Abstract
Objective
To evaluate the feasibility and acceptability of a school-based intervention for diverse children exposed to a range of traumatic events, and to examine its effectiveness in improving symptoms of posttraumatic stress, depression, and anxiety.
Method
Participants were 74 school children (grades 1-5) and their primary caregivers. All participating students endorsed clinically significant posttraumatic stress symptoms. School clinicians were trained to deliver Bounce Back, a 10-session cognitive-behavioral group intervention. Children were randomized to Immediate or Delayed (3-month waitlist) Intervention. Parent- and child-report of posttraumatic stress and depression, and child report of anxiety symptoms, were assessed at baseline, 3 months, and 6 months.
Results
Bounce Back was implemented with excellent clinician fidelity. Compared to children in the Delayed condition, children who received Bounce Back immediately demonstrated significantly greater improvements in parent- and child-reported posttraumatic stress and child-reported anxiety symptoms over the 3-month intervention. Upon receipt of the intervention, the Delayed intervention group demonstrated significant improvements in parent- and child-reported posttraumatic stress, depression, and anxiety symptoms. The Immediate treatment group maintained or showed continued gains in all symptom domains over the 3-month follow-up period (6 month assessment).
Conclusions
Findings support the feasibility, acceptability, and effectiveness of the Bounce Back intervention as delivered by school-based clinicians for children with traumatic stress. Implications are discussed.
Keywords: child, traumatic stress, school, intervention
Prevalence of Traumatic Experiences
Prevalence rates of traumatic events among children and youth are striking. Approximately 60-70% of youth are exposed to traumatic events by age 17 (Briggs-Gowan et al., 2010; Copeland, Keeler, Angold, & Costello, 2007; Finkelhor, Turner, Ormrod, Hamby, & Kracke, 2009). Early school-age children are also affected. Approximately 40% of 8-11-year-old Latino children in an inner-city elementary school reported having their life threatened, a rate similar to their middle school counterparts (Stein, Jaycox, Kataoka, Rhodes, & Vestal, 2003). Moreover, children in vulnerable populations, including lower income inner city youth and immigrants, are often exposed to multiple traumatic events and secondary adversities (Jaycox et al., 2010; Osofsky, 2004).
Impact of Trauma
The range of negative psychological sequelae of trauma exposure in children is well-documented. While a relatively small percentage of youth develop posttraumatic stress disorder (PTSD), untreated subclinical PTSD symptoms pose significant risk for the development of other mental health disorders (Copeland et al., 2007), and a substantial portion of youth subsequently develop significant symptoms of depression, anxiety, and disruptive behaviors (Freeman, Mokros, & Poznanski, 1993; Kliewer, Lepore, Oskin, & Johnson, 1998; Lonigan, Shannon, Finch, & Daugherty, 1991; Lynch & Cicchetti, 1998). Exposure to multiple traumatic events further increases the risk of traumatic stress and depressive symptoms (Suliman et al., 2009). In addition to psychological symptoms, exposure to traumatic events is linked to impaired academic functioning (Hurt, Malmud, Brodsky, & Giannetta, 2001; Schwab-Stone et al., 1995) including decreased reading ability (Delaney-Black et al., 2002); lower grade-point average (GPA) (Hurt et al., 2001); more days of school absence (Hurt et al., 2001); and decreased high school graduation rates (Grogger, 1997). These findings clearly highlight the need for effective interventions for children exposed to traumatic events, with attention to a range of psychological and functional outcomes.
Evidence-based Interventions for Child Traumatic Stress
Recently, research examining interventions for child traumatic stress has increased (see recent reviews: Dorsey, Briggs, & Woods, 2011; Foa, Keane, Friedman, & Cohen, 2009). Treatments with the strongest evidence base have utilized cognitive behavioral approaches, including psychoeducation, relaxation, cognitive coping, systematic desensitization, trauma narrative, and parental involvement in supporting the youth. To date, only trauma-focused cognitive behavioral therapy (TF-CBT) (Silverman et al., 2008) meets criteria for a well-established (Cohen & Mannarino, 2008) psychosocial treatment and has demonstrated efficacy across several randomized controlled trials (RCTs) for use with youth ages 7-17 (for review, see Silverman et al., 2008). A second program, Cognitive Behavioral Intervention for Trauma in the Schools (CBITS; Stein, Jaycox, Kataoka, Wong, Tu, Elliot, et al., 2003), is a group treatment delivered by school clinicians in the school setting. CBITS meets criteria for probably efficacious as it has only been tested in one RCT, one field trial (Jaycox et al., 2010), and one quasi-experimental design in a school setting (Kataoka et al., 2003). Nevertheless, CBITS has demonstrated great promise in terms of effectiveness and access to underserved youth with posttraumatic stress (Jaycox et al., 2010).
Relevance of School-based Services for Child Trauma
While the use of TF-CBT in mental health clinic settings is well-supported, it has not been evaluated in a school setting. Given practical and psychological barriers associated with attending mental health clinics (Kazdin, Holland, & Crowley, 1997; McKay & Bannon, 2004), access to and engagement in TF-CBT may be limited for many families. Notably, of children who access mental health services, three-fourths receive care through the education sector (Farmer, Stangl, Burns, Costello, & Angold, 1999), highlighting the public health utility of providing mental health services in school settings. In a study following Hurricane Katrina, students with trauma-related symptoms were randomized to clinic-based TF-CBT or school-based CBITS. The two interventions were similarly effective among treatment completers; however, there were significant differences in engagement and retention. Only 12% of those assigned to TF-CBT completed treatment, compared to 93% of those assigned to CBITS (Jaycox et al., 2010). This underscores the potential benefits of quality school-based programs in improving access and positively impacting a large portion of youth.
School-based group interventions are cost-effective and a good match for school mental health clinicians who are able to serve more students in need; it would not be feasible for such clinicians to work with each student individually within the school day given their competing responsibilities. Programs like CBITS also require less parental involvement than is typically required in TF-CBT, which can be a critical issue for underserved families facing obstacles such as multiple work schedules, transportation, and competing stressors. The group venue also provides a unique opportunity for children to recognize that they are not alone in having been through difficult experiences, adding essential elements of normalization and validation of symptoms, impact, and peer support. Notably, while CBITS has produced favorable results in school settings, the treatment was designed for adolescents ages 11 and older. Given important developmental differences between children and adolescents with regard to cognitive, interpersonal, and emotional functioning, there is currently little to recommend for elementary-aged children in school settings.
Integration of TF-CBT and CBITS
Given the existence of two evidence-based interventions for youth with posttraumatic stress, the Bounce Back Intervention was developed with the goal of integrating elements from each to optimize child outcomes. The first author consulted with a panel of national experts, including the developers of TF-CBT (J. Cohen) and CBITS (L. Jaycox) and experts in the areas of school mental health, randomized clinical trial with ethnically diverse youth, and child anxiety treatment. The development process also included regular meetings with community mental health partners, including school-based clinicians and their supervisors from community mental health agencies and the school district. Finally, Bounce Back and its implementation plan were designed based on feedback from stakeholders, including both English and Spanish-speaking parent focus groups and educator focus groups (Langley, DeCarlo Santiago, Rodriguez, & Zelaya, 2013).
Feedback from these processes suggested that a successful intervention would include: 1) a group format to maximize efficiency and enable providers to reach more children in need; 2) inclusion of children with a broad range of traumatic experiences (i.e., not waiting for a shared community or school event), and doing universal screening with limited exclusionary criteria; 3) inviting some targeted parent participation and psychoeducation, but not requiring regular parent involvement due to limited availability of many working parents; and 4) having the groups be skills-based and only working on/sharing traumatic event in one-on-one sessions with the clinician – also deemed the most developmentally appropriate way of managing potential issues of confidentiality in groups with children. To address these needs, the Bounce Back intervention follows a similar school-based group format of CBITS, while including increased parental involvement in the individual trauma narrative process as in TF-CBT which is appropriate for younger school children. These two interventions share many of the core skills (e.g., psychoeducation, relaxation, cognitive coping, exposure to avoided stimuli) which are likewise included in Bounce Back.
Current Study
The aim of the current study was to address existing gaps in the childhood trauma intervention literature by combining elements of these two successful interventions (e.g., youth group-based format in CBITS, parental involvement in individual sessions in TF-CBT). Specifically, we developed and evaluated an intervention, Bounce Back, to be used in K-5 elementary school settings to serve children from diverse backgrounds who have been exposed to a range of traumatic events and endorse clinically significant symptoms of traumatic stress. We sought to evaluate the feasibility and acceptability of Bounce Back and to assess its effectiveness compared to a delayed treatment group (waitlist control). We anticipated that Bounce Back would be implemented by school-based clinicians with an acceptable degree of fidelity to the treatment manual and that parents and children would endorse high levels of satisfaction with the intervention. In addition, we hypothesized that children who received Bounce Back immediately would demonstrate significantly greater symptom reductions at 3-month assessment (post-intervention) than children assigned to delayed receipt of Bounce Back. Given the focus of the cognitive behavioral skills included in the intervention and based on previous intervention studies for posttraumatic stress, we expected improvements in three primary domains: posttraumatic stress, anxiety, and depressive symptoms. We further expected that over the 3-6 month follow-up period, the immediate Bounce Back group would maintain their treatment gains, while the delayed intervention group would show significant improvement following receipt of the program. Finally, we planned to explore the effects of Bounce Back on secondary outcomes, including disruptive behavior, social adjustment, emotion regulation, coping efficacy, and functional impairment.
Method
Participants
Children from four elementary schools in Los Angeles County participated in this study during the 2011-2012 and 2012-2013 school years. The schools serve a diverse ethnic and linguistic student body from grades K-5 and qualify as Title I schools under the No Child Left Behind Act of 2001, indicating that at least 40% of the students were eligible for free or reduced lunch. Participants in the analytic sample were 74 students in 1st-5th grade (Mean age: 7.65 years, SD = 1.36; 50% boys) and were ethnically diverse: 49% Latino, 27% Caucasian, 18% African American, 5% biracial, 1% Asian. Nearly one-quarter (24.3%) of families had a highest household education level of less than high school, 20.3% had at least one caregiver who earned a high school degree, and 55.4% had at least one caregiver who had completed at least some college. Nearly half of the participants (43.3%) had a household income of $40,000 or less, supporting an average of four individuals (Mean = 3.81 individuals, SD = 1.15). Although we were unable to obtain demographic details for students whose parents/guardians did not provide consent to be screened, the children who participated in this study reflected the general demographics of their schools.
Recruitment and Screening Procedures
This study was conducted in compliance with the Institutional Review Board at UCLA. A two-stage recruitment and active parental consent process was employed for the (1) screening and (2) intervention procedures. First, a description of the study and screening consent forms were sent home during the first week of school to all students in grades 1-5, in the same packet as all the regular school forms requiring completion and/or signature. Across the four schools, 1,050 forms were sent home over two academic years, with 789 (73%) returned and 417 (53%) of those consenting for their child to be screened. All 417 children assented and were individually screened, and 113 (28%) were eligible for the intervention, meeting the following inclusion criteria: 1) experience of one or more traumatic events, and 2) current symptoms of PTSD indicating moderate or higher levels of symptom severity (score of ≥ 20 on the PTSD Reaction Index) (Steinberg, Brymer, Decker, & Pynoos, 2004). Exclusion criteria were kept to a minimum and included 1) presence of a severe psychiatric disturbance (i.e., acute suicidal behavior, current psychotic symptoms), and 2) sexual abuse as only and primary trauma. The decision to exclude children who reported sexual abuse as a primary trauma was based on consultation with national experts and community stakeholders; given that the Bounce Back intervention is completed in a mixed-gender group format, individual treatment (e.g, TF-CBT) might be a more appropriate modality for individuals with sexual abuse histories. Students who met either of these exclusion criteria were referred for individual mental health treatment through the school.
Second, parents of these eligible children were contacted by research staff, and those interested in having their child participate in Bounce Back met with research staff to complete intervention consent and baseline assessment measures at a single visit. Seventy-four children completed this second step. Participant flow can be seen in Figure 1.
Figure 1.
Participant flow chart
Research staff completed baseline measures with all consented and assented children. The 74 participating children were randomized to receive Bounce Back in the Immediate intervention group or the Delayed group (waitlist control). Randomization was conducted separately within each school and was stratified by grade and gender by the blinded study statistician using a standard table of random assignment (Cochran, 1977, pg. 19). Those assigned to Immediate intervention began the group program within a few weeks, while the Delayed group waited approximately three months without intervention. All participants were re-assessed three months after baseline (after the Immediate group had completed Bounce Back). Following this assessment, the Delayed group received the Bounce Back program while the Immediate group continued without further intervention, and then all participants completed a final assessment at the 6-months post-baseline mark.
Bounce Back Intervention
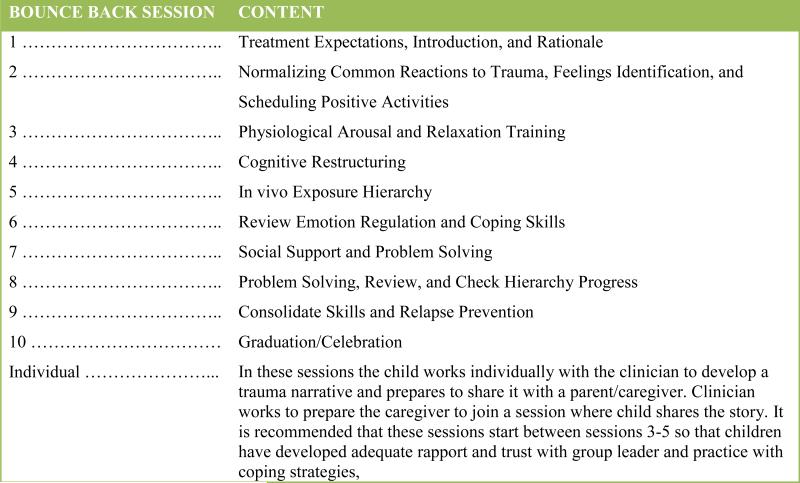
The Bounce Back program consists of 10 group sessions, 2-3 individual sessions, and 1-3 parent education sessions designed to reduce posttraumatic, anxious, and depressive symptoms and to improve functioning in multicultural elementary school students who have been exposed to traumatic events (Langley, A.K., & Jaycox, L.H., 2011; Bounce Back: An Intervention for Elementary School Children Exposed to Traumatic Events.Manuscript in preparation.). Group sessions lasted 50-60 minutes and individual sessions ranged from 30-50 minutes. The intervention incorporates therapeutic elements similar to those used in other CBT interventions for children and youth with PTSD, including psychoeducation, relaxation training, cognitive restructuring, social problem solving, positive activities, and trauma-focused intervention strategies, including gradual approach of anxiety-provoking situations and trauma narrative (Cohen & Mannarino, 2008; Stein et al., 2003). The trauma narrative involves exposure to the memory of the traumatic event via repeated retelling of the trauma story until associated anxiety and fear decrease. However, significant modifications were made to successfully deliver these components to 5-11 year-old students in a group format. These included introducing more foundational elements (e.g., identifying feelings before describing the link between thoughts and feelings), making concepts very concrete (e.g., trauma narratives conveyed through storybooks with pictures created by students, ‘courage cards’ tailored to each student, use of published children's books to introduce certain topics), and creating games and other experiential activities to engage younger students in the skills and strategies. In addition, parents of students in Bounce Back were invited to a one-on-one session with the child and the group leader in order to have the child share their trauma narrative. Ninety seven percent of the students (72 out of 74) had at least one parent attend a one-on-one session. Throughout the program, parents and teachers of participating students received a brief weekly handout (parents) or email (teachers) describing the skill that the child would be learning in group that week. This was based on feedback from key stakeholders who expressed that keeping parents and teachers informed might increase buy-in and engagement (Langley et al., 2013). Session content is outlined in Figure 2.
Figure 2.
Description of Bounce Back session content
Groups included four to six students within one grade year of one another (i.e., 1st and 2nd graders; 3rd and 4th graders) and were run during the school day. Each group session involved setting an agenda; reviewing activity assignments; introducing a new concept through a combination of didactics, games, stories, and experiential activities; and assigning activities for the next group. At each school, two groups were formed (one Immediate and one Delayed) for each of the two academic years. Four schools participated the first year, and three of these four participated the second year, for a total of 14 groups.
Clinician Training, Supervision, and Fidelity
School-based clinicians provided the intervention as part of their job responsibilities. All clinicians were part of the existing school mental health program and were masters level Social Workers or licensed Clinical Psychologists who were employees of local mental health agencies who contracted with the city and school district to have one clinician in each school full time. The first author trained the clinicians in a one-day session. During the first year, clinicians met weekly as a group for consultation with treatment developers. Consultations were reduced to biweekly supervision during the second year.
All Bounce Back sessions were audiotaped and 20% of the tapes (N = 28) were randomly selected to be rated by experienced CBT clinicians for fidelity. Fidelity measures were co-rated by two study staff members (first and second authors, both clinicians) until an inter-rater reliability of 95% was reached. The rest were rated by one of the clinicians. Mean ratings were calculated for (a) session-specific adherence to the treatment manual and (b) session quality. All items were on a 0-3 scale, with 3 representing high adherence or quality.
Measures
Data from students, parents, and teachers were collected at baseline, three months (post-intervention for the Immediate group, post-waitlist for the Delayed group), and six months (i.e., three months post-intervention for the Immediate group, immediate post-intervention for the Delayed group). All of the following measures were administered at all three time points in the study.
Trauma exposure
The Modified Traumatic Events Screening Inventory for Children – Brief Form (TESI-C-Brief) (Ford et al., 2000), child and parent versions, was used at baseline to assess exposure to direct or witnessed trauma via 21 items. Items query a range of traumatic experiences, including accidental trauma (e.g., car accident, injury), physical abuse, violence, loss, and substance abuse. The TESI has been used extensively by the National Child Traumatic Stress Network (SAMHSA) (Edwards & Rogers, 1997) and reviews of instruments to measure history of traumatic events support its strong psychometric properties, including reliabilities of > .80 and interrater reliability ranging from .73-1.00 (e.g., Ribbe, 1996). Endorsement of at least one traumatic event at baseline was required for participation.
Primary outcome measures
The UCLA Posttraumatic Stress Disorder Reaction Index (RI) (Pynoos, Rodriguez, Steinberg, Struber, & Fredrick, 1998) is a 20-item parent and child report of posttraumatic stress symptom frequency during the previous month. Items correspond to symptoms listed in DSM-IV PTSD criteria and are rated on a 5-point Likert-type scale from Never (0) to Most of the time (4). The questionnaire was administered verbally by research staff to children and parents. This instrument has been used among a variety of samples experiencing a variety of traumas with strong support for internal consistency, test-retest reliability, and convergent validity as evidenced by agreement of cut-off scores with a diagnosis of PTSD (Steinberg, Brymer, Decker, & Pynoos, 2004). In this sample, Cronbach's α = .88 and α = .83 for parents and children, respectively. A total score in the clinical range of ≥ 20 at baseline was required for participation.
Children's Depression Inventory (CDI) (Kovacs, 1981), child and parent versions, is a 27-item measure that assesses children's depressive symptoms. The scale has high internal consistency and construct validity (Kendall et al.,, 1989). Normative data are available (Finch, Saylor, & Edwards, 1985). We used a 26-item version of the scale that omitted an item about suicidal ideation per the request of school personnel who had concerns about asking this question to their young students. The current sample had Cronbach's α = .84 for parent and α = .82 for child reports.
Screen for Child Anxiety Related Emotional Disorders (SCARED-C), Child Report (Birmaher, 1999) is a 41-item youth-report measure designed to assess symptoms corresponding to DSM-IV anxiety disorders. Items include three answer choices of Not True or Hardly Ever True (0), Somewhat or Sometimes True (1), or Very True or Often True (2) (Birmaher et al., 1997). Responses are summed and scores of ≥25 are considered to be in the clinical range (Birmaher et al., 1997; Bailey, Chavira, Stein, & Stein, 2006), and several independent studies provide strong support of its test-retest reliability (Muris, Merckelbach, van Brakel, & Mayer, 1999) and concurrent and discriminative validity (Birmaher et al., 1997), as well as measurement invariance across ethnically diverse youth samples (Gonzalez, Weersing, Warnick, Scahill, & Woolston , 2012; Skriner & Chu, 2014). In this sample, the SCARED-C had Cronbach's α = .92.
Secondary outcome measures
Strengths and Difficulties Questionnaire (SDQ) Parent Report, and Teacher Report (Goodman, 1997; Goodman, Meltzer, & Bailey, 1998). This questionnaire contains 25 items, 20 assessing problem areas (emotional, conduct, hyperactivity/inattention, and peer relationships) and functional impairment related to those problems, and five assessing prosocial behavior (Goodman, 1999). The scale demonstrates excellent convergent validity with measures of related constructs, including the Rutter scales (Goodman et al., 1998) and the Child Behavior Checklist (Goodman & Scott, 1999). Cronbach's alpha for the current sample was α = .61 for parents and α = .74 for teachers.
The Social Adjustment Scale-Self-Report for Youth (SAS-SR-Y) (Weissman, Orvaschel, & Padian, 1980) contains 21 items and evaluates the degree of cohesion, communication, support and understanding within the interpersonal contexts of school behavior, friends, spare time, and family behavior. The SAS-SR-Y has demonstrated good internal consistency in previous samples (α = .84; Rohde, Seeley, Kaufman, Clarke, & Stice, 2006) as well as strong support for test-retest reliability and sensitivity to treatment (Stice, Marti, Spoor, Presnell, & Shaw, 2008). In this sample, the SAS-SR had a Cronbach's alpha coefficient of α = .80.
The Coping Efficacy measure (Sandler, Tein, Mehta, Wolchik, & Ayers, 2000) contains six items to assess children's satisfaction with handling past and current stressors, and their anticipated effectiveness in handling future stressors. Participants respond on a 4-point scale from Not at all good (0) to Very good (4). Scores have been shown to negatively relate to internalizing and externalizing symptoms and this measure has shown adequate internal consistency (α = .74; Sandler et al., 2000). Sample items include “The things people do to handle stressful problems sometimes work really well to make them feel better and sometimes they don't work at all. How well do you think the things you do to cope work to make you feel better?” Cronbach's alpha in this sample was α = .77.
The Emotion Regulation Checklist (ERC) (Shields & Cicchetti, 1997) is a 24-item parent-report questionnaire that yields two subscales: Negativity/Lability (10 items) which represents negative affect and mood lability and includes such items as “Is easily frustrated”, and Emotion Regulation (14 items) which assesses adaptive regulation and includes such items as “Gets over it quickly when he/she is upset or unhappy”. Previous research with the ERC has demonstrated good construct and discriminative validity between typically developing and maltreated youth (Shields & Cicchetti, 1997; Shields, Ryan, & Cicchetti, 2001). For the current sample, Cronbach's alpha was α = .82 for the Negativity/Lability scale and α = .69 for the Emotion Regulation subscale.
Satisfaction measures
Parent and child satisfaction with the Bounce Back program was assessed post-intervention for both conditions. Parental satisfaction was based on 13 questions about privacy and quality of services to the child and family, explanation of the intervention, and the professionalism of the group leaders. Items ranged from Very poor (0) to Outstanding (6). The child survey included 15 questions ranging from Not at all true (0) to Very true (3) and inquired about satisfaction with the group leader, the group in general, and intervention content. For both parents and children, items were averaged to get a mean satisfaction score. The child satisfaction survey also had two open-ended questions on which the child could list things he or she liked best or did not like about the group.
Analyses
All analyses were conducted in SAS, Version 9.3 (SAS Institute Inc, Cary, NC, USA). Demographic and clinical characteristics of the sample are displayed in Table 1. T-tests, chi-square tests, and ANOVAs were used to compare the early treatment and waitlist control groups at baseline to assess the success of randomization, check for differential dropout or other evidence of non-random missingness patterns, and to look for school effects. To assess feasibility and acceptability, we computed mean scores of parent and child satisfaction with Bounce Back and implementer fidelity to the model.
Table 1.
Demographic and Baseline Clinical Characteristics for the Immediate and Delayed Treatment Groups
| Variable | Full Samplea (N=74) | Immediate Treatment Group (N=36) | Delayed Treatment Group (N=38) | p-value |
|---|---|---|---|---|
| Gender | .35 | |||
| Male | 37 (50.00) | 20 (55.56) | 17 (44.74) | |
| Female | 37 (50.00) | 16 (44.44) | 21 (55.26) | |
| Race/Ethnicity | .50 | |||
| African American | 13 (17.57) | 6 (16.67) | 7 (18.42) | |
| Asian | 1 (1.35) | 1 (2.78) | 0 (0.00) | |
| Caucasian | 20 (27.03) | 11 (30.56) | 9 (23.68) | |
| Hispanic | 36 (48.65) | 17 (47.22) | 19 (50.00) | |
| Afr. Amer/Hispanic | 1 (1.35) | 0 (0.00) | 1 (2.63) | |
| Asian/Caucasian | 1 (1.35) | 1 (2.78) | 0 (0.00) | |
| Hispanic/Caucasian | 2 (2.70) | 0 (0.00) | 2 (5.26) | |
| Income Category | .94 | |||
| $4,999 or less | 5 (6.76) | 2 (5.56) | 3 (7.89) | |
| $5,000 - $14,999 | 8 (10.81) | 4 (11.11) | 4 (10.53) | |
| $15,000 - $24,999 | 8 (10.81) | 3 (8.33) | 5 (13.16) | |
| $25,000 - $39,999 | 12 (16.21) | 5 (13.89) | 7 (18.42) | |
| $40,000 or more | 35 (47.30) | 19 (52.78) | 16 (42.11) | |
| Don't Know | 6 (8.11) | 3 (8.33) | 3 (7.89) | |
| Grade | 2.73 (1.26) | 2.63 (1.22) | 2.38 (1.31) | .55 |
| Age | 7.65 (1.36) | 7.58 (1.32) | 7.71 (1.41) | .69 |
| Highest Parental Education | 13.28 (3.95) | 14.32 (3.46) | 12.32 (4.16) | .032 |
| TESI | 4.70 (3.36) | 4.85 (3.68) | 3.54 (3.06) | .73 |
| Child CDI | 11.14 (7.01) | 11.18 (6.60) | 11.10 (7.47) | .96 |
| Parent CDI | 7.23 (6.30) | 6.82 (6.37) | 7.66 (6.30) | .58 |
| Child RI | 33.80 (14.32) | 33.14 (14.25) | 34.44 (14.55) | .70 |
| Parent RI | 18.98 (12.97) | 17.85 (13.32) | 20.11 (12.70) | .46 |
| Child SCARED | 33.13 (15.47) | 34.31 (16.03) | 31.98 (15.04) | .52 |
| Child Efficacy | 16.90 (4.58) | 16.77 (4.13) | 17.03 (5.03) | .81 |
| Child SAS | ||||
| Total Score | 21.38 (11.92) | 20.31 (12.64) | 22.42 (11.26) | .45 |
| Academic Subscale | 5.05 (3.98) | 4.93 (4.32) | 3.93 (3.69) | .81 |
| Parent ERC | ||||
| Negativity/Lability | 28.38 (6.84) | 28.54 (8.03) | 28.20 (5.52) | .83 |
| Emotion Regulation | 26.54 (3.70) | 26.89 (3.80) | 26.18 (3.62) | .42 |
| Parent SDQ | 11.43 (5.61) | 11.50 (6.17) | 11.37 (5.07) | .92 |
| Teacher SDQ | 10.81 (7.16) | 11.32 (8.38) | 10.34 (5.92) | .58 |
Note.
Nine subjects did not provide information on income and three subjects were missing parental education data. One subject was missing the clinical measures at baseline. TESI= traumatic events screening inventory; CDI= Children's Depression Inventory; RI= Reaction Index; SCARED=Screen for Child Anxiety and Related Disorder; SAS=Social Adjustment Scale; ERC=Emotion Regulation Checklist; SDQ= Strengths and Difficulties Questionnaire.
Linear mixed-effects models were used to evaluate the five primary outcome measures, with group (Immediate, Delayed) as a between-subjects factor, time (Baseline, 3 months, 6 months) as a within-subjects factor, and a group by time interaction to examine differential treatment effects. Parallel models were fit for secondary outcomes. Unstructured covariance matrices were used to allow maximum flexibility in the modeling of the correlations induced by the repeated measures within subjects; the models were fit via restricted maximum likelihood (REML) to minimize bias in these parameter estimates. Main effects of site and group by site interactions were included in the models to control for possible effects of clustering within schools or intervention groups.
Our primary hypotheses about treatment effects corresponded to follow-up contrasts examining the group by time interaction from Baseline to 3 months. Additional contrasts were used to assess maintenance in the Immediate treatment group (operationalized as still showing significant improvement at 6 months relative to baseline), to examine treatment effects in the Delayed group from 3-6 months, and to compare the groups at the end of follow-up to determine whether the Delayed group differed from the Immediate treatment group. Following Jacobson and Truax (1991), we also computed the fraction of subjects who showed reliable change (from 0-3 months in the immediate group and 3-6 months in the delayed group) for the primary outcomes which showed differential treatment effects.
Mixed-effects models automatically handle missing values via likelihood-based methods, producing unbiased parameter estimates provided observations are missing at random. Because of this, and our low attrition rate (9.5%), we did not impute outcome values where an entire questionnaire was missing. However, there were instances in which one or more individual items on a measure were missing. If more than 25% of the items were unanswered, we treated the total score for the instrument as missing. If 75% or more of the items were completed, we computed an expected total based on the average of the completed items. In almost all cases where a total score was adjusted, only one or two items had been left blank.
Results
Summary statistics at baseline are shown in Table 1. There were no statistically significant group differences on any of these measures except for highest level of parental education (p-value = .032), with the Immediate treatment group parents being slightly more highly educated than those of the Delayed group. Parental education was therefore included as a covariate in the mixed models to protect against potential confounding. There were no significant differences in outcome measures by school, although there were gender and grade level differences (p = .0175 and .0197, respectively). However, the randomization within school successfully balanced these characteristics so they did not need to be adjusted for in subsequent models. There was no evidence of differential attrition by treatment group or school. Seven participants withdrew before completing the study (Figure 1). There was no evidence of a baseline difference between the subjects who did and did not complete the study except with regard to ethnicity: six of the 13 African American participants did not complete the study (five of these six because they relocated from the area and changed schools) compared to one of 36 Hispanic participants and none in the other ethnic groups (Fisher's exact test, p = .0016). Children in this study endorsed a range of different types of traumatic and stressful events. The proportions of children, and their parents, endorsing each type of child traumatic event are listed in Table 2.
Table 2.
Types and Frequencies of Traumatic Events Endorsed
| Type of Traumatic Event | Percentage of Students Endorsing Event |
|---|---|
| Witnessed/ know of family member arrested | 30.56 |
| Witnessed physical violence | 26.39 |
| Victim of physical violence | 24.66 |
| Witnessed or heard about neighborhood or school violence | 24.66 |
| Separated from parent(s) (e.g., deportation, deployment, hospitalization) | 21.92 |
| Witnessed a serious accident | 17.81 |
| Threatened by someone (violence) | 17.81 |
| Someone close to child very sick or hurt badly | 16.44 |
| Serious Ulness/hospitalization of loved one | 15.07 |
| Someone close to child died | 13.89 |
| Been in a serious accident | 13.70 |
| Attacked by a dog/animal | 11.11 |
| Threatened to steal from child | 10.96 |
| Parent/caregiver abusing drugs | 9.59 |
| Other stressful event | 9.59 |
| Witnessed weapon violence | 6.85 |
| Witnessed someone threatening violence | 6.85 |
| Kidnapped or someone close to child was kidnapped | 4.17 |
| Homelessness/extreme poverty | 4.11 |
| Attacked by a gun, knife, or weapon | 2.74 |
| Experienced a natural disaster | 1.37 |
Feasibility and Acceptability
Fidelity ratings indicated excellent therapist adherence to the intervention manual (Mean = 2.91/3, SD = .18) and excellent overall quality of content implementation (Mean = 2.94/3, SD = .26). Bounce Back was acceptable to families as indicated by high satisfaction ratings from parents (Mean = 5.31/6, SD = .71) and children (Mean = 2.66/3. SD = .41). Moreover, satisfaction ratings did not significantly differ across ethnic groups for parents (p = .269) or children (p= .139).
Primary Analyses of Intervention Effects
Consistent with our hypotheses, our primary analyses focused on differential treatment effects over the first three months of the intervention program for posttraumatic stress, anxiety, and depressive symptoms. Results, including effect sizes (Cohen's f2) .02 for a small effect, .15 for a medium effect and .35 for a large effect (Cohen, 1988), are shown in Table 3. There were significant group by time interactions for both child- and parent-reported youth posttraumatic stress symptoms (RI-C: f2 = .15, p = .0029: RI-P: f2 = .09, p = .022) and youth reported anxiety symptoms (SCARED-C: f2 = .26, p = .0002). In all cases, the Immediate group showed significant improvement over this period while the delayed group did not show evidence of significant change. The group by time interactions on the parent and child reports of depressive symptoms were not significant. We note that the results for the RI-C, RI-P and SCARED-C are jointly significant under the Benjamini-Hochberg false discovery rate approach to correcting for multiple comparisons (Benjamini & Hochberg, 1995; Benjamini & Yekutieli, 2001). There were no effects of parental education except for the CDI-C. There were no group by school interactions or school main effects on any of the five outcomes. Means and standard deviations for primary and secondary outcomes at each assessment point are listed in Table 4.
Table 3.
Treatment and Maintenance Effects on Primary and Secondary Outcomes for Immediate and Delayed Intervention with Bounce Backa
| Differential Treatment Effect (0-3 months) | Immediate Treatment Group (0-6 months) | Delayed Treatment Group (3-6 months) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| F (1,62) | f2 | p-value | F (1,62) | f2 | p-value | F (1,62) | f2 | p-value | |
| Primary Outcomes | |||||||||
| Child CDI | 3.76 | .06 | .057 | 21.36 | .34 | <.001 | 15.29 | .25 | <.001 |
| Parent CDI | 0.64 | .01 | .43 | 9.27 | .15 | .003 | 6.09 | .10 | .016 |
| Child RI | 9.60 | .15 | .003 | 49.55 | .80 | <.001 | 46.81 | .76 | <.001 |
| Parent RI | 5.50 | .09 | .02 | 19.90 | .32 | <.001 | 21.12 | .34 | <.001 |
| Child SCARED | 16.23 | .26 | <.001 | 24.69 | .40 | <.001 | 14.66 | .24 | <.001 |
| Secondary Outcomes | |||||||||
| Child Efficacy | 3.70 | .06 | .059 | 16.36 | .26 | <.001 | 12.27 | .20 | <.001 |
| Child SAS | |||||||||
| Total Score | 5.97 | .10 | .017 | 14.87 | .24 | <.001 | 29.44 | .47 | <.001 |
| Academic Subscale | 8.23 | .13 | .006 | 8.17 | .13 | .006 | 21.32 | .34 | <.001 |
| Parent ERC | |||||||||
| Negativity/Lability | 9.41 | .15 | .003 | 12.89 | .21 | <.001 | 3.34 | .05 | .073 |
| Emotion Regulation | 3.13 | .05 | .082 | 8.74 | .14 | .004 | 12.74 | .21 | <.001 |
| Parent SDQ | 4.26 | .07 | .043 | 0.16 | .003 | .69 | 0.67 | .01 | .42 |
| Teacher SDQ | 2.11 | .03 | .15 | 0.44 | .007 | .88 | 0.04 | <.001 | .84 |
Note.
Results shown are contrasts from the mixed models for (i) differential treatment effects (measured by a group by time interaction from 0-3 months), (ii) maintenance of effects in the Immediate treatment group (measured by comparing outcome measures at 6-month follow-up to those at baseline) and (iii) changes in the Delayed treatment group over the follow-up period (3-6 months) for the primary and secondary outcome measures. All effects shown are adjusted for parental education, site, and a site by treatment group interaction to control for potential confounding and within-school clustering. Effect sizes are given as Cohen's f2. CDI= Children's Depression Inventory; RI= Reaction Index; SCARED= Screen for Child Anxiety and Related Disorder; SAS=Social Adjustment Scale; ERC=Emotion Regulation Checklist; SDQ= Strengths and Difficulties Questionnaire.
Table 4.
Means and Standard Deviations on Primary and Secondary Outcomes across Assessment Time Points
| Baseline | 3 Months | 6 Months | ||||
|---|---|---|---|---|---|---|
| Measure | Immediate | Delayed | Immediate | Delayed | Immediate | Delayed |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| PTSD Reaction Index – Child | 33.15 (14.25) | 34.44 (14.55) | 18.74 (13.75) | 32.39 (12.89) | 11.00 (10.87) | 15.76 (12.69) |
| PTSD Reaction Index – Parent | 17.85 (13.32) | 20.11 (12.70) | 10.45 (10.25) | 23.54 (17.29) | 7.25 (8.54) | 13.10 (12.59) |
| SCARED | 34.31 (16.03) | 31.98 (15.04) | 25.22 (14.54) | 34.36 (15.67) | 19.09 (14.03) | 25.24 (16.10) |
| Children's Depression Inventory – Child | 11.18 (6.60) | 11.10 (7.47) | 7.03 (6.33) | 10.14 (6.47) | 5.29 (4.99) | 6.56 (6.59) |
| Children's Depression Inventory – Parent | 6.82 (6.37) | 7.66 (6.29) | 5.03 (5.36) | 8.89 (7.43) | 3.95 (4.32) | 6.87 (7.19) |
| Social Adjustment Scale – Youth Self report | 20.31 (12.64) | 22.42 (11.26) | 12.84 (9.33) | 21.72 (10.83) | 11.42 (9.13) | 12.21 (9.92) |
| Strengths and Difficulties – Parent report | 11.50 (6.17) | 11.37 (5.07) | 8.39 (5.85) | 12.17 (7.10) | 10.25 (5.50) | 13.02 (5.60) |
| Strengths and Difficulties – Teacher report | 11.32 (8.38) | 10.34 (5.92) | 9.96 (6.99) | 10.88 (6.81) | 11.52 (6.87) | 11.00 (7.09) |
| Emotion Regulation Checklist – Negativity/Lability | 28.55 (8.03) | 28.20 (5.52) | 24.65 (7.01) | 28.93 (7.19) | 23.60 (5.74) | 26.79 (6.75) |
| Emotion Regular Checklist – Emotion Regulation | 26.89 (3.80) | 26.18 (3.62) | 28.64 (3.25) | 26.43 (3.56) | 28.62 (3.28) | 27.93 (3.29) |
| Coping Efficacy | 16.77 (4.13) | 17.03 (5.03) | 19.21 (4.76) | 16.92 (4.58) | 20.69 (3.20) | 20.00 (3.28) |
Note. PTSD= posttraumatic stress disorder, SCARED= Screen for Child Anxiety and Related Disorder.
For the stress and anxiety measures, which showed differential treatment effects, we computed the fraction of subjects who experienced reliable change (RC) using the definition of Jacobson and Truax (1991) which is based on the expected distribution of the change scores that would be expected if no actual change had occurred. Specifically, the RC index is a function of the pretreatment variability (calculated using the full sample) and the test-retest reliability of the measure (based on prior studies from the literature [r=.81 Roussous et al., 2005 for the RI-C/RI-P; r=.81 Muris et al., 1999 for the SCARED]). During the initial treatment period, 49% of subjects receiving Immediate Bounce Back showed reliable change on the RI-C compared to 9% in the Delayed Group; 53% of the Delayed Group showed reliable change when they received the treatment. For the RI-P, the rates of reliable change were 19% (Immediate) vs 9% (Delayed) during the initial treatment period with 28% of the Delayed group showing reliable change during the follow-up period. For the SCARED-C, the rates were 24% (Immediate) vs 3% (Delayed) during the initial period and 26% for the Delayed Group during the follow-up period. It is worth noting that the SCARED-C also has a well-defined threshold score, with values ≥25 being considered in the clinical range. 56% of the Immediate Bounce Back Group lowered their scores below this threshold during the initial treatment period compared to 22% in the Delayed Group; similarly 53% of the Delayed Group dropped below the threshold over the follow-up period.
Significant treatment effects at the α=.05 level favoring the Immediate Bounce Back group were also found for several of the secondary measures (Table 3), including social functioning (SAS; driven primarily by strong results for the Academic subscale) and parent-rated ERC Negativity/Lability, both of which remain significant following correction for multiple comparisons, as well as SDQ-P Total.
Maintenance in the Immediate Group and Intervention Effects in the Delayed Group
On all five of the primary outcomes, the Immediate group showed significant improvements at the 6 month observation compared to baseline (all p-values < .0035), with significant continued improvement over the 3-6 month follow-up period on the RI-C and SCARED-C (p-values .011 and .027, respectively; results not shown in the table). The Delayed group showed significant improvement on all five primary outcomes for the 3-6 month period, during which they received intervention (all p-values < .02).
For the secondary measures, the Immediate group remained significantly improved relative to baseline on the Coping Efficacy, SAS and Emotion Regulation measures and the Delayed group showed significant improvement on these same outcomes over the 3-6 month period (see Table 3). Means and standard deviations for primary and secondary outcomes at each assessment point are listed in Table 4.
Discussion
This study reports on the initial outcomes of a school-based intervention program, Bounce Back, designed to help elementary-aged students recover from a range of traumatic events. Following on the success of a similar program for students in middle school through secondary school (Stein et al., 2003; Jaycox, 2003), and a parent-child clinical model (TF-CBT) (Cohen, Mannarino, & Deblinger, 2006), Bounce Back was designed to fit a need for such programming for younger children in the school setting. Similar cognitive-behavioral concepts and techniques to both TF-CBT and CBITS are used in Bounce Back; however, significant developmental modifications were made to teach the therapeutic skills to younger students in a group format conducive to school-based mental health service delivery with less demand for parent involvement. Modifications included obtaining parental input in identifying areas of functional impairment on which to focus, introducing more foundational elements (such as identifying feelings before moving to the link between thoughts and feelings, use of published story books to introduce the topic of traumatic events), developing ways to make concepts very concrete (such as ‘courage cards’ tailored to each student and planning positive activities that were feasible), adapting trauma narratives into story books created by the children, and creating games and other experiential activities to help engage young children in learning the intervention skills in a group.
Symptom Reduction/Primary and Secondary Outcomes
Results indicated that symptoms of posttraumatic stress and anxiety were significantly improved in children who received the intervention compared to those randomized to a three-month waitlist. Effects of the intervention were medium to large in magnitude and are consistent with findings from previous individual therapies (e.g., TF-CBT; Cohen & Mannarino, 2008) and school-based interventions for trauma in adolescents (Kataoka et al., 2003; Stein et al., 2003). These results are promising and indicate that younger pre-adolescent children who experience stress-related mental health symptoms may benefit from a developmentally-tailored school-based group intervention. Emerging research indicates that pre-adolescent children may experience traumatic events at rates similar to those observed in later childhood and adolescence (Stein et al., 2003) and this is concerning given the well-documented risk inferred by trauma exposure in youth. Recent studies demonstrate that early identification and treatment of mental health problems can have a positive impact on mental health and academic functioning years later (e.g., Guzman et al., 2011). Taken together, the need for and benefits of effective interventions for elementary school children are clear.
Our hypotheses that the Bounce Back intervention would be associated with significant reductions in posttraumatic stress and anxiety symptoms were supported. These hypotheses were based on extant literature on cognitive behavioral treatment using similar therapeutic components (e.g., relaxation, behavioral exposure, increased social support, and exposure to the memory of traumatic event) and their associated reductions in internalizing symptoms (Dorsey et al., 2011; Silverman et al., 2008). Results indicate that by relying on the existing evidence-base and tailoring to the population and setting, we could achieve favorable outcomes similar to those of other efficacious interventions.
Although there was significant improvement in child-reported depression within the Immediate intervention group in the first phase of the study, the group by time interaction for a differential intervention effect on depressive symptoms failed to reach significance (p = .057). These findings are inconsistent with those of a previous study of a school-based trauma intervention that was associated with a reduction in depressive symptoms in adolescents (Stein et al., 2003). Of note, depression scores in this sample of pre-pubertal school-aged children were relatively low from the start, likely reflecting differences in the prevalence of depressive symptoms across youth development, and thus limiting the extent of possible improvement in depression. In the second phase, when the Delayed intervention group received Bounce Back, these students demonstrated within-group improvement on all three domains per both parent and child report. Moreover, the students who received Bounce Back in the Immediate intervention group sustained their gains, continuing to show significant improvements relative to baseline during their follow-up period. Some positive influences on secondary outcomes (social adjustment, behavior, emotion expression, and coping) were also observed. Thus, Bounce Back appears to have the intended effect of reducing anxiety, posttraumatic stress, and to a lesser extent, depression, and appears to improve some of the related functional outcomes.
Advantage of Study Setting
Numerous publications highlight the need to improve and expand mental health programs for young children in school settings (e.g., Fazel, Hoagwood, Stephan, & Ford, 2014; President's New Freedom Commission on Mental Health, 2003), which may decrease the risk for future emotional, academic, and social difficulties. School-based services such as Bounce Back may circumvent common treatment barriers, including transportation difficulties, time constraints of families, and stigma of attending services in specialty mental health clinics (Jaycox et al., 2010). In addition, this modality and setting may facilitate access for ethnically and socioeconomically diverse youth who are often underserved in mental health. The majority of children who access mental health services do so through the education sector (Farmer, Burns, Phillips, Angold, & Costello, 2003), and school-based mental health services may be a particularly viable pathway for underserved children who would benefit from services (Bledsoe, 2008; Fazel et al., 2014). Further, school-based services may improve treatment attrition rates. In this sample 90.5% of children completed the treatment and 97% of those parents attended the minimum required session. These findings are in accordance with previous research suggesting that referrals to school-based services are associated with higher rates of service utilization compared to referral to community-based services (Husky et al., 2011; Jaycox et al., 2010).
An additional advantage of this study was its mixed efficacy-effectiveness hybrid approach designed to optimize the balance of both internal and external validity of findings and increase the speed of treatment dissemination. Our overall approach is consistent with recommendations to test interventions early in their development in real world contexts, including incorporation of stakeholder perspectives in the initial development of an intervention, and evaluation of the practice-ready intervention with the kinds of clients, delivered by the kinds of clinicians, that represent the particular setting (Weisz, Ng, & Bearman, 2014; Weisz & Gray, 2008). The delivery of Bounce Back by clinicians who were already providing clinical services in the school setting also provided a representative evaluation of feasibility of training and implementation of the core content. The quality and high fidelity ratings suggest that this model can be successful in elementary school settings with existing mental health personnel. Program sustainability was considered at all stages of study design. In addition to training school-based personnel to deliver the intervention, inclusion criteria were kept to a minimum and well-validated assessment instruments were selected for their low-cost availability and ease of administration.
Limitations
Several limitations to the current study must be considered. First, this study was initially designed as a pilot intervention program. Accordingly, the study included a relatively small sample size and was not specifically designed to definitively detect differential treatment effects, so the results warrant replication with a larger sample. Our sample of 74 children was sufficient to detect a group by time interaction corresponding to a change from no difference between the treatment groups at baseline to a difference of d = .65 SDs (or equivalently f2 =.11) with 80% power using a two-sided significance level of α=.05. The study was well-powered in that we were able to find significant treatment effects on three of the five primary outcomes; however it may have been underpowered for the parent and child reports of depressive symptoms, particularly the latter for which the observed interaction effect size was f2 = .06 with a p-value of p = .057, as well as for several of the secondary outcomes which showed a similar pattern of estimated effects. Second, because this was an initial evaluation of a novel intervention, we included a waitlist control to assess efficacy. Future research should compare Bounce Back to a comparison intervention, including treatment as usual, to determine its relative effectiveness. Additionally, we did not collect information regarding receipt of concurrent or additional treatment which may hold particular relevance for youth in the waitlist group.
Third, some limitations regarding study assessment should be noted. While the use of multiple informants is a strength, this study did not include objective assessment from assessors blind to treatment group. The participant-reported assessment methods were selected to model conditions that are likely under real world conditions where blind assessment is likely not feasible or sustainable. With respect to fidelity measures, the fidelity rating instrument was designed by the intervention developer to be most face valid with the specific content of the intervention to assess if the content could be sufficiently covered by real-world school-based mental health providers. While the rating forms were designed to be very specific to the content (i.e., checklist of content and skills in addition to quality ratings), there is the possibility of rater bias given the raters’ involvement in the present study. The satisfaction measure was modified from existing measures to assess parental satisfaction for the purposes of identifying potential problems with the intervention to inform future improvements; it was not designed to provide a formal measure of satisfaction, and information regarding reliability and validity have not been investigated.
Finally, we found unexpected ethnic differences in study attrition such that a higher proportion of African American students discontinued study involvement compared to other ethnic groups. However, it is important to note that five of the six African American students who discontinued participation did so because the family moved at some point during the study, requiring a change in schools. This illustrates that non-completions were unrelated to the study itself, and there were no racial/ethnic differences in parent- or child-rated satisfaction, indicating high levels of satisfaction across all groups. Nevertheless, this finding highlights one challenge of working with urban families who may experience transiency and potential housing instability. A future direction may be to create interventions designed to be delivered over a shorter duration to prevent high turnover of students.
Future research should attend to issues of implementation and sustainability of school-based services beyond the research study period. Although issues if implementation were considered throughout the design and conduct of this study, schools nevertheless received many resources from research staff, including staff support for screening procedures, supplies for assessment and intervention materials (e.g., photocopying, small rewards for children), and therapist training and ongoing supervision. One study explored facilitators and barriers of implementation of CBITS in several schools across the nation (Langley, Nadeem, Kataoka, Stein, & Jaycox, 2010). Site administrators and clinicians cited competing responsibilities, lack of parent engagement, and lack of support from school administrators as barriers to implementation. However, sites that successfully implemented the school-based intervention on an ongoing basis cited the availability of implementation support (e.g., knowing someone else in their school, district, or region who was conducting the same intervention or having access to program trainer, consultant, or developer) as an important factor in sustainability.
Conclusions
Despite these limitations, the school-based Bounce Back program holds great promise. It may be particularly valuable for students that might have difficulty accessing specialty mental health settings, such as urban and ethnic minority youth. By delivering Bounce Back in schools, specific barriers to services such as transportation and stigma can be reduced, and required parent participation is kept to a minimum. Parents tend to be more involved with their younger elementary age students than they are with their middle and high school students, and the Bounce Back program necessarily capitalizes on that involvement to include parents to a greater degree in the trauma narrative portion of the intervention. This is a higher level of involvement than in the CBITS program, which showed significant impacts on student mental health despite low levels of parental involvement (Kataoka, 2003; Stein et al., 2003). In this study, parents attended one to three sessions to receive psychoeducation and to participate in the trauma narrative; nevertheless, parents in this study endorsed high levels of satisfaction with the intervention and overall parent compliance with the program showed that this level of participation was reasonable and acceptable. Overall, parents provided high satisfaction ratings. However, because all child participants received the group intervention, it is possible that parents’ reports of satisfaction and acceptability may actually reflect a sense of gratitude due to the receipt of no-cost intervention. Future investigations with comparison treatment groups should include satisfaction and acceptability measures to rule out this potential confound.
In summary, this study provides initial support that Bounce Back, a cognitive-behavioral, trauma-focused intervention, can be successfully delivered in schools to groups of elementary school children who have been impacted by various types of traumatic events and reduce associated symptoms of posttraumatic stress. During a time when school crises and community disasters are relatively common and significantly impact students of all ages, it will be worthwhile to assess the degree to which this program may hold promise in filling an essential niche toward bringing necessary services to the elementary aged students least likely to obtain mental health services in the specialty mental health sector.
Public Health Significance.
“This study suggests that Bounce Back, an intervention for elementary school students exposed to traumatic events, is an effective school-based, group treatment in reducing symptoms of post-traumatic stress and anxiety for children.”
Contributor Information
Audra K. Langley, University of California, Los Angeles
Araceli Gonzalez, California State University, Long Beach.
Catherine A. Sugar, University of California, Los Angeles
Diana Solis, University of California, Los Angeles.
Lisa Jaycox, RAND Corporation.
References
- Bailey KA, Chavira DA, Stein MT, Stein MB. Brief measures to screen for social phobia in primary care pediatrics. Journal of Pediatric Psychology. 2006;31(5):513–521. doi: 10.1093/jpepsy/jsj044. Retrieved from http://search.proquest.com/docview/621303273?accountid=14512. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. 1995;57(1):289–300. [Google Scholar]
- Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Annals of Statistics. 2001;29(4):1165–1188. [Google Scholar]
- Bledsoe SE. Barriers and promoters of mental health services utilization in a Latino context: A literature review and recommendations from an ecosystems perspective. Journal of Human Behavior in the Social Environment. 2008;18(2):151–183. doi: http://dx.doi.org/10.1080/10911350802285870. [Google Scholar]
- Briggs-Gowan M, Carter AS, Clark R, Augustyn M, McCarthy KJ, Ford JD. Exposure to potentially traumatic events in early childhood: Differential links to emergent psychopathology. Journal Child Psychology and Psychiatry. 2010;51:1132–1140. doi: 10.1111/j.1469-7610.2010.02256.x. doi: http://dx.doi.org/10.1111/j.1469-7610.2010.02256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorder (SCARED): A replication study. Journal of the Academy of Child & Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the Academy of Child & Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Cochran WG. Sampling Techniques. 3rd edition John Wiley & Sons; New York, NY: 1977. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. Guilford Press; New York: 2006. [Google Scholar]
- Cohen JA, Mannarino AP. Trauma-focused cognitive behavioural therapy for children and parents. Child and Adolescent Mental Health. 2008;13:158–162. doi: 10.1111/j.1475-3588.2008.00502.x. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64(5):577–584. doi: 10.1001/archpsyc.64.5.577. doi: http://dx.doi.org/10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Delaney-Black V, Covington C, Ondersma S, Nordstrom-Klee B, Templin T, Ager J, Sokol RJ. Violence exposure, trauma, and IQ and/or reading deficits among urban children. Archives of Pediatric & Adolescent Medicine. 2002;156(3):280–285. doi: 10.1001/archpedi.156.3.280. [DOI] [PubMed] [Google Scholar]
- Dorsey S, Briggs EC, Woods BA. Cognitive behavioural treatment for posttraumatic stress disorder in children and adolescents. Child and Adolescent Psychiatrics Clinics of North America. 2011;20:255–269. doi: 10.1016/j.chc.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards JH, Rogers KC. The traumatic events screening inventory: assessing trauma in children. Sage Publications, Inc; Thousand Oaks, CA.: 1997. pp. 113–118. http://search.proquest.com/docview/619154890?accountid=14512. [Google Scholar]
- Farmer EM, Burns BJ, Phillips SD, Angold A, Costello EJ. Pathways into and through mental health services for children and adolescents. Psychiatric Services. 2003;54(1):60–66. doi: 10.1176/appi.ps.54.1.60. [DOI] [PubMed] [Google Scholar]
- Farmer EMZ, Stangl DK, Burns BJ, Costello EJ, Angold A. Use, persistence, and intensity: patterns of care for children's mental health across one year. Community Mental Health Journal. 1999;35:31–46. doi: 10.1023/a:1018743908617. [DOI] [PubMed] [Google Scholar]
- Fazel M, Hoagwood K, Stephan S, Ford T. Mental health interventions in schools with high-income countires. The Lancet Psychiatry. 2014;1(5):387–388. doi: 10.1016/S2215-0366(14)70312-8. Retrieved from doi: 10.1016/S2215-0366(14)70312-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch AJ, Saylor CF, Edwards GL. Children's depression inventory: sex and grade norms for normal children. Journal of Consulting and Clinical Psychology. 1985;53:424–425. doi: 10.1037//0022-006x.53.3.424. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner H, Ormrod R, Hamby S, Kracke K. Children's exposure to violence: A comprehensive national survey. U.S. Department of Justice; 2009. Retrieved from: http://www.unh.edu/ccrc/pdf/DOJ-NatSCEV-bulletin.pdf. [Google Scholar]
- Foa EB, Keane TM, Friedman MJ, Cohen JA. Effective Treatments for PTSD, Second Edition: Practice Guidelines from the International Society for Traumatic Stress Studies. Guilford Press; New York, NY: 2009. [Google Scholar]
- Ford JD, Racusin R, Ellis C, Daviss WB, Reiser J, Fleischer A, Thomas J. Child maltreatment, other trauma exposure, and posttraumatic symptomatology among children with Oppositional Defiant and Attention Deficit Hyperactivity Disorders. Child Maltreatment. 2000;5:205–217. doi: 10.1177/1077559500005003001. [DOI] [PubMed] [Google Scholar]
- Freeman LN, Mokros HB, Poznanski EO. Violent events reported by normal school-aged children: Characteristics and depression correlates. Journal of American Academy of Child & Psychiatry. 1993;32:419–423. doi: 10.1097/00004583-199303000-00025. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Weersing VR, Warnick E, Scahill L, Woolston J. Cross-ethnic measurement equivalence of the SCARED in an outpatient sample of african american and non-hispanic white youths and parents. Journal of Clinical Child and Adolescent Psychology. 2012;41(3):361–369. doi: 10.1080/15374416.2012.654462. doi: http://dx.doi.org/10.1080/15374416.2012.654462. [DOI] [PubMed] [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. Journal of Child Psychology and Psychiatry. 1999;40(5):791–799. [PubMed] [Google Scholar]
- Goodman R, Meltzer H, Bailey V. The Strengths and Difficulties Questionnaire: a pilot study on the validity of the self-report version. European Child & Adolescent Psychiatry. 1998;7:125–130. doi: 10.1007/s007870050057. [DOI] [PubMed] [Google Scholar]
- Goodman R, Scott S. Comparing the Strengths and Difficulties Questionnaire and the Child Behaviour Checklist: Is small beautiful? Journal of Abnormal Child Psychology. 1999;27(1):17–24. doi: 10.1023/a:1022658222914. [DOI] [PubMed] [Google Scholar]
- Grogger J. Incarceration-related costs of early childbearing. In: Maynard RA, editor. Kids having kids. Urban Institute; Washington, DC: 1997. pp. 231–256. [Google Scholar]
- Guzman MP, Jellinek M, George M, Hartley M, Squicciarini AM, Canenguez KM, Murphy JM. Mental health matters in elementary school: First-grade screening predicts fourth grade achievement test scores. European Child & Adolescent Psychiatry. 2011;20(8):401–411. doi: 10.1007/s00787-011-0191-3. doi: http://dx.doi.org/10.1007/s00787-011-0191-3. [DOI] [PubMed] [Google Scholar]
- Hurt H, Malmud E, Brodsky NL, Giannetta J. Exposure to violence: Psychological and academic correlates in child witnesses. Archives of Pediatric and Adolescent Medicine. 2001;155(12):1351–1356. doi: 10.1001/archpedi.155.12.1351. [DOI] [PubMed] [Google Scholar]
- Hurt RA, Qiu X, Wu L, Roh Y, Palumbo AV, Tiedje JM, Zhou J. Simultaneous recovery of RNA and DNA from soils and sediments. Applied and Environmental Microbiology. 2001;67:4495–4503. doi: 10.1128/AEM.67.10.4495-4503.2001. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC93195/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husky MM, Kaplan A, McGuire L, Flynn L, Chrostowski C, Olfson M. Identifying adolescents at risk through voluntary school-based mental health screening. Journal of Adolescence. 2011;34(3):505–511. doi: 10.1016/j.adolescence.2010.05.018. doi: http://dx.doi.org/10.1016/j.adolescence.2010.05.018. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical Significance: A Statistical Approach to Defining Meaningful Change in Psychotherapy Research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jaycox L. Cognitive-Behavioral Intervention for Trauma in Schools. Sopris West Educational Services; Longmont, CO: 2003. [Google Scholar]
- Jaycox LH, Cohen J, Mannarino A, Walker DW, Langley AK, Gegenheimer KL, Schonlau M. Children's mental health care following Hurricane Katrina: A field trial of trauma-focused Psychotherapies. Journal of Traumatic Stress. 2010;23:223–231. doi: 10.1002/jts.20518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kataoka SH, Stein BD, Jaycox LH, Wong M, Escudero P, Tu W, Fink A. A school-based mental health program for traumatized Latino immigrant children. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(3):311–318. doi: 10.1097/00004583-200303000-00011. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M. Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology. 1997;65:453–463. doi: 10.1037//0022-006x.65.3.453. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Cantwell DP, Kazdin AE. Depression in children and adolescents: Assessment issues and recommendations. Cognitive Therapy and Research. 1989;13:109–146. [Google Scholar]
- Kliewer W, Lepore SJ, Oskin D, Johnson PD. The role of social and cognitive processes in children's adjustment to community violence. Journal of Consulting and Clinical Psychology. 1998;66:199–209. doi: 10.1037//0022-006x.66.1.199. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Actapaedopsychiatrica. 1981;46:305–315. [PubMed] [Google Scholar]
- Langley AK, Nadeem E, Kataoka SH, Stein BD, Jaycox LH. Evidence-based mental health programs in schools: Barriers and facilitators of successful implementation. School Mental Health. 2010;2(3):105–113. doi: 10.1007/s12310-010-9038-1. doi: http://dx.doi.org/10.1007/s12310-010-9038-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langley A, DeCarlo Santiago C, Rodríguez A, Zelaya J. Improving implementation of mental health services for trauma in multicultural elementary schools: Stakeholder perspectives on parent and educator engagement. The Journal of Behavioral Health Services & Research. 2013;40(3):247–262. doi: 10.1007/s11414-013-9330-6. doi: http://dx.doi.org/10.1007/s11414-013-9330-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonigan CJ, Shannon MP, Finch AJ, Daugherty TK. Children's reactions to a natural disaster: Symptom severity and degree of exposure. Advances in Behaviour Research and Therapy. 1991;13:135–154. [Google Scholar]
- Lynch M, Cicchetti D. An ecological-transactional analysis of children and contexts: The longitudinal interplay among child maltreatment, community violence, and children's symptomatology. Development of Psychopathology. 1998;10:235–257. doi: 10.1017/s095457949800159x. [DOI] [PubMed] [Google Scholar]
- McKay MM, Bannon WMJ. Engaging families in child mental health services. Child & Adolescent Psychiatrics Clinics of North America. 2004;13(4):905–921. doi: 10.1016/j.chc.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, van Brakel A, Mayer B. The revised version of the screen for child anxiety related emotional disorders (SCARED-R): Further evidence for its reliability and validity. Anxiety, Stress & Coping: An International Journal. 1999;12(4):411–425. doi: 10.1080/10615809908249319. doi: http://dx.doi.org/10.1080/10615809908249319. [DOI] [PubMed] [Google Scholar]
- Osofsky J. Young children and trauma: Intervention and treatment. Guildford Publications; New York, NY: 2004. [Google Scholar]
- Pynoos RS, Rodriguez N, Steinberg AS, Struber A, Fredrick C. The UCLA PTSD Reaction Index for DSM IV (Revision 1) UCLA Trauma Psychiatry Program; Los Angeles: 1998. [Google Scholar]
- Ribbe D. Psychometric review of Traumatic Events Screening Inventory for Children (TESI-C). In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Sidran; Lutherville, MD: 1996. pp. 386–387. [Google Scholar]
- Rohde P, Seeley JR, Kaufman NK, Clarke GN, Stice E. Predicting time to recovery among depressed adolescents treated in two psychosocial group interventions. Journal of Consulting and Clinical Psychology. 2006;74(1):80–88. doi: 10.1037/0022-006X.74.1.80. doi: http://dx.doi.org/10.1037/0022-006X.74.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roussos A, Goenjian AK, Steinberg AM, Sotiropoulou C, Kakaki M, Kabakos C, Manouras V. Posttraumatic stress and depressive reactions among children and adolescents after the 1999 earthquake in ano liosia, greece. The American Journal of Psychiatry. 2005;162(3):530–537. doi: 10.1176/appi.ajp.162.3.530. doi: http://dx.doi.org/10.1176/appi.ajp.162.3.530. [DOI] [PubMed] [Google Scholar]
- Sandler IN, Tein JY, Mehta P, Wolchik S, Ayers T. Coping efficacy and psychological problems in children of divorce. Child Development. 2000;1:1099–1118. doi: 10.1111/1467-8624.00212. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone M, Ayers TS, Kasprow W, Voyce C, Barone C, Shriver T, Weissberg R. No safe haven: A study of violence exposure in an urban community. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:1343–1352. doi: 10.1097/00004583-199510000-00020. [DOI] [PubMed] [Google Scholar]
- Shields A, Cicchetti D. Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology. 1997;33:906–916. doi: 10.1037//0012-1649.33.6.906. [DOI] [PubMed] [Google Scholar]
- Shields AM, Ryan RM, Cicchetti D. Narrative representations of caregivers and emotion regulation as predictors of maltreated children's rejection by peers. Developmental Psychology. 2001;37(3):321–337. doi: 10.1037//0012-1649.37.3.321. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Ortiz CD, Viswesvaran C, Burns BJ, Kolko DJ, Putnam FW, Amaya-Jackson L. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child & Adolescent Psychology. 2008;37(1):156–183. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Skriner LC, Chu BC. Cross-ethnic measurement invariance of the SCARED and CES-D in a youth sample. Psychological Assessment. 2014;26(1):332–337. doi: 10.1037/a0035092. doi: http://dx.doi.org/10.1037/a0035092. [DOI] [PubMed] [Google Scholar]
- Stein BD, Jaycox LH, Kataoka SH, Rhodes HJ, Vestal KD. Prevalence of child and adolescent exposure to community violence. Clinical Child and Family Psychology Review. 2003;6:247–264. doi: 10.1023/b:ccfp.0000006292.61072.d2. [DOI] [PubMed] [Google Scholar]
- Stein BD, Jaycox LH, Kataoka SH, Wong M, Tu W, Elliot MN, Fink Al. A mental health intervention for school children exposed to violence: A randomized controlled trial. Journal of the American Medical Record Association. 2003;290:603–611. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index. Current Psychiatry Reports. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti N, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suliman S, Mkabile SG, Fincham DS, Ahmed R, Stein DJ, Seedat S. Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Comprehensive Psychiatry. 2009;50:121–127. doi: 10.1016/j.comppsych.2008.06.006. [DOI] [PubMed] [Google Scholar]
- The President's New Freedom Commission on Mental Health. 2003 Retrieved from http://govinfo.library.unt.edu/mentalhealthcommission/reports/reports.htm.
- Weissman MM, Orvaschel H, Padian N. Children's symptom and social functioning self-report scales: Comparison of mothers' and children's reports. Journal of Nervous and Mental Disease. 1980;168(12):736–740. doi: 10.1097/00005053-198012000-00005. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Gray JS. Evidence-based psychotherapies for children and adolescents: Data from the present and a model for the future. Child and Adolescent Mental Health. 2008;13:54–65. doi: 10.1111/j.1475-3588.2007.00475.x. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Ng MY, Bearman SK. Odd couple? Reenvisioning the relation between science and practice in the dissemination-implementation era. Clinical Psychological Science. 2014;2.1:58–74. [Google Scholar]