Abstract
INTRODUCTION
Descent of the ureter into the inguinal canal or scrotum is rare but undoubtedly underreported. Most known cases were recognized at the time of surgery for hernia repair. We encountered five cases recently.
PRESENTATION OF CASE
We reviewed the records and CT images of five patients with inguinal hernias containing a segment of the ureter. All of our cases, like most reported cases, featured obese adult males. Our cases had different outcomes, ranging from inadvertent injury of the displaced ureter to correction of the anomaly at the time of hernia repair.
DISCUSSION
In all of our cases, the affected ureter was displaced anteriorly from the psoas muscle by greater than 1 cm at the level of the L4 vertebra on abdominal CT. This association has not been previously described.
CONCLUSION
Pre-operative diagnosis by CT can prevent injury to the ureter. We hypothesize that anterior displacement of the ureter at the level of L4 as seen on CT may be predictive of inguinoscrotal herniation of the ureter.
1. Introduction
Descent of the distal aspect of the ureter into the inguinal canal or scrotum is a rare condition. There are 64 cases of inguinoscrotal herniation of the ureter in the English language literature [1]. Most reported cases were noted at the time of surgical exploration for inguinal hernia repair, or later as a result of an operative injury. In five years, we encountered five patients with inguinal hernias in whom the ipsilateral ureter coursed into the inguinal canal or scrotum before ascending to enter the bladder at the usual site.
2. Presentation of cases
We describe pertinent clinical and imaging details of our five cases. None of the patients had a history of prior inguinal or ureteral surgery. All were very obese. We scrutinized the available clinical records and imaging studies, searching for anatomic details that might be helpful in predicting the ureteral abnormality. We found no articles or abstracts describing CT evidence that identifies this aberrant ureteral course when otherwise unsuspected.
2.1. Patient 1
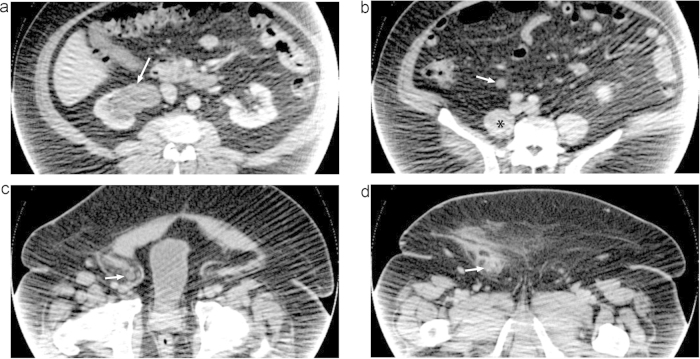
This was a 57-year-old extremely obese (BMI of 55 kg/m2) Caucasian man who had a symptomatic communicating right hydrocele. Hernia repair and fenestration of the hydrocele was performed via an inguinal incision. Abdominal-pelvic CT before and immediately after surgery did not reveal a dilated right ureter. The post-operative course was complicated by wound drainage. Several months later, repeat CT disclosed marked right hydronephrosis (Fig. 1a) with renal atrophy due to injury of the ureter in the area of the hernia repair (Fig. 1c and d). As measured on CT, the right ureter was 1.4 cm anterior to the psoas muscle at the L3–L4 intervertebral level and 2.2 cm anterior to the psoas muscle at L4–L5 (Fig. 1b). The left ureter could not be definitively identified on this study. Subsequent renal scan revealed minimal function of the right kidney.
Fig. 1.
Post-operative venous phase CT images of Patient 1. Image quality is degraded due to incomplete projection artifact where the patient's body exceeds the field of view. (a) Right renal atrophy and severe hydronephrosis (arrow). (b) Dilated right ureter (arrow) displaced anteriorly from the psoas muscle (*) at the level of L4–L5. (c) Right ureter (arrow) in the inguinal hernia. (d) Right ureter (arrow) in the inguinal hernia with adjacent fat stranding reflecting post-operative changes.
2.2. Patient 2
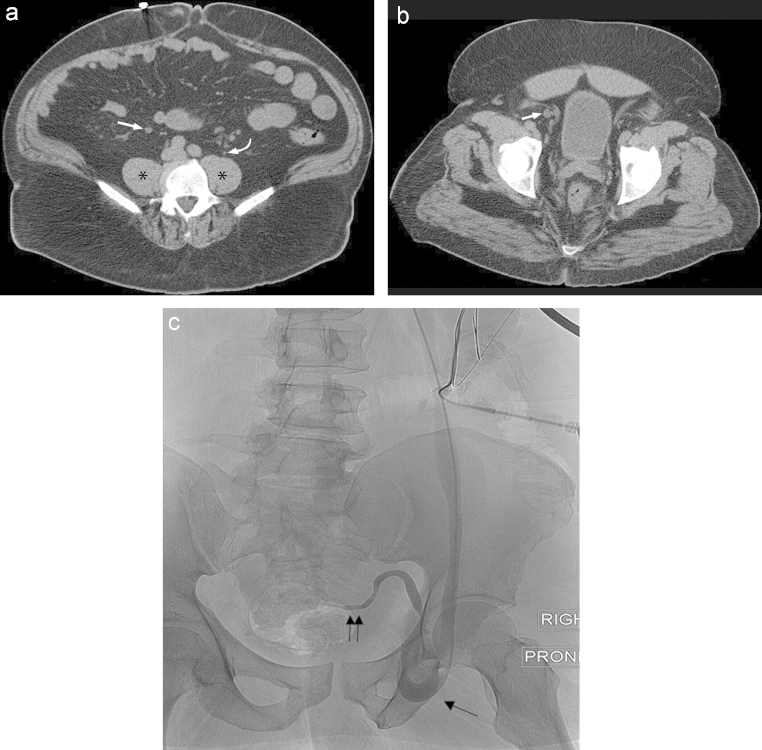
This was a 63-year-old extremely obese (BMI of 40 kg/m2) African American man who was evaluated for chronic renal insufficiency and found to have marked right hydronephrosis. He also had a large right indirect inguinal hernia. Abdominal-pelvic CT revealed that the ureter coursed close to the hernia (Fig. 2b). The CT also demonstrated marked deviation of the right ureter in its mid-course, measuring 3.7 cm anterior to the psoas muscle at L3–L4 and 3.1 cm at L4–L5 (Fig. 2a). The left ureter was poorly visualized but was approximately 1.1 cm anterior to the psoas muscle at L3–L4 and 0.3 cm at L4–L5. Attempted retrograde ureteral stent placement was unsuccessful; subsequent placement of a right percutaneous nephrostomy tube was successful. Antegrade nephrostogram revealed a tortuous right ureter looping below the level of the pubic symphysis into the inguinal hernia, with evidence of obstruction at the level of the ureterovesical junction (Fig. 2c). The patient was managed with inguinal exploration, herniorrhaphy, resection of redundant ureter, and ureterocystostomy. The right hydronephrosis resolved promptly.
Fig. 2.
Pre-operative non-contrast CT and fluoroscopic images of Patient 2. (a). Right ureter (straight arrow) displaced anteriorly from the psoas muscle (*) at the level of L4–L5. Compare this to the normally positioned left ureter (curved arrow) in close proximity to the psoas muscle (*). (b) Right ureter (straight arrow) in the inguinal hernia. (c) Anterograde nephrostogram with the patient in prone position at the time of nephrostomy tube insertion. The right ureter loops below the level of the pubic symphysis into a large right inguinal hernia (one arrow) with evidence of obstruction at the level of the ureterovesical junction (two arrows).
2.3. Patient 3
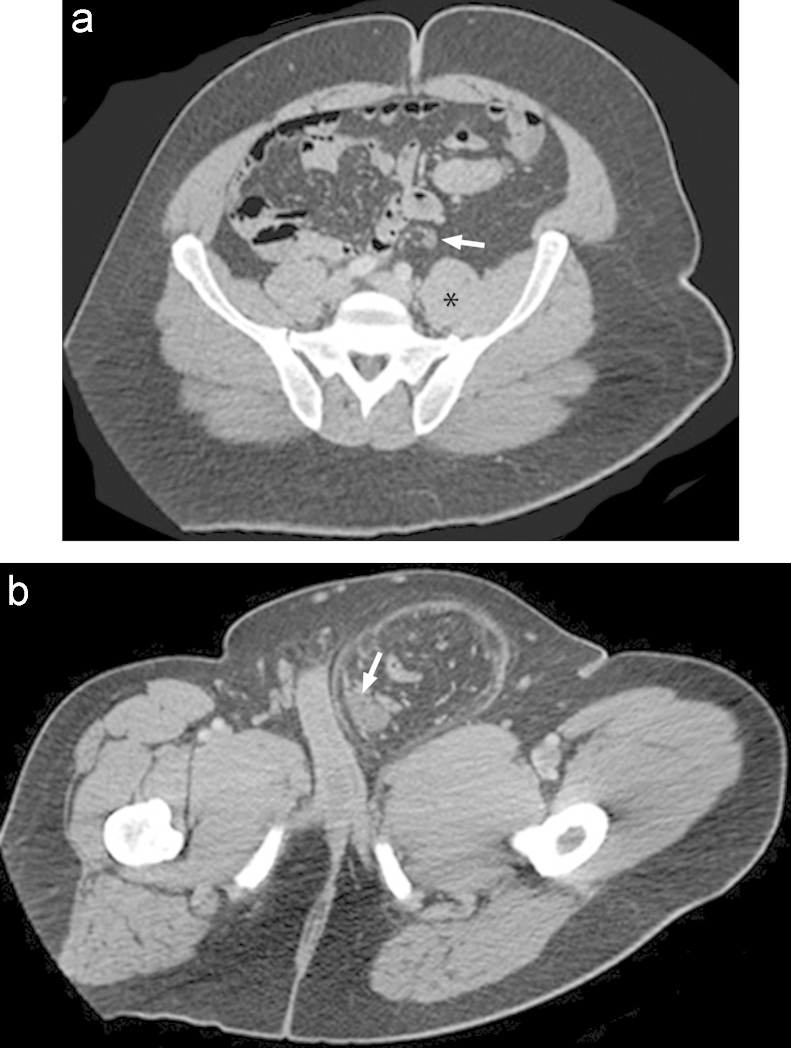
This was a 46-year-old obese (exact BMI not known) man with a massive noncommunicating hydrocele and chronic left scrotal swelling. On abdominal-pelvic CT scan, he was found to have a left hydrocele and indirect inguinal hernia containing colon and the left ureter (Fig. 3b). The left ureter was displaced anteriorly from the psoas muscle by 1 cm at the level of L4–L5 (Fig. 3a). The CT scan also revealed severe left hydroureteronephrosis with an atrophic left kidney. A MAG-3 (mercaptoacetyltriglycine) renal scan confirmed a nonfunctioning left kidney. The patient underwent exploratory laparotomy, reduction of the displaced viscera, repair of the hernia, hydrocelectomy, and scrotoplasty. The left ureter was identified over the psoas muscle through the midline incision and ligated at the level of the external iliac vessels to prevent ascending infection. The patient recovered well.
Fig. 3.
Pre-operative venous phase CT images of Patient 3. (a) Left ureter (arrow) displaced anteriorly from the psoas muscle (*). (b) Left ureter (arrow) in the inguinal hernia.
2.4. Patient 4
This was a 52-year-old obese (BMI of 33 kg/m2) Caucasian man with a history of midline ventral hernia status post repair. A noncontrast CT demonstrated a separate right inguinal hernia with the right ureter in close proximity. Therefore, CT urography was performed which confirmed that the right ureter entered the hernia (Fig. 4c) before coursing posteriorly and inserting into the bladder. There was no hydronephrosis or hydroureter. The right ureter was 1.2 cm anterior to the psoas muscle at L4 (Fig. 4b) whereas the normal left ureter was only 0.2 cm anterior to the psoas muscle at the same level (Fig. 4a). The patient's renal function was normal. Awareness of this ureteral anomaly prompted a urologic consultation. Pre-operative cystoscopic right ureteral stent placement was performed which assisted in identification of the ureter and avoided ureteral injury during surgery. The stent was removed immediately after the hernia repair.
Fig. 4.
Pre-operative urographic phase CT images of Patient 4. The ureters are opacified with contrast. (a) Normal left ureter (curved arrow) within 1 cm of the psoas muscle (*). (b) Right ureter (straight arrow) displaced anteriorly from the psoas muscle (*) at L4–L5. (c) Right ureter (straight arrow) in the inguinal hernia.
2.5. Patient 5
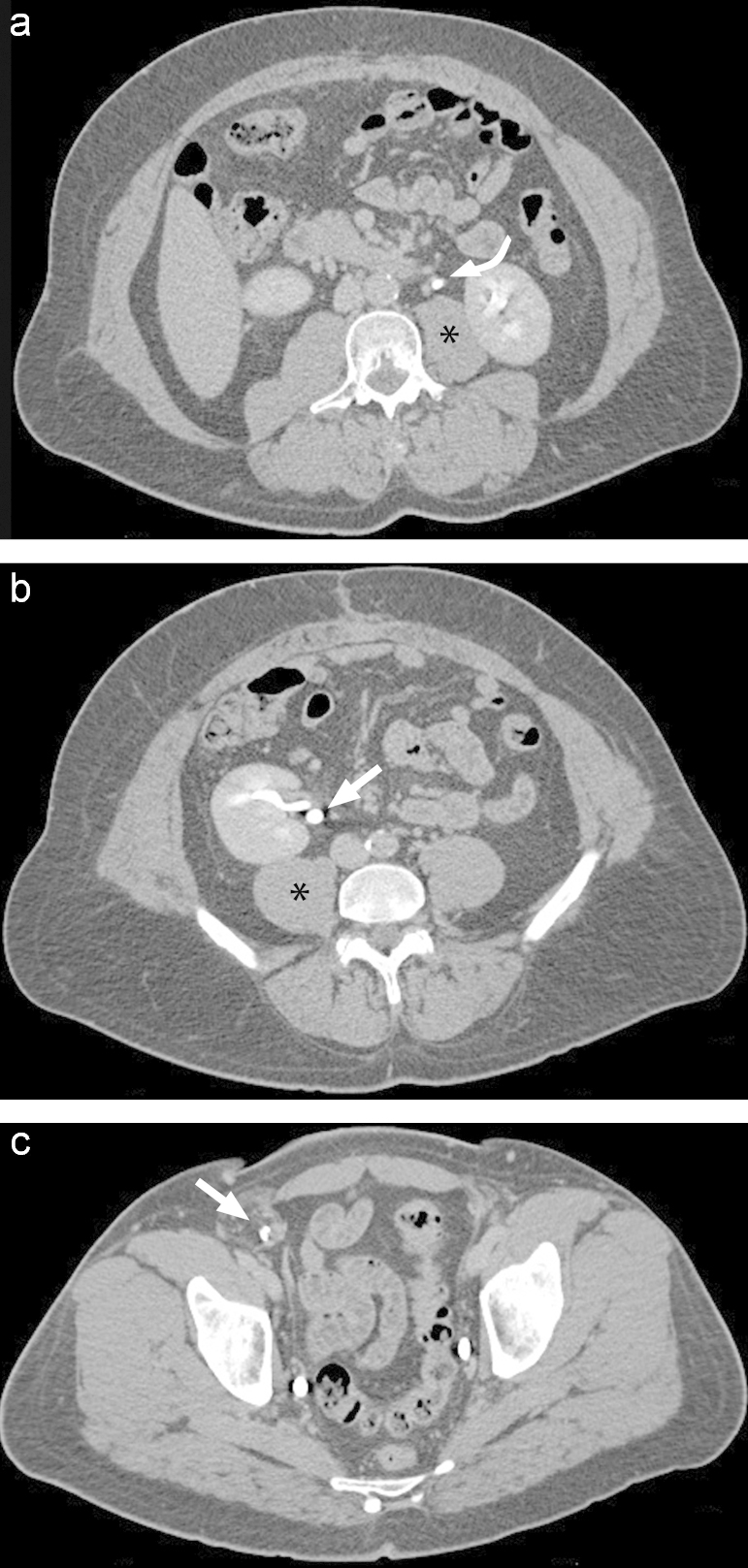
This was a 69-year-old obese (BMI of 36 kg/m2) Caucasian man with a history of penile cancer status post partial penectomy 7 years earlier. He reported increasing swelling and discomfort in his left groin. His renal function was normal. Of note, the patient had an atonic bladder and required clean intermittent catherization. CT urography showed severe left hydronephrosis and hydroureter with the distal left ureter clearly extending into a left inguinal hernia. The left kidney was atrophic consistent with chronic obstruction. The left ureter was compressed as it entered and exited the hernia neck with dilatation of the entrapped ureter within the hernia (Fig. 5). The posterior aspect of the dilated left ureter was 1.0 cm anterior to the psoas muscle at the level of L4 whereas the normal right ureter was only 0.1 cm anterior to the psoas muscle at this level. Given the tortuosity of the left ureter, ureteric stent placement was deemed unfeasible. A left percutaneous nephrostomy tube was inserted for decompression prior to successful herniorrhaphy.
Fig. 5.
Pre-operative urographic phase CT image of Patient 5 demonstrating a distended left ureter (arrow) entrapped within the inguinal hernia. No excretion of contrast is seen into this ureter. The bladder wall is thickened consistent with chronic atony (#).
3. Discussion
Inguinal hernia is a common indication for surgery and the ureter is rarely drawn toward or into the scrotum because of adhesion to the posterior wall of the hernia sac [2]. They are found more frequently in obese men during the fifth to sixth decades of life [3]. Most are asymptomatic. Urinary symptoms such as dysuria, frequency, and urgency may be present, but these symptoms are non-specific and may not raise the suspicion of ureteroinguinal herniation [4]. It is important to diagnose this anomaly because there is a high risk of iatrogenic injury to the ureter at the time of hernia repair if the condition is not recognized.
Our five cases had markedly different outcomes. In Patient 1 (Section 2.1), lack of knowledge of the anomaly resulted in inadvertent injury to the displaced ureter and subsequent loss of renal function. In Patient 2 (Section 2.2), awareness of the anomaly prompted surgical intervention that corrected the obstructive uropathy. In Patient 3 (Section 2.3), awareness of the lack of function in the affected kidney allowed ligation of the obstructed ureter, thus minimizing the risk of subsequent upper urinary tract infection. In Patient 4 (Section 2.4), the displaced ureter was recognized and temporarily stented prior to hernia repair to decrease the risk of ureteral injury. In Patient 5 (Section 2.5), the ureter was entrapped and obstructed in the inguinal hernia, and a percutaneous nephrostomy was required for decompression.
In each case, abdominal-pelvic CT revealed an abnormal course of the mid-portion of the ureter that accompanied the anomaly seen more distally. The ureter with the abnormal pelvic course also had an abnormal position at the L4 level, lying in retroperitoneal fat markedly anterior to the psoas muscle by at least 1 cm in all five cases. In contrast, the ureter with the normal proximal course immediately anterior to the psoas muscle also had a normal distal course, best depicted in Fig. 2a. This deviation of the herniated ureter in its mid-course was evident on CT even without a dedicated urographic phase of contrast. None of the prior reports mention this relationship.
4. Conclusion
Pre-operative diagnosis of inguinoscrotal herniation of the ureter, when available, enables the surgeon to avoid accidental damage to the ureter during a groin operation. All cases described in this series occurred in obese men. We hypothesize that anterior displacement of the ureter from the ipsilateral psoas muscle by greater than 1 cm at the level of the L4 vertebra as seen on CT is associated with inguinoscrotal herniation of the ureter. Further investigation is required and should stratify subjects by BMI.
References
- 1.Oruç M.T., Akbulut Z., Ozozan O., Coşkun F. Urological findings in inguinal hernias: a case report and review of the literature. Hernia. 2004;8(1):76–79. doi: 10.1007/s10029-003-0157-6. [DOI] [PubMed] [Google Scholar]
- 2.Giglio M., Medica M., Germinale F. Scrotal extraperitoneal hernia of the ureter: case report and literature review. Urol. Int. 2001;66(3):166–168. doi: 10.1159/000056601. [DOI] [PubMed] [Google Scholar]
- 3.Ballard J.L., Dobbs R.M., Malone J.M. Ureteroinguinal hernia: a rare companion of sliding inguinal hernias. Am. Surg. 1991;57(11):720–722. [PubMed] [Google Scholar]
- 4.Akpinar E., Turkbey B., Ozcan O. Bilateral scrotal extraperitoneal herniation of ureters: computed tomography urographic findings and review of the literature. J. Comput. Assist. Tomogr. 2005;29(6):790–792. doi: 10.1097/01.rct.0000180191.39137.07. [DOI] [PubMed] [Google Scholar]