepatocytes isolated from normal rat, the two types of cells were divided into 7 groups randomly, including control cells, cells added with LPS (5 µg/mL) alone, cells added with LPS (5 µg/mL) simultaneously with melatonin (5 different concentrations including 10-9, 10-8, 10-7, 10-6, 10-5 mol/L). Every group had triplicate wells and the experiment above was repeated twice.
Isolation and culture of Kupffer cells and hepatocytes
In vitro experiment, the direct effect of melatonin on Kupffer cells was studied by isolating Kupffer cells from the livers of normal rat. Rat liver perfusion was performed using a modification of the two-step collagenase perfusion technique introduced by previous studies[35,36].
In brief, the rat liver was perfused through the portal vein with D-Hank’s until blood free, and then with Hank’s containing 0.5 g/L collagenase IV. The latter was administered by recirculation until the vessels were digested (up to 20 min). The liver was then scraped using a cell scraper, filtered through a 100-µm filter, and stirred in Hank’s containing 2.5 g/L pronase and 0.05 g/L DNase for 20 min at 37 °C. After three times of centrifugation and washing at 300 × g for 10 min at 4 °C in Gey’s balanced salt solution (GBSS), cells were centrifuged in an 180 g/L Nycodenz gradient at 2500 × g for 20 min. Kupffer cells were carefully sucked by cusp-straws at the pearl layer inderphase. At last, purified Kupffer cell fractions were obtained by centrifugal elutriation. The viability of Kupffer cells prepared was more than 95% as determined by trypan blue exclusion. The purity of Kupffer cells was greater than 90% based on a peroxidase activity assay[37].
Kupffer cells, obtained as described above, were washed with Hanks’ and resuspended in RPMI 1640 medium containing antibiotics (penicillin, 100 U/mL; streptomycin, 100 mg/mL), 2 mmol/L glutamine, and 100 mL/L fetal calf serum. One-milliliter aliquots containing 1 × 106 cells were added to 24-well culture plates. The cells were incubated for 60 min in a humidified atmosphere containing 50 mL/L CO2 at 37 °C. Nonadherent cells were removed, and adherent cells were washed twice with PBS. The cells at a density of 1 × 106/mL were incubated with different concentrations of melatonin (10-9, 10-8, 10-7, 10-6, 10-5 mol/L). They (1 × 106/well) were cultured for 48 h with 5 µg/mL LPS and the supernatants were collected and TNF-α and NO concentration measured with the methods described below.
In in vitro liver injury model, BCG induced Kupffer cells were isolated from the livers of the rats which were injected via the tail vein with 3 mg of BCG 10 d before, at the same time hepatocytes isolated from normal rat. The hepatocytes at a density of 1 × 109/mL were incubated with different concentrations of melatonin (10-9, 10-8, 10-7, 10-6, 10-5 mol/L) and BCG-induced Kupffer cells (1 × 106/well). They were co-cultured for 48 h with 5 µg/mL LPS and the supernatants were collected.
Measurement of serum ALT and AST
Serum ALT and AST were determined using commercial kits produced by Jiancheng Institute of Biotechnology (Nanjing, China). Their activities were expressed as an international unit (U/L).
Measurement of NO in serum and cell culture supernatants
Nitric oxide (NO) in Kupffer cells was measured by a microplate assay using Griess reagent, which produces a chromophore with the nitrite[38]. Briefly, 100 µL of cell culture supernatants was removed and incubated with 100 µL of Griess reagent (10 g/L sulfanilamide and 1 g/L N-1-naphthylethylenediamine dihydrochloride in 25 mL/L phosphoric acid) in a 96-well plate. The plate was incubated for 10 min at room temperature. Nitrite production was quantified spectrophotometrically using an automated colorimetric procedure. Absorbance at 540 nm was measured using a microplate reader (Bio-Tek, USA). The nitrite concentration was calculated by comparing samples with standard solutions of sodium nitrite produced in the culture medium. All samples were assayed in triplicate. Results were expressed as µmol/L.
Measurement of MDA and SOD in liver homogenates
Livers were thawed, weighed and homogenized with Tris-HCl (5 mmol/L containing 2 mmol/L EDTA, pH7.4). Homogenates were centrifuged (1000 r/min, 10 min, 4 °C) and the supernatant was used immediately for the assays of MDA and SOD. MDA and SOD were determined following the instructions of the kit. In brief, MDA in liver tissue was determined by the thiobarbituric acid method[39]. All samples were assayed in triplicate. The content of MDA was expressed as nmol per gram liver tissue. The assay for total SOD was based on its ability to inhibit the oxidation of oxyamine by the xanthine-xanthine oxidase system. The red product (nitrite) produced by the oxidation of oxyamine has an absorbance at 550 nm. One unit (U) of SOD activity was defined as the quantity that reduced the absorbance at 550 nm by 50%. All samples were assayed in triplicate. Results were expressed as U per gram liver tissue.
Measurement of TNF-α in serum and cell culture supernatants
Serum was assayed according to procedures described by the instruction of the commercial kits. The standard curve of TNF-α measured was between 2 and 160 pg/mL.
Bioassay of IL-1 activity in serum and cell culture supernatants
IL-1 activity was measured by mouse thymocyte activation assayed by MTT (Sigma) reduction[40]. MTT was dissolved in sterile PBS to a concentration of 5 mg/mL and stored in the dark at 4 °C for up to 1 wk. Immediately before use, stock MTT was filtered (0.22 µm) to remove any formazan precipitate. Thymocytes (2 × 106/well) from mice were cultured for 48 h in 96-well plates containing RPMI 1640 medium supplemented with 5 µg/mL concanavalin A and 0.1 mL collected supernatants in triplicate. Three hours before the termination of culture, cells were pulsed with MTT stock (20 µL/well), returned to 37 °C and incubated for another 3 h. The plates were centrifuged for 10 min at 1000 g to cell pellets and MTT formazan products. The supernatant was carefully aspirated without disturbing the pellets, and formazan was solubilized by addition of isopropanol (100 µL/200 µL supernatant). Insoluble material was then removed by centrifugation for 10 min at 1000 g. The solubilized formazan in isopropanol was collected and distributed into 12-well flat-bottom ELASA plates at a final volume of 100 µL/well. Plates were read at 570 nm in EL 301 Strip Reader (Bio-Tek, USA) within 1 h of addition of isopropanol. Values were expressed as mean absorbance (A) of triplicate wells.
Histological analysis
Formalin-fixed specimens were embedded in paraffin and stained with hematoxylin and eosin for conventional morphological evaluation. After decapitation of rats, small liver specimens were placed in 100 mL/L formalin solution and processed routinely by embedding in paraffin. Tissue sections (4-5 µm) were stained with hematoxylin and eosin and examined under light microscope (Olympus). An experienced histologist who was unaware of the treatment conditions made histological assessments.
Statistical analyses
All values were presented as mean ± SE. Statistical analysis of the data for multiple comparisons was performed by one-way analysis of variance (ANOVA) followed by Duncan’s test. For a single comparison, the significance of differences between means was determined by the t-test, A level of P < 0.05 was accepted as statistical significant.
RESULTS
Effect of melatonin on serum ALT and AST
Activities of both serum AST and ALT, indices of hepatic cell damage, were significantly higher in BCG- and LPS-induced group than in the control group. Melatonin (0.25, 1.0, 4.0 mg/kg bm) significantly reduced the activities of serum AST and ALT (Table 1).
Table 1.
Effects of melatonin on serum ALT and AST activities in immunological liver injury in mice (n = 10, mean ± SE)
| Group | Dose (mg/kg bm) | ALT (U/L) | AST (U/L) |
| Normal | --- | 28.2 ± 8.8 | 26.8 ± 8.5 |
| Model | --- | 224 ± 40d | 205 ± 40d |
| Melatonin | 0.25 | 187 ± 21a | 129 ± 13b |
| 1.0 | 119 ± 41b | 124 ± 36b | |
| 4.0 | 163 ± 44b | 162 ± 33a |
P < 0.05,
P < 0.01 vs model group;
P < 0.01 vs normal control group.
Effect of melatonin on liver homogenate MDA and total SOD
Liver homogenate malondialdehyde (MDA) content in BCG- and LPS-induced group was significantly higher than that in the control group while liver total SOD activity was lower. Melatonin (0.25, 1.0, 4.0 mg/kg bm) significantly attenuated MDA generation and increased liver total SOD activity (Table 2).
Table 2.
Effects of melatonin on MDA level and SOD activity of liver homogenates of immunological injury mice (n = 10, mean ± SE)
| Group | Dose (mg/kg bm) | MDA (nmol/g tissue) | SOD (U/g tissue) |
| Normal | --- | 92 ± 26 | 297 ± 22 |
| Model | --- | 439 ± 25d | 202.46 ± 26d |
| Melatonin | 0.25 | 335 ± 37b | 266 ± 71b |
| 1.0 | 332 ± 28b | 273 ± 31b | |
| 4.0 | 346 ± 17b | 244 ± 27b |
aP < 0.05,
P < 0.01 vs model group;
P < 0.01 vs normal control group.
Effect of melatonin on serum and liver homogenate TNF-α, IL-1 and NO concentration
As shown in Table 3, when mice were first injected with BCG and then challenged with LPS, the levels of TNF-α, IL-1 and NO were elevated significantly. Melatonin (0.25, 1.0 and 4.0 mg/kg bm) obviously reversed these effects. Similarly, in liver homogenates of immunological injury mice the levels of above three indices increased and melatonin (0.25, 1.0 and 4.0 mg/kg bm) significantly inhibited the production of TNF-α and NO while melatonin (4 mg/kg bm) inhibited IL-1(Table 4).
Table 3.
Effects of melatonin on serum TNF-α, IL-1 and NO levels in immunological liver injury mice (n = 10, mean ± SE)
| Group | Dose (mg/kg bm) | TNF-α (ng/L) | IL-1 (A570 nm) | NO (μmol/L) |
| Normal | --- | 1.61 ± 0.76 | 0.107 ± 0.001 | 9.82 ± 1.92 |
| Model | --- | 4.80 ± 1.61d | 0.242 ± 0.03d | 73 ± 19d |
| Melatonin | 0.25 | 3.42 ± 1.08a | 0.183 ± 0.07a | 55 ± 18a |
| 1.0 | 3.26 ± 0.73a | 0.131 ± 0.04b | 28 ± 14b | |
| 4.0 | 2.64 ± 1.19b | 0.158 ± 0.04b | 56 ± 19a |
P < 0.05,
P < 0.01 vs model group;
P < 0.01 vs normal control group.
Table 4.
Effects of melatonin on TNF-α, IL-1 and NO levels of liver homogenates in immunological injury mice (n = 10, mean ± SE)
| Group | Dose (mg/kg bm) | TNF-α (ng/L) | IL-1 (A570 nm) | NO (μmol/L) |
| Normal | --- | 3.1 ± 8.3 | 0.15 ± 0.03 | 9.5 ± 2.7 |
| Model | --- | 26.6 ± 2.3d | 0.41 ± 0.03d | 45.0 ± 9.8d |
| Melatonin | 0.25 | 13.9 ± 2.9b | 0.38 ± 0.13 | 25.6 ± 9.5b |
| 1.0 | 12.4 ± 2.9b | 0.22 ± 0.05b | 17 ± 11b | |
| 4.0 | 17.9 ± 4.8b | 0.35 ± 0.04b | 24 ± 10b |
aP < 0.05,
P < 0.01vs model group;
P < 0.01 vs normal control group.
Effect of melatonin on NO, TNF-α and IL-1 production of isolated Kupffer cells
In vitro, melatonin at the concentrations of 10-8-10-6 mol/L was able to inhibit directly the production of TNF-α while only at the concentrations of 10-6 mol/L decreased IL-1 production of Kupffer cells co-cultured with LPS (5 µg/mL). However, melatonin had no effect on NO production (Table 5).
Table 5.
Effect of melatonin on TNF-α, IL-1 and NO released from cultured normal Kupffer cells of rats (n = 10, mean ± SE)
| Group | Concentration of melatonin (mol/L) | TNF-α (ng/L) | IL-1 (A570 nm) | NO (μmol/L) |
| KC | --- | 4.25 ± 0.79 | 0.137 ± 0.03 | 13.65 ± 0.21 |
| KC + LPS | 11.21 ± 1.63d | 0.233 ± 0.03d | 18.85 ± 0.88d | |
| KC + LPS + melatonin | 10-9 | 9.96 ± 0.24 | 0.238 ± 0.02 | 19.08 ± 0.40 |
| 10-8 | 9.31 ± 0.53a | 0.223 ± 0.02 | 19.13 ± 0.46 | |
| 10-7 | 8.35 ± 0.82b | 0.201 ± 0.01 | 18.90 ± 0.77 | |
| 10-6 | 8.01 ± 0.38b | 0.177 ± 0.01b | 18.65 ± 0.61 | |
| 10-5 | 9.74 ± 0.39 | 0.216 ± 0.02 | 18.70 ± 0.57 |
KC: Kupffer cells;
P < 0.05,
P < 0.01 vs model group;
P < 0.01 vs normal control group.
Effect of melatonin on liver injury in mice in vitro
Immunological liver injury model in vitro was established by hepatocytes incubated with BCG- and LPS-induced Kuppfer cells. Activities of ALT, TNF-α, IL-1 and MDA in supernatant were significantly increased. Melatonin had little effect on the level of ALT, but at concentrations of 10-7-10-5 mol/L it reduced the content of TNF-α and MDA while at concentrations of 10-6-10-5 mol/L it decreased the content of IL-1 (Table 6).
Table 6.
Effects of melatonin on MDA, TNF-α and IL-1 released from co-cultured normal rat hepatocytes and Kupffer cells activated by BCG (n = 5, mean ± SE)
| Group | Concentration of melatonin (mol/L) | ALT (U/L) | MDA (nmol/L) | TNF-α (ng/L) | IL-1 (A570 nm) |
| KC + HC | --- | 37.1 ± 3.7 | 0.506 ± 0.029 | 4.50 ± 0.78 | 0.16 ± 0.03 |
| KC + HC + LPS | 81.4 ± 6.4d | 0.849 ± 0.062d | 11.36 ± 1.6d | 0.25 ± 0.03d | |
| KC + HC + LPS + Melatonin | 10-9 | 82.4 ± 4.3 | 0.809 ± 0.015 | 10.13 ± 0.23 | 0.26 ± 0.02 |
| 10-8 | 79.6 ± 5.4 | 0.789 ± 0.036 | 9.49 ± 0.52 | 0.24 ± 0.02 | |
| 10-7 | 74.9 ± 4.2 | 0.706 ± 0.014b | 8.54 ± 0.81b | 0.22 ± 0.01 | |
| 10-6 | 72.9 ± 6.6 | 0.676 ± 0.043b | 8.21 ± 0.37b | 0.19 ± 0.01a | |
| 10-5 | 83.8 ± 3.3 | 0.69 ± 0.04b | 8.39 ± 1.22b | 0.20 ± 0.01b |
KC: Kupffer cell;
P < 0.05,
P < 0.01 vs model group;
P < 0.01 vs normal control group.
Histological results
In normal group, there was no pathological abnormality. Liver parenchyma was in good morphology and hepatocytes were arranged around the central vein. No congestion and inflammation were observed in the sinusoids (Figure 1A).
Figure 1.
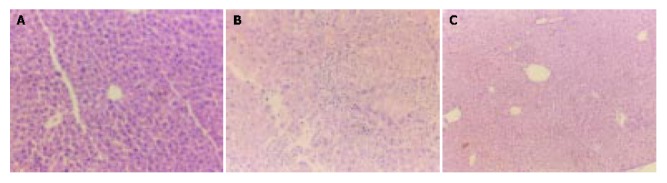
Histological results of tissues stained with hematoxylin and eosin under light microscope. A: Normal control group; B: Model group; C: Melatonin-treated group.
In model group, there was a severe pathological abnormality. Hepatocytes were with marked vacuolization, moreover, hepatocytes dot necrosis, striped necrosis, bridging necrosis appeared and inflammatory cells arranged around the necrotic tissue. Congestion in liver sinusoids was significant with scattered infiltration of inflammatory cells (Figure 1B).
In melatonin-treated group, the area and extent of necrosis attenuated and the immigration of inflammatory cells reduced. Liver parenchyma was well preserved with radially arranged hepatocytes around the central vein. Regular sinusoidal structures were seen without congestion (Figure 1C).
DISCUSSION
Injection of BCG followed by LPS is useful for the creation of experimental models of acute hepatic damage[13,16,22,41]. In the present study, immunological liver injury in mice was successfully induced by BCG and LPS and the model in vitro also duplicated. On this basis, administration of melatonin in vivo resulted in marked reduction of acute liver injury, as demonstrated by significant reduction of serum transaminase concentration and amelioration of severe hepatic pathological abnormalities. Meanwhile, melatonin decreased MDA content and increased total SOD activity in liver homogenates. Furthermore, melatonin significantly reduced TNF-α, IL-1 and NO production in serum and liver homogenates. The in vitro experiment also supported the direct protective role of melatonin in suppression of Kupffer cell function. Although melatonin had no direct protection on hepatocytes injury in vitro induced by BCG and LPS, it could inhibit the production of MDA and pro-inflammatory cytokines such as TNF-α and IL-1. Based on the current results, we propose that the mode of melatonin’s hepatic protective action is, at least in part, related to its antioxidative and immunoregulatory properties.
As it is well known, melatonin, the chief secretory product of the pineal gland, was found to be a multi-faceted free radical scavenger and antioxidant. It detoxifies a variety of free radicals and reactive oxygen intermediates, including the hydroxyl radical, singlet oxygen, peroxynitrite anion and nitric oxide[29,30]. In both in vitro and in vivo experiments, melatonin has been found to protect cells, tissues, and organs against oxidative damage induced by a variety of free-radical-generating agents and processes, e.g., the carcinogen safrole, LPS, carbon tetrachloride, ischemia-reperfusion, amyloid-protein, and ionizing radiation[42,43]. Melatonin also has been reported to stimulate the activities of enzymes and increase gene expression that improves the total antioxidative defense capacity of the organism, i.e., SOD, glutathione peroxidase, glutathione reductase[44,45]. Moreover, recent studies indicate that melatonin is effective on inhibiting oxidative liver damage. Calvo et al[46] found that melatonin protected against ANIT-induced liver injury with cholestasis in rats, and suggested that this protective effect was likely due to its antioxidative properties and above all to its capacity to inhibit liver neutrophil infiltration, a critical factor in the pathogenesis of ANIT-induced liver injury. Melatonin also could dose-dependently reduce liver lipid peroxide content in CCl4 treated rats. This indicated that melatonin exerted a therapeutic effect on CCl4-induced acute liver injury in rats, possibly through its antioxidant action. Melatonin plays a cytoprotective role in the liver insulted by ischemia and reperfusion by virtue of its ability to prevent hepatic malfunction and inhibit the generation of free radicals and accumulation of neutrophils in the damaged hepatic tissue[35]. In the present study, the effects of melatonin on immunological liver injury model were firstly investigated. The results showed that melatonin decreased MDA content in liver homogenates, meanwhile, SOD activity rose significantly. Those results are in accordance with the findings of melatonin’s antioxidant properties.
A growing body of evidence suggests that nitric oxide (NO) may also modulate different experimental liver injuries. The role, that NO plays in the process of liver injury has been the subject of active debate. In vitro and in vivo data suggest that NO may act to protect tissue by virtue of its ability to react with and decompose superoxide radical[47-49]. It has also been suggested that NO may act to modulate the activity of certain transcription factors such as NF-κ B[50]. Although some studies demonstrate that NO may act to limit or down-regulate liver injury, there are other reports suggesting that NO may actually promote hepatocellular damage possibly due to the formation of strongly oxidizing species peroxynitrite[51]. Much of the controversy may be related to the use of non-specific inhibitors of different NOS isoforms and the concentration of NO[52]. Melatonin is reported to inhibit peroxynitrite induced oxidative reactions. Additionally, melatonin under or near physiological concentration inhibits the prooxidative enzyme nitric oxide synthase (NOS) activity[14,49] and thereby influences NO production. It was also reported that melatonin had protective effect in an endotoxic and non-septic shock partly related to prevention of NO overproduction. The present study showed that melatonin significantly inhibited serum NO and did not directly inhibit Kupffer cells and generate NO in vitro. The results demonstrated that melatonin might modulate the generation of NO at a whole body level but had no direct effect on Kupffer cells. It seems likely that melatonin regulated NO production to a certain extent, but more studies should be carried out to clarify it.
As it is well known, TNF-α is a multifunctional cytokine mostly secreted by inflammatory cells and is involved in numerous pathological states. TNF-α is considered to be a common early effector molecule for liver injury, in addition to its direct cytotoxic effects, this cytokine is able to induce chemokines, macrophage chemotactic protein-1 and adhesive molecules, vascular-cell adhesion molecule-1, which are key to inflammation and consequent liver damage[9-11]. Prevention of liver injury has been observed upon neutralization of TNF-α with anti-TNF-α antibody, prevention of translation of primary RNA transcript of TNF-α by antisense oligonucleotide and interaction of TNF-α with soluble TNF-α receptors[53]. Although IL-1 itself does not exert damage on liver, its elevation could stimulate inflammatory cells to excrete many other cytokines including TNF-α, IL-6 and IL-8. Our results suggest that the elevation of inflammatory cytokines including TNF-α and IL-1 in serum, liver homogenates and Kupffer cell culture supernatants contributes to the mechanisms of immunological liver injury.
It is now well recognized that melatonin plays an important immunoregulatory role. Shin et al[54] found that low levels of Bacillus anthracis were known to induce release of cytokines such as TNF-α, and thereby exposure of melatonin (10-7-10-6 mol/L) to anthrax lethal toxin-treated macrophages also decreased the release of TNF-α to extracellular medium as compared to the control. Sacco found that administration of melatonin to mice (5 mg/kg bm, s.c. 30 min before or simultaneously with LPS) inhibited serum TNF-α levels by 50%-80% and improved survival of mice treated with a lethal dose of LPS. Melatonin did not increase serum corticosterone and did not modify the elevation of serum corticosterone levels by LPS or by IL-1. Furthermore, it exerted its inhibitory effect in adrenalectomized or hypophysectomized mice also, indicating that its effect is independent of the hypothalamus-pituitary-adrenal axis[55]. It was previously reported melatonin had a protective role in LPS-induced septic shock by suppressing pro-inflammatory cytokines, prostaglandins and NO production[31,32]. However, other studies indicated melatonin did not alter cytokines including TNF-α and IL-1 secretion by LPS-stimulated macrophages[56]. The inconsistencies in the literature suggested that the effect of melatonin on macrophages was complex. In our experimental condition, we found that in in vitro experiments melatonin at the concentrations of 10-8-10-6 mol/L directly inhibited production of TNF-α while only at the concentrations of 10-6 mol/L decreased IL-1 production of Kupffer cell co-cultured with LPS (5 μg/mL). In in vitro liver injury model,we also found that melatonin at the concentrations of 10-7-10-5 mol/L reduced the content of TNF-α while at concentrations of 10-6-10-5 mol/L decreased the content of IL-1. Even more, in vivo experiment showed that melatonin at the dose between 0.25 mg/kg bm and 4.0 mg/kg bm significantly inhibited serum TNF-α and IL-1 level. Thus suppression of TNF-α and IL-1 could be one of the means by which melatonin attenuated immunological liver injury in mice.
Therefore, the protective effects of melatonin on immunological liver injury might relate to free radical scavenging, increased content of SOD, decreased expression of procytokines.
Footnotes
Supported by Funds From State Key Programs of Science and Technology of China, No. 969010652
Edited by Chen WW and Zhu LH Proofread by Xu FM
References
- 1.Decker K. Biologically active products of stimulated liver macrophages (Kupffer cells) Eur J Biochem. 1990;192:245–261. doi: 10.1111/j.1432-1033.1990.tb19222.x. [DOI] [PubMed] [Google Scholar]
- 2.Edwards MJ, Keller BJ, Kauffman FC, Thurman RG. The involvement of Kupffer cells in carbon tetrachloride toxicity. Toxicol Appl Pharmacol. 1993;119:275–279. doi: 10.1006/taap.1993.1069. [DOI] [PubMed] [Google Scholar]
- 3.elSisi AE, Earnest DL, Sipes IG. Vitamin A potentiation of carbon tetrachloride hepatotoxicity: role of liver macrophages and active oxygen species. Toxicol Appl Pharmacol. 1993;119:295–301. doi: 10.1006/taap.1993.1072. [DOI] [PubMed] [Google Scholar]
- 4.Shiratori Y, Kawase T, Shiina S, Okano K, Sugimoto T, Teraoka H, Matano S, Matsumoto K, Kamii K. Modulation of hepatotoxicity by macrophages in the liver. Hepatology. 2002;8:815–821. doi: 10.1002/hep.1840080420. [DOI] [PubMed] [Google Scholar]
- 5.Kukan M, Vajdová K, Horecký J, Nagyová A, Mehendale HM, Trnovec T. Effects of blockade of Kupffer cells by gadolinium chloride on hepatobiliary function in cold ischemia-reperfusion injury of rat liver. Hepatology. 1997;26:1250–1257. doi: 10.1002/hep.510260524. [DOI] [PubMed] [Google Scholar]
- 6.Kayano K, Sakaida I, Kubota M, Yasunaga M, Okita K. Functional differences between activated and normal rat liver macrophages: LPS uptake capacity by flow cytometric analysis in contrast with TNF-alpha release. Liver. 1995;15:253–259. doi: 10.1111/j.1600-0676.1995.tb00681.x. [DOI] [PubMed] [Google Scholar]
- 7.Arthur MJ, Kowalski-Saunders P, Wright R. Corynebacterium parvum-elicited hepatic macrophages demonstrate enhanced respiratory burst activity compared with resident Kupffer cells in the rat. Gastroenterology. 1986;91:174–181. doi: 10.1016/0016-5085(86)90455-5. [DOI] [PubMed] [Google Scholar]
- 8.Zhang GL, Wang YH, Ni W, Teng HL, Lin ZB. Hepatoprotective role of Ganoderma lucidum polysaccharide against BCG-induced immune liver injury in mice. World J Gastroenterol. 2002;8:728–733. doi: 10.3748/wjg.v8.i4.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muto Y, Nouri-Aria KT, Meager A, Alexander GJ, Eddleston AL, Williams R. Enhanced tumour necrosis factor and interleukin-1 in fulminant hepatic failure. Lancet. 1988;2:72–74. doi: 10.1016/s0140-6736(88)90006-2. [DOI] [PubMed] [Google Scholar]
- 10.Nagakawa J, Hishinuma I, Hirota K, Miyamoto K, Yamanaka T, Tsukidate K, Katayama K, Yamatsu I. Involvement of tumor necrosis factor-alpha in the pathogenesis of activated macrophage-mediated hepatitis in mice. Gastroenterology. 1990;99:758–765. doi: 10.1016/0016-5085(90)90965-4. [DOI] [PubMed] [Google Scholar]
- 11.Arthur MJ, Bentley IS, Tanner AR, Saunders PK, Millward-Sadler GH, Wright R. Oxygen-derived free radicals promote hepatic injury in the rat. Gastroenterology. 1985;89:1114–1122. doi: 10.1016/0016-5085(85)90218-5. [DOI] [PubMed] [Google Scholar]
- 12.Ferluga J, Allison AC. Role of mononuclear infiltrating cells in pathogenesis of hepatitis. Lancet. 1978;2:610–611. doi: 10.1016/s0140-6736(78)92828-3. [DOI] [PubMed] [Google Scholar]
- 13.Ferluga J. Tuberculin hypersensitivity hepatitis in mice infected with Mycobacterium bovis (BCG) Am J Pathol. 1981;105:82–90. [PMC free article] [PubMed] [Google Scholar]
- 14.Tsutsui H, Nakanishi K, Matsui K, Higashino K, Okamura H, Miyazawa Y, Kaneda K. IFN-gamma-inducing factor up-regulates Fas ligand-mediated cytotoxic activity of murine natural killer cell clones. J Immunol. 1996;157:3967–3973. [PubMed] [Google Scholar]
- 15.Smith SR, Calzetta A, Bankowski J, Kenworthy-Bott L, Terminelli C. Lipopolysaccharide-induced cytokine production and mortality in mice treated with Corynebacterium parvum. J Leukoc Biol. 1993;54:23–29. doi: 10.1002/jlb.54.1.23. [DOI] [PubMed] [Google Scholar]
- 16.Tsuji H, Harada A, Mukaida N, Nakanuma Y, Bluethmann H, Kaneko S, Yamakawa K, Nakamura SI, Kobayashi KI, Matsushima K. Tumor necrosis factor receptor p55 is essential for intrahepatic granuloma formation and hepatocellular apoptosis in a murine model of bacterium-induced fulminant hepatitis. Infect Immun. 1997;65:1892–1898. doi: 10.1128/iai.65.5.1892-1898.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fujioka N, Mukaida N, Harada A, Akiyama M, Kasahara T, Kuno K, Ooi A, Mai M, Matsushima K. Preparation of specific antibodies against murine IL-1ra and the establishment of IL-1ra as an endogenous regulator of bacteria-induced fulminant hepatitis in mice. J Leukoc Biol. 1995;58:90–98. doi: 10.1002/jlb.58.1.90. [DOI] [PubMed] [Google Scholar]
- 18.Ikeda N, Mukaida N, Kaneko S, Fujioka N, Su S, Nariuchi H, Unoura M, Harada K, Nakanuma Y, Kobayashi K. Prevention of endotoxin-induced acute lethality in Propionibacterium acnes-primed rabbits by an antibody to leukocyte integrin beta 2 with concomitant reduction of cytokine production. Infect Immun. 1995;63:4812–4817. doi: 10.1128/iai.63.12.4812-4817.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu P, Ohnishi H, Moriwaki H, Muto Y. Enhanced tumor necrosis factor and interleukin-1 in an experimental model of massive liver cell necrosis/fatal hepatitis in mice. Gastroenterol Jpn. 1990;25:339–342. doi: 10.1007/BF02779448. [DOI] [PubMed] [Google Scholar]
- 20.Tsuji H, Mukaida N, Harada A, Kaneko S, Matsushita E, Nakanuma Y, Tsutsui H, Okamura H, Nakanishi K, Tagawa Y, et al. Alleviation of lipopolysaccharide-induced acute liver injury in Propionibacterium acnes-primed IFN-gamma-deficient mice by a concomitant reduction of TNF-alpha, IL-12, and IL-18 production. J Immunol. 1999;162:1049–1055. [PubMed] [Google Scholar]
- 21.Tsutsui H, Matsui K, Kawada N, Hyodo Y, Hayashi N, Okamura H, Higashino K, Nakanishi K. IL-18 accounts for both TNF-alpha- and Fas ligand-mediated hepatotoxic pathways in endotoxin-induced liver injury in mice. J Immunol. 1997;159:3961–3967. [PubMed] [Google Scholar]
- 22.Yao HW, Li J, Jin Y, Zhang YF, Li CY, Xu SY. Effect of leflunomide on immunological liver injury in mice. World J Gastroenterol. 2003;9:320–323. doi: 10.3748/wjg.v9.i2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shands JW, Senterfitt VC. Endotoxin-induced hepatic damage in BCG-infected mice. Am J Pathol. 1972;67:23–40. [PMC free article] [PubMed] [Google Scholar]
- 24.Nagai H, Yakuo I, Yamada H, Shimazawa T, Koda A, Niu K, Asano K, Shimizu T, Kasahara M. Liver injury model in mice for immunopharmacological study. Jpn J Pharmacol. 1988;46:247–254. doi: 10.1254/jjp.46.247. [DOI] [PubMed] [Google Scholar]
- 25.Cuzzocrea S, Reiter RJ. Pharmacological actions of melatonin in acute and chronic inflammation. Curr Top Med Chem. 2002;2:153–165. doi: 10.2174/1568026023394425. [DOI] [PubMed] [Google Scholar]
- 26.Guerrero JM, Reiter RJ. Melatonin-immune system relationships. Curr Top Med Chem. 2002;2:167–179. doi: 10.2174/1568026023394335. [DOI] [PubMed] [Google Scholar]
- 27.Skwarlo-Sonta K. Melatonin in immunity: comparative aspects. Neuro Endocrinol Lett. 2002;23 Suppl 1:61–66. [PubMed] [Google Scholar]
- 28.Reiter RJ, Tan DX, Manchester LC, Qi W. Biochemical reactivity of melatonin with reactive oxygen and nitrogen species: a review of the evidence. Cell Biochem Biophys. 2001;34:237–256. doi: 10.1385/CBB:34:2:237. [DOI] [PubMed] [Google Scholar]
- 29.Reiter RJ, Tan DX, Osuna C, Gitto E. Actions of melatonin in the reduction of oxidative stress. A review. J Biomed Sci. 2000;7:444–458. doi: 10.1007/BF02253360. [DOI] [PubMed] [Google Scholar]
- 30.Tan DX, Reiter RJ, Manchester LC, Yan MT, El-Sawi M, Sainz RM, Mayo JC, Kohen R, Allegra M, Hardeland R. Chemical and physical properties and potential mechanisms: melatonin as a broad spectrum antioxidant and free radical scavenger. Curr Top Med Chem. 2002;2:181–197. doi: 10.2174/1568026023394443. [DOI] [PubMed] [Google Scholar]
- 31.Sewerynek E, Melchiorri D, Reiter RJ, Ortiz GG, Lewinski A. Lipopolysaccharide-induced hepatotoxicity is inhibited by the antioxidant melatonin. Eur J Pharmacol. 1995;293:327–334. doi: 10.1016/0926-6917(95)90052-7. [DOI] [PubMed] [Google Scholar]
- 32.Maestroni GJ. Melatonin as a therapeutic agent in experimental endotoxic shock. J Pineal Res. 1996;20:84–89. doi: 10.1111/j.1600-079x.1996.tb00244.x. [DOI] [PubMed] [Google Scholar]
- 33.Sewerynek E, Reiter RJ, Melchiorri D, Ortiz GG, Lewinski A. Oxidative damage in the liver induced by ischemia-reperfusion: protection by melatonin. Hepatogastroenterology. 1996;43:898–905. [PubMed] [Google Scholar]
- 34.Sener G, Tosun O, Sehirli AO, Kaçmaz A, Arbak S, Ersoy Y, Ayanoğlu-Dülger G. Melatonin and N-acetylcysteine have beneficial effects during hepatic ischemia and reperfusion. Life Sci. 2003;72:2707–2718. doi: 10.1016/s0024-3205(03)00187-5. [DOI] [PubMed] [Google Scholar]
- 35.Lepay DA, Nathan CF, Steinman RM, Murray HW, Cohn ZA. Murine Kupffer cells. Mononuclear phagocytes deficient in the generation of reactive oxygen intermediates. J Exp Med. 1985;161:1079–1096. doi: 10.1084/jem.161.5.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hasegawa T, Sakurai K, Kambayashi Y, Saniabadi AR, Nagamoto H, Tsukada K, Takahashi A, Kuwano H, Nakano M. Effects of OPC-6535 on lipopolysaccharide-induced acute liver injury in the rat: involvement of superoxide and tumor necrosis factor-alpha from hepatic macrophages. Surgery. 2003;134:818–826. doi: 10.1016/s0039-6060(03)00297-6. [DOI] [PubMed] [Google Scholar]
- 37.Mustafa SB, Gandhi CR, Harvey SA, Olson MS. Endothelin stimulates platelet-activating factor synthesis by cultured rat Kupffer cells. Hepatology. 1995;21:545–553. [PubMed] [Google Scholar]
- 38.Kiechle FL, Malinski T. Nitric oxide. Biochemistry, pathophysiology, and detection. Am J Clin Pathol. 1993;100:567–575. doi: 10.1093/ajcp/100.5.567. [DOI] [PubMed] [Google Scholar]
- 39.Gavino VC, Miller JS, Ikharebha SO, Milo GE, Cornwell DG. Effect of polyunsaturated fatty acids and antioxidants on lipid peroxidation in tissue cultures. J Lipid Res. 1981;22:763–769. [PubMed] [Google Scholar]
- 40.Mosmann T. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods. 1983;65:55–63. doi: 10.1016/0022-1759(83)90303-4. [DOI] [PubMed] [Google Scholar]
- 41.Wang GS, Liu GT. Influences of Kupffer cell stimulation and suppression on immunological liver injury in mice. Zhongguo Yaoli Xuebao. 1997;18:173–176. [PubMed] [Google Scholar]
- 42.Reiter RJ, Melchiorri D, Sewerynek E, Poeggeler B, Barlow-Walden L, Chuang J, Ortiz GG, Acuña-Castroviejo D. A review of the evidence supporting melatonin's role as an antioxidant. J Pineal Res. 1995;18:1–11. doi: 10.1111/j.1600-079x.1995.tb00133.x. [DOI] [PubMed] [Google Scholar]
- 43.Marchiafava PL, Longoni B. Melatonin as an antioxidant in retinal photoreceptors. J Pineal Res. 1999;26:184–189. doi: 10.1111/j.1600-079x.1999.tb00582.x. [DOI] [PubMed] [Google Scholar]
- 44.Kotler M, Rodríguez C, Sáinz RM, Antolín I, Menéndez-Peláez A. Melatonin increases gene expression for antioxidant enzymes in rat brain cortex. J Pineal Res. 1998;24:83–89. doi: 10.1111/j.1600-079x.1998.tb00371.x. [DOI] [PubMed] [Google Scholar]
- 45.Antolín I, Rodríguez C, Saínz RM, Mayo JC, Uría H, Kotler ML, Rodríguez-Colunga MJ, Tolivia D, Menéndez-Peláez A. Neurohormone melatonin prevents cell damage: effect on gene expression for antioxidant enzymes. FASEB J. 1996;10:882–890. doi: 10.1096/fasebj.10.8.8666165. [DOI] [PubMed] [Google Scholar]
- 46.Calvo JR, Reiter RJ, García JJ, Ortiz GG, Tan DX, Karbownik M. Characterization of the protective effects of melatonin and related indoles against alpha-naphthylisothiocyanate-induced liver injury in rats. J Cell Biochem. 2001;80:461–470. doi: 10.1002/1097-4644(20010315)80:4<461::aid-jcb1000>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 47.Harbrecht BG, Wu B, Watkins SC, Billiar TR, Peitzman AB. Inhibition of nitric oxide synthesis during severe shock but not after resuscitation increases hepatic injury and neutrophil accumulation in hemorrhaged rats. Shock. 1997;8:415–421. [PubMed] [Google Scholar]
- 48.Symington PA, Ma XL, Lefer AM. Protective actions of S-nitroso-N-acetylpenicillamine (SNAP) in a rat model of hemorrhagic shock. Methods Find Exp Clin Pharmacol. 1992;14:789–797. [PubMed] [Google Scholar]
- 49.Mojena M, Hortelano S, Castrillo A, Diaz-Guerra MJ, Garcia-Barchino MJ, Saez GT, Bosca L. Protection by nitric oxide against liver inflammatory injury in animals carrying a nitric oxide synthase-2 transgene. FASEB J. 2001;15:583–585. doi: 10.1096/fj.00-0509fje. [DOI] [PubMed] [Google Scholar]
- 50.Marshall HE, Merchant K, Stamler JS. Nitrosation and oxidation in the regulation of gene expression. FASEB J. 2000;14:1889–1900. doi: 10.1096/fj.00.011rev. [DOI] [PubMed] [Google Scholar]
- 51.Isobe M, Katsuramaki T, Hirata K, Kimura H, Nagayama M, Matsuno T. Beneficial effects of inducible nitric oxide synthase inhibitor on reperfusion injury in the pig liver. Transplantation. 1999;68:803–813. doi: 10.1097/00007890-199909270-00013. [DOI] [PubMed] [Google Scholar]
- 52.Wang Y, Lawson JA, Jaeschke H. Differential effect of 2-aminoethyl-isothiourea, an inhibitor of the inducible nitric oxide synthase, on microvascular blood flow and organ injury in models of hepatic ischemia-reperfusion and endotoxemia. Shock. 1998;10:20–25. doi: 10.1097/00024382-199807000-00004. [DOI] [PubMed] [Google Scholar]
- 53.Van Zee KJ, Kohno T, Fischer E, Rock CS, Moldawer LL, Lowry SF. Tumor necrosis factor soluble receptors circulate during experimental and clinical inflammation and can protect against excessive tumor necrosis factor alpha in vitro and in vivo. Proc Natl Acad Sci USA. 1992;89:4845–4849. doi: 10.1073/pnas.89.11.4845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shin S, Hur GH, Kim YB, Yeon GB, Park KJ, Park YM, Lee WS. Dehydroepiandrosterone and melatonin prevent Bacillus anthracis lethal toxin-induced TNF production in macrophages. Cell Biol Toxicol. 2000;16:165–174. doi: 10.1023/a:1007606921569. [DOI] [PubMed] [Google Scholar]
- 55.Sacco S, Aquilini L, Ghezzi P, Pinza M, Guglielmotti A. Mechanism of the inhibitory effect of melatonin on tumor necrosis factor production in vivo and in vitro. Eur J Pharmacol. 1998;343:249–255. doi: 10.1016/s0014-2999(97)01545-8. [DOI] [PubMed] [Google Scholar]
- 56.Williams JG, Bernstein S, Prager M. Effect of melatonin on activated macrophage TNF, IL-6, and reactive oxygen intermediates. Shock. 1998;9:406–411. doi: 10.1097/00024382-199806000-00003. [DOI] [PubMed] [Google Scholar]


