Abstract
Background
Minority and low-income cancer patients are underrepresented in clinical trials, contributing to diminished access to state-of-the-art care and disparities in cancer outcomes including survivorship issues. In cervical cancer, there is a disproportionate disease burden among minority and underserved women and persistent quality of life disruption. We encountered significant challenges in both recruitment and retention in a randomized biobehavioral clinical trial for cervical cancer survivors, identified through California Cancer Registries, leading to this investigation.
Methods
To determine differential rates of accrual and retention, data from our trial are analyzed using descriptive statistics, logistic regression and multivariate analysis of variance. Ethnic differences in associations between covariables and attrition rates were tested by interaction factors. Process evaluation and focus group data were obtained to inform improvement strategies.
Results
Of eligible subjects with viable phone numbers, 29% enrolled and 71% actively or passively refused. Enrolled Hispanic women were more likely to have less education (p<0.001), lower income (p=0.003), and more children (p=0.028). The drop out rate was associated with less education (p=0.012), foreign-birth (p=0.061), speaking Spanish in the home (p=0.012). Reported reasons for active refusal were ‘too busy’ for all women, ‘too emotional’ for non-Hispanic women, ‘too ill’ and phlebotomy for Hispanic women. Subsequent focus groups identified specific strategies to improve study materials.
Conclusion
Although population-based recruitment of minority and underserved cancer patients continues to be a challenge, specific sociodemographic and disease variables can predict accrual difficulties. The information herein, taken together with disease and culturally relevant strategies, can be useful when recruiting underserved cancer survivors.
Keywords: Cervical Cancer, Recruitment, Retention, Randomized Clinical Trial, Quality of Life, Psychosocial, Telephone Counseling
Introduction
Attention to the recruitment of minorities into cancer clinical trials has grown in importance with the recognition that minorities and other underserved populations bear a far greater cancer burden than the general population [1]. Although strategies to enhance recruitment of minorities into cancer screening trials have been successful [2-4], these or similar strategies have not translated into adequate multiethnic participation in cancer treatment or survivorship trials. Participation of racial/ethnic minorities and other underrepresented groups in clinical trials is a critical link between scientific innovation and improvements in healthcare delivery since clinical trials provide patients with access to new and state-of-the art treatments and help with the translation of findings into mainstream clinical practice. Despite decades of effort by NCI to increase clinical trial participation, only 2.5 % of cancer patients participate and the rates are even lower for underserved populations [1, 5]. This lack of diversity in randomized study populations reduces opportunities for discovering effects that may be particularly relevant to underrepresented populations and contributes to inequitable distribution of benefits and risks of trial participation. Studies also show that individuals from medically underserved populations are more likely to be diagnosed with advanced stage diseases that might have been treated more effectively if diagnosed earlier [6]. These racial differences in access to state-of-the-art care contribute to disparities in cancer mortality and survival after cancer diagnosis. Data indicate these disparities disappear when minorities and Caucasians receive similar cancer treatment for same-stage disease [7].
Although Hispanic women are at lower risk for most cancers in comparison to non-Hispanic whites, they experience a higher incidence of cervical cancer [8, 9]. The age-adjusted incidence rate in California in 2002 was 14.5 per 100,000 for Hispanic women, two times higher than the incidence rate for non-Hispanic white, African American or Asian and Pacific Island women (7.3, 7.6 and 8.4 per 100,000 respectively) [9]. Ethnic differences are even greater for cervical cancers diagnosed at a later stage. Both incidence and mortality rates increase with increasing poverty and decreasing levels of education, with Hispanic women experiencing higher rates of cervical cancer than other women from lower socioeconomic groups [10].
Following diagnosis and treatment for cervical cancer, patients may experience long-term disruptions in quality of life (QOL) [11]. Adverse psychological consequences can include depression, sleeping difficulties, difficulty concentrating, and anxiety related to risk of recurrence. Sexual dysfunction, alterations in fertility, and the physical effects resulting from treatment also impact QOL [12]. Due to higher incidence rates and lifetime risk, Hispanic women represent a high risk population which would greatly benefit from interventions designed to improve overall QOL after cervical cancer. Presumed obstacles to successful recruitment and retention into disease treatment trials, and quality of life/psychosocial counseling trials exist; however there is a paucity of literature which carefully measures recruitment and retention in such studies. This would be a necessary first step toward more accurately defining problems and offering solutions.
A randomized clinical trial was conducted in cervical cancer survivors (n=50), to compare a unique psychosocial telephone counseling (PTC) intervention to usual care. QOL and biological specimens (saliva and blood) were collected at baseline and four months post enrollment. In this study, the PTC intervention yielded significantly improved QOL (p=0.011) [13]. Changes in QOL were significantly associated with a shift of immune system T helper type (Th)1:Th2 bias, as measured by Interferon gamma:Interleukin- (IL-) 5 ELISpot T lymphocyte precursor frequency, with improved QOL associated with increased Th1 bias (p=0.012). Serum IL-10 and the neuroendocrine parameters of cortisol & DHEA revealed trends supporting this shift in immunologic stance, and suggested a PTC-mediated decrease of participant's chronic stress response. Although this study provides novel mechanistic hypotheses by which interventions leading to enhanced QOL could result in improved clinical outcome, the primary study shortfall was the failure to adequately recruit or retain minority women, despite the prevalence of cervical cancer among minority populations. Therefore, the purpose of this paper is to examine population-based recruitment and retention outcomes based on key sociodemographic and disease variables, and identify strategic suggested changes based on process and qualitative measures.
Method
Human investigations were performed after approval by the local institutional review board (IRB) and in accord with an assurance filed with and approved by the U.S. Department of Health and Human Services. All written correspondence required IRB approval. Patients with a documented diagnosis of squamous cell carcinoma of the uterine cervix pathological stage I, II or III through the Cancer Surveillance Program of Orange, Imperial and San Diego Counties (CSPOC/SanDIOC), the Los Angeles Cancer Surveillance Program (LACSP), and the UC Irvine Medical Center (UCIMC) clinic were considered eligible for the study. Eligible patients included women with access to a telephone who were aged 21 years or older, fluent in English or Spanish as their primary language, diagnosed at least 13 months but less than 22 months prior to enrollment and who had completed definitive treatment. Patients with stage IV disease or receiving ongoing cancer treatment were ineligible. Because this study incorporated longitudinal psychoneuroimmune biomarker analyses, patients were further excluded if they had undergone treatment within four weeks of study enrollment with a biological response modifier (interferon, interleukin) or prior immunotherapy, used investigational drugs within 30 days of execution of the informed consent, required corticosteroids or were immune suppressed for any reason including organ allograft or HIV infection.
The cancer registry databases provided initial information used to direct recruitment efforts. Specifically, when available, contact phone numbers and addresses were provided along with race and ethnicity (including Spanish/Hispanic origin) as determined by the registering institution. The focus of the interaction between our study team and the potential participant, first through introductory letter then follow-up phone call(s) was an invitation to join a project to better understand the physical and emotional effects of recovering from cervical cancer, and to improve the quality of life of women who become diagnosed with cervical cancer in the future. Further discussion included how their names were identified through the cancer registry, and the specific components of the study (survey, blood draw, saliva collection, +/− counseling). The letter was signed by the Co-PIs (LW & ELN), and the study research assistant, on UCI letterhead.
One to two weeks after sending the introductory letter, a bilingual female research assistant attempted to contact patients by telephone. Initial selection of English or Spanish for the introductory letter was based upon ethnicity and surname data obtained from the cancer registry. At least 7 attempts, including at least 3 in the evening and on weekends, were made to contact a patient before they were considered a passive refusal. If contact was not made in one language in the first four attempts, the alternate language was incorporated into subsequent attempts. The research assistant followed a standardized script for both initial phone contact, detailed description of the study, and for the process of obtaining informed consent. Eligible women who desired to participate and provided informed consent (initially recorded verbal informed consent) were scheduled for a baseline field visit for collection of QOL data and biological specimens (blood and saliva) and upon data collection, were randomized to PTC or UC. Confirming written informed consent was obtained from each participant at the baseline field visit before any study related procedures were undertaken.
The baseline questionnaire obtained additional information on race/ethnicity, place of birth, education, occupation, income and language spoken at home. Participants randomized to the PTC arm were scheduled for six telephone counseling sessions with a bilingual female mental health professional. Counseling sessions were approximately one hour each over a 10 week period, and were scheduled at the convenience of the participant. Usual care participants received a follow-up thank you note, and information regarding the date of their next survey and blood draw. All interactions with potential and enrolled subjects, unless enrolled in the intervention arm and receiving telephone counseling, were focused on recruitment and/or logistics of biospecimen collection. A process evaluation survey was administered at the end of this study for those participants who were retained.
Subsequent to the end of this trial, and in preparation for a larger confirmatory trial, two focus groups were conducted with a cohort of cervical cancer survivors identified through the UCI medical records. Fifty cervical cancer patients not enrolled in the study described herein were identified and invited to participate in a focus group. The following themes were discussed over a 60 minute time period: invitation to participate, study logo, pictorial consent, study protocol/timeline, compensation, and retention. All participants received $25 for their participation. The sessions were recorded and transcribed by a member of the research team. The focus group transcripts were examined and segregated based on the questions asked. Three members of the research team, excluding the member who transcribed the sessions, then met to place the participants’ responses into 4 themes: psychoemotional, physical/functional, sociocultural, and knowledge. Various subthemes were then discussed and agreed upon within these 4 categories. The analytic strategy for the focus group data fundamentally followed that employed by Erwin et al, who used the PEN-3 model for developing an educational program for breast and cervical cancer screening in African-American and Latina women [9,10]. Although the PEN-3 model refers specifically to health education programming, the model was adopted for the improvement of existing study materials as a means to update the content of educating participants regarding a clinical trial. Categorizing subthemes, grouped under these categories/components, helped the researchers conceptualize and standardize the group concerns while informing the design of revisions and improvements.
Statistical Analysis
Data from this pilot study are presented using descriptive statistics (frequencies and percents or means and standard deviations). Subjects were grouped by ethnicity into Hispanic and non-Hispanic women. The Hispanic subgroup included all Latina women of Puerto Rican, Cuban, Mexican, South/Central American or Spanish origin in addition to Spanish surname only. For comparison and because of smaller numbers, all other women including Caucasian/Non-Hispanic, African-American, Asian/Pacific Islander, Native American and bi-racial women were grouped together. Ethnic groups were compared with respect to demographic characteristics and quality of life (FACT-Cx) at baseline using two-group t-tests for continuous variables or two-tailed Fisher's Exact tests for categorical variables. Subjects who dropped from the study were compared to those who completed the study with respect to demographic characteristics and baseline quality of life (QOL). Logistic regression and multivariate analysis of variance were used for multivariable analyses. Differences between ethnic groups in associations between covariables and attrition rates were tested by inclusion of interaction factors. Statistical significance is indicated by p<0.05. However because this is a pilot study with small sample size and limited power to detect differences, p-values ≤0.2 suggest a trend that may be significant and informative in a larger study.
Results
Recruitment and Enrollment
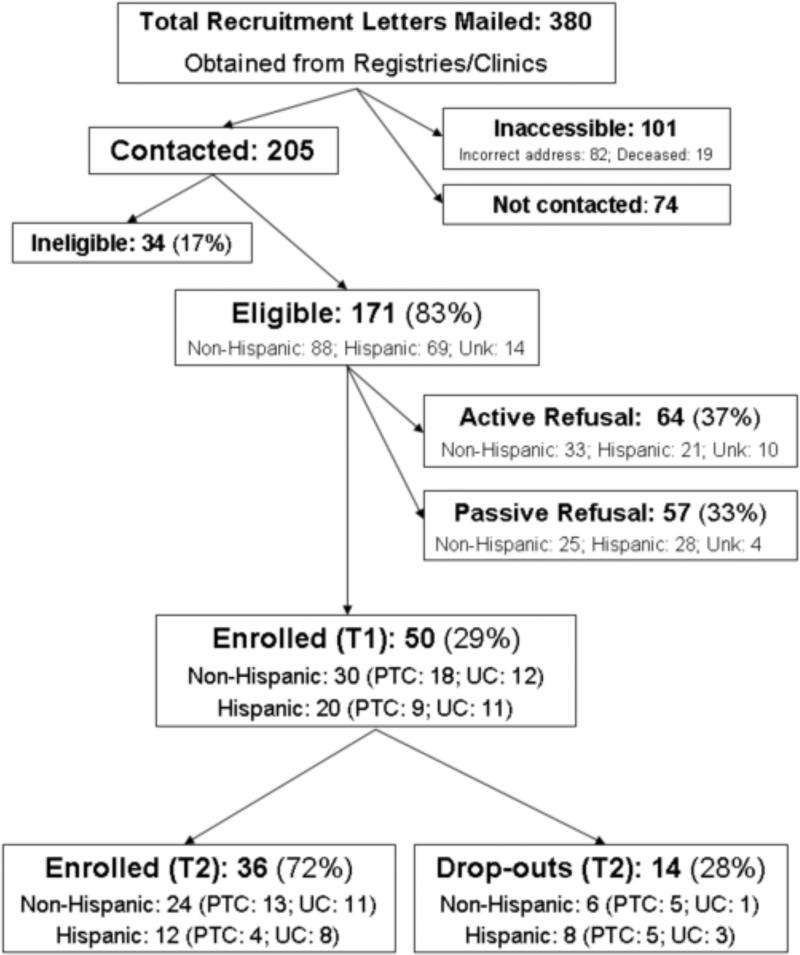
A total of 380 introductory letters were sent to cervical cancer patients identified through the UCIMC clinic and the CSPOC/SanDIOC and LACCSP cancer registries, Figure 1. Fifty-four percent (205/380) were contacted (personal contact or answering machine), 27% (101/380) were inaccessible due to incorrect address or death and 19% (74/380) were not contacted because enrollment targets had already been met. Following initial contact, 34 subjects did not meet one or more eligibility criteria, leaving a total of 171 eligible subjects with active phone numbers. Fifty (29%) enrolled in the study and were randomized, 64 (37%) refused when contacted and 57 (33%) were classified as passive refusals (eligible patient not reached by phone after a minimum of 7 attempts at various times including normal business hours, weekends, and evenings). Ninety percent of randomized subjects were recruited through the regional cancer registries with 10% recruited from a hospital clinic. Race/ethnicity was identified from cancer registry information for 92% (157/171) of eligible subjects contacted.
Figure 1.
Consort Diagram for Recruitment of Subjects
Overall refusal rates did not differ between Hispanic women (49/69=71%) and non-Hispanic women (58/93=66%; chi-square=0.464, p=0.496). There was a nonsignificant trend for non-Hispanic women to provide active versus passive refusal (57% active vs. 43% passive refusal), while the reverse was true of Hispanic women. When queried about reasons for refusal, women were most likely to prefer to give no reason, state that they were too busy, state that issues were too emotionally difficult to discuss, too much blood was required, or they were too ill to participate.
Women who self-identified as Hispanic and enrolled in the study (N=20) were well matched for numerous social, disease, and treatment variables, but differed significantly from non-Hispanic women (N=30) on certain sociodemographic characteristics including reporting more children (p=0.028), less education (p<0.001), lower income (p=0.003), greater likelihood of being born outside of the U.S. (p<0.001) and as expected, speaking Spanish as the preferred language in the home (p=0.023), Table 1. While Hispanics had less stage I disease and were more frequently treated with radiation or chemotherapy, differences were not significant. Baseline quality of life did not differ by ethnicity.
Table 1.
Descriptive Characteristics of Recruitment Sample
| Non-Hispanic (N=30) | Hispanic (N=20) | ||||
|---|---|---|---|---|---|
| Mean | SE | Mean | SE | p-value | |
| Age | 48.1 | 2.5 | 50.8 | 3.2 | 0.500 |
| # Children | 2.6 | 0.4 | 4.3 | 0.7 | 0.028 |
| FACT-Cx | 125.3 | 3.5 | 125.9 | 4.3 | 0.921 |
| N | % | N | % | p-valuea | |
|---|---|---|---|---|---|
| Birthplace | |||||
| U.S. | 25 | 83.3 | 4 | 20.0 | <0.001 |
| Other | 5 | 16.7 | 16 | 80.0 | |
| Language at Homeb | |||||
| English | 29 | 100.0 | 6 | 30.0 | 0.023 |
| Spanish | 0 | 0.0 | 14 | 70.0 | |
| Marital Status | |||||
| Married | 15 | 50.0 | 10 | 50.0 | 1.000 |
| Single/Wid/Div | 15 | 50.0 | 10 | 50.0 | |
| Education | |||||
| ≤High School | 6 | 20.0 | 15 | 75.0 | <0.001 |
| College | 24 | 80.0 | 5 | 25.0 | |
| Income | |||||
| ≤$25,000 | 5 | 16.7 | 10 | 62.5 | 0.003 |
| >$25,000 | 25 | 83.3 | 6 | 37.5 | |
| Cancer Stagec | |||||
| Stage I | 15 | 50.0 | 6 | 30.0 | 0.452 |
| Stage II-III | 8 | 26.7 | 7 | 35.0 | |
| Don't know | 7 | 23.3 | 7 | 35.0 | |
| Hysterectomyc | |||||
| No | 10 | 33.3 | 7 | 35.0 | 1.000 |
| Yes | 20 | 66.7 | 13 | 65.0 | |
| Radiationc | |||||
| No | 14 | 46.7 | 4 | 20.0 | 0.074 |
| Yes | 16 | 53.3 | 16 | 80.0 | |
| Chemotherapyc | |||||
| No | 19 | 63.3 | 9 | 45.0 | 0.251 |
| Yes | 11 | 36.7 | 11 | 55.0 |
Two-tail Fisher Exact Test
Excludes one subject speaking Chinese at home
Self-reported
Retention
Twenty-eight percent (14/50) of subjects did not complete the study, Table 2. Retention rates were significantly lower for women who spoke Spanish at home (57% vs. 17% for English speakers; p=0.012) and women with less education (48% for high school or less education compared to 14% for college-educated women, p=0.012). Retention rates were non-significantly lower in the PTC arm (63% compared to 83% in the UC arm, p=0.21), for Hispanic women (60% compared to 80% in non-Hispanic women, p=0.20), and for women born outside the U.S. (p=0.06). Importantly and somewhat unexpectedly, no significant differences were noted between women who completed the study and those who dropped with respect to age, income, cancer stage, cancer treatment or baseline QOL suggesting that other non-disease specific parameters play a more significant role in study population retention.
Table 2.
Attrition Rates by Ethnicity
| All Subjects | Non-Hispanic | Hispanic | ||||
|---|---|---|---|---|---|---|
| Covariable | N | Retained | Dropped | Dropped | Dropped | |
| Mean (SE) | Mean (SE) | p-valuea | Mean (SE) | Mean (SE) | ||
| Age | 50 | 47.9 (2.1) | 52.4 (4.5) | 0.311 | 41.5 (4.8) | 60.5 (5.5)* |
| # Children | 50 | 2.4 (0.3) | 3.3 (0.8) | 0.245 | 1.2 (0.6) | 4.6 (1.0) |
| FACT-Cx | 50 | 124.8 (3.3) | 127.6 (4.5) | 0.612 | 133.0 (6.2) | 123.0 (6.1) |
| N (%) | N (%) | p-valueb | N (%) | N (%) | ||
|---|---|---|---|---|---|---|
| Total | 50 | 36 (72) | 14 (28) | 6/30 (20) | 8/20 (40) | |
| Study Arm | 0.206 | |||||
| PTC | 27 | 17 (63) | 10 (37) | 5/18 (28) | 5/9 (56) | |
| UC | 23 | 19 (83) | 4 (17) | 1/12 (8) | 3/11 (27) | |
| Birthplace | 0.061 | |||||
| U.S. | 29 | 24 (83) | 5 (17) | 5/25 (20) | 0/6 (0) | |
| Other | 21 | 12 (57) | 9 (43) | 1/5 (20) | 8/16 (50) | |
| Language at Home c | 0.012 | |||||
| English | 35 | 29 (83) | 6 (17) | 6/29 (21) | 0 (0) | |
| Spanish | 14 | 6 (43) | 8 (57) | n/a | 8/14 (57)* | |
| Marital Status | 0.754 | |||||
| Married | 25 | 17 (68) | 8 (32) | 4/15 (27) | 4/10 (40) | |
| Single/Wid/Div | 25 | 19 (76) | 6 (24) | 2/15 (13) | 4/10 (40) | |
| Education | 0.012 | |||||
| ≤High School | 21 | 11 (52) | 10 (48) | 2/6 (33) | 8/15 (53) | |
| College | 29 | 25 (86) | 4 (14) | 4/24 (17) | 0/5 (0) | |
| Income | 1.000 | |||||
| ≤$25,000 | 15 | 11 (73) | 4 (27) | 0/5 (0) | 4/10 (40) | |
| >$25,000 | 31 | 23 (74) | 8 (26) | 6/25 (24) | 2/6 (33) | |
| Cancer Staged | 0.144 | |||||
| Stage I | 21 | 17 (47) | 4 (29) | 3/15 (20) | 1/6 (17) | |
| Stage II-III | 15 | 12 (33) | 3 (21) | 2/8 (25) | 1/7 (14) | |
| Don't know | 14 | 7 (19) | 7 (50) | 1/7 (14) | 6/7 (86) | |
| Hysterectomyd | 0.511 | |||||
| No | 17 | 11 (65) | 6 (35) | 2/10 (20) | 4/7 (57) | |
| Yes | 33 | 25 (76) | 8 (24) | 4/20 (20) | 4/13 (31) | |
| Radiationd | 0.744 | |||||
| No | 18 | 14 (78) | 4 (22) | 4/14 (29) | 0/4 (0) | |
| Yes | 32 | 22 (69) | 10 (31) | 2/16 (12) | 8/16 (50) | |
| Chemotherapyd | 0.344 | |||||
| No | 28 | 22 (79) | 6 (21) | 5/19 (26) | 1/9 (11) | |
| Yes | 22 | 14 (64) | 8 (36) | 1/11 (9) | 7/11 (64)* |
Two-tail t-test for difference between dropped and retained
Two-tail Fisher Exact test for association between attrition and covariable
Excludes one subject speaking Chinese at home
Self-reported
p<0.05 for association between attrition and covariable within ethnic group, Fisher's Exact test
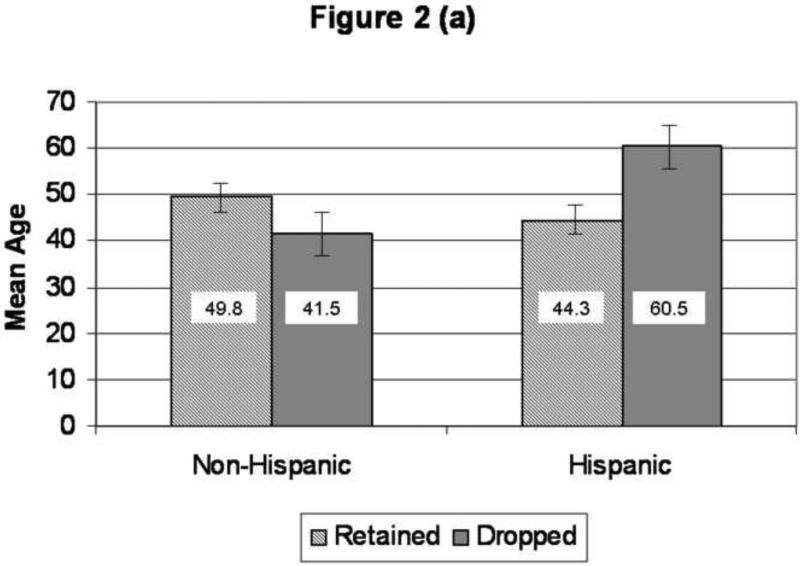
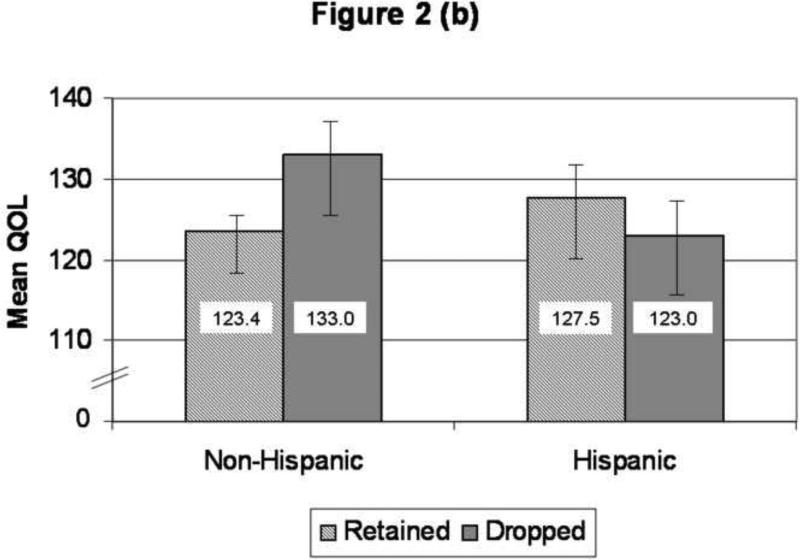
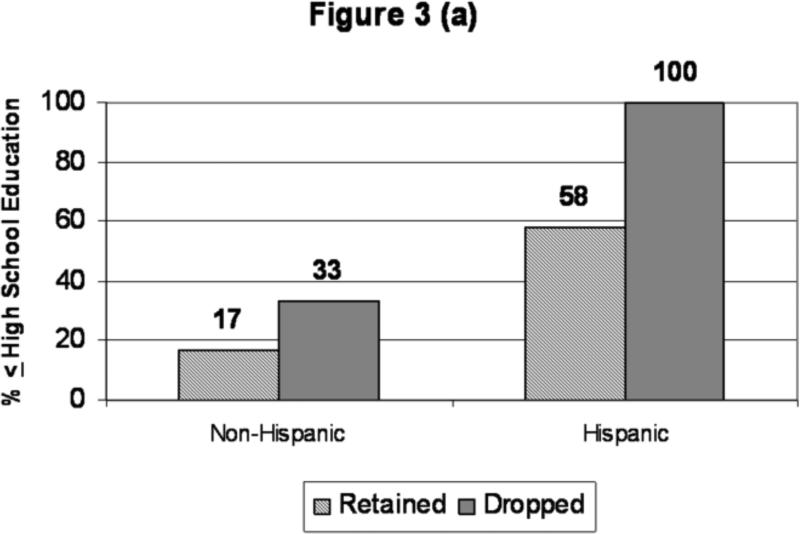
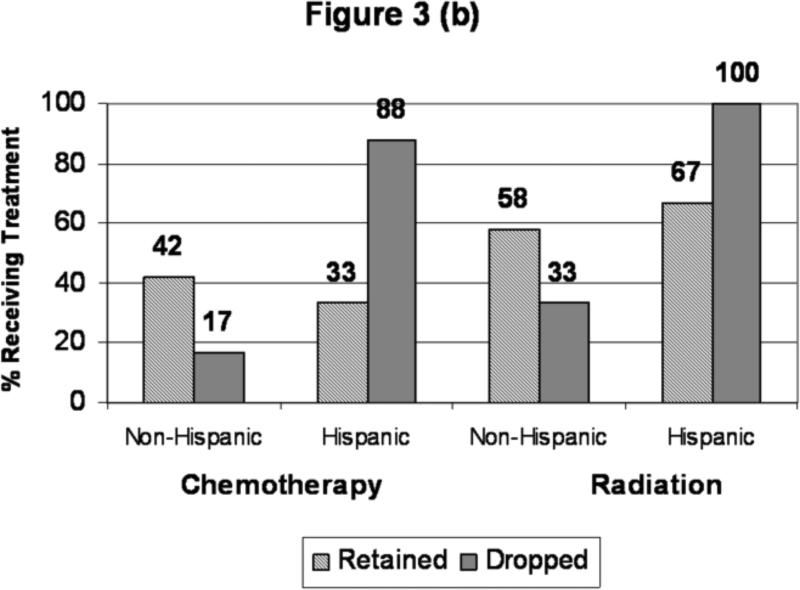
Although the sample size is small, because of the importance of retaining minority and disadvantaged populations we further investigated characteristics associated with attrition by ethnic group. Hispanic women who dropped out of the study were older than women who were retained (60.5 years at diagnosis vs. 44.3 years, p=0.01) In non-Hispanic women, we observed the opposite pattern; women who dropped out of the study were younger (p=0.01 for interaction between ethnicity and age), Figure 2, panel A. Differences in QOL between dropped and retained subjects did not reach statistical significance for either ethnic group, Figure 2, panel B. Further, attrition in Hispanics was more common in Spanish-speakers (p=0.04) and women with less education (p=0.06), Figure 3, panel A. Despite the absence of significant differences in disease stage, type of treatment was associated with study retention. Hispanic women who dropped from the study were more likely to have received chemotherapy (p=0.03) and radiation (p=0.12) compared to Hispanic women who were retained. Non-Hispanic women who dropped were less likely to have received chemotherapy (p=0.02 for interaction between ethnicity and treatment), panel B. Although multivariable analysis on a total sample of 50 subjects is limited in its capacity to detect significant differences, multivariable analyses demonstrated that attrition is significantly associated with study arm (higher for PTC; OR=5.92, 95% CI: 1.04-33.67) and speaking Spanish at home (OR=12.02, 95% CI: 2.17-66.47).
Figure 2.
Age and Baseline Quality of Life by Ethnicity and Study Retention.
Panel A, graph depicting mean age for non-Hispanic and Hispanic women who were retained in and dropped from the study. Mean values are included on each column and error bars depict standard error values. Significant differences in age was detected for Hispanic women (p=0.008) whereas non-Hispanic women who dropped were younger than those retained (p=0.19; p=0.01 for interaction between ethnicity and attrition). Panel B, graph depicting mean baseline quality of life as measured by the FACT-Cx for non-Hispanic and Hispanic women who were retained in and dropped from the study. Mean values are included on each column and error bars depict standard error values. Hispanic women who dropped out had lower QOL compared to those retained (p=0.60) whereas non-Hispanic women who dropped had higher QOL) compared to those who completed the study (p=0.23; p=0.27 for interaction).
Figure 3.
Education Level and Treatment Received by Ethnicity and Study Retention. Panel A, graph depicting percentage of non-Hispanic (n=30) and Hispanic (n=20) women who had less than a full high school education, who were retained in and dropped from the study. Exact percentages are noted above each column. Women who dropped out had less education than women retained (p=0.01) regardless of ethnicity.
Panel B, graph depicting the percentage of non-Hispanic (n=30) and Hispanic (n=20) women who received chemotherapy and radiation therapy, who were retained in and dropped from the study. Exact percentages are noted above each column. Hispanic women who dropped out had received more treatment with chemotherapy (p=0.03) and radiation (p=0.12) than those retained; in contrast, non-Hispanic women who dropped out were less likely to have received chemotherapy (p=0.40) and radiation (p=0.40) than those who remained in the study (p=0.02 and p=0.9 for interactions)
Process Evaluation
The process evaluation was completed at the end of the study by 64% (32/50) of the enrolled participants and 89% (32/36) of individuals completing the study. Women who spoke Spanish at home were significantly less likely than English-speakers to complete the evaluation (43% vs. 72% respectively, p=0.052). Women reported a high level of satisfaction with all aspects of the study and counseling process, with the exception of the blood draws. No significant differences were observed between Hispanics and non-Hispanics with respect to level of satisfaction with recruitment procedures, collection of biological specimens, or telephone counseling. However, Hispanic women were more likely to attribute greater importance to the honorarium offered than were non-Hispanics (χ2=12.2 with 4df, p=0.016).
Focus Group Evaluation
We hypothesized that some of the difficulty recruiting and retaining certain populations in this study was due, in part, to ethnic and cultural differences in the response to and perceptions of the study materials we used for recruitment, study conduct and retention. As previously noted, subsequent focus groups were conducted in order to confirm or dispute this hypothesis and solicit suggestions from cervical cancer survivors for improving study methodologies specifically by providing comments on study invitations, logo, pictorial and written informed consent, compensation and retention materials. Fifty three total patients were identified as being eligible for participation, although 15 were unable to be reached. Of the 38 remaining who were invited, 26 (68%) declined, yielding a total of 12 patients participating in one of two focus groups (6 English speaking, 6 Spanish speaking). Reasons provided for nonparticipation included: primary language other than English or Spanish; no transportation; work schedule conflict; no show/no reason; illness and other. The majority of participants had undergone both chemotherapy and radiation. English and Spanish-speakers expressed interest in new beginnings, peacefulness and hopefulness as an overall focus of the study (28%). Amidst this search for peace, 26% of participants voiced confusion regarding the lack of knowledge of side effects and treatment. This confusion was accompanied by subthemes including information overload (reported by 20% of English-speakers) and the need for clarity of both the study language and design (reported by 36% of Spanish-speakers). However, accompanying this sense of confusion and disorganization (inability to organize oneself enough mentally to understand one's own cancer diagnosis), both groups communicated emotions related to fear and depression regarding their diagnoses (16%). The women expressed disappointment in the lack of unity in cervical cancer survivors (26%) and both groups sought to encourage others by educating and helping others to promote health and prevent disease. All of the participants looked for positive words to encourage women to participate while avoiding language that specifically referred to cervical cancer. After group review of all materials, future study materials were revised to emphasize clarity and hope using language such as “promoting women's health” on study materials and removing all references to cervical cancer, stress, or other negative cancer topics which group members found threatening and distasteful. Informed consent and study procedure materials were also subsequently revised to simplify study description and include pictographic components for non-English speakers who preferred this approach to the multi-page written informed consent.
Discussion
Persistent deficiencies remain in the inclusion of representative populations in completed clinical studies, including supportive care or survivorship studies, suggesting that additional efforts and methods should be dedicated to improving recruitment and retention of target populations. Strategies set forth from Paskett and colleagues [14, 15] provide current and thoughtful guidance as we continue to be challenged by traditional strategies to recruit and retain representative samples of Hispanic and Non-Hispanic cervical cancer survivors from population-based regional cancer registries. Some of these previously tested successful strategies include adequately characterizing the target population, involving the target population in planning efforts, explaining the message to the target population, giving something back to the community, enhancing the study's credibility by using a community spokesperson, identifying and removing barriers to participation, improving staff sensitivity, and educating the target population about the importance of the trial. The example of our biobehavioral trial illustrates contemporary recruitment and retention issues, and speaks to the necessity to attend to many of the strategies noted above. Therefore, due to compromised accrual and retention of Hispanic and lower income non-Hispanic women in our initial randomized clinical trial, we considered it essential to identify sociodemographic and study-specific barriers which would inform subsequent strategies to improve clinical trial participation in these survivor populations prior to embarking on a larger, confirmatory study. Consequently, this analysis of SEER cancer registry data combined with patient report is instructive in potentially improving overall trial fidelity.
Acknowledged strengths and weaknesses exist when utilizing population-based registries for clinical trial recruitment. Some advantages include 1) identification of large numbers of potentially eligible participants, which 2) increases the likelihood of recruiting a representative sample, and thereby 3) leads to results that can be more widely generalized. Challenges include use of contact and other descriptive information from population-based registries, which may not be current or accurate. It is necessary to recognize and plan for the inevitability that many cervical cancer survivors in southern California are a mobile population who may have changed addresses and phone numbers many times since their initial diagnosis and treatment. In addition, unlike familiar clinic-based communications to existing patients, letters from an unknown institution (e.g., UC Irvine) stating that information was obtained from a state cancer registry may be viewed with suspicion or disinterest. On balance, however, utilization of a SEER registry is preferred for a relatively low incidence disease, which is prevalent in multiethnic communities. This deserves mention since, as noticed in Figure 1, a relatively large bolus of potential participants dissipates quickly.
The ratio of Hispanic to Non-Hispanic participants in our study (20/30) is representative of the proportion of Hispanics among new cases in the underlying population [16, 17]. With the enrollment of 40% Hispanics and 14% other minorities, we have also shown that it is possible to recruit a significant minority population through this methodology. Newcomb and colleagues reported use of a population-based registry for recruitment of breast cancer patients in a randomized toxicity trial [18]. The proportion of all contacted patients successfully enrolled in their study was 18%. In our study, 24% successfully enrolled (50/205) and 29% of eligible subjects (50/171) agreed to participate when contacted by phone, while 37% actively refused. An additional 33% did not answer or return messages and were deemed passive refusals although the phone number was active. In general, differences between studies in enrollment fraction may be related to differences in the underlying populations from which subjects are recruited in addition to eligibility requirements and recruitment methods (registry vs. clinic or community-based recruitment). For example, this study included a significant Hispanic population (40%) who were predominantly foreign-born (80%), Spanish-speaking (70%), with low income (63% <$25,000 per year) and high school education or less (75%). Although no statistically significant differences were observed in this small sample, trends in refusal suggested that non-Hispanic women were more likely to utilize active refusal whereas Hispanic women were more likely to utilize passive refusal. We speculate that with a larger initial sample, significant differences in refusal rates would have been evident. Further, we speculate that the manner of refusal (active vs passive) is culturally driven, and has clear implications for estimating actual participation rates.
Although sociodemographic characteristics are known predictors to trial participation, the differences between participation in a traditional cancer treatment trial compared to a quality of life or supportive care trial deserves acknowledgement. Unlike an invitation to participate in a cancer treatment trial, which classically occurs in the clinic with in-person interaction, our contact occurred via mail and phone. It is likely that this unavoidable population-based impersonal approach hampers recruitment, or enthusiasm to participate. We would like to believe, however, that follow-up culturally sensitive materials and messages from bilingual staff subsequently reduce some of the initial barriers. Quality of life/supportive care studies also impose an unavoidable difference from recruiting to a cancer treatment trial. Specifically, in this study, many women had a clear preference regarding whether or not they would want to be randomized to counseling (versus usual care). The nature of cervical cancer, in particular, often raises a sense of stigma and distress which places women at a self-disclosure disadvantage. Therefore, it is likely not only that a randomized counseling trial, with biomarker collection, may affect recruitment, but also the type of diagnosis for which this intervention is provided. One might speculate, for example, that an intervention for breast cancer survivors might have a higher recruitment yield.
The literature indicates a number of barriers to recruitment and retention among minority women, and specifically women at risk for cervical cancer. These include low income, language difficulties, lack of health insurance, limited telephone access, lack of transportation and childcare, and cultural attitudes related to health [19-22]. At minimum language, limited telephone access and cultural attitudes related to health may have affected recruitment rates among those identified as potential participants for our study. However, issues of transportation, childcare, finances or health insurance would not be directly linked to participation in this trial, since biomarkers and questionnaires were collected at the home at the convenience of the participant, and telephone counseling was also scheduled at her convenience. In our study, lower income, lower education, language spoken at home and foreign birth were all factors consistently identified as barriers to recruitment and retention, and were all significantly more frequent in Hispanic women compared to Non-Hispanics. These socioeconomic and ethnic factors were highly correlated. Thus, when factors associated with attrition were explored separately by ethnicity and in multivariable analysis only language spoken at home significantly predicted attrition. The inability to reach a potential participant by telephone even when an active number was established (57/171=33%) was a significant challenge to recruitment in our study.
Although 72% of participants were retained in the study, retention rates were lower in older Hispanic participants and younger Non-Hispanic women. The loss to follow-up of older Hispanic women may be related to cultural attitudes, which influence their willingness to document or discuss sexual dysfunction and other adverse health consequences of cancer treatment. Among the younger Caucasian population, research staff noted that several women expressed distress over discussing relationship and sexual issues and subsequently dropped from the study.
Importantly, Hispanic women treated with chemotherapy and radiation were more likely to drop out of the study (p=0.03 and p=0.12 respectively) than those not receiving these treatments, in contrast to non-Hispanic women where a trend in the opposite direction was observed that did not reach statistical significance. The increased likelihood of treatment with chemotherapy and/or radiation has notable adverse effects, coupled with the lower reported QOL in Hispanic women who dropped from the study. This information suggests that this is a group of women with significant disruption in QOL who stand to benefit from an intervention designed to improve quality of life if they could be retained.
Specific to study procedures, the requirement for blood and saliva collection at two time points may have influenced both recruitment and retention. Fourteen percent of active refusals specified the blood sample as their reason for non-participation. Although 70% of subjects completing the process evaluation noted high to very high levels of satisfaction with the blood draw, two subjects were very dissatisfied and opinions of the 14 subjects who dropped out are unknown. This points out one of the challenges of collection of biological specimens in the settings of a biobehavioral clinical study.
The focus group results, obtained from the target population, have informed strategies now ongoing to improve recruitment materials and retention efforts in future studies, including how the initial study information and informed consent material are designed, emphasizing the desire to contribute and “give back” to the community. Recruitment letter, brochure and consent language were fundamentally changed to address this stigmatizing illness in the best culturally- and disease-sensitive manner. Materials were revised to emphasize clarity, hope and peace by using language such as “promoting health” and encouraging survival while removing references to cervical cancer, stress, or other negative topics commonly associated with cancer. The study brochure was revised to avoid symbols commonly associated with breast cancer (i.e., a pink ribbon), and any imagery or language that provoked depression and fear such as the word “stress” or images of the location of the cervix. The informed consent and study procedure materials were revised to simplify the description of the study and include pictographic components to enhance the conceptualization of study procedures for non-English speakers. Finally, the logo was re-designed. Because the same imagery that evoked perceptions of humility and peacefulness in the English speaking participants evoked very different perceptions of shame or embarrassment in the Spanish speaking focus group participants, a new logo was chosen which conveyed themes of rebirth and hope but was not tied specifically to cervical cancer.
Information gleaned from this study demonstrates some of the challenges associated with population-based recruitment and retention of cervical cancer survivors, the majority of whom are underserved, and provides data which could be useful during trial development. As a result, our ongoing trial incorporates a multi-level approach for effective strategies to enhance recruitment and retention among cervical cancer survivors.
Research Highlights.
Sociodemographic factors can predict accrual & retention in cervical cancer studies.
Culturally relevant strategies are useful when recruiting minority cancer survivors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest statement:
There is no conflict of interest for any of the authors listed.
References
- 1.NCI [December 5, 2010];2010 Available from: < http://www.cancer.gov/cancertopics/factsheet/cancer-health-disparities>.
- 2.Paskett ED, et al. Recruitment of minority and underserved populations in the United States: the Centers for Population Health and Health Disparities experience. Contemp Clin Trials. 2008;29(6):847–61. doi: 10.1016/j.cct.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamilton AS, et al. Latinas and breast cancer outcomes: population-based sampling, ethnic identity, and acculturation assessment. Cancer Epidemiol Biomarkers Prev. 2009;18(7):2022–9. doi: 10.1158/1055-9965.EPI-09-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinsky PF, et al. Enrollment of racial and ethnic minorities in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial. J Natl Med Assoc. 2008;100(3):291–8. doi: 10.1016/s0027-9684(15)31241-4. [DOI] [PubMed] [Google Scholar]
- 5.Sateren WB, et al. How sociodemographics, presence of oncology specialists, and hospital cancer programs affect accrual to cancer treatment trials. J Clin Oncol. 2002;20(8):2109–17. doi: 10.1200/JCO.2002.08.056. [DOI] [PubMed] [Google Scholar]
- 6.Sheppard VB, et al. Brief report: if you build it, they will come: methods for recruiting Latinos into cancer research. J Gen Intern Med. 2005;20(5):444–7. doi: 10.1111/j.1525-1497.2005.0083.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bach PB, et al. Survival of blacks and whites after a cancer diagnosis. JAMA. 2002;287(16):2106–13. doi: 10.1001/jama.287.16.2106. [DOI] [PubMed] [Google Scholar]
- 8.ACS [August 25, 2010];2010 Available from: < http://www.cancer.org/Cancer/CervicalCancer/DetailedGuide/cervical-cancer-key-statistics>.
- 9.Nasserri K CR, Leiserowitz G, editors. Cervical Cancer in California, 2006. California Public Health Institute, Tri-counties Cancer Surveillance Program; Santa Barbara: 2006. [Google Scholar]
- 10.Singh GK, et al. Persistent area socioeconomic disparities in U.S. incidence of cervical cancer, mortality, stage, and survival, 1975-2000. Cancer. 2004;101(5):1051–7. doi: 10.1002/cncr.20467. [DOI] [PubMed] [Google Scholar]
- 11.Wenzel L, et al. Quality of life in long-term cervical cancer survivors. Gynecol Oncol. 2005;97(2):310–7. doi: 10.1016/j.ygyno.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Ashing-Giwa KT, Lim JW, Tang J. Surviving cervical cancer: does health-related quality of life influence survival? Gynecol Oncol. 118(1):35–42. doi: 10.1016/j.ygyno.2010.02.027. [DOI] [PubMed] [Google Scholar]
- 13.Nelson EL, et al. Stress, immunity, and cervical cancer: biobehavioral outcomes of a randomized clinical trial [corrected]. Clin Cancer Res. 2008;14(7):2111–8. doi: 10.1158/1078-0432.CCR-07-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paskett ED, et al. The recruitment of African-Americans to cancer prevention and control studies. Prev Med. 1996;25(5):547–53. doi: 10.1006/pmed.1996.0088. [DOI] [PubMed] [Google Scholar]
- 15.Paskett ED, et al. Participation in cancer trials: recruitment of underserved populations. Clin Adv Hematol Oncol. 2003;1(10):607–13. [PubMed] [Google Scholar]
- 16.Ikei R, R.K., Zell JA, Bringman D, Taylor TH. Cancer Surveillance Program of Orange/San Diego-Imperial Organization for Cancer Control, Epidemiology Division. University of California; Irvine: Mar, 2006. Cancer Incidence and Mortality in Orange County, 1999-2003. [Google Scholar]
- 17.Liu L ZJ, Deapen D, Bernstein L. Los Angeles County Cancer Surveillance Program. University of Southern California; 2006. Cancer in Los Angeles County: Incidence and Mortality by Race/Ethnicity 1988-2003. [Google Scholar]
- 18.Newcomb PA, et al. Using a population-based cancer registry for recruitment in a pilot cancer control study. Prev Med. 1990;19(1):61–5. doi: 10.1016/0091-7435(90)90008-8. [DOI] [PubMed] [Google Scholar]
- 19.Perez-Stable EJ, et al. Self-reported use of cancer screening tests among Latinos and Anglos in a prepaid health plan. Arch Intern Med. 1994;154(10):1073–81. doi: 10.1001/archinte.1994.00420100041007. [DOI] [PubMed] [Google Scholar]
- 20.Hubbell FA, et al. Access to medical care for documented and undocumented Latinos in a southern California county. West J Med. 1991;154(4):414–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Hubbell FA, et al. Beliefs about sexual behavior and other predictors of Papanicolaou smear screening among Latinas and Anglo women. Arch Intern Med. 1996;156(20):2353–8. [PubMed] [Google Scholar]
- 22.Shavers VL, Lynch CF, Burmeister LF. Racial differences in factors that influence the willingness to participate in medical research studies. Ann Epidemiol. 2002;12(4):248–56. doi: 10.1016/s1047-2797(01)00265-4. [DOI] [PubMed] [Google Scholar]