Abstract
Background
The National Healthcare Safety Network (NHSN) classifies surgical procedures into 40 categories. The objective of this study was to determine surgical site infection (SSI) incidence for clinically defined subgroups within 5 heterogeneous NHSN surgery categories.
Methods
This is a retrospective cohort study using the longitudinal State Inpatient Database. We identified 5 groups of surgical procedures (amputation; biliary, liver and pancreas [BILI]; breast; colon and hernia) using ICD-9-CM procedure codes in community hospitals in California, Florida and New York from January 2009 through September 2011 in persons aged ≥18 years. Each of these 5 categories was classified to more specific surgical procedures within the group. 90-day SSI rates were calculated using ICD-9-CM diagnosis codes.
Results
There were 62,901 amputation, 33,358 BILI, 72,058 breast, 125,689 colon and 85,745 hernia surgeries in 349,298 people. 90-day SSI rates varied significantly within each of the 5 subgroups. Within the BILI category, bile duct, pancreas and laparoscopic liver procedures had SSI rates of 7.2%, 17.2%, and 2.2%, respectively (p<0.0001 for each) compared to open liver procedures (11.1% SSI).
Conclusion
90-day SSI rates varied widely within certain NHSN categories. Risk adjustment for specific surgery type is needed in order to make valid comparisons between hospitals.
Keywords: surgical site infection, surveillance, risk adjustment, National Healthcare Safety Network
Introduction
The estimated number of surgical site infections (SSIs) in the US was 157,500 in 2011, making SSIs the most common (tied with pneumonia) healthcare associated infection (HAI) among inpatients in acute care hospitals (21.8% of HAIs).(1) SSIs increase healthcare costs (2, 3) and postoperative hospital length of stay(3).
The National Healthcare Safety Network (NHSN) is a web-based surveillance system used by the Centers for Disease Control and Prevention (CDC) to track HAIs, including SSIs. NHSN allows hospitals, dialysis centers and other medical facilities to collect and report infection rates and other important healthcare process measures. NHSN classifies surgical procedures into 40 categories ranging from very specific procedures (e.g. coronary artery bypass graft with chest incision only) to more heterogeneous procedures such as bile duct, liver and pancreas surgeries grouped together(4).
NHSN recently improved their SSI risk prediction models by identifying specific factors associated with SSI risk for each NHSN procedure category. The variables included in some or all of the individual models are: wound class, duration of procedure, American Society of Anesthesiology (ASA) score, gender, age, emergency, trauma, general anesthesia, medical school affiliation, number of hospital beds, endoscope, outpatient setting and other procedure-specific variables (5). NHSN also started collecting information on diabetes, height and weight for all procedures in 2014, although these variables are not yet used for risk adjustment of SSI rates(4).
SSIs after colon surgery and abdominal hysterectomy from over 4,000 hospitals in the U.S. are publically reported through Hospital Compare, based on NHSN definitions. Hospital Compare is a website created by the Centers for Medicare and Medicaid Services (CMS) to help patients choose hospitals and to encourage hospitals to improve quality of care(6). SSIs reported on the Hospital Compare website include deep incisional and organ/space SSIs within 30 days of surgery in adults diagnosed during the index surgery hospitalization, subsequent readmissions and SSIs identified from post-discharge surveillance. The reported SSI rates on the Hospital Compare website are risk adjusted only for age and ASA score(7). Beginning in fiscal year 2016, SSIs complicating NHSN-defined colon and abdominal hysterectomy procedures will be added to the list of measures used by CMS to calculate a hospital-acquired condition score; hospitals with scores in the lowest performing quartile will be financially penalized(8).
Hospitals that perform higher proportions of complex surgeries may have higher SSI rates. For example, NHSN reported higher SSI rates for spinal re-fusion procedures compared to initial spinal fusion and laminectomy procedures, and higher SSI rates for abdominal hysterectomy compared to vaginal hysterectomy(9). Appropriate risk adjustment is needed to accurately compare SSI rates between hospitals, especially when these comparisons are associated with public perceptions of quality of care in hospitals and reimbursement.
The objective of this study was to analyze SSI incidence for specific clinically defined procedures in 5 heterogeneous NHSN surgery categories (amputation; biliary, liver or pancreas [BILI]; breast; colon and hernia), to determine if adjustment for specific procedure type should be incorporated into the standard risk adjustment algorithm.
Materials and Methods
This was a retrospective cohort study using the State Inpatient Database (SID), which is part of the Healthcare Cost and Utilization Project (HCUP)(10). The SID contains inpatient discharge records from U.S. community hospitals in participating states and includes all patients regardless of insurance status. An encrypted person identifier allows longitudinal follow-up in some of the states. The primary (first) diagnosis variable is the primary reason in retrospect for hospitalization; all other diagnosis variables are referred to as secondary diagnoses.
We identified 5 groups of surgical procedures (amputation, BILI, breast, colon and hernia) in community hospitals in California, Florida and New York from January 2009 through September 2011 in persons aged ≥18 years. Using the American Hospital Association (AHA) Annual Survey of Hospitals (Chicago, IL), rehabilitation, psychiatric and dependency, and long-term acute care hospitals were excluded. The AHA Annual Survey data were also used to determine the teaching status of hospitals. Surgeries were identified according to the NHSN classification for SSI surveillance (4) using International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) procedure codes. Each of these 5 categories was further classified into more specific operative subgroups (Appendix with list of ICD-9-CM codes available upon request from authors).
Discharges for persons with residency in a state different from the hospital or with missing person identifier, length of stay or gender during the index surgical hospitalization were excluded. Discharges with a primary diagnosis of SSI (Appendix with list of ICD-9-CM codes used to identify SSI is available upon request from authors) in the index hospitalization or with coding for SSI in a previous hospital admission within 30 days were also excluded in order to identify incident SSIs only. Because of the high proportions of multiple procedures among BILI, colon and hernia surgeries, certain surgery combinations were allowed (i.e., BILI surgeries performed during the same hospitalization with gastric, gall bladder and/or exploratory laparotomy; open colectomy surgeries with small bowel, appendix, rectal or exploratory laparotomy; and hernia surgeries with exploratory laparotomy). These combinations follow the NHSN procedure category hierarchical selection list that ranks surgeries by their SSI risk (4). Discharges with all other combinations of surgical procedures were excluded.
Readmissions within 90 days of the index surgery were identified starting from the day of index surgery (considered day 0). The observation period for SSI was censored if the person had a subsequent NHSN surgery within 90 days of the index surgery. SSIs were identified using ICD-9-CM diagnosis codes tailored to the individual surgical grouping, including secondary diagnosis variables in the index hospitalization, any diagnosis codes during a non-censored readmission, and the primary diagnosis code of a readmission censored at the time of a subsequent operation. Infections that could have been the reason for the index surgery (e.g., gas gangrene, necrotizing fasciitis) were considered SSIs only if they were coded during a readmission. The Washington University Human Research Protection Office declared this study exempt from Institutional Review Board oversight.
Baseline characteristics were identified from the index hospitalization including age, diabetes, hospital teaching status and health insurance type and their distributions were reported by surgery type. SSI rates per 100 procedures were calculated for the 5 surgery categories and their subgroups. This calculation was repeated including all SSIs, without censoring for a subsequent surgery. The Chi square test was used to test the association between surgery subgroups and SSI using the most common subgroup as the reference category. The significance level was adjusted for multiple comparisons according to the Bonferroni method. SAS Enterprise Guide version 5.1 (SAS Institute Inc., Cary, NC, USA) was used for all data management and analyses.
Results
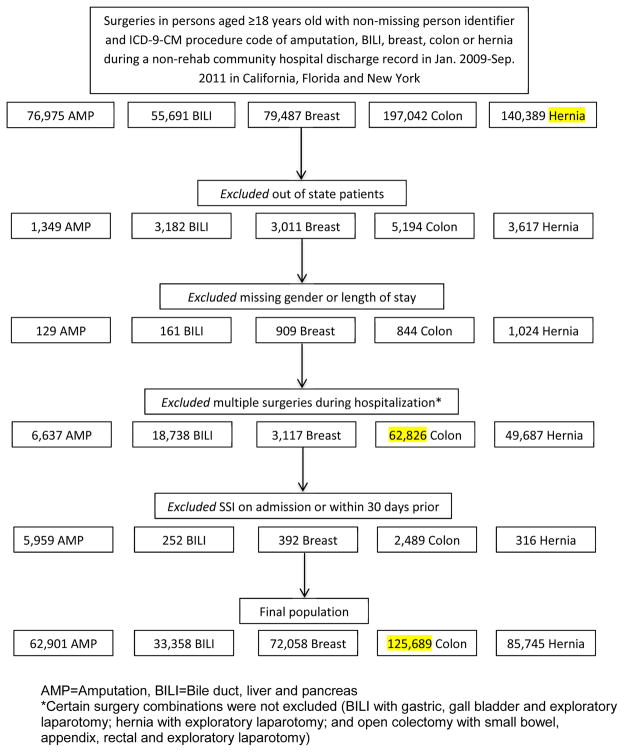
There were 62,901 amputation, 33,358 BILI, 72,058 breast, 125,689 colon and 85,745 hernia index surgeries performed in 349,298 persons in California, Florida and New York from January 2009 through September 2011. 26,691 (7.6%) of study subjects had more than 1 index surgery. Figure 1 shows the inclusion and exclusion criteria and the algorithm that resulted in the final population for analysis.
Figure 1.
Inclusion/exclusion criteria algorithm that resulted in final population
Table 1 shows select baseline characteristics for index hospitalizations. Upper limb amputation procedures were more likely to be performed in teaching hospitals (58.6%) than lower limb amputation procedures (47.8%–51.1%). Discharges with above-knee amputations were less likely to be coded for diabetes compared to more distal lower limb amputations (Table 1). 80% of pancreas and 74.7% of open liver surgeries were performed in teaching hospitals, vs. 50.3% of bile duct and 50% of laparoscopic liver surgeries. Laparoscopic liver surgeries were more likely to have private insurance as the expected payer (51.4%) compared to Medicare or other health insurance coverage.
Table 1.
Baseline characteristics of index hospitalization population
| Surgery | Age (years) Median (range) |
Diabetes N (%) |
Teaching hospital N (%) |
Medicare N (%) |
Private N (%) |
|---|---|---|---|---|---|
|
| |||||
| Amputation | |||||
| Upper limb | 54 (18–99) | 1,375 (35) | 2,305 (58.6) | 1,545 (39.3) | 756 (19.2) |
| Toe | 61 (18–103) | 23,703 (84.6) | 13,378 (47.8) | 14,458 (51.6) | 5,727 (20.4) |
| Ankle and foot | 62 (18–105) | 6,292 (85.3) | 3,769 (51.1) | 4,189 (56.8) | 1,285 (17.4) |
| Knee and leg | 65 (18–110) | 10,172 (75.4) | 6,570 (48.7) | 8,587 (63.7) | 1,921 (14.2) |
| Above knee | 73 (18–107) | 5,662 (56.1) | 5,098 (50.5) | 7,799 (77.3) | 863 (8.5) |
|
| |||||
| BILI | |||||
| Pancreas | 63 (18–100) | 1,962 (29.7) | 5,287 (80) | 2,971 (44.9) | 2,565 (38.8) |
| Bile duct | 63 (18–102) | 1,850 (22.5) | 4,126 (50.3) | 3,871 (47.2) | 2,438 (29.7) |
| Open liver | 61 (18–98) | 2,233 (22) | 7,585 (74.7) | 4,035 (39.7) | 4,128 (40.6) |
| Laparoscopic liver | 54 (18–104) | 2,676 (31.9) | 4,191 (50) | 2,639 (31.5) | 4,309 (51.4) |
|
| |||||
| Breast | |||||
| Flap | 51 (18–86) | 177 (7.4) | 1,645 (68.8) | 291 (12.2) | 1,719 (71.9) |
| Mastectomy+flap | 52 (21–91) | 175 (6.8) | 1,790 (69.1) | 271 (10.5) | 2,004 (77.4) |
| Mastectomy+expander/implant | 51 (19–93) | 873 (6.8) | 6,735 (52.5) | 1,925 (15) | 9,640 (75.1) |
| Mastectomy | 66 (18–101) | 5,065 (19.3) | 12,520 (47.7) | 13,431 (51.2) | 8,496 (32.4) |
| Expander/implant | 52 (18–93) | 160 (7.5) | 1,248 (58.8) | 431 (20.3) | 1,254 (59) |
| Breast conserving surgery | 60 (18–101) | 1,889 (20.7) | 4,487 (49.2) | 3,763 (41.3) | 3,139 (34.4) |
| Reduction/mastopexy/other | 48 (18–90) | 320 (7.9) | 2,127 (52.6) | 566 (14) | 2,537 (62.7) |
| Multiple | 52 (18–103) | 932 (7.3) | 7,704 (60.6) | 2,213 (17.4) | 8,971 (70.5) |
|
| |||||
| Colon | |||||
| Open colectomy | 67 (18–104) | 7,703 (20.5) | 14,221 (37.8) | 20,663 (54.9) | 11,954 (31.8) |
| Open colectomy+SB | 67 (18–103) | 1,522 (20.9) | 3,595 (49.3) | 4,143 (56.8) | 1,949 (26.7) |
| Open colectomy+APPY | 54.5 (18–99) | 240 (15.2) | 617 (39.1) | 493 (31.2) | 708 (44.9) |
| Open colectomy+REC | 66 (18–96) | 125 (15.9) | 356 (45.4) | 406 (51.7) | 271 (34.5) |
| Open colectomy+XLAP | 67 (18–101) | 2,173 (20.7) | 4,575 (43.6) | 5,770 (55) | 3,243 (30.9) |
| Open colectomy±other bowel +colostomy | 67 (18–101) | 3,167 (18.6) | 6,246 (36.7) | 9,398 (55.2) | 4,756 (28) |
| Laparoscopic colectomy | 64 (18–104) | 6,013 (16.8) | 16,924 (47.3) | 16,823 (47) | 16,330 (45.6) |
| Laparoscopic colectomy +colostomy | 66 (18–98) | 171 (16.5) | 420 (40.6) | 563 (54.4) | 349 (33.7) |
| Colostomy | 64 (18–100) | 891 (24.6) | 1,628 (45) | 2,075 (57.3) | 750 (20.7) |
| Other | 62 (18–103) | 1,838 (17.6) | 4,958 (47.6) | 4,880 (46.8) | 3,432 (32.9) |
|
| |||||
| Hernia | |||||
| Incisional/anterior abdominal | 60 (18–102) | 13,087 (23.6) | 25,381 (45.8) | 24,569 (44.3) | 20,597 (37.2) |
| Umbilical | 55 (18–107) | 2,240 (22.7) | 4,663 (47.3) | 3,383 (34.3) | 3,622 (36.7) |
| Inguinal/femoral | 70 (18–104) | 2,874 (14) | 8,739 (42.7) | 11,763 (57.5) | 3,935 (19.2) |
SB=Small bowel surgery, APPY= Appendix surgery, REC= Rectal surgery, XLAP= Exploratory laparotomy
Mastectomies were performed on older patients (median age 66), compared to mastectomies plus flap or expander/implant reconstruction. 69.1% of mastectomy plus flap reconstruction and 52.5% of mastectomy plus expander/implant were performed in teaching hospitals, compared to 47.7% of mastectomy alone. The proportions of mastectomy and breast conserving surgery discharges that were coded for diabetes were 19.3% and 20.7%, respectively, which were higher compared to other breast surgeries.
Higher percentages of open colectomies plus other bowel surgeries were done in teaching hospitals than open colectomy alone (Table 1). Discharges with laparoscopic colectomies and open colectomies plus either appendix or rectum surgeries were less likely to be coded for diabetes, compared to discharges with open colectomies with/without small bowel or exploratory laparotomy.
The median age of patients undergoing incisional/anterior abdominal, umbilical and inguinal/femoral hernia surgeries were 60, 55 and 70 years, respectively. 42.7% of inguinal/femoral hernia surgeries were performed in teaching hospitals, compared to 47.3% and 45.8% of umbilical and incisional/anterior abdominal hernia repairs, respectively.
Surgery and SSI counts, SSI rates with and without censoring and overall SSI rates are shown in Table 2 and the comparison of SSI rates for select subgroups is shown in Table 3. Among amputation surgeries, the SSI rate was lowest for upper limb (6.8%) and highest for ankle and foot amputation (17.9%). Both ankle and foot amputations were significantly different compared to toe amputation, the most common amputation procedure. Among BILI surgeries, SSI rates after laparoscopic liver, bile duct, and pancreas procedures were 2.2%, 7.2%, and 17.2%, respectively. All were significantly different from the SSI rate after open liver procedures (11.1%).
Table 2.
Surgery and SSI counts and SSI rates with/without censoring
| With censoring* | Without censoring† | ||||
|---|---|---|---|---|---|
|
| |||||
| Surgery | Surgery count | SSI count | SSI rate‡ | Overall SSI rate‡ | SSI rate‡ |
|
| |||||
| Amputation | 13.7 | ||||
| Upper limb | 3,934 | 267 | 6.8 | 8.0 | |
| Toe | 28,014 | 3,582 | 12.8 | 19.6 | |
| Ankle and foot | 7,373 | 1,322 | 17.9 | 25.4 | |
| Knee and leg | 13,485 | 2,108 | 15.6 | 19.1 | |
| Above knee | 10,095 | 1,332 | 13.2 | 14.4 | |
|
| |||||
| BILI | 9.1 | ||||
| Pancreas | 6,610 | 1,136 | 17.2 | 17.4 | |
| Bile duct | 8,205 | 589 | 7.2 | 7.3 | |
| Open liver | 10,159 | 1,125 | 11.1 | 10.9 | |
| Laparoscopic liver | 8,384 | 182 | 2.2 | 2.6 | |
|
| |||||
| Breast | 3.6 | ||||
| Flap | 2,392 | 152 | 6.4 | 6.2 | |
| Mastectomy+flap | 2,589 | 125 | 4.8 | 5.2 | |
| Mastectomy+expander/implant | 12,834 | 654 | 5.1 | 5.2 | |
| Mastectomy | 26,239 | 602 | 2.3 | 2.4 | |
| Expander/implant | 2,124 | 156 | 7.3 | 6.3 | |
| Breast conserving surgery | 9,115 | 219 | 2.4 | 2.4 | |
| Reduction/mastopexy/other | 4,046 | 81 | 2.0 | 2.0 | |
| Multiple | 12,719 | 624 | 4.9 | 5.0 | |
|
| |||||
| Colon | 19.2 | ||||
| Open colectomy | 37,634 | 5,913 | 15.7 | 16.2 | |
| Open colectomy+SB | 7,298 | 2,138 | 29.3 | 29.8 | |
| Open colectomy+APPY | 1,578 | 255 | 16.2 | 16.3 | |
| Open colectomy+REC | 785 | 147 | 18.7 | 19.4 | |
| Open colectomy+XLAP | 10,492 | 2,258 | 21.5 | 22.0 | |
| Open colectomy±other bowel +colostomy | 17,013 | 8,936 | 52.5 | 52.9 | |
| Laparoscopic colectomy | 35,808 | 2,732 | 7.6 | 8.1 | |
| Laparoscopic colectomy +colostomy | 1,035 | 333 | 32.2 | 32.9 | |
| Colostomy | 3,621 | 357 | 9.9 | 10.3 | |
| Other | 10,425 | 998 | 9.6 | 10.4 | |
|
| |||||
| Hernia | 4.9 | ||||
| Incisional/anterior abdominal | 55,416 | 3,363 | 6.1 | 6.4 | |
| Umbilical | 9,862 | 420 | 4.3 | 4.5 | |
| Inguinal/femoral | 20,467 | 395 | 1.9 | 2.2 | |
SB=Small bowel surgery, APPY= Appendix surgery, REC= Rectal surgery, XLAP= Exploratory laparotomy
Follow-up for SSI was censored at time of a subsequent NHSN surgery within 90 days of the earlier surgery. SSIs identified within 90 days after the 2nd surgery were attributed to the 2nd surgery.
The denominator could change when censoring was not implemented because subsequent surgeries within 90 days of a previous surgery in the same category were not counted. The numerator could also change; when there were 2 surgeries within 90 days of each other, an SSI that was within 90 days after the 2nd surgery but >90 days after the 1st surgery was not counted when censoring was not performed because the 2nd surgery was not counted.
SSI rate/100 procedures.
Table 3.
Comparison of SSI rates for surgery subgroups
| Surgery | SSI rate/100 procedures | p* |
|---|---|---|
|
| ||
| Amputation | ||
| Toe | 12.8 | Reference |
| Upper limb | 6.8 | <0.0001 |
| Ankle and foot | 17.9 | <0.0001 |
| Knee and leg | 15.6 | <0.0001 |
| Above knee | 13.2 | 0.2941 |
|
| ||
| BILI | ||
| Open liver | 11.1 | Reference |
| Bile duct | 7.2 | <0.0001 |
| Pancreas | 17.2 | <0.0001 |
| Laparoscopic liver | 2.2 | <0.0001 |
|
| ||
| Breast | ||
| Mastectomy | 2.3 | Reference |
| Mastectomy+flap | 4.8 | <0.0001 |
| Mastectomy+expander/implant | 5.1 | <0.0001 |
|
| ||
| Colon | ||
| Open colectomy | 15.7 | Reference |
| Open colectomy+SB | 29.3 | <0.0001 |
| Open colectomy+APPY | 16.2 | <0.6322 |
| Open colectomy+REC | 18.7 | 0.0218 |
| Open colectomy+XLAP Open colectomy ±other | 21.5 | <0.0001 |
| bowel+colostomy | 52.5 | <0.0001 |
| Laparoscopic colectomy | 7.6 | <0.0001 |
|
| ||
| Hernia | ||
| Incisional/anterior abdominal | 6.1 | Reference |
| Umbilical | 4.3 | <0.0001 |
| Inguinal/femoral | 1.9 | <0.0001 |
SB=Small bowel surgery, APPY= Appendix surgery, REC= Rectal surgery, XLAP= Exploratory laparotomy
Alpha adjusted for multiple comparisons was: amputation (0.012), BILI (0.016), breast (0.025), colon (0.008) and hernia (0.025).
Mastectomy plus flap and mastectomy plus insertion of an expander/implant (SSI rates, 4.8% and 5.1%, respectively) were both associated with higher SSI rates compared to mastectomy alone (2.3%, p <0.0001). Open colectomy alone had a significantly lower SSI rate (15.7%) compared to open colectomy performed with small bowel, exploratory laparotomy or colostomy procedures (all p <0.0001). However, the SSI incidence of open colectomy was not significantly different compared to open colectomy with either appendix or rectum surgeries (p=0.6322 and 0.0218, respectively, alpha=0.008). Incisional/anterior abdominal hernia procedures had significantly higher SSI rates (6.1%) compared to umbilical (4.3%) and inguinal/femoral (1.9%) procedures (Table 3).
In general, the overall SSI incidence of a category differed from the SSI incidence of the individual subgroups. In addition, SSI rates were generally higher when follow up was not censored at the time of a subsequent surgery within 90 days (Table 2). Lack of censoring in amputation procedures increased the SSI rates by 1.2–7.5 SSI/100 procedures. For other surgeries (BILI, breast, colon and hernia), SSI rates increased by an average of 0.24 SSI/100 procedures when censoring was not performed.
Discussion
Our results suggest that specific types of procedures within the NHSN surgical categories amputation, BILI, breast, colon and hernia have wide variation in their 90-day SSI risk and vary significantly compared to the overall SSI rates of the NHSN category. Since individual hospitals perform varying proportions of high and low SSI risk procedures that are reported in one NHSN category, this potentially leads to confounding by procedure type. Our results suggest that using procedure-specific SSI rates or controlling for procedure type may improve SSI risk adjustment for amputation, BILI, breast, colon and hernia surgeries.
The most common surgery type in a heterogeneous NHSN category had the most influence on the overall SSI rate (e.g. toe amputation, 44.5% of amputation, had SSI rate of 12.8% vs. 13.7% overall amputation SSI). We found that the most common surgical procedure varied by hospital teaching status and likely varies also by surgeon. Procedures varied in their SSI risk and in the proportions performed in teaching hospitals. For example, within the BILI category, pancreas and open liver surgeries were more likely to be performed at teaching hospitals and had the highest SSI risk (17.2% and 11.1%, respectively vs. 9.1% overall). Thus teaching hospitals that perform higher proportions of more complex surgeries would be expected to have higher BILI SSI rates.
Certain NHSN procedure categories are very specific (e.g., NHSN categories for coronary artery bypass graft based on whether there was only a chest incision or both chest and donor site incisions) but other NHSN surgical categories are not very specific at all. In the most recent 2009 NHSN report, SSI rates stratified by the old risk index (procedure duration, wound class and ASA score) were reported. Laminectomy, spinal fusion and re-fusion surgeries had SSI rates of 0.72–2.3, 0.7–4.15 and 2.3–8.73 per 100 procedures, respectively. Abdominal and vaginal hysterectomies had SSI rates of 1.1–4.05 and 0 per 100 procedures, respectively.(9) This shows the varied SSI risk among different types of spinal orthopedic surgeries and hysterectomy surgical approaches that warranted separating them into distinct categories. In contrast, other NHSN procedure categories that include a diverse group of procedures (e.g. amputation and BILI) are not yet adjusted sufficiently for specific surgery type. Mu et al used procedure-specific variables already collected by NHSN to risk adjust hip procedures for type of surgery (total primary, partial primary, partial revision or total revision), knee prosthesis for type of surgery (primary or revision), spinal fusion for surgical approach and spinal level, and colon for endoscope use. These variables were independently associated with SSI risk, (5) confirming the importance of these procedure-specific factors in determining SSI risk.
In agreement with our findings, SSI risk has been shown previously by other investigators to vary within some surgery groups. Higher SSI proportions were reported after colon surgery with colostomy vs. no colostomy at a single hospital in Italy, (11) and left sided colectomy was independently associated with higher SSI risk compared to other colectomies in New York state hospitals.(12) Trans-tibial amputations had significantly higher 30-day deep incisional SSI risk than trans-femoral amputations in people ≥50 years old in a study by Hasanadka et al using data from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP).(13) Olsen found that mastectomy plus immediate implant and mastectomy plus flap had higher 1-year SSI risk than mastectomy only at a tertiary care university hospital.(14) Using the NSQIP data, De Blacam found that mastectomy was associated with higher 30-day SSI risk compared to breast-conserving surgery.(15) In this current study, we found similar SSI risk for mastectomy and breast conserving surgery, possibly because our data included only breast-conserving surgeries performed during inpatient hospital stays, which are more likely to be performed in higher-risk women compared to breast-conserving surgeries performed as outpatient surgery (95.5% of breast-conserving surgeries are outpatient procedures(16)). Using commercial insurer claims data, Nickel found that 90-day SSI rates after hernia repair surgeries varied by anatomic location(17).
Limitations and Strengths
There are several limitations to this study. First, only inpatient hospitalizations billing records were used, and therefore, SSIs diagnosed and treated in outpatient settings would not be captured. Most SSIs treated as outpatients are superficial incisional SSIs (18). Using post-discharge surveillance to identify SSIs in outpatient settings will lead to detection of more SSIs (19–21). However, in the absence of a reliable method used consistently across facilities (22), variation in performance of post-discharge outpatient surveillance will result in reduced comparability of SSI rates among facilities. The inpatient billing data we used also did not capture surgeries performed in ambulatory settings within a hospital. Patients who undergo surgery in outpatient settings are likely healthier than persons who have surgery during an inpatient hospitalization, and therefore the SSI rates after these outpatient procedures may be lower than what we found after inpatient surgery. The proportions of ambulatory procedures we examined are likely low in all categories except breast conserving surgery, cosmetic augmentation/breast implant reconstruction only, and hernia repair(16). ICD-9-CM diagnosis codes are assigned at hospital discharge and do not carry date stamps. Therefore, it is not known whether some infections coded during the original surgical admission were present before surgery and so should not be attributed to that procedure. We tried to minimize SSI present at admission or present during the index surgery in two ways: by excluding procedures with a primary diagnosis of SSI during the index surgery hospitalization, and by restricting identification of infections that could have been the reason for surgery (e.g. gas gangrene) to only readmission hospitalizations. These steps probably minimize but not completely eliminate this bias.
The NHSN surgery list used for this study does not include all possible surgical procedures. This could lead to misclassification since an SSI might have been falsely attributed to an NHSN surgery instead of a prior or subsequent non-NHSN surgery. Finally, the SID data were developed for billing purposes, not research, and ICD-9-CM codes are not perfectly accurate, which might lead to misclassification of the outcome. However, there is no evidence for variation in accuracy of coding of SSIs across subgroups within the same NHSN category. Therefore, this bias would likely be non-differential, resulting in bias towards the null hypothesis. The strengths of this study are the large population size and generalizability since all eligible procedures from 3 large and diverse states in the U.S. were used. The SID includes approximately 97% of all community hospital discharges. Because our data included records from almost all hospitals in a state, it is unlikely that we missed many readmission records, especially since we excluded out-of-state patients who might be more likely to seek subsequent care at a hospital in their state of residence. We also censored follow-up after subsequent procedures to avoid misattribution of SSIs and to replicate NHSN SSI surveillance guidelines. Our findings show that lack of censoring results in higher SSI rates generally. In addition, we excluded surgeries with pre-existing infections in order to identify SSIs attributable to the individual procedures.
Conclusion
In conclusion, some NHSN surgical categories include groups of procedures that are heterogeneous with respect to their SSI risk, suggesting that these categories should either be split into multiple specific subgroups or that the relevant operative variables should be added to risk adjustment models to account for differences in complexity of procedures between institutions. Further research is needed to more precisely determine what operative and patient-level factors are independently associated with SSI risk in these heterogeneous groups of surgical procedures. Our findings are particularly relevant to the NHSN SSI surveillance and the CMS Hospital Compare data, in which SSI rates are tied to public perception of quality of care and reimbursement. Our results suggest that inclusion of specific operative risk factors to the NHSN risk adjustment models or stratification by specific procedure subgroups is important in order to make valid comparisons of SSI rates between hospitals.
Highlights.
We identified surgical site infection (SSI) in subgroups of 5 NHSN defined groups.
The groups included amputation, biliary-liver-pancreas, breast, colon and hernia.
Subgroups within a category were heterogeneous in their 90-day SSI rates.
Proportions of operations performed in teaching hospitals varied within categories.
Controlling for surgery type might facilitate SSI rate comparison among hospitals.
Acknowledgments
We thank Cherie Hill for database management and computer support.
ERD, VJF, and MAO were supported in part by the Centers for Disease Control and Prevention (CDC) Epicenters Program (U54CK000162) (VJF).
Appendices
Appendix A — Surgery Subgroups and their ICD-9-CM procedures codes
| Surgery | ICD-9-CM procedure codes |
|---|---|
|
| |
| Amputation | 8400, 8401, 8402, 8403, 8404, 8405, 8406, 8407, 8408, |
| Upper limb | 8409 |
| Toe* | 8411, 8410, 8491 |
| Ankle and foot | 8412, 8413 |
| Knee and leg | 8414, 8415, 8416 |
| Above knee | 8417, 8418, 8419 |
|
| |
| BILI | 5209, 5212, 5222, 523, 524, 5251, 5252, 5253, 5259, |
| Pancreas | 526, 527, 5292, 5295, 5296, 5299 |
| Bile duct | 5131, 5132, 5133, 5134, 5135, 5136, 5137, 5139, 5141, 5142, 5143, 5149, 5151, 5159, 5161, 5162, 5163, 5169, 5171, 5172, 5179, 5181, 5182, 5183, 5189, 5191, 5192, 5193, 5194, 5195, 5199 |
| Open liver | 500, 5012, 5021, 5022, 5023, 5026, 5029, 503, 504, 5061, 5069 |
| Laparoscopic liver | 5014, 5025 |
|
| |
| Breast† | 8570, 8571, 8572, 8573, 8574, 8575, 8576, 8579 |
| Flap | |
| Mastectomy | 8541, 8542, 8543, 8544, 8545, 8546, 8547, 8548 |
| Expander/implant | 8553, 8554, 8595 |
| Breast conserving surgery | 8512, 8520, 8521, 8522, 8523 |
| Reduction/mastopexy/other | 8531, 8532, 8534, 8536, 856, 8550, 8555, 8593, 8533, 8535 |
|
| |
| Colon | 4571, 4572, 4573, 4574, 4575, 4576, 4579, 4582, 4583 |
| Open colectomy | |
| Laparoscopic colectomy | 1731, 1732, 1733, 1734, 1735, 1736, 1739, 4581 |
| Colostomy | 4610, 4611, 4613, 4614, 4643 |
| Other | 4503, 4526, 4541, 4549, 4552, 4603, 4604, 4675, 4676, 4592, 4593, 4594, 4595, 4694, 4652 |
|
| |
| Hernia | 5362, 5363, 5351, 5361, 5359, 5369 |
| Incisional/anterior abdominal | |
| Umbilical | 5341, 5349, 5342, 5343 |
| Inguinal/femoral | 1711, 1712, 1713, 1721, 1722, 1723, 1724, 5300, 5301, 5302, 5303, 5304, 5305, 5310, 5311, 5312, 5313, 5314, 5315, 5316, 5317, 5321, 5329, 5331, 5339 |
Amputation lower limb, NOS, 8410 and amputation, NOS 8491 (n=23 surgeries) were added to the amputation toe subgroup since it was the most common group
The following procedures were removed from the NHSN category list (breast implant removal [8594] and breast tissue expander removal [8596])
Appendix B — ICD-9-CM diagnosis codes used to identify SSI
| General SSI codes | 998.5 | Postoperative infection |
| 998.51 | Infected postoperative seroma | |
| 998.59 | Other postoperative infection | |
| Conditional*: | ||
| 729.4 | Fasciitis, unspecified | |
| 728.86 | Necrotizing fasciitis | |
| 728.0 | Infective myositis | |
| 040.0 | Gas gangrene | |
|
| ||
| Amputation | 711.0 | Pyogenic arthritis [0–9] |
| Conditional: | ||
| 997.62 | Amputation stump infection | |
| 730.0 | Acute osteomyelitis [0–9] | |
| 730.2 | Unspecified osteomyelitis [0–9] | |
|
| ||
| BILI, colon and hernia | 567.1 | Pneumococcal peritonitis |
| 567.2 | Other suppurative peritonitis | |
| 567.21 | Peritonitis (acute) generalized | |
| 567.29 | Other suppurative peritonitis. Subphrenic peritonitis | |
| 567.39 | Other retroperitoneal infections | |
| 567.9 | Unspecified peritonitis | |
| 567.22 | Peritoneal abscess. | |
| 567.38 | Other retroperitoneal abscess | |
| 569.5 | Abscess of intestine | |
|
| ||
| BILI and colon | 572.0 | Abscess of liver |
|
| ||
| Hernia or breast prosthesis | 996.69 | [Infection] due to other internal prosthetic device, implant, and graft. |
| Breast prosthesis | ||
Conditional infections were only counted as SSI if they were coded during a readmission and not the index hospitalization. However, index hospitalizations with conditional or non-conditional infections coded in the primary diagnosis variable or within 30 days prior were excluded.
Footnotes
Preliminary results of this work have been presented at the ID Week Meeting, Philadelphia, PA, October, 2014.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370(13):1198–208. doi: 10.1056/NEJMoa1306801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scott RD., II . The Direct Medical costs of Healthcare-Associated Infections in US Hospitals and the Benefits of Prevention. Centers for Disease Control and Prevention; 2009. www.cdc.gov/HAI/pdfs/hai/Scott_CostPaper.pdf. [Google Scholar]
- 3.Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039–46. doi: 10.1001/jamainternmed.2013.9763. [DOI] [PubMed] [Google Scholar]
- 4.National Healthcare Safety Network. Surgical Site Infection (SSI) Event. 2014 www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf.
- 5.Mu Y, Edwards JR, Horan TC, Berrios-Torres SI, Fridkin SK. Improving risk-adjusted measures of surgical site infection for the national healthcare safety network. Infect Control Hosp Epidemiol. 2011;32(10):970–86. doi: 10.1086/662016. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare and Medicaid Services. Hospital Compare Website. 2014 www.medicare.gov/hospitalcompare.
- 7.Centers for Disease Control and Prevention. Operational Guidance for Reporting Surgical Site Infection (SSI) Data to CDC’s NHSN for the Purpose of Fulfilling CMS’s Hospital Inpatient Quality Reporting (IQR) Program Requirements 2012. www.cdc.gov/nhsn/PDFs/FINAL-ACH-SSI-Guidance.pdf.
- 8.Centers for Medicare and Medicaid Services. CMS Proposals to Improve Quality of Care during Hospital Inpatient Stays. 2014 www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2014-Fact-sheets-items/2014-04-30-2.html.
- 9.Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37(10):783–805. doi: 10.1016/j.ajic.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP) Rockville, MD: 2014. HCUP Home. www.hcup-us.ahrq.gov/home.jsp. [Google Scholar]
- 11.Degrate L, Garancini M, Misani M, Poli S, Nobili C, Romano F, et al. Right colon, left colon, and rectal surgeries are not similar for surgical site infection development. Analysis of 277 elective and urgent colorectal resections. Int J Colorectal Dis. 2011;26(1):61–9. doi: 10.1007/s00384-010-1057-8. [DOI] [PubMed] [Google Scholar]
- 12.Tserenpuntsag B, Haley V, Van Antwerpen C, Doughty D, Gase KA, Hazamy PA, et al. Surgical site infection risk factors identified for patients undergoing colon procedures, New York State 2009–2010. Infect Control Hosp Epidemiol. 2014;35(8):1006–12. doi: 10.1086/677156. [DOI] [PubMed] [Google Scholar]
- 13.Hasanadka R, McLafferty RB, Moore CJ, Hood DB, Ramsey DE, Hodgson KJ. Predictors of wound complications following major amputation for critical limb ischemia. J Vasc Surg. 2011;54(5):1374–82. doi: 10.1016/j.jvs.2011.04.048. [DOI] [PubMed] [Google Scholar]
- 14.Olsen MA, Chu-Ongsakul S, Brandt KE, Dietz JR, Mayfield J, Fraser VJ. Hospital-associated costs due to surgical site infection after breast surgery. Arch Surg. 2008;143(1):53–60. doi: 10.1001/archsurg.2007.11. discussion 1. [DOI] [PubMed] [Google Scholar]
- 15.de Blacam C, Ogunleye AA, Momoh AO, Colakoglu S, Tobias AM, Sharma R, et al. High body mass index and smoking predict morbidity in breast cancer surgery: a multivariate analysis of 26,988 patients from the national surgical quality improvement program database. Ann Surg. 2012;255(3):551–5. doi: 10.1097/SLA.0b013e318246c294. [DOI] [PubMed] [Google Scholar]
- 16.Russo A, Elixhauser A, Steiner C, Wier L. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): 2006. Hospital-Based Ambulatory Surgery, 2007: Statistical Brief #86. [Google Scholar]
- 17.Nickel KB, Wallace AE, Warren DK, Mines D, Olsen MA. Using Claims Data to Perform Surveillance for Surgical Site Infection: The Devil Is in the Details. In: Battles JB, Cleeman JI, Kahn KK, Weinberg DA, editors. Advances in the Prevention and Control of Health Care-Associated Infections. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014. publication No. 14-0003. www.ahrq.gov/professionals/quality-patient-safety/patient-safety-resources/resources/advances-in-hai/hai-article13.html. [Google Scholar]
- 18.Ming DY, Chen LF, Miller BA, Anderson DJ. The impact of depth of infection and postdischarge surveillance on rate of surgical-site infections in a network of community hospitals. Infect Control Hosp Epidemiol. 2012;33(3):276–82. doi: 10.1086/664053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mannien J, Wille JC, Snoeren RL, van den Hof S. Impact of postdischarge surveillance on surgical site infection rates for several surgical procedures: results from the nosocomial surveillance network in The Netherlands. Infect Control Hosp Epidemiol. 2006;27(8):809–16. doi: 10.1086/506403. [DOI] [PubMed] [Google Scholar]
- 20.Kent P, McDonald M, Harris O, Mason T, Spelman D. Post-discharge surgical wound infection surveillance in a provincial hospital: follow-up rates, validity of data and review of the literature. ANZ J Surg. 2001;71(10):583–9. doi: 10.1046/j.1445-2197.2001.02215.x. [DOI] [PubMed] [Google Scholar]
- 21.Sands K, Vineyard G, Platt R. Surgical site infections occurring after hospital discharge. J Infect Dis. 1996;173(4):963–70. doi: 10.1093/infdis/173.4.963. [DOI] [PubMed] [Google Scholar]
- 22.Anderson DJ, Podgorny K, Berrios-Torres SI, Bratzler DW, Dellinger EP, Greene L, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(6):605–27. doi: 10.1086/676022. [DOI] [PMC free article] [PubMed] [Google Scholar]