Abstract
AIM: To investigate inpatient length of stay (LOS), complication rates, and readmission rates for sacral fracture patients based on operative approach.
METHODS: All patients who presented to a large tertiary care center with isolated sacral fractures in an 11-year period were included in a retrospective chart review. Operative approach (open reduction internal fixation vs percutaneous) was noted, as well as age, gender, race, and American Society of Anesthesiologists’ score. Complications included infection, nonunion and malunion, deep venous thrombosis, and hardware problems; 90-d readmissions were broken down into infection, surgical revision of the sacral fracture, and medical complications. LOS was collected for the initial admission and readmission visits if applicable. Fisher’s exact and non-parametric t-tests (Mann-Whitney U tests) were employed to compare LOS, complications, and readmissions between open and percutaneous approaches.
RESULTS: Ninety-four patients with isolated sacral fractures were identified: 31 (30.4%) who underwent open reduction and internal fixation (ORIF) vs 63 (67.0%) who underwent percutaneous fixation. There was a significant difference in LOS based on operative approach: 9.1 d for ORIF patients vs 6.1 d for percutaneous patients (P = 0.043), amounting to a difference in cost of $13590. Ten patients in the study developed complications, with no significant difference in complication rates or reasons for complications between the two groups (19.4% for ORIF patients vs 6.3% for percutaneous patients). Eight patients were readmitted, with no significant difference in readmission rates or reasons for readmission between the two groups (9.5% percutaneous vs 6.5% ORIF).
CONCLUSION: There is a significant difference in LOS based on operative approach for sacral fracture patients. Given similar complications and readmission rates, we recommend a percutaneous approach.
Keywords: Sacral fractures, Open reduction and internal fixation, Percutaneous complications, Readmissions, Length of stay
Core tip: Few studies in orthopaedics have investigated complication rates, readmission rates, and length of stay differences with respect to surgical approach for patients with sacral fractures. Investigating these issues in an era of rising healthcare costs will help determine cost-effective care. We reviewed patients presenting with isolated sacral fractures at a large, level-I trauma center, and found those treated with open reduction internal fixation stayed nearly 3 d longer compared to patients treated with percutaneous approaches. With similar complication and readmission rates between the two groups, we recommend a percutaneous approach to help lower total hospital costs for more value-based practice.
INTRODUCTION
Forty-five percent of all pelvic fractures include sacral involvement[1,2]. These fractures often occur in the secondary to high-energy mechanisms, with motor vehicle accidents causing up to 57% of these injuries[2]. Traumatic force may also lead to nearby neurovascular compression, which can precipitate adverse neurological events[3]. For these reasons, sacral fractures are musculoskeletal injuries requiring emergent action at trauma centers to reduce the risk of complications.
While open reduction and internal fixation (ORIF) methods allow for broad visualization of the sacrum and surrounding structures, highly variable wound complication rates range from 3.9% to 27% of study populations[4]. ORIF specifically has been linked to high rates of infection, which can complicate 18% to 27% of sacral fractures treated early and late, respectively[5]. Given these high complication rates, it is therefore reasonable to consider a more minimally invasive technique such as percutaneous fixation to stabilize the sacrum[6]. Percutaneous fixation with iliosacral screws, for example, have led to decreases in overall operative time and soft-tissue disruption, thereby providing avenues to prevent complications[7].
With the recent focus on healthcare cuts due to escalating costs in the United States, it is important to investigate postoperative length of stay (LOS), 90-d readmissions, and complication rates with respect to operative approach for sacral fracture patients. Although sacral fractures constitute a large component of pelvic fractures, little data exists exploring these issues with the most available knowledge regarding stress fractures secondary to osteoporosis[8]. This study therefore seeks to explore differences in LOS, complications, and readmissions based on operative technique to determine the most value-based approach in treating this patient cohort.
MATERIALS AND METHODS
After obtaining approval from our institutional review board, we identified all patients who sustained operative sacral fractures at a major academic level I trauma center from January 1, 2000 to December 31, 2011 through a Current Procedural Terminology code search (Supplementary Table 1). Two hundred and fifty patients were identified, and 102 of those patients were found to have isolated sacral injuries without other concomitant orthopaedic or medical injuries. Ninety-four patients were identified out of these 102 for analysis with isolated sacral fractures fitting the criteria for the operative approach (ORIF vs percutaneous).
Table 1.
Demographic characteristics of patients
| ORIF (n = 31) | Percutaneous (n = 63) | Total | |
| Average age (yr) | 44 | 37.1 | 39.3 |
| Gender (n) | |||
| Male | 19 | 22 | 41 |
| Female | 12 | 41 | 53 |
| Average BMI (kg/m2) | 26.1 | 24.8 | 25.5 |
ORIF: Open reduction and internal fixation; BMI: Body mass index.
Data extrapolated from patient chart review included demographics such as age, gender, and race; verification of operative approach (percutaneous vs open), American Society of Anesthesiologists’ (ASA) classification, complication rates, and readmission rates. Complications included infection, nonunion and malunion, deep venous thrombosis, and hardware problems. Ninety-day readmissions were broken down into three different categories: infection, surgical revision of the fracture, and medical complications such as urinary tract infections, pneumonia, hypotension, and anemia among others.
The LOS in days was collected for the initial admission and for 90-d readmissions if any existed. Additional data concerning the days from discharge to readmission were also collected for each patient, including the number of emergency room visits and clinic visits before a patient was admitted or readmitted to the hospital. The average cost per inpatient day ($4530/d) as well as all costs associated with anesthesia, surgery, and ancillary support (i.e., postoperative lab tests, radiography, consults, etc.) was obtained from the institution’s patient financial services department.
Fisher’s exact, student’s t-tests (for parametric variables such as LOS), and Mann-Whitney U tests (for non-parametric variables such as number of clinic visits) were employed to compare patients undergoing ORIF to those undergoing percutaneous fixation to note differences in hospital LOS and subsequent inpatient costs, complication rates, and readmission rates.
RESULTS
Ninety-four patients with isolated sacral injuries were identified for analysis: 31 patients (30.4%) underwent ORIF vs 63 patients (67.0%) who underwent percutaneous fixation (Table 1). The average age of all patients was 39.3 years, with ORIF patients older than percutaneous patients. There were 53 females and 41 males included in the study, with more men in the ORIF group and more women in the percutaneous group. The average BMI of all patients was 25.5. There were no significant differences in any baseline demographic between the ORIF and percutaneous groups. The majority of patients (51.1%) had an ASA score of 2, with similar distributions of ASA scores between the ORIF and percutaneous groups.
Table 2 lists hospital LOS, inpatient costs, and average number of emergency room and clinic visits based on operative approach. The mean LOS in the hospital for all patients was 7.1 d, with ORIF patients staying significantly longer (9.1 d) than percutaneous patients (6.1 d) (P = 0.043). There was no significant difference in the amount of time from admission to surgery for both groups, but ORIF patients stayed significantly longer after surgery (6.6 d) compared to percutaneous patients (4.6 d, P = 0.045). Using an average cost of $4530/d, this corresponds to average inpatient costs of $45300 for ORIF patients and $31710 for percutaneous patients - a difference of $13590 (Figure 1). Furthermore, when breaking down total costs for the patients based on operative approach, anesthesia costs were on average $1769 more for ORIF patients compared to percutaneous patients (P = 0.001), and surgical costs were on average $4401 more for ORIF patients (P < 0.001). Ancillary costs were statistically similar between the groups.
Table 2.
Hospital length of stay, costs, and emergency room and clinic visits based on operative approach
| ORIF (n = 31) | Percutaneous (n = 63) | P value | |
| Initial hospitalization | |||
| Average LOS (d) | 9.1 | 6.1 | 0.043 |
| Average time (admission-surgery) | 2.4 | 1.5 | 0.062 |
| Average time (surgery-discharge) | 6.6 | 4.6 | 0.045 |
| Average LOS costs | $45300 | $31710 | 0.043 |
| Average anesthesia costs | $4265 | $2496 | 0.001 |
| Average surgical costs | $13490 | $9089 | < 0.001 |
| Average ancillary costs | $27811 | $18476 | 0.239 |
| Average clinic visits | 4.1 | 3.5 | 0.123 |
| Average ER visits | 1.1 | 1.0 | 0.465 |
| Readmissions | |||
| Average LOS (d) | 5.5 | 5.7 | 0.954 |
| Average days to readmission | 13.5 | 16.5 | 0.552 |
| Average ER visits | 0.0 | 0.5 | 0.267 |
| Average clinic visits | 5.0 | 3.5 | 0.323 |
LOS: Length of stay.
Figure 1.
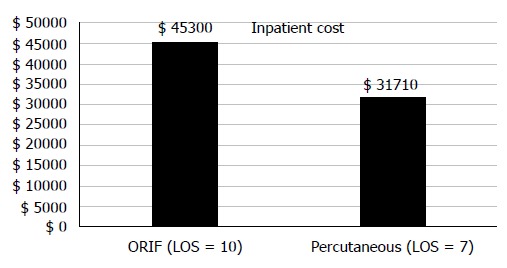
Differences in inpatient costs based on operative approach. ORIF: Open reduction and internal fixation; LOS: Length of stay.
ORIF patients and percutaneous patients had similar numbers of ER and clinic visits before initial hospitalization. Readmissions were rare, with ORIF patients spending an average of 13.5 d between discharge and readmission compared to 16.5 d for percutaneous patients. There were similar numbers of ER and clinic visits occurring in this period for the two groups. The average LOS (about 5.6 d) for readmissions was similar for the two groups (P = 0.954).
Table 3 lists the reasons for complications and readmissions for the two surgical groups. Overall, 10 (10.6%) patients developed complications. While there was a difference in complications between the two groups as shown in Figure 2 (19.4% for ORIF vs 6.3% for percutaneous), this was not statistically significant. The distributions of the complications were similar for the ORIF and percutaneous groups (Figure 3). Similarly, 8 (8.5%) patients had readmissions within 90-d, with a difference in readmission rates based on operative approach (9.5% for percutaneous vs 6.5% for ORIF) that did not reach statistical significance. The distributions of readmissions was also similar between the two groups (Figure 4). When comparing those who sustained complications to those who did not in the ORIF and percutaneous groups, there were no significant differences with respect to age or BMI.
Table 3.
Differences in complications and readmissions based on operative approach
| ORIF (n = 31) | Percutaneous (n = 63) | P value | |
| Complications | |||
| Infection | 1 (3.2) | 1 (1.6) | |
| Nonunion | 1 (3.2) | 1 (1.6) | |
| Hardware failure | 2 (6.4) | 2 (3.2) | |
| DVT | 2 (6.4) | 0 (0) | |
| Total | 6 (19.4) | 4 (6.3) | 0.062 |
| Readmission | |||
| Infection | 0 (0) | 1 (1.6) | |
| Surgical | 2 (6.4) | 1 (1.6) | |
| Medical | 0 (0) | 4 (6.3) | |
| Total | 2 (6.4) | 6 (9.5) | 0.473 |
ORIF: Open reduction and internal fixation; DVT: Deep venous thrombosis.
Figure 2.
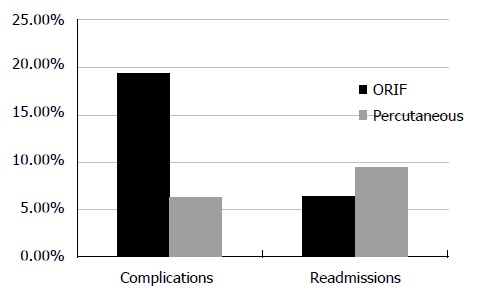
Differences in complication and readmission rates based on operative approach. ORIF: Open reduction and internal fixation.
Figure 3.
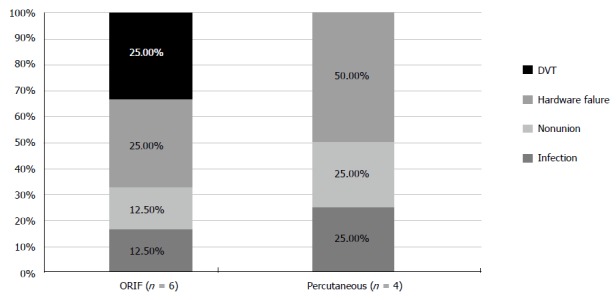
Reasons for complications based on operative approach. ORIF: Open reduction and internal fixation; DVT: Deep venous thrombosis.
Figure 4.
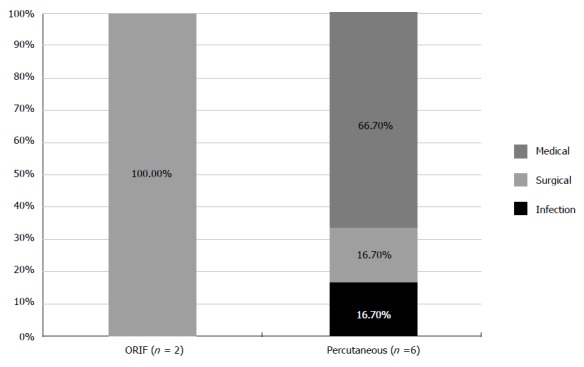
Reasons for readmission based on operative approach. ORIF: Open reduction and internal fixation.
DISCUSSION
LOS during initial hospital admissions has been shown to affect readmission rates, thereby affecting overall quality of care delivered to patients[9]. Based on our study, we have demonstrated a significant difference in the LOS in patients undergoing ORIF vs percutaneous fixation of sacral injuries, with ORIF patients on average staying 3 d longer in the hospital. This amounts to, on average, a difference in LOS costs of close to $14000 for ORIF patients.
The average LOS we obtained for all patients (7.05 d) is within range of similar studies in Level I trauma centers. Vallier et al[10] calculated a LOS of 9.2 d for patients undergoing operative fixation of pelvic and acetabular fractures; in comparison, Dechert et al found an average LOS of 11.5 ± 14.1 d in patients under 65 years of age with pelvic trauma[10,11]. With regards to operative approach, our difference in LOS of 3 d is similar to other orthopaedic studies which show minimally invasive surgical techniques decrease LOS compared to open approaches. For example, decreases up to 3.8 d in LOS due to minimally invasive techniques have been demonstrated in sacroiliac joint fusions[12,13]. Similar decreases in LOS up to 3.2 d have been shown for patients undergoing minimally invasive lumbar fusions compared to open approaches[14-16]. Finally, open dynamic hip screw (DHS) fixation of the femur increases LOS by 4.5 d compared to a minimally invasive DHS[17].
LOS is particularly important as it can also have consequences with respect to rehabilitation[18]. It is also a reliable tool for cost analysis of facility charges. For example, the cost of inpatient rooms are included in total facility charges, which are on average almost 4 times greater than orthopaedic professional charges[19]. An important factor affecting LOS with regard to operative approach reflects how orthopaedic surgeons may postpone surgical fixation. For example, open surgical approaches are often delayed for days for patients with pelvic ring fractures to prevent disruption of tamponade and clot formation[7]. Although percutaneous approaches for sacral fractures may also occur days after admission, with one study finding a delay of 4.2 d prior to fixation, definitive fixation may occur much sooner after admission[20]. Given a decreased delay to fixation coupled with fewer bleeding episodes and other complications, a percutaneous approach for sacral fractures may be a more time-effective procedure leading to savings in LOS costs.
Our study further demonstrated surprisingly high overall readmission (8.5%) and complication (10.6%) rates. Although there were trends toward higher rates of readmissions (9.5%) in the percutaneous group and complications (19.4%) in the ORIF group, these did not reach statistical significance. Nevertheless, our overall complication rate (10.6%) falls within the range of pelvic and acetabular complications reported by Vallier et al[10] study, which found a 12% (58/465 patients with 95 complications) rate of post-operative adverse events.
When comparing complication rates for the two approaches, ORIF treatment outcomes differ across various fracture types. For example, reconstruction plate internal fixation of type C unstable sacral fractures can have a 12.5% infection rate and 15.6% complication rate secondary to urological problems[21]. Conversely, Hsu et al[22] found a low complication rate (1/19 patients) when following-up two post-operatively a patient cohort with displaced sacral fractures treated with open reductions and internal. Other studies showed 2.8% infections in internal fixation[23]. Based on our results for ORIF patients, hardware failure and infection are the top two causes of complications, similar to published results[21-23]. In comparison, percutaneous screw fixation complications can result from poor visualization of relevant anatomy, incomplete fluoroscopy, unexpected anatomic variations, and malreduction[4]. Most common complications, based on our results, include implant failure and infection. Routt et al[24] described fixation failure in 4.5% of patients using a percutaneous iliosacral screw technique, which is close to our 3.17% hardware failure in patients treated percutaneously. Avoidance of deep tissue exposure to the environment in percutaneous approaches is one main reason that is postulated to result in theoretically fewer complications with this approach compared to open techniques[25], although this was not seen in our results. Nevertheless, our results suggest that the percutaneous approach may be just as safe as ORIF in preventing surgical complications. This early data may serve in the future as a quantitative factor for the surgical team to plan and decide whether an open or percutaneous approach is the most efficient manner to approach a fracture. Given that a percutaneous approach is less invasive and faster, allowing for less pain and early post-operative mobilization, our data may implicate that a percutaneous approach is a better “value” approach given shorter LOS and ultimately lower hospital costs. Our results have even demonstrated lower costs associated with anesthesia and surgery for percutaneous patients, highlighting the added value of a percutaneous approach.
Limitations of our study include the retrospective nature of our methodology, which could not account if surgeons may be driven to favor a certain operative approach for specific patient populations. Although the ASA classification was taken into account as a risk-stratifying mechanism, many patient risk factors were not accounted for during data collection. For example, patients referred to our tertiary care center could be held at other centers prior to transportation. Some research suggests a delay to ORIF that may be upwards of 7 d due to delays in transfer[26]. In some cases, ORIF is actually preferred after 7 d because soft-tissue fibrosis may prevent a successful approach with percutaneous fixation[7]. The longer nature of the ORIF approach may therefore confound LOS when compared to the immediacy of a percutaneous approach, with inherent differential risk stratification for the two approaches. In our study, there was no difference in time to surgery once patients were admitted, but ORIF patients did stay significantly longer after surgery, perhaps highlighting more extensive recovery following an open approach. Furthermore, our study only involved patients treated at a single, level-I tertiary care trauma center. These patients may not be representative of the general population, with some bias in the severity of traumatic fractures that may bias our results. High-volume centers like ours often have patients with more medical comorbidities, which factor into LOS calculations due to more hospital days necessary to address these other medical concerns[27]. In our cost analyses, we used a fixed-cost calculation based on total inpatient duration. In this analysis, the use of fluoroscopy or electromyographic monitoring in percutaneous operations was not specifically studied. Yet, the use of these technologies has been shown to impact both safety and cost[28,29]. In addition, hospital legal procedures, insurance status, and the variations in surgeon-specific complication and readmission rates may affect discharge planning, LOS, and ultimately total cost.
The results presented in this study suggest an avenue for quality improvement for patients presenting with sacral fractures. Many health systems have tried to improve patient satisfaction, LOS, complication rates with better discharge planning and education[30,31]. Our study is the first of its kind to demonstrate a significant difference in LOS between ORIF vs percutaneous fixation of sacral injuries, with an average difference of $13590 based on difference in LOS. With similar complication and 90-d readmission rates compared to ORIF, we recommend a percutaneous approach when possible. Our results will provide orthopaedic surgeons with some predictive information as a risk stratification tool to potentially reduce postoperative costs related to sacral fractures.
COMMENTS
Background
In an era with rising healthcare costs, avenues to reduce expenses must be explored including costs associated with length of stay (LOS), complications, and readmissions. Despite sacral fractures constituting a majority of all pelvic trauma, relatively little data exists exploring differences in these areas based on operative approach. The aim of this study is to investigate inpatient LOS, complication rates, and readmission rates for sacral fracture patients based on surgical technique to determine the most cost-effective approach in treating these patients.
Research frontiers
No study to date has investigated LOS, complication, and readmission differences for patients sustaining sacral fracture based on operative approach.
Innovations and breakthroughs
The authors’ study is the first of its kind to show a significant difference in LOS for open reduction and internal fixation (ORIF) vs percutaneous patients, with ORIF patients on average staying 3 more days in the hospital amounting to a cost of approximately $14000 more when compared to percutaneous patients.
Applications
Given similar rates of complications and readmissions, yet an overall decreased LOS and subsequent hospital-related costs when compared percutaneous patients to ORIF patients, patients with sacral fractures should be treated with a percutaneous approach. Percutaneous approaches are common techniques now for most major orthopaedic fractures and can be implemented in any major hospital system, providing an avenue for benchmarking quality based on costs.
Terminology
Open reduction internal fixation is a surgical approach used by orthopaedic surgeons in which a fracture is placed in normal, anatomic position with the aid of implants, often necessitating a large incision. Percutaneous fixation is another surgical approach used by orthopaedic surgeons where a fracture is placed in a normal, anatomic position with pins or other stabilizing devices through the use of X-rays, thereby avoiding the need for large incisions.
Peer-review
The authors have performed a good study, the manuscript is interesting.
Footnotes
Institutional review board statement: This retrospective study was approved by the Vanderbilt University Institutional Review Board, with all data from human subjects appropriately reviewed by the study personnel.
Informed consent statement: This retrospective study was in accordance with the Vanderbilt IRB and required no active informed consent from patients. All the patients information was used in an de-identified manner.
Conflict-of-interest statement: Author William T Obremskey has previously consulted for biometrics and done expert testimony in legal matters. The institution of WTO has received a grant from the Department of Defense. For the remaining authors, none were declared.
Data sharing statement: Statistical output and dataset are available upon request.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: March 4, 2015
First decision: May 13, 2015
Article in press: July 24, 2015
P- Reviewer: Hasegawa M, Kovar FM, Schmitz MR, Vaishya R S- Editor: Tian YL L- Editor: A E- Editor: Jiao XK
References
- 1.Hak DJ, Baran S, Stahel P. Sacral fractures: current strategies in diagnosis and management. Orthopedics. 2009;32:752–757. doi: 10.3928/01477447-20090818-18. [DOI] [PubMed] [Google Scholar]
- 2.Mehta S, Auerbach JD, Born CT, Chin KR. Sacral fractures. J Am Acad Orthop Surg. 2006;14:656–665. doi: 10.5435/00124635-200611000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Park YS, Baek SW, Kim HS, Park KC. Management of sacral fractures associated with spinal or pelvic ring injury. J Trauma Acute Care Surg. 2012;73:239–242. doi: 10.1097/TA.0b013e31825a79d2. [DOI] [PubMed] [Google Scholar]
- 4.Barei DP, Bellabarba C, Mills WJ, Routt ML. Percutaneous management of unstable pelvic ring disruptions. Injury. 2001;32 Suppl 1:SA33–SA44. doi: 10.1016/s0020-1383(01)00059-6. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein A, Phillips T, Sclafani SJ, Scalea T, Duncan A, Goldstein J, Panetta T, Shaftan G. Early open reduction and internal fixation of the disrupted pelvic ring. J Trauma. 1986;26:325–333. doi: 10.1097/00005373-198604000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Simonain PT, Routt C, Harrington RM, Tencer AF. Internal fixation for the transforaminal sacral fracture. Clin Orthop Relat Res. 1996;(323):202–209. doi: 10.1097/00003086-199602000-00028. [DOI] [PubMed] [Google Scholar]
- 7.Routt ML, Meier MC, Kregor PJ, Mayo KA. Percutaneous iliosacral screws with the patient supine technique. Operative Techniques in Orthopaedics. 1993;3:35–45. [Google Scholar]
- 8.Tsiridis E, Upadhyay N, Giannoudis PV. Sacral insufficiency fractures: current concepts of management. Osteoporos Int. 2006;17:1716–1725. doi: 10.1007/s00198-006-0175-1. [DOI] [PubMed] [Google Scholar]
- 9.Carey K, Lin MY. Hospital length of stay and readmission: an early investigation. Med Care Res Rev. 2014;71:99–111. doi: 10.1177/1077558713504998. [DOI] [PubMed] [Google Scholar]
- 10.Vallier HA, Cureton BA, Patterson BM. Factors affecting revenue from the management of pelvis and acetabulum fractures. J Orthop Trauma. 2013;27:267–274. doi: 10.1097/BOT.0b013e318269b2c3. [DOI] [PubMed] [Google Scholar]
- 11.Switzer JA, Gammon SR. High-energy skeletal trauma in the elderly. J Bone Joint Surg Am. 2012;94:2195–2204. doi: 10.2106/JBJS.K.01166. [DOI] [PubMed] [Google Scholar]
- 12.Lorio MP, Polly DW, Ninkovic I, Ledonio CG, Hallas K, Andersson G. Utilization of Minimally Invasive Surgical Approach for Sacroiliac Joint Fusion in Surgeon Population of ISASS and SMISS Membership. Open Orthop J. 2014;8:1–6. doi: 10.2174/1874325001408010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith AG, Capobianco R, Cher D, Rudolf L, Sachs D, Gundanna M, Kleiner J, Mody MG, Shamie AN. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res. 2013;7:14. doi: 10.1186/1750-1164-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2009;34:1385–1389. doi: 10.1097/BRS.0b013e3181a4e3be. [DOI] [PubMed] [Google Scholar]
- 15.Schizas C, Tzinieris N, Tsiridis E, Kosmopoulos V. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop. 2009;33:1683–1688. doi: 10.1007/s00264-008-0687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shunwu F, Xing Z, Fengdong Z, Xiangqian F. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976) 2010;35:1615–1620. doi: 10.1097/BRS.0b013e3181c70fe3. [DOI] [PubMed] [Google Scholar]
- 17.Mahmood A, Kalra M, Patralekh MK. Comparison between Conventional and Minimally Invasive Dynamic Hip Screws for Fixation of Intertrochanteric Fractures of the Femur. ISRN Orthop. 2013;2013:484289. doi: 10.1155/2013/484289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loganathan V, Yazeedi WA, George LA. Predictors of the Length of Stay of Inpatients in Rehabilitation Setting After Traumatic Spinal Cord Injury. Open Access Scientific Reports. 2012;1:141. [Google Scholar]
- 19.Vallier HA, Patterson BM, Meehan CJ, Lombardo T. Orthopaedic traumatology: the hospital side of the ledger, defining the financial relationship between physicians and hospitals. J Orthop Trauma. 2008;22:221–226. doi: 10.1097/BOT.0b013e31815e92e5. [DOI] [PubMed] [Google Scholar]
- 20.Nork SE, Jones CB, Harding SP, Mirza SK, Routt ML. Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma. 2001;15:238–246. doi: 10.1097/00005131-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Ayoub MA. Vertically unstable sacral fractures with neurological insult: outcomes of surgical decompression and reconstruction plate internal fixation. Int Orthop. 2009;33:261–267. doi: 10.1007/s00264-007-0468-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hsu JR, Bear RR, Dickson KF. Open reduction internal fixation of displaced sacral fractures: technique and results. Orthopedics. 2010;33:730. doi: 10.3928/01477447-20100826-07. [DOI] [PubMed] [Google Scholar]
- 23.Matta JM, Tornetta P. Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res. 1996;(329):129–140. doi: 10.1097/00003086-199608000-00016. [DOI] [PubMed] [Google Scholar]
- 24.Routt ML, Simonian PT, Mills WJ. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997;11:584–589. doi: 10.1097/00005131-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Giannoudis PV, Tzioupis CC, Pape HC, Roberts CS. Percutaneous fixation of the pelvic ring: an update. J Bone Joint Surg Br. 2007;89:145–154. doi: 10.1302/0301-620X.89B2.18551. [DOI] [PubMed] [Google Scholar]
- 26.Templeman D, Goulet J, Duwelius PJ, Olson S, Davidson M. Internal fixation of displaced fractures of the sacrum. Clin Orthop Relat Res. 1996;(329):180–185. doi: 10.1097/00003086-199608000-00021. [DOI] [PubMed] [Google Scholar]
- 27.Genuario J, Koval KJ, Cantu RV, Spratt KF. Does hospital surgical volume affect in-hospital outcomes in surgically treated pelvic and acetabular fractures? Bull NYU Hosp Jt Dis. 2008;66:282–289. [PubMed] [Google Scholar]
- 28.Dzaja I, MacDermid JC, Roth J, Grewal R. Functional outcomes and cost estimation for extra-articular and simple intra-articular distal radius fractures treated with open reduction and internal fixation versus closed reduction and percutaneous Kirschner wire fixation. Can J Surg. 2013;56:378–384. doi: 10.1503/cjs.22712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wiss DA. What’s new in orthopaedic trauma. J Bone Joint Surg Am. 2001;83-A:1762–1772. doi: 10.2106/00004623-200111000-00032. [DOI] [PubMed] [Google Scholar]
- 30.Shepperd S, Parkes J, McClaren J, Phillips C. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2004;(1):CD000313. doi: 10.1002/14651858.CD000313.pub2. [DOI] [PubMed] [Google Scholar]
- 31.Sanders R. The economics of trauma. J Orthop Trauma. 2008;22:215. doi: 10.1097/BOT.0b013e3181739395. [DOI] [PubMed] [Google Scholar]


