Abstract
AIM: To assess the expression of cyclooxygenase-2 (COX-2), nitric oxide synthase (iNOS), p53 and Ki-67 in gastric mucosa-associated lymphoid tissue (MALT) lymphoma and clarify the relationship between COX-2 expression and iNOS or p53 expression in these patients.
METHODS: The expressions of COX-2, iNOS, p53 and Ki-67 were detected in 32 gastric MALT lymphoma specimens and 10 adjacent mucosal specimens by immunohistochemical Envision method.
RESULTS: COX-2 and iNOS expressions were significantly higher in gastric MALT lymphoma tissues than those in adjacent normal tissues. The expression of COX-2 was observed in 22 of 32 cases of MALT lymphoma tissues (68.8%). A positive cytoplasmic immunoreactivity for iNOS was detected in 17 of 31 cases (53.1%). COX-2 expression in gastric MALT lymphoma tissues was positively correlated with iNOS expression (r = 0.448, P = 0.010) and cell proliferative activity analyzed by Ki-67 labeling index (r = 0.410, P = 0.020). The expression of COX-2 protein did not correlate with age, sex, stage of disease, lymph node metastasis or differentiation. The accumulation of p53 nuclear phosphoprotein was detected in 19 (59.4%) of tumors. p53 protein was expressed in 11 of 23 assessed LG tumors and in 8 of 9 assessed HG tumors. The difference of p53 positivity was found statistically significant between LG and HG cases (P = 0.0302). The p53 accumulation correlated with advanced clinical stage (stage III + IV vs stage I + II, P = 0.017). There was a significant positive correlation between COX-2 expression and p53 accumulation status (r = 0.403, P = 0.022). The mean PI of Ki-67 in each grade group were 36.0% ± 7.73% in HG and 27.4% ± 9.21% in LG. High-proliferation rate correlated with HG tumors (r = 0.419, P = 0.017). The correlation coefficient showed a significant positive correlation between PI and COX-2 expression in MALT lymphoma patients (r = 0.410, P = 0.020).
CONCLUSION: COX-2 expresses in the majority of gastric MALT lymphoma tissues and correlates with cellular proliferation and iNOS expression. COX-2 overexpression is closely associated with p53 accumulation status. iNOS and COX-2 may play a synergistic role in the pathogenesis of gastric MALT lymphoma.
INTRODUCTION
Lymphomas of mucosa-associated lymphoid tissue (MALT) are a distinct subgroup of extranodal B-cell non-Hodgkin’s lymphomas. Gastric MALT lymphomas are the majority of the cases and account for 1%-10% of all gastric malignant neoplasms[1]. Epidemiological and clinical studies demonstrated a link between gastric MALT lymphoma and chronic infection with Helicobacter pylori (H pylori)[2,3]. Cyclooxygenase-2 (COX-2) and nitric oxide synthase (iNOS) are important enzymes that mediate inflammatory processes. In recent years, it has been demonstrated that both COX-2 and iNOS play important roles in various tumors, including gastric MALT lymphoma[4,5]. COX-2, a key isoenzyme in conversion of arachidonic acid to prostaglandins, is inducible by various agents such as growth factors and tumor promoters, and is frequently overexpressed in various tumors[6,7]. iNOS are isoenzymes that catalyze the synthesis of nitric oxide (NO). Overexpression of iNOS has been demonstrated in various human neoplasms, such as breast cancer[8], colorectal cancer[9], and gastric cancer[10]. The p53 tumor suppressor protein is a critical mediator of apoptosis and tumorigenesis. Although studies have suggested interactions between COX-2 and iNOS or p53 in different tumors, the relationship between COX-2 expression and a variety of other molecular markers of tumor progression has not been reported for gastric MALT lymphomas. In the present study, we conducted to determine the expressions of COX-2, iNOS and p53 expression as well as cell proliferative index (Ki-67) in 32 gastric MALT lymphomas by using immunohistochemistry.
MATERIALS AND METHODS
Specimens
Thirty-two gastric MALT lymphoma specimens and 10 adjacent specimens were obtained from surgical resection. The patients underwent surgery at Xijing Hospital of the Fourth Military Medical University (Xi’an, China) between January 1996 and September 2002. The tumor specimens were retrieved from the archives of the Department of Pathology, Xijing Hospital. The mean age of the gastric MALT lymphoma group was 52.8 years (range 29-70 years), and there were 22 males and 10 females. All cases were of B-cell origin as immunohistochemistry showed CD20 expression in all MALT cases. The cases were categorized in two basic groups, according to (REAL) Classification[11] and the WHO Classification[12] for MALT lymphomas: low-grade lymphoma of MALT (composed of centrocyte-like cells, lymphoid follicles and plasma cell differentiation) and high-grade lymphoma of MALT (diffuse large B cell lymphoma (DLBCL) with or without low grade MALT + lymphoma component). Of the 32 patients, 23 were low grade MALT lymphoma (LG) and 9 high grade MALT lymphoma (HG). Patients were staged according to the Ann Arbor system. All specimens were fixed in 40 g/L buffered formaldehyde, and embedded in paraffin wax.
Immunohistochemical assay for expression of COX-2, iNOS, p53 and Ki-67
The expression of COX-2, iNOS, p53 and Ki-67 was studied by immunohistochemical Envision method according to the manufacturer’s instructions. H-62 (COX-2) is a rabbit polyclonal antibody raised against a recombinant protein corresponding to amino acids 50-111 mapping near the amino terminus of COX-2 of human origin (sc-7951, Santa Cruz Biotechnology, dilution 1:50). M-19 (iNOS) was provided as a rabbit affinity-purified polyclonal antibody raised against a peptide mapping at the carboxyl terminus of iNOS of mouse origin (sc-650, Santa Cruz Biotechnology, dilution 1:50). The Ki-67 antibody recognizes the Ki-67 antigen of paraffin-embedded tissues. To detect the p53 protein, a mouse monoclonal antibody (sc-126, Santa Cruz Biotechnology, dilution 1:50) was used which recognizes an epitope in the N-terminus of the human p53 protein. Staining for Ki-67 was performed by using an anti-Ki-67 monoclonal mouse antibody (ZM-0166, Zhongshan Biotechnology, dilution 1:50). Briefly, 5-µm sections cut from formalin-fixed, paraffin-embedded specimens were deparaffinized in xylene and rehydrated in graded alcohol. For antigen retrieval, the deparaffinized slides were microwaved in 0.01 mol/L sodium citrate buffer (pH6.0) for 10 min. Endogenous peroxidase activity was then blocked by incubating the sections with 30 mL/L H2O2 in 0.05 mol/L phosphate buffer (pH7.4), containing 0.45 mol/L NaCl for 15 min. Non-specific antibody binding was blocked by pretreatment with PBS containing 5 g/L bovine serum albumin. The sections were then incubated with the primary antibodies diluted as described above. After incubation, these sections were washed with 0.02 mol/L sodium phosphate buffer. The slides were then incubated with a secondary antibody for 30 min. Diaminobenzidine was used as chromogen and the sections were counterstained with hematoxylin. Negative controls were established by replacing the primary antibody with PBS.
Assessment of immunohistochemical results
The slides were evaluated independently by two observers who were unknown to the histological status. At the cellular level, COX-2 and iNOS staining was cytoplasmic in most cases, however, p53 and Ki-67 staining was nuclear. COX-2 is cytoplasmic enzyme detectable in tumor cells, epithelial cells, endothelial cells, smooth muscle cells and inflammatory cells. For final analysis, the expression of COX-2 was scored in the tumor cells. Staining for COX-2 and iNOS was considered positive only when more than 10% of the tumor cells in the entire tumor area were judged to be positive. The level of p53 was calculated by expressing the number of p53-positive cancer cells as a percentage of the total number of cancer cells in a high-power field. For analysis, tumors were classified as p53-negative (less than 10% positive nuclei) or p53-positive (more than 10% positive nuclei). The Ki-67 labeling index (proliferation index, PI) was determined by counting the percentage of positive cells among 1000 tumor cells in 10 random regions in 400-fold fields.
Statistical analysis
Statistical comparisons for significance were made with the Student’s t test and Chi-square test. Spearman correlation test was used for the correlation between positive rates. A P value < 0.05 was considered statistically significant.
RESULTS
Expression of COX-2 and iNOS in gastric MALT lymphoma
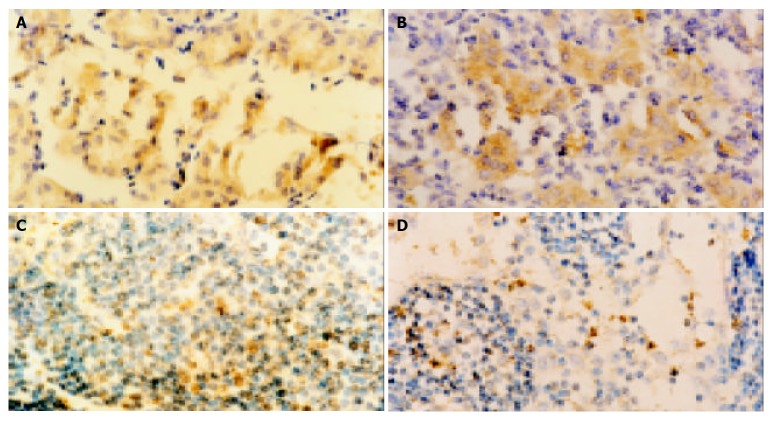
The expression of COX-2 was observed in 22 of 32 cases of MALT lymphoma tissues (68.8%). Immunohistochemically, COX-2 was stained diffusely in cytoplasm of the tumor cells (Figure 1A). In contrast, no or very faint signal was found in neighboring normal tissues. A positive cytoplasmic immunoreactivity for iNOS was detected in 17 of 31 cases (53.1%, Figure 1B). However, no staining could be observed in neighboring normal tissues.
Figure 1.
Results of immunohistochemical staining (Original magnification: × 400). A: Expression of COX-2 in gastric MALT lymphoma; B: Expression of iNOS in gastric MALT lymphoma; C: Expression of p53 in gastric MALT lymphoma; D: Expression of Ki-67 in gastric MALT lymphoma.
There was a significant correlation between COX-2 and iNOS expression (r = 0.448, P = 0.010). The positive expression rate of iNOS (88.2%) in the COX-2 positive group was significantly higher than that in the COX-2-negative group (46.7%, P = 0.011).
Correlation between COX-2 expression and clinicopathological factors
The correlation between COX-2 expression and the clinicopathologic findings was analyzed by Spearman correlation test. All the parameters analyzed in COX-2 positive cases, including age, gender, stage of disease, lymph node metastasis and differentiation degree of the tumor, did not reached statistical significance (P > 0.05, Table 1).
Table 1.
Correlation between expression of COX-2 and iNOS/p53 and clinicopathological factors in gastric MALT lym-phoma (n, %)
| Variable | Total | COX-2 | COX-2 | P value | |
| positive | negative | ||||
| Gender | Male | 22 | 15 (68.2) | 7 (31.8) | 0.918 |
| Female | 10 | 7 (70.0) | 3 (30.0) | ||
| Age (yr) | ≤ 5 0 | 9 | 6 (66.7) | 3 (33.3) | 0.874 |
| > 50 | 23 | 16 (69.6) | 7 (30.4) | ||
| Lymph node | + | 10 | 8 (80.0) | 2 (20.0) | 0.355 |
| Metastasis | - | 22 | 14 (63.6) | 8 (36.4) | |
| Histological | Low | 23 | 14 (60.7) | 9 (39.1) | 0.124 |
| Grade | High | 9 | 8 (88.9) | 1 (11.1) | |
| Histological | I + II | 22 | 16 (72.7) | 6 (27.3) | 0.472 |
| Stage | III + IV | 10 | 6 (60.0) | 4 (40.0) | |
| INOS | + | 17 | 15 (88.2) | 2 (11.8) | 0.011 |
| - | 15 | 7 (46.7) | 8 (53.3) | ||
| p53 | + | 19 | 16 (84.2) | 3 (15.8) | 0.022 |
| - | 13 | 6 (46.2) | 7 (53.8) | ||
Expression of p53 in gastric MALT lymphoma
The accumulation of p53 nuclear phosphoprotein was detected in 19 (59.4%) of tumors (Table 1, Figure 1C), whereas the p53 accumulation was undetectable in normal gastric tissues. A relationship between p53 status and several clinicopathological characteristics was investigated. p53 protein was expressed in 11 of 23 assessed LG tumors and in 8 of 9 assessed HG tumors. The difference of p53 positivity was found statistically significant between LG and HG cases (P = 0.033). The p53 accumulation correlated with advanced clinical stage (stage III + IV vs stage I + II, P = 0.017). The other parameters, such as age, gender and lymph node metastasis did not show any significant relation to the expression of p53.
There was a significant positive correlation between COX-2 expression and p53 accumulation status (r = 0.403, P = 0.022). Tumors that overexpressed p53 had higher expression levels of COX-2 than those without p53 overexpression (P = 0.022, Table 1).
Expression of Ki-67 in gastric MALT lymphoma
Ki-67 staining was nuclear (Figure 1D). Very few cells were positive for Ki-67 in non-neoplastic gastric tissues. The mean PI of Ki-67 in the tumors was 29.81% ± 9.54% (mean ± SD). Mean values in each grade group were 36.0% ± 7.73% in HG and 27.4% ± 9.21% in LG. A significant correlation was observed between the high-proliferation rate and HG tumors (r = 0.419, P = 0.017).
The PI in COX-2 positive group was significantly higher than that in COX-2 negative group (P = 0.031). The correlation coefficient showed a significant positive correlation between PI and COX-2 expression in MALT lymphoma patients (r = 0.410, P = 0.020). However, no significant correlation between PI and iNOS expression was found (r = -0.037, P = 0.839).
DISCUSSION
Gastric MALT lymphoma is a unique disease. Normal human gastric mucosa is devoid of MALT. MALT accumulates within gastric mucosa as a result of long-standing H pylori infection in a subset of infected patients, and from this acquired MALT, low-grade B cell MALT lymphoma may eventually develop[13]. H pylori can be demonstrated in the gastric mucosa of the majority of cases of gastric MALT lymphoma[14,15]. Additionally, eradication of H pylori was reported to result in the complete regression of the majority of these tumors[16,17]. However, the exact mechanism responsible for the development of MALT lymphoma still remains obscure.
The contribution of COX-2 to carcinogenesis and the malignant phenotype of tumor cells have been thought to be related to its abilities: (1) increase production of prostaglandins[18]; (2) convert procarcinogens to carcinogens[19]; (3) inhibit apoptosis[20]; (4) promote angiogenesis[21]; (5) modulate inflammation and immune function[22,23]; (6) increase tumor cell invasiveness[24,25]. Like COX-2, iNOS is also involved in the process of carcinogenesis. Sustained induction of iNOS in chronic inflammation may be mutagenic through NO-mediated DNA damage or hindrance to DNA repair, and thus potentially carcinogenic. In addition, NO can favour tumor growth and development by stimulating angiogenesis[10,26-28] and causing immunosuppression[29].
In the current study, we demonstrated that a high positive immunostaining rate for COX-2 and iNOS was observed in gastric MALT lymphoma. Our results agree with the findings of previous investigations[4,5,14,17]. The present results indicated that the increased expression of COX-2 and iNOS might be important molecular events that contribute to gastric MALT lymphoma carcinogenesis. We speculate that H pylori infection might induce gastric carcinogenesis via overexpression of COX-2. These processes may be completed by the expression of COX-2 as an inflammation enzyme to release excessive amounts of prostaglandins, leading to further proliferation, reduction in apoptosis, angiogenesis and tumor growth.
It has been reported that COX-2 overexpression in tumors significantly correlates with iNOS overexpression[4,5]. In the current study, we also discovered that COX-2 expression was positively correlated with iNOS expression, suggesting a link between the COX-2 and iNOS pathways. In addition, iNOS and COX-2 may play a synergistic role in the pathogenesis of gastric MALT lymphoma. Because the product of iNOS catalysis, NO, is an important regulator of COX-2 activity and expression[30,31], and the products of COX-2 (diverse prostaglandins) may also influence iNOS expression[32]. Furthermore, prostaglandins and NO have been proposed to be involved in angiogenesis in vivo[33]. The inhibition of NO production by COX-2 inhibitors suggests NO-COX cross-talk between COX-2 and iNOS pathways[34].
Our results demonstrated that COX-2 expression in MALT lymphoma tissues was positively correlated with cell proliferative activity analyzed by Ki-67 labeling index. Ki-67 is expressed in cells that undergo active proliferation and have left the G0 phase of the cell cycle[35]. These results suggest that COX-2 expression may be actively associated with the modulation of cellular proliferation and transformation during the evolution of H pylori-associated gastritis to MALT lymphoma.
So far, there have been some ambiguous points with regard to relationships between COX-2 overexpression and clinicopathological characteristics of tumors. Several reports have demonstrated that COX-2 expression in various tumors influences tumor cell differentiation, invasiveness, size, and survival[36]. However, we found no significant relation between COX-2 expression and clinicopathological characteristics in our study, which was compatible with previous reports on other organs[37].
Low-grade MALT lymphoma can transform into high-grade lymphoma and is associated with other genetic events such as p53 inactivation[38,39]. In the current study, p53 positivity increased significantly as the histological grade advanced. The results of our study support the concept that the expression of p53 in gastric lymphomas may be associated with transformation from low-grade to high-grade disease. In addition, there have been many workers reporting that high-proliferation rate is associated with the presence of a large cell component of MALT lymphoma[40,41]. The results of our experiments showed that high proliferation rate expressed by Ki-67 was correlated with HG tumors. These suggested that high proliferation index in MALT lymphoma may help in identifying a population of patients with an increased risk of developing MALT lymphoma.
Consistent with the findings of others[40], we found that COX-2 overexpression was closely associated with p53 accumulation status. With regard to the negative regulation of COX-2, it has recently been shown that wild-type p53 suppresses promoter activities of COX-2 and the expression of COX-2 protein. Wild-type p53 was shown to suppress COX-2 promoter activity by competing with TATA-binding proteins[41]. Han et al[42] identified that COX-2 expression was inducible by wild-type p53 and DNA damage. They also found that p53-induced COX-2 expression resulted from p53-mediated activation of the Ras/Raf/MAPK cascade, as demonstrated by suppression of COX-2 induction in response to p53 by dominant-negative Ras or Raf1 mutants. Furthermore, heparin-binding epidermal growth factor-like growth factor (HB-EGF), a p53 downstream target gene, induced COX-2 expression, implying that COX-2 is an ultimate effector in the p53→HB-EGF→Ras/Raf/MAPK→COX-2 pathway.
In conclusion, COX-2 is expressed in the majority of gastric MALT lymphoma tissues and correlates with cellular proliferation and iNOS expression. iNOS and COX-2 may play a synergistic role in the pathogenesis of gastric MALT lymphoma. COX-2 overexpression is closely associated with p53 accumulation status. The molecular basis for the expression of COX-2 and iNOS and their roles in the evolution of H pylori-associated gastritis to gastric MALT lymphoma requires to be carefully investigated in follow-up studies.
Footnotes
Edited by Kumar M Proofread by Chen WW and Xu FM
References
- 1.Nakamura S, Akazawa K, Yao T, Tsuneyoshi M. A clinicopathologic study of 233 cases with special reference to evaluation with the MIB-1 index. Cancer. 1995;76:1313–1324. doi: 10.1002/1097-0142(19951015)76:8<1313::aid-cncr2820760804>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 2.Konturek PC, Konturek SJ, Starzyska T, Marlicz K, Bielanski W, Pierzchalski P, Karczewska E, Hartwich A, Rembiasz K, Lawniczak M, et al. Helicobacter pylori-gastrin link in MALT lymphoma. Aliment Pharmacol Ther. 2000;14:1311–1318. doi: 10.1046/j.1365-2036.2000.00832.x. [DOI] [PubMed] [Google Scholar]
- 3.Fu S, Ramanujam KS, Wong A, Fantry GT, Drachenberg CB, James SP, Meltzer SJ, Wilson KT. Increased expression and cellular localization of inducible nitric oxide synthase and cyclooxygenase 2 in Helicobacter pylori gastritis. Gastroenterology. 1999;116:1319–1329. doi: 10.1016/s0016-5085(99)70496-8. [DOI] [PubMed] [Google Scholar]
- 4.Kong G, Kim EK, Kim WS, Lee KT, Lee YW, Lee JK, Paik SW, Rhee JC. Role of cyclooxygenase-2 and inducible nitric oxide synthase in pancreatic cancer. J Gastroenterol Hepatol. 2002;17:914–921. doi: 10.1046/j.1440-1746.2002.02829.x. [DOI] [PubMed] [Google Scholar]
- 5.Nose F, Ichikawa T, Fujiwara M, Okayasu I. Up-regulation of cyclooxygenase-2 expression in lymphocytic thyroiditis and thyroid tumors: significant correlation with inducible nitric oxide synthase. Am J Clin Pathol. 2002;117:546–551. doi: 10.1309/9CCJ-XQ8P-PMFM-M65K. [DOI] [PubMed] [Google Scholar]
- 6.Denkert C, Winzer KJ, Müller BM, Weichert W, Pest S, Köbel M, Kristiansen G, Reles A, Siegert A, Guski H, et al. Elevated expression of cyclooxygenase-2 is a negative prognostic factor for disease free survival and overall survival in patients with breast carcinoma. Cancer. 2003;97:2978–2987. doi: 10.1002/cncr.11437. [DOI] [PubMed] [Google Scholar]
- 7.Liu JW, Li KZ, Dou KF. Expression of cyclooxygenase-2 in pancreatic cancer and its correlation with p53. Shijie Huaren Xiaohua Zazhi. 2003;11:229–232. [Google Scholar]
- 8.Bing RJ, Miyataka M, Rich KA, Hanson N, Wang X, Slosser HD, Shi SR. Nitric oxide, prostanoids, cyclooxygenase, and angiogenesis in colon and breast cancer. Clin Cancer Res. 2001;7:3385–3392. [PubMed] [Google Scholar]
- 9.Xu MH, Deng CS, Zhu YQ, Lin J. Role of inducible nitric oxide synthase expression in aberrant crypt foci-adenoma-carcinoma sequence. World J Gastroenterol. 2003;9:1246–1250. doi: 10.3748/wjg.v9.i6.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song ZJ, Gong P, Wu YE. Relationship between the expression of iNOS,VEGF,tumor angiogenesis and gastric cancer. World J Gastroenterol. 2002;8:591–595. doi: 10.3748/wjg.v8.i4.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, Delsol G, De Wolf-Peeters C, Falini B, Gatter KC. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood. 1994;84:1361–1392. [PubMed] [Google Scholar]
- 12.Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J, Lister TA, Bloomfield CD. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee meeting-Airlie House, Virginia, November 1997. J Clin Oncol. 1999;17:3835–3849. doi: 10.1200/JCO.1999.17.12.3835. [DOI] [PubMed] [Google Scholar]
- 13.Du MQ, Isaacson PG. Recent advances in our understanding of the biology and pathogenesis of gastric mucosa-associated lymphoid tissue (malt) lymphoma. Forum (Genova) 1998;8:162–173. [PubMed] [Google Scholar]
- 14.Konturek PC, Konturek SJ, Pierzchalski P, Bielański W, Duda A, Marlicz K, Starzyńska T, Hahn EG. Cancerogenesis in Helicobacter pylori infected stomach--role of growth factors, apoptosis and cyclooxygenases. Med Sci Monit. 2001;7:1092–1107. [PubMed] [Google Scholar]
- 15.Konturek SJ, Konturek PC, Hartwich A, Hahn EG. Helicobacter pylori infection and gastrin and cyclooxygenase expression in gastric and colorectal malignancies. Regul Pept. 2000;93:13–19. doi: 10.1016/s0167-0115(00)00173-7. [DOI] [PubMed] [Google Scholar]
- 16.Ohashi S, Segawa K, Okamura S, Urano H, Kanamori S, Ishikawa H, Hara K, Hukutomi A, Shirai K, Maeda M. A clinicopathologic study of gastric mucosa-associated lymphoid tissue lymphoma. Cancer. 2000;88:2210–2219. doi: 10.1002/(sici)1097-0142(20000515)88:10<2210::aid-cncr3>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 17.Konturek PC, Konturek SJ, Pierzchalski P, Starzyńska T, Marlicz K, Hartwich A, Zuchowicz M, Darasz Z, Papiez D, Hahn EG. Gastric MALT-lymphoma, gastrin and cyclooxygenases. Acta Gastroenterol Belg. 2002;65:17–23. [PubMed] [Google Scholar]
- 18.Zweifel BS, Davis TW, Ornberg RL, Masferrer JL. Direct evidence for a role of cyclooxygenase 2-derived prostaglandin E2 in human head and neck xenograft tumors. Cancer Res. 2002;62:6706–6711. [PubMed] [Google Scholar]
- 19.Hosomi Y, Yokose T, Hirose Y, Nakajima R, Nagai K, Nishiwaki Y, Ochiai A. Increased cyclooxygenase 2 (COX-2) expression occurs frequently in precursor lesions of human adenocarcinoma of the lung. Lung Cancer. 2000;30:73–81. doi: 10.1016/s0169-5002(00)00132-x. [DOI] [PubMed] [Google Scholar]
- 20.Miyata Y, Koga S, Kanda S, Nishikido M, Hayashi T, Kanetake H. Expression of cyclooxygenase-2 in renal cell carcinoma: correlation with tumor cell proliferation, apoptosis, angiogenesis, expression of matrix metalloproteinase-2, and survival. Clin Cancer Res. 2003;9:1741–1749. [PubMed] [Google Scholar]
- 21.Kim MH, Seo SS, Song YS, Kang DH, Park IA, Kang SB, Lee HP. Expression of cyclooxygenase-1 and -2 associated with expression of VEGF in primary cervical cancer and at metastatic lymph nodes. Gynecol Oncol. 2003;90:83–90. doi: 10.1016/s0090-8258(03)00224-5. [DOI] [PubMed] [Google Scholar]
- 22.Ermert L, Dierkes C, Ermert M. Immunohistochemical expression of cyclooxygenase isoenzymes and downstream enzymes in human lung tumors. Clin Cancer Res. 2003;9:1604–1610. [PubMed] [Google Scholar]
- 23.Sharma S, Stolina M, Yang SC, Baratelli F, Lin JF, Atianzar K, Luo J, Zhu L, Lin Y, Huang M, et al. Tumor cyclooxygenase 2-dependent suppression of dendritic cell function. Clin Cancer Res. 2003;9:961–968. [PubMed] [Google Scholar]
- 24.Zhang H, Sun XF. Overexpression of cyclooxygenase-2 correlates with advanced stages of colorectal cancer. Am J Gastroenterol. 2002;97:1037–1041. doi: 10.1111/j.1572-0241.2002.05625.x. [DOI] [PubMed] [Google Scholar]
- 25.Wu QM, Li SB, Wang Q, Wang DH, Li XB, Liu CZ. The expres-sion of COX-2 in esophageal carcinoma and its relation to clini-copathologic characteristics. Shijie Huaren Xiaohua Zazhi. 2001;9:11–14. [Google Scholar]
- 26.Cianchi F, Cortesini C, Fantappie O, Messerini L, Schiavone N, Vannacci A, Nistri S, Sardi I, Baroni G, Marzocca C, et al. Inducible nitric oxide synthase expression in human colorectal cancer: correlation with tumor angiogenesis. Am J Pathol. 2003;162:793–801. doi: 10.1016/S0002-9440(10)63876-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tao WH, Deng CS, Zhu YQ. Expression of inducible nitric oxide synthase and angiogenesis in gastric cancer. Shijie Huaren Xiaohua Zazhi. 2003;11:33–35. [Google Scholar]
- 28.Franchi A, Gallo O, Paglierani M, Sardi I, Magnelli L, Masini E, Santucci M. Inducible nitric oxide synthase expression in laryngeal neoplasia: correlation with angiogenesis. Head Neck. 2002;24:16–23. doi: 10.1002/hed.10045. [DOI] [PubMed] [Google Scholar]
- 29.Kojima M, Morisaki T, Tsukahara Y, Uchiyama A, Matsunari Y, Mibu R, Tanaka M. Nitric oxide synthase expression and nitric oxide production in human colon carcinoma tissue. J Surg Oncol. 1999;70:222–229. doi: 10.1002/(sici)1096-9098(199904)70:4<222::aid-jso5>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 30.Liu Q, Chan ST, Mahendran R. Nitric oxide induces cyclooxygenase expression and inhibits cell growth in colon cancer cell lines. Carcinogenesis. 2003;24:637–642. doi: 10.1093/carcin/bgg014. [DOI] [PubMed] [Google Scholar]
- 31.Pérez-Sala D, Lamas S. Regulation of cyclooxygenase-2 expression by nitric oxide in cells. Antioxid Redox Signal. 2001;3:231–248. doi: 10.1089/152308601300185197. [DOI] [PubMed] [Google Scholar]
- 32.Kobayashi O, Miwa H, Watanabe S, Tsujii M, Dubois RN, Sato N. Cyclooxygenase-2 downregulates inducible nitric oxide synthase in rat intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2001;281:G688–G696. doi: 10.1152/ajpgi.2001.281.3.G688. [DOI] [PubMed] [Google Scholar]
- 33.Davel L, D'Agostino A, Español A, Jasnis MA, Lauría de Cidre L, de Lustig ES, Sales ME. Nitric oxide synthase-cyclooxygenase interactions are involved in tumor cell angiogenesis and migration. J Biol Regul Homeost Agents. 2002;16:181–189. [PubMed] [Google Scholar]
- 34.Fantappiè O, Masini E, Sardi I, Raimondi L, Bani D, Solazzo M, Vannacci A, Mazzanti R. The MDR phenotype is associated with the expression of COX-2 and iNOS in a human hepatocellular carcinoma cell line. Hepatology. 2002;35:843–852. doi: 10.1053/jhep.2002.32469. [DOI] [PubMed] [Google Scholar]
- 35.Scholzen T, Gerdes J. The Ki-67 protein: from the known and the unknown. J Cell Physiol. 2000;182:311–322. doi: 10.1002/(SICI)1097-4652(200003)182:3<311::AID-JCP1>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 36.Rajnakova A, Moochhala S, Goh PM, Ngoi S. Expression of nitric oxide synthase, cyclooxygenase, and p53 in different stages of human gastric cancer. Cancer Lett. 2001;172:177–185. doi: 10.1016/s0304-3835(01)00645-0. [DOI] [PubMed] [Google Scholar]
- 37.Kokawa A, Kondo H, Gotoda T, Ono H, Saito D, Nakadaira S, Kosuge T, Yoshida S. Increased expression of cyclooxygenase-2 in human pancreatic neoplasms and potential for chemoprevention by cyclooxygenase inhibitors. Cancer. 2001;91:333–338. doi: 10.1002/1097-0142(20010115)91:2<333::aid-cncr1006>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 38.Insabato L, Di Vizio D, Tornillo L, D'Armiento FP, Siciliano A, Milo M, Palmieri G, Pettinato G, Terracciano LM. Clinicopathologic and immunohistochemical study of surgically treated primary gastric MALT lymphoma. J Surg Oncol. 2003;83:106–111. doi: 10.1002/jso.10241. [DOI] [PubMed] [Google Scholar]
- 39.Pozzi B, Hotz AM, Feltri M, Cornaggia M, Campiotti L, Bonato M, Pinotti G, Capella C. [Primary gastric lymphomas. Clinico-pathological study and evaluation of prognostic factors in 65 cases treated surgically] Pathologica. 2000;92:503–515. [PubMed] [Google Scholar]
- 40.Niki T, Kohno T, Iba S, Moriya Y, Takahashi Y, Saito M, Maeshima A, Yamada T, Matsuno Y, Fukayama M, et al. Frequent co-localization of Cox-2 and laminin-5 gamma2 chain at the invasive front of early-stage lung adenocarcinomas. Am J Pathol. 2002;160:1129–1141. doi: 10.1016/s0002-9440(10)64933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Subbaramaiah K, Altorki N, Chung WJ, Mestre JR, Sampat A, Dannenberg AJ. Inhibition of cyclooxygenase-2 gene expression by p53. J Biol Chem. 1999;274:10911–10915. doi: 10.1074/jbc.274.16.10911. [DOI] [PubMed] [Google Scholar]
- 42.Han JA, Kim JI, Ongusaha PP, Hwang DH, Ballou LR, Mahale A, Aaronson SA, Lee SW. P53-mediated induction of Cox-2 counteracts p53- or genotoxic stress-induced apoptosis. EMBO J. 2002;21:5635–5644. doi: 10.1093/emboj/cdf591. [DOI] [PMC free article] [PubMed] [Google Scholar]