Abstract
Objective
The Institute of Medicine recommends cancer survivors completing treatment be provided with a treatment summary to facilitate delivery of patient-centered survivorship care. However, the relationship between treatment summary receipt and patient-centered communication (PCC) and overall quality of care (QOC) are not well understood.
Methods
Cancer survivors responding to the Health Information National Trends Survey reported treatment summary receipt, QOC, and experiences of six core functions of PCC. Multivariable logistic regression assessed the relationship between treatment summary receipt and PCC. The prevalence of survivors’ treatment summary receipt and demographic/clinical characteristics predictive of treatment summary receipt were also assessed.
Results
Of 359 respondents with a cancer history, 34.5% reported receiving a treatment summary. Greater treatment burden was associated with increased treatment summary receipt. Treatment summary receipt was associated with higher QOC and more PCC, both overall and for five of the six PCC functions.
Conclusion
The receipt of cancer treatment summaries may improve PCC and QOC for survivors.
Practice Implications
The positive relationship between treatment summary receipt and survivors’ PCC experience substantiates continued efforts to provide treatment summaries to survivors transitioning from active treatment to survivorship care. Future research should characterize mechanisms by which treatment summary provision may enhance PCC.
Graphical Abstract
1. Introduction
There are currently more than 14 million cancer survivors in the United States and this number is expected to grow substantially as the population ages and survival rates improve1. Cancer survivors must often coordinate care with multiple healthcare providers to address their complex needs, including the late and long term effects of their cancer treatments2. Treatment summaries are documents containing information about the survivor’s cancer history and specific treatments received. These summaries, as part of a comprehensive survivorship care plan, have been recommended by the Institute of Medicine and other organizations as a way to help cancer survivors communicate with future healthcare providers about their cancer history2–4. The American College of Surgeons’ Commission on Cancer accreditation standards will require all patients completing active cancer treatment be provided with a treatment summary to support the delivery of patient-centered care and facilitate transition to post-treatment survivorship care3,5.
Many survivors have difficulty reporting on their cancer or treatment history6,7, yet are often tasked with communicating this information to their healthcare providers during post-treatment survivorship care. While treatment summaries are meant to facilitate communication and coordination among providers and between survivors and providers, reports from survivors, providers, and oncology clinics suggest that their uptake is not as wide-spread as recommended8–11. However, beyond prevalence, we know less about the outcomes associated with receipt of these documents or their impact on clinical care. Specifically, the relationship between receipt of these treatment summaries and subsequent survivor reports of factors recognized by the Institute of Medicine as critical to solving the current “crisis in cancer care12, such as patient-centered communication (PCC) and quality of care (QOC) have not been examined.
Patient-centered communication (PCC) is essential for delivering quality cancer care12. In a monograph published by the National Cancer Institute10, Epstein and Street outlined six core functions of PCC: 1. Fostering a healing patient-provider relationship through building rapport and trust; 2. Exchanging clinical information and understanding patients’ representations of that information; 3. Responding to patients’ emotional needs; 4. Helping patients manage uncertainty; 5. Involving patients in the decision-making process; and 6. Enabling patient self-management through supporting patient autonomy and providing appropriate resources13. In survivorship care, these functions are essential. Survivors have complex emotional needs, often surrounding adjusting to a new “normal” after cancer14,15. They face uncertainty about their future health and report that fears about cancer recurrence are among their greatest worries16. These fears and uncertainties do not subside for long term survivors17. Survivors must make decisions about follow-up care preferences18,19. Survivors report feeling abandoned, as many are tasked to communicate information about their cancer and treatment history with future healthcare providers2.
We used data from the 2012 Health Information National Trends Survey (HINTS) to assess the relationship between receipt of treatment summaries and reports of PCC overall and for each of the six PCC functions. We hypothesize that receipt of treatment summaries will be associated with better PCC. We also aim to contribute to a growing evidence base on the use of treatment summaries by describing the overall prevalence of cancer survivors’ receipt of treatment summaries and demographic and clinical characteristics associated with receipt of treatment summaries.
2. Methods
2.1 Survey and Sample
Data were obtained from the second cycle of the fourth administration of the Health Information National Trends Survey (HINTS 4 Cycle 2). HINTS is a nationally representative survey funded by the National Cancer Institute to track health communication20. HINTS 4 Cycle 2 was fielded between October 2012 and January 2013, surveying 3,630 respondents for an overall response rate of 39.97%. For survey instruments and full methodology report, visit hints.cancer.gov.
For this analysis we limited our sample to those respondents who reported a personal history of cancer (N = 464). We further excluded individuals who had never received treatment for their cancer or were still in active treatment (N= 97) as these individuals would not be expected to have received a treatment summary. Survivors who did not respond to the main outcome question about treatment summary receipt (N=8) were also excluded; in sensitivity analysis the inclusion of these survivors in the group of individuals reporting not having received a treatment summary did not change our results. The final sample size was 359 cancer survivors (9.9% of HINTS 4 Cycle 2 respondents).
2.2 Measures
2.2.1 Receipt of treatment summaries
Respondents indicating a previous history of cancer answered the following question: “Did you ever receive a summary document from your doctor or other health care professional that listed all of the treatments you received for your cancer?” Response options were yes or no.
2.2.2 Patient-centered communication and quality of care
To assess PCC, respondents were asked six questions corresponding to the six functions of PCC outlined in the NCI monograph: “How often did the doctors, nurses, or other health care professionals you saw during the past 12 months do each of the following: 1. Give you the chance to ask all the health-related questions you had? (exchanging information) 2. Give the attention you needed to your feelings and emotions? (responding to emotions) 3. Involve you in decisions about your health care as much as you wanted? (making decisions) 4. Make sure you understood the things you needed to do to take care of your health? (enabling self-management) 5. Help you deal with feelings of uncertainty about your health or healthcare? (managing uncertainty) and 6. In the past 12 months, how often did you feel you could rely on your doctors, nurses, or other health care professionals to take your of your health care needs?” (fostering healing relationships). Response options were always, usually, sometimes or never. Consistent with prior use of these items, we analyzed the responses to the individual items by dichotomizing the responses to each PCC function as optimal (always) vs. suboptimal (usually/sometimes/never)21. In order to create an overall PCC scale, we averaged the scores from the individual items and linearly transformed the scale score to a 0–100 format.
Respondents also responded to: “Overall, how would you rate the quality of health care you received in the past 12 months?” Response options (excellent, very good, good, fair, poor) were dichotomized as excellent/very good or good/fair/poor.
2.2.3 Demographic, cancer-related and clinical characteristics
Survivors reported demographic characteristics including age, gender, education, race/ethnicity, and annual income. Survivors reported cancer-related characteristics including cancer type, time since cancer treatment (<1 yr, 1–5 yrs, 5–10 yrs, 10+ yrs), and types of treatment received (chemotherapy, radiation, surgery, other). Consistent with previous literature, a treatment burden variable was created based number of treatment modalities (one type of cancer treatment, 2 types of treatment, or 3 or more types of cancer treatment)10.
Current clinical characteristics measured included: overall health status (poor, fair, good, very good, excellent), usual source of care (yes, no), and comorbid conditions. To measure comorbid conditions, survivors were asked whether a healthcare professional had ever diagnosed them with the following conditions: diabetes or high blood sugar; high blood pressure or hypertension; a heart condition such as heart attack, angina or congestive heart failure a heart condition; chronic lung disease, asthma, emphysema, or chronic bronchitis; arthritis or rheumatism; and depression or anxiety disorder. A variable was created for the number of conditions selected (0 conditions, 1 condition, or 2+ conditions).
2.3 Analyses
Univariate statistics produced the overall proportion of cancer survivors who reported receiving treatment summaries. Pearson chi-squared analyses were used to analyze the association between demographic, cancer-related and clinical characteristics and the receipt of treatment summaries. Separate multivariable logistic regression models, with age, gender, race/ethnicity, education, income, time since treatment, health status, having a regular provider, treatment burden, number of comorbid conditions as covariates, were used to assess the association of receipt of treatment summaries on QOC and optimal PCC for each of the six dichotomized functions. An adjusted linear regression model assessed whether the continuous PCC score was predicted by receipt of a treatment summary. Due to small cell sizes, cancer type was not included in the models. Sensitivity analyses adding cancer type did not significantly change results of the analysis. All data were analyzed in SPSS v22.
3. Results
The majority of survivors in our sample were over the age of 65 (55.7%), female (56.8%), Non-Hispanic White (74.1%) and had at least some college education (68.8%) (Table 1). Survivors varied in time since treatment and cancer type, including survivors of multiple cancers (18.7%) and the majority reported receiving only one type of treatment for their cancer (61%). Most reported a regular source of care (85.2%) and at least one chronic condition (79.1%).
Table 1.
Characteristics of cancer survivors in the Health Information National Trends Survey (HINTS 4 Cycle 2) by treatment summary receipt.
| Total Samplea,b | Did not receive treatment summary | Received treatment summary | X2 p-value (unadjusted) | |
|---|---|---|---|---|
| N = 359 | 235 (65.5) | 124 (34.5) | ||
| Demographic and Socioeconomic Factors | ||||
| Gender | .847 | |||
| Male | 153 (42.6) | 99 (42.5) | 54 (43.5) | |
| Female | 204 (56.8) | 134 (57.5) | 70 (56.5) | |
| Age | .258 | |||
| 18–49 | 51 (14.2) | 29 (12.5) | 22 (17.7) | |
| 50–64 | 105 (29.2) | 64 (27.6) | 41 (33.1) | |
| 65–74 | 104 (29.0) | 72 (31.0) | 32 (25.8) | |
| 75+ | 96 (26.7) | 67 (28.9) | 29 (23.4) | |
| Education | .496 | |||
| Less than High School | 24 (6.7) | 19 (8.2) | 5 (4.0) | |
| High School | 85 (23.7) | 53 (22.8) | 32 (25.8) | |
| Some College | 122 (34.0) | 79 (34.1) | 43 (34.7) | |
| College Graduate | 125 (34.8) | 81 (34.9) | 44 (35.5) | |
| Annual Income | .926 | |||
| < $20K | 57 (15.9) | 39 (16.6) | 18 (14.5) | |
| $20K to < $50K | 101 (28.1) | 64 (27.2) | 37 (29.8) | |
| $50K to < $75K | 55 (15.3) | 37 (15.7) | 18 (14.5) | |
| $75K or more | 88 (24.5) | 59 (25.1) | 29 (23.4) | |
| Refused/don’t know/missing | 58 (16.2) | 36 (15.3) | 22 (17.7) | |
| Race/ethnicity | .060 | |||
| White (Non-Hispanic) | 266 (74.1) | 184 (78.3) | 82 (66.1) | |
| Hispanic/Latino(a) | 26 (7.2) | 15 (6.4) | 11 (8.9) | |
| NH African American | 24 (6.7) | 11 (4.7) | 13 (10.5) | |
| NH Other/Not reported | 43 (12.0) | 25 (10.6) | 18 (14.5) | |
| Cancer-Related Factors | ||||
| Time Since Treatment | .456 | |||
| Less than 1 yr | 54 (15.0) | 33 (14.0) | 21 (16.9) | |
| 1 to less than 5yrs | 102 (28.4) | 63 (26.8) | 39 (31.5) | |
| 5 to less than 10 yrs | 83 (23.1) | 54 (23.0) | 29 (23.4) | |
| 10 or more yrs | 120 (33.4) | 85 (36.2) | 35 (28.2) | |
| Treatment Burden | .007 | |||
| Received one type of cancer treatment | 219 (61.0) | 157 (67.4) | 62 (50.4) | |
| Received two types of cancer treatment | 100 (27.9) | 55 (23.6) | 45 (36.6) | |
| Received three or more types of cancer treatment | 37 (10.3) | 21 (9.0) | 16 (13.0) | |
| Cancer Type | .460 | |||
| Breast | 53 (14.8) | 31 (13.4) | 22 (17.7) | |
| Colorectal | 8 (2.2) | 6 (2.6) | 2 (1.6) | |
| Prostate | 41 (11.4) | 26 (11.3) | 15 (12.1) | |
| Melanoma | 19 (5.3) | 11 (4.8) | 8 (6.5) | |
| Other Female Cancers | 38 (10.6) | 21 (9.1) | 17 (13.7) | |
| Other Cancers | 129 (35.9) | 87 (37.7) | 42 (33.9) | |
| Multiple cancers | 67 (18.7) | 49 (21.2) | 18 (14.5) | |
| Current Clinical Factors | ||||
| Overall Health Status | .129 | |||
| Poor/fair | 84 (23.4) | 49 (21.5) | 35 (28.9) | |
| Good | 117 (32.6) | 74 (32.5) | 43 (35.5) | |
| Very good/excellent | 148 (41.2) | 105 (46.1) | 43 (35.5) | |
| Number of Comorbid Conditions | .764 | |||
| 0 | 65 (18.1) | 45 (19.7) | 20 (16.5) | |
| 1–2 | 174 (48.5) | 112 (49.1) | 62 (51.2) | |
| 3+ | 110 (30.6) | 71 (31.1) | 39 (32.2) | |
| Regular Provider | .594 | |||
| No | 47 (13.1) | 29 (12.6) | 18 (14.6) | |
| Yes | 306 (85.2) | 201 (87.4) | 105 (85.4) | |
Total sample limited to those who reported a personal history of cancer who had undergone and completed treatment.
Subcategories for each factor may not sum to total N due to missing data.
Of the 359 respondents with a cancer history who had completed active treatment, 126 (34.5%) reported receiving a treatment summary from their doctor or other health care provider (Table 1). In unadjusted, bivariate analyses, survivors who had received treatment summaries were more likely to have had two or more types of treatments for their cancer (χ2 = 9.84, p = .007). This relationship remained significant in multivariable logistic regression controlling for demographic and clinical characteristics (Wald F = 10.89, p = .004). Survivors who had reported two or three or more types of cancer treatments were over two times as likely to have received a treatment summary compared with survivors who only had a single type of cancer treatment (OR = 2.30, p = .003 and OR = 2.49, p = .03, respectively). Other demographic and clinical characteristics were not associated with receipt of survivorship care plans at the end of treatment.
In support of our hypothesis, receipt of treatment summaries was associated with higher ratings of care quality and overall PCC (Table 2). Survivors who received a treatment summary were over 3 times as likely to report excellent/very good care quality compared to those who did not receive a treatment summary (OR = 3.44, p = .005). Survivors reported a high overall level of PCC (mean = 81.54, SD = 20.60), but survivors who received a treatment summary reported higher PCC scores compared with survivors who did not receive a treatment summary (unstandardized beta = 7.03, p = .004).
Table 2.
Relationship between receipt of treatment summary and patient-centered communication and quality of care ratings.
| OR (95%CI) or Unstandardized Beta (SE) | p-valuea | |
|---|---|---|
| Overall Patient-Centered Communication Scoreb | 7.40 (2.43) | .004 |
| Six Functions of Patient-Centered Communicationc,d | ||
| Exchanging Information | 1.93 (1.09–3.40) | .024 |
| Responding to Emotions | 1.54 (.92–2.59) | .103 |
| Making Decisions | 1.96 (1.11–3.45) | .020 |
| Enabling Self-Management | 1.91 (1.08–3.37) | .027 |
| Managing Uncertainty | 1.94 (1.14–3.32) | .015 |
| Fostering Healing Relationships | 2.13 (1.20–3.79) | .010 |
| Quality of Care Ratinge | 3.44 (1.44–8.19) | .005 |
Adjusted for age, gender, race/ethnicity, education, income, time since treatment, health status, having a regular provider, treatment burden, and number of comorbid conditions.
Linear regression of patient-centered communication scale on receipt of treatment summary.
Separate logistic regressions of six functions and quality of care on receipt of treatment summary.
Dichotomized as optimal (always) vs. suboptimal (usually/sometimes/never). Suboptimal is the reference group.
Dichotomized as Excellent/Very good vs. Good/Fair/Poor. Good/Fair/Poor is the reference group.
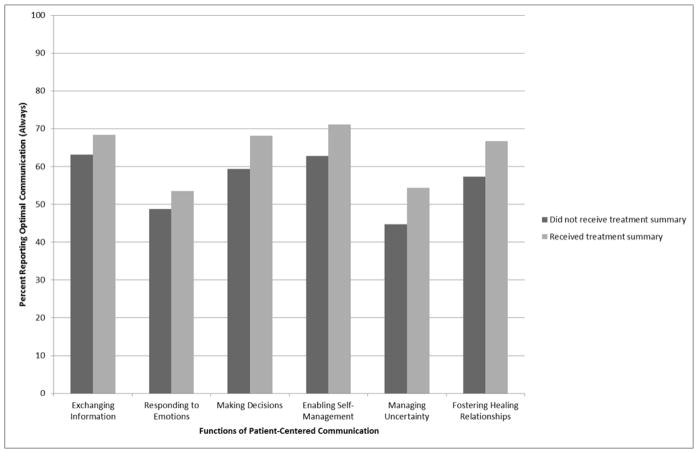
Many survivors reported suboptimal communication on each of the 6 functions (35% for exchanging information, 50% for responding to emotions, 38% for making decisions, 34% for enabling self-management, 52% for managing uncertainty, and 40% for fostering healing relationships). Survivors who had received treatment summaries were significantly more likely to report optimal PCC for five of the six functions of PCC in cancer care (Figure 1). In separate multivariable logistic regression models adjusting for demographic and clinical characteristics, receipt of treatment summaries was associated with a higher likelihood of optimal PCC for exchanging information (OR = 1.93, p = .024), making decisions (OR = 1.96, p = .020), enabling self-management (OR = 1.91, p = .027), managing uncertainty (OR = 1.94, p = .015), and fostering healing relationships (OR = 2.13, p = .010). Receipt of treatment summary was not significantly related to responding to emotions (OR = 1.54, p = .103).
Figure 1.
Percent of optimal patient-centered communication for six functions by receipt of treatment summary
4. Discussion and Conclusion
4.1 Discussion
Results from this analysis are unique in that they demonstrate that receipt of cancer treatment summaries is related to higher levels of survivor-reported PCC and QOC. The positive relationship between receipt of treatment summaries and survivors’ reports of PCC supports the continued push to make treatment summaries the standard of care for cancer survivors transitioning from active treatment to survivorship care. In this survey, PCC experience was reported for the previous year and for many survivors, treatment ended some years before. This suggests, and proponents of treatment summaries would certainly argue, that use of these documents potentially led to a more patient-centered care experience, through better care coordination, more survivor involvement, and less uncertainty about survivorship care. With the present data we are unable to make causal arguments or disentangle whether survivors who have a better relationship with their providers at the time of treatment are more likely to receive the treatment summaries and this patient-centered experience simply continues throughout survivorship.
Consistent with previous estimates, Health Information National Trends Survey data suggest that receipt of treatment summaries is relatively low, with just over a third of survivors reporting having received these documents at the end of their cancer treatment10,22,23. Survivors’ demographic characteristics did not predict receipt of treatment summaries. However, survivors with a more complex treatment history were more likely to report receiving treatment summaries. Treatment summaries may be particularly helpful in coordinating follow-up care with multiple providers for those survivors with a more complex treatment history and therefore more potential late and long term effects of treatment. However, future research on the prevalence and utilization of treatment summaries for individuals with more complex treatment histories is warranted as some previous literature has demonstrated that individuals receiving more than one type of treatment are less likely to receive a treatment summary10.
Given the cross-sectional nature of these results, no causal argument can be made. The patient-centered and QOC measures do not specify whether survivors are reporting communication and the care experience with oncologists or other types of healthcare providers. In addition, this study is limited by a relatively small number of cancer survivors and a lack of data on provider characteristics (i.e., length of relationship with provider). Receipt of treatment summaries is based only on survivor reports and may be misclassified if an individual did not remember receiving the summary. We also have no information on how the treatment summary was subsequently utilized or shared. Moreover, these data only address treatment summaries; they do not assess receipt of more comprehensive follow-up care plans, which is a separate component of the survivorship care planning process2.
The exact process by which treatment summaries may impact PCC is unknown. The relationship between treatment summary receipt and the six functions of PCC suggests that these documents may foster the relationship between survivors and their healthcare providers and lead to communication that is in line with survivor preferences. Receipt of treatment summaries and other written survivorship care plans may foster healing relationships through reduced feelings of abandonment and increased care coordination between oncologists and primary care physicians9. Treatment summaries may facilitate the exchange of information through increased discussion with primary care providers8 or survivors more accurately reporting their treatment history24. Treatment summaries may help providers manage uncertainty through an increase in recommendations for continued surveillance and prevention10. Treatment summaries may enable self-management by increasing discussions about health promotion. For many survivors, cancer represents is a “teachable moment” to begin to improve lifestyle and promote healthy living25. A study of lung and colorectal cancer survivors from the Cancer Care Outcomes Research and Surveillance Consortium demonstrated that survivors who reported receiving a treatment summary as part of a comprehensive survivorship care plan were more likely to have talked with their doctor about health promotion23. However it is important to note that the present analyses cannot distinguish potential pathways by which treatment summaries may improve these functions of PCC or discern whether receiving a treatment summary is simply a marker of patient-centered and high-quality care.
Interestingly, receipt of treatment summaries was not significantly associated with increased reports of healthcare providers addressing survivors’ emotional needs. Despite evidence that psychosocial concerns are exceedingly common in the post-treatment period26, communication about psychosocial needs between survivors and providers frequently does not occur27,28, perhaps because comprehensive survivorship care plans often fail to address the emotional aspects of follow-up care11 and there is no consensus about who should provide psychosocial care29. Ensuring that survivors feel their emotions are adequately addressed is an important aspect of patient-centered survivorship care, but a function that may not be improved with increased provision of treatment summaries.
4.2 Conclusions
Despite being unable to draw causal conclusions from our data, results represent a starting point to begin to understand potential effects of receipt of a treatment summary at the end of active cancer treatment on survivors’ PCC experience going forward. The positive association between receiving a treatment summary and experience with many of the functions of PCC is promising.
4.3 Practice Implications
This research adds to the growing, albeit limited, body of evidence that treatment summaries, ideally as part of a comprehensive survivorship care plan, are associated with positive outcomes10,23. As new mandates increase the prevalence of treatment summaries5, we must continue to carefully examine their impact on clinical communication. We know that discussions between providers and survivors of these treatment summaries and other survivorship care planning tools do not always occur8. If these treatment summaries are solely pieces of paper or documents in a digital record created to fulfill a requirement, they may not be effective in engaging survivors in the survivorship care planning process and improving PCC30. Optimal implementation of treatment summaries in survivorship care planning should include discussions between survivors and their provider team and assistance with sharing these documents with other providers via integration into the medical informatics infrastructure of the care setting31. Future research should track how treatment summaries are shared and used from the end of treatment forward to establish how treatment summaries may enhance PCC and ultimately improved clinical outcomes.
Highlights.
34.5% Health Information National Trends Survey respondents with a cancer history reported treatment summary receipt.
Greater treatment burden was associated with increased treatment summary receipt.
Treatment summary receipt was associated with greater patient-centered communication.
Treatment summary receipt was associated with higher quality of care ratings.
Acknowledgments
Role of Funding and Conflict of Interest:
The Health Information National Trends Survey is supported by contract number HHSN26120100064C from the National Cancer Institute. The views expressed in the manuscript do not necessarily represent the views of the US federal government.
Footnotes
Conflict of interest:
The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.de Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22:561–70. doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hewitt M, Greenfield S, Stovall E. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington DC: National Academies Press; 2006. [Google Scholar]
- 3.Commission on Cancer. Cancer program standards 2012: Ensuring patient-centered care. V1.0. Chicago, IL: American College of Surgeons; 2012. [Google Scholar]
- 4.Hewitt M, Ganz PA. Implementing Cancer Survivorship Care Planning. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 5.Shulman LN, Ferris L, Takanishi DM, McKellar D. Treatment Summaries and Survivorship Care Plans: The Approach by the Commission on Cancer to Increase Use. J Oncol Pract. 2014 doi: 10.1200/JOP.2014.002329. [DOI] [PubMed] [Google Scholar]
- 6.Kadan-Lottick NS, Robison LL, Gurney JG, et al. Childhood cancer survivors’ knowledge about their past diagnosis and treatment: Childhood Cancer Survivor Study. J Amer Med Assoc. 2002;287:1832–9. doi: 10.1001/jama.287.14.1832. [DOI] [PubMed] [Google Scholar]
- 7.Nissen MJ, Tsai ML, Blaes AH, Swenson KK. Breast and colorectal cancer survivors’ knowledge about their diagnosis and treatment. J Cancer Surviv. 2012;6:20–32. doi: 10.1007/s11764-011-0189-3. [DOI] [PubMed] [Google Scholar]
- 8.Blanch-Hartigan D, Forsythe LP, Alfano CM, et al. Provision and discussion of survivorship care plans with cancer survivors: Results of a nationally representative survey of oncologists and primary care physicians. J Clin Onc. 2013 doi: 10.1200/JCO.2013.51.7540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Forsythe LP, Parry C, Alfano CM, et al. Use of survivorship care plans in the United States: associations with survivorship care. J Natl Cancer Inst. 2013;105:1579–87. doi: 10.1093/jnci/djt258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sabatino S, Thompson T, Smith J, et al. Receipt of cancer treatment summaries and follow-up instructions among adult cancer survivors: results from a national survey. J Cancer Surviv. 2012:1–12. doi: 10.1007/s11764-012-0242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salz T, Oeffinger KC, McCabe MS, Layne TM, Bach PB. Survivorship care plans in research and practice. Cancer. 2012 doi: 10.3322/caac.20142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington (DC): 2013. [PubMed] [Google Scholar]
- 13.Epstein RM, Street RL. Patient communication in cancer care: Promoting healing and reducing suffering. (NIH Publication No. 07-6225) Bethesda, MD: National Cancer Institute; 2007. [Google Scholar]
- 14.Alfano CM, Rowland JH. Recovery issues in cancer survivorship: a new challenge for supportive care. Cancer. 2006;12:432–43. doi: 10.1097/00130404-200609000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Stanton AL, Ganz PA, Rowland JH, Meyerowitz BE, Krupnick JL, Sears SR. Promoting adjustment after treatment for cancer. Cancer. 2005;104:2608–13. doi: 10.1002/cncr.21246. [DOI] [PubMed] [Google Scholar]
- 16.Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7:300–22. doi: 10.1007/s11764-013-0272-z. [DOI] [PubMed] [Google Scholar]
- 17.Koch L, Jansen L, Brenner H, Arndt V. Fear of recurrence and disease progression in long-term (>/= 5 years) cancer survivors--a systematic review of quantitative studies. Psycho-oncology. 2013;22:1–11. doi: 10.1002/pon.3022. [DOI] [PubMed] [Google Scholar]
- 18.Chawla N, Arora NK. Why do some patients prefer to leave decisions up to the doctor: lack of self-efficacy or a matter of trust? J Cancer Surviv. 2013;7:592–601. doi: 10.1007/s11764-013-0298-2. [DOI] [PubMed] [Google Scholar]
- 19.Arora NK, Weaver KE, Clayman ML, Oakley-Girvan I, Potosky AL. Physicians’ decision-making style and psychosocial outcomes among cancer survivors. Patient Educ Couns. 2009;77:404–12. doi: 10.1016/j.pec.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nelson DE, Kreps GL, Hesse BW, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9:443–60. doi: 10.1080/10810730490504233. [DOI] [PubMed] [Google Scholar]
- 21.Arora NK, Reeve BB, Hays RD, Clauser SB, Oakley-Girvan I. Assessment of quality of cancer-related follow-up care from the cancer survivor’s perspective. J Clin Oncol. 2011;29:1280–9. doi: 10.1200/JCO.2010.32.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rechis R, Beckjord EB, Nutt S. Potential benefits of treatment summaries for survivors’ health and information needs: results from a LIVESTRONG survey. J Oncol Pract. 2014;10:75–8. doi: 10.1200/JOP.2013.000973. [DOI] [PubMed] [Google Scholar]
- 23.Chrischilles EA, McDowell BD, Rubenstein L, et al. Survivorship care planning and its influence on long-term patient-reported outcomes among colorectal and lung cancer survivors: the CanCORS disease-free survivor follow-up study. J Cancer Surviv. 2014 doi: 10.1007/s11764-014-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nissen MJ, Tsai ML, Blaes AH, Swenson KK, Koering S. Effectiveness of treatment summaries in increasing breast and colorectal cancer survivors’ knowledge about their diagnosis and treatment. J Cancer Surviv. 2013;7:211–8. doi: 10.1007/s11764-012-0261-7. [DOI] [PubMed] [Google Scholar]
- 25.Ganz PA. A teachable moment for oncologists: cancer survivors, 10 million strong and growing! J Clin Oncol. 2005;23:5458–60. doi: 10.1200/JCO.2005.04.916. [DOI] [PubMed] [Google Scholar]
- 26.Beckjord EB, Reynolds KA, van Londen GJ, et al. Population-level trends in posttreatment cancer survivors’ concerns and associated receipt of care: results from the 2006 and 2010 LIVESTRONG surveys. J Psychosoc Oncol. 2014;32:125–51. doi: 10.1080/07347332.2013.874004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forsythe LP, Kent EE, Weaver KE, et al. Receipt of psychosocial care among cancer survivors in the United States. J Clin Oncol. 2013;31:1961–9. doi: 10.1200/JCO.2012.46.2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adler N, Page A, editors. Cancer Care for the Whole Patient: Meeting Psychosocial Healthcare Needs. Washington DC: Institute of Medicine (IOM); 2008. [Google Scholar]
- 29.Forsythe LP, Alfano CM, Leach CR, Ganz PA, Stefanek M, Rowland JH. Who Provides Psychosocial Follow-up Care for Post-Treatment Cancer Survivors?: A Survey of Medical Oncologists and Primary Care Physicians. Journal of Clinical Oncology. 2012;30:2897–905. doi: 10.1200/JCO.2011.39.9832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beckjord E. The need for focus on outcomes and the role of informatics. J Oncol Pract. 2014;10:93–4. doi: 10.1200/JOP.2014.001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parry C, Kent EE, Forsythe LP, Alfano CM, Rowland JH. Can’t see the forest for the care plan: a call to revisit the context of care planning. J Clin Oncol. 2013;31:2651–3. doi: 10.1200/JCO.2012.48.4618. [DOI] [PMC free article] [PubMed] [Google Scholar]