Abstract
Objective
Adolescents with Anorexia Nervosa (AN), treated with family-based treatment (FBT) who fail to gain 2.3 kg by the fourth week of treatment have a 40–50% lower chance of recovery than those who do. Because of the high risk of developing enduring AN, improving outcomes in this group of poor responders is essential. This study examines the feasibility and effects of a novel adaptive treatment (i.e., Intensive Parental Coaching-IPC) aimed at enhancing parental self-efficacy related to re-feeding skills in poor early responders to FBT.
Method
45 adolescents (12 – 18 years of age) meeting DSM TR IV criteria for AN were randomized in an unbalanced design (10 to standard FBT; 35 to the adaptive arm). Attrition, suitability, expectancy rates, weight change, and psychopathology were compared between groups.
Outcomes
There were no differences in rates of attrition, suitability, expectancy ratings, or most clinical outcomes between randomized groups. However, the group of poor early responders that received IPC achieved full weight restoration (>95% of expected mean BMI) by EOT at similar rates as those who had responded early.
Conclusions
The results of this study suggest that it is feasible to use an adaptive design to study the treatment effect of IPC for those who do not gain adequate weight by session 4 of FBT. The results also suggest that using IPC for poor early responders significantly improves weight recovery rates to levels comparable to those who respond early. A sufficiently powered study is needed to confirm these promising findings.
Keywords: anorexia nervosa, family therapy, adolescents
Anorexia Nervosa (AN) is a life threatening disorder that usually onsets during adolescence. Studies suggest that AN in youth is responsive to early treatment (Le Grange, Accurso, Lock, Agras, & Bryson, 2014; Treasure & Russell, 2011), but becomes highly resistant to treatment once it has taken an enduring course (Touyz et al., 2013). Though treatment studies of AN remain limited, several randomized clinical trials support the effectiveness of a specific form of family therapy (Family-Based Treatment—FBT) for the disorder in adolescents (Lock, 2015). In these studies, FBT leads to recovery in between 35–50% of participants by the end of treatment (EOT). Follow-up studies suggest that once recovered, few relapse, but among those who do not recover, the majority (75%) were not recovered 3–5 years post treatment (Le Grange, Lock, et al., 2014; Lock, Couturier, & Agras, 2006).
To advance precision medicine by matching treatments to specific patient groups (McMahon & Insel, 2012), and because of the high risk of developing enduring AN and the associated poor prognosis, there is a need to develop and test novel interventions for those who are unlikely to recover with standard FBT. Previous studies of FBT found that a weight gain of less than 2.3 kg by session 4 of treatment predicted poorer outcome, with about 75% not achieving weight restoration by EOT (Doyle, Le Grange, Loeb, Celio-Doyle, & Crosby, 2010; Le Grange, Accurso, et al., 2014; Madden et al., 2015). Thus, an alternative way to improve outcomes would be to address this group of poor early responders using a stepped care adaptive intervention for those that needed it. In the current study, we developed a novel 3 session intervention that is conceptually and procedurally compatible with FBT called Intensive Parental Coaching (IPC). IPC provides in vivo coaching that specifically targets parental self-efficacy related to re-feeding strategies (detailed below) so that their child starts to regain weight faster (Darcy et al., 2013; Doyle et al., 2010; White et al., 2015).
Because treatment research in AN is fraught with practical challenges related to recruitment, treatment acceptability, and attrition (Lock et al., 2012), our initial aim was to examine whether a multi-site randomized clinical trial (RCT) using an adaptive or stepped care approach was feasible and acceptable to families with an adolescent with AN. We hypothesized that data would support the feasibility and acceptability of the design by demonstrating similar recruitment, retention and suitability ratings in both treatment arms. Our second aim was to gather preliminary data on the treatment effect of IPC in the context of FBT for early poor responders. In addition, previous studies suggest that improving parental self-efficacy is a possible mechanism leading to successful re-feeding efforts by parents and weight gain in their child with AN (Byrne, Accurso, Arnow, Lock, & Le Grange, 2015; White et al., 2015). We therefore also examined changes in parental self-efficacy as a treatment target in FBT and FBT+IPC. This pilot study was not powered to examine treatment effects between the randomized groups, but we were able to compare the weight gain during treatment of early poor responders in this study to an independent historical sample of adolescents treated within another RCT who also did not respond early to FBT, but did not receive any additional parental coaching.
Method
Participants
Participants for this two-site study were recruited by informing colleagues, organizations and other clinics treating eating disorders of our protocol. The study was also publicized on the Internet as well as in the local media. Potential participants could be included in the study if they were adolescents between 12 and 18 years of age living with their families and met DSM-IV criteria for AN, except for the amenorrhea requirement. Participants also had to be medically stable for outpatient treatment according to the recommended thresholds of the American Academy of Pediatrics and the Society of Adolescent Medicine (Golden et al., 2003). Potential participants taking a psychotropic medication for a co-morbid psychiatric condition (i.e., depression or anxiety), were entered into the study if they met all eligibility criteria while on stable dose of psychotropic medication for at least 8 weeks. Participants were excluded if they had an associated physical illness that necessitated hospitalization, psychotic illness/other mental illness requiring hospitalization, were dependent on drugs or alcohol or had physical conditions (e.g., diabetes mellitus, pregnancy) known to influence eating or weight. Participants were also excluded if they had previous FBT. Participants were withdrawn from the study if they were hospitalized for more than 30 days during the study or if they missed more than 4 consecutive therapy sessions.
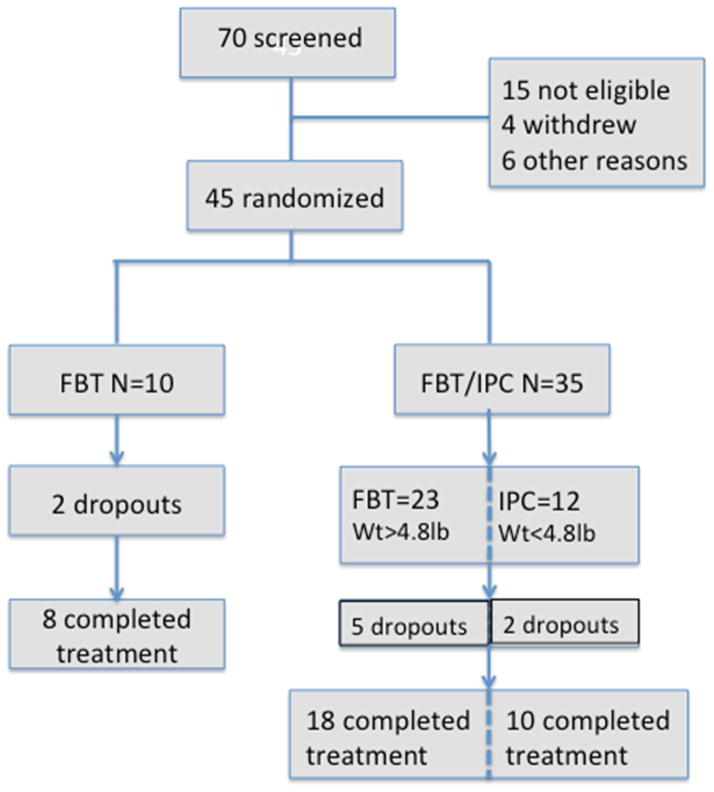
Human subjects approvals were obtained from both participating institutional IRBs. After consent by parents and adolescents over the age of 18 years (and assent in adolescents under the age of 18 years), participants were randomized in a ratio of 3.5:1 to increase the number of participants in the experimental (adaptive care arm) to maximize data about feasibility, suitability, and treatment effects of the novel focused parental coaching (Efron, 1971). There were two planned assessments (baseline and end of treatment—EOT). In addition, weight and height were obtained at each session. Suitability and expectancy ratings by the participants and parents were conducted at the conclusion of sessions at 2, 4, 6, and 8. Parental self-efficacy was rated at the conclusions of sessions 2–8. Independent trained assessors conducted assessments blind to participant randomization. See Figure 1 for our CONSORT chart.
Figure 1.
Consort chart
Measures
The following measures were used to assess study outcomes:
Recruitment and attrition rates.
Weight and height were recorded at each time points on calibrated digital scales and stadiometer. Percentile body weight was calculated using an Excel program based on the CDC tables for height, weight, gender, age, and percent expected body weight (EBW).
Therapy Suitability and Patient Expectancy (TSPE): Patients’ and parental perceptions of the suitability of the treatment provided were rated on a visual analogue scale (0–10) at sessions 2, 4, 6, 8, and end of treatment.
Eating Disorder Examination (EDE) (Cooper & Fairburn, 1987): The EDE is a standardized investigator-based interview that measures the severity of the characteristic psychopathology of eating disorders.
Schedule for Affective Disorders and Schizophrenia for School-Aged Children (6–18 years) - Present and Lifetime Version (K-SADS-PL) (Kaufman et al., 1997): The KSADS-PL was adapted from the K-SADS-P that surveys additional disorders not assessed in the K-SADS, contains improved probes and anchor points, includes diagnosis specific impairment ratings and generates DSM-IV diagnoses.
Yale-Brown-Cornell Eating Disorder Scale (YBCEDS) (Mazure, Halmi, Sunday, Romano, & Einhorn, 1994): Developed by Mazure and Halmi, the YBCEDS assesses the impairment, persistence and degree of obsessionality and compulsiveness about eating behaviors, weight, and exercise.
Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) (Goodman & al, 1989a, 1989b; Scahill et al., 1997): The CY-BOCS is a modified version of the Y-BOCS, is a 10-item, clinician-rated, semi-structured instrument that assesses symptom severity of OCD over the previous week.
Rosenberg Self-Esteem Scale (RSE) (Rosenberg, 1979): The RSE is a widely used 10-item self-report of an individual’s overall self-esteem.
Beck Depression Inventory (BDI) (A. Beck, Steer, & Garbin, 1988; A. T. Beck, 1987): The BDI is a 21-question scale with answers rated 0–3 used in numerous studies of adolescent depression.
Helping relationship questionnaire (HRQ) (Luborsky, 1984): The HRQ measures two main aspects of the therapeutic relationship: the experience of being understood and receiving a helpful attitude, and the experience of being involved in a collaborative effort with the therapist.
Parents Versus Anorexia Nervosa Scale (PvAN) (Rhodes, Baillie, Brown, & Madden, 2005): This is a validated self-report measure of parental self-efficacy specifically developed to address parental belief about their abilities to re-feed their children with anorexia nervosa.
Treatments
Family-Based Treatment (FBT)
BT is a manualized treatment divided into 3 phases (Lock & Le Grange, 2013). In the version used in this treatment, the first phase (sessions 1–6), is focused on the eating disorder and includes a family meal. This phase is characterized by attempts to absolve the parents from the responsibility of causing the disorder and by complimenting them on the positive aspects of their parenting. In Phase 2 (sessions 6–12), once weight restoration is nearing completion, parents are helped to transition eating and weight control back to the adolescent in an age appropriate manner. The third phase (sessions 13–15) is initiated when the patient achieves a healthy weight and self-starvation has abated and if focused on issues related to normal adolescent development. A total of 15 sessions were to be provided over 6 months in this treatment arm.
Intensive Family Coaching (FBT/IPC+)
This new treatment was developed and piloted, refined, and piloted again in an iterative process involving 21 cases prior to finalizing the format to be used in the current study. In the adaptive treatment arm, FBT/IPC+ provides 3 sessions added to standard FBT (described above) focused on mealtime coaching for families whose child had not gained 2.3kg by session 4. These additional sessions were inserted after session 4. The basis for IPC data collected during observational studies of the family meals comparing early responders to poor early responders (Darcy et al., 2013; White et al., 2015). These studies suggested that direct coaching at meal times might improve parental efficacy at weight restoration. The first of these sessions (new session 5) is a family session designed to present the failure in sufficient weight gain by this point as a crisis and strives to re-invigorate the family to make definitive behavioral changes to support weight restoration. Following this session (new session 6), a session with the parents only is held to identify what impediments the parents perceive might be interfering with successful re-feeding. Finally, a second family meal (new session 7) is held which includes direct coaching by the therapist to help the parents address the specific challenges identified during the meeting with the parents alone. Following these three sessions, the treatment resumes the regular course of standard FBT. Thus, a total of 18 sessions were to be provided over 6 months. Details of mealtime coaching used in the IPC adaptation of FBT have been published before (Fitzpatrick, Darcy, Le Grange, & Lock, 2015).
Statistical Approach
Baseline measures were summarized using means and SDs for continuous and using counts and proportions for categorical measures (Table 1). Our primary aim in this study was to assess the feasibility, suitability, and expectancy using an adaptive randomized design where one group received standard FBT (FBT condition) and the other had the possibility of receiving IPC should weight gain fall below 2.3kg by session 4 (FBT/IPC condition). We compared feasibility and acceptability across the randomized groups (FBT vs. FBT/IPC) using chi-square test and two-sample t-test. Feasibility of treatment was assessed by examination of recruitment and retention rates in assessment and treatment. Acceptability of treatment was assessed with a treatment suitability questionnaire. T-tests were used to compare parental self-efficacy. Finally, as an exploratory analysis, we compared the weight gain trajectory of the FBT/IPC+ group to a larger historical sample of adolescents treated with FBT in a previous RCT who were poor early responders, but whose parents did not receive IPC. These two samples were compared in terms of weight at baseline and at EOT using two-sample t-test.
Table 1.
Sample Statistics of Baseline Variables (Counts (%) for categorical and Mean (SD) for continuous variables)
| FBT (N=10) | FBT/IPC | |||
|---|---|---|---|---|
| IPC− (N=23) | IPC+ (N=12) | Total (N=35) | ||
|
| ||||
| Comorbidity | 3 (30.0%) | 12 (52.2%) | 6 (50.0%) | 18 (51.4%) |
| Depression disorders | 3 | 9 | 3 | 12 |
| Anxiety disorders | 2 | 4 | 2 | 6 |
| OCD | 1 | 2 | 1 | 3 |
| Panic | 0 | 1 | 0 | 1 |
| Phobia | 0 | 2 | 1 | 3 |
| Adjustment disorder | 0 | 0 | 1 | 1 |
| Race | ||||
| Caucasian | 9 (90.0%) | 17 (73.9%) | 11 (91.7%) | 28 (80.0%) |
| Asian | 1 (10.0%) | 3 (13.0%) | 1 (8.3%) | 4 (11.4%) |
| More than one race | 0 (0.0%) | 3 (13.0%) | 0 (0.0%) | 3 (8.6%) |
| Hispanic | 1 (10.0%) | 1 (4.3%) | 0 (0.0%) | 1 (2.9%) |
| Male | 1 (10.0%) | 20 (87.0%) | 10 (83.3%) | 30 (85.7%) |
| Intact family | 8 (80.0%) | 19 (86.4%) | 10 (83.3%) | 29 (85.3%) |
| Medication use | 3 (30.0%) | 5 (21.7%) | 4 (33.3%) | 9 (25.7%) |
| Previous Hospitalizations | 3 (30.0%) | 11 (47.8%) | 6 (50.0%) | 17 (48.6%) |
| Age | 14.3 (1.5) | 14.5 (1.3) | 14.9 (1.7) | 14.6 (1.4) |
| Duration of illness (months) | 4.3 (1.6) | 9.8 (9.0) | 18.0 (19.4) | 12.6 (13.7) |
| BMI | 16.1 (1.1) | 16.1 (0.8) | 16.4 (0.9) | 16.2 (0.9) |
| %IBW | 82.8 (3.8) | 82.0 (3.3) | 83.2 (2.9) | 82.4 (3.2) |
| Global EDE | 1.8 (1.6) | 1.5 (1.3) | 2.7 (1.6) | 1.9 (1.5) |
| CYBOCS Total | 6.3 (13.4) | 3.7 (5.2) | 5.5 (8.2) | 4.3 (6.3) |
| YBC Total | 9.1 (10.5) | 8.7 (7.8) | 12.7 (8.0) | 10.1 (8.0) |
| BDI Score | 14.2 (10.4) | 15.0 (14.2) | 19.8 (11.4) | 16.7 (13.3) |
| Rosenberg Score | 17.7 (9.7) | 19.3 (8.7) | 14.0 (5.8) | 17.5 (8.1) |
Results
We randomized 45 participants (see Consort Figure 1) to either FBT (N=10) or to FBT with adaptive treatment (FBT/IPC: 4 sessions of FBT plus IPC if necessary) for those not meeting weight gain criteria at week 4 of treatment (N=35). Recruitment rates in this study were similar to those in other RCTs utilizing FBT, averaging 1 new participant per month (Lock, Agras, Bryson, & Kraemer, 2005; Lock, Couturier, Bryson, & Agras, 2006; Lock et al., 2010). See Figure 1 for the adaptive design and Table 1 for participant baseline characteristics.
We present results in order of our aims: 1) retention and treatment use; 2) suitability and expectancy; 3) clinical outcomes; 4) changes in parental self-efficacy (target engagement); and 5) comparison of change in expected change in weight trajectory in IPC group compared to a historical sample of similar adolescents who were poor early responders treated using FBT without IPC. Our primary outcomes (attrition and treatment suitability, expectancy) were compared across the two randomized arms (FBT vs. FBT/IPC) as shown in Table 2. Note that our project was mainly intended to provide the feasibility information and was not properly powered for formal group comparisons. We still provide here preliminary group comparison results, although they should be interpreted with caution given the limited sample size employed.
Table 2.
Group Differences (FBT vs. FBT/IPC) for the Primary and Secondary Outcomes at EOT
| Mean (SD) or Counts (%)
|
|||
|---|---|---|---|
| FBT (N=10) | FBT/IPC (N=35) | p-value | |
|
| |||
| Primary Outcomes | |||
| Dropout | 2 (20.0%) | 7 (20.0%) | .655 |
| Number of Sessions | 12.9 (3.6) | 13.9 (4.3) | .511 |
| Child Suitability | 5.1 (3.4) | 5.0 (3.3) | .914 |
| Child Expectancy | 5.8 (3.1) | 5.6 (3.0) | .801 |
| Mother Suitability | 7.6 (2.1) | 8.1 (2.2) | .563 |
| Mother Expectancy | 7.6 (1.6) | 7.8 (2.0) | .837 |
| Father Suitability | 8.6 (1.6) | 8.3 (1.5) | .577 |
| Father Expectancy | 8.9 (0.9) | 8.2 (1.5) | .195 |
| Secondary Outcomes | |||
| Recovery (%EBW >= 95) | 5 (63.0%) | 17 (51.5%) | .576 |
| Weight | 114.4 (12.9) | 111.6 (13.5) | .598 |
| BMI | 18.9 (1.2) | 19.0 (1.4) | .735 |
| %EBW | 96.5 (4.7) | 95.7 (7.2) | .759 |
| Global EDE | 0.3 (0.4) | 1.1 (1.4) | .143 |
| CYBOCS Total | 3.6 (8.9) | 3.7 (6.1) | .947 |
| YBC Total | 3.8 (7.8) | 5.2 (7.1) | .615 |
| BDI Score | 10.8 (13.9) | 10.7 (12.6) | .990 |
| Rosenberg Score | 19.3 (7.8) | 19.7 (8.5) | .903 |
| HRQ score | 52.8 (19.3) | 49.6 (16.6) | .666 |
For group comparisons, we used independent sample t-test for continuous variables and used Pearson chi-square test for the binary variables (dropout and recovery).
Retention and treatment: There were no differences in attrition rates between those randomized to FBT or FBT/IPC groups (20% in both groups; N=2 in FBT; N=7 in FBT/IPC). One participant was withdrawn from the study. The number of treatment sessions also did not differ between the randomized groups at EOT (12.9 sessions for FBT; 13.9 sessions in FBT/IPC). We also compared the attrition rate and the number of sessions within the FBT/IPC+ group to examine whether having additional IPC has any impact on patients’ participation. Neither the attrition rate (23% for FBT/IPC- and 17% for FBT/IPC+), nor the number of sessions attended (12.6 sessions for FBT/IPC- and 16.3 sessions for FBT+IPC) was considerably different, indicating the feasibility of applying the adaptive treatment in practice. Approximately 1/3 of the participants were taking psychotropic medications for co-morbid conditions (e.g., antidepressants, antipsychotics, anxiolytics, mood stabilizers, and medication for attention deficit hyperactivity disorder).
Suitability and Expectancy Ratings: Ratings of the suitability and expectancy of treatment were assessed by the patient participant and both parents independently. These ratings were assessed at sessions 2, 4, 6, and 8. No statistically significant differences were found between ratings across the treatment arms (see Table 2). Patient ratings were mostly mid-range (5 to 6 on the Likert 10 point scale), while parental ratings were relatively high (7–9 on the Likert 10 point scale).
-
Clinical Outcomes: There were no noticeable differences between randomized groups in terms of the recovery rate, weight, BMI, and %EBW. Table 2 also shows that the two groups are quite comparable in terms of other secondary outcomes, though a significant difference was found in scores on the global EDE.
We also examined the differences within the adaptive arm (FBT/IPC) as shown in Table 3. The differences between those who received IPC (IPC+) and those who did not (IPC−) were not significant in both the primary and secondary outcomes except global EDE. Note that the comparison results provided here are preliminary and should be interpreted with caution given the limited sample size employed in the study.
Target Engagement: Comparing scores on the PvAN at session 2 of FBT between those who respond early and those who do not, there was a significant difference suggesting that mothers whose children respond earlier believe they are more self-efficacious (early responders: M=25.09, SD=3.31 vs non early responders: M=21.82, SD=3.57, t(30)=2.587, p = .015). However after additional treatment aimed at improving parental self-efficacy through IPC, scores on the PvAN improved in this group and no longer differed between early responders and those who did not (early responders M=24.41, SD=2.48 vs non early responders M=24.1, SD=2.96, t (25)=.294, p = .771).
Changes in expected weight trajectory after IPC: As a consequence of the use of an unbalanced randomization procedure, we could not compare the outcomes of the poor responders in the FBT arm (N=2) and the poor responders in the FBT/IPC arm (N=12) even in a preliminary manner. Given that, as an exploratory investigation, we compared the poor early responders in the FBT/IPC+ arm (N=12) in the current study to a similar group of poor early responders (i.e., those who did not gain 2.3 kgs by session 4) from a previous RCT (N=28) that did not include the IPC treatment (Agras et al., 2014). The criteria for entry and FBT treatment were the same in these two studies. At baseline, relevant clinical variables were also remarkably similar at baseline between the two samples with no statistically significantly difference identified on between them except for family income and the RSE. Family income was greater and self-esteem scores lower in the sample used in the study. Given complete absence of information regarding adaptive versus standard FBT treatments, we believe this comparison provides some insights on potential efficacy of the adaptive FBT. However, note that this comparison result should be interpreted with caution as the compared data are from outside our current study. Figure 2 shows a comparison between these two groups. At baseline, the two groups are similar in terms of weight (Cohen’s d = 0.06, p = .417). The difference in weight trajectories after session 4 between treated (current FBT/IPC+) and non-treated (standard FBT in previous RCT) groups is apparent, as shown in Figure 2. By EOT, the two samples are considerably different in terms of weight (Cohen’s d = 0.82, p = .002).
Table 3.
Differences between Patients with and without IPC among Those Randomized to the FBT/IPC Condition in terms of the Primary and Secondary Outcomes at EOT
| Mean (SD) or Counts (%)
|
|||
|---|---|---|---|
| FBT/IPC− (N=23) | FBT/IPC+ (N=12) | p-value | |
|
| |||
| Primary Outcomes | |||
| Dropout | 5 (21.7%) | 2 (16.7%) | .722 |
| Number of Sessions | 12.6 (4.6) | 16.3 (2.1) | .012 |
| Child Suitability | 5.5 (3.5) | 4.2 (2.9) | .295 |
| Child Expectancy | 6.1 (3.1) | 4.7 (2.9) | .219 |
| Mother Suitability | 7.6 (2.4) | 9.0 (1.5) | .079 |
| Mother Expectancy | 7.4 (2.3) | 8.5 (1.2) | .123 |
| Father Suitability | 8.3 (1.7) | 8.3 (0.8) | .955 |
| Father Expectancy | 8.3 (1.5) | 7.9 (1.4) | .467 |
| Secondary Outcomes | |||
| Recovery (%IBW >= 95) | 10 (47.6%) | 7 (58.3%) | .554 |
| Weight | 111.5 (16.1) | 111.7 (8.0) | .955 |
| BMI | 18.9 (1.6) | 19.3 (0.9) | .487 |
| %IBW | 95.1 (7.6) | 96.7 (6.5) | .552 |
| Global EDE | 0.7 (1.0) | 1.9 (1.7) | .013 |
| CYBOCS Total | 2.6 (4.9) | 5.9 (7.9) | .150 |
| YBC Total | 3.5 (5.1) | 8.5 (9.4) | .056 |
| BDI Score | 7.9 (10.9) | 15.2 (14.2) | .151 |
| Rosenberg Score | 22.5 (7.0) | 15.7 (9.3) | .053 |
| HRQ score | 54.6 (16.5) | 40.9 (13.6) | .059 |
For group comparisons, we used independent sample t-test for continuous variables and used Pearson chi-square test for the binary variables (dropout and recovery).
Figure 2.
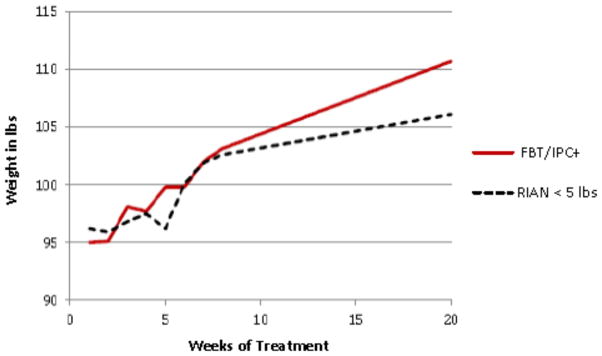
Weekly weights comparing FBT/IPC+ in the current trial with a sample of poor early responders (weight gain less than 5 pounds by 4 weeks) from a previous controlled trial (RIAN: Agras et al., 2014)
Discussion
This study demonstrates that a multi-site RCT using an adaptive treatment is feasible and acceptable to families being treated using FBT for adolescent AN. Overall recruitment and attrition rates were typical of other studies using standard FBT (Lock et al., 2005; Lock et al., 2010). In addition, weight gain was similar in both groups and reached recovery (i.e., >95% of mean expected BMI), or near recovery levels, on average in both groups (Bardone-Cone et al., 2010; Couturier & Lock, 2006). While these data might appear to suggest no added benefit of the additional IPC treatment, the small sample size in the FBT group makes this comparison on this variable of limited value as there were only 2 of the 12 participants who were not early responders in this group. Instead, the data related to the FBT/IPC+ group who were expected to do comparatively poorly if the IPC intervention was not effective, actually did well. Particularly noteworthy in this regard is the finding that the rates of weight restoration in the poor early responders who received IPC (FBT/IPC+) reached 58.3%, which is similar to that achieved in those who had responded early (63% in this study). Further, in an exploratory analysis comparing an independent sample of adolescents with AN who were also poor early responders to FBT, but did not receive IPC, there was a statistically significant difference between the groups in terms of weight gain by the EOT associated with a large effect size (see Figure 2). It might be suggested that despite the lack of a statistical difference in numbers of sessions used between the groups, the IPC group still had more treatment on average, and it was additional sessions rather than the specific interventions offered in IPC that were responsible for the improvements in this group. However, arguing against this supposition are prior studies showing that simply adding more sessions of standard FBT did not improve outcome (Le Grange, Accurso, et al., 2014; Lock et al., 2005). Among the secondary measures examined, only the global EDE differed between groups. This finding could mean that although IPC improves weight outcome it has less effect on eating relatead psychopathology. Alternatively, it is possible that these secondary measures have yet to change. Previous studies of FBT (Couturier & Lock, 2006; Lock, Couturier, & Agras, 2006) suggest that improvement in EDE lags 6–12 months after weight restoration; hence, the fact that there was a delay in weight restoration in the poor early responding group may lead to a consequent delay in changes in eating related psychopathology. Longer-term follow-up of this sample might shed additional light on these preliminary findings.
FBT targets improving and supporting parental self-efficacy about re-feeding as a starting point in treatment. FBT assumes a primary reason that parents are ineffective in successfully re-feeding their children is that they are uncertain and ambivalent about taking on the difficult behavioral challenges that an adolescent with AN presents. From the first session forward, therapists encourage parents to believe in their own abilities rather than allow the protests and behaviors associated with AN to subvert their efforts. There are many reasons that parents feel ineffective in the face of AN--guilt for having caused the problem, stigma associated by being blamed by professionals, a lack of knowledge about how to confront and disrupt the maintaining behaviors (i.e., caloric restriction, over exercise, and purging that lead to starvation), a lack of assistance in developing a manageable approach to disrupting these behaviors at home, and a fear of doing harm to their relationship with their child if they insist on behavioral change.
Data suggests that measures of parental self-efficacy change as a result of FBT. A study by Bryne and colleagues that compared parental self-efficacy in 121 adolescents with AN randomized to receive either FBT of individual therapy (Adolescent Focused Therapy—AFT) found that increases in self-efficacy using the Parents versus Anorexia Nervosa Scale (PvAN) predicted significantly greater weight gain for adolescents who received FBT, but not for adolescents who received AFT (Byrne et al., 2015). Data from our current trial provides further support that FBT targets and engages parental self-efficacy. Comparing scores on the PvAN at session 2 of FBT between those who respond early and those who do not, there was a significant difference suggesting that mothers whose children respond earlier believe they are more self-efficacious after only one session of FBT than those mothers whose children do not respond early. However after additional treatment aimed at improving parental self-efficacy through IPC, scores on the PvAN improved in the mothers of the poor early responders to the point they and no longer differed from those of early responders at the end of IPC (session 8). These preliminary data suggest that treatment for poor early responders, i.e., FBT/IPC+) engages parental self-efficacy, albeit later than in those who respond early.
There are important limitations to this study. The sample size is modest and results of a larger study based on the demonstrated feasibility of the design and efficacy of the intervention are warranted to systematically examine and confirm these preliminary findings. Further, because of the unbalanced randomization procedure used to enhance data from the experimental adaptive arm, conclusions about comparable effects are tentative. In addition, though the use of a historical comparison group of similar randomized participants from these same research sites provides possible additional insight into the potential benefits of the adaptive intervention, these data cannot replace a true randomized comparison. Finally, though treatment studies suggest that outcomes of those treated with FBT are stable at 3–5 year follow-up, (Eisler et al., 1997; Le Grange, Lock, et al., 2014; Lock, Couturier, & Agras, 2006) longer term follow-up of this sample examining maintenance of treatment effects is needed.
Taken together, the data from the current study provide preliminary support for the feasibility of recruiting and treating participants to an adaptive study of family treatment for adolescents with AN. Moreover, those in the FBT/IPC+ group gained weight to reach normal weight thresholds of remission even though at session 4, approximately 75% of them would not have been expected to do so (Doyle et al., 2010). However, until an adequately powered RCT is conducted to confirm these preliminary findings, conclusions about how best to treat these early non-responders who are at high risk of developing enduring AN must be tempered by the exploratory nature of the findings of this study.
Highlights for review.
pilot adaptive RCT (stepped care) employed a novel treatment (intensive parental coaching—IPC) to further increase parental ability to re-feed their children with anorexia nervosa
study suggests conducting an adequately powered adaptive RCT is feasible and acceptable to parents
suitability and expectancy ratings for treatments used in the RCT are good
use of early response (weight gain of 2.3 Kg) as cut point for adding adaptive intervention is feasible
preliminary evidence that novel treatment improves outcomes in those who previously would not have been expected to remit given their poor early response to FBT
evidence of target engagement related to parental self-efficacy is provided
Acknowledgments
Funding for the study was provided by NIMH to Dr. Lock (PI) R34MH09349303, Dr. Le Grange (PI) R34-MH093768, and Dr. Agras, (co-PI), R34MH09349303. This work has not been previously published or submitted elsewhere for consideration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
James Lock, Email: jimlock@stanford.edu, Department of Psychiatry and Behavioral Sciences, 401 Quarry Road, Stanford, CA 94305. TeL: 650-723-5473; FAX: 650-7235531
Daniel Le Grange, Department of Psychiatry, UCSF
W. Stewart Agras, Department of Psychiatry, Stanford University.
Kathleen Kara Fitzpatrick, Department of Psychiatry, Stanford University
Booil Jo, Department of Psychiatry, Stanford University
Erin Accurso, Department of Psychiatry, UCSF
Sarah Forsberg, Department of Psychiatry, Stanford University
Kristen Anderson, Department of Psychiatry& Behavioral Neuroscience, The University of Chicago
Kate Arnow, Department of Psychiatry, Stanford University.
Maya Stainer, Department of Psychiatry& Behavioral Neuroscience, The University of Chicago.
References
- Agras W, Lock J, Brandt H, Bryson S, Dodge E, Halmi K, Woodside BA. Comparison of 2 family therapies for adolescent anorexia nervosa: A randomized parallel trial. JAMA Psychiatry. 2014;72:1279–1286. doi: 10.1001/jamapsychiatry.2014.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardone-Cone A, Harney M, Maldonado C, Lawson M, Robinson D, Smith R, Tosh A. Defining recovery from an eating disorder: conceptualization, validation, and examination of psychosocial functioning and psychiatric comorbidity. Behav Res Ther. 2010;48:194–202. doi: 10.1016/j.brat.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Steer R, Garbin M. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psycho Rev. 1988;8:77–100. [Google Scholar]
- Beck AT. Beck Depression Inventory. San Antonio, TX: The Psychological Corporation; 1987. [Google Scholar]
- Byrne C, Accurso E, Arnow K, Lock J, Le Grange D. An exploratory examination of patient and parental self-efficacy in predicting weight gain in adolescents with anorexia nervosa. IJED. 2015 doi: 10.1002/eat22376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper Z, Fairburn CG. The Eating Disorder Examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. IJED. 1987;6:1–8. [Google Scholar]
- Couturier J, Lock J. What is recovery in adolescent anorexia nervosa? IJED. 2006;39:550–555. doi: 10.1002/eat.20309. [DOI] [PubMed] [Google Scholar]
- Darcy A, Bryson S, Agras W, Fitzpatrick K, Le Grange D, Lock J. Do in vivo behaviors predict early response in family-based treatment for adolescent anorexia nervosa. Behav Res Ther. 2013:51. doi: 10.1016/j.brat.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle P, Le Grange D, Loeb K, Celio-Doyle A, Crosby R. Early response to Family-Based Treatment for adolescent anorexia nervosa. IJED. 2010;43:659–662. doi: 10.1002/eat.20764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403–417. 17. [Google Scholar]
- Eisler I, Dare C, Russell GFM, Szmukler GI, Le Grange D, Dodge E. Family and individual therapy in anorexia nervosa: A five-year follow-up. Arch Gen Psychiatry. 1997;54:1025–1030. doi: 10.1001/archpsyc.1997.01830230063008. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick K, Darcy A, Le Grange D, Lock J. In vivo meal training for intial nonresponders. In: Loeb K, Le Grange D, Lock J, editors. Family therapy for adolescent eating and weight disorders: New applications. New York, New York: Routledge; 2015. pp. 45–58. [Google Scholar]
- Golden N, Katzman D, Kreipe R, Stevens S, Sawyer S, Rees J, Rome E. Eating disorders in adolescents: position paper of the Society for Adolescent Medicine: Medical Indications for Hospitalization in an Adolescent with an Eating Disorder. J Adolesc Health. 2003;33:496–503. doi: 10.1016/s1054-139x(03)00326-4. [DOI] [PubMed] [Google Scholar]
- Goodman W, et al. The Yale-Brown Obsessive Compulsive Scale (Y-BOCS) 1: development, use, and reliability. Arch Gen Psychiatry. 1989a:46. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Goodman W, et al. The Yale-Brown Obsessive Compulsive Scale (Y-BOCS) 2: validity. Arch Gen Psychiatry. 1989b;46:1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmhaher B, Brent D, Rao U, Flynn C, Moreci P, Ryan N. Schedule for affective disorders and schizophrenia for school-age children--present and lifetime version (KSADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Accurso E, Lock J, Agras W, Bryson S. Early weight gain predicts outcome in two treatments for adolescent anorexia nervosa. IJED. 2014;47:124–129. doi: 10.1002/eat.22221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Lock J, Accurso E, Darcy A, Forsberg S, Bryson S. Relapse from remission at two to four year follow-up in two treatments of adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry. 2014;53:1162–1167. doi: 10.1016/j.jaac.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J. An update on evidence-based psychosocial treatments for eating disorders in children and adolescents. J Clin Child Adolesc Psychology. 2015 doi: 10.1080/15374416.2014.971458. [DOI] [PubMed] [Google Scholar]
- Lock J, Agras WS, Bryson S, Kraemer H. A comparison of short- and long-term family therapy for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry. 2005;44:632–639. doi: 10.1097/01.chi.0000161647.82775.0a. [DOI] [PubMed] [Google Scholar]
- Lock J, Brandt H, Woodside B, Agras W, Halmi K, Johnson C, Wilfley D. Challenges in conducting a multi-site randomized clinical trial comparing treatments for anorexia nervosa. IJED. 2012;45:202–213. doi: 10.1002/eat.20923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J, Couturier J, Agras WS. Comparison of long term outcomes in adolescents with anorexia nervosa treated with family therapy. J Am Acad Child Adolesc Psychiatry. 2006;45:666–672. doi: 10.1097/01.chi.0000215152.61400.ca. [DOI] [PubMed] [Google Scholar]
- Lock J, Couturier J, Bryson S, Agras WS. Predictors of dropout and remission in family therapy for adolescent anorexia nervosa in a randomized clinical trial. Int J Eat Disord. 2006;39:639–647. doi: 10.1002/eat.20328. [DOI] [PubMed] [Google Scholar]
- Lock J, Le Grange D. Treatment Manual for Anorexia Nervos: A Family-Based Approach. 2. New York: Guilford Press; 2013. [Google Scholar]
- Lock J, Le Grange D, Agras WS, Moye A, Bryson S, Jo B. A randomized clinical trial comparing family based treatment to adolescent focused individual therapy for adolescents with anorexia nervosa. Arch Gen Psychiatry. 2010;67:1025–1032. doi: 10.1001/archgenpsychiatry.2010.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luborsky L. Principles of psychoanalytic psychotherapy. New York: Basic Books; 1984. [Google Scholar]
- Madden S, Miskovic-Wheatley J, Wallis A, Kohn M, Hay P, Touys S. Early weight gain in family based treatment predicts weight gain and remission at end of treatment and remission at 12-m month follow-up for adolescent anorexia nervosa. IJED. 2015 doi: 10.1002/eat22414. [DOI] [PubMed] [Google Scholar]
- Mazure S, Halmi CA, Sunday S, Romano S, Einhorn A. The Yale-Brown-Cornell Eating Disorder Scales: Development, use, reliability, and validity. J Psychiatr Res. 1994;28:425–445. doi: 10.1016/0022-3956(94)90002-7. [DOI] [PubMed] [Google Scholar]
- McMahon F, Insel T. Pharmacogenetics and personalized medicine in neuropsychiatry. Neuron. 2012;74:773–776. doi: 10.1016/j.neuron.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes P, Baillie A, Brown J, Madden S. Parental efficacy in the family-based treatment of anorexia: preliminary development of the Parents Versus Anorexia Scale (PVA) Eur Eat Disord Rev. 2005;13:399–405. [Google Scholar]
- Rosenberg M. Conceiving the Self. New York: Basic Books; 1979. [Google Scholar]
- Scahill L, Riddle M, McSwiggin-Hardin M, Ort S, King R, Goodman W, Leckman J. Children’s Yale-Brown Obsessive Compulsive Scale: Reliability and Validity. J Am Acad Child Adolesc Psychiatry. 1997;36:844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- Touyz S, Le Grange D, Hay P, Smith R, Maguire S, Bamford B, Crosby R. Treating severe and enduring anorexia nervosa: a randomized controlled trial. Psychol Med. 2013;43:2501–2511. doi: 10.1017/S0033291713000949. [DOI] [PubMed] [Google Scholar]
- Treasure J, Russell G. The case for early intervention in anorexia nervosa: theoretical exploration of maintaining factors. Br J Psychiatry. 2011;199:5–7. doi: 10.1192/bjp.bp.110.087585. [DOI] [PubMed] [Google Scholar]
- White H, Haycraft E, Madden S, Rhodes P, Miskovic-Wheatly J, Wallis A, Meyer C. How do parents of adolescent patients with anorexia nervosa interact with their child at mealtiems? A study of parental strategies used in the family meal session of Family-Based Treatment. IJED. 2015;48:72–80. doi: 10.1002/eat.22328. [DOI] [PubMed] [Google Scholar]