Abstract
Background and Purpose:
In patients with acute stroke, undernutrition and aspiration pneumonia are associated with increased mortality and length of hospital stay. Formal screening for nutritional risk and dysphagia helps to ensure optimal nutritional management in all patients with stroke and to reduce the risk of aspiration in patients with dysphagia. We developed a national guideline for nutritional and dysphagia screening in acute stroke, which was introduced in our stroke unit on June 1, 2012. The primary objective was to audit adherence to the guideline and to achieve full implementation. Second, we assessed the prevalence of nutritional risk and dysphagia.
Methods:
We performed a chart review to assess performance of screening for nutritional risk and dysphagia in all patients with stroke hospitalized for ≥48 hours between June 1, 2012, and May 31, 2013. Next we applied a “clinical microsystems approach” with rapid improvement cycles and audits over a 6-month period to achieve full implementation.
Results:
The chart review showed that nutritional risk screening was performed in 65% and swallow testing in 91% of eligible patients (n = 185). Proactive implementation resulted in >95% patients screened (n = 79). The overall prevalence of nutritional risk was 29%, and 23% of the patients failed the initial swallow test.
Conclusions:
Proactive implementation is required to obtain high screening rates for nutritional risk and swallowing difficulties using validated screening tools. The proportion of patients at nutritional risk and the prevalence of dysphagia at initial swallow test were in the lower range of previous reports.
Keywords: acute stroke, nutrition, dysphagia, quality improvement
Introduction
Undernutrition and dysphagia put patients with stroke at risk of worse outcome. Studies in different patient populations indicate that up to half of the patients admitted to hospital with acute stroke may be undernourished and that probably as many initially present with dysphagia.1-7
Undernutrition develops as a consequence of insufficient protein and energy intake over time, leading to altered body composition and impaired biological function. In patients with acute stroke, undernutrition is an independent risk factor for poorer functional outcomes that is potentially modifiable.8-11 Most recently, attention has been drawn to metabolic changes that occur after a stroke, and it has been suggested that treating this imbalance may improve outcome.12
Nutritional intake can be substantially reduced in patients with dysphagia. Also, factors reducing ability to self-feed (eg, upper extremity paresis, apraxia, cognitive or visuospatial perceptual deficits, visual neglect, and agnosia) and depression may affect nutrition in people with stroke. Not unexpectedly, the proportion of patients with undernutrition has been shown to increase during the hospital stay.12,13
Dysphagia can cause undernutrition and carries a high risk of aspiration, which in turn predisposes for pulmonary infection. Pneumonia is the most common medical complication after stroke, with an estimated incidence ranging from 5% to 20% in large studies.14-16 Patients with dysphagia have a 3-fold increased risk of developing pneumonia5 and have worse outcome in terms of inpatient mortality and length of hospital stay.7,14,16 A swallow test before offering food, drink, or medication can identify patients with dysphagia. Studies have shown that a failed swallow test independently predicted pneumonia15 and that introducing a formal swallow test more than halved pneumonia rate.2,17-19
Thus, identifying patients at nutritional risk and patients with dysphagia as soon as possible after admission helps to ensure optimal nutritional management in all patients with stroke and to reduce the risk of aspiration in patients with dysphagia. Application of formal screening tests is likely to reduce complications, prolonged hospital stay, poor functional outcomes, and mortality.
We have developed an evidence-based national guideline integrating measures to detect and manage patients with acute stroke having nutritional risk or dysphagia.20 Here we report the results of the audits, our experience with implementation of the screening tests, the proportion of patients at risk of undernutrition, and the proportion of patients who failed the initial swallow test.
Methods
Guideline Development
A team consisting of clinical nutritionists (HN and IR), a speech and language therapist (MTB), stroke nurses, and physicians (MK and MTK) developed the Norwegian guideline for nutrition in acute stroke, following the Appraisal of Guidelines, Research and Evaluation (AGREE) framework (e-Supplement).
Ethical Issues
The patients were managed according to a mandatory guideline. Patient consent was not required. Data collection was approved by the hospital’s data protection officer (project number 0442).
Implementation Activities
Period I (June 1, 2012 to May 31, 2013)
One of the authors (HN) gave a lecture on nutrition for all neurologists in May 2012. Swallow testing at admission has since 2010 been an item on the checklist that is used in our stroke unit. In an educational session for nurses on June 1, 2012, instruction on how to perform a swallow test was repeated, and the electronic nutritional status screening tool was introduced. The item “nutritional risk screening,” (NRS) to be performed the day after admission within seven days, was added to the checklist. The head nurse focused on completeness of checklists during the first year of implementation of the guideline.
Period II (December 1, 2013 to May 31, 2014)
Starting on December 1, 2013, we applied a “clinical microsystems approach” for improvement in care.21 Instruction on how to screen for nutritional risk and dysphagia was repeated. A multidisciplinary team consisting of the nutrition nurse, the nurse educator, the head nurse, a nutritionist (IR), and a neurologist (MTK) met in fortnightly improvement meetings to discuss the data collected the past half month, identify barriers for improvement, and find ways to overcome them. Our aim was full implementation by May 31, 2014, defined as screening for swallowing problems and nutritional risk in 95% of eligible patients.
Audit
Patients
The Stroke Unit of the University Hospital of North Norway serves an unselected population of 124 000. The audit included patients who were admitted with a cerebral infarction or intracerebral hemorrhage on the day of the stroke or the day after and who stayed in the stroke unit for at least 48 hours after admission. Patients who according to notes received terminal care only or who died during the first 2 weeks after the stroke were excluded from analyses.
Outcomes and data collection
We assessed 2 primary outcomes: whether a swallow test had been performed on the day of admission or the day after (day 0/1) and whether patients were screened for nutritional risk during the first week of the hospital stay (days 0-7). Secondary outcomes consisted of the proportion of patients who were at nutritional risk or who had swallowing problems. For period I, information on whether screening tests were performed was obtained by retrospective review of electronic patient records of persons registered in the Department’s stroke register. During period II (December 1, 2013, to May 31, 2014), data on the same items were collected consecutively as patients were admitted to the stroke unit. Time from admission to screening was measured, and time limits were set to 6 hours for performing the swallow test and to 48 hours for NRS. Patients who were not able to perform the swallow test because of reduced consciousness and were given nil by mouth were considered “tested and failed.” Qualitative data on the process of implementation were extracted from the team meeting minutes.
Statistical analysis
We used IBM SPSS Statistics version 21 for descriptive analyses, Microsoft Office Excel 2007 for graphs, and EpiData Software for statistical process control (EpiData Association, www.epidata.dk).
Results
Guideline Development
Recommendations in the Norwegian guideline
The evidence base for the recommendation that patients with acute stroke should be screened for undernutrition and nutritional risk and that a swallow test should be performed before offering food or drink to the patients (SIGN grade B22) is documented in the e-Supplement. The guideline contains an electronic tool for nutritional risk assessment and an instructional video showing how to perform the swallow test.20
Choice of screening instrument for undernutrition and nutritional risk
Ideally, screening tools consider body mass index at admission, unintentional weight loss, the time over which nutrient intake has been reduced, and the likelihood of future impaired nutrient intake caused by the present condition.23 No specific tool for NRS has been developed for patients with stroke. We chose the NRS tool (NRS 2002) that was developed for in-hospital use. NRS 2002 is the only validated instrument that considers both age and severity of disease, and a moderate nutritional risk is assigned to having a stroke.24 In a comparison of the best documented tools, NRS 2002 had the highest sensitivity, specificity, and positive and negative predictive values.25 It is also the preferred tool for in-hospital use in the Norwegian guidelines for prevention and treatment of malnutrition.26 Even in a well-nourished patient, having a major stroke confers a high risk of developing undernutrition. Therefore, we assigned high nutritional risk (NRS score 3) to having a stroke with a severity of ≥15 (of maximum 42) points on the National Institutes of Health Stroke Scale.27
Choice of screening tool for dysphagia
The best protocol for swallow tests remains unclear. With few exceptions, a water swallow test is the central item in dysphagia screening.28 The swallow test that is part of the Norwegian guideline for treatment of stroke contains nonswallowing items and a water swallow test that offers a teaspoon full of water 3 times before the patients tries to drink 50 mL of water, closely resembling the Standardized Swallowing Assessment with modifications as suggested by Perry.29,30 This test reliably identified patients with acute stroke who can safely eat and drink, having a negative predictive value of 96%.31
Implementation Activities
Period I
Implementation activities were limited to the time of guideline introduction and are described in the methods section.
Period II—clinical microsystems approach
Discussing performance in fortnightly team meetings and implementing necessary changes immediately was essential for achieving optimal performance. Nurses were reminded of the rationale for NRS of all patients, also those with minor strokes and those who appeared to be well nourished.
A few simple practical improvements made “doing the right thing easy.” Body mass index is a central item in NRS. Weighing the patient appeared to be the main barrier to NRS. A wheelchair scale was available in the stroke unit from January 2014 and increased the number of patients who could be weighed. In critically ill patients, measuring height and weight is practically challenging and strenuous for the patient. We decided to accept weight estimates based on reliable information from the patient or from other sources, thus allowing for proactive nutritional management from admission. As soon as the patient was able to sit in a wheelchair, a body weight measurement was performed. Including NRS in admission routines for all patients with stroke by enforcing a 48-hour time limit increased performance: “don’t put off until tomorrow what you can do today.” In patients who were critically ill and who received standard intravenous or tube feeding, we considered performing NRS within 7 days to be acceptable. From April 2014, physicians were encouraged to actively use checklists during ward rounds and ask for screening results. The nurses found close cooperation with the nutritionist rewarding. Their competence increased and resulted in an increased focus on nutritional management in all patients.
Audit
Patients
Patient characteristics are summarized in Table 1. During period I (12 months) and period II (6 months), respectively, 199 and 86 patients were admitted to our stroke unit and stayed for at least 48 hours. Patients who died within 2 weeks of admission were excluded from the audit.
Table 1.
Proportion of Patients Screened for Nutritional Risk and Swallowing Difficulties.
| Period I (12 Months, June 1, 2012 to May 31, 2013) | Period II (6 Months, December 1, 2013 to May 31, 2014) | |
|---|---|---|
| Individuals admitted to the stroke unit, n | 199 | 86 |
| On the day of stroke, % (n) | 79.9 (159) | 68.6 (59) |
| On the day after stroke, % (n) | 20.1 (40) | 31.4 (27) |
| Age, median (range) | 75 (20-94) | 75 (22-92) |
| Women, % (n) | 44.7 (89) | 38.4 (33) |
| Death within 2 weeks of admission, % (n) | 7.0 (14) | – |
| Death within 2 weeks of admission or terminal care only, % (n) | – | 8.1 (7) |
| Individuals included in analyses,a n | 185 | 79 |
| Nutritional risk | ||
| NRSb days 0-7, % (n) | 65.4 (121) | 87.3 (69) |
| NRS days 0-2 (period II <48 h), % (n) | 47.6 (88) | 72.2 (57) |
| Nutritional risk (NRS score ≥3) days 0-7, % (n) | 31.4 (38) | 24.6 (17) |
| Swallowing difficulties | ||
| Swallow test days 0-1/<6 h | 90.8% (168)/- | 97.5% (77)/92.4% (73) |
| Time to swallow test, median | – | 2 h 13 minc |
| Failed initial swallow test, % (n) | 23.3% (39) | 23.4% (18) |
Abbreviation: NRS, nutritional risk screening.
aPatients who died within 2 weeks of admission or who received terminal care only were excluded.
bNutritional risk screening using the NRS 2002 instrument.24
cLongest time to swallow test was 9 hours 53 minutes, 94.8% were tested within 6 hours.
Performance of screening tests
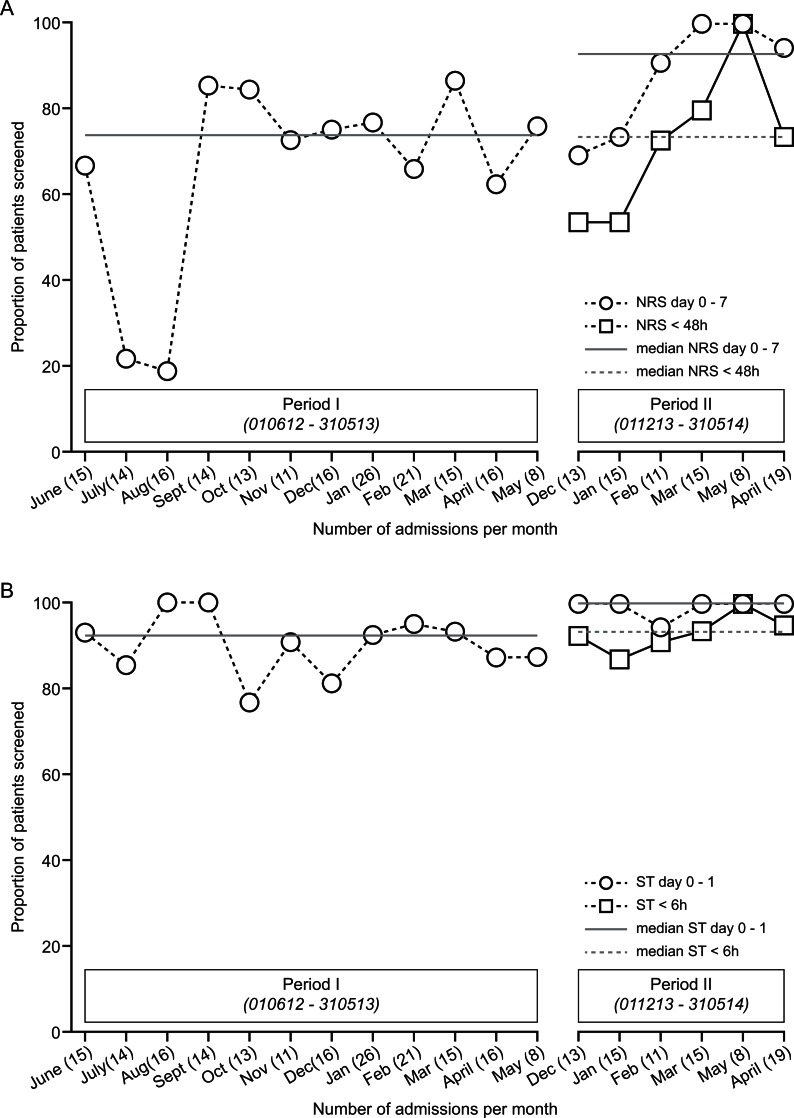
Nutritional risk screening was performed within 7 days after admission in 65.4% (period I)/87.3% (period 2) of patients (Table 1). During the last 4 months of period II, NRS was performed in 96% of patients within 7 days of admission. Figure 1A shows the proportion of eligible patients screened for nutritional risk each month.
Figure 1.
A, Nutritional risk screening (NRS): proportion of eligible patients screened each month. Numbers in parentheses on the x-axis indicate number of patients admitted. Statistical process control (SPC) identified values for proportion of patients screened during July and August 2012 as being statistical outliers. These observations were excluded from calculation of the median. During the last 4 months of period II, NRS was performed in 96% of patients within 7 days of admission. B, Swallow test (ST): proportion of eligible patients screened each month. Numbers in parentheses on the x-axis indicate number of patients admitted.
During period I, 65.4% of the patients were screened, and 31.4% were at nutritional risk. During period II, the proportion screened increased to 87.3%, while the proportion of patients at nutritional risk decreased to 24.6% (Table 1).
A swallowing test was performed before food or drink was offered in 90.8%/97.5% of the patients. During period II, 94.8% of patients were screened within 6 hours. Median time to swallow test was 2 hours 13 minutes. During both periods, 23% of patients failed the initial swallow test.
Discussion
The goal of full implementation was reached by continuous proactive implementation of the guideline during a 6-month period. We found working in a team performing rapid improvement cycles highly rewarding. Some of our experiences are detailed in the Results section. Combining focus on nutritional risk and swallowing problems improved nutritional management of the patients in our stroke unit.
In this unselected population of patients with acute stroke, the proportion of individuals at nutritional risk and the prevalence of dysphagia at initial swallow test were in the lower range of previous reports.
The Norwegian guideline for nutrition in patients with acute stroke recommends combining validated screening instruments for nutritional risk and dysphagia at admission. We graded the recommendation for both NRS and performing a swallow test before offering food or drink as SIGN grade B,22 which is in accordance with most published guidelines (e-Supplement). The guideline contains an electronic tool for nutritional risk assessment and an instructional video showing how to perform the swallow test.20
There is no evidence supporting specific time frames for completion of nutritional screening.32 Nutritional risk screening during the first week in the stroke unit increased from 65.4% in period I to 87.3% after proactive implementation in period II. This is considerably higher than 18% compliance for screening during a 7-month period reported earlier.33
During period II, 82.6% of screenings were performed within 48 hours after admission. Continuous active implementation was required to reach the goal of full implementation during the last 4 months of period II: 96% of patients were screened for nutritional risk within 7 days upon admission to the stroke unit. Systematically identifying and treating patients at nutritional risk also increased reimbursement.
In our stroke unit, the proportion of patients screened for swallowing problems was high at onset and approached 100% without specific implementation efforts. Very few (2.5%) patients were not screened at all, and some (5.3%) were screened between 6 and 10 hours after admission.
Large studies have shown a clear association of more frequent screening in patients with increasing stroke severity but also a nontrivial risk of pneumonia in patients with very mild deficits.16 Perry and McLaren reported that nurses used validated tools for swallow testing in 39% of 200 patients studied during a 7-month period after implementation of a guideline.33
Lakshminarayan et al increased the proportion of patients screened from 36% to 74% by introducing an electronic medical record-based clinical decision support tool but concluded that dysphagia screening is a difficult performance measure to improve.34 In recent years, dysphagia screening before oral intake in patients with acute stroke has become a hospital-level performance measure in many countries. A national audit in the United Kingdom found that 86% of the patients admitted to stroke units were screened for swallowing disorders within 24 hours of admission.35 Another quality initiative to maximize dysphagia screening obtained similar results, increasing compliance with guidelines from 39.3% to 74.2%.18 The authors also report that increasing the percentage of patients with stroke screened for dysphagia coincided with a drop in hospital-acquired pneumonia from 6.5% to 2.8%.18 Increasing the proportion screened to more than 95% probably confers less benefit. However, inexperienced nurses and junior doctors may not be able to select patients who might have swallowing difficulties. In our stroke unit, screening all patients at admission avoided delay of nutrition by mouth or by feeding tube.
Nutritional risk was identified by NRS 200224 in close to 30% of patients screened, which is in the range reported previously by authors using a variety of methods for NRS.3,11,13,23,36,37 When the proportion of patients who were screened for nutritional risk increased in period II, the proportion of patients at nutritional risk decreased. Although this change was not statistically significant, it might indicate increased screening of persons who appeared to be well nourished to nurses and therefore were not formally screened during period I.16
Early recognition of nutritional risk allows necessary measures to be taken before loss of weight occurs. Nutritional risk increases substantially during the first week in hospital in patients who cannot maintain nutritional intake due to dysphagia or other stroke-related factors. Therefore, both stroke severity and presence of dysphagia should be included in screening tools to be used in patients with acute stroke.
We found that 23.3% of the patients failed the initial swallowing test, 29.4% including those who died within 2 weeks of admission or received terminal care only, assuming they had a reduced level of consciousness and were not able to cooperate during testing. Our findings are in the lower range of previous reports indicating that dysphagia is present in one-third to one-half of the patients with acute stroke.2-7
Although swallowing function improves during the first days after the stroke in many patients,38 appropriate management is essential not only to prevent aspiration pneumonia but also to ensure that nutritional needs are met early.
The strength of this study is that we report complete data on all patients who were admitted to our acute stroke unit. The retrospective data collected from electronic hospital records in period I may underestimate the proportion screened for nutritional risk or swallowing problems, because of lacking or ambiguous documentation. Collecting data while the patient was in the stroke unit (period II) allowed for correcting or completing the data.
We have not collected data to support our assumption that the clinical microsystem approach or specific interventions were effective. Neither did we attempt to measure the effect of detecting nutritional risk or swallowing problems soon after admission on short-term or long-term outcomes in this small study. Studying the individual and combined effects of screening for nutritional risk and swallowing problems requires large unselected groups of patients, preferably data collected in a Stroke Registry.
Conclusion
Both undernutrition and dysphagia are prevalent in patients with acute stroke and contribute, alone or in combination, to poor outcome in stroke. Based on the importance of swallowing for nutrition, we assume a synergistic effect of combining nutritional status assessment with a swallow test at admission, immediately followed by appropriate management. We suggest that dysphagia and stroke severity be included in nutritional screening tools used in patients with acute stroke.
Implementation of screening tests and follow-up assessments for nutritional risk and swallowing difficulties require continuous efforts. We highly recommend the “clinical microsystems approach” for achieving improvement.
Supplementary Material
Acknowledgments
We highly appreciate the contribution of the nurses in the stroke unit and the members of the improvement team.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: The online data supplement is available at http://nhos.sagepub.com/supplemental.
References
- 1. Ha L, Hauge T, Iversen PO. Body composition in older acute stroke patients after treatment with individualized, nutritional supplementation while in hospital. BMC Geriatr. 2010;10:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lakshminarayan K, Tsai AW, Tong X, et al. Utility of dysphagia screening results in predicting poststroke pneumonia. Stroke. 2010;41(12):2849–2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Crary MA, Carnaby-Mann GD, Miller L, Antonios N, Silliman S. Dysphagia and nutritional status at the time of hospital admission for ischemic stroke. J Stroke Cerebrovasc Dis. 2006;15(4):164–171. [DOI] [PubMed] [Google Scholar]
- 4. Ickenstein GW, Hohlig C, Prosiegel M, et al. Prediction of outcome in neurogenic oropharyngeal dysphagia within 72 hours of acute stroke. J Stroke Cerebrovasc Dis. 2012;21(7):569–576. [DOI] [PubMed] [Google Scholar]
- 5. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–2763. [DOI] [PubMed] [Google Scholar]
- 6. Flowers HL, Silver FL, Fang J, Rochon E, Martino R. The incidence, co-occurrence, and predictors of dysphagia, dysarthria, and aphasia after first-ever acute ischemic stroke. J Commun Disord. 2013;46(3):238–248. [DOI] [PubMed] [Google Scholar]
- 7. Guyomard V, Fulcher RA, Redmayne O, Metcalf AK, Potter JF, Myint PK. Effect of dysphasia and dysphagia on inpatient mortality and hospital length of stay: a database study. J Am Geriatr Soc. 2009;57(11):2101–2106. [DOI] [PubMed] [Google Scholar]
- 8. FOOD Trial Collaboration. Poor nutritional status on admission predicts poor outcomes after stroke: observational data from the FOOD trial. Stroke. 2003;34(6):1450–1456. [DOI] [PubMed] [Google Scholar]
- 9. Shen HC, Chen HF, Peng LN, et al. Impact of nutritional status on long-term functional outcomes of post-acute stroke patients in Taiwan. Arch Gerontol Geriatr. 2011;53(2):e149–e152. [DOI] [PubMed] [Google Scholar]
- 10. Yoo SH, Kim JS, Kwon SU, Yun SC, Koh JY, Kang DW. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Arch Neurol. 2008;65(1):39–43. [DOI] [PubMed] [Google Scholar]
- 11. Davis JP, Wong AA, Schluter PJ, Henderson RD, O’Sullivan JD, Read SJ. Impact of premorbid undernutrition on outcome in stroke patients. Stroke. 2004;35(8):1930–1934. [DOI] [PubMed] [Google Scholar]
- 12. Scherbakov N, Dirnagl U, Doehner W. Body weight after stroke: lessons from the obesity paradox. Stroke. 2011;42(12):3646–3650. [DOI] [PubMed] [Google Scholar]
- 13. Gariballa SE, Parker SG, Taub N, Castleden M. Nutritional status of hospitalized acute stroke patients. Br J Nutr. 1998;79(6):481–487. [DOI] [PubMed] [Google Scholar]
- 14. Hannawi Y, Hannawi B, Rao CP, Suarez JI, Bershad EM. Stroke-associated pneumonia: major advances and obstacles. Cerebrovasc Dis. 2013;35(5):430–443. [DOI] [PubMed] [Google Scholar]
- 15. Sellars C, Bowie L, Bagg J, et al. Risk factors for chest infection in acute stroke: a prospective cohort study. Stroke. 2007;38(8):2284–2291. [DOI] [PubMed] [Google Scholar]
- 16. Masrur S, Smith EE, Saver JL, et al. Dysphagia screening and hospital-acquired pneumonia in patients with acute ischemic stroke: findings from Get with the Guidelines—Stroke. J Stroke Cerebrovasc Dis. 2013;22(8):e301–e309. [DOI] [PubMed] [Google Scholar]
- 17. Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S. Formal dysphagia screening protocols prevent pneumonia. Stroke. 2005;36(9):1972–1976. [DOI] [PubMed] [Google Scholar]
- 18. Titsworth WL, Abram J, Fullerton A, et al. Prospective quality initiative to maximize dysphagia screening reduces hospital-acquired pneumonia prevalence in patients with stroke. Stroke. 2013;44(11):3154–3160. [DOI] [PubMed] [Google Scholar]
- 19. Ickenstein GW, Riecker A, Hohlig C, et al. Pneumonia and in-hospital mortality in the context of neurogenic oropharyngeal dysphagia (NOD) in stroke and a new NOD step-wise concept. J Neurol. 2010;257(9):1492–1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kampman MT, Johnsen SH. Hjerneslag—ernæring i akuttfasen [Nutrition in acute stroke]. The Norwegian Electronic Health Library’s website; 2012. Web site http://www.helsebiblioteket.no/microsite/fagprosedyrer/fagprosedyrer/hjerneslag-ern%C3%A6ring-i-akuttfasen. Accessed May 22, 2015. [Google Scholar]
- 21. Nelson EC, Batalden PB, Godfrey MM. Quality by Design: A Clinical Microsystems Approach. 1st ed. San Francisco: Jossey-Bass; 2005. [Google Scholar]
- 22. SIGN grading system 1999–2012. Web site http://www.sign.ac.uk/guidelines/fulltext/50/annexoldb.html. Accessed May 22, 2015.
- 23. Foley NC, Salter KL, Robertson J, Teasell RW, Woodbury MG. Which reported estimate of the prevalence of malnutrition after stroke is valid? Stroke. 2009;40(3):e66–e74. [DOI] [PubMed] [Google Scholar]
- 24. Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321–336. [DOI] [PubMed] [Google Scholar]
- 25. Kyle UG, Kossovsky MP, Karsegard VL, Pichard C. Comparison of tools for nutritional assessment and screening at hospital admission: a population study. Clin Nutr. 2006;25(3):409–417. [DOI] [PubMed] [Google Scholar]
- 26. Norwegian Directorate of Health: Nasjonal faglig retningslinje for forebygging og behandling av underernæring [Norwegian guideline for prevention and treatment of malnutrition]; 2009. Web site http://helsedirektoratet.no/publikasjoner/nasjonal-faglig-retningslinje-for-forebygging-og-behandling-av-underernering/Sider/default.aspx. Accessed May 22, 2015.
- 27. National Institutes of Health Stroke Scale. National Institute of Neurological Disorders and Stroke; 2003. Web site http://www.ninds.nih.gov/doctors/NIH_Stroke_Scale.pdf. Accessed May 22, 2015.
- 28. Donovan NJ, Daniels SK, Edmiaston J, Weinhardt J, Summers D, Mitchell PH. Dysphagia screening: state of the art: invitational conference proceeding from the State-of-the-Art Nursing Symposium, International Stroke Conference 2012. Stroke. 2013;44(4):e24–e31. [DOI] [PubMed] [Google Scholar]
- 29. Norwegian Directorate of Health: Behandling og rehabilitering ved hjerneslag [Norwegian stroke guideline]; 2010. Web site http://helsedirektoratet.no/publikasjoner/nasjonal-retningslinje-for-behandling-og-rehabilitering-ved-hjerneslag-fullversjon/Sider/default.aspx. Accessed May 22, 2015.
- 30. Perry L. Screening swallowing function of patients with acute stroke. Part two: detailed evaluation of the tool used by nurses. J Clin Nurs. 2001;10(4):474–481. [DOI] [PubMed] [Google Scholar]
- 31. Perry L. Screening swallowing function of patients with acute stroke. Part one: identification, implementation and initial evaluation of a screening tool for use by nurses. J Clin Nurs. 2001;10(4):463–473. [DOI] [PubMed] [Google Scholar]
- 32. Luker JA, Wall K, Bernhardt J, Edwards I, Grimmer-Somers K. Measuring the quality of dysphagia management practices following stroke: a systematic review. Int J Stroke. 2010;5(6):466–476. [DOI] [PubMed] [Google Scholar]
- 33. Perry L, McLaren S. Nutritional support in acute stroke: the impact of evidence-based guidelines. Clin Nutr. 2003;22(3):283–293. [DOI] [PubMed] [Google Scholar]
- 34. Lakshminarayan K, Rostambeigi N, Fuller CC, Peacock JM, Tsai AW. Impact of an electronic medical record-based clinical decision support tool for dysphagia screening on care quality. Stroke. 2012;43(12):3399–3401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Royal College of Physicians: National Sentinel Stroke Clinical Audit 2010, Round 7; 2011. Web site https://www.rcplondon.ac.uk/sites/default/files/national-sentinel-stroke-audit-2010-public-report-and-appendices_0.pdf. Accessed February 1, 2015.
- 36. Ha L, Hauge T, Spenning AB, Iversen PO. Individual, nutritional support prevents undernutrition, increases muscle strength and improves QoL among elderly at nutritional risk hospitalized for acute stroke: a randomized, controlled trial. Clin Nutr. 2010;29(5):567–573. [DOI] [PubMed] [Google Scholar]
- 37. Martineau J, Bauer JD, Isenring E, Cohen S. Malnutrition determined by the patient-generated subjective global assessment is associated with poor outcomes in acute stroke patients. Clin Nutr. 2005;24(6):1073–1077. [DOI] [PubMed] [Google Scholar]
- 38. Smithard DG, O’Neill PA, England RE, et al. The natural history of dysphagia following a stroke. Dysphagia. 1997;12(4):188–193. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.