Abstract
Introduction
Consensus criteria for pediatric severe sepsis have standardized enrollment for research studies. However, the extent to which critically ill children identified by consensus criteria reflect physician diagnosis of severe sepsis, which underlies external validity for pediatric sepsis research, is not known. We sought to determine the agreement between physician diagnosis and consensus criteria to identify pediatric patients with severe sepsis across a network of international pediatric intensive care units (PICUs).
Methods
We conducted a point prevalence study involving 128 PICUs in 26 countries across 6 continents. Over the course of 5 study days, 6925 PICU patients <18 years of age were screened, and 706 with severe sepsis defined either by physician diagnosis or on the basis of 2005 International Pediatric Sepsis Consensus Conference consensus criteria were enrolled. The primary endpoint was agreement of pediatric severe sepsis between physician diagnosis and consensus criteria as measured using Cohen’s κ. Secondary endpoints included characteristics and clinical outcomes for patients identified using physician diagnosis versus consensus criteria.
Results
Of the 706 patients, 301 (42.6 %) met both definitions. The inter-rater agreement (κ ± SE) between physician diagnosis and consensus criteria was 0.57 ± 0.02. Of the 438 patients with a physician’s diagnosis of severe sepsis, only 69 % (301 of 438) would have been eligible to participate in a clinical trial of pediatric severe sepsis that enrolled patients based on consensus criteria. Patients with physician-diagnosed severe sepsis who did not meet consensus criteria were younger and had lower severity of illness and lower PICU mortality than those meeting consensus criteria or both definitions. After controlling for age, severity of illness, number of comorbid conditions, and treatment in developed versus resource-limited regions, patients identified with severe sepsis by physician diagnosis alone or by consensus criteria alone did not have PICU mortality significantly different from that of patients identified by both physician diagnosis and consensus criteria.
Conclusions
Physician diagnosis of pediatric severe sepsis achieved only moderate agreement with consensus criteria, with physicians diagnosing severe sepsis more broadly. Consequently, the results of a research study based on consensus criteria may have limited generalizability to nearly one-third of PICU patients diagnosed with severe sepsis.
Electronic supplementary material
The online version of this article (doi:10.1186/s13054-015-1055-x) contains supplementary material, which is available to authorized users.
Introduction
Sepsis is a leading cause of death in children worldwide, responsible for an estimated 75,000 hospitalizations annually in the United States and nearly 50 % of all childhood hospital deaths worldwide [1–5]. Within the spectrum of this syndrome, severe sepsis refers to children with shock or other organ dysfunction and is the high-risk group targeted for interventional studies in the pediatric intensive care unit (PICU) [6].
Investigators in clinical trials of severe sepsis face important challenges that have contributed to high failure rates for many promising novel therapies, with few attempts to include children [7]. One fundamental issue is that the sepsis syndrome is characterized by non-specific physiologic abnormalities that encompass a heterogeneous population. Consensus criteria for pediatric sepsis were therefore established to facilitate consistent enrollment across research studies [6]. Many of these criteria have since been adopted for use in clinical practice [8]; however, published reports have demonstrated only moderate overlap of physician diagnosis of severe sepsis with consensus criteria [9, 10]. These findings raise concern that many children diagnosed and treated for severe sepsis in clinical practice may have important physiologic—and outcome—differences from those studied in interventional trials [9, 10].
The degree to which a study population is representative of patients diagnosed and treated in clinical practice has a major impact on the external validity of a study [11–13]. Although physician diagnosis serves clinical practice and consensus criteria were intended primarily for research, the alignment of these two methods to identify children with severe sepsis will significantly impact the extent to which study results translate into effective care at the bedside. Moreover, criteria that purposely define a disorder as a decompensated state at one extreme of the entire spectrum—as the existing pediatric consensus definitions currently do for severe sepsis and septic shock—may hinder early clinical diagnosis or delay enrollment in a clinical trial. Although the inherent challenge between research efficacy and clinical effectiveness is not limited to sepsis [14–17], understanding the extent to which consensus criteria for pediatric severe sepsis are in agreement with clinical practice will help to improve understanding of the utility of these criteria and to identify ways to improve both physician diagnosis and consensus definitions. To date, the agreement of physician diagnosis with consensus criteria for pediatric severe sepsis has not been evaluated in a large-scale setting.
The Sepsis PRevalence, OUtcomes, and Therapies (SPROUT) study researchers screened nearly 7000 PICU patients for severe sepsis at 128 sites across 26 countries using consensus criteria [18]. In addition, the attending physician caring for each patient provided an independent diagnostic assessment for severe sepsis. Using these data, we determined the level of agreement between consensus criteria [6] and attending physician diagnostic assessment (“physician diagnosis”) for pediatric severe sepsis. We hypothesized that agreement would be moderate at best, and thus we aimed to compare differences in patient characteristics, treatment strategies, and outcomes for children identified as having severe sepsis by consensus criteria versus physician diagnosis.
Material and methods
Study design
SPROUT was a prospective point prevalence study performed at 128 PICUs in 26 countries over the course of 5 study days spaced over 1 year [18]. Sites were recruited by open invitation through established research networks, and participation was voluntary. Ethical approval was obtained at all sites, and waiver of informed consent was granted at all but three sites, at which written consent was required for data collection (see Additional file 1 for a list of all approving ethical bodies). The details of the SPROUT study methodology have been published previously [18].
Study population
All patients <18 years of age being treated in a participating PICU at 9:00 am local time on each study day were screened for severe sepsis using a standardized form incorporating the 2005 International Pediatric Sepsis Consensus Conference criteria: (1) at least two systemic inflammatory response syndrome criteria; (2) confirmed or suspected invasive infection; and (3) cardiovascular dysfunction, acute respiratory distress syndrome (ARDS), or at least two organ dysfunctions [6]. The subset of patients with septic shock defined by cardiovascular dysfunction were included within the spectrum of severe sepsis. Only data available within the 24 h preceding the 9:00 am study day time were considered for screening, yielding a study cohort with active severe sepsis. Patients who were ≥18 years of age, corrected gestational age <42 weeks, or had surgery involving cardiopulmonary bypass in the preceding 5 days were excluded.
To ascertain physician diagnosis of severe sepsis, an investigator at each site provided a list of patients, using a standardized form, to the attending physician of record on each study day. Attending physicians were instructed as follows: “In your clinical opinion, does this patient (yes or no) meet criteria for severe sepsis and/or septic shock when considering data only from the past 24 h (i.e., 9:00 am yesterday to 9:00 am today)?” Attending physicians who provided diagnoses were not involved with screening of patients for severe sepsis by consensus criteria. Similarly, site investigators screening for consensus criteria were blinded to physician diagnosis.
Data collection
Data were collected about demographics, comorbid conditions, admission source, laboratory results, and therapies within a 48-h window around the study day (9:00 am before to 9:00 am after the study day). Definitions for the primary site of infection were adapted from published criteria [18]. The day of severe sepsis recognition was identified as the first calendar day on which a patient met consensus conference criteria for severe sepsis [6], and the presence of new or progressive multiorgan dysfunction syndrome (NPMODS) was measured for 7 days following severe sepsis recognition [19–21]. New MODS was defined as no or one organ dysfunction at sepsis recognition with subsequent development of at least two organ dysfunctions. Progressive MODS was defined as existing multiorgan dysfunction syndrome (MODS) (at least two organ dysfunctions) at sepsis recognition with development of at least one other concurrent organ dysfunction. For severe sepsis screening, organ dysfunctions were defined using pediatric sepsis consensus conference criteria [6], whereas more stringent criteria were used to define NPMODS [21]. For severity of illness, the Pediatric Index of Mortality (PIM)-3 score [22] was calculated at PICU admission, whereas the Pediatric Logistic Organ Dysfunction (PELOD) score [23] was calculated on the study day.
Patients with severe sepsis were followed for 90 days or until death or hospital discharge. Outcomes included vasoactive- and ventilator-free days from day of severe sepsis recognition through day 28, NPMODS, change in functional status from admission to hospital discharge (using the Pediatric Overall Performance Category [POPC] 1–6 ordinal scale [24]), and all-cause mortality at PICU discharge. Patients surviving to hospital discharge were classified as having “at least mild disability” for any increase in POPC and “at least moderate disability” if discharge POPC was 3 or higher and increased by at least 1 from baseline [25].
All data were recorded and managed using standardized case report forms within the web-based Research Electronic Data Capture (or REDCap) system, a secure database that provides an intuitive interface for validated data entry and audit trails for tracking data [26]. The methods used to ensure data quality and confidentiality have been published previously [18].
The primary outcome was the level of agreement in identification of pediatric severe sepsis between physician diagnosis and consensus criteria. Secondary outcomes included differences in patient characteristics, therapies used, and clinical outcomes between patients identified using physician diagnosis versus consensus criteria.
Statistical analysis
Analyses were performed using STATA software (version 12.1; College Station, TX, USA). Data are presented as medians with interquartile ranges for continuous variables and frequencies with percentages for categorical variables. Comparisons between groups were performed using the Kruskal-Wallis test for continuous variables, and categorical variables were compared using Fisher’s exact test. For variables in which significant differences were identified across all three groups, pairwise comparisons were performed using Wilcoxon rank-sum or Fisher’s exact tests for continuous or categorical variables, respectively. The level of agreement between the two methods to identify patients with severe sepsis was quantified using percentage agreement and Cohen’s κ. Multivariable logistic regression was used to test the independent association of each definition of severe sepsis with PICU mortality after controlling for patient-level variables found to be significantly different across groups. Status as a developed (North America, Australia/New Zealand, and Europe) or resource-limited (Asia, Africa, and South America) region did not provide significant effect modification when tested as an interaction term with definition of severe sepsis (p = 0.36), but it was included as a confounder in the final logistic regression model. Statistical significance was defined as a p value <0.05.
Results
Over the 5 study days, 6925 PICU patients were screened across all sites. In total, 706 were identified with severe sepsis by either consensus criteria or physician diagnosis, with 137 patients (19.4 %) identified by physician diagnosis only, 301 (42.6 %) by both definitions, and 268 (38.0 %) by consensus criteria only (Fig. 1). The percentage agreement between consensus criteria and physician diagnosis for identifying severe sepsis in the entire cohort of screened patients was 94 %, but it was only 43 % for identifying severe sepsis among the 706 patients with sepsis by either definition. The inter-rater agreement between physician diagnosis and consensus criteria achieved a moderate κ ± standard error of 0.57 ± 0.02. The percentage agreement between physician diagnosis and consensus criteria varied significantly across geographic regions (p < 0.001). Agreement was lowest in North America (31 % agreement of 444 patients identified with severe sepsis by any criteria); moderate in Australia and New Zealand (45 %) and Europe (51 %); and highest in Asia (72 %), Africa (72 %), and South America (85 %). The percentage agreement was 44 %, 49 %, 45 %, 38 %, and 39 % across study days 1–5, respectively, suggesting that clinicians did not alter their diagnostic assessment to better comply with consensus criteria over time.
Fig. 1.
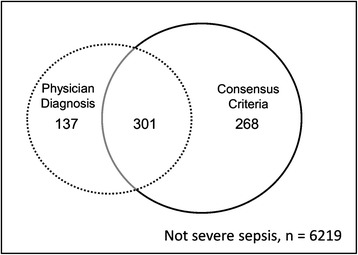
Venn diagram of the overlap between patients identified with severe sepsis by attending physician diagnostic assessment (“physician diagnosis”) and the 2005 International Pediatric Sepsis Consensus Conference (“consensus criteria”). Of the 6925 pediatric intensive care unit patients screened, 706 were identified with severe sepsis but only 301 (43 %) were concurrently identified by both physician diagnosis and consensus criteria (κ 0.57 ± 0.02)
Of the 438 total patients with a physician diagnosis of severe sepsis, 31 % were not concurrently identified with severe sepsis by consensus criteria and thus would have been ineligible to participate in a clinical trial that enrolled patients based on the criteria established by consensus guidelines. Moreover, 47 % of the patients identified as having severe sepsis by consensus criteria—and thus potentially eligible for a clinical trial—were not simultaneously considered to have severe sepsis by physician diagnosis.
Characteristics of 704 of the patients identified with severe sepsis by physician diagnosis alone, by both definitions, or by consensus criteria alone are shown in Table 1. Data could not be obtained for two patients (both identified by consensus criteria alone) who did not consent to data collection at one site that required informed consent for this purpose. Patients identified only by physician diagnosis were younger (p = 0.008), had a lower severity of illness (lower PIM-3 [p < 0.001] and PELOD [p < 0.001] scores), and a lower proportion of cardiovascular (p = 0.006) and hematologic dysfunction (p < 0.001) at sepsis recognition than patients identified by consensus criteria alone or both definitions. Patients identified by consensus criteria alone were less likely to be previously healthy (p = 0.002) and more likely to have neuromuscular comorbidities (p < 0.001) than patients identified by physician diagnosis alone or both definitions. Patients identified by consensus criteria alone were more likely to have respiratory (p = 0.004) or unknown primary site of infection (p = 0.002) and less likely to have primary bloodstream infection (p < 0.001).
Table 1.
Characteristics of patients identified with severe sepsis by physician diagnosis, consensus criteria, or both
| Characteristic | Physician diagnosis | Both criteria | Consensus criteria | p value* |
|---|---|---|---|---|
| N | 137 | 301 | 266 | |
| Age (yr) | 1 (0.5–7) | 3 (0.7–10) | 3 (0.7–11) | 0.03 |
| Sex, n (%) | 0.74 | |||
| Male | 76 (55) | 164 (55) | 138 (52) | |
| Female | 61 (45) | 137 (45) | 128 (48) | |
| Comorbid conditions, n (%) | ||||
| Respiratory | 54 (39) | 73 (24) | 99 (37) | 0.001 |
| Gastrointestinal | 40 (29) | 62 (21) | 79 (30) | 0.03 |
| Cardiovascular | 34 (25) | 62 (21) | 74 (28) | 0.13 |
| Genetic | 35 (26) | 54 (18) | 61 (23) | 0.14 |
| Hematologic/immunologic | 28 (20) | 69 (23) | 45 (17) | 0.21 |
| Neuromuscular | 11 (8) | 37 (12) | 60 (23) | <0.001 |
| Neoplastic | 18 (13) | 51 (17) | 29 (11) | 0.11 |
| Prematurity | 37 (12) | 24 (18) | 39 (15) | 0.35 |
| Metabolic | 17 (12) | 28 (9) | 34 (13) | 0.38 |
| Renal | 15 (11) | 24 (8) | 31 (12) | 0.31 |
| Solid organ/stem cell transplant | 8 (6) | 28 (9) | 26 (10) | 0.39 |
| Comorbid conditions, n (%) | <0.001 | |||
| None | 30 (22) | 85 (28) | 43 (16) | |
| 1 | 21 (15) | 77 (26) | 64 (24) | |
| ≥ 2 | 86 (63) | 21 (15) | 159 (60) | |
| Admission POPC, n (%) | 0.13 | |||
| Good performance | 70 (51) | 170 (56) | 120 (45) | |
| Mild disability | 26 (19) | 44 (15) | 41 (15) | |
| Moderate disability | 22 (16) | 44 (15) | 46 (17) | |
| Severe disability or coma | 19 (14) | 43 (14) | 59 (22) | |
| PIM-3 scorea | 3.6 (1.4–5.5) | 4.4 (1.9–9.2) | 4.3 (1.8–9.9) | <0.001 |
| PELOD scoreb | 10 (1–11) | 11 (2–13) | 11 (2–12) | <0.001 |
| Source of admission, n (%) | 0.86 | |||
| Emergency departmentc | 41 (30) | 89 (30) | 78 (29) | |
| Hospital floor | 39 (29) | 92 (31) | 66 (25) | |
| Operating room | 12 (9) | 28 (9) | 22 (8) | |
| Other hospitald | 39 (28) | 77 (26) | 89 (33) | |
| Organ dysfunction at sepsis recognitione | ||||
| Cardiovascular | 51 (37) | 182 (61) | 106 (40) | <0.001 |
| Respiratory | 88 (64) | 211 (70) | 197 (74) | 0.12 |
| Renal | 5 (4) | 19 (6) | 7 (3) | 0.10 |
| Hepatic | 2 (1) | 16 (5) | 6 (2) | 0.07 |
| Hematologic | 4 (3) | 49 (16) | 24 (9) | <0.001 |
| Neurologic | 9 (7) | 28 (9) | 33 (12) | 0.17 |
| Primary site of infection, n (%) | ||||
| Respiratory | 60 (44) | 101 (34) | 127 (48) | 0.002 |
| Primary bloodstream | 25 (18) | 82 (27) | 26 (10) | <0.001 |
| Abdominal | 15 (11) | 31 (10) | 16 (6) | 0.11 |
| Central nervous system | 3 (2) | 9 (3) | 16 (6) | 0.11 |
| Genitourinary | 7 (5) | 12 (4) | 9 (3) | 0.67 |
| Skin | 4 (3) | 16 (5) | 4 (2) | 0.04 |
| Other | 6 (4) | 16 (5) | 13 (5) | 0.95 |
| Unknown | 17 (12) | 34 (11) | 55 (21) | 0.006 |
| Microbiology,f,g n (%) | ||||
| Gram-positive bacteria | 39 (28) | 90 (30) | 60 (23) | 0.13 |
| Gram-negative bacteria | 27 (20) | 95 (32) | 63 (24) | 0.02 |
| Fungus | 9 (7) | 39 (13) | 37 (14) | 0.07 |
| Virus | 35 (26) | 50 (17) | 69 (26) | 0.01 |
| No organism identified | 50 (36) | 95 (32) | 101 (38) | 0.25 |
Data are presented as median (IQR) unless otherwise noted
POPC Pediatric Overall Performance Category, ScvO 2 central venous oxygen saturation, PIM-3 Pediatric Index of Mortality-3, PELOD Pediatric Logistic Organ Dysfunction, PICU pediatric intensive care unit
*Statistical comparisons using Kruskal-Wallis or Fisher’s exact test
aPIM-3 measured at time of PICU admission
bPELOD score calculated from data within a 48-h time window around the study day (9:00 am before to 9:00 am after the study day)
cEmergency department at the same hospital as the PICU
dOther hospital includes emergency department at another hospital
eBased on organ dysfunction criteria defined by the International Pediatric Sepsis Consensus Conference [6]
fCategories do not add up to 100 %, as some infections were polymicrobial
gSources of positive isolates included blood, urine, cerebrospinal fluid, respiratory (nasopharynx, tracheal, bronchoalveolar lavage), stool, wound, and other normally sterile body fluids (pleural, pericardial, peritoneal)
Patients identified concurrently by both physician diagnosis and consensus criteria had lower platelet counts and higher blood lactate, C-reactive protein, and procalcitonin levels than patients identified by either criterion alone (all p < 0.01) (Table 2). Similarly, patients identified by both physician diagnosis and consensus criteria were also more likely to be treated with vasoactive infusions, albumin, blood products, granulocyte/granulocyte macrophage colony-stimulating factor, intravenous immunoglobulin, and renal replacement therapy than patients identified by either criterion alone (all p < 0.05) (Table 3).
Table 2.
Laboratory values within the 48-h data collection window by definition of severe sepsis
| Laboratory examination | Physician diagnosis | Both criteria | Consensus criteria | p value* | |||
|---|---|---|---|---|---|---|---|
| Percenta | Median (IQR) | Percenta | Median (IQR) | Percenta | Median (IQR) | ||
| WBC, max (103/μl) | 92 % | 10.1 (7.3–16.6) | 97 % | 14.9 (7.5–22.7) | 91 % | 14.6 (8.8–20.8) | <0.001 |
| Platelets, min (103/μl) | 91 % | 148 (70–262) | 96 % | 95 (39–195) | 89 % | 157 (77–287) | <0.001 |
| BUN, max (mg/dl) | 83 % | 13 (8–22) | 93 % | 21 (12–41) | 92 % | 18 (10–31) | <0.001 |
| Creatinine, max (mg/dl) | 92 % | 0.4 (0.3–0.6) | 97 % | 0.5 (0.3–0.9) | 97 % | 0.4 (0.3–0.7) | <0.001 |
| ALT, max (IU/L) | 55 % | 39 (25–67) | 77 % | 53 (28–123) | 62 % | 50 (26–110) | 0.09 |
| Total bilirubin, max (mg/dl) | 53 % | 0.7 (0.4–1.7) | 73 % | 1.0 (0.5–2.9) | 59 % | 0.7 (0.4–3.0) | 0.02 |
| Albumin, min (g/dl) | 66 % | 2.6 (2.2–3.0) | 81 % | 2.5 (2.2–3.0) | 71 % | 2.8 (2.3–3.3) | <0.001 |
| INR, max | 37 % | 1.3 (1.2–1.7) | 64 % | 1.3 (1.2–1.8) | 42 % | 1.3 (1.1–1.8) | 0.80 |
| Lactate, max (mmol/L) | 62 % | 1.4 (1.1–2.0) | 75 % | 2.0 (1.2–3.8) | 62 % | 1.6 (1.1–2.8) | 0.001 |
| ScvO2, min (%) | 28 % | 70 (57–75) | 46 % | 65 (52–74) | 30 % | 65 (49–73) | 0.50 |
| PaO2/FiO2 ratio, min (mmHg) | 47 % | 138 (89–233) | 72 % | 160 (100–236) | 51 % | 144 (87–275) | 0.79 |
| C-reactive peptide, max (mg/dl) | 39 % | 7.1 (2.1–17.8) | 64 % | 9.3 (2.8–20.8) | 43 % | 3.8 (1.6–9.7) | <0.001 |
| Procalcitonin, max (ng/ml) | 12 % | 3.5 (1.1–11.6) | 22 % | 6.4 (1.4–23.0) | 6 % | 1.3 (0.24–5.4) | 0.01 |
max maximum value within the 48-h window around the study day (9:00 am before to 9:00 am after the study day), min minimum value within the 48-h window around the study day (9:00 am before to 9:00 am after the study day), PaO 2 /FiO 2 ratio of partial pressure of oxygen to fraction of inspired oxygen, WBC white blood cell count, BUN blood urea nitrogen, ALT alanine aminotransferase, INR international normalized ratio, ScvO 2 central venous oxygen saturation
*Statistical comparisons using Kruskal-Wallis test
aProportion of each group with available laboratory results
Table 3.
Therapies used within the 48-h data collection window by definition of severe sepsis
| Therapy | Physician diagnosis | Both criteria | Consensus criteria | p value* |
|---|---|---|---|---|
| Vasoactive infusionsa | 53 (39) | 209 (69) | 105 (39) | <0.001 |
| Invasive mechanical ventilation | 92 (67) | 229 (76) | 192 (72) | 0.14 |
| Corticosteroids | 46 (36) | 132 (44) | 110 (41) | 0.13 |
| Albumin | 24 (18) | 90 (30) | 45 (17) | <0.001 |
| Blood productsb | 39 (28) | 159 (53) | 73 (27) | <0.001 |
| Insulinc | 4 (3) | 32 (11) | 25 (9) | 0.02 |
| G/GM-CSF | 2 (1) | 17 (6) | 6 (2) | 0.04 |
| IVIG | 7 (5) | 28 (9) | 10 (4) | 0.02 |
| RRTd | 13 (9) | 57 (19) | 24 (9) | 0.001 |
| Plasma exchange | 1 (1) | 3 (1) | 2 (1) | 0.94 |
| ECMO | 3 (2) | 14 (5) | 16 (6) | 0.23 |
Data presented as n (%)
G/GM-CSF granulocyte/granulocyte-monocyte colony stimulating factor, IVIG intravenous immunoglobulin, RRT renal replacement therapy, ECMO extracorporeal membrane oxygenation
*Statistical comparisons using Fisher’s exact test
aIncludes dopamine >5 μg/kg/min, dobutamine >5 μg/kg/min, or any dose of epinephrine, norepinephrine, vasopressin, phenylephrine, milrinone, levosimendan, or vasodilator
bIncludes packed red blood cells, platelets, fresh frozen plasma, cryoprecipitate, granulocytes, and whole blood
cIncludes intravenous insulin by continuous infusion only
dIncludes hemodialysis, all continuous renal replacement modalities, and peritoneal dialysis
PICU mortality was significantly lower for patients with only a physician diagnosis of severe sepsis (18 %) than with both definitions (27 %; p = 0.02) and trended lower than for consensus criteria alone (21 %; p = 0.29; Table 4). The proportion with NPMODS, at least mild disability, and at least moderate disability all trended lower for patients identified with severe sepsis by physician diagnosis alone, but none reached statistical significance. After controlling for age, PIM-3 score, number of comorbid conditions, and treatment in developed versus resource-limited regions, patients identified with severe sepsis by physician diagnosis only or by consensus criteria only did not have PICU mortality different from that of patients identified by both physician diagnosis and consensus criteria (Table 5).
Table 4.
Clinical outcomes by definition of severe sepsis
| Outcome | Physician diagnosis | Both criteria | Consensus criteria | p value* |
|---|---|---|---|---|
| Vasoactive-free days, median (IQR) | 27 (22–28) | 22 (6–26) | 26 (17–28) | <0.001 |
| Ventilator-free days, median (IQR) | 19 (2–27) | 16 (0–24) | 18 (0–26) | 0.07 |
| NPMODSa | 47 (34) | 131 (44) | 97 (36) | 0.10 |
| PICU mortality | 23 (17) | 82 (27) | 57 (21) | 0.042 |
| At least mild disabilityb | 24 (22) | 67 (31) | 50 (24) | 0.15 |
| At least moderate disabilityc | 14 (13) | 36 (17) | 37 (18) | 0.46 |
Data presented as n (%) unless otherwise noted
IQR interquartile range, NPMODS new or progressive multiorgan dysfunction syndrome, PICU pediatric intensive care unit
*Statistical comparisons using Kruskal-Wallis or Fisher’s exact test
aNPMODS considered starting the day after sepsis recognition
bAny increase in Pediatric Overall Performance Category from baseline to hospital discharge in the 534 hospital survivors
cDischarge Pediatric Overall Performance Category ≥3 and an increase of at least 1 from baseline in the 534 hospital survivors
Table 5.
Multivariable logistic regression model of the association of severe sepsis definition with PICU mortality
| Variable | Adjusted ORa | 95 % confidence interval | p value |
|---|---|---|---|
| Severe sepsis definition | |||
| Both criteria | Reference | ||
| Physician diagnosis, only | 0.64 | 0.37–1.11 | 0.12 |
| Consensus criteria, only | 0.73 | 0.48–1.12 | 0.15 |
| Age, yr | 0.99 | 0.95–1.02 | 0.45 |
| PIM-3 score | 1.04 | 1.03–1.06 | <0.001 |
| Comorbid conditions | |||
| None | Reference | ||
| 1 comorbid condition | 1.11 | 0.62–2.01 | 0.72 |
| ≥2 comorbid conditions | 1.78 | 1.07–2.99 | 0.03 |
| Developed regionb | 0.63 | 0.37–1.06 | 0.08 |
OR odds ratio, PIM-3 Pediatric Index of Mortality-3
aOdds ratios are adjusted for all of the variables listed
bSites included as “developed regions” were located in North America, Australia/New Zealand, and Europe
Discussion
Across this large international network of PICUs, physician diagnosis and consensus criteria achieved only a moderate level of agreement in identifying critically ill children with severe sepsis. These findings suggest that the results of a research study with enrollment based only on current consensus criteria may not be generalizable to nearly one-third of pediatric patients diagnosed with severe sepsis in a PICU. Moreover, for nearly half of the patients identified with severe sepsis by consensus criteria, and thus eligible for clinical trials, a diagnosis of severe sepsis was not corroborated by the treating attending physician.
The data in this study demonstrate that PICU physicians worldwide commonly diagnose critically ill children with severe sepsis who do not meet consensus criteria. This finding is consistent with a prior report of a single-center study in the United States [10]. In general, patients with physician-diagnosed severe sepsis tended to be younger, less severely ill, and less likely to receive several sepsis-related therapies than patients who also met consensus criteria. These observations likely reflect the intention of the International Pediatric Sepsis Consensus Conference to identify a more severely ill subgroup of critically ill children with severe sepsis for enrollment in clinical trials [6]. It may therefore be appropriate for physicians to diagnose severe sepsis more often than consensus criteria, particularly in children with a lower severity of illness who may need fewer adjunctive sepsis-related therapies. Physicians may also have been recognizing and treating children with sepsis earlier in their illness course, at a point when they may not yet have manifested the physiologic and laboratory derangements required by consensus criteria. The loss of a statistical difference in PICU mortality between patients identified by physician diagnosis alone and those identified by both definitions after correcting for severity of illness is consistent with these suppositions. A lower threshold for diagnosing severe sepsis in clinical practice likely accounts for the generally better outcome metrics identified in epidemiologic studies using administrative databases [1, 2, 5] than has been reported in clinical trials [20, 27-29]. Our study therefore suggests caution when extrapolating results from epidemiologic, observational, and interventional studies to this less severely ill subgroup of patients who are diagnosed on the basis of physician impression and do not meet consensus criteria. Conversely, the absence of certain features, such as two or more systemic inflammatory response syndrome criteria [30, 31], hypotension only after 40 ml/kg of intravenous fluid, and laboratory derangements beyond arbitrary cutpoints (e.g., international normalized ratio >2), should not preclude the clinical diagnosis of severe sepsis and/or septic shock. A refined consensus definition that more closely matches the clinical definition and establishes a spectrum of risk concordant with outcome, similar to that of the recent at-risk, mild, moderate, and severe pediatric ARDS definitions [32], would benefit both research scientists and clinicians.
By quantifying the extent to which physician diagnosis and consensus criteria overlap, one can better understand the potential loss of efficacy as research findings are adopted at the bedside. Previous studies show that efficacious therapies in clinical trials are often extended to a broader patient population, with a more variable and perhaps even a distinct pathophysiology [14–17]. To our knowledge, this is the first multicenter, international study of the generalizability of consensus criteria for pediatric severe sepsis. Because only 69 % of patients with a physician’s diagnosis of severe sepsis met consensus criteria, it may not be appropriate to apply the results of a clinical trial to up to one-third of children treated for severe sepsis in a general PICU practice. Although a potential decrement from efficacy to effectiveness may not dissuade widespread implementation of a new therapy, enthusiasm could be altered if concerns over adverse effects, resource utilization, or costs were taken into consideration.
It is also noteworthy that nearly half of patients in the SPROUT study were identified as having severe sepsis by consensus criteria without corroboration by physician diagnosis. This likely reflects that both physician diagnosis and consensus criteria rely on relatively non-specific changes in physiology that are commonly found in critically ill children in general, not just in children with sepsis. Still, this observation highlights an opportunity to refine future iterations of consensus criteria and address variability in physician diagnosis to identify sepsis. Patients with preexisting neuromuscular disorders, such as cerebral palsy and epilepsy, were particularly likely to meet consensus criteria for severe sepsis despite an alternative clinical diagnosis. Many of these patients have dysautonomia or altered physiologic responses to illness that make it challenging to apply predefined rigid criteria. The higher rate of unknown primary site of infection suggests that consensus criteria may be less specific than physician diagnosis in identifying patients with a true infection. It is also possible that consensus criteria include PICU patients with a high severity of illness, namely those with shock and multiorgan system dysfunction caused by non-septic insults, who are commonly treated empirically for infection even if clinical suspicion is low. Alternatively, if physician diagnosis does not corroborate consensus criteria despite true presence of severe sepsis, there may be a higher rate of parental or clinician refusal to participate in research because the clinicians managing the patient may not agree on the diagnosis of concern. The incorporation of new biomarkers or novel microbiologic detection systems that improve early sensitivity and specificity for invasive infections into future revisions of the consensus criteria may improve alignment with physician diagnosis.
There are several limitations to this study. First, physician diagnosis and the application of consensus criteria to identify patients with severe sepsis could not be independently verified. The reasons why patients were not identified as having severe sepsis by one or both definitions were also not available. Although these concerns may have led to misclassification of some patients, it is unlikely that such a bias would have preferentially affected one group. Moreover, because we included only physicians practicing in a PICU setting, 89 % of whom were trained in pediatric critical care medicine, the level of agreement for other providers who commonly treat sepsis (e.g., emergency physicians) may differ from our results. A second limitation is that criteria used for physician diagnosis were not standardized. Although this may have increased variability in physician diagnosis across providers and sites, such an approach reflects that physicians often differ in their diagnostic approach. Third, the higher proportion of patients with available laboratory measures in the consensus criteria only and both definition groups may itself have increased the likelihood of identification by consensus criteria because, in the absence of available data, these measures were assumed to be within normal limits. Although it is more likely that sicker patients had directed laboratory testing performed than unsuspected organ dysfunction was discovered through routine laboratory testing, differential availability of laboratory results may have been a source of misclassification bias. Finally, because a “gold standard” does not exist, it is not possible to determine the degree to which either definition correctly identified pediatric patients with severe sepsis or compared the sensitivity and specificity of the two definitions.
Conclusions
Physician diagnosis of pediatric severe sepsis achieved only a moderate level of agreement with consensus criteria across this multicenter, international point prevalence study. The results of a research study based on current consensus criteria may not be generalizable to nearly one-third of pediatric patients diagnosed with severe sepsis in a PICU. Further research is needed to understand the extent to which the specificity of consensus criteria and variability in physician diagnosis may be contributing to this discordant identification of pediatric severe sepsis. Attempts to better align consensus definitions with clinical diagnosis by establishing a continuous spectrum of illness severity are needed.
Key messages
Although consensus criteria for pediatric sepsis were established to facilitate consistent enrollment across research studies, the extent to which these criteria reflect physician diagnosis of severe sepsis, which underlies external validity for pediatric sepsis research, is not known.
Of 6925 PICU patients screened at 128 PICUs in 26 countries, 706 patients were identified by physician diagnosis and/or consensus criteria as having severe sepsis.
Only 301 patients (42.6 %) were identified by both physician diagnosis and consensus criteria (κ 0.57 ± 0.02).
The 31 % of patients with physician-diagnosed severe sepsis who did not meet consensus criteria were younger, had a lower severity of illness, and a lower PICU mortality than those who met consensus criteria or both definitions.
The results of a research study based on consensus criteria may have limited generalizability to nearly one-third of PICU patients diagnosed with severe sepsis.
Acknowledgments
Financial support was provided by the Division of Critical Care and the Center for Pediatric Clinical Effectiveness at The Children’s Hospital of Philadelphia and University of Pennsylvania Perelman School of Medicine. SLW is also supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development grant K12HD047349 and National Institute of General Medical Sciences grant K23 GM110496. The study sponsors/funders had no role in the design and conduct of the study; the collection, management, analysis, or interpretation of the data; or the preparation, review, or approval of the manuscript. We thank the World Federation of Pediatric Intensive and Critical Care Societies for help in site recruitment. We thank the Australian and New Zealand Intensive Care Society for review of the study protocol and for their support in site recruitment within Australia and New Zealand. We are grateful to all local investigators at participating SPROUT study sites for their contributions to this study.
SPROUT study investigators
North America:Canada: P. Fontela (Montreal Children’s Hospital-McGill University Health Centre), M. Tucci, M. Dumistrascu (Sainte Justine Hospital), P. Skippen, G. Krahn (BC Children’s Hospital); Puerto Rico: E. Bezares (Centro Cardiovascular de Puerto Rico y el Caribe), G. Puig, A. Puig-Ramos (San Jorge Children’s Hospital), R. Garcia, M. Villar (University Pediatric Hospital); United States: M. Bigham, T. Polanski, S. Latifi, D. Giebner, H. Anthony (Akron Children’s Hospital), J. Hume, A. Galster, L. Linnerud (Amplatz Children’s Hospital), R. Sanders, G. Hefley (Arkansas Children’s Hospital), K. Madden (Boston Children’s Hospital), A. Thompson, S. Shein (Children’s Hospital of Pittsburgh), S. Gertz (Joseph M. Sanzari Children’s Hospital-Hackensack University Medical Center), Y. Han, T. Williams, A. Hughes-Schalk (Children’s Mercy Hospital), H. Chandler (Children’s Healthcare of Atlanta), A. Orioles, E. Zielinski, A. Doucette (Children’s Hospitals and Clinics of Minnesota), A. Orioles, E. Zielinski, A. Doucette (Children’s St. Paul Pediatric Hospital), C. Zebuhr, T. Wilson (Children’s Hospital Colorado), C. Dimitriades, J. Ascani, S. Layburn, S. Valley (Children’s Hospital, New Orleans), B. Markowitz, J. Terry, R. Morzov (Children’s Hospital Los Angeles), A. McInnes (Unterberg Children’s Hospital at Monmouth Medical Center), J. McArthur, K. Woods, K. Murkowski (Children’s Hospital of Wisconsin), M. Spaeder, M. Sharron (Children’s National Medical Center), D. Wheeler, E. Beckman, E. Frank, K. Howard (Cincinnati Children’s Hospital Medical Center), C. Carroll (Connecticut Children’s Medical Center), S. Nett, D. Jarvis (Dartmouth-Hitchcock Medical Center), V. Patel (Dayton Children’s Hospital), R. Higgerson, L. Christie (Dell Children’s Medical Center of Central Texas), K. Typpo, J. Deschenes (Diamond Children’s Medical Center), A. Kirby (Doernbecher Children’s Hospital), T. Uhl, K. Rehder, I. Cheifetz, S. Wrenn (Duke Children’s Hospital & Health Center), K. Kypuros (El Paso Children’s Hospital), K. Ackerman (Golisano Children’s Hospital), F. Maffei, G. Bloomquist (Janet Weis Children’s Hospital/Geisinger Health System), N. Rizkalla (Johns Hopkins Hospital), D. Kimura, S. Shah, C. Tigges (Le Bonheur Children’s Hospital), F. Su, C. Barlow (Lucile Packard Children’s Hospital), K. Michelson, K. Wolfe, D. Goodman, L. Campbell, L. Sorce (Ann & Robert H. Lurie Children’s Hospital of Chicago), K. Bysani, T. Monjure (Medical City Children’s Hospital-Dallas), M. Evans (Medical University of South Carolina), B. Totapally, M. Chegondi, C. Rodriguez (Miami Children’s Hospital), J. Frazier, L. Steele (Nationwide Children’s Hospital), S. Viteri, A. Costarino (Nemours/Alfred I. duPont Hospital for Children), N. Thomas, D. Spear (Penn State Hershey Medical Center), E. Hirshberg, J. Lilley (Primary Children’s Medical Center), C. Rowan, C. Rider (Riley Hospital for Children), J. Kane (Rush Children’s Hospital), J. Zimmerman, C. Greeley (Seattle Children’s Hospital), J. Lin, R. Jacobs (St. Louis Children’s Hospital), M. Parker, K. Culver (Stony Brook University), L. Loftis, N. Jaimon, M. Goldsworthy (Texas Children’s Hospital), J. Fitzgerald, S. Weiss, V. Nadkarni, J. Bush, M. Diliberto (The Children’s Hospital of Philadelphia), C. Alen, M. Gessouroun (Oklahoma University Medical Center), A. Sapru, T. Lang, M. Alkhouli (University of California San Francisco), S. Kamath, D. Friel, J. Daufeldt (University of Iowa), D. Hsing, C. Carlo, S. Pon (Weill Cornell Medical Center), J. Scimeme, A. Shaheen (Wolfson Children’s Hospital), A. Hassinger, H. Qiao (Women & Children’s Hospital of Buffalo), J. Giuliano, J. Tala (Yale-New Haven Children’s Hospital).
South America:Argentina: D. Vinciguerra, A. Fernandez (Hospital Carlos G. Durand); Colombia: R. Carrero (Clínica Infantil Colsubsidio), P. Hoyos (Hospital de San José), J. Jaramillo, A. Posada (Hospital General de Medellín), L. Izquiierdo (Central Military Hospital), B.E. Piñeres Olave, J. Donado (Hospital Pablo Tobón Uribe); Chile: R. Dalmazzo, S. Rendich (Clínica Las Condes), L. Palma, M. Lapadula (Clínica Santa María), C. Acuna (Hospital Luis Calvo Mackenna), P. Cruces (Hospital Padre Hurtado).
Europe:Belgium: S. Clement De Clety, M. Dujardin, C. Berghe, S. Renard (St. Luc University Hospital); Czech Republic: J. Zurek (Masaryk University); Germany: H. Steinherr (Klinikum Augsburg); Greece: K. Mougkou (Aghia Sophia Children’s Hospital), E. Critselis, K. Mougkou (P. & A. Kyriakou Children’s Hospital); Italy: M. Di Nardo, S. Picardo, F. Tortora (Bambino Gesu Area Rossa); E. Rossetti (Bambino Gesu Children’s Hospital); T. Fragasso, P. Cogo, R. Netto (Bambino Gesu Pediatrico); Lithuania: A. Dagys, V. Gurskis, R. Kevalas (Lithuanian University of Health Sciences); The Netherlands: C. Neeleman, J. Lemson, C. Luijten (Radboud University Medical Centre); Poland: K. Wojciech, I. Pagowska-Klimek (Polish Mother Memorial Hospital), M. Szczepanska, J. Karpe (Stanisława Szyszko Śląskiego University); Portugal: P. Nunes, H. Almeida (Hospital Prof Doutor Fernando Fonseca), J. Rios, M. Vieira (Centro Hospitalar Lisboa Norte); Spain: P. Revilla (Children’s Hospital Miguel Servet), J. Urbano, J. Lopez-Herce, A. Bustinza (Hospital General Universitario Gregorio Marañón), A. Cuesta, S. Hofheinz (Hospital Universitario 12 de Octubre), A. Rodriguez-Nunez (Hospital Clínico Universitario), S. Sanagustin, E. Gonzalez (Hospital de la Santa Creu i Sant Pau), M. Riaza, R. Piaya (Hospital Universitario de Madrid), P. Soler (Hospital Regional Universitario Carlos Haya Hospital Materno-Infantil), E. Esteban (Hospital Sant Joan de Déu Barcelona), J. Laraudogoitia, C. Monge (Hospital Universitario Donostia), V. Herrera, J. Granados (Hospital Universitario Salamanca), C. Gonzalez (Hospital Universitario Virgen de la Arrixaca); Turkey: T. Koroglu, E. Ozcelik (Dokuz Eylül University); United Kingdom: P. Baines (Alder Hey Children’s Hospital), A. Plunkett (Birmingham Children’s Hospital), P. Davis, S. George (Bristol Royal Hospital for Children), S. Tibby, J. Harris (Evelina Children’s Hospital), R. Agbeko, R. Lampitt (Great North Children’s Hospital–Newcastle), J. Bierley, M. Peters, A. Jones, T. Dominguez, T. Thiruchelvam (Great Ormond Street Hospital), A. Deep, L. Ridley, W. Bowen (King’s College Hospital), R. Levin, I. Macleod (Royal Hospital for Sick Children), M. Gray, N. Hemat (St George’s Hospital), J. Alexander, S. Ali (University Hospital of North Staffordshire NHS Trust), J. Pappachan, J. McCorkell (University Hospitals of North Midlands NHS Trust), P. Fortune, M. MacDonald, P. Hudnott (Royal Manchester Children’s Hospital).
Asia-Pacific:Australia: A. Schibler, A. Fernandez (Mater Children’s Hospital), S. Erickson (Princess Margaret Hospital for Children), J. Millar, C. Delzoppo (Royal Children’s Melbourne), G. Williams, M. Morritt (Sydney Children’s Hospital), J. McEneiry, D. Long, T. Dorofaeff, M. Coulthard (Royal Children’s Hospital Brisbane), N. Watts, M. Morritt (Children’s Hospital at Westmead); China: Q. Suyun (Beijing Children’s Hospital); India: S. Singhi, K. Nallasamy (Advanced Pediatrics Centre, Postgraduate Institute of Medical Education and Research - Advanced Pediatric Centre), R. Lodha (All India Institute of Medical Sciences); Japan: N. Shime, Y. Tabata (Kyoto Prefectural University of Medicine), O. Saito, T. Ikeyama (Tokyo Metropolitan Children’s Medical Center), T. Kawasaki (Shizuoka Children’s Hospital); Malaysia: L. Lum, A. Abidin, S. Kee (University Malaya Medical Centre), S. Tang, R. Jalil (UKM Medical Centre); New Zealand: J. Beca, C. Sherring, T. Bushell (Starship Children’s Health); Singapore: Y. Guan, L. Yao (KK Women’s and Children’s Hospital), K. Lin, J. Ong (National University Hospital).
Africa:South Africa: A. Salloo, L. Doedens, L. Mathivha (Chris Hani Baragwanath Hospital), G. Reubenson, S. Moaisi (Rahima Moosa Mother and Child Hospital), A. Pentz, R. Green (Steve Biko Academic Hospital).
Abbreviations
- ALT
alanine aminotransferase
- ARDS
acute respiratory distress syndrome
- BUN
blood urea nitrogen
- ECMO
extracorporeal membrane oxygenation
- G/GM-CSF
granulocyte/granulocyte macrophage colony-stimulating factor
- INR
international normalized ratio
- IQR
interquartile range
- IVIG
intravenous immunoglobulin
- MODS
multiorgan dysfunction syndrome
- NPMODS
new or progressive multiorgan dysfunction syndrome
- OR
odds ratio
- PaO2/FiO2
ratio of partial pressure of oxygen to fraction of inspired oxygen
- PELOD
Pediatric Logistic Organ Dysfunction score
- PICU
pediatric intensive care unit
- PIM
Pediatric Index of Mortality score
- POPC
Pediatric Overall Performance Category
- REDCap
Research Electronic Data Capture
- RRT
renal replacement therapy
- ScvO2
central venous oxygen saturation
- SPROUT
Sepsis PRevalence, OUtcomes, and Therapies study
- WBC
white blood cells
Additional file
Approving ethical bodies at each study site. (DOCX 16 kb)
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SLW, JCF, NJT, and VMN conceived the study. SLW, JCF, JLB, NJT, and VMN participated in the design of the study. SLW, JCF, FAM, JMK, ARN, DDH, DF, SYK, JLB, and NJT participated in data collection. SLW, JCF, JAR, NJT, and VMN performed the statistical analyses. SLW, JCF, NJT, and VMN helped to draft the manuscript. SLW, JCF, NJT, and VMN had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Contributor Information
Scott L. Weiss, Phone: (215) 590-2356, weisss@email.chop.edu
Julie C. Fitzgerald, fitzgeraldj@email.chop.edu
Frank A. Maffei, Email: famaffei@geisinger.edu
Jason M. Kane, Email: jmkanemd@gmail.com
Antonio Rodriguez-Nunez, Email: antonio.rodriguez.nunez@sergas.es.
Deyin D. Hsing, Email: ddh9002@med.cornell.edu
Deborah Franzon, Email: dfranzon@stanford.edu.
Sze Ying Kee, Email: sy_kee2004@icloud.com.
Jenny L. Bush, bushj1@email.chop.edu
Jason A. Roy, Email: jaroy@mail.med.upenn.edu
Neal J. Thomas, Email: nthomas@hmc.psu.edu
Vinay M. Nadkarni, nadkarni@email.chop.edu
References
- 1.Hartman ME, Linde-Zwirble WT, Angus DC, Watson RS. Trends in the epidemiology of pediatric severe sepsis. Pediatr Crit Care Med. 2013;14:868–693. doi: 10.1097/PCC.0b013e3182917fad. [DOI] [PubMed] [Google Scholar]
- 2.Ruth A, McCracken CE, Fortenberry JD, Hall M, Simon HK, Hebbar KB. Pediatric severe sepsis: current trends and outcomes from the pediatric health information systems database. Pediatr Crit Care Med. 2014;15:828–38. doi: 10.1097/PCC.0000000000000254. [DOI] [PubMed] [Google Scholar]
- 3.Jaramillo-Bustamante JC, Marín-Agudelo A, Fernández-Laverde M, Bareño-Silva J. Epidemiology of sepsis in pediatric intensive care units: first Colombian multicenter study. Pediatr Crit Care Med. 2012;13:501–8. doi: 10.1097/PCC.0b013e31823c980f. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Sun B, Yue H, Lin X, Li B, Yang X, et al. An epidemiologic survey of pediatric sepsis in regional hospitals in China. Pediatr Crit Care Med. 2014;15:814–20. doi: 10.1097/PCC.0000000000000247. [DOI] [PubMed] [Google Scholar]
- 5.Balamuth F, Weiss SL, Neuman MI, Scott H, Brady PW, Paul R, et al. Pediatric severe sepsis in U.S. children’s hospitals. Pediatr Crit Care Med. 2014;15:798–805. doi: 10.1097/PCC.0000000000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldstein B, Giroir B, Randolph A. International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6:2–8. doi: 10.1097/01.PCC.0000149131.72248.E6. [DOI] [PubMed] [Google Scholar]
- 7.Opal SM, Dellinger RP, Vincent JL, Masur H, Angus DC. The next generation of sepsis clinical trial designs: what is next after the demise of recombinant human activated protein C? Crit Care Med. 2014;42:1714–21. doi: 10.1097/CCM.0000000000000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brierley J, Carcillo JA, Choong K, Cornell T, Decaen A, Deymann A, et al. Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med. 2009;37:666–88. doi: 10.1097/CCM.0b013e31819323c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iwashyna TJ, Odden A, Rohde J, Bonham C, Kuhn L, Malani P, et al. Identifying patients with severe sepsis using administrative claims: patient-level validation of the Angus implementation of the international consensus conference definition of severe sepsis. Med Care. 2012;52:e39–43. doi: 10.1097/MLR.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiss SL, Parker B, Bullock ME, Swartz S, Price C, Wainwright MS, et al. Defining pediatric sepsis by different criteria: discrepancies in populations and implications for clinical practice. Pediatr Crit Care Med. 2012;13:e219–26. doi: 10.1097/PCC.0b013e31823c98da. [DOI] [PubMed] [Google Scholar]
- 11.Dougherty D, Conway PH. The “3T’s” road map to transform US health care: the “how” of high-quality care. JAMA. 2008;299:2319–21. doi: 10.1001/jama.299.19.2319. [DOI] [PubMed] [Google Scholar]
- 12.Rothwell PM. External validity of randomised controlled trials: “to whom do the results of this trial apply?”. Lancet. 2005;365:82–93. doi: 10.1016/S0140-6736(04)17670-8. [DOI] [PubMed] [Google Scholar]
- 13.Partridge SR, Juan SJ, McGeechan K, Bauman A, Allman-Farinelli M. Poor quality of external validity reporting limits generalizability of overweight and/or obesity lifestyle prevention interventions in young adults: a systematic review. Obes Rev. 2014;16:13–31. doi: 10.1111/obr.12233. [DOI] [PubMed] [Google Scholar]
- 14.Charlson ME, Horwitz RI. Applying results of randomised trials to clinical practice: impact of losses before randomisation. Br Med J (Clin Res Ed). 1984;289:1281–4. doi: 10.1136/bmj.289.6454.1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hagg L, Johansson C, Jansson JH, Johansson L. External validity of the ARISTOTLE trial in real-life atrial fibrillation patients. Cardiovasc Ther. 2014;32:214–8. doi: 10.1111/1755-5922.12087. [DOI] [PubMed] [Google Scholar]
- 16.Lee S, Monz BU, Clemens A, Brueckmann M, Lip GYH. Representativeness of the dabigatran, apixaban and rivaroxaban clinical trial populations to real-world atrial fibrillation patients in the United Kingdom: a cross-sectional analysis using the General Practice Research Database. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-001768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maasland L, van Oostenbrugge RJ, Franke CF, Scholte Op Reimer WJ, Koudstaal PJ, Dippel DW. Patients enrolled in large randomized clinical trials of antiplatelet treatment for prevention after transient ischemic attack or ischemic stroke are not representative of patients in clinical practice: the Netherlands Stroke Survey. Stroke. 2009;40:2662–8. doi: 10.1161/STROKEAHA.109.551812. [DOI] [PubMed] [Google Scholar]
- 18.Weiss SL, Fitzgerald JC, Pappachan J, Wheeler D, Jaramillo-Bustamante JC, Salloo A, et al. Global epidemiology of pediatric severe sepsis: the Sepsis PRevalence, OUtcomes, and Therapies study. Am J Respir Crit Care Med. 2015;191:1147–57. doi: 10.1164/rccm.201412-2323OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lacroix J, Hebert PC, Hutchison JS, Hume HA, Tucci M, Ducruet T, et al. Transfusion strategies for patients in pediatric intensive care units. N Engl J Med. 2007;356:1609–19. doi: 10.1056/NEJMoa066240. [DOI] [PubMed] [Google Scholar]
- 20.Karam O, Tucci M, Ducruet T, Hume HA, Lacroix J, Gauvin F. Red blood cell transfusion thresholds in pediatric patients with sepsis. Pediatr Crit Care Med. 2011;12:512–8. doi: 10.1097/PCC.0b013e3181fe344b. [DOI] [PubMed] [Google Scholar]
- 21.Proulx F, Fayon M, Farrell CA, Lacroix J, Gauthier M. Epidemiology of sepsis and multiple organ dysfunction syndrome in children. Chest. 1996;109:1033–7. doi: 10.1378/chest.109.4.1033. [DOI] [PubMed] [Google Scholar]
- 22.Straney L, Clements A, Parslow RC, Pearson G, Shann F, Alexander J, et al. Paediatric index of mortality 3: an updated model for predicting mortality in pediatric intensive care. Pediatr Crit Care Med. 2013;14:673–81. doi: 10.1097/PCC.0b013e31829760cf. [DOI] [PubMed] [Google Scholar]
- 23.Leteurtre S, Martinot A, Duhamel A, Proulx F, Grandbastien B, Cotting J, et al. Validation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre study. Lancet. 2003;362:192–7. doi: 10.1016/S0140-6736(03)13908-6. [DOI] [PubMed] [Google Scholar]
- 24.Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. 1992;121:68–74. doi: 10.1016/S0022-3476(05)82544-2. [DOI] [PubMed] [Google Scholar]
- 25.Farris RW, Weiss NS, Zimmerman JJ. Functional outcomes in pediatric severe sepsis: further analysis of the researching severe sepsis and organ dysfunction in children: a global perspective trial. Pediatr Crit Care Med. 2013;14:835–42. doi: 10.1097/PCC.0b013e3182a551c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choong K, Bohn D, Fraser DD, Gaboury I, Hutchison JS, Joffe AR, et al. Vasopressin in pediatric vasodilatory shock: a multicenter randomized controlled trial. Am J Respir Crit Care Med. 2009;180:632–9. doi: 10.1164/rccm.200902-0221OC. [DOI] [PubMed] [Google Scholar]
- 28.Nadel S, Goldstein B, Williams MD, Dalton H, Peters M, Macias WL, et al. Drotrecogin alfa (activated) in children with severe sepsis: a multicentre phase III randomised controlled trial. Lancet. 2007;369:836–43. [DOI] [PubMed]
- 29.de Oliveira CF, de Oliveira DSF, Gottschald AFC, Moura JDG, Costa GA, Ventura AC, et al. ACCM/PALS haemodynamic support guidelines for paediatric septic shock: an outcomes comparison with and without monitoring central venous oxygen saturation. Intensive Care Med. 2008;34:1065–75. doi: 10.1007/s00134-008-1085-9. [DOI] [PubMed] [Google Scholar]
- 30.Kaukonen KM, Bailey M, Pilcher D, Cooper DJ, Bellomo R. Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med. 2015;372:1629–38. [DOI] [PubMed]
- 31.Scott HF, Deakyne SJ, Woods JM, Bajaj L. The prevalence and diagnostic utility of systemic inflammatory response syndrome vital signs in a pediatric emergency department. Acad Emerg Med. 2015;22:381–9. [DOI] [PubMed]
- 32.Pediatric Acute Lung Injury Consensus Conference Group Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015;16:428–39. doi: 10.1097/PCC.0000000000000350. [DOI] [PMC free article] [PubMed] [Google Scholar]


