Highlights
-
•
This paper demonstrates that oral EHE is an unpredictable lesion that seems to behave in a relatively benign fashion. This is in contrast with non-oral EHE where up to one third of cases may metastasize.
-
•
Because of the propensity to recur locally after excision and curettage, a wide local excision with close clinical follow has been suggested in the literature as the treatment of choice for oral lesions.
-
•
However, the lack of metastases from oral lesions, the small size, mandibular site and bland histology in this case suggests that a limited soft tissue excision and bone curettage, with long term follow-up would be appropriate for similar gingival lesions in future.
Keywords: Epithelioid hemangioendothelioma, Vascular neoplasm, Neoplasm of the oral cavity
Abstract
Introduction
Epithelioid hemangioendothelioma (EHE) is a rare vascular neoplasm that exhibits the potential for recurrence and metastasis but rarely involves the oral cavity.
Presentation Of Case
We report the management and long term follow up of recurrent EHE in a 23- year-old woman. The lesion initially presented as a small area of erythematous gingival swelling with localised bone loss around the lower anterior teeth. It was treated by buccal and lingual stripping of the gingival tissues. The patient suffered local recurrence after 7 years and was treated with a wider surgical excision of the buccal and lingual gingivae, conserving the adjacent teeth and bone with an excellent cosmetic outcome. Over 21 years later, there have been no further recurrences.
Discussion
This case highlights the management challenges of EHE and is the only case in the literature to have reported a case of mandibular gingivae with a long review period of 21 years.
Conclusion
Oral EHE is an unpredictable lesion with a relatively benign course, unlike non-oral EHE where up to one third of cases may metastasise. Because of the propensity to recur locally after excision and curettage, a wide local excision with close clinical follow has been suggested in the literature as the treatment of choice for oral lesions. However, the lack of metastases from oral lesions, the small size, mandibular site and bland histology in this case suggests that a limited soft tissue excision and bone curettage, with long term follow-up would be appropriate for similar gingival lesions in future.
1. Introduction
Epithelioid hemangioendothelioma (EHE) is an uncommon neoplasm of vascular endothelium, first described by Weiss et al. [1]. It is caused by a fusion gene; either a t(1;3)(p36;q23–5) reciprocal translocation between WWTR1 and CAMTA1 or a t(11;X) (q13;p11) between YAP1 and TFE3 (2) . EHE arises most frequently in young and middle aged adults, often in the lower extremities and in male patients. Initially, and at the time of diagnosis, EHE was considered a low grade or intermediate malignant neoplasm, with a propensity to recur and a low risk of metastasis. However, it is now considered malignant, and it is recognised that the previously described multicentric presentation in some patients was accounted for by multiple clonal, and therefore metastatic, deposits [3]. The outcome of EHE varies between sites; solitary and skin lesions appear relatively slow-growing, whereas multicentric lesions or those with histological atypia, and lesions from sites such as bone or lungs may metastasize and carry a fatal outcome. We present a case and long term follow up (21 years) of EHE in a 23 year old woman. The lesions developed in the lower anterior attached gingivae and followed a relatively indolent course with a single recurrence following conservative surgical management.
2. Case report
A 23 year old fit and healthy Caucasian woman was referred regarding a gingival lesion. She presented with a five year history of a small area of gingival swelling and erythema buccally and lingually around the lower left incisors, which were slightly mobile (Fig. 1). There was a small amount of supra- and sub-gingival calculus in this region with localized recession, but the rest of the gingivae were healthy. Intraoral radiographs showed that the lesion was associated with a vertical bony defect of approximately 3 mm (Fig. 5a).
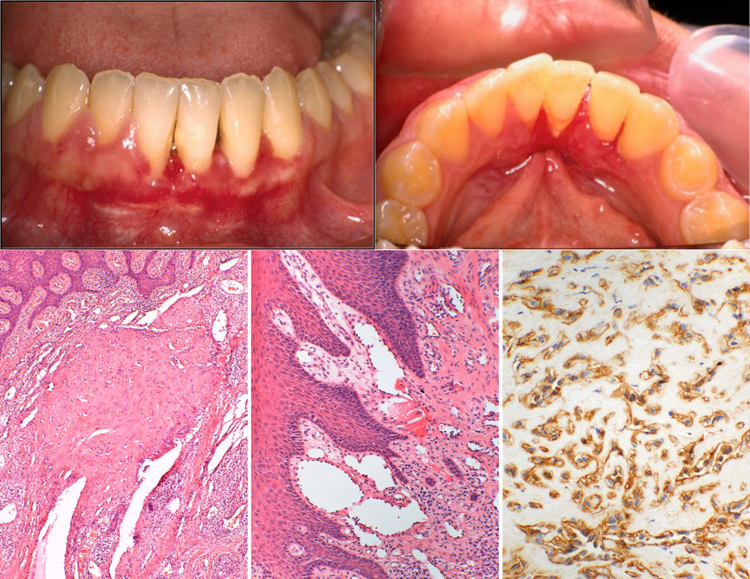
Fig. 1.
Initial presentation showing a small area of gingival swelling and erythema labially and lingually around the LL1 and LL2. Histological appearance of the initial lesion shows: left; area with typical zoning and central hyalinised nodule, centre; area with haemangioma-like vessels with prominent endothelium (haematoxylin and eosin), right; positive pericytic staining with smooth muscle actin immunohistochemistry.
Fig. 5.

Upper row; radiographic presentation at time of diagnosis showing vertical bone loss around the LL1 and LL2. Middle row; appearance at recurrence 7 years after diagnosis showing increased bone loss. Bottom row; 19 years after initial presentation showing stability of bone levels.
Review of two previous biopsy specimens of the initial lesion, that had proved inconclusive when reported at another hospital, showed features of EHE (Fig. 1). The superficial gingival tissues contained a haemangioma-like cluster of large irregular vessels with a prominent pericytic cuff, surrounded by solid sheets and dispersed epithelioid cells in a lightly and evenly hyalinised slightly myxoid stroma. There were no mitoses, necrosis or cytological atypia detected, suggesting this lesion was on the benign end of the spectrum of activity that was accepted at the time of diagnosis. It was therefore decided to treat the lesion conservatively. The lesion was treated with local stripping of the gingival tissues around both lingual and buccal aspects of the lower incisors.
The patient was followed up closely, and the condition remained stable for the following 7 years at which point a new lesion presented as an erythematous patch with associated gingival swelling on the buccal gingivae between LR1 to LL3, and on the lingual gingival between LR1 and LL4 (Fig. 2). Radiographs showed further horizontal and vertical bone loss around these teeth. (Fig. 5b).
Fig. 2.

Clinical presentation 7 years after formal diagnosis (a) labial aspect showing gingival swelling and erythema between LR1 to LL4, and (b) lingual aspect (mirror image).
A biopsy was taken and histological analyisis confirmed recurrence of EHE. In the specimen of the recurrence there were increased numbers of convoluted and dissecting reteform vessels that had not been prominent on initial presentation. This combination of reteform haemangioendothelioma and epithelioid haemangioendothelioma is now considered a distinct sub-type termed composite haemangioendothelioma. These lesions do occasionally metastasize but most commonly seem to occur in the skin and have a clinical course towards the more benign end of the spectrum [4]. A wider soft-tissue excision and curettage of the lingual gingivae between the LR2 and the LL4 and the buccal gingivae between LR1 to the LL3 was performed by an oral surgeon, within an excision margin of 3 mm. The excision did not involve removal of any bone or teeth. Fig. 3 shows the postoperative presentation shortly after soft-tissue surgical excision of the recurrence.
Fig. 3.

showing postoperative healing shortly after soft- tissue surgical excision of the recurrence.
At around the time of the recurrence, the patient was also diagnosed with papillary carcinoma of the thyroid gland and underwent a total thyroidectomy followed by radioiodine ablation and thyroxine T4 suppression. We are unaware of any previous reports of EHE and papillary carcinoma of the thyroid occurring in the same patient and these conditions appeared unrelated. The patient has been reviewed regularly, and the condition has remained stable for a further nine years. Radiographic estimation of the bone loss in annual sequential radiographs suggested no further loss of bone, and clinical signs remained stable. (Fig. 5c).
During this period the patient gave birth to a healthy child. The clinical signs remained unchanged during her pregnancy. Sixteen years after the initial presentation, the patient developed more gingival recession lingual to the lower incisors, but further biopsies showed no evidence of recurrence. The patient was given further detailed oral hygiene instructions and saw a hygienist regularly for scaling. She has been reviewed for a further five years, with no change in clinical signs or symptoms and no evidence of recurrence (Fig. 4). She remains well twenty one years after the initial presentation and sixteen years after formal diagnosis.
Fig. 4.

Clinical presentation 21 years after initial presentation showing some calculus deposits and recession around the lower incisors, but no evidence of recurrence.
3. Discussion
Several types of haemangioendothelioma are recognised and this heterogeneous group has undergone several reclassifications in the past decades, both gaining and losing members. The epithelioid hemangioendothelioma is a well-defined and distinctive vascular neoplasm of endothelial cells that can both recur locally and metastasize [5]. The tumour has a characteristic zoning pattern of vessels with prominent pericytic cells, and islands and strands of epithelioid endothelium in a myxoid or hyalinised stroma. The cause is either a t(1;3)(p36;q23–5) translocation between WWTR1 and CAMTA1 or a t(11;X)(q13;p11) between YAP1 and TFE3 [2]. Both translocations produce fusion genes including a transcriptional co-activator and a known oncogene. Currently, these fusion genes appear distinctive to EHE but detection is not required for diagnosis because the histological appearances are diagnostic, aided by immunohistochemistry to delineate the contractile pericytic cells around the vessels using smooth muscle actin or calponin if necessary.
EHE is currently believed to be an intermediate grade malignancy, having the ability to recur locally as well as to metastasize, but much less frequently than angiosarcoma [6]. While there are no reliable histological features that allow prediction of the biologic behaviour of EHE, features such as mitotic activity, a greater number of spindle cells rather than epithelioid cells, focal necrosis, cellular pleomorphism, and metaplastic bone formation within the tumour have been suggested to be associated with more aggressive behaviour [7], and any cases with histological atypia should be regarded with suspicion. EHE rarely involves the oral cavity, and a review of intraoral EHE by Gordon-Nunez et al., reported a total of only 27 cases in the literature [8]. The common clinical presentation is reported as an asymptomatic solitary mass of red-purplish colour which can occur on the alveolar gingivae, the tongue, the buccal mucosa, the lip, the palate and the maxillary or mandibular bone.
The literature shows that the most prevalent intraoral site for EHE is the tongue (26%), followed by the mandibular (22%) and maxillary gingiva (19%) [9]. Erosion of the underlying alveolar bone, tooth mobility and mucosal ulceration are also reported as features of gingival EHE. Clinical differential diagnosis of gingival EHE includes pyogenic granuloma, peripheral giant cell granuloma, haemangiomas, inflammatory fibrous hyperplasias and necrotizing ulcerative gingivitis depending on presentation [8]. The age of first presentation of the current case was 18 years which is consistent with all six of the cases so far reported where mandibular mucosa has been the presenting site, all of whom have been aged 18 years or less. The age of presentation of the 5 cases reported of EHE in maxillary mucosa has ranged from 9 to 45 years with three patients aged 12 or younger. Thus, a young age of presentation seems to be a feature of most cases of gingival EHE.
In the oral cavity, local recurrence has been noted but no metastasis or associated mortality appears to have been reported, suggesting that mucosal lesions have a similar behaviour to solitary skin lesions. This finding is of clinical importance and well illustrated by the current case. Of the 5 cases of EHE reported in the literature appearing on the maxillary gingivae, 2 have shown local recurrences within one year, whilst of the 6 cases of EHE arising on the mandibular gingivae, none have reported recurrences over a review period of up to 6 years. The total review period of 21 years appears to be the longest reported in the literature so far. Whilst 8 of the 27 cases of intra-oral EHE in the literature have reported local recurrence, none of have been associated with distant metastases. This is in contrast with non-oral EHE where up to one third of cases may metastasize. Nevertheless, it would be prudent to regard with suspicion any cases with histological atypia and frequent mitoses even if arising in the oral cavity.
Because of the propensity to recur locally after excision and curettage, a wide local excision with close clinical follow has been suggested in the literature as the treatment of choice for oral lesions. [10]. However, the lack of metastases from oral lesions, the historical perspective seen in this patient, the small size, mandibular site and bland histology suggest that a limited soft tissue excision and bone curettage would be appropriate for similar lesions in future. The patient suffered local recurrence in the gingival soft tissues after seven years but repeat excision appears to have ablated the lesion with an excellent cosmetic outcome. It is therefore possible that conservative treatment should now be considered as the management of choice for gingival lesions of EHE.
Conflict of interest
There are no disclosures to be made. There are no commercial associations, current and within the past five years, that might pose a potential, perceived, or real conflict of interest.
Sources of funding
No sources of funding.
Ethical approval
Patient is not identifiable therefore ethical approval not deemed to be required.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author contributions
Shabnum Ali: Primary author of paper, study concept, literature review, Academic Clinical Fellow/Specialist Registrar in Special Care Dentisty.
Odell E.W.: Professor of Oral Pathology and Medicine, Histopathologist, Supervisor.
Whaites E.: Radiologist.
Robinson P.D.: Oral surgeon.
Challacombe S.J.: Professor of Oral Medicine Supervisor, study concept.
Guarantor
Shabnum Ali.
Acknowledgement
We would like to thank Dr. E. Calonje, Guy’s and St. Thomas’ NHS Foundation Trust for reviewing the pathology specimens.
References
- 1.Weiss S.W., Enzinger F.M. Epithelioid Hemangioendothelioma — a distinctive vascular tumor often mistaken for a carcinoma. Lab. Invest. 1981;44(1) doi: 10.1002/1097-0142(19820901)50:5<970::aid-cncr2820500527>3.0.co;2-z. A75-A. [DOI] [PubMed] [Google Scholar]
- 2.Flucke U., Vogels R.J.C., Somerhausen N.D., Creytens D.H., Riedl R.G., van G., orp J.M. Epithelioid hemangioendothelioma: clinicopathologic, immunhistochemical, and molecular genetic analysis of 3 cases. Diagn. Pathol. 2014;9 doi: 10.1186/1746-1596-9-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Errani C., Sung Y.S., Zhang L., Healey J.H., Antonescu C.R. Monoclonality of multifocal epithelioid hemangioendothelioma of the liver by analysis of WWTR1-CAMTA1 breakpoints. Cancer Genet- Ny. 2012;205(1–2):12–17. doi: 10.1016/j.cancergen.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nayler S.J., Rubin B.P., Calonje E., Chan J.K.C., Fletcher C.D.M. Composite hemangioendothelioma — a complex, low-grade vascular lesion mimicking angiosarcoma. Am. J. Surg. Pathol. 2000;24(3):352–361. doi: 10.1097/00000478-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Deyrup A.T., Tighiouart M., Montag A.G., Weiss S.W. Epithelioid hemangioendothelioma of soft tissue: a proposal for risk stratification based on 49 cases. Am. J. Surg. Pathol. 2008;32(6 (June)):924–927. doi: 10.1097/pas.0b013e31815bf8e6. [DOI] [PubMed] [Google Scholar]
- 6.Hemangioendothelioma: vascular tumors of intermediate malignancy, In: S.W. Weiss, J.R.G., editor, Enzinger and Weiss’s soft tissue tumors, (Ed.) 2, 001, 891–915
- 7.Ellis G.L., Kratochvil F.J. 3rd Epithelioid hemangioendothelioma of the head and neck: a clinicopathologic report of twelve cases. Oral Surg. Oral Med. Oral Pathol. 1986;61(1):61–68. doi: 10.1016/0030-4220(86)90204-5. [DOI] [PubMed] [Google Scholar]
- 8.Gordon-Nunez M.A., Silva e M., Lopes M.F., de Oliveira- Neto S.F., Maia A.P., Galvao H.C. Intraoral epithelioid hemangioendothelioma: a case report and review of the literature. Medicina Oral Patologia Oral Y Cirugia Bucal. 2010;15(2) e340-6. [PubMed] [Google Scholar]
- 9.Marrogi A.J., Boyd D., Elmofty S.K., Waldron C. Epithelioid Hemangioendothelioma of the Oral Cavity — report of 2 cases and review of literature. J. Oral Maxil. Surg. 1991;49(6):633–638. doi: 10.1016/0278-2391(91)90346-n. [DOI] [PubMed] [Google Scholar]
- 10.Ramer M.A., Lumerman H., Kopp W., Fisher K.S., Cohen S.A. Epithelioid hemangioendothelioma of the maxilla: case report and review of literature. Periodon. Clin. invest.: Off. Pub. Northeastern Soc. Periodont. 2001;23(1):31–35. [PubMed] [Google Scholar]