Abstract
We presented a 20-year-old patient with Crohn’s disease (CD). Colonoscopy revealed longitudinal ulceration in the terminal ileum and rectal aphtoid ulcers. After treatment with mesalamine and total parenteral nutrition, repeat colonoscopy revealed a granular elevated area in the terminal ileum, which appeared as an irregular dome-like elevation with irregularly arranged villi on magnifying endoscopy. Biopsy specimens taken from the region showed microgranulomas and lymphoid hyperplasia. Scanning electron microscopy revealed the presence of M cells, confirming that the area corresponded to Peyer’s patches. Peyer’s patches by magnifying endoscopy and electron microscopy may provide insights into the pathogenesis of CD.
INTRODUCTION
The gut-associated lymphoid tissue (GALT) is composed of Peyer’s patches, peripheral lymphoid tissues and appendix and plays an important role in the immune system of the gastrointestinal tract[1]. The importance of Peyer’s patches in the development of Crohn’s disease (CD) is generally accepted[1-8], but there have been only a few reports focusing on the endoscopic appearance of Peyer’s patches of the terminal ileum in CD[3-5].
We presented a patient with CD in whom specific CD lesions were found in the Peyer’s patches of the terminal ileum by magnifying endoscopy, histopathology and scanning electron microscopy. We also discussed the importance of endoscopic observation of the Peyer’s patches of the terminal ileum in the diagnosis and assessment of the pathogenesis of CD.
CASE REPORT
A 20-year-old man was admitted to our hospital with right lower abdominal pain, diarrhea and anal fistula for 4 wk. Physical examination revealed localized guarding with tenderness in the right lower quadrant of the abdomen as well as anal discharge. Laboratory analysis showed leukocytosis (10700/μL), elevated C-reactive protein (27 mg/L) and slight hypoproteinemia, while other biochemical and serological data were within normal limits. Repeated stool cultures yielded no enteric pathogens including Yersinia and tubercle bacilli. Colonoscopy showed longitudinal ulcers in the terminal ileum (Figure 1A), ileocecal valve, hepatic flexure, and anal canal. A subsequent radiological examination of the small bowel disclosed three discrete longitudinal ulcers with cobblestone appearance in the ileum. After treatment with a total of 2250 mg of mesalamine for 2 wk under total parenteral nutrition, repeat colonoscopy revealed improvement of the above lesions, leaving deformity of the ileocecal valve and anal stenosis. In addition to multiple aphthoid ulcers in the rectum, a granular elevated area was noted in the terminal ileum, which corresponded to the lymph follicle type of the Peyer’s patches according to a classification proposed by Fujikura (Figure 1B)[9]. On magnifying endoscopy, the surface of the Peyer’s patches appeared as an irregular dome-like elevation with irregularly arranged villi (Figure 1C). Histopathological examination of the biopsy specimens taken from the region and rectal aphthoid ulcers disclosed the presence of microgranulomas and lymphoid hyperplasia (Figure 2). Scanning electron microscopy of the specimen taken from the Peyer’s patch revealed the presence of M cells (Figure 3).
Figure 1.

Endoscopic findings. A: Endoscopic view showing an ulceration of the terminal ileum. B: Endoscopic view showing granularly elevated mucosa consistent with the lymphoid follicle type of the Payer’s patches. C: Magnifying endoscopy showing the irregular villi and the dome.
Figure 2.

Histological finding of a biopsy specimen obtained from the Peyer’s patches in the terminal ileum disclosing the presence of a microgranuloma and lymphoid hyperplasia.
Figure 3.
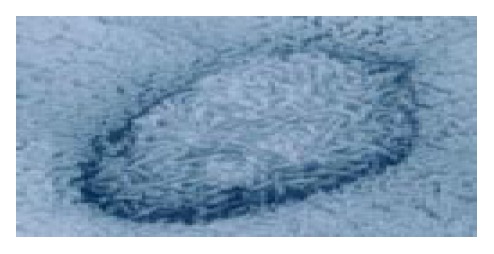
Scanning electron microscopy of the Peyer’s patches demonstrating M cells with microfolds.
DISCUSSION
Major advances have been made in every aspect of CD and ulcerative colitis (UC), but several problems in the etiology and pathogenesis of inflammatory bowel diseases (IBD) remain unresolved[1-8]. It has been recognized that the disorder of GALT plays a crucial role in the development of IBD[1-8]. Peyer’s patches and related lymphoid follicles have specialized follicle-associated epithelia (FAE) which serve as sites for the induction of mucosal immune responses[4,5]. In particular, it has been found that M cells serve as an important first step in this process[1,4,5], and Peyer’s patches are abundantly distributed in the terminal ileum[7,9], an area predisposed to CD. However, little attention has been paid to endoscopic observation of Peyer’s patches, and therefore, only a few studies[3-5] have described endoscopic appearance of Peyer’s patches in the terminal ileum. In this regard, Fujikura[9] examined the terminal ileum by colonoscopy in 110 normal cases and grossly in 48 autopsy cases, and classified Peyer’s patches into three categories as follows; lymph follicle, lymph border and lymphocyte aggregation types[9]. Macroscopically, the lymph follicle type appeared as granular or convolute elevation and was associated with lymphoid hyperplasia. The lymphocyte aggregation type appeared as a flat area associated with mild lymphocytic infiltration and few lymphoid follicles[9]. Recently, Van Kruiningen et al[7] examined 55 adults without intestinal disease and reported that Peyer's patches were concentrated in the distal 25 cm of ileum but extended proximally to 200 cm from the ileac end.
In the present case, magnifying endoscopy identified the irregular surface of Peyer’s patches, which harbored microgranulomas and lymphoid hyperplasia when examined histopathologically. Scanning electron microscopy identified the presence of M cells, confirming that the specimens were taken from the Peyer’s patches.
Our findings pose an important question: does the CD lesion selectively originate from the Peyer’s patch? In this regard, Lockhart-Mummery and Morson[2] reported in 1960 that the earliest microscopic change in CD was ulceration of the lymphoid follicles and Peyer’s patches in the terminal ileum. Since then, several investigators have reported that CD initially occurs as tiny aphthoid lesions at the sites of mucosal lymphoid follicles in the gastrointestinal tract[3-5]. Recently, Fujishima et al[3-5] investigated ultrastructurally the epithelium covering solitary lymphoid nodules using biopsy samples obtained from the colorectum during colonoscopy, and indicated that the red halo appearance of such epithelia seemed to precede visible aphthoid ulcers. They suggested that ulcerations in CD might originate from the follicle-associated epithelium (FAE), possibly related to its role as a portal entry for potentially pathogenic agents. These studies have led to the concept that CD could originate from GALT including Peyer’s patches and lymphoid follicles in the terminal ileum[3-8]. With this concept[3-7], one can explain the reason for the occurrence of the skip lesions and the frequent involvement of the terminal ileum in CD.
Fujikura[9] showed that M cells of the Peyer’s patches were more frequently seen in the dome area of the lymph follicle and lymph border types than in that of the lymphocyte aggregation type, emphasizing its pathogenetic functions. Further studies of the ultrastructure of M cells should enhance our understanding of their role in the development of IBD. However, it is difficult to obtain M cells by conventional endoscopic biopsy because they are located in the dome area (FAE), but not in the villi of Peyer’s patches[9]. Our experience indicates that biopsy using magnifying endoscopy is beneficial for accurate biopsy sampling to obtain tissue segments containing M cells, because this tool allows us to clearly recognize the dome area.
In conclusion, we identified CD-specific lesions in the Peyer’s patch of the terminal ileum by endoscopy and histopathological examination. Although the pathogenic role of M cells in the development of IBD is still unknown, examination of the Peyer’s patches by magnifying endoscopy and electron microscopy may provide insights into the pathogenesis of CD.
Footnotes
Edited by Wang XL Proofread by Xu FM
References
- 1.Elson CO. The Immunology of inflammatory bowel disease. In: Kirsner JB, editor. 5th ed. Inflammatory bowel disease. Philadelphia: Saunders. 2000:208–239. [Google Scholar]
- 2.LOCKHART-MUMMERY HE, MORSON BC. Crohn's disease (regional enteritis) of the large intestine and its distinction from ulcerative colitis. Gut. 1960;1:87–105. doi: 10.1136/gut.1.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hizawa K, Iida M, Aoyagi K, Fujishima M. The significance of colonic mucosal lymphoid hyperplasia and aphthoid ulcers in Crohn's disease. Clin Radiol. 1996;51:706–708. doi: 10.1016/s0009-9260(96)80243-1. [DOI] [PubMed] [Google Scholar]
- 4.Fujimura Y, Kamoi R, Iida M. Pathogenesis of aphthoid ulcers in Crohn's disease: correlative findings by magnifying colonoscopy, electron microscopy, and immunohistochemistry. Gut. 1996;38:724–732. doi: 10.1136/gut.38.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fujimura Y, Owen R. The intestinal Epithelial M cell: Properties and function. In: Kirsner JB, ed. Inflammatory bowel disease. 5th ed. Inflammatory bowel disease. Philadelphia: Saunders. 2000:33–44. [Google Scholar]
- 6.Van Kruiningen HJ, Ganley LM, Freda BJ. The role of Peyer's patches in the age-related incidence of Crohn's disease. J Clin Gastroenterol. 1997;25:470–475. doi: 10.1097/00004836-199709000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Van Kruiningen HJ, West AB, Freda BJ, Holmes KA. Distribution of Peyer's patches in the distal ileum. Inflamm Bowel Dis. 2002;8:180–185. doi: 10.1097/00054725-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Chiba M, Komatsu M, Iizuka M, Masamune O, Hoshina S, Kono M. Microbiology of the intestinal lymph follicle: a clue to elucidate causative microbial agent(s) in Crohn's disease. Med Hypotheses. 1998;51:421–427. doi: 10.1016/s0306-9877(98)90039-1. [DOI] [PubMed] [Google Scholar]
- 9.Fujikura S. A study of Peyer's patch of the terminal ileum (part 1): A study of the mucosal surface appearance and histological finding in endoscopic cases and autopsy cases (in Japanese) Gastroenterol Endosc. 1984;26:1246–1261. [Google Scholar]


