Abstract
Background
Beach chair positioning during general anesthesia is associated with cerebral oxygen desaturation. Changes in cerebral oxygenation resulting from the interaction of inspired oxygen fraction, end-tidal carbon dioxide and anesthetic choice have not been fully evaluated in anesthetized patients in the beach chair position.
Methods
This was a prospective interventional within-group study of patients undergoing shoulder surgery in the beach chair position that incorporated a randomized comparison between two anesthetics. Fifty-six patients were randomized to receive desflurane or total intravenous anesthesia with propofol. Following induction of anesthesia and positioning, inspired oxygen fraction (Fio2) and minute ventilation were sequentially adjusted for all patients. Regional cerebral oxygenation (rSO2) was the primary outcome and was recorded at each of five set points.
Results
While maintaining Fio2 at 0.3 and end tidal carbon dioxide (PETCO2) at 30mmHg there was a decrease in rSO2 from 68%, SD 12 to 61%, SD 12 (p<0.001) following beach chair positioning. The combined interventions of increasing Fio2 to 1.0 and increasing Petco2 to 45mmHg resulted in a 14% point improvement in rSO2 to 75%, SD 12 (p <0.001) for patients anesthetized in the beach chair position. There was no significant interaction effect of the anesthetic at the study intervention points.
Conclusions
Increasing Fio2 and Petco2 resulted in a significant increase in rSO2 that overcomes desaturation in patients anesthetized in the beach chair position and that appears independent of anesthetic choice.
Introduction
Catastrophic neurological injury following anesthesia in the beach chair position has been reported in the literature1 and is thought to be due to cerebral hypoperfusion. Anatomic abnormalities in the Circle of Willis have been rarely discovered as the etiology2 and the majority of adverse events have occurred in healthy patients with recorded blood pressures that many anesthesiologists would consider acceptable.3
The measurement of regional cerebral oxygenation (rSO2) has been employed in routine clinical practice to detect cerebral desaturation in potential low-flow states for patients undergoing cardiac4 and vascular surgery.5,6 Monitoring of rSO2 in anesthetized patients undergoing surgery in beach chair position has been evaluated7 and revealed a high incidence of cerebral desaturation (rSO2 ≥ 20% below baseline).8 By measuring the relative concentrations of oxyhemoglobin and deoxyhemoglobin, cerebral near infra-red spectroscopy (NIRS) provides an estimate of the balance between cerebral oxygen supply and demand within the field of view.9
Reports in conscious volunteers10 and anesthetized patients without vascular disease11 demonstrate a relationship between rSO2 and both inspired oxygen fraction (Fio2) and end-tidal carbon dioxide (Petco2) . Observational data specifically captured during beach chair positioning suggest a relationship between Petco2 and rSO212 and, in a recent randomized controlled trial, ventilation at a higher Petco2 was associated with higher rSO2 values for patients anesthetized in the beach chair position.13
Anesthetic agents have distinct effects on cerebral hemodynamics and metabolism,14,15 which may have implications for beach chair positioning. Agents with greater preservation of cerebral blood flow (CBF) to cerebral metabolic rate for oxygen (CMRO2) ratio may allow for greater tolerance of cerebral hypoperfusion. Cerebral oxygenation appears better preserved in the beach chair position with a combination of sevoflurane-nitrous oxide compared to propofol-remifentanil16 yet the presence of either nitrous oxide or remifentanil could have confounded results for the primary anesthetics. In an additional study,17 rSO2 decreased less when using desflurane compared to propofol for the first 9 minutes of beach chair position but the desflurane group received thiopental for induction, which might have also confounded the results. The effect on rSO2 due to interactions between inspired gas composition and anesthetic choice is of clinical interest, especially when comparing propofol to desflurane, the halogenated ether with the greatest potential for cerebral vasodilatation.18
This study tested the hypothesis that modulation of Fio2 and Petco2 results in significant changes in rSO2 in patients anesthetized in the beach chair position. The influence of two anesthetic techniques with distinct effects on the cerebral vasculature was tested as a secondary outcome.
Materials and Methods
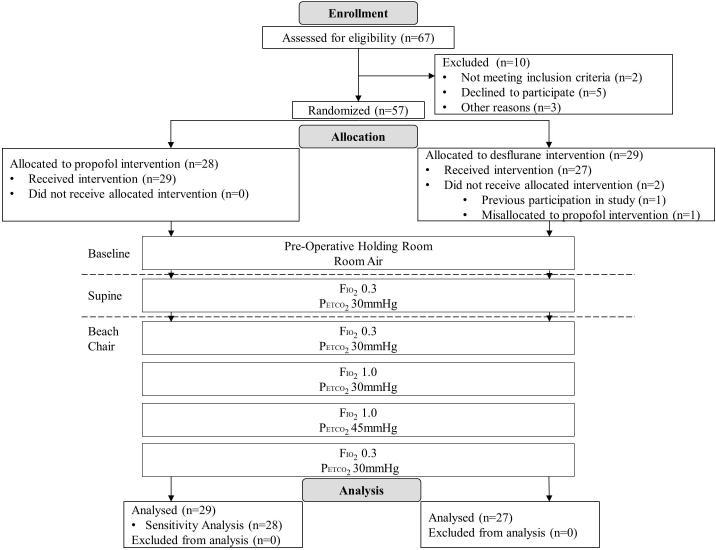
A detailed description of the study protocol (ClinicalTrials.gov No. NCT01535274) has previously been published.19 This was a prospective within-group study that incorporated a randomized comparison of two anesthetic regimens (figure 1). The study was approved by the Institutional Review Board of the University of Michigan, Ann Arbor, and written informed consent was obtained after a detailed discussion with patients regarding risks and benefits. The primary outcome was the effect of increasing Fio2 or Petco2 on rSO2 in patients anesthetized in the beach chair position. The secondary outcome was the effect of desflurane vs. propofol on ventilation-related changes in rSO2 and on cerebral desaturation in patients anesthetized in the beach chair position.
Figure 1.
Consort diagram illustrating the overall study design
Fio2 = Fraction of inspired oxygen; Petco2 = partial pressure of end-tidal carbon dioxide
Inclusion Criteria
We recruited adult patients scheduled for elective arthroscopic shoulder surgery in the beach chair position under general anesthesia with a supplemental interscalene brachial plexus block at an ambulatory surgery facility. All surgeries were conducted by a single surgeon (BSM); regional and general anesthetic procedures were conducted by a single anesthesiologist (AD). Patients were excluded if they refused to give consent, could not speak English, had contraindications for an interscalene brachial plexus block, or had a history of cardiovascular disease, cerebrovascular disease, respiratory failure, or hypertension determined by: 1) medical diagnosis, 2) the surrogate of pharmacologic treatment with an anti-hypertensive, or 3) a blood pressure measured in the surgical preoperative clinic of greater than 140/90.
Randomization and Blinding
Patients underwent computer-generated randomization to receive desflurane or total intravenous anesthesia (TIVA) with propofol for maintenance of anesthesia. These agents were chosen because of their differential effects on cerebral vasodilation, autoregulation and CO2 responsiveness.15,20,21 Patients and data analysts were blinded to the anesthetic choice; the anesthesiologist caring for the patient was blinded to rSO2 values. If the absolute rSO2 was < 55% or decreased from baseline by ≥ 20% the anesthesiologist was informed, as instructed by our Institutional Review Board.
Protocol
Baseline rSO2 was measured in the preoperative holding area with patients sitting and breathing room air. All patients had a single-shot, ultrasound-guided, interscalene brachial plexus block performed before induction of anesthesia (20ml 0.5% ropivacaine). The adequacy of the block was clinically assessed using a combination of motor and sensory evaluation before proceeding to the operating room. Patients were premedicated with midazolam 0.5-2mg; following preoxygenation, anesthesia was induced using fentanyl (1-2 mcg/kg) and propofol (0.5-2mg/kg). For muscle relaxation, a combination of succinylcholine and/or non-depolarizing muscle relaxants was used as was deemed clinically appropriate. The patient’s trachea was intubated, the lungs were ventilated and general anesthesia was maintained as dictated by randomization.
The primary interventions related to Fio2 and minute ventilation were sequentially adjusted to the following five set points:
1) Fio2 0.3 and Petco2 30mmHg – supine position.
2) Fio2 0.3 and Petco2 30mmHg – beach chair position.
3) Fio2 1.0 and Petco2 30mmHg – beach chair position.
4) Fio2 1.0 and Petco2 45mmHg – beach chair position.
5) Fio2 0.3 and Petco2 30mmHg – beach chair position.
The initial tidal volume was set at 6-8 cc/kg body weight and minute ventilation adjusted first by changing respiratory rate rather than manipulating tidal volume. Blood pressure was recorded by noninvasive cuff placed on the non-operative arm. No correction factor was applied to account for the difference in vertical height between the blood pressure measurement site and the Circle of Willis. All patients were placed at 80-90° in the beach chair position depending upon body habitus. The surrogate for depth of anesthesia was the Bispectral Index (BIS; Covidien, Boulder, CO), which was targeted to the range 40-60. Nitrous oxide could potentially confound results and was therefore avoided. The first measurement in the beach chair position (set point two) was obtained either, 1) 15 minutes after positioning, allowing the maximal decrease in rSO2 to occur,8 or 2) immediately if cerebral desaturation (defined as absolute value rSO2 < 55% or a decrease from baseline of ≥ 20%) was sustained for ≥ 3 minutes in either hemisphere. Since the change in rSO2 is typically complete and stable within 5 minutes following a change in inspired gas composition,5 rSO2 was recorded as a ‘snap shot’ after a minimum of 5 minutes at each subsequent set point. All cerebral desaturation events (absolute value rSO2 < 55% or a decrease from baseline of ≥ 20% sustained for ≥ 3 minutes) were recorded and communicated by the clinical coordinator to allow intervention as deemed appropriate by the anesthesiologist: exclude and treat hypotension, exclude and treat excessive depth of anesthesia, move to the next ventilation set point if that included increasing Fio2 or Petco2. If cerebral desaturation occurred moving from set point 4 to set point 5, rSO2 was recorded before full equilibrium had been reached and Fio2 and/or Petco2 were increased. Hematocrit was measured at the beginning and end of the study period (set point 1 and set point 5). Demographic and intraoperative data were retrieved from the patient’s electronic anesthetic and medical records.
Blood pressure management has been detailed in the published protocol.19 Briefly, either ephedrine (5mg) and/or phenylephrine (50-100mcg) were used as intravenous bolus medications for the treatment of intraoperative hypotension. If bolus dose phenylephrine was used first, we delayed the recording of results following a trial intervention by at least 8 minutes in order to allow rSO2 to normalize.22 For patients requiring more than 400mcg of phenylephrine during a 20 minute period, phenylephrine by infusion (200mcg/ml) was titrated to maintain blood pressure within 20% of preoperative mean arterial pressure (MAP).
Standard American Society of Anesthesiologists monitoring was used for all patients. The BIS Quatro electrode was placed diagonally on the patient’s left forehead. rSO2 was measured using the INVOS 5100C monitor (Covidien, Boulder, CO). Prior to induction of anesthesia, a single trained researcher applied optodes to either side of the forehead in conjunction with the BIS Quatro sensor as recommended by the manufacturer.
Sample Size and Statistical Analysis
The reported mean rSO2 is 67.1% ± 6.2 for patients placed in beach chair position.8 Based on a previous investigation,11 we expected a 6-8 percentage point difference in rSO2 due to the planned change in Fio2 and a 2-4 percentage point difference due to the planned change in Petco2. A total percentage point increase in excess of 10 was pre-specified19 as an outcome of clinical relevance. A sample size of 24 has a power of greater than 0.8 to detect a 4-5% increase in the planned pairwise comparisons related to the primary intervention of ventilation strategy. The power for the comparison between the two anesthetic regimens (48 subjects) is better than 85% for a difference of 6%, which was pre-specified19 as a clinically important difference for the secondary outcome.
Data were analyzed with a repeated-measures analysis of variance with ventilation strategy as the within-subjects factor (primary outcome) and anesthetic regimen as the between-subjects factor (secondary outcome). Residuals were assessed for normality and equal variances. A post hoc Tukey’s honest significant difference (HSD) procedure was used to correct for all pairwise comparisons between ventilation strategies. All analyses were performed using SPSS version 21.0 (SPSS inc., Chicago, IL). A p value of <0.05 was considered statistically significant.
Results
Study populations
Fifty-six patients were recruited and none were withdrawn (figure 1); all patients tolerated their procedure and recovered without complication. Twenty-eight patients were randomized to receive propofol and 28 patients were randomized to receive desflurane; secondary to the misallocation of one patient, 29 patients received propofol and 27 patients received desflurane. All patients had a functional brachial plexus block before leaving the preoperative holding area. None required supplementation with additional local anesthesia. There were no significant differences in patient characteristics or baseline data between groups (table 1). When patients were awake and breathing room air, the mean rSO2 on the left was 71%, SD 13, and on the right was 69%, SD 11. There was no significant difference in rSO2 between operative and nonoperative sides at any of the measurement points. There were three outliers, one in the desflurane group and two in the propofol group, who displayed mean room air rSO2 between 36 and 40%; none of the study or clinical interventions achieved a clinically meaningful increment in rSO2 in these patients. All patients were included for complete analysis.
Table 1.
Patient characteristics and baseline data.
| Propofol N=29 |
Desflurane N=27 |
||
|---|---|---|---|
|
| |||
| N (%) | N (%) | p-value** | |
| Sex | 0.945 | ||
| Female | 11 (37.9) | 10 (37.0) | |
| Male | 18 (62.1) | 17 (63.0) | |
| ASA Physical Status | 0.899 | ||
| 1 | 8 (27.6) | 6 (22.2) | |
| 2 | 20 (69.0) | 20 (74.1) | |
| 3 | 1 (3.4) | 1 (3.7) | |
| BMI Category* | 0.176 | ||
| Normal (18.5-24.9) | 7 (24.1) | 4 (14.8) | |
| Overweight (25.0-29.9) | 14 (48.3) | 9 (33.3) | |
| Obese (≥30.0) | 8 (27.6) | 14 (51.9) | |
| Smoking Status | 0.419 | ||
| Non-Smoker | 23 (79.3) | 19 (70.4) | |
| Previous Smoker | 4 (13.8) | 3 (11.1) | |
| Current Smoker | 2 (6.9) | 5 (18.5) | |
| Comorbidities | |||
| Sleep Apnea | 8 (27.6) | 5 (18.5) | 0.422 |
| Hypercholesterolemia | 5 (17.2) | 2 (7.4) | 0.424 |
| Asthma/COPD | 7 (24.1) | 3 (11.1) | 0.299 |
| Diabetes | 1 (3.4) | 0 | 1.000 |
| Heart Disease | 0 | 0 | N/A |
| Medications | |||
| Beta Adrenergic Blockers | 0 | 1 (3.7) | 0.482 |
| Calcium Channel Blockers | 2 (6.9) | 2 (7.4) | 1.000 |
| ACE Inhibitors | 0 | 0 | N/A |
| Angiotensin Receptor Blockers | 0 | 0 | N/A |
| Diuretics | 0 | 0 | N/A |
|
| |||
| Mean (SD) | Mean (SD) | p-value** | |
|
| |||
| Age (yrs) | 51.3 (10.0) | 49.3 (13.3) | 0.524 |
| Baseline Systolic Blood Pressure | 124.3 (15.4) | 123.2 (11.7) | 0.775 |
| Baseline Diastolic Blood Pressure | 74.8 (8.3) | 73.0 (9.1) | 0.432 |
| Baseline Left rSO2 | 71.0 (13.0) | 70.3 (11.4) | 0.831 |
| Baseline Right rSO2 | 69.1 (11.3) | 68.4 (9.8) | 0.798 |
Note. ACE = Angiotensin-Converting-Enzyme; ASA = American Society of Anesthesiologists; BMI = Body Mass Index; COPD = Chronic Obstructive Pulmonary Disease; rSO2 = Regional Cerebral Oxygen Saturation.
BMI categories based on World Health Organization classification.
P-values calculated using Pearson Chi-Square or Fisher’s Exact Test as appropriate for categorical variables, and a t-test for continuous variables.
Influence of beach chair positioning on rSO2
While maintaining Fio2 0.3 and Petco2 30mmHg there was a decrease in rSO2 from 68%, SD 12 to 61%, SD 12, p<0.001 following beach chair positioning when compared to stable supine patients with the same ventilation parameters for the combined data set (table 2).
Table 2.
Regional cerebral oxygenation (rSO2) values (mean ± standard deviation) at the set ventilatory points of the study for the study group and for each anesthetic choice.
| Supine | Beach Chair | ||||
|---|---|---|---|---|---|
|
| |||||
| Set Point 1 | Set Point 2 | Set Point 3 | Set Point 4 | Set Point 5 | |
| Fio2 0.3 Petco2 30 mmHg |
Fio2 0.3 Petco2 30 mmHg |
Fio2 1.0 Petco2 30 mmHg |
Fio2 1.0 Petco2 45 mmHg |
Fio2 0.3 Petco2 30 mmHg |
|
| Combined N=56 |
68 ± 12 | 61 ± 12 (p<0.001) |
66 ± 12 (p<0.001) |
75 ± 12 (p<0.001) |
65 ± 13 (p<0.001) |
| Propofol N=29 |
67 ± 13 | 59 ± 13 (p<0.001) |
64 ± 14 (p<0.001) |
74 ± 12 (p<0.001) |
64 ± 14 (p<0.001) |
| Desflurane N=27 |
69 ± 11 | 62 ± 10 (p<0.001) |
67 ± 11 (p<0.001) |
76 ± 11 (p<0.001) |
67 ± 12 (p<0.001) |
Fio2 = Fraction of inspired oxygen; Petco2 = partial pressure of end-tidal carbon dioxide
P-values represent comparison of successive set points within anesthetic type (ie: Set Point 1 compared to Set Point 2, Set Point 2 compared to Set Point 3, etc).
Influence of ventilation strategy on rSO2
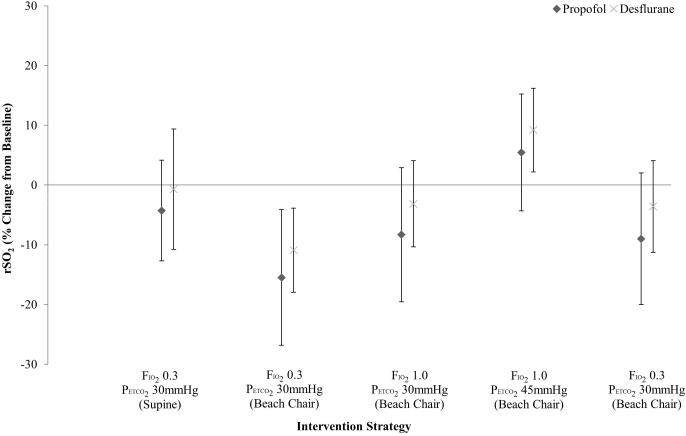
The overall repeated measures ANOVA, including the first 5 set points, revealed that ventilation strategy had a significant within-subjects effect on rSO2, p<0.001. While maintaining Petco2 at 30mmHg, rSO2 improved by 5% points when Fio2 1.0 was delivered compared to Fio2 0.3 (mean 66%, SD 12 vs. mean 61%, SD 12, p < 0.001). At 1.0 inspired oxygen fraction an additional 9% point improvement was observed at Petco2 45mmHg when compared to Petco2 30mmHg (mean 75%, SD 12 vs. 66%, SD 12, p < 0.001). A total increment of 14% points was achieved comparing Fio2 0.3 and Petco2 30mmHg (mean 61%, SD 12) to Fio2 1.0 and Petco2 45mmHg (mean 75%, SD 12) in the beach chair position, p < 0.001. This value is also 7% points higher than that measured in supine anesthetized patients at Fio2 0.3 and Petco2 30mmHg (mean 75%, SD 12 vs. mean 68%, SD 12, p < 0.001). With the exception of the three outliers, all patients responded consistently to the changes in ventilation strategy with the same direction of change in rSO2. Table 2 summarizes the rSO2 during the trial interventions for the combined sample and for each anesthetic choice. Figure 2 illustrates the percentage change from baseline rSO2.
Figure 2.
Percentage change from baseline rSO2 at each study point for propofol and desflurane groups.
Fio2 = Fraction of inspired oxygen; Petco2 = partial pressure of end-tidal carbon dioxide; rSO2 = Regional cerebral oxygenation
Influence of anesthetic regimen on rSO2
There was no significant interaction effect of the anesthetic on rSO2 as a between-subjects factor at the study intervention points. Ten patients in the propofol group and 9 in the desflurane group exhibited rSO2 < 55% or a decrease from baseline of ≥ 20% sustained for ≥ 3 minutes in either hemisphere, necessitating an early increase in Fio2 to 1.0 during the first 15 minutes following beach chair positioning. There was no statistically significant difference in cerebral desaturation rate between groups.
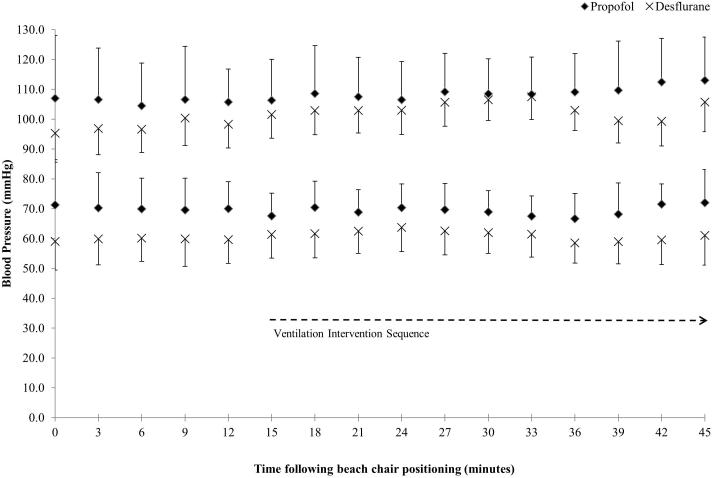
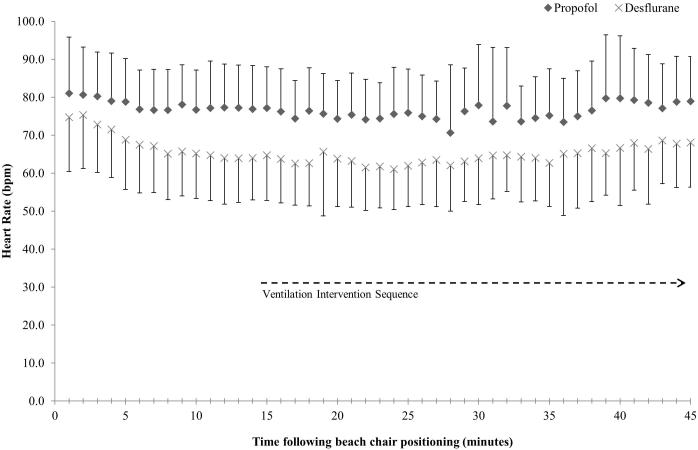
Controlling for BIS values, anesthetic concentrations, hemodynamics and hematocrit
The mean time interval between interventions 1 and 2 was 16 minutes (SD 5), between 2 and 3 was 10 minutes (SD 3), between 3 and 4 was 12 minutes (SD 3) and between 4 and 5 was 10 minutes (SD 2). The mean BIS at each study intervention point was held within 2 points of the lower limit of our target range (40) for the combined sample (table 3). There was no difference in BIS as a between-subjects factor when comparing the propofol and desflurane groups. There was no statistically significant change in either propofol infusion rate or end-tidal desflurane throughout the study (table 4). There was no statistically significant change in systolic or diastolic blood pressure throughout the intervention period in either the propofol or desflurane groups. There was no statistically significant difference in systolic blood pressure during the intervention period seen between the propofol and desflurane groups but the diastolic blood pressure was consistently and significantly lower in the desflurane group when analyzed as a between-subjects factor, p = 0.001 (figure 3). The mean difference seen in diastolic blood pressure throughout the intervention period was 11 mmHg. There was no significant variation in heart rate throughout the intervention period but heart rate was consistently lower in the desflurane group, mean 77 (propofol) vs. 65 (desflurane) beats per minute, p = 0.002 (figure 4). There was no significant difference in the number of patients receiving ephedrine as a bolus medication 8 (propofol) vs. 10 (desflurane), the total number of doses 14 (propofol) vs. 18 (desflurane), or the total dose 70 mg (propofol) vs. 90 mg (desflurane), administered during the study period to each of the anesthetic groups when considered as entire groups. There was no significant difference in the number of patients receiving phenylephrine as a bolus medication (5 in the propofol group, 7 in the desflurane group within the intervention period). The total number of phenylephrine doses (17 vs. 31) and the total dose (1000 mg vs. 1800 mg) administered to each group, throughout the study period were both significantly higher in the desflurane group, p < 0.01. No patient required phenylephrine by infusion. There was a statistically significant difference between hematocrit measured at set point 1 (median 43, IQR 38-46) and set point 5 (median 41, IQR 38-44, p=0.001).
Table 3.
BIS values (mean ± standard deviation) at the set ventilatory points of the study for the study group and for each anesthetic choice.
| Supine | Beach Chair | ||||
|---|---|---|---|---|---|
|
| |||||
| Set Point 1 | Set Point 2 | Set Point 3 | Set Point 4 | Set Point 5 | |
| Fio2 0.3 Petco2 30 mmHg |
Fio2 0.3 Petco2 30 mmHg |
Fio2 1.0 Petco2 30 mmHg |
Fio2 1.0 Petco2 45 mmHg |
Fio2 0.3 Petco2 30 mmHg |
|
| Combined N=56 |
38 ± 10 | 41 ± 11 (p=0.04) |
39 ± 9 (p=0.15) |
42 ± 8 (p=0.04) |
39 ± 8 (p=0.01) |
| Propofol N=29 |
42 ± 11 | 42 ± 13 (p=0.86) |
40 ± 11 (p=0.23) |
42 ± 10 (p=0.18) |
41 ± 10 (p=0.27) |
| Desflurane N=26* |
34 ± 7 | 40 ± 8 (p=0.04) |
39 ± 4 (p=0.40) |
41 ± 6 (p=0.03) |
38 ± 5 (p<0.01) |
BIS = Bispectral index; Fio2 = Fraction of inspired oxygen; Petco2 = partial pressure of end-tidal carbon dioxide
One patient with missing BIS data.
P-values represent comparison of successive set points within anesthetic type (ie: Set Point 1 compared to Set Point 2, Set Point 2 compared to Set Point 3, etc).
Table 4.
Propofol infusion (mean ± standard deviation) and end-tidal desflurane (mean ± standard deviation) at the set ventilatory points.
| Supine | Beach Chair | ||||
|---|---|---|---|---|---|
|
| |||||
| Set Point 1 | Set Point 2 | Set Point 3 | Set Point 4 | Set Point 5 | |
| Fio2 0.3 Petco2 30 mmHg |
Fio2 0.3 Petco2 30 mmHg |
Fio2 1.0 Petco2 30 mmHg |
Fio2 1.0 Petco2 45 mmHg |
Fio2 0.3 Petco2 30 mmHg |
|
| Propofol Infusion Rates (mcg/kg/min) N=29 |
108.8 ± 25.5 | 115.9 ± 16.4 | 114.7 ± 17.3 | 112.2 ± 17.3 | 108.7 ± 19.4 |
| End-tidal Desflurane (%) N=27 |
4.4 ± 0.9 | 4.7 ± 0.8 | 4.8 ± 0.8 | 4.6 ± 0.8 | 5.0 ± 0.7 |
Fio2 = Fraction of inspired oxygen; Petco2 = partial pressure of end-tidal carbon dioxide
Figure 3.
Mean systolic and diastolic blood pressure, with one standard deviation, throughout the intervention period for the propofol and desflurane groups.
Figure 4.
Mean heart rate, with one standard deviation, throughout the study period for propofol and desflurane groups
bpm = Beats per Minute
Sensitivity Analysis
The misallocation carried the potential to impact the results of the secondary outcome; one patient in the propofol group was excluded from the sensitivity analysis of the remaining fifty-five patients (28 in the propofol group and 27 in the desflurane group). The analysis revealed no significant differences compared to the full study population. As in the complete cohort, the increase in Fio2 and Petco2 resulted in a significant increase in rSO2 (p<0.001 for comparisons of each consecutive set-point), which was independent of anesthetic choice (p=0.513).
Discussion
The results of this dynamic interventional study demonstrate that simple modulation of inspired gas composition leads to an elevation in rSO2 for patients anesthetized in the beach chair position. The magnitude (14 percentage points) of the combined intervention not only increased rSO2 but did so to a level surpassing that measured in the supine position. The relative increments seen with increasing Fio2 and Petco2 were 5 and 9% points respectively. Except for three outliers who demonstrated low baseline cerebral saturations, the responses were consistent throughout our study population. The results are not only highly statistically significant but have also exceeded–our prespecified threshold for clinical relevance.19 The data can help guide the clinical management of patients anesthetized in the beach chair position and prioritize interventions for the treatment of cerebral desaturation. Our results also demonstrate that ventilation strategy is a more powerful intervention to improve rSO2 than anesthetic choice. In this study, there was no significant interaction effect of the two anesthetics studied as a between-subjects factor at the study intervention points. The lack of an anesthetic effect in our research is a potentially generalizable observation, given the relative effects of propofol and desflurane on CBF:CMRO2 ratio.
It is important to note that the functional relevance of rSO2 changes was not evaluated in this study and the risk of cerebrovascular compromise with beach chair positioning is unclear. Overt stroke was not reported in a retrospective evaluation of more than 5000 patients anesthetized in the sitting position. The intraoperative mean arterial pressure (MAP) of that population was maintained at approximately 75mmHg or greater.23 However, the interpretation of this value is problematic because cerebral autoregulation is attenuated (CBF becomes more dependent on systemic blood pressure) with a wide range of MAP at the lower limit of autoregulation24 during anesthesia in the beach chair position. Until the lower limit of autoregulation can be routinely monitored, blood pressure control alone cannot be assumed sufficient to protect patients from neurological injury during anesthesia in the beach chair position.
The modulation of inspired gas composition has been previously shown to improve cerebral oxygenation measured by NIRS in awake subjects,10 healthy supine anesthetized patients11 and in patients undergoing carotid endarterectomy with either general or regional anesthesia.5,6 Increasing Fio2 during carotid endarterectomy with regional anesthesia has also been reported to reverse neurological deficits seen with carotid cross clamp placement.25 Our results are consistent with these data as well as with findings from the static comparison of two Petco2 ranges in the beach chair position;13 rSO2 was better preserved with fewer cerebral desaturation events at the higher Petco2 range. However, our study advances the field by demonstrating that interventions related to carbon dioxide can help reverse decreases in rSO2 in the beach chair position, supporting a causal influence. The partial pressure of arterial carbon dioxide (PaCO2) is a direct determinant of CBF;26 the impact upon cerebral autoregulation remains to be fully elucidated. The combination of hypocapnia and hypotension is particularly associated with cerebral desaturation, as measured by NIRS, during anesthesia in the beach chair position.13
The measurement of cerebral oxygenation by NIRS and its application to patients anesthetized in the beach chair position remains controversial. There is wide intersubject variability but a change is considered to be of greater significance than baseline readings.9 Reductions below 50% absolute value27,28 and reductions of ≥ 20% from baseline29-32 have been associated with cerebral ischemia. Reductions of similar magnitude have been measured in patients placed in the beach chair position using the INVOS12 and FORE-SITE13 series of cerebral oximeters but was not detected when NIRO instruments have been used33 in this context. As the three outliers from our study demonstrate, patients may exhibit rSO2 below 50% or exhibit a reduction of ≥20% from baseline without any other correlate of cerebral ischemia. The INVOS system is susceptible to extracranial signal contamination34 but data gained during sequential clamping of the external and internal carotid artery suggest that the signal is predominantly intracranial in origin.35 Near infrared light penetrates the grey matter by a few millimeters36 and therefore oxygenation is measured only in the superficial cortex. Cerebral oximetry values are impacted by systemic blood pressure,37 sensor location,38 anesthetic depth for vapor-based anesthetic techniques39 and hematocrit.38 The cerebral a:v ratio is assumed constant within device algorithms and therefore rSO2 can vary without a true change in cerebral oxygenation.
When making a choice between general anesthetic agents for patients with potential cerebral hypoperfusion, the balance between cerebral blood supply and oxygen demand is of logical importance. In our study, statistical significance was not achieved for any difference relating to anesthetic choice but this potentially relates to the particular monitor used. Differences in cerebral saturation measured by an alternative methodology may have been detected. It is interesting to note that diastolic blood pressure and heart rate were consistently lower within the desflurane group and that, although a similar number of patients within both anesthetic groups required bolus dose ephedrine and phenylephrine, the total number of doses and the total dose of phenylephrine was higher in the desflurane group. Per the study protocol, measurements were avoided following phenylephrine bolus medication to avoid the potentially confounding effect on rSO2 seen with this drug. However, differences in hemodynamic control between the two groups may have confounded the comparison between anesthetic methodologies. There are insufficient data to help estimate the potential change in rSO2 caused by heart rate. Diastolic blood pressure shows positive correlation, approximately 1-2% per 10mmHg, with cerebral oximetry in congestive heart failure.40 It is possible that a similar relationship exists in patients without heart failure or those in the beach chair position, but this has not been determined.
There are a number of limitations to this study. The anesthesiologist was informed of cerebral desaturation when it occurred, thus allowing for protocol modification that may have impacted the results. The measured lower level of rSO2 with beach chair positioning was potentially limited, and therefore, we may have underestimated the magnitude of the response subsequent to increasing Fio2 and Petco2. We waited for stability in rSO2 following manipulation of ventilation and inspired oxygen before recording, with a mean time between measurements of 10 minutes or greater, but it is possible that brain equilibrium was not complete at the time of data measurement. More precise reporting of respiratory gases and blood pressure could have been facilitated by the placement of intra-arterial catheters. A small number of active smokers and patients with airway disease were included; Petco2 may not have reliably reflected PaCO2 in these patients. However, we have demonstrated predictable increments in both PaO2 and PaCO2 with similar inspired gas modulation in previous studies6 and, for healthy individuals, Petco2 provides a reliable estimate of PaCO2.41 Invasive blood pressure measurement with the transducer zeroed at the level of the Circle of Willis would have compensated for differences in patient height and the angle of beach chair placement (which could have confounded the secondary outcome) and would have allowed better appreciation of changes in cerebral perfusion pressure. Our initial plan19 involved the measurement of hematocrit at each set point. This proved practically difficult during the first few subjects so the protocol was amended to include a hematocrit check at points 1 and 5 only. It is possible that the small statistically significant negative change in hematocrit (median 43 to 41) during the entire study period blunted the effect of our interventions designed to improve rSO238 but the impact in all likelihood is clinically negligible. Unmeasured potential confounders include cerebral a:v ratio and cerebral metabolic rate for oxygen, which present major challenges for data interpretation based upon cerebral NIRS methodology.
In conclusion, increasing Fio2 and Petco2 resulted in a reliable and measureable increase in rSO2 that overcame cerebral desaturation associated with general anesthesia in the beach chair position. Furthermore, ventilation strategy had a greater influence on rSO2 than choice of anesthetic.
Acknowledgments
Financial support:
Supported by the National Center for Advancing Translational Sciences of the National Institutes of Health, Bethesda, MD under Award Number UL1TR000433,
The INVOS 5100C cerebral oxygenation and BIS monitor were lent for this project and cerebral oxygenation optodes were provided at no cost by the manufacturer (Covidien, Boulder, CO).
Additional funding was gained from the Department of Anesthesiology, University of Michigan.
Footnotes
Conflict of interest for all authors: The authors declare no competing interests.
Trial Registration: NCT01535274
References
- 1.Pohl A, Cullen DJ. Cerebral ischemia during shoulder surgery in the upright position: a case series. J Clin Anesth. 2005;17:463–9. doi: 10.1016/j.jclinane.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 2.Drummond JC, Lee RR, Howell JP., Jr. Focal cerebral ischemia after surgery in the "beach chair" position: the role of a congenital variation of circle of Willis anatomy. Anesth Analg. 2012;114:1301–3. doi: 10.1213/ANE.0b013e31823aca46. [DOI] [PubMed] [Google Scholar]
- 3.Cullen DJ, Kirby RR. Beach chair position may decrease cerebral perfusion: Catastrophic outcomes have occurred. APSF Newsletter. 2007;22:25–27. [Google Scholar]
- 4.Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009;103(Suppl 1):i3–13. doi: 10.1093/bja/aep299. [DOI] [PubMed] [Google Scholar]
- 5.Stoneham MD, Lodi O, de Beer TC, Sear JW. Increased oxygen administration improves cerebral oxygenation in patients undergoing awake carotid surgery. Anesth Analg. 2008;107:1670–5. doi: 10.1213/ane.0b013e318184d6c3. [DOI] [PubMed] [Google Scholar]
- 6.Picton P, Chambers J, Shanks A, Dorje P. The influence of inspired oxygen fraction and end-tidal carbon dioxide on post-cross-clamp cerebral oxygenation during carotid endarterectomy under general anesthesia. Anesth Analg. 2010;110:581–7. doi: 10.1213/ANE.0b013e3181c5f160. [DOI] [PubMed] [Google Scholar]
- 7.Fischer GW, Torrillo TM, Weiner MM, Rosenblatt MA. The use of cerebral oximetry as a monitor of the adequacy of cerebral perfusion in a patient undergoing shoulder surgery in the beach chair position. Pain Pract. 2009;9:304–7. doi: 10.1111/j.1533-2500.2009.00282.x. [DOI] [PubMed] [Google Scholar]
- 8.Murphy GS, Szokol JW, Marymont JH, Greenberg SB, Avram MJ, Vender JS, Vaughn J, Nisman M. Cerebral oxygen desaturation events assessed by near-infrared spectroscopy during shoulder arthroscopy in the beach chair and lateral decubitus positions. Anesth Analg. 2010;111:496–505. doi: 10.1213/ANE.0b013e3181e33bd9. [DOI] [PubMed] [Google Scholar]
- 9.Casati A, Spreafico E, Putzu M, Fanelli G. New technology for noninvasive brain monitoring: continuous cerebral oximetry. Minerva Anestesiol. 2006;72:605–25. [PubMed] [Google Scholar]
- 10.Tisdall MM, Taylor C, Tachtsidis I, Leung TS, Elwell CE, Smith M. The effect on cerebral tissue oxygenation index of changes in the concentrations of inspired oxygen and end-tidal carbon dioxide in healthy adult volunteers. Anesth Analg. 2009;109:906–13. doi: 10.1213/ane.0b013e3181aedcdc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Picton P, Shanks A, Dorje P, Mashour GA. The influence of basic ventilation strategies on cerebral oxygenation in anesthetized patients without vascular disease. J Clin Monit Comput. 2010;24:421–425. doi: 10.1007/s10877-010-9265-x. [DOI] [PubMed] [Google Scholar]
- 12.Moerman AT, De Hert SG, Jacobs TF, De Wilde LF, Wouters PF. Cerebral oxygen desaturation during beach chair position. Eur J Anaesthesiol. 2012;29:82–7. doi: 10.1097/EJA.0b013e328348ca18. [DOI] [PubMed] [Google Scholar]
- 13.Murphy GS, Szokol JW, Avram MJ, Greenberg SB, Shear TD, Vender JS, Levin SD, Koh JL, Parikh KN, Patel SS. Effect of ventilation on cerebral oxygenation in patients undergoing surgery in the beach chair position: a randomized controlled trial. Br J Anaesth. 2014;113:618–27. doi: 10.1093/bja/aeu109. [DOI] [PubMed] [Google Scholar]
- 14.Iwata M, Inoue S, Kawaguchi M, Takahama M, Tojo T, Taniguchi S, Furuya H. Jugular bulb venous oxygen saturation during one-lung ventilation under sevoflurane- or propofol-based anesthesia for lung surgery. J Cardiothorac Vasc Anesth. 2008;22:71–6. doi: 10.1053/j.jvca.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 15.Mielck F, Stephan H, Buhre W, Weyland A, Sonntag H. Effects of 1 MAC desflurane on cerebral metabolism, blood flow and carbon dioxide reactivity in humans. Br J Anaesth. 1998;81:155–60. doi: 10.1093/bja/81.2.155. [DOI] [PubMed] [Google Scholar]
- 16.Jeong H, Jeong S, Lim HJ, Lee J, Yoo KY. Cerebral oxygen saturation measured by near-infrared spectroscopy and jugular venous bulb oxygen saturation during arthroscopic shoulder surgery in beach chair position under sevoflurane-nitrous oxide or propofol-remifentanil anesthesia. Anesthesiology. 2012;116:1047–56. doi: 10.1097/ALN.0b013e31825154d2. [DOI] [PubMed] [Google Scholar]
- 17.Kim JY, Lee JS, Lee KC, Kim HS, Kim SH, Kwak HJ. The effect of desflurane versus propofol on regional cerebral oxygenation in the sitting position for shoulder arthroscopy. J Clin Monit Comput. 2014;28:371–6. doi: 10.1007/s10877-013-9543-5. [DOI] [PubMed] [Google Scholar]
- 18.Holmstrom A, Akeson J. Cerebral blood flow at 0.5 and 1.0 minimal alveolar concentrations of desflurane or sevoflurane compared with isoflurane in normoventilated pigs. J Neurosurg Anesthesiol. 2003;15:90–7. doi: 10.1097/00008506-200304000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Picton P, Dering A, Miller B, Shanks A, Mashour GA. The influence of basic ventilation strategies and anesthetic techniques on cerebral oxygenation in the beach chair position: study protocol. BMC Anesthesiol. 2012;12:23. doi: 10.1186/1471-2253-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conti A, Iacopino DG, Fodale V, Micalizzi S, Penna O, Santamaria LB. Cerebral haemodynamic changes during propofol-remifentanil or sevoflurane anaesthesia: transcranial Doppler study under bispectral index monitoring. Br J Anaesth. 2006;97:333–9. doi: 10.1093/bja/ael169. [DOI] [PubMed] [Google Scholar]
- 21.McCulloch TJ, Visco E, Lam AM. Graded hypercapnia and cerebral autoregulation during sevoflurane or propofol anesthesia. Anesthesiology. 2000;93:1205–9. doi: 10.1097/00000542-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Meng L, Cannesson M, Alexander BS, Yu Z, Kain ZN, Cerussi AE, Tromberg BJ, Mantulin WW. Effect of phenylephrine and ephedrine bolus treatment on cerebral oxygenation in anaesthetized patients. Br J Anaesth. 2011;107:209–17. doi: 10.1093/bja/aer150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pin-on P, Schroeder D, Munis J. The hemodynamic management of 5177 neurosurgical and orthopedic patients who underwent surgery in the sitting or "beach chair" position without incidence of adverse neurologic events. Anesth Analg. 2013;116:1317–24. doi: 10.1213/ANE.0b013e31828446bb. [DOI] [PubMed] [Google Scholar]
- 24.Laflam A, Joshi B, Brady K, Yenokyan G, Brown C, Everett A, Selnes O, McFarland E, Hogue CW. Shoulder surgery in the beach chair position is associated with diminished cerebral autoregulation but no differences in postoperative cognition or brain injury biomarker levels compared with supine positioning: the anesthesia patient safety foundation beach chair study. Anesth Analg. 2015;120:176–85. doi: 10.1213/ANE.0000000000000455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stoneham MD, Martin T. Increased oxygen administration during awake carotid surgery can reverse neurological deficit following carotid cross-clamping. Br J Anaesth. 2005;94:582–5. doi: 10.1093/bja/aei089. [DOI] [PubMed] [Google Scholar]
- 26.Ide K, Eliasziw M, Poulin MJ. Relationship between middle cerebral artery blood velocity and end-tidal PCO2 in the hypocapnic-hypercapnic range in humans. J Appl Physiol (1985) 2003;95:129–37. doi: 10.1152/japplphysiol.01186.2002. [DOI] [PubMed] [Google Scholar]
- 27.Cho H, Nemoto EM, Yonas H, Balzer J, Sclabassi RJ. Cerebral monitoring by means of oximetry and somatosensory evoked potentials during carotid endarterectomy. J Neurosurg. 1998;89:533–8. doi: 10.3171/jns.1998.89.4.0533. [DOI] [PubMed] [Google Scholar]
- 28.Cuadra SA, Zwerling JS, Feuerman M, Gasparis AP, Hines GL. Cerebral oximetry monitoring during carotid endarterectomy: effect of carotid clamping and shunting. Vasc Endovascular Surg. 2003;37:407–13. doi: 10.1177/153857440303700604. [DOI] [PubMed] [Google Scholar]
- 29.Samra SK, Dy EA, Welch K, Dorje P, Zelenock GB, Stanley JC. Evaluation of a cerebral oximeter as a monitor of cerebral ischemia during carotid endarterectomy. Anesthesiology. 2000;93:964–70. doi: 10.1097/00000542-200010000-00015. [DOI] [PubMed] [Google Scholar]
- 30.Hirofumi O, Otone E, Hiroshi I, Satosi I, Shigeo I, Yasuhiro N, Masato S. The effectiveness of regional cerebral oxygen saturation monitoring using near-infrared spectroscopy in carotid endarterectomy. J Clin Neurosci. 2003;10:79–83. doi: 10.1016/s0967-5868(02)00268-0. [DOI] [PubMed] [Google Scholar]
- 31.Rigamonti A, Scandroglio M, Minicucci F, Magrin S, Carozzo A, Casati A. A clinical evaluation of near-infrared cerebral oximetry in the awake patient to monitor cerebral perfusion during carotid endarterectomy. J Clin Anesth. 2005;17:426–30. doi: 10.1016/j.jclinane.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 32.Moritz S, Kasprzak P, Arlt M, Taeger K, Metz C. Accuracy of cerebral monitoring in detecting cerebral ischemia during carotid endarterectomy: a comparison of transcranial Doppler sonography, near-infrared spectroscopy, stump pressure, and somatosensory evoked potentials. Anesthesiology. 2007;107:563–9. doi: 10.1097/01.anes.0000281894.69422.ff. [DOI] [PubMed] [Google Scholar]
- 33.Tange K, Kinoshita H, Minonishi T, Hatakeyama N, Matsuda N, Yamazaki M, Hatano Y. Cerebral oxygenation in the beach chair position before and during general anesthesia. Minerva Anestesiol. 2010;76:485–90. [PubMed] [Google Scholar]
- 34.Davie SN, Grocott HP. Impact of extracranial contamination on regional cerebral oxygen saturation: a comparison of three cerebral oximetry technologies. Anesthesiology. 2012;116:834–40. doi: 10.1097/ALN.0b013e31824c00d7. [DOI] [PubMed] [Google Scholar]
- 35.Samra SK, Stanley JC, Zelenock GB, Dorje P. An assessment of contributions made by extracranial tissues during cerebral oximetry. J Neurosurg Anesthesiol. 1999;11:1–5. doi: 10.1097/00008506-199901000-00001. [DOI] [PubMed] [Google Scholar]
- 36.Harris DN, Bailey SM. Near infrared spectroscopy in adults. Does the Invos 3100 really measure intracerebral oxygenation? Anaesthesia. 1993;48:694–6. doi: 10.1111/j.1365-2044.1993.tb07183.x. [DOI] [PubMed] [Google Scholar]
- 37.Fearn SJ, Mead GE, Picton AJ, Mortimer AJ, McCollum CN. Cerebral oximetry: a useful monitor during carotid artery surgery. Anaesthesia. 1996;51:610–1. doi: 10.1111/j.1365-2044.1996.tb12599.x. [DOI] [PubMed] [Google Scholar]
- 38.Kishi K, Kawaguchi M, Yoshitani K, Nagahata T, Furuya H. Influence of patient variables and sensor location on regional cerebral oxygen saturation measured by INVOS 4100 near-infrared spectrophotometers. J Neurosurg Anesthesiol. 2003;15:302–6. doi: 10.1097/00008506-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Fassoulaki A, Kaliontzi H, Petropoulos G, Tsaroucha A. The effect of desflurane and sevoflurane on cerebral oximetry under steady-state conditions. Anesth Analg. 2006;102:1830–5. doi: 10.1213/01.ane.0000205739.37190.14. [DOI] [PubMed] [Google Scholar]
- 40.Rifai L, Winters J, Friedman E, Silver MA. Initial description of cerebral oximetry measurement in heart failure patients. Congest Heart Fail. 2012;18:85–90. doi: 10.1111/j.1751-7133.2011.00284.x. [DOI] [PubMed] [Google Scholar]
- 41.McSwain SD, Hamel DS, Smith PB, Gentile MA, Srinivasan S, Meliones JN, Cheifetz IM. End-tidal and arterial carbon dioxide measurements correlate across all levels of physiologic dead space. Respir Care. 2010;55:288–93. [PMC free article] [PubMed] [Google Scholar]