Abstract
Objectives
This study examined (1) the relationship between ease of access to needed community-based services (ease of access) and educational services receipt and (2) variation in educational services receipt by sociodemographic and need factors among a nationally representative sample of children with autism spectrum disorder (ASD), developmental delay (DD), and/or intellectual disability (ID).
Methods
Data from the 2009–10 National Survey of Children with Special Health Care Needs were linked to the 2011 Survey of Pathways to Diagnosis and Services on a sample of 3,502 US children aged 6–17 years with ASD, DD, and/or ID. Descriptive statistics, chi-square tests, and multivariable logistic regression models were used to determine associations of educational services receipt with (1) ease of access and (2) sociodemographic and need factors.
Results
Among children with developmental conditions, nearly half (49.7%) lacked easy access to services and 16.9% did not have an individualized education program (IEP). Among children with an IEP, those with ease of access were more likely to have an IEP that addressed parent concerns about the child’s development and education than those unable to easily access services (aOR: 2.77; 95% CI: 1.71–4.49). Need factors, including functional limitations status, care coordination need, developmental condition type, and early intervention receipt, were significantly associated with educational services receipt.
Conclusions
Cross-systems initiatives facilitating service access remain important to ensuring the developmental needs of children with ASD, DD, and/or ID are met. Increased inter-professional collaboration promoting quality educational services receipt for children diagnosed with developmental conditions may further reduce disparities.
Keywords: children with special health care needs, developmental conditions, ease of access, individualized education program, school-based therapy
Introduction
The prevalence of developmental conditions,1 including autism spectrum disorder (ASD),2,3 developmental delay (DD),1 and intellectual disability (ID),1 among US children has risen markedly. Children with developmental conditions more commonly experience functional impairment,4 poor academic achievement,5,6 and greater healthcare needs than other children.7 They are also prone to experience unmet healthcare needs,8 poor quality of care,9 and family financial and employment impacts,10 even compared to other children with special health care needs (CSHCN).11,12,13,14
Children are often diagnosed with developmental conditions in early childhood.3,15 Under the Individuals with Disabilities Education Act (IDEA), US children with qualifying disabilities (e.g., ASD, DD, ID) whose educational performance is negatively impacted by their disability are eligible to receive an Individualized Education Program (IEP).16 An IEP can help children with disabilities receive specialized services, instruction, and/or accommodations at school to meet their needs thereby promoting functioning, academic achievement, and health.17
Although most children with ASD, DD, and/or ID18 meet IEP eligibility criteria, disparities in IEP receipt7,19,20 and quality21—particularly among children with ASD—persist. Recent research suggests certain sociodemographic and need factors (e.g., race/ethnicity, maternal education level, care coordination need) may also contribute to disparities in IEP receipt among children with ASD19 and other disabilities.17 Yet, little is known about factors contributing to disparities in IEP receipt among children with developmental conditions more broadly, or if additional factors such as parent experiences accessing needed community-based services for children influence educational services receipt.
Overarching frameworks to promote health among CSHCN,22,23 including those with developmental conditions, and policy statements from the pediatric medical community24,25 recommend all needed services—delivered in healthcare or school-based settings—should be easily accessed and received via interconnected, community-based systems of care. However, little evidence documents linkages between ease of access to needed community-based services (ease of access) and educational services receipt among children with ASD, DD, and/or ID (children with developmental conditions).26 Rather, research to date on children with developmental conditions has been focused either on health services27,28 or educational services access.17,19
It is important to elucidate this relationship given developmental conditions in early childhood are common and access to community-based health services generally—from basic medical and dental care to more specialized medical and early intervention (EI) services—may predict how likely children are to subsequently receive health promoting services in school settings. Increased evidence in this area may help policymakers and practitioners improve service access and receipt across historically separated community, medical, and educational systems for children with developmental conditions. This study therefore examined (1) the relationship between ease of access and educational services receipt and (2) variation in educational services receipt by sociodemographic and need factors among a nationally representative sample of school-aged children with developmental conditions.
Methods
Study Design and Data Sources
This was a secondary analysis of publicly available data linked from the 2009–10 National Survey of Children with Special Health Care Needs (NS-CSHCN)29 to the 2011 Survey of Pathways to Diagnosis and Services (Pathways).30 Pathways was a follow-up survey of CSHCN aged 6–17 years ever diagnosed with ASD, DD, or ID by a doctor or other healthcare provider in the 2009–10 NS-CSHCN according to a parent or other caregiver (parent). The same parent reported all data on the child for each survey after informed consent was obtained. The 2009–10 NS-CSHCN had a 25.5% response rate,29 and Pathways had a weighted completion rate of 62%.30 Pathways was only administered in English. Detailed survey methodology has been previously documented.29,30
Sample
The study sample included 3,502 US children aged 6–17 years currently with ASD, DD, and/or ID and enrolled in school. Given the study’s focus, 530 children were excluded because the parent indicated the child did not currently have ASD, DD, or ID and/or was not enrolled in school when Pathways was administered. Mutually exclusive developmental condition subgroups were defined as (1) DD only (DD), (2) ASD with or without ID and/or DD (ASD), and (3) ID with or without DD (ID). Since children with ASD or ID commonly experience comorbid conditions, including DD,8,9 we were unable to stratify children with ASD or ID alone due to sample size constraints.
Measures
Three binary educational services receipt indicators from Pathways were used as dependent variables: (1) if the child had an IEP (“does [your child] have a written intervention plan called an Individualized Education Plan or IEP?”); (2) if the child’s IEP addressed parent concerns (“does [your child’s] IEP address all of your concerns about [his/her] development and education?”); and (3) if the child currently used on a regular basis ≥1 of four school-based therapies (occupational therapy, physical therapy, social skills training, speech or language therapy) to meet his/her developmental needs. The central tendency of the number of school-based therapies children in the study sample received (mean=1.401.31) was used to define the ≥1 cut-off in addition to wanting to determine factors associated with the receipt of any school-based therapy versus none. The second educational services receipt measure was only assessed among children with an IEP because of the survey’s skip pattern, and the third educational receipt measure was only assessed among children with an IEP to reduce selection bias given most (95.2%) of children who received ≥1 school-based therapy had an IEP.
The main independent variable was an ease of access composite measure from the 2009–10 NS-CSHCN. It is one of six age-relevant core outcomes in the Federal Maternal and Child Health Bureau’s System of Care for CSHCN framework.22 The measure includes one ordinal item about how often the parent was frustrated accessing “all the types of services children may need or use” in home, school, and health care settings. Examples of services included medical care, specialized therapies, counseling, medical equipment, special education, and early intervention (EI). This item was selected because we felt it best represented families’ overall ability to access services in their community. The item was assessed for the past 12-months, as were six binary items about the following difficulties accessing needed services: child ineligible for services, services unavailable in the family’s area, child put on a waiting list or parent experienced other problems getting appointments, issues related to costs, trouble getting needed information, and any other difficulties. If the parent never or sometimes (versus usually or always) was frustrated getting services for the child and did not experience any of the six difficulties accessing services for the child, then those children were considered to have easily accessed services.
To reduce confounding in the associations related to the ease of access measure’s inclusion of educational services the child may have needed, an additional binary measure from the 2009–10 NS-CSHCN of whether children “receive[d] services from a program called Special Education Services” was included in multivariable analyses. Other covariates used to characterize the study sample and controlled for in multivariable analyses were child age, sex, race/ethnicity, household income relative to federal poverty level (FPL),31 insurance type, highest parent education level, region, family structure, school type, care coordination need, EI receipt, and functional limitations status. These factors have been theorized32 with health services access and are associated with educational services receipt among children with developmental conditions.7,8,19
Statistical Analyses
Descriptive statistics, including weighted percentages and 95% confidence intervals, were initially computed. Chi-square tests were used to determine differences in the sociodemographic and need characteristics of children by developmental condition, as well as differences in educational services receipt according to ease of access. Multivariable logistic regression models controlling for special education services receipt in 2009–10 and sociodemographic and need factors were fitted to determine associations of ease of access with each educational services receipt indicator among children with developmental conditions overall and by developmental condition. Variance inflation factors computed were <2 suggesting multicollinearity did not substantially affect model estimates. The Holm method, a step-down multiple test procedure, was used to control the family-wise error rate of the multiple regression models.33 All analyses were weighted to account for the complex survey sampling design and performed in Stata 13.1 (College Station, Texas).
Results
Sample Characteristics
The study sample represented an estimated 1,794,524 US children aged 6–17 years currently with ASD, DD, and/or ID and enrolled in school. Most children were male, white, had two biological or adoptive parents, had a parent with >high school education, were privately insured, were enrolled in public school, experienced functional limitations, did not need care coordination, and did not receive EI (Table 1). More children with ID were older, had functional limitations, and received EI compared to the rest of the sample. Children with ASD were more likely than the rest of the sample to be male, white, had a household income >FPL, were privately insured, had two biological or adoptive parents, and did not need care coordination. Children with DD were more likely than the rest of the sample to have had a household income <FPL, been uninsured or publicly insured, had a parent with ≤high school education, not had functional limitations, and not received EI.
Table 1.
Sociodemographic and Need Characteristicsa of US Children Aged 6–17 Years with ASD, DD, and/or ID
| Overall (n = 3,502) |
Developmental Delay (n = 1,434) |
Autism Spectrum Disorder (n = 1,416) |
Intellectual Disability (n = 652) |
DD vs. ASD/ID P value |
ASD vs.DD/ID P value |
ID vs. DD/ASD P value |
|
|---|---|---|---|---|---|---|---|
| Weighted percentageb | 100.0% | 46.5% | 36.3% | 17.2% | |||
| Estimated number | 1,794,524 | 834,591 | 650,891 | 309,042 | |||
| Sociodemographic Factors | |||||||
| Age, y | |||||||
| Elementary, 6–11 (n = 1,718) | 50.7% | 50.6% | 54.7% | 42.3% | 0.96 | 0.046 | 0.046 |
| Middle/High School, 12–17 (n = 1,784) | 49.4% | 49.4% | 45.3% | 57.7% | |||
| Gender | |||||||
| Male (n = 2,426) | 69.9% | 67.3% | 82.1% | 51.1% | 0.10 | < .001 | < .001 |
| Female (n = 1,073) | 30.1% | 32.7% | 17.9% | 48.9% | |||
| Race/ethnicity | |||||||
| Hispanic (n = 310) | 13.3% | 14.2% | 13.1% | 11.1% | 0.08 | 0.038 | 0.42 |
| White, NH (n = 2,507) | 62.4% | 60.8% | 66.3% | 58.1% | |||
| Black, NH (n = 301) | 15.5% | 18.2% | 10.6% | 18.4% | |||
| Other, NH (n = 353) | 9.0% | 6.8% | 10.1% | 12.5% | |||
| Household income | |||||||
| 0%–99% FPL (n = 629) | 25.6% | 31.1% | 16.8% | 29.4% | < .001 | < .001 | 0.51 |
| 100%–199% FPL (n = 724) | 21.6% | 23.4% | 20.6% | 18.8% | |||
| 200%–399% FPL (n = 1,124) | 28.9% | 25.2% | 32.8% | 30.3% | |||
| ≥400% FPL (n = 1,025) | 24.0% | 20.3% | 29.8% | 21.5% | |||
| Health insurance type | |||||||
| Any private (n = 2,132) | 53.9% | 45.5% | 66.3% | 50.3% | < .001 | < .001 | 0.37 |
| Public only or uninsured (n = 1,260) | 46.1% | 54.5% | 33.7% | 49.8% | |||
| Census region | |||||||
| Northeast (n = 656) | 19.8% | 18.8% | 21.4% | 19.4% | 0.74 | 0.79 | 0.63 |
| Midwest (n = 804) | 24.6% | 25.2% | 24.6% | 22.9% | |||
| South (n = 1,033) | 34.6% | 35.9% | 33.8% | 32.7% | |||
| West (n = 1,009) | 21.1% | 20.2% | 20.3% | 25.0% | |||
| Family structure | |||||||
| 2 Biological/adoptive (n = 2,146) | 52.4% | 46.9% | 60.6% | 50.2% | 0.009 | 0.001 | 0.38 |
| Single mother (n = 671) | 27.5% | 29.7% | 22.5% | 32.2% | |||
| Other (n = 665) | 20.1% | 23.4% | 17.0% | 17.6% | |||
| Highest parental education level | |||||||
| ≤High school (n = 696) | 32.3% | 39.2% | 23.3% | 32.6% | < .001 | < .001 | 0.94 |
| >High school (n = 2,806) | 67.7% | 60.8% | 76.7% | 67.4% | |||
| School Type | |||||||
| Public (n = 3,037) | 88.1% | 88.8% | 86.8% | 89.0% | 0.49 | 0.28 | 0.63 |
| Private or home schooled (n = 465) | 11.9% | 11.2% | 13.2% | 11.0% | |||
| Need Factors | |||||||
| Functional limitations status | |||||||
| No (n = 1,517) | 43.9% | 57.6% | 35.4% | 25.0% | < .001 | < .001 | < .001 |
| Yes (n = 1,985) | 56.1% | 42.4% | 64.6% | 75.0% | |||
| Care coordination need | |||||||
| Needed care coordination (n = 1,038) | 31.6% | 25.8% | 38.0% | 33.7% | 0.001 | 0.001 | 0.62 |
| No care coordination need (n = 2,443) | 68.5% | 74.2% | 62.0% | 66.3% | |||
| Early intervention receipt | |||||||
| EI receipt (n = 1,298) | 40.5% | 29.7% | 44.5% | 61.2% | < .001 | 0.06 | < .001 |
| No EI (n = 1,954) | 59.5% | 70.3% | 55.5% | 38.8% |
Abbreviations: ASD, autism spectrum disorder; DD, developmental delay; EI, early intervention; FPL, federal poverty level; ID, intellectual disability; NH, non-Hispanic.
Weighted Pearson χ2 tests compare the distributions of each factor between each designated developmental condition subgroup and the other two developmental condition subgroups, combined.
All column percentages do not sum to 100 due to rounding.
Source: 2011 Survey of Pathways to Diagnosis and Services
Ease of Access and Educational Services Receipt
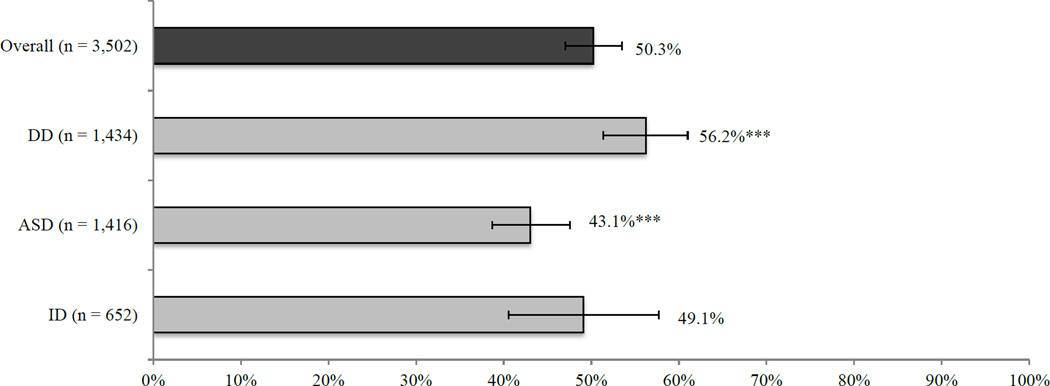
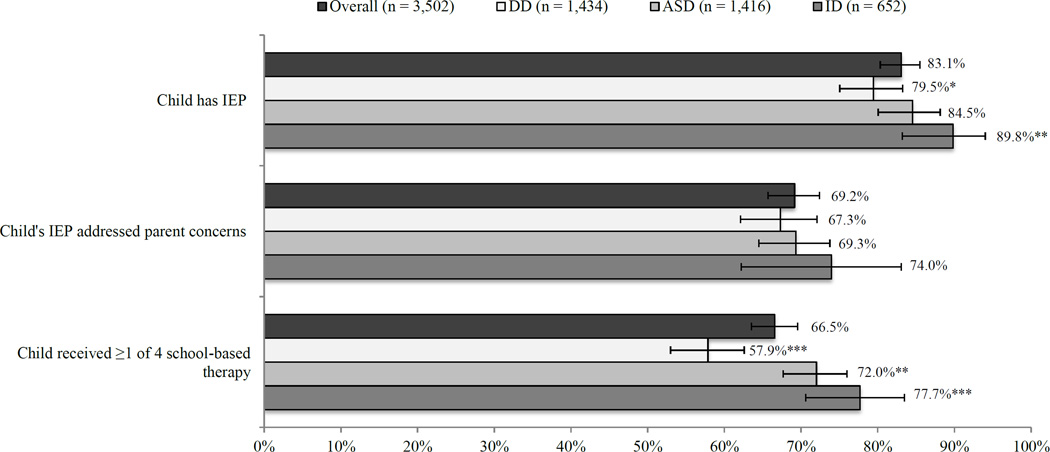
Both ease of access and educational services receipt were lacking among children with developmental conditions, with significant variation by condition (Figures 1 & 2). Children with ASD were less likely than the rest of the sample to have easily accessed services, while children with DD were more likely than the rest of the sample to have easily accessed services. Children with ID were more likely than the rest of the sample to have had an IEP and to have received ≥1 school-based therapy, and children with ASD were also more likely than the rest of the sample to have received ≥1 school-based therapy. By contrast, children with DD were less likely than the rest of the sample to have had an IEP or to have received ≥1 school-based therapy.
Figure 1.
Weighted Percentage and 95% Confidence Interval of US Children Aged 6–17 Years Who Were Able to Easily Access Needed Community-Based Services, Overall and by Developmental Condition
***Indicates the proportion was significantly different from the proportion for the rest of the sample at the P< .001 level.
Figure 2.
Weighted Percentages with 95% Confidence Intervals of Educational Services Receipta
Among US Children Aged 6–17 Years, Overall and by Developmental Condition
***Indicates the proportion was significantly different from the proportion for the rest of the sample at the P < .001 level, **P < .01 level, or *P < .05 level.
aThe denominators for measures of having an IEP that addressed parent concerns about the child's development and education as well as receipt of ≥1 school-based therapy include all children in the study sample in order to show the proportion of children who could have potentially received such services regardless of whether they had an IEP.
Source: 2011 Survey of Pathways to Diagnosis and Services
Ease of access was neither associated with receipt of an IEP nor ≥1 school-based therapy among children with developmental conditions (Table 2). Developmental condition type did not significantly modify associations between ease of access and any of the educational services receipt indicators. However, among children with an IEP, those whose parents easily accessed services were more likely to have an IEP that addressed parent concerns than children whose parents were unable to easily access services, even after adjusting for covariates. Results from stratified analyses suggest this finding was most pronounced for children with ASD.
Table 2.
Educational Services Receipt According to Ease of Service Access Among US Children Aged 6–17 Years with ASD, DD, and/or ID: Weighted Percentages, Adjusted Odds Ratiosa (95% CIs), and P valuesb
| Overall (n = 3,502) | ||||||
| IEP (n = 3,318) |
IEP addresses parent concerns (n = 2,789) |
≥1 school-based therapy (n = 2,684) |
||||
| % | aOR | % | aOR | % | aOR | |
| Able to easily access services | 83.5 (79.5–86.9) | 0.92 (0.55–1.55) | 91.8 (86.9–94.9) | 2.77 (1.71–4.49) | 77.3 (73.6–80.7) | 1.27 (0.86–1.86) |
| Unable to easily access services | 82.4 (78.5–85.8) | Referent | 76.3 (70.5–81.2) | Referent | 78.3 (74.2–81.8) | Referent |
| P value | 0.68 | 0.76 | < .001 | < .001* | 0.72 | 0.22 |
| Children with DD (n = 1,434) | ||||||
| IEP (n = 1,368) |
IEP addresses parent concerns (n = 1,053) |
≥1 school-based therapy (n = 1,003) |
||||
| % | aOR | % | aOR | % | aOR | |
| Able to easily access services | 82.8 (76.5–87.6) | 1.47 (0.77–2.82) | 90.4 (80.6–95.6) | 2.86 (1.39–5.91) | 70.9 (64.3–76.7) | 0.95 (0.56–1.61) |
| Unable to easily access services | 75.0 (68.5–80.6) | Referent | 78.4 (71.0–84.3) | Referent | 68.2 (60.9–74.7) | Referent |
| P value | 0.06 | 0.25 | 0.016 | 0.004NS | 0.57 | 0.84 |
| Children with ASD (n = 1,416) | ||||||
| IEP (n = 1,335) |
IEP addresses parent concerns (n = 1,160) |
≥1 school-based therapy (n = 1,124) |
||||
| % | aOR | % | aOR | % | aOR | |
| Able to easily access services | 82.3 (75.7–87.4) | 0.39 (0.14–1.10) | 93.6 (90.1–95.8) | 4.83 (2.37– 9.84) | 83.4 (78.3–87.5) | 1.86 (0.99–3.51) |
| Unable to easily access services | 85.9 (79.3–90.7) | Referent | 75.6 (69.6–80.8) | Referent | 83.5 (78.0–87.9) | Referent |
| P value | 0.38 | 0.08 | < .001 | < .001* | 0.97 | 0.06 |
| Children with ID (n = 652) | ||||||
| IEP (n = 615) |
IEP addresses parent concerns (n = 576) |
≥1 school-based therapy (n = 557) |
||||
| % | aOR | % | aOR | % | aOR | |
| Able to easily access services | 88.0 (77.0–94.1) | 1.69 (0.60–4.75) | 92.5 (86.6–96.0) | 1.93 (0.86–4.33) | 84.9 (77.1–90.3) | 1.12 (0.51–2.51) |
| Unable to easily access services | 91.9 (82.9–96.3) | Referent | 73.6 (49.5–88.8) | Referent | 85.6 (75.9–91.7) | Referent |
| P value | 0.47 | 0.32 | 0.08 | 0.11 | 0.89 | 0.77 |
Abbreviations: ASD, autism spectrum disorder; CI, confidence interval; DD, developmental delay; ID, intellectual disability; IEP, individualized education program.
Odds ratios were adjusted for child age, race/ethnicity, sex, household income level, census region, health insurance, family structure, school type, functional limitations status, care coordination need, and early intervention receipt. Models for estimating the adjusted odds of educational services receipt indicators in 2011 additionally controlled for special education services receipt during 2009/10. Models fitted for the sample overall were additionally adjusted for developmental condition type.
The Holm procedure was used to determine statistical significance given multiple comparisons: NS = not statistically significant at the < 0.05 level after applying the Holm procedure, and
= statistically significant at the < 0.05 level after applying the Holm procedure.
Source: 2011 Survey of Pathways to Diagnosis and Services
Educational Services Receipt by Sociodemographic and Need Factors
Certain sociodemographic and need factors were also associated with educational services receipt among children with developmental conditions (Table 3). Children with functional limitations had higher adjusted odds of IEP receipt than children without functional limitations. Among children with an IEP, those whose parents needed care coordination had lower adjusted odds of having an IEP that addressed parent concerns than those whose parents did not need for care coordination. Also among children with an IEP, those in elementary school (versus middle or high school), who had ASD or ID (versus DD), who had functional limitations (versus did not), and who received EI (versus did not) had higher adjusted odds of having received ≥1 school-based therapy.
Table 3.
Receipt of Educational Services Among US Children Aged 6–17 Years with ASD, DD, and/or ID, by Sociodemographic and Need Factors: Weighted Percentages, Adjusted Odds Ratios (95% CIs)a and P valuesb
| IEP (n = 3,051) |
IEP Addresses Parent Concerns (n = 2,571) |
≥1 School-Based Therapy (n = 2,486) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| % | aOR | P value | % | aOR | P value | % | aOR | P value | |
| Sociodemographic Factors | |||||||||
| Age, y | |||||||||
| Elementary, 6–11 | 83.0 | 1.26 (0.84–1.90) | 0.26 | 83.0 | 1.11 (0.68–1.81) | 0.69 | 86.4 | 3.85 (2.68–5.53) | < .001* |
| Middle or High School, 12–17 | 83.1 | Referent | 84.6 | Referent | 68.1 | Referent | |||
| Gender | |||||||||
| Male | 84.2 | 1.42 (0.92–2.19) | 0.11 | 82.7 | 0.78 (0.47–1.31) | 0.35 | 76.1 | 0.96 (0.62–1.47) | 0.84 |
| Female | 80.3 | Referent | 86.4 | Referent | 78.1 | Referent | |||
| Race/Ethnicity | |||||||||
| Hispanic | 91.2 | 2.92 (1.44–5.92) | 0.003NS | 77.4 | 0.66 (0.31–1.43) | 0.30 | 81.8 | 1.88 (0.95–3.71) | 0.07 |
| White, NH | 82.2 | Referent | 85.2 | Referent | 75.0 | Referent | |||
| Black, NH | 77.6 | 0.78 (0.38–1.59) | 0.49 | 90.4 | 1.48 (0.63–3.49) | 0.37 | 80.3 | 1.17 (0.68–2.04) | 0.57 |
| Other Race, NH | 86.2 | 0.61 (0.29–1.27) | 0.19 | 73.4 | 0.60 (0.29–1.25) | 0.17 | 85.0 | 1.47 (0.77–2.83) | 0.25 |
| Household income | |||||||||
| 0%–99% FPL | 80.1 | 0.51 (0.23–1.15) | 0.10 | 86.1 | 1.38 (0.60–3.20) | 0.45 | 79.2 | 0.93 (0.48–1.82) | 0.84 |
| 100%–199% FPL | 83.1 | 0.67 (0.35–1.25) | 0.21 | 87.1 | 1.72 (0.91–3.27) | 0.10 | 79.7 | 1.04 (0.58–1.87) | 0.89 |
| 200%–399% FPL | 84.9 | 1.02 (0.62–1.69) | 0.93 | 83.1 | 1.28 (0.76–2.14) | 0.36 | 78.4 | 1.20 (0.75–1.91) | 0.44 |
| ≥400% FPL | 83.8 | Referent | 79.4 | Referent | 73.0 | Referent | |||
| Health insurance type | |||||||||
| Any private insurance | 81.7 | Referent | 0.49 | 83.1 | Referent | 0.53 | 74.6 | Referent | 0.16 |
| Public insurance only | 84.8 | 1.26 (0.64–2.48) | 84.4 | 0.83 (0.46–1.50) | 81.7 | 1.44 (0.87–2.39) | |||
| Census region | |||||||||
| Northeast | 88.0 | Referent | 86.2 | Referent | 81.3 | Referent | |||
| Midwest | 81.5 | 0.63 (0.30–1.32) | 0.22 | 89.6 | 1.42 (0.72–2.83) | 0.31 | 78.8 | 1.02 (0.60–1.73) | 0.95 |
| South | 78.3 | 0.64 (0.32–1.25) | 0.19 | 85.6 | 1.02 (0.53–1.98) | 0.95 | 75.8 | 0.62 (0.38–1.00) | 0.049NS |
| West | 87.9 | 0.88 (0.40–1.96) | 0.76 | 72.6 | 0.60 (0.30–1.17) | 0.14 | 74.7 | 0.77 (0.42–1.40) | 0.39 |
| Family structure | |||||||||
| 2 Biological/adoptive parents | 85.1 | Referent | 83.2 | Referent | 77.0 | Referent | |||
| Single mother | 82.0 | 1.43 (0.84–2.41) | 0.19 | 81.3 | 0.89 (0.43–1.82) | 0.75 | 80.4 | 1.16 (0.74–1.82) | 0.51 |
| Other family structure | 79.9 | 1.13 (0.65–1.95) | 0.66 | 89.0 | 1.69 (0.82–3.48) | 0.15 | 74.8 | 0.97 (0.59–1.60) | 0.90 |
| Highest parental education | |||||||||
| ≤High school | 80.7 | 0.89 (0.51–1.58) | 0.70 | 89.1 | 1.39 (0.77–2.52) | 0.27 | 83.3 | 1.73 (1.06– 2.82) | 0.027NS |
| >High school | 84.1 | Referent | 81.3 | Referent | 75.1 | Referent | |||
| School Type | |||||||||
| Public school | 83.6 | Referent | 0.09 | 84.2 | Referent | 0.84 | 77.9 | Referent | 0.71 |
| Private school or home schooled | 76.7 | 0.62 (0.36–1.08) | 78.4 | 0.92 (0.41–2.04) | 72.4 | 1.11 (0.64–1.93) | |||
| Need Factors | |||||||||
| Developmental condition | |||||||||
| DD | 79.5 | Referent | 85.3 | Referent | 69.9 | Referent | |||
| ASD | 84.5 | 0.96 (0.62–1.49) | 0.87 | 82.3 | 1.52 (0.91–2.52) | 0.11 | 85.2 | 2.31 (1.54–3.46) | < .001* |
| ID | 89.8 | 1.30 (0.64–2.65) | 0.47 | 82.9 | 1.49 (0.74–3.04) | 0.27 | 82.6 | 2.40 (1.39–4.15) | 0.002* |
| Functional limitations status | |||||||||
| No functional limitations | 76.5 | Referent | 0.001* | 88.6 | Referent | 0.005NS | 68.3 | Referent | 0.001* |
| Functional limitations | 88.3 | 2.15 (1.35–3.44) | 80.4 | 0.45 (0.26–0.79) | 84.1 | 1.89 (1.29–2.76) | |||
| Care coordination need | |||||||||
| Needed care coordination | 83.0 | 0.82 (0.49–1.38) | 0.46 | 72.3 | 0.50 (0.33–0.77) | 0.002* | 78.0 | 0.82 (0.53–1.26) | 0.367 |
| No care coordination need | 83.3 | Referent | 89.0 | Referent | 77.2 | Referent | |||
| Early intervention receipt | |||||||||
| EI receipt | 90.3 | 1.67 (1.03–2.71) | 0.039NS | 85.5 | 1.75 (1.08–2.83) | 0.022NS | 88.0 | 2.31 (1.57–3.39) | < .001* |
| No EI | 78.2 | Referent | 82.6 | Referent | 69.3 | Referent | |||
Abbreviations: ASD, autism spectrum disorder; CI, confidence interval; DD, developmental delay; EI, early intervention; FPL, federal poverty level; ID, intellectual disability; IEP, individualized education program.
Odds ratios also adjusted for ease of access to community-based services and receipt of special education services in 2009–10.
P values were computed from the multivariable models. The Holm method was applied to P values to determine statistical significance given multiple comparisons: NS = not statistically significant at the 0.05 level after applying the Holm procedure, and
= statistically significant at the < 0.05 level after applying the Holm procedure.
Source: 2011 Survey of Pathways to Diagnosis and Services
Discussion
Both ease of access to needed community-based services and educational services receipt were poor in this nationally representative sample of school-aged children with developmental conditions, particularly considering national child health priorities and IDEA legislative mandates. Among children with an IEP, ease of access in 2009–10 was positively associated with receipt of an IEP that addressed parent concerns about the child’s development and education in 2011. Many families struggle accessing services children with developmental conditions need and the ease by which they are able to access such services is associated with IEP quality. Screening families of children diagnosed with developmental conditions about special education access and quality during pediatric healthcare visits and incentivizing providers to help families access the education services their children need may increase educational services receipt.26
Ease of access was neither associated with having an IEP nor routine receipt of ≥1 school-based therapy, suggesting other factors (e.g., elementary school grade retention, geographic location)34 may influence whether children with developmental conditions receive education services. Although younger age was positively associated with receipt of ≥1 school-based therapy, significant variation in educational services receipt by other sociodemographic factors among children with developmental conditions was not generally found. Some research shows variation in educational services receipt by certain sociodemographic factors (e.g., race/ethnicity, maternal education) among US children with special needs17 and ASD.19 Methodological differences (e.g., use of different data sources and measures) between this study and previous studies likely contribute to such discrepancies.
Consistent with past research,19,35 this study’s findings suggest certain need factors are associated with educational services receipt among children with developmental conditions. A child’s impairment level due to a developmental condition may influence whether he/she receives EI services, one factor found to be positively associated with routine school-based therapy receipt among children with an IEP. In turn, EI receipt may better enable parents of children with developmental conditions to subsequently access special education services. Still questions remain as to how children diagnosed with developmental conditions who experience little or no functional impairment could better access special education services.
Due to how the ease of access survey item was framed, we cannot know from this study exactly which services or service settings families experienced difficulty accessing. Despite controlling for special education services receipt in 2009–10 to reduce confounding in the associations estimated and tested between ease of access in 2009–10 and educational services receipt in 2011, the ease of access measure’s inclusivity may overstate these associations. Still, the negative association shown between care coordination need and receipt of an IEP addressing parent concerns suggests that when quality educational services are received care coordination needs may be better met, because children with developmental conditions are accessing the services they need.
Several additional limitations should be considered in interpreting this study’s findings. First, the observational data used make selection bias and confounding plausible. Second, all data were reported by a single source (the child’s parent), and because of this we cannot know the extent to which data on child service access and receipt as well as diagnoses, particularly DD which is not typically diagnosed after early childhood, are valid. Third, the list of school-based therapies asked about in Pathways was not exhaustive, and parents may not be aware of all of the school-based services their children received, which would lead to underestimates of school-based therapy receipt. Fourth, although ease of access was measured in 2009–10 and educational services receipt was measured in 2011, making temporal associations more likely, the exact items assessing educational services receipt differed across surveys. Last, the 2009–10 NS-CSHCN and by association Pathways response rates were relatively low, possibly limiting generalizability.
Nonetheless, our findings extend past research by comparing several educational services receipt indicators among school-aged children with three developmental conditions and by illuminating associations between educational services receipt and ease of access as well as child sociodemographic and need factors. Cross-systems interventions designed to holistically address the healthcare needs of children and their families, such as the Nurse-Family Partnership program36 and the School-Based Health Center Capital Program,37 may advance access to needed services among children with developmental conditions. Recent legislative initiatives (e.g., the Autism Understanding and Training in School Methodologies for Educators Act introduced in 2013) should also be considered to better understand and improve educational services for children with developmental conditions. Given the nexus between the healthcare and educational systems in delivering needed services to children with developmental conditions, supporting collective improvement efforts remains essential to promoting child health.
What’s New.
Among US school-aged children with developmental conditions who had an IEP, those whose parents easily accessed services were more likely to have an IEP addressing parent concerns about the child’s development and education than those whose parents did not easily access services.
Acknowledgements
We thank Julie Robertson, MSW, MPH and Christina Bethell, PhD, MPH, MBA for their assistance with data management and analysis. We also thank Ellen Smit, PhD, MS for providing the opportunity to refine the study’s design and data analyses through the graduate public health surveillance course at Oregon State University.
Funding Sources: The Medical Research Foundation of Oregon funded this project. Dr. Zuckerman’s effort was also funded by #1K23MH095828 from the National Institute of Mental Health. The funders had no involvement in the study design, data collection or analysis, results interpretation, in writing the manuscript, or in the decision to submit the article for publication.
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest to disclose.
Contributor Information
Olivia J. Lindly, Email: lindlyo@onid.oregonstate.edu.
Brianna K. Sinche, Email: brianna.sinche@gmail.com.
Katharine E. Zuckerman, Email: zuckerma@ohsu.edu.
References
- 1.Boyle CA, Boulet S, Schieve LA, et al. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics. 2011;127:1034–1042. doi: 10.1542/peds.2010-2989. [DOI] [PubMed] [Google Scholar]
- 2.Blumberg SJ, Bramlett MD, Kogan M, et al. Changes in parent-reported prevalence of autism spectrum disorder in school-aged U.S. children: 2007 to 2011–12. 2013;65 [PubMed] [Google Scholar]
- 3.Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill Summ. 2014;63(2):1–21. [PubMed] [Google Scholar]
- 4.Sabornie EJ, Cullinan D, Osborne SS, Brock LB. Intellectual, academic, and behavioral functioning of students with high-incidence disabilities: a cross-categorical meta-analysis. Exceptional Children. 2005;72(1):47–63. [Google Scholar]
- 5.Wei X, Lenz KB, Blackorby J. Math growth trajectories of students with disabilities: disability category, racial, and socioeconomic status differences from ages 7 to 17. Remedial and Special Education. 2013;34(3):154–165. [Google Scholar]
- 6.Wei X, Blackorby J, Schiller E. Growth in reading achievement of students with disabilities, ages 7 to 17. Exceptional Children. 2011;78(1):89–106. [Google Scholar]
- 7.Boulet SL, Boyle CA, Schieve LA, et al. Health care use and functional impact of developmental disabilities among US children, 1997–2005. Arch Pediatr Adolesc Med. 2009;163(1):19–26. doi: 10.1001/archpediatrics.2008.506. [DOI] [PubMed] [Google Scholar]
- 8.Schieve LA, Gonzalez V, Boulet SL, et al. Concurrent medical conditions and health care use and needs among children with learning and behavioral developmental disabilities, National Health Interview Survey, 2006–2010. Research in Developmental Disabilities. 2012;33:467–476. doi: 10.1016/j.ridd.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Ahmedani BK, Hock RM. Health care access and treatment for children with co-morbid autism and psychiatric conditions. Soc Psychiatry Pscyhiatr Epidemiol. 2012;47:1807–1814. doi: 10.1007/s00127-012-0482-0. [DOI] [PubMed] [Google Scholar]
- 10.Cidav Z, Marcus SC, Mandell DS. Implications of childhood autism for parental employment and earnings. Pediatrics. 2012;129:617–623. doi: 10.1542/peds.2011-2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nageswaran S, Parish SL, Rose RA, Grady MD. Do children with developmental disabilities and mental health conditions have greater difficulty using health services than children with physical disorders? Matern Child Health J. 2011;15:634–641. doi: 10.1007/s10995-010-0597-4. [DOI] [PubMed] [Google Scholar]
- 12.Kogan MD, Strickland BB, Blumberg SJ, et al. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics. 2008 Dec;122(6):e1149–e1158. doi: 10.1542/peds.2008-1057. [DOI] [PubMed] [Google Scholar]
- 13.Bethell CD, Kogan MD, Strickland BB, et al. A national and state profile of leading health problems and health care quality for US children: key insurance disparities and across-state variations. Acad Pediatr. 2011 May-Jun;11(3 Suppl):S22–S33. doi: 10.1016/j.acap.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Zuckerman KE, Lindly OJ, Bethell CD, Kuhlthau K. Family impacts among children with autism spectrum disorder: the role of health care quality. Academic Pediatrics. 2014;14(4):398–407. doi: 10.1016/j.acap.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mann JR, Crawford S, Wilson L, McDermott S. Does race influence age of diagnosis for children with developmental delay? Disabil Health J. 2008;1(3):157–162. doi: 10.1016/j.dhjo.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 16.Individuals With Disabilities Education Act, 20 U.S.C. § 1400. 2004 [Google Scholar]
- 17.Child Trends. Individualized education plans: Indicators on children and youth. [Accessed January 16, 2015]; Updated September 2012. Available from http://www.childtrends.org/?indicators=individualized-education-plans. [Google Scholar]
- 18.World Health Organization. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- 19.Harstad E, Huntington N, Bacic J, Barbaresi W. Disparity of care for children with parent-reported autism spectrum disorders. Academic Pediatrics. 2013;13(4):334–339. doi: 10.1016/j.acap.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Montes G, Halterman JS. Characteristics of school-age children with autism. J Dev Behav Pediatr. 2006;27:379–385. doi: 10.1097/00004703-200610000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Ruble LA, McGrew J, Dalrymple N, Jung LA. Examining the quality of IEPs for young children with autism. J Autism Dev Disord. 2010;40:1459–1470. doi: 10.1007/s10803-010-1003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. The National Survey of Children with Special Health Care Needs Chartbook 2009–2010. Rockville, MD: U.S. Department of Health and Human Services; [Google Scholar]
- 23.Medical Home Initiatives for Children With Special Needs Project Advisory Committee. The medical home. Pediatrics. 2002;110:184. [Google Scholar]
- 24.Committee on Children With Disabilities. The pediatrician's role in development and implementation of an individual education plan (IEP) and/or an individual family service plan (IFSP) Pediatrics. 1999;104:124. doi: 10.1542/peds.104.1.124. [DOI] [PubMed] [Google Scholar]
- 25.American Academy of Pediatrics. The Medical Home and Early Intervention: Linking Services for Children With Special Needs. Elk Grove Village, IL: American Academy of Pediatrics; 1995. [Google Scholar]
- 26.Shah RP, Kunnavakkam R, Msall ME. Pediatricians’ knowledge, attitudes, and practice patterns regarding special education and individualized education programs. Academic Pediatrics. 2013;13:430–435. doi: 10.1016/j.acap.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chiri G, Warfield ME. Unmet need and problems accessing core health care services for children with autism spectrum disorder. Matern Child Health J. 2012;16(5):1081–1091. doi: 10.1007/s10995-011-0833-6. [DOI] [PubMed] [Google Scholar]
- 28.Inkelas M, Smith KA, Kuo AA, Rudolph L, Igdaloff S. Health care access for children with special health care needs in California. Matern Child Health J. 2005;9(2 Suppl):S109–S116. doi: 10.1007/s10995-005-4351-2. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. 2009–2010 National Survey of Children with Special Health Care Needs Frequently Asked Questions. 2011 Dec; Available from URL: http://www.cdc.gov/nchs/slaits/cshcn.htm.
- 30.Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. 2011 Survey of Pathways to Diagnosis and Services Frequently Asked Questions. 2012 Apr; Available from URL: http://www.cdc.gov/nchs/slaits/spds.htm.
- 31. 31Federal Register. Vol 742009:4199–4201. [Google Scholar]
- 32.Aday LA, Andersen R. A framework for the study of access to medical care. Health Services Research. 1974 Fall;:208–220. [PMC free article] [PubMed] [Google Scholar]
- 33.Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics. 1979;6(2):65–70. [Google Scholar]
- 34.Silverstein M, Guppy N, Young R, et al. The receipt of special education services following elementary school grade retention. Archives of Pediatric and Adolescent Medicine. 2009;163(6):547–553. doi: 10.1001/archpediatrics.2009.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murray DW, Molina BS, Glew K, et al. Prevalence and characteristics of school services for high school students with Attention-Deficit/Hyperactivity Disorder. School Mental Health. 2014;1(6):264–278. doi: 10.1007/s12310-014-9128-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eckenrode J, Campa M, Luck DW, Henderson CR, et al. Long-term effects of prenatal and infancy nurse home visitation on the life course of youth: 19-year follow-up of a randomized trial. Arch Pediatr Adolesc Med. 2010;164(1):9–15. doi: 10.1001/archpediatrics.2009.240. [DOI] [PubMed] [Google Scholar]
- 37.US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Primary Health Care. School-Based Health Centers. Available from URL: http://www.bphc.hrsa.gov/about/schoolbased/index.html.