Abstract
Objective
Although direct-to-consumer (DTC) marketing of pharmacologic interventions is effective and common, similar approaches have yet to be evaluated in the promotion of psychological treatments (PTs). This is the first randomized controlled trial evaluating the potential of DTC marketing of PTs.
Method
Participants (N=344; 75.0% female, mean age=18.6, 48.5% non-Hispanic Caucasian) were randomly assigned to consume one of four extended commercial campaigns embedded within unrelated programming across 3 weeks. The four campaign conditions were: [1] PT campaign; [2] PT informing about Medication Side Effects campaign; [3] Medication campaign; and [4] Neutral campaign. Attitudes about and intention to seek psychological treatment were assessed prior to campaign exposure (T1), 1 week following the final week of campaign exposure (T2), and at a 3-month follow-up evaluation (T3).
Results
The percentage of participants who newly intended psychological treatment at T2 or T3 differed by condition, with those assigned to the PT campaign slightly more likely to have intended to receive psychological treatment at T2 or T3 than those in other conditions. Baseline reports of emotional symptoms moderated the effect of condition on attitudes toward PT and perceived likelihood of seeking treatment in the future.
Conclusions
Findings support the preliminary utility of DTC marketing of psychological treatments. Increasing consumer knowledge of PTs may be a worthwhile complement to current dissemination and implementation efforts aimed at promoting the uptake of PTs in mental health care.
Keywords: dissemination, direct-to-consumer marketing, psychotherapy, psychological treatment
Despite the high prevalence and burdens associated with mental disorders, most affected individuals do not receive treatment (Kessler et al., 2005) and those who do, show long delays between disorder onset and service utilization (Wang et al., 2005). Consensus guidelines emphasize the important role of psychological treatments (PTs) in the management of mental disorders, but in recent years psychological treatments have assumed a less prominent role in outpatient mental health care (Olfson & Marcus, 2010).
To some extent, the diminishing role of PTs in mental health care may reflect an underinformed general population of individuals with mental disorders who are unaware of important advances in psychological intervention science. To date, the most common strategy for promoting the increased use of quality PTs for affected individuals has been to target providers with dissemination and implementation efforts (McHugh & Barlow, 2010). Dissemination and implementation efforts should involve many stakeholders, including consumers, who have their own goals and priorities for mental health services (Proctor et al., 2011). Although traditional dissemination and implementation efforts hold enormous promise for improving the quality of mental health care, these efforts do not address patient-level barriers such as consumer awareness of or negative attitudes about services, and accordingly do little to improve rates of PT utilization.
Whereas systematic efforts to date promoting the uptake of PTs have focused almost exclusively “top-down” on increasing provider knowledge and skill, efforts to promote pharmacologic treatments have—in addition to provider-focused dissemination—additionally featured “bottom-up” direct-to-consumer (DTC) marketing. In the context of pervasive advertisements for psychopharmacological interventions, consumers are saturated with information about the potential utility of medications in the treatment of mental disorders without comparable information about the benefits of PTs. While there are differences between the marketing of pharmacological interventions (which are tangible products) and PTs (which are less tangible services), given the success of DTC marketing efforts in the pharmaceutical industry, and given that consumers are often choosing between PTs and/or medication, corresponding DTC marketing of PTs may help to promote initial treatment-seeking behavior and to direct more treatment-seeking individuals toward PTs.
Research to date has yet to systematically examine the potential impact of DTC marketing, although the strategy of DTC for PT promotion has been suggested in the literature (Gallo, Comer, & Barlow, 2013). The present study evaluated via a randomized controlled design the preliminary utility of DTC advertising of PTs by having participants indirectly experience 1 of 4 different commercial campaigns across a 3-week period. Randomly assigned commercial campaigns systematically differed in treatment-related content. Treatment-related attitudes and intentions were prospectively assessed 3 times: prior to campaign exposure, 1 week following the final week of campaign exposure, and at a 3-month follow-up evaluation. It was hypothesized that each of the campaigns highlighting the benefits of PT, relative to a medication-oriented campaign and to a neutral campaign would be associated with increased (a) intentions to pursue PTs, (b) likelihood to pursue PT if one developed emotional problems, and (c) perceptions of PT effectiveness. We hypothesized that elevated emotional symptoms at baseline would be associated with greater campaign effects; mental health campaigns are more relevant to individuals with emotional problems, which may result in increased attention during viewing, which in turn may cause higher “dosages” of campaign consumption.
Method
Participants
The sample consisted of 344 undergraduate psychology students across two universities (MAge =18.56; SD=2.79; 75% female), and 38.2% of the sample reported a family income of below $50,000, 33.9% of $50,001-$100,000, and 27.9% of above $100,000. In addition, 11.3% of the sample self-reported a past or present diagnosis of a mental disorder.
Procedure
All study procedures were conducted in accordance with and under the approval of the [redacted] Institutional Review Board and the [redacted] Research Ethics Board. Participants were recruited from undergraduate psychology courses at 1 of 2 large urban universities and were informed that the study was examining media consumption. After obtaining informed consent, participants were randomly assigned to view 1 of 4 3-week commercial campaigns via the Internet across 3 weekly viewing sessions. To enhance external validity and make campaigns similar to real-world DTC marketing campaigns, within each campaign each viewing session consisted of 3 related but different 30-second target commercials embedded within unrelated content (i.e., other commercials and a television episode).
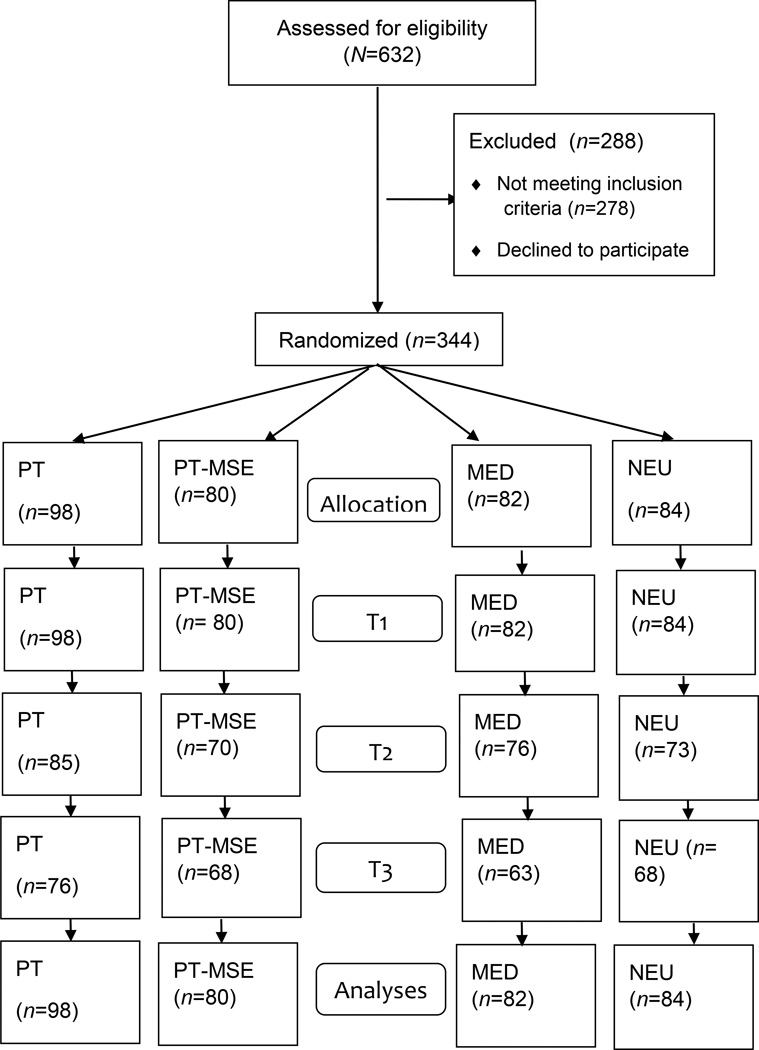
Participants were randomly assigned to view either the: [1] PT campaign (e.g., the “Psychotherapy can help” campaign); [2] PT informing about medication side effects campaign (PT-MSE; e.g., the “Psychotherapy works without side effects” campaign); [3] medication campaign (MED; e.g., “many medications can help you feel better”); or [4] neutral campaign, consisting of commercials unrelated to mental health [NEU]. The 4 campaigns were equal in length. Eighty-four (24.4%) of the participants were assigned to the NEU condition, 82 (23.8%) to the MED condition, 98 (28.5%) to the PT condition, and 80 (23.3%) to the PT-MSE condition. See Figure 1 for data regarding participant randomization and retention. All 4 groups of participants viewed the video campaigns, embedded within unrelated content, via the Internet 3 times (once per week for 3 weeks), for a total of 4.5 minutes of target DTC/control content embedded within 90 minutes of unrelated content across the 3-week study period. Examples of commercials from the campaigns can be found at http://youtu.be/R_V5kx1r0ug. Data were collected prior to campaign exposure (T1), 1 week following the final viewing session (T2), and 3 months after the final viewing session (T3). DTC advertisements were all 30 seconds long.
Figure 1.
Summary of Linear Regression Analysis Examining Moderating Role of Emotional Symptoms when Predicting Changes in Reported Likelihood of Seeking PT if Needed
Measures
Demographic information
Data on demographics were collected via self-report at T1.
Intention to seek treatment, and attitudes about PTs
Rates of intended action to seek treatment and attitudes about PTs were measured at T1, T2, and T3 using a self-report measure adapted from the National Comorbidity Survey Replication (http://www.hcp.med.harvard.edu/ncs/replication.php). Specifically, participants were asked about (a) current intentions to seek PT (yes/no), (b) their expectation to seek PT if they were to experience a serious emotional problem (yes/no), and (c) the percent of people they believed to be helped by PT (“Of the people who get psychotherapy for serious emotional problems, what percent do you think are helped?” (1) 0–25%, (2) 26–50%, (3) 51–75%, (4) 76–100%).
Symptoms of emotional disorders
Symptoms of emotional disorders were measured at T1, T2, and T3 using the Depression Anxiety Stress Scales total score (DASS), a 42-item questionnaire that assesses negative emotions (i.e., depression, anxiety, and stress; Lovibond & Lovibond, 1995) and has shown good reliability and validity (Antony, Bieling, Cox, Enns, & Swinson, 1998). Internal consistency in the present sample was good (Cronbach’s α=0.76).
Results
To examine changes over time across conditions, analyses of covariance (ANCOVAs) examining postcampaign data as dependent variables (DVs) across conditions after controlling for T1 data were conducted (Rausch, Maxwell, & Kelley, 2003). Significant omnibus tests were followed-up with Bonferonni-adjusted contrasts. For categorical variables, chi-square tests examined associations between campaign condition and status of the categorical variable (i.e., moved in the hypothesized direction or not) following campaign/control consumption.
Hierarchical linear regressions (for continuous DVs) and logistic regressions (for categorical DVs) were performed to examine the hypothesized moderation effect. The model consisted of 2 predictor steps: the main effects [campaign condition and emotional symptoms (centered)] were simultaneously entered in Step 1, and the main effects and the interaction term [main effects and product term of emotional symptoms X condition] were simultaneously entered into Step 2 (Baron & Kenny, 1986). Posthoc probing tests were conducted for significant interactions to reveal the nature of the interaction.
Randomization check
Chi-square tests and one way analyses of variance indicated that participants did not differ across conditions on gender, χ2 (3, N = 342) = 2.82, p =.42, family income, F(3, 326) = 0.89, p = .45, age, F(3, 339) = 0.29, p =.84, baseline self-report of past or present mental disorder diagnosis, χ2 (3, N =343) = 6.94, p =0.07, and emotional symptoms F(3, 339) = 0.40, p =.76.
Effects of campaign assignment on intended PT seeking
Table 1 presents the frequencies of participants who intended to seek PT at T1-T3, by study condition. The percentage of participants who newly intended PT following campaign exposure differed by condition, with those in the PT condition slightly more likely to intend to receive PT at T2 or T3 than those in the other three conditions, demonstrating a small effect. χ2(3, N = 309) = 4.20, p = .04.
Table 1.
Frequencies of Intended and Actual Treatment Seeking Behavior across Conditions
| Condition | T1 | T2 | T3 | ||||
|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | ||
| Ever Received PT |
Overall (N=344) | 108 (31.6%) | 234 (68.4%) | 90 (29.7%) | 213 (70.3%) | 77 (28.6%) | 192 (71.4%) |
| NEU (n=84) | 31 (37.3%) | 52 (62.7%) | 24 (33.8%) | 47 (66.2%) | 25 (37.3%) | 42 (62.7%) | |
| MED (n =82) | 20 (24.7%) | 61 (75.3%) | 23 (30.3%) | 53 (69.7%) | 14 (23.7%) | 45 (76.3%) | |
| PT (n =98) | 32 (32.7%) | 66 (67.3%) | 21 (24.7%) | 64 (75.3%) | 19 (25.0%) | 57 (75.0%) | |
| PT-MSE (n =80) | 25 (31.3%) | 55 (68.8%) | 22 (31.0%) | 49 (69.0%) | 19 (28.4%) | 48 (71.6%) | |
| Intention to seek PT |
Overall (N=344) | 18 (6.4%) | 264 (93.6%) | 13 (5.5%) | 224 (94.5%) | 11 (5.2%) | 199 (94.8%) |
| NEU (n =84) | 9 (13.0%) | 60 (87.0%) | 5 (8.6%) | 53 (91.4%) | 2 (4.1%) | 47 (95.9%) | |
| MED (n =82) | 4 (5.6%) | 67 (94.4%) | 2 (3.4%) | 57 (96.6%) | 2 (4.0%) | 48 (96.0%) | |
| PT (n =98) | 1 (1.3%) | 76 (98.7%) | 3 (4.7%) | 61 (95.3%) | 4 (6.8%) | 55 (93.2%) | |
| PT-MSE (n =80) | 4 (6.2%) | 61 (93.8%) | 3 (5.4%) | 53 (94.6%) | 3 (5.8%) | 49 (94.2%) | |
Note. T1 = prior to campaign exposure; T2 = 1 week following the final week of campaign exposure; T3 = at a 3-month follow-up evaluation; NEU = Neutral campaign; MED = Medication campaign; PT = Psychological treatment campaign; PT-MSE = Psychological treatment informing about medication side effects campaign.
Effects of campaign assignment on perceived likelihood of seeking PT in the future
ANCOVA using condition as a between-subjects variable and baseline perceived likelihood of seeking PT if presented with an emotional problem as a covariate revealed no overall differences across conditions in participants’ reported postcampaign likelihood to seek PT if needed at T2, F(4, 304) = 0.86, p=.46, or T3, F(4, 274) = 2.12, p=.098. Emotional symptoms at baseline were examined as a proposed moderator of T1-T2 and T1-T3 changes in reported likelihood of obtaining PT if one developed an emotional problem in the future. To predict T2 likelihood of seeking PT if one developed an emotional problem, the main effects of condition assignment (dummy coded) and DASS total score were entered as independent variable main effects, F(4, 304) = 0.44, p = n.s. Next interaction terms for condition assignment dummy codes and emotional symptoms were calculated and added to step two of the regression. Entering the interaction terms did not add a significant contribution to the prediction of T2 likelihood of obtaining PT if emotional problems developed, FChange(3, 297) = 1.36, p =n.s. To predict T3 likelihood of seeking PT if one developed an emotional problem, the main effects of condition assignment (dummy coded) and DASS total score were entered as independent variable main effects, F(4, 228) = 1.20, p = n.s. Next, interaction terms for condition assignment dummy codes and emotional symptoms were calculated and added to step two of the regression. Entering the interaction terms added a significant contribution to the prediction of T3 likelihood of obtaining PT if emotional problems developed, FChange(3, 221) = 3.76, p = .01, accounting for an additional 6.9% of variance over the nonsignificant main effects included in the first step (ΔR2 = .069). Specifically, PT-MSE participants with lower DASS scores reported a significantly increased likelihood at T3 to seek PT in the future if an emotional problem presented, whereas those with higher DASS scores assigned to PT-MSE reported a decreased likelihood at T3 of seeking PT in the future if an emotional problem presented. Emotional symptoms did not moderate T3 effects for the other three conditions.
Effect of campaign assignment on perceived PT effectiveness
ANCOVA using condition as a between-subjects variable and baseline perceived PT effectiveness as a covariate revealed no overall differences across conditions in participants’ reported beliefs regarding the helpfulness of PTs at T2, F(4, 299) = 0.64 p=.59, or T3, F(4, 271) = 1.35 p=.26 (see Table 2).
Table 2.
Perceived Effectiveness of Psychological Treatments Across Condition
| T1 | T2 | T3 | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Perceived PT Effectiveness |
Overall | 2.60 | 0.74 | 2.63 | 0.83 | 2.66 | 0.75 |
| NEU | 2.69 | 0.75 | 2.71 | 0.75 | 2.70 | 0.72 | |
| MED | 2.54 | 0.77 | 2.58 | 0.88 | 2.67 | 0.70 | |
| PT | 2.55 | 0.71 | 2.54 | 0.79 | 2.52 | 0.83 | |
| PT-MSE | 2.63 | 0.72 | 2.73 | 0.88 | 2.78 | 0.73 | |
Note: Values reflect mean responses to the following question: “Of the people who get psychotherapy for serious emotional problems, what percent do you think are helped?” (1) 0–25%, (2) 26–50%, (3) 51–75%, (4) 76–100%. T1 = prior to campaign exposure; T2 = 1 week following the final week of campaign exposure; T3 = at a 3-month follow-up evaluation; NEU = Neutral campaign; MED = Medication campaign; PT = Psychological treatment campaign; PT-MSE = Psychological treatment informing about medication side effects campaign.
Discussion
Whereas DTC marketing strategies have been shown to be enormously effective in the promotion of pharmaceutical products, to our knowledge the present findings offer the first preliminary experimental evidence of the potential utility of DTC marketing strategies for promoting PTs. In the context of a randomized trial, exposure to a consumer-focused campaign highlighting the potential benefits of PTs was associated with slightly increased reports of intention to seek PT. Among individuals with lower current emotional symptoms, exposure to a consumer-focused campaign highlighting the potential benefits of PTs that also addressed medication side effects not linked with PTs was associated with increased self-reports of future likelihood to seek PT. At a time when we are simultaneously witnessing the greatest accumulated empirical support for psychological treatments, as well as a diminishing role of psychological treatments in mental health care (Olfson & Marcus, 2010), the present findings provide encouraging preliminary evidence that DTC marketing efforts may offer a useful tool with which to promote PTs.
Interestingly, whereas PT participants showed significantly greater intention to seek PT after campaign consumption, PT-MSE participants did not. It is possible that PT advertisements were more straightforward than PT-MSE advertisements, and that the relatively clearer message of PT advertisements more effectively resulted in intention to seek PTs. Such an explanation would be in line with the “information overload” hypothesis (Reutskaja & Hogarth, 2009), which posits that increased complexity of presented options increases cognitive efforts needed to make choices, which in turn constrains decision-making and/or reduces satisfaction with one’s choices. At the same time, among participants with relatively lower compared to higher current emotional symptoms, PT-MSE—but not PT—exposure was associated with increased perceived likelihood of seeking treatment in the future should emotional problems develop. Indeed, PT campaigns may be more broadly effective in persuading individuals to intend to seek current care for their problems regardless of current symptoms, but when an individual does not currently have symptoms PT-MSE may be relatively more effective in getting people to entertain future PT in the event that they were to develop emotional symptoms in the future. Importantly, a common critique of pharmaceutical advertisements is that they are particularly effective at reaching people with relatively low intervention needs (Lyles, 2002). The present finding that the largest increases among PT-MSE participants were in perceived likelihood to seek PT in the future if an emotional problem developed may reflect this concern. Additionally, participants with higher current emotional symptoms may have been more likely to have previous experience with psychopharmaceutical interventions, which could have led to this differential response.
Given the absence of large centralized profits from psychological treatment use that could be in turn reinvested into marketing efforts, and given the lack of an infrastructure for marketing public health interventions (Kreuter & Bernhardt, 2009), dollar-for-dollar matching of the pharmaceutical industry’s vast financial resources for marketing is not feasible. Nonetheless, increased funding for DTC advertising of PTs may offer an important complement to current PT dissemination and implementation efforts. This presents a challenge to secure resources to finance such efforts. Amidst the changing health care climate in the United States, increasing rates of efficacious, cost-effective treatments such as PTs should appeal to healthcare policymakers. While the pharmaceutical industry’s influence on Capitol Hill has been well documented, efforts should also be made to inform policymakers about PTs’ clinical utility and cost-effectiveness. A public educational campaign funded with government resources could be a powerful way to direct people who need mental health treatments to appropriate care.
Advertisements in the pharmaceutical industry create selective demand (i.e., for a specific drug) rather than primary demand, (i.e., for psychotropic drugs as a whole). It would be prudent for DTC advertisements for PTs to consider this approach as well (e.g., educating about specific treatments, and not just psychotherapy broadly), so that consumers know exactly what treatments may be used for which disorders. The pharmaceutical industry has also, in one of their most profitable practices, utilized medication samples. Providers of PTs might consider whether this could be an ethical and useful practice to increase initial PT utilization as well, for example, by leveraging online resources (e.g., video hosting websites) to describe ones therapeutic techniques or to showcase a sample therapy session. Product placement (e.g., in television shows) and targeted advertisements (e.g., via Internet search engines) might also offer useful vehicles for DTC PT promotion efforts. As the pharmaceutical industry has demonstrated, frequent, simple, targeted messages (“ask your doctor about…”) can change behavior.
Limitations
Although the intention of the study was not made clear to participants, measures were all face-valid self-report measures, and the same measures were administered across time points, which may have led to practice effects. Also, we used single item measures, which may be less reliable than multi-item measures, possibly leading to extreme responses or leading respondents to display a social desirability bias. Single-item measures can also reduce clarity about whether participants understood the question.
The sample was comprised of undergraduate psychology students (the majority of whom were female), which is not fully representative of broader unselected community populations. Additionally, psychology students may be savvier about treatments for mental disorders than the general population. Future studies should examine a clinical sample as well as parents of youth who need mental health treatments. Concerns related to the clinical make-up of college students, however, are somewhat tempered by research showing that the rate of psychological disorders is no different among college-attending individuals and their non-college-attending peers (Blanco et al., 2008). Finally, as a preliminary investigation, the advertisements in the present study were developed on a small budget, perhaps negatively affecting their external validity and/or impact.
Public Health Significance Statement.
This is the first randomized controlled trial evaluating the potential utility of direct-to-consumer marketing of psychological treatments. This study demonstrated that increasing consumer knowledge of psychological treatments may be a worthwhile complement to current dissemination and implementation efforts, which frequently target providers.
Acknowledgments
This work was supported by the Clara Mayo Memorial Fellowship Award, by the Association of Behavioral and Cognitive Therapies Virginia A. Roswell Dissertation Award, and by the National Institute of Mental Health [K23 MH090247].
Contributor Information
Kaitlin P. Gallo, Email: kgallo@post.harvard.edu.
Jonathan S. Comer, Email: jocomer@fiu.edu.
David H. Barlow, Email: dhbarlow@bu.edu.
Roberta N. Clarke, Email: rclarke@bu.edu.
Martin M. Antony, Email: mantony@psych.ryerson.ca.
References
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10:176–181. [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu S-M, Olfson M. Mental health of college students and their non-college-attending peers: results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry. 2008;65:1429. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo KP, Comer JS, Barlow DH. Direct-to-consumer marketing of psychological treatments for anxiety disorders. Journal of Anxiety Disorders. 2013;27:793–801. doi: 10.1016/j.janxdis.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, Zaslavsky AM. Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter MW, Bernhardt JM. Reframing the dissemination challenge: a marketing and distribution perspective. American Journal of Public Health. 2009;99:2123. doi: 10.2105/AJPH.2008.155218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Lyles A. Direct marketing of pharmaceuticals to consumers. Annual Review of Public Health. 2002;23:73. doi: 10.1146/annurev.publhealth.23.100901.140537. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Barlow DH. The dissemination and implementation of evidence-based psychological treatments: A review of current efforts. American Psychologist. 2010;65:73–84. doi: 10.1037/a0018121. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC. National trends in outpatient psychotherapy. The American Journal of Psychiatry. 2010;167:1456–1463. doi: 10.1176/appi.ajp.2010.10040570. [DOI] [PubMed] [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Hensley M. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research. 2011;38:65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rausch JR, Maxwell SE, Kelley K. Analytic methods for questions pertaining to a randomized pretest, posttest, follow-up design. Journal of Clinical Child and Adolescent Psychology. 2003;32:467–486. doi: 10.1207/S15374424JCCP3203_15. [DOI] [PubMed] [Google Scholar]
- Reutskaja E, Hogarth RM. Satisfaction in choice as a function of the number of alternatives: When 'goods satiate'. Psychology & Marketing. 2009;26:197–203. [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]