Abstract
Situs inversus totalis (SIT) is a rare anomaly in which the abdominal and thoracic cavity structures are located opposite to their usual positions. Occasionally, patients with this condition are diagnosed with malignant tumors. We report a case of a 60-year-old woman with gastric cancer and SIT. Laparoscopy-assisted distal gastrectomy (LADG) with D2 lymph node dissection and Billroth II anastomosis were performed successfully on the patient by careful consideration of the mirror-image anatomy. The operation required 230 min, and no intraoperative complications occurred. The final pathological report was pT4aN0M0, according to the American Joint Committee on Cancer 7th edition staging guidelines. The postoperative course was favorable, and the patient was discharged on postoperative day 8. We believe that this is the first case of LADG with D2 lymphadenectomy reported in a SIT patient with advanced gastric cancer.
Keywords: Situs inversus totalis, Laparoscopy-assisted gastrectomy, Gastric cancer, Lymph node dissection, Laparoscopic surgery
Core tip: Laparoscopic surgery in situs inversus totalis patients with gastric cancer is very rare. We performed laparoscopy-assisted distal gastrectomy with D2 lymph node dissection and Billroth II anastomosis successfully in such a patient. We hope to share the experience of laparoscopic gastrectomy in a situs inversus totalis patient with this case report.
INTRODUCTION
Situs inversus totalis (SIT) is defined as the complete mirror-image transposition of the thoracic and abdominal viscera. It is a rare congenital condition occurring at an incidence of 1:4000 to 1:8000[1]. Laparoscopic surgery in SIT patients with gastric cancer is very rare. Few cases have been reported of laparoscopy-assisted distal gastrectomy (LADG) for gastric cancer combined with SIT, and the previous cases have involved early gastric cancer with D1+ lymph node dissection. Here, we report a case of LADG with standard D2 lymph node dissection and Billroth II reconstruction for advanced gastric cancer in a patient with SIT. To the best of our knowledge, our case is the first case in China.
CASE REPORT
A 60-year-old woman was admitted to our gastroenterology ward on March 20, 2013, with dull upper abdominal pain that had persisted for the past month. Physical examination revealed mild upper abdominal tenderness. Laboratory investigation showed a hemoglobin concentration of 9.0 g/dL. SIT was diagnosed via chest radiography and abdominal computed tomography (CT). Upper endoscopy identified a large gastric antrum ulcer (Figure 1), and low-differentiated adenocarcinoma was diagnosed based on tissue biopsy. Abdominal CT showed that all of the organs inside of the abdomen were inversely positioned and that the wall of the antrum was thickened, without enlarged lymph nodes, distant metastasis or an abnormal course of vascularity (Figure 2A and B).
Figure 1.
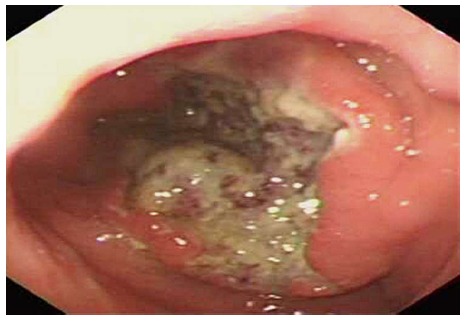
Endoscopic imaging of the gastric tumor.
Figure 2.
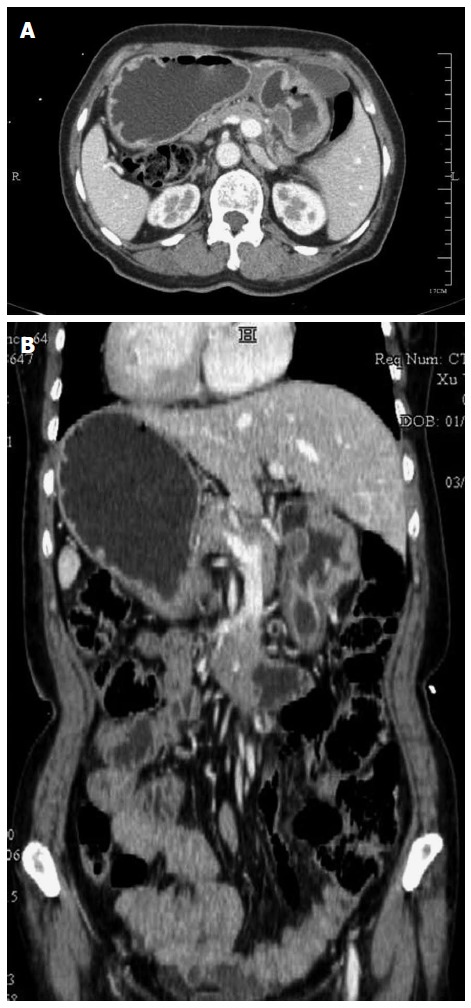
Enhanced abdominal computed tomography imaging. A: Computed tomography (CT) scan revealing thickening of the wall of the antrum, without enlarged lymph nodes. B: CT scan showing that all of the organs inside of the abdomen are inversely positioned.
Standard LADG and D2 lymph node dissection were performed. The surgeon stood on the right side of the patient (opposite the usual side for surgery at our hospital). A 10-mm camera port was created at 2 cm below the umbilicus using an open technique, and pneumoperitoneum was induced using pressure of up to 12 mm Hg of carbon dioxide. Four trocars were inserted in the left and right subcostal areas, and in the lateral abdominal region by the surgeon and the assistant (Figure 3).
Figure 3.
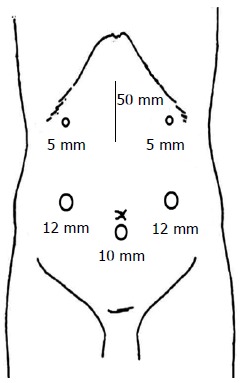
Sites of trocar placement. A camera was inserted into the subumbilical area through a 10-mm trocar.
The laparoscopic view showed inversus of the intraabdominal organs, including the stomach and spleen (Figure 4A). Dissection was initiated from the separation of the omentum using ultrasonic shears, along the border of the transverse colon from the middle to the right side. The position of the spleen was confirmed, and the left gastroepiploic vessels were exposed and ligated (Figure 4B). Then, the omentum was resected at the layer above the anterior membrane of the transverse colon. After exposure of the root of the middle colic vein and gastrocolic trunk, the station No. 14v lymph node, bound by the inferior edge of the pancreatic head and the anterior plane of the superior mesenteric vein, was dissected (Figure 4C). In the pyloric region, the location of the pancreas was confirmed, and the area between this region and the mesocolon was cut using ultrasonic shears to expose and ligate the right gastroepiploic vein, which was located on the left side. The right gastroepiploic artery, located on the left side and bifurcating from the gastroduodenal artery, was then confirmed and ligated (Figure 4D). Next, the lesser omentum was dissected. The right gastric artery, located on the left side and bifurcating from the proper hepatic artery, was confirmed and ligated, and the station No. 5 and 12a lymph nodes were resected. Then, the common hepatic artery was exposed along the plane of the periarterial plexus. After lymph node no. 8a was dissected, the coronary vein and left gastric artery, which were located on the right side, were ligated, and the station No. 7 and 9 lymph nodes were successively dissected (Figure 4E). The station No. 11p lymph node was dissected to the dorsal plane of the proximal splenic artery. The perigastric lymph nodes were dissected along the lesser curvature, up to the esophagogastric junction. Node dissection was completed, and the duodenum was divided with a linear stapler. A 5-cm incision was created at the middle of the epigastric region. Through this small incision, the stomach was pulled out of the peritoneal cavity, and the distal two-thirds of the stomach was resected using a linear stapler. A loop of the jejunum was brought up to the greater curvature side, and routine Billroth II antecolic gastrojejunostomy was performed (Figure 4F).
Figure 4.
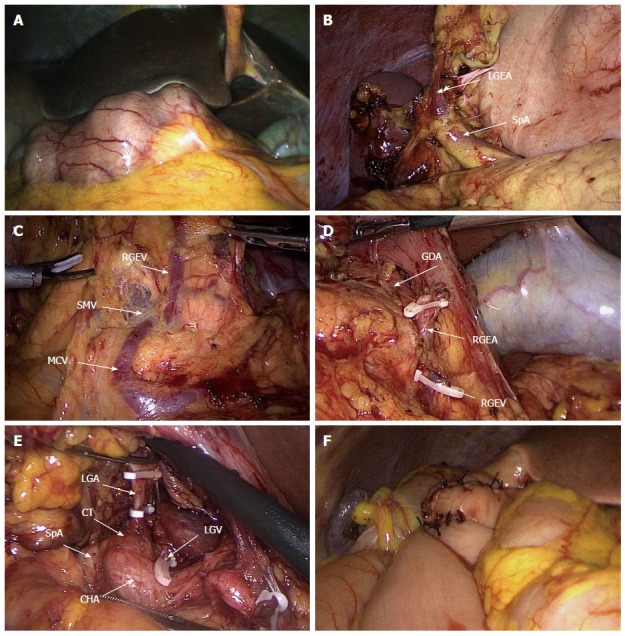
Intraoperative findings. A: Laparoscopic view showing inversion of the intraabdominal organs. B: The left gastroepiploic artery located on the right side was exposed. C: After exposure of the root of the middle colic vein and superior mesenteric vein, station no. 14v lymph node dissection was completed. D: The right gastroepiploic artery located on the left side, bifurcating from the gastroduodenal artery, was ligated. E: The left gastric artery located on the right side was ligated, allowing for dissection of station nos. 7 and 9 lymph nodes. F: Billroth II reconstruction was performed. SpA: Splenic artery; LGEA: Left gastroepiploic artery; SMV: Superior mesenteric vein; MCV: Middle colic vein; RGEV: Right gastroepiploic vein; RGEA: Right gastroepiploic artery; GDA: Gastroduodenal artery; CHA: Common hepatic artery; LGA: Left gastric artery; LGV: Left gastric vein; CT: Celiac trunk.
The operation time was 230 min, and the blood loss was 50 mL. Histopathological examination showed a 7 cm × 5 cm, poorly differentiated adenocarcinoma with serosal invasion into the posterior wall of the antrum. Thirty-five lymph nodes were examined, none of which showed metastasis (pT4aN0M0, IIB according to the American Joint Committee on Cancer, 7th edition). The postoperative course was favorable, and the patient was discharged on postoperative day 8. The patient underwent adjuvant chemotherapy and has had no recurrence for 2 years.
DISCUSSION
SIT is a relatively rare anomaly that occurs at an incidence of 1 in 4000-8000 in the population[1]. This condition is defined as congenital inverted positioning of all of the viscera, with mirror image positioning relative to their normal locations. It is usually detected incidentally during radiological examination. Anomalies of the organs in SIT include the following: a bilobed or symmetric liver; an absent spleen or the presence of multiple spleens; malrotation of the gut with abnormal mesentery; and reversed pulmonary lobulation of the lungs. Cardiac defects are common, and vascular abnormalities can involve the inferior vena cava, portal vein and hepatic artery[2]. No major abnormalities were found in our patient. The etiology of SIT remains obscure, and this condition does not influence normal health or life expectancy; however, it has important surgical implications[2].
Open surgery for gallstones or acute appendicitis in SIT patients has been reported[3,4]. Laparoscopic surgery has been performed more often in recent years, including laparoscopic cholecystectomy[5,6], laparoscopic colectomy[7-9], laparoscopic fundoplication[10] and laparoscopic gastric band surgery[11].
Few cases of LADG for gastric cancer combined with SIT have been reported previously. The first case report, published in 2003, did not mention the extent of lymph node dissection[12], and D1+ dissection was performed in the others. The present patient is the first advanced gastric cancer with SIT to undergo standard D2 lymph node dissection according to the gastric cancer treatment guidelines. Our case is likely also the first case in China.
SIT presents commonly with abnormal vascularization of the arteries and veins, and it is important to confirm the vascular anomalies on preoperative CT or angiography, particularly for laparoscopic surgery[13]. CT did not show any clear vascular anomalies in the present case.
During LADG of SIT patients, a surgeon and assistant typically stand on opposite sides of the patients to perform regular surgery. Only two authors have reported standing on the usual sides during surgery[14,15]. Seo et al[14] reported that the “mirror image” positioning of the viscera led to confusion with a surgeon’s hands. In the present case, the surgeon and assistant stood on opposite sides of the patient during surgery, which was performed using the usual procedure by completely ascertaining the anatomical features, and hand confusion was resolved by the cooperation of the surgeon and assistant.
As a result, LADG with D2 dissection and Billroth II reconstruction in our patient were completed in 230 minutes with 50 mL of bleeding. Thirty-five lymph nodes were examined histopathologically. Compared with previously reported cases, our operation led to the dissection of a sufficient number of lymph nodes without any additional blood loss or time. To prevent surgery-related complications, such as intraoperative bleeding or pancreatic injury, knowledge of the vascular anatomy and procedural caution are mandatory[14].
Laparoscopy-assisted gastrectomy (LAG) for advanced gastric cancer is performed more widely at many medical centers. Reports have demonstrated that LAG accompanied by D2 lymph node dissection for advanced gastric cancer provides an acceptable prognosis[16]. As exemplified by our patient, LAG with standard D2 lymph node dissection could be used successfully to treat advanced gastric cancer in SIT patients by predicting the vascularization based on preoperative diagnostic imaging and by ascertaining the anatomy carefully.
COMMENTS
Case characteristics
A 60-year-old woman presented with dull upper abdominal pain for the past month.
Clinical diagnosis
A large ulcer was found at the antrum of stomach by gastroduodenal endoscopy.
Differential diagnosis
Gastric ulcer or gastric neoplasm
Laboratory diagnosis
Hemoglobin: 9.0 g/dL, with other laboratory values within the normal limits
Imaging diagnosis
Computed tomography revealed a localized lesion without regional lymph node enlargement or distant metastasis, and all of the organs inside of the abdominal and thoracic cavities were inversely positioned.
Pathological diagnosis
Histopathological examination showed a 7 cm × 5 cm poorly differentiated adenocarcinoma with serosal invasion of the posterior wall of the antrum.
Treatment
The patient received laparoscopy-assisted distal gastrectomy (LADG) with D2 lymph node dissection and Billroth II anastomosis.
Related reports
Very few cases of laparoscopic surgery for gastric cancer combined with situs inversus totalis (SIT) have been reported in the literature. The previous cases have involved early gastric cancer with D1+ lymph node dissection. The authors report a case of LADG with standard D2 lymph node dissection for advanced gastric cancer in a patient with SIT.
Term explanation
SIT is defined as congenital inverted positioning of all of the viscera, with mirror-image positioning relative to their normal locations.
Experiences and lessons
Laparoscopy-assisted distal gastrectomy with standard D2 lymph node dissection can be performed successfully to treat advanced gastric cancer in SIT patients by predicting vascularization based on preoperative diagnostic imaging and by ascertaining the anatomy carefully.
Peer-review
The authors have described the use of laparoscopic surgery to treat a patient with gastric malignancy with SIT, which is rare and should, therefore, be reported. The surgical procedure was performed successfully because of the elaborate preparation and perfect cooperation of the surgeons.
Footnotes
Institutional review board statement: This study was reviewed and approved by the Institutional Review Board of the Shaoxing People’s Hospital.
Informed consent statement: The study participant provided written informed consent prior to study enrollment.
Conflict-of-interest statement: The authors have no conflicts of interest to declare.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: March 16, 2015
First decision: April 13, 2015
Article in press: July 15, 2015
P- Reviewer: Anis S, Tsytsarev V S- Editor: Yu J L- Editor: Stewart G E- Editor: Liu XM
References
- 1.Iwamura T, Shibata N, Haraguchi Y, Hisashi Y, Nishikawa T, Yamada H, Hayashi T, Toyoda K. Synchronous double cancer of the stomach and rectum with situs inversus totalis and polysplenia syndrome. J Clin Gastroenterol. 2001;33:148–153. doi: 10.1097/00004836-200108000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Patel RB, Gupta NR, Vasava NC, Khambholja JR, Chauhan S, Desai A. Situs Inversus Totalis (SIT) with Hepatocellular Carcinoma (HCC): A Rare Case Report and Review of 12 Other Cases. Indian J Surg. 2013;75:424–429. doi: 10.1007/s12262-012-0744-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kapoor R, Dhanoa J, Afzal L, Verghese M, Jacob S. Cholecystectomy under regional anesthesia in a patient with total Kartagener’s syndrome. Indian J Gastroenterol. 1997;16:64–65. [PubMed] [Google Scholar]
- 4.Akbulut S, Caliskan A, Ekin A, Yagmur Y. Left-sided acute appendicitis with situs inversus totalis: review of 63 published cases and report of two cases. J Gastrointest Surg. 2010;14:1422–1428. doi: 10.1007/s11605-010-1210-2. [DOI] [PubMed] [Google Scholar]
- 5.Aydin U, Unalp O, Yazici P, Gurcu B, Sozbilen M, Coker A. Laparoscopic cholecystectomy in a patient with situs inversus totalis. World J Gastroenterol. 2006;12:7717–7719. doi: 10.3748/wjg.v12.i47.7717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Machado NO, Chopra P. Laparoscopic cholecystectomy in a patient with situs inversus totalis: feasibility and technical difficulties. JSLS. 2006;10:386–391. [PMC free article] [PubMed] [Google Scholar]
- 7.Fujiwara Y, Fukunaga Y, Higashino M, Tanimura S, Takemura M, Tanaka Y, Osugi H. Laparoscopic hemicolectomy in a patient with situs inversus totalis. World J Gastroenterol. 2007;13:5035–5037. doi: 10.3748/wjg.v13.i37.5035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kobus C, Targarona EM, Bendahan GE, Alonso V, Balagué C, Vela S, Garriga J, Trias M. Laparoscopic surgery in situs inversus: a literature review and a report of laparoscopic sigmoidectomy for diverticulitis in situs inversus. Langenbecks Arch Surg. 2004;389:396–399. doi: 10.1007/s00423-004-0500-0. [DOI] [PubMed] [Google Scholar]
- 9.Sumi Y, Tomono A, Suzuki S, Kuroda D, Kakeji Y. Laparoscopic hemicolectomy in a patient with situs inversus totalis after open distal gastrectomy. World J Gastrointest Surg. 2013;5:22–26. doi: 10.4240/wjgs.v5.i2.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koo KP. Laparoscopic Nissen fundoplication in a patient with situs inversus totalis: an ergonomic consideration. J Laparoendosc Adv Surg Tech A. 2006;16:271–273. doi: 10.1089/lap.2006.16.271. [DOI] [PubMed] [Google Scholar]
- 11.Samaan M, Ratnasingham A, Pittathankal A, Hashemi M. Laparoscopic adjustable gastric banding for morbid obesity in a patient with situs inversus totalis. Obes Surg. 2008;18:898–901. doi: 10.1007/s11695-008-9445-7. [DOI] [PubMed] [Google Scholar]
- 12.Yamaguchi S, Orita H, Yamaoka T, Mii S, Sakata H, Hashizume M. Laparoscope-assisted distal gastrectomy for early gastric cancer in a 76-year-old man with situs inversus totalis. Surg Endosc. 2003;17:352–353. doi: 10.1007/s00464-002-4504-y. [DOI] [PubMed] [Google Scholar]
- 13.Futawatari N, Kikuchi S, Moriya H, Katada N, Sakuramoto S, Watanabe M. Laparoscopy-assisted distal gastrectomy for early gastric cancer with complete situs inversus: report of a case. Surg Today. 2010;40:64–67. doi: 10.1007/s00595-009-4007-8. [DOI] [PubMed] [Google Scholar]
- 14.Seo KW, Yoon KY. Laparoscopy-assisted distal gastrectomy for early gastric cancer and laparoscopic cholecystectomy for gallstone with situs inversus totalis: a case report. J Korean Surg Soc. 2011;81 Suppl 1:S34–S38. doi: 10.4174/jkss.2011.81.Suppl1.S34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Min SH, Lee CM, Jung HJ, Lee KG, Suh YS, Shin CI, Kim HH, Yang HK. Laparoscopic distal gastrectomy in a patient with situs inversus totalis: a case report. J Gastric Cancer. 2013;13:266–272. doi: 10.5230/jgc.2013.13.4.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang YL, Lin HG, Yang JW, Jiang FQ, Zhang T, Yang HM, Li CL, Cui Y. Laparoscopy-assisted versus open gastrectomy with D2 lymph node dissection for advanced gastric cancer: a meta-analysis. Int J Clin Exp Med. 2014;7:1490–1499. [PMC free article] [PubMed] [Google Scholar]


