Abstract
Both maladaptive and adaptive emotion regulation strategies have been linked with psychopathology. However, previous studies have largely examined them separately, and little research has examined the interplay of these strategies cross-sectionally or longitudinally in patients undergoing psychological treatment. This study examined the use and interplay of adaptive and maladaptive emotion regulation strategies in 81 patients receiving cognitive-behavioral interventions for comorbid alcohol use and anxiety disorders. Patients completed measures of emotion regulation strategy use and symptoms of psychopathology pre- and post-treatment. Cross-sectionally, higher use of maladaptive strategies (e.g., denial) was significantly related to higher psychopathology pre- and post-treatment, whereas higher use of adaptive strategies (e.g., acceptance) only significantly related to lower psychopathology post-treatment. Prospectively, changes in maladaptive strategies, but not changes in adaptive strategies, were significantly associated with post-treatment psychopathology. However, for patients with higher pre-treatment maladaptive strategy use, gains in adaptive strategies were significantly associated with lower post-treatment psychopathology. These findings suggest that psychological treatments may maximize efficacy by considering patient skill use at treatment outset. By better understanding a patient's initial emotion regulation skills, clinicians may be better able to optimize treatment outcomes by emphasizing maladaptive strategy use reduction predominately, or in conjunction with increasing adaptive skill use.
Keywords: adaptive and maladaptive emotion regulation strategies, anxiety disorders, alcohol use disorders, cognitive behavioral therapy
Emotion regulation is an important set of processes by which an individual manages and responds to their emotions (Gross & Muñoz, 1995). Previous researchers have shown particular interest in the regulation of distressing negative emotional states, such as sadness or anxiety (Campbell-Sills, Barlow, Brown, & Hofmann, 2006; Gross, 1998). As a consequence, emotion regulation has been increasingly incorporated into conceptualizations of psychopathology development and maintenance (Aldao & Nolen-Hoeksema, 2010; Kring & Sloan, 2010) and has also become a focus of treatment (e.g., Barlow, Allen, & Choate, 2004; Hayes & Feldman, 2004; Mennin, 2004).
Cross-sectional studies of emotion regulation have identified relationships between psychopathology and greater use of maladaptive emotion regulation. Strategies are considered maladaptive when they fail to modulate the intensity of an emotional experience, despite an individual's intention to the contrary (Gross, 1998). For example, rumination, defined as passive focus on one's symptoms and their causes and consequences, has been shown to exacerbate negative moods (Nolen-Hoeksema, 1991). Similarly, both deliberately pushing away emotional thoughts and suppressing the outward expression of emotions are considered ineffective emotion regulation strategies because they are often unsuccessful at reducing negative emotions (Gross, 1998) or, in the case of thought suppression, can create paradoxical rebound effects where the suppressed emotion returns with greater frequency and intensity (Wegner, Schneider, Carter, & White, 1987). The results of a recent meta-analysis suggest that there are significant relationships between higher levels of rumination and depression, anxiety, and substance use disorders, as well as significant relationships between suppression and anxiety and depression (Aldao, Nolen-Hoeksema, & Schweizer, 2010). Behavioral avoidance, defined as a pervasive pattern of evading or removing oneself from distressing situations, also has significant relationships with depression, anxiety, and substance use disorders (Aldao et al., 2010). These results indicate that both internalizing and externalizing disorders are associated with greater use of maladaptive emotion regulation strategies, though these relationships appear to be stronger for mood and anxiety disorders than for substance use disorders. It is possible that those with substance use disorders rely on substances, which can fulfill a similar avoidant function, as their primary emotion regulation strategy instead (Sher & Grekin, 2007).
In parallel, some attention has also been paid to relationships between active adaptive strategy use and psychological health, though adaptive strategy use tends to exhibit weaker relationships with psychopathology than does the use of maladaptive strategies (Aldao et al., 2010). A few examples of adaptive strategies that have demonstrated relationships with (less severe) psychopathology include mindful awareness, the process of approaching emotions nonjudgmentally (for a review, see: Keng, Smoski, & Robins, 2011), and positive reappraisal of emotion-eliciting situations (Garnefski & Kraaij, 2006; Martin & Dahlen, 2005). Aldao and colleagues (2010) have suggested the less robust nature of the relationships observed between adaptive strategies and psychopathology may be because the usefulness of these strategies is more context dependent (e.g., reappraisal skills may only be beneficial when a situation can realistically be reframed).
Recently, there has been increased interest in understanding the dynamic role of adaptive and maladaptive emotion regulation strategies as they relate to each other and to psychological health. In a nonclinical community sample, Aldao and Nolen-Hoeksema (2012) noted that greater use of maladaptive strategies was related to more severe psychopathology concurrently and predicted higher psychopathology symptom severity one year later, even after controlling for initial symptom severity. Interestingly, there were no direct associations between the use of adaptive strategies and psychopathology symptoms concurrently or prospectively. During further examination of concurrent relationships, the authors noted that the relationship between the use of adaptive strategies and psychopathology symptoms was moderated by the use of maladaptive strategies. Their results suggest that more frequent use of adaptive strategies confer a benefit only in individuals who report greater use of maladaptive strategies. Aldao and Nolen-Hoeksema conclude that their cross-sectional results support a compensatory hypothesis of psychopathology; that is, adaptive strategies serve to compensate for elevated use of maladaptive strategies. These findings point to more complex associations between cumulative adaptive strategies and psychopathology than previously recognized, particularly when considering the dynamic role of maladaptive strategies as well.
Traditionally researchers have focused on adaptive strategies or maladaptive strategies individually, which is consistent with the literature reviewed above; however, results like Aldao and Nolen-Hoeksema's indicate that we can miss important connections between constructs when we are too focused on one type of strategy. Also, given that individuals use a range of strategies to regulate their emotions, both adaptive and maladaptive (Carver, Scheier, & Weintraub, 1989), it is essential that progressive research explore the extent to which these types of strategies interact with each other or carry differing predictive abilities in order to provide a more comprehensive understanding of emotion regulation and mental health. Furthermore, these implications may be relevant for better understanding the skills that should be emphasized (e.g., targeting the reduction of the use of maladaptive coping and/or enhancing the use of adaptive coping) for individuals engaged in various psychological treatments.
In general, evidence-based treatments for psychological disorders tend to emphasize both increasing adaptive emotion regulation strategies, such as positive reappraisal in cognitive behavioral therapy (Barlow et al., 2011; Beck, Emery, & Greenberg, 1985; Beck, Rush, Shaw, & Emery, 1979) or acceptance in mindfulness-based cognitive therapy (Segal, Williams, & Teasdale, 2002) and acceptance and commitment therapy (Hayes, Strosahl, & Wilson, 1999), as well as reducing maladaptive emotion regulation strategies, such as avoidance in cognitive behavioral therapy (Barlow, Allen, & Choate, 2004). A recent treatment study found patients with social anxiety in CBT experienced weekly increases in adaptive emotion regulation strategies (a composite of reappraisal and acceptance use) and reductions in maladaptive strategies (e.g., avoidance, suppression) across treatment (Aldao, Jazaieri, Goldin, & Gross, 2014). They found that the strength of the relationship between maladaptive strategy use and social anxiety symptom severity depended on the frequency with which patients were also using adaptive skills, a result that is similar to the prospective nonclinical study described above (Aldao & Nolen-Hoeksema, 2012). Research involving clinical samples is essential insofar as results obtained from nonclinical samples may indicate different effect size estimates in primary relationships of interest (e.g., as evidenced by significant sample-type [clinical vs. nonclinical] moderation effects in Aldao et al., 2010) or have uncertain generalizability to individuals with significantly distressing psychopathology. Thus, this gap in the literature must be addressed to begin answering these pivotal clinical questions.
While research thus far has primarily examined changes in the specific skills targeted in treatment, less research has evaluated the influence of treatment on adaptive and maladaptive skill use more broadly. There is evidence, however, that psychological treatments can have relatively broad effects on emotion-regulation strategies, suggesting that strategies not directly targeted in treatment can also evidence improvement (Alvarez et al., 2011; Boswell, Anderson, & Barlow, 2014; Kocovski, Fleming, Hawley, Ho, & Antony, 2015). For example, one study found that cognitive processing therapy, which explicitly targets reframing of beliefs, also reduced reliance on emotion-avoidant strategies and increased access to positive coping strategies beyond reappraisal (Alvarez et al., 2011). It may be useful to consider the broad impact of our treatments, in addition to their narrow effects on targeted skills, as our understanding of the mechanisms through which treatments enact their benefit is still underdeveloped. It is possible that psychological treatments lead to unexpected positive benefits, such as the increase of non-targeted overt skill use (e.g., increased mindful awareness of thoughts in a mindfulness-based treatment leads to improved cognitive reappraisal) or less overt mechanisms of change (e.g., increased behavioral activation leading to reduced negative thinking, as seen in Jacobson et al., 1996). A better understanding of the pathways to symptom improvement can allow the field to hone in on core mechanisms of change, leading to more streamlined, efficient interventions.
To expand upon the current literature on the relationships between emotion regulation strategies and psychopathology, we modeled our analyses after Aldao and colleague's (2012) study. Building upon their findings in a nonclinical sample, we sought to examine the relationships between adaptive and maladaptive strategies in a sample of adults with comorbid anxiety and alcohol use disorders receiving cognitive-behavioral interventions. Like Aldao and Nolen-Hoeksema (2012), we assessed psychopathology severity broadly using assessments of depression symptoms, anxiety symptoms, and severity of alcohol cravings and related problems. We also utilized a similar (though not identical) assessment of adaptive and maladaptive emotion regulation skills using the Brief COPE (Carver, 1997).
The first goal of this study was to examine relationships between maladaptive and adaptive strategies and psychopathology cross-sectionally at both pre- and post-treatment. In line with Aldao and Nolen-Hoeksema's (2012) previous findings, we hypothesized that maladaptive strategies would be related to psychopathology prior to treatment, and that adaptive strategies would exhibit a weaker relationship with psychopathology. However, as our second assessment followed psychological treatment as opposed to just the passage of time, we predicted both adaptive and maladaptive strategies would be related to psychopathology at post-treatment. While more exploratory due to the lack of research on general emotion regulation skill use in the context of treatment, this hypothesis is consistent with the idea that patients who are able to respond to stressful situations with greater adaptive and fewer maladaptive strategies during treatment would also be experiencing lower psychopathology by the conclusion of therapy. We also explored whether there were interactions between use of adaptive and maladaptive strategies in predicting concurrent psychopathology, as found in Aldao and Nolen-Hoeksema's observations.
The second goal of the study was to assess whether initial levels of maladaptive and adaptive regulation strategies prospectively predicted psychopathology severity post-treatment. Again, in line with Aldao and Nolen-Hoeksema's (2012) results, we predicted that maladaptive strategies at pre-treatment would predict post-treatment levels of psychopathology. However, it was less clear whether initial levels of adaptive strategies would predict post-treatment levels of psychopathology in the context of treatment.
Additionally, we sought to explore dynamic relationships between adaptive and maladaptive strategy use and psychopathology across treatment. We predicted that both increases in adaptive strategies and decreases in maladaptive strategies would each independently relate to improvements in psychopathological symptoms over time. Finally, to extend previous findings from Aldao and Nolen-Hoeksema (2012) suggesting use of maladaptive strategies may moderate the impact of adaptive strategies on symptom levels, we chose to explore the interaction of pre-treatment maladaptive strategy use and adaptive strategy changes on psychopathology following a full course of treatment.
Method
Participants
Eighty-one patients with comorbid alcohol use and anxiety disorders completed a baseline assessment and were randomized to one of four treatment conditions. All diagnoses were made using DSM-IV criteria (American Psychiatric Association, 2000). Seventy-three (90.1%) patients were diagnosed with alcohol dependence and 8 (9.9%) were diagnosed with alcohol abuse. With respect to the comorbid anxiety disorders represented, 55 (67.9%) were diagnosed with generalized anxiety disorder, 41 (50.6%) were diagnosed with social phobia, and 8 (9.9%) were diagnosed with panic disorder. The patients' ages ranged from 18 to 64 (M = 43.6, SD = 10.6). The majority of participants identified as male (n = 63, 77.8%) and Caucasian (n = 70, 86.4%). Five patients (6%) identified as African American, and six patients (7.4%) identified as another race. Detailed information regarding the sample can be found in Ciraulo et al. (2013).
Measures
In the present study, the Brief COPE (Carver, 1997) was used to assess various strategies people use to cope with stressful situations. The Brief COPE is a self-report assessment that consists of 28 statements regarding how people respond to stressful situations. Participants rate how typical each statement is of them on a scale from one (“I usually don't do this at all”) to four (“I usually do this a lot”). The original Brief COPE contains 14 subscales: self-distraction, active coping, denial, substance use, use of emotional support, use of instrumental support, behavioral disengagement, venting, positive reframing, planning, humor, acceptance, religion, and self-blame. As detailed later, we included 13 of the 14 subscales in this study to create two composite scores: adaptive and maladaptive coping.
Depression symptom severity was assessed using the Hamilton Rating Scale for Depression (HAM-D; Hamilton, 1960) and the depression subscale of the Depression Anxiety and Stress Scale (DASS; Lovibond and Lovibond, 1995a). The HAM-D is a 17-item clinician-administered interview that has been used extensively in studies of depression (Demyttenaere & De Fruyt, 2002). In this study, the internal consistency at pre-treatment was good (α = .75). The DASS is a self-report measure, and the depression subscale contains 14 items. The DASS-depression subscale had excellent internal consistency in this study at pre-treatment (α = .95).
Anxiety symptom severity was assessed using the Hamilton Rating Scale for Anxiety (HAM-A; Hamilton, 1959) and the anxiety subscale of the DASS. The HAM-A is a 14-item clinician-administered interview. This measure has been used extensively in clinical trials as a measure of anxiety severity (Shear et al., 2001). Pre-treatment internal consistency for the HAM-A was good (α = .74). The DASS-anxiety subscale, like the DASS-depression subscale, is a 14-item self-report measure that exhibited good pre-treatment internal consistency in our sample (α = .87).
Alcohol craving and related problems were assessed with the Obsessive Compulsive Drinking Scale (OCDS; Anton, Moak, & Latham, 1995). The OCDS is a 14-item self-report measure that assesses drinking-related obsessions, automaticity of drinking, alcohol consumption, and interference due to drinking and is a widely used self-report measure of craving in alcohol research (Bohn, Barton, & Barron, 1996; Schmidt, Helten, & Soyka, 2011). This measure had good internal consistency in our sample (α = .84).
Procedures
The current study was conducted using data from a clinical trial, which utilized a 2×2 design to investigate the efficacy of 11 weekly sessions of transdiagnostic cognitive-behavioral therapy (the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders; Barlow, Allen, & Choate, 2004) versus progressive muscle relaxation combined with either venlafaxine or placebo as a treatment for patients with comorbid alcohol use and anxiety disorders (for full study description, see Ciraulo et al., 2013). The procedures of the aforementioned clinical trial were approved by Institutional Review Boards (IRBs) at the following institutions: Boston University, Boston University Medical Center, and Central Texas Veterans Health Care System. The data used in this study were collected at the pre- and post-treatment visits. In the current study, the effects of emotion regulation strategies on psychopathology were examined across treatment groups; when explored, there were no significant differences between groups on the observed relationships.
Variable creation
In order to emulate the research completed by Aldao et al., (2012), we created a psychopathology variable consisting of the DASS depression and anxiety subscales, HAM-A, HAM-D, and OCDS. All of these measures were significantly intercorrelated (all ps < .007). We standardized the scores on each measure and averaged them to create an overall psychopathology variable. The psychopathology variable showed good internal consistency (α = .81).
We also created adaptive and maladaptive strategy variables to examine the relationships between strategy use and psychopathology. The adaptive strategy variable was initially constructed by averaging items from the eight subscales identified as adaptive by Meyer (2001): active coping, planning, use of emotional support, use of instrumental support, positive reframing, acceptance, religion, and humor subscales. After examining inter-item correlations, we also included items from the venting subscale (originally considered maladaptive) because the items could reflect sharing emotions in the context of therapy as well as sharing emotions in a healthy way (e.g. “I've been saying things to let my unpleasant feelings escape” and “I've been expressing my negative feelings.”). Consistent with this interpretation, both venting items (or sharing emotions) exhibited item-total correlations of .34 with the adaptive strategy variable and exhibited low item-total correlations with the maladaptive variable (.10 for “letting feelings escape” and -.11 for “expressing my negative feelings”). The internal consistency for this subscale was acceptable (α = .80) and is slightly higher than when the measure does not include the “venting” subscale (α = .79).
The maladaptive strategy variable was initially constructed by averaging items from five of the six subscales (excluding venting) identified as maladaptive by Meyer (2001): denial, self-blame, self-distraction, behavioral disinhibition, and substance use. This initial maladaptive strategy variable had a Cronbach's alpha of .67. We elected to remove the items from the self-distraction subscale, as they exhibited low item-total correlations (rs = <.17). The resulting final maladaptive variable contained the denial, self-blame, behavioral disinhibition, and substance use subscales and had a Cronbach's alpha of .74. The adaptive and maladaptive variables were moderately correlated, r = -.28, p = .016.
Results
Cross-Sectional Analyses
Zero-order correlations
We first examined zero-order correlations between strategy use (adaptive and maladaptive) and psychopathology at both pre-treatment and post-treatment for the full sample. In line with Aldao and Nolen-Hoeksema (2012), we found that pre-treatment psychopathology was positively correlated with concurrent maladaptive strategy use, r = .51, p <.0001, but was not significantly correlated with concurrent adaptive strategy use, r = - .15, p = .17. Additionally, post-treatment psychopathology was significantly correlated with concurrent maladaptive strategy use, r = .61, p <.0001, and concurrent adaptive strategy use, r = - .32, p = .009, both in the expected directions.
Regression analyses
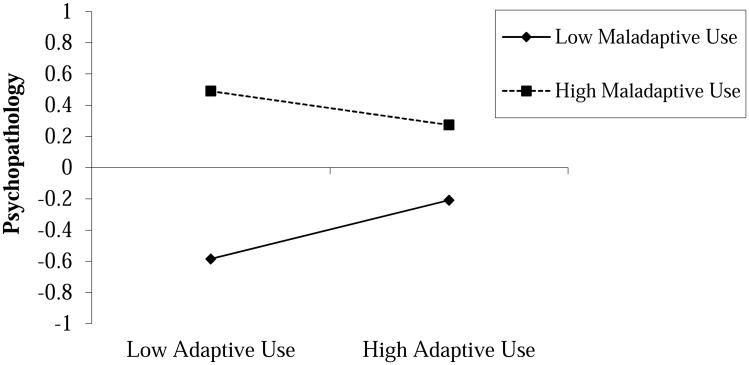
We then conducted hierarchical regression analyses to examine unique and interactive cross-sectional effects of adaptive and maladaptive strategies on psychopathology at both pre- and post-treatment. For pre-treatment, adaptive and maladaptive strategy variables were initially centered to reduce multicollinearity, and each centered variable was entered in the first step, R2 = .26, F(2, 72) = 12.96, p = <.0001. Consistent with correlational results, when both strategy variables were included in the model, maladaptive strategy use remained a significant predictor of psychopathology at pre-treatment, β = .52, t(72) = 4.95, p = <.0001, whereas adaptive strategy use continued to be a non-significant predictor, β = .02, t(72) = .21, p = .83. For the second step, the interaction term of adaptive and maladaptive strategy use was included. Somewhat consistent with previous research findings by Aldao and Nolen-Hoeksema (2012), there was a non-significant trend-level interaction between adaptive and maladaptive strategy use in predicting pre-treatment psychopathology, β = - .18, ΔR2 = .04, t(71) = - 1.78, p = .079. When plotting the simple slopes at ± 1 SD for maladaptive strategy use, the direction of the effects was consistent with Aldao and Nolen-Hoekema's finding that adaptive strategy use was negatively associated with psychopathology only at higher levels of maladaptive strategy use, see Figure 1. However, tests of the simple slopes indicated neither the slope for higher maladaptive strategy use (+ 1 SD) nor lower maladaptive strategy use (- 1 SD) was significantly different than zero in our sample, t(71) = - 1.03, p = .30 and t(71) = 1.52, p = .13, respectively.
Figure 1.
Cross-sectional trend-level interaction between adaptive and maladaptive strategy use at pre-treatment. High and low levels correspond to ±1 SD from the mean on their respective variables. Simple slope analyses indicated neither slope was significantly different from zero (ps > .13).
For post-treatment, adaptive and maladaptive variables were also centered and entered into the first step of our post-treatment regression analysis, R2 = .39, F(2,59) = 19.24, p = < .0001. Post-treatment maladaptive strategy use remained a significant predictor of concurrent post-treatment psychopathology, β = .56, t(59) = 5.38, p = < .0001, whereas post-treatment adaptive strategy use was not significantly predictive above and beyond the effects of maladaptive strategy use, β = -.17, t(59) = -1.66, p = .10. An interaction term of adaptive and maladaptive use was included in the second step, however results were non-significant, β = .04, ΔR2 = .00, t(58) = .35, p = .73.
Longitudinal (Prospective) Analyses
Correlations
We next examined the relationship between strategy use at pre-treatment and psychopathology scores at post-treatment. In contrast to the cross-sectional results, both pre-treatment adaptive and maladaptive strategy use were significantly correlated with psychopathology at post-treatment, r = - .29, p = .02 and r = .25, p = .048, respectively. When controlling for pre-treatment psychopathology, the strength of the relationship between post-treatment psychopathology and pre-treatment adaptive strategy use was slightly reduced and now at the level of a non-significant trend, r = - .24, p = .06. The relationship between pre-treatment maladaptive strategy use and post-treatment psychopathology, on the other hand, became nonsignificant after controlling for pre-treatment psychopathology, r = .05, p = .70.
Regression Analyses
Additional hierarchical regression analyses were conducted to examine whether there was an interaction between pre-treatment use of adaptive and maladaptive strategies as predictors of post-treatment psychopathology, controlling for pre-treatment psychopathology. In the first step, we entered pre-treatment psychopathology, pre-treatment maladaptive strategy use, and pre-treatment adaptive strategy use as predictors of post-treatment psychopathology, R2 = .195, F(3, 58) = 4.74, p = .005. Pre-treatment psychopathology was a significant predictor, β = .36, t(58) = 2.51, p = .015. Consistent with correlational analyses, pre-treatment adaptive strategy use predicted post-treatment psychopathology at the level of a nonsignificant trend when controlling for pre-treatment psychopathology and maladaptive strategy use, β = - .23, t(58) = -1,87, p = .067. Pre-treatment maladaptive strategy use was not significantly predictive of post-treatment psychopathology levels, β = - .004, t(58) = - .03, p = .98. The second step introduced the product term of adaptive and maladaptive strategy use at pre-treatment. There was no interaction between adaptive and maladaptive strategy use, β = .03, ΔR2 = .00, t(57) = .23, p = .82.
Changes in Emotion Regulation Strategies Across Treatment
We next sought to examine whether changes in strategy use across treatment groups were associated with post-treatment psychopathology or changes in psychopathology. 1 As a first step, we tested whether there were significant changes in adaptive and maladaptive strategy use from pre- to post-treatment. Maladaptive strategy use significantly improved from pre- to post-treatment (Pre: M = 2.44, SD = .52; Post: M = 2.00, SD = .56; d = .812, t[57] = 6.03, p < .0001), as did adaptive strategy use (Pre: M = 2.32, SD = .41; Post: M = 2.43, SD = .51; d = -.24, t[61] = -2.03, p = .046).3
Correlations
Residualized change scores from pre- to post-treatment were then calculated for adaptive, maladaptive, and psychopathology. Changes in maladaptive strategy use were significantly correlated with post-treatment psychopathology, r = .57, p < .0001, and changes in psychopathology scores over the course of treatment, r = .59, p < .0001. Changes in adaptive strategy use, on the other hand, were not associated with post-treatment psychopathology, r = - .14, p = .29, but were associated with changes in psychopathology at the level of a non-significant trend, r = - .25, p = .054.
Regression Analyses
We then examined the relative contributions adaptive and maladaptive residualized change scores as predictors of post-treatment psychopathology by entering both in the same model. Changes in maladaptive strategy use, but not changes in adaptive strategy use, were significantly and uniquely associated with post-treatment psychopathology, β = .57, t(55) = 5.08, p < .0001 and β = -.05, t(55) = -.41, p = .68, respectively. When controlling for pre-treatment psychopathology, changes in maladaptive strategy use continued to be a significant, unique predictor of post-treatment psychopathology, β = .48, t(54) = 5.00, p = < .0001, whereas changes in adaptive strategy use were associated with post-treatment psychopathology at the level of a non-significant trend, β = -.18, t(54) = -1.87, p = .067.
Relationships among Pre-Treatment Maladaptive Strategy Use and Changes in Adaptive Strategy Use as Predictors of Post-Treatment Psychopathology
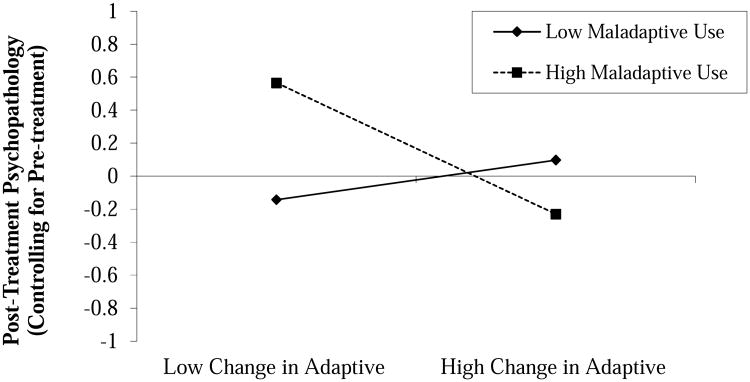
Finally, given our results were consistent with, though weaker than, the previously observed interactions by Aldao and Nolen-Hoeksema (2012) that suggest the use of adaptive skills confers a benefit for those with higher use of maladaptive strategies cross-sectionally, we wished to examine whether pre-treatment maladaptive skill use serves as a moderator between changes in adaptive strategies and post-treatment psychopathology. In other words, do changes in adaptive skill use during treatment predict post-treatment symptom levels differently depending on a patient's frequency of maladaptive skill use coming into treatment? We identified a significant interaction between pre-treatment maladaptive strategy use and changes in adaptive strategy use predicting post-treatment psychopathology, β = - .28, ΔR2 = .068, t(55) = - 2.19, p = .033. Controlling for pre-treatment psychopathology, we continued to find a significant interaction between these two variables when predicting post-treatment psychopathology, β = - .29, ΔR2 = .074, t(54) = - 2.57, p = .013, see Figure 2. A test of the simple slopes at ± 1 SD for pre-treatment maladaptive strategy use indicated that for individuals with higher use of maladaptive strategies at pre-treatment, change in adaptive strategies was important to predicting post-treatment psychopathology—individuals with less improvement in adaptive strategy use did significantly worse at post-treatment, whereas individuals with more improvement in adaptive strategy use had lower post-treatment psychopathology, t(54) = -3.55, p = .0008. Amongst individuals with lower use of maladaptive strategy use at pre-treatment (for whom post-treatment psychopathology was generally lower), there was not a significant effect of adaptive strategy use change on post-treatment psychopathology, t(54) = .79, p = .43.
Figure 2.
Interaction between pre-treatment maladaptive strategy use and changes in adaptive strategy use. High and low levels correspond to ±1 SD from the mean on their respective variables. Simple slope analyses indicated the slope for high maladaptive use was significantly different from zero (p = .0008), whereas the slope for low maladaptive use was not (p = .43).
Discussion
The purpose of the present study was to explore patterns of associations among the use of adaptive and maladaptive emotion regulation strategies and psychopathology before and after psychological treatment for individuals with alcohol use-disorders and co-occurring anxiety disorders. We first consider our results on the role of maladaptive strategy use in predicting psychopathology. As expected, in cross-sectional analyses, the use of maladaptive strategies (denial, self-blame, behavioral disinhibition, and substance use) was positively related to symptom severity at both pre- and post-treatment. This finding is consistent with a robust research literature implicating maladaptive strategy use and psychopathology (for a review, see: Aldao et al., 2010). In contrast, the use of maladaptive strategies at pre-treatment did not prospectively predict psychopathology at post-treatment, indicating initial levels of maladaptive strategy use are not a helpful indicator of patient prognosis above and beyond pre-treatment symptom severity. However, decreases in maladaptive strategies across treatment (change in this variable from pre- to post-treatment) were significantly related to decreases in psychopathology across treatment. Together, these findings suggest that when it comes to overall symptom improvement in treatment, successful reduction in a patient's use of maladaptive emotion regulation strategies is more important than their use of these strategies at the start of treatment.
Relationships between concurrent adaptive strategy use and psychopathology also yielded interesting results. Consistent with previous work in non-clinical samples (Aldao & Nolen-Hoeksema, 2012), we found that the use of adaptive regulation strategies was not significantly related to symptom severity prior to the start of treatment. While we identified a trend-level interaction suggesting that adaptive strategy use was associated with lower symptom severity only for individuals engaging in a higher degree of maladaptive coping, our finding was less robust in magnitude than Aldao and Nolen-Hoeksema's similar finding. These divergent results may reflect differences in the populations under study (a nonclinical versus a clinical sample of substance users). Low power for detecting interaction effects may also have contributed to these weaker results. Thus, our findings provide preliminary weak support for the pattern of interactions observed in their nonclinical sample, however further research into these relationships is warranted.
Additionally, adaptive strategy use both at pre-treatment and post-treatment was significantly associated with post-treatment symptom severity, though the strength of these effects were ultimately reduced to non-significance, either when controlling for the effects of pre-treatment psychopathology (for the relationship between pre-treatment adaptive strategy use and post-treatment psychopathology) or post-treatment maladaptive strategy use (for the relationship between post-treatment adaptive strategy use and psychopathology). Our findings suggest the use of adaptive strategies, at either pre- or post-treatment, are not incrementally useful predictors of how patients fare at the end of treatment above and beyond other indicators such as maladaptive use or symptom severity.
Despite the fact that pre-, post-, or changes in adaptive strategy use were not uniquely related to post-treatment symptom severity in the overall sample, greater increases in adaptive strategy use during the course of treatment were associated with lower symptom severity post-treatment among individuals with higher maladaptive strategy use at pre-treatment. On the other hand, for individuals with lower use of maladaptive strategies at the beginning of treatment, changes in adaptive strategy use were not related to post-treatment severity. It appears that changes in adaptive skill use during treatment are particularly beneficial for individuals that begin treatment with higher levels of maladaptive skill use. These particular findings in adaptive strategy use are consistent with a compensatory explanation of strategy use (e.g., Bonanno, Papa, O'Neill, Westphal, & Coifman, 2004), suggesting that greater flexibility and utilization of adaptive strategies in relevant circumstances may be related to lower psychopathology for those individuals who engage in more frequent use of maladaptive strategies.
The findings of the present study must, of course, be considered in the context of its limitations. First, it is important to note we examined a broad set of emotion regulation strategies, which do not all map onto the strategies targeted by the treatment approaches delivered in this study. For example, the COPE does not include a subscale that reflects the use of relaxation training that is taught in progressive muscle relaxation. It is possible that adaptive strategy use evidenced weaker relationships with other variables because our measure was limited in its ability to pick up changes in adaptive strategy use as a function of treatment. Future research should examine changes in intervention-specific strategies and more broad-based strategy use to better understand how our treatments are leading to symptom change. Secondly, we also examined participants engaged in two different treatments (a transdiagnostic cognitive-behavioral therapy and progressive muscle relaxation). While we did not observe significant effects of treatment condition, suggesting these relationships were not strikingly different across treatments, future research should be more adequately powered to examine unique effects of different treatment approaches and include measures that more closely reflect the emotion regulation skills presented. Finally, all measures were given only at pre- and post-treatment time points, making it difficult to make temporal inferences about the data. Specifically, despite an a priori theoretical rationale suggesting that changes in strategy use precedes changes in psychopathology, it is possible lowered symptoms may facilitate less reliance on maladaptive strategies or foster the use of adaptive strategies.
Despite these limitations, the findings of the present study have important implications for the effective utilization of patient assessment to inform optimal treatment. Consistent with previous research and longstanding rationale in clinical treatment, our results indicate maladaptive strategy use has strong relationships with psychopathology and reduced reliance on maladaptive strategies is associated with symptom improvements. Although the relationship between adaptive strategy use and psychopathology is less robust, the present findings suggest that greater change in adaptive strategies during treatment is associated with greater symptom improvements for individuals who begin treatment with more frequent use of maladaptive strategies. Conversely, for those individuals with less frequent use of maladaptive strategies, change in adaptive strategy use does not appear to confer a benefit. As such, care should be taken to assess patients' level of adaptive and maladaptive strategy usage at the outset of treatment in order to identify particular areas of strength and weakness in individual coping style. While emphasis on reducing maladaptive strategy use appears to be beneficial overall for reducing psychopathology, targeting increases in adaptive strategy use appears to be differentially beneficial depending on a patient's initial reliance on maladaptive strategy use. Given the complexity of these findings, future research is needed to confirm these findings and to establish recommendations regarding the circumstances under which clinicians should emphasize discontinuation of maladaptive strategy use predominately or also focus on building a repertoire of adaptive coping skills proportional to patients' presenting maladaptive skill use.
Highlights.
Examines adaptive and maladaptive emotion regulation strategy use in CBT.
Change in maladaptive, not adaptive, strategy use predicted lower psychopathology.
For patients with higher maladaptive strategy use, adaptive strategy change did predict lower psychopathology.
Findings emphasize importance of examining both adaptive and maladaptive skill use.
Acknowledgments
This study was supported by an NIAA grant (R01-AA013727) awarded to Domenic A. Ciraulo (Principal Investigator) and David H. Barlow (Investigator).
Footnotes
There were significant improvements in depression, anxiety, and craving from pre- to post-treatment, though no significant differences were observed between treatment conditions, see Ciraulo et al., (2013) for details of these analyses.
Reported ds are Becker's g ([Mpost-test - Mpre-test]/SDpre), which is a recommended alternative to Cohen's d for within-person mean comparisons (Kline, 2004).
To examine potential differences according to treatment group on changes in adaptive and maladaptive strategy use, we conducted two separate mixed ANOVA analyses with time-point (pre- and post) as the within-subject variable, treatment group (Unified Protocol versus progressive muscle relaxation) as the between-subject variable, and their interaction entered as predictors of adaptive and maladaptive strategy use. There were no interactions between treatment group and time-point for either maladaptive strategy use, t(133) = .31, p = .58, or adaptive strategy use, t(139) = .89, p = .38.
Conflicts of Interest: There are no other potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Laren R. Conklin, Boston University
Clair Cassiello-Robbins, Boston University.
C. Alex Brake, University of Kentucky.
Shannon Sauer-Zavala, Boston University.
Todd J. Farchione, Boston University
Domenic A. Ciraulo, Boston University Medical Center
David H. Barlow, Boston University
References
- Aldao A, Jazaieri H, Goldin PR, Gross JJ. Adaptive and maladaptive emotion regulation strategies: Interactive effects during CBT for social anxiety disorder. Journal of Anxiety Disorders. 2014;28(4):382–389. doi: 10.1016/j.janxdis.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research and Therapy. 2010;48(10):974–983. doi: 10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S. When are adaptive strategies most predictive of psychopathology? Journal of Abnormal Psychology. 2012;121(1):276–281. doi: 10.1037/a0023598. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30(2):217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Alvarez J, McLean C, Harris AS, Rosen CS, Ruzek JI, Kimerling R. The comparative effectiveness of cognitive processing therapy for male veterans treated in a VHA posttraumatic stress disorder residential rehabilitation program. Journal of Consulting and Clinical Psychology. 2011;79(5):590–599. doi: 10.1037/a0024466. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. 2000. text rev. [DOI] [Google Scholar]
- Anton RF, Moak DH, Latham P. The Obsessive Compulsive Drinking Scale: A self-rated instrument for the quantification of thoughts about alcohol and drinking behavior. Alcoholism: Clinical and Experimental Research. 1995;19(1):92–99. doi: 10.1111/j.1530-0277.1995.tb01475.x. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35(2):205–230. doi: 10.1016/S0005-7894(04)80036-4. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May J. Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York, NY, US: Oxford University Press; 2011. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: A cognitive perspective. New York, NY: Basic Books; 1985. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- Bohn MJ, Barton BA, Barron KE. Psychometric properties of the Obsessive Compulsive Drinking Scale. Alcoholism: Clinical and Experimental Research. 1996;20(5):817–823. doi: 10.1111/j.1530-0277.1996.tb05257.x. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Papa A, Lalande K, Westphal M, Coifman K. The importance of being flexible: The ability to both enhance and suppress emotional expression predicts long-term adjustment. Psychological Science. 2004;15:482–487. doi: 10.1111/j.0956-7976.2004.00705.x. [DOI] [PubMed] [Google Scholar]
- Boswell JF, Anderson LM, Barlow DH. An idiographic analysis of change processes in the unified transdiagnostic treatment of depression. Journal of Consulting and Clinical Psychology. 2014;82(6):1060–1071. doi: 10.1037/a0037403. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH, Brown TA, Hofmann SG. Acceptability and suppression of negative emotion in anxiety and mood disorders. Emotion. 2006;6(4):587–595. doi: 10.1037/1528-3542.6.4.587. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol's too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Ciraulo DA, Barlow DH, Gulliver S, Farchione T, Morissette SB, Kamholz BW, et al. Knapp CM. The effects of venlafaxine and cognitive behavioral therapy alone and combined in the treatment of co-morbid alcohol use-anxiety disorders. Behaviour Research and Therapy. 2013;51(11):729–735. doi: 10.1016/j.brat.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demyttenaere K, De Fruyt JUR. Getting what you ask for: on the selectivity of depression rating scales. Psychotherapy and Psychosomatics. 2002;72(2):61–70. doi: 10.1159/000068690. [DOI] [PubMed] [Google Scholar]
- Garnefski N, Kraaij V. Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Personality and Individual Differences. 2006;40(8):1659–1669. doi: 10.1016/j.paid.2005.12.009. [DOI] [Google Scholar]
- Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998;2(3):271–299. doi: 10.1037/1089-2680.2.3.271. [DOI] [Google Scholar]
- Gross JJ, Muñoz RF. Emotion regulation and mental health. Clinical Psychology: Science and Practice. 1995;2(2):151–164. doi: 10.1111/j.1468-2850.1995.tb00036.x. [DOI] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes M, Feldman G. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clinical Psychology: Science and Practice. 2004;11(3):255–262. doi: 10.1093/clipsy.bph080. [DOI] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY, US: Guilford Press; 1999. [Google Scholar]
- Hayes-Skelton SA, Calloway A, Roemer L, Orsillo SM. Decentering as a potential common mechanism across two therapies for generalized anxiety disorder. Journal Of Consulting and Clinical Psychology. 2015;83(2):395–404. doi: 10.1037/a0038305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Dobson KS, Truax P, Addis ME, Koerner K, Gollan JK, Gortner E, Prince SE. A component analysis of cognitive behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;64:295–304. doi: 10.1037/1522-3736.3.1.323a. [DOI] [PubMed] [Google Scholar]
- Keng S, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: A review of empirical studies. Clinical Psychology Review. 2011;31(6):1041–1056. doi: 10.1016/j.cpr.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Beyond significance testing: Reforming data analysis methods in behavioral research. Washington, DC, US: American Psychological Association; 2004. [Google Scholar]
- Kocovski NL, Fleming JE, Hawley LL, Ho MR, Antony MM. Mindfulness and acceptance-based group therapy and traditional cognitive behavioral group therapy for social anxiety disorder: Mechanisms of change. Behaviour Research and Therapy. 2015:7011–22. doi: 10.1016/j.brat.2015.04.005. [DOI] [PubMed] [Google Scholar]
- Kring AM, Sloan DM. Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment. New York, NY, US: Guilford Press; 2010. [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- Martin RC, Dahlen ER. Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Personality and Individual Differences. 2005;39(7):1249–1260. doi: 10.1016/j.paid.2005.06.004. [DOI] [Google Scholar]
- Meyer B. Coping with severe mental illness: Relations of the Brief COPE with symptoms, functioning, and well-being. Journal of Psychopathology and Behavioral Assessment. 2001;23(4):265–277. doi: 10.1023/A:1012731520781. [DOI] [Google Scholar]
- Mennin DS. Emotion Regulation Therapy for Generalized Anxiety Disorder. Clinical Psychology & Psychotherapy. 2004;11(1):17–29. doi: 10.1002/cpp.389. [DOI] [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100:569–582. doi: 10.1037/0021-843X.100.4.569. [DOI] [PubMed] [Google Scholar]
- Romero-Moreno RR, Márquez-González MM, Mausbach BT, Losada AA. Variables modulating depression in dementia caregivers: A longitudinal study. International Psychogeriatrics. 2012;24(8):1316–1324. doi: 10.1017/S1041610211002237. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York, NY, US: Guilford Press; 2002. [Google Scholar]
- Shear M, Vander Bilt J, Rucci P, Endicott J, Lydiard B, Otto MW, et al. Frank DM. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depression and Anxiety. 2001;13(4):166–178. doi: 10.1002/da.1033.abs. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Grekin ER. Alcohol and affect regulation. In: Gross JJ, editor. Handbook of emotion regulation. New York, NY, US: Guilford Press; 2007. pp. 560–580. [Google Scholar]
- Schmidt P, Helten C, Soyka M. Predictive value of obsessive-compulsive drinking scale (OCDS) for outcome in alcohol-dependent inpatients: Results of a 24-month follow-up study. Substance Abuse Treatment, Prevention, and Policy. 2011;6:14. doi: 10.1186/1747-597X-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobel Michael E. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological methodology. Washington, DC: American Sociological Society; 1982. pp. 290–312. [Google Scholar]
- Wegner DM, Schneider DJ, Carter SR, White TL. Paradoxical effects of thought suppression. Journal of Personality and Social Psychology. 1987;53(1):5–13. doi: 10.1037/0022-3514.53.1.5. [DOI] [PubMed] [Google Scholar]
- Wirtz CM, Hofmann SG, Riper H, Berking M. Emotion regulation predicts anxiety over a five - year interval: A cross - lagged panel analysis. Depression and Anxiety. 2014;31(1):87–95. doi: 10.1002/da.22198. [DOI] [PubMed] [Google Scholar]