Abstract
Objective
This report presents national estimates of the use of complementary health approaches among adults in the United States across three time points. Trends in the use of selected complementary health approaches are compared for 2002, 2007, and 2012, and differences by selected demographic characteristics are also examined.
Methods
Combined data from 88,962 adults aged 18 and over collected as part of the 2002, 2007, and 2012 National Health Interview Survey were analyzed for this report. Sample data were weighted to produce national estimates that are representative of the civilian noninstitutionalized U.S. adult population. Differences between percentages were evaluated using two-sided significance tests at the 0.05 level.
Results
Although the use of individual approaches varied across the three time points, nonvitamin, nonmineral dietary supplements remained the most popular complementary health approach used. The use of yoga, tai chi, and qi gong increased linearly across the three time points; among these three approaches, yoga accounted for approximately 80% of the prevalence. The use of any complementary health approach also differed by selected sociodemographic characteristics. The most notable observed differences in use were by age and Hispanic or Latino origin and race.
Keywords: prevalence, nonvitamin, nonmineral dietary supplements, yoga
Introduction
Complementary health approaches include an array of modalities and products with a history of use or origins outside of conventional Western medicine. Previous studies have shown that individuals often use complementary health approaches to improve health and wellbeing (1,2) or to relieve symptoms associated with chronic diseases or the side effects of conventional medicine (3,4). In the United States, most persons who use complementary health approaches do so to complement conventional care, rather than as a replacement (5–7). Using data from the 2002 National Health Interview Survey (NHIS), Nahin et al. (8) found that less than 5% of all U.S. adults used complementary health approaches but not conventional care. Previous research has also shown differences in the use of complementary health approaches by demographic characteristics such as sex and age (9,10). While knowledge of various types of complementary health approaches has increased among the U.S. population, the use of individual approaches has fluctuated across the years (11).
To better understand the patterns of use of complementary health approaches, this report describes the prevalence of adults using selected complementary health approaches and characterizes selected sociodemographic characteristics of such users. Because nonvitamin, nonmineral dietary supplements are the most commonly used complementary health approach among U.S. adults, after vitamins and prayer (12), individual supplements are also examined.
Methods
Data source
Analyses in this report were based on data collected from a combined sample of 88,962 adults aged 18 and over as part of the 2002, 2007, and 2012 Adult Alternative Medicine (ALT) supplements to NHIS, with demographic and other health information from the Household, Sample Adult Core, and Family Core components. NHIS is a nationally representative, cross-sectional household interview survey that is fielded continuously by the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics (NCHS), and it produces annual estimates of the health of the U.S. civilian noninstitutionalized population. Interviews are conducted in the home using a computer-assisted personal interview questionnaire, with telephone follow-up permitted if necessary. A detailed description of the NHIS sample design and the survey questionnaires for specific years are available elsewhere (13–15).
The Household and Family Core of NHIS collect health and sociodemographic information on each member of all families residing within a sampled household. Within each family, additional information is collected from one randomly selected adult (the “sample adult”) aged 18 and over with the Sample Adult Core.
In 2002, 2007, and 2012, the ALT supplement was administered to the sample adult respondent. Sponsored by the National Center for Complementary and Integrative Health [(NCCIH) formerly the National Center for Complementary and Alternative Medicine], part of the National Institutes of Health (NIH), the ALT supplement was implemented in order to provide a national data source on complementary medicine use. Since its inception in 2002, much of the content of the ALT supplement has remained constant, but modifications have been made in order to accommodate emerging scientific information, expert panel input, and societal shifts. Although the approaches included have varied slightly across survey years, the following were included in all three questionnaires: acupuncture; Ayurveda; biofeedback; chelation therapy; chiropractic care; energy healing therapy; hypnosis; massage; naturopathy; nonvitamin, nonmineral dietary supplements; homeopathic treatment; diet-based therapies; yoga; tai chi; qi gong; and meditation and other relaxation techniques.
Detailed differences between the three NHIS ALT supplement questionnaires can be found elsewhere (10,16). Briefly, use of a practitioner for chiropractic care was asked about in 2002. In 2007, participants were asked about use of a chiropractor or osteopath, however no real specificity was gained, as use of both types of manipulation were grouped together. This question was repeated in 2012, with the addition of follow-up questions asking whether a chiropractor, osteopath, or both were seen. Also in 2007, a list of named traditional healers replaced the more general question of seeing a practitioner of folk medicine, and questions about the use of movement therapies were added. In 2012, craniosacral therapy was added to the questionnaire.
In order to provide greater detail on meditation, in 2012 the type of meditation practiced was specified as mantra, mindfulness, or spiritual. Combining the prevalence of all three types of meditation may permit the comparison of the general practice of meditation across the three time points; however, these comparisons may be affected by the change in question format on the 2012 supplement. Based on cognitive testing and recommendations from a NCCIH think tank in 2012, information about the use of deep-breathing exercises was not asked as a stand-alone question but was collected as part of other approaches, including hypnosis, biofeedback, meditation, guided imagery, progressive relaxation, yoga, tai chi, and qi gong. While this change reduced the percentage of false-positive responses, direct comparison to previous survey years was lost. The list of nonvitamin, nonmineral dietary supplements was expanded from 35 in 2002, to 45 in 2007, and 119 in 2012. In addition, the 2002 questionnaire included a 12-month recall period for use of named nonvitamin, nonmineral dietary supplements, whereas the 2007 questionnaire included a 30-day recall period. As an improvement, the 2012 survey included both 30-day and 12-month recall periods for named nonvitamin, nonmineral dietary supplements. Comparisons of use in the past 30 days were consequently restricted to 2007 and 2012.
In order to compare overall use of complementary health approaches across all three time points, recalculation of approaches that changed across years was restricted to the narrowest definition on any one questionnaire. Individual approaches that were not directly comparable across all three time points were not included in trend analyses.
Measure of complementary health approach use
For this report, the definition of any complementary approach included the use of one or more of the following during the past 12 months: acupuncture; Ayurveda; biofeedback; chelation therapy; chiropractic care; energy healing therapy; special diets (including vegetarian and vegan, macrobiotic, Atkins, Pritikin, and Ornish); folk medicine or traditional healers; guided imagery; homeopathic treatment; hypnosis; naturopathy; nonvitamin, nonmineral dietary supplements; massage; meditation; progressive relaxation; qi gong; tai chi; or yoga. Due to the modifications in the three questionnaires as outlined above, only these approaches were asked about consistently across the three time points. Their use creates the most uniformed definition to assess trends.
Demographic variables
Demographic characteristics of U.S. adults presented in this report include sex, age group, Hispanic or Latino origin and race, educational attainment, poverty status, and health insurance coverage. All demographic characteristics were measured at the time of the interview.
Hispanic or Latino origin and race were determined from two separate questions, and individuals may have identified as Hispanic or Latino origin regardless of race. For conciseness, the text and tables in this report use shorter versions of the 1997 Office of Management and Budget terms for Hispanic origin and race. For example, the category “Non-Hispanic or non-Latino, black or African American, single race” is referred to as “non-Hispanic black.” Due to insufficient sample size, “non-Hispanic Asian,” “non-Hispanic Other Pacific Islander,” and “non-Hispanic American Indian Alaska Native” were combined to form the category “non-Hispanic other races.”
Educational attainment was collected from all adults aged 18 and over and was categorized in reference to the highest degree completed at the date of the interview. Household income was also collected, and percentage of poverty level was based on a comparison of each respondent’s household income with the poverty thresholds for the family size, as defined by the U.S. Census Bureau. Imputations for income were not used.
Health insurance was categorized into three mutually exclusive categories: private, public, and uninsured. Persons with more than one type of health insurance were assigned to their primary insurance category in the following hierarchy: private, public, and uninsured. A more detailed description of these demographic variables can be found in Technical Notes.
Statistical analyses
Estimates in this report were calculated using the sample adult sampling weights and are representative of the noninstitutionalized population of U.S. adults aged 18 and over. Data weighting procedures are described in more detail elsewhere (17,18). Point estimates, and estimates of their variances, were calculated using SAS-callable SUDAAN version 11.0.0 (19), a software package that accounts for the complex sample design of NHIS. Estimates were age-adjusted using the projected 2000 U.S. population as the standard population in order to compare various demographic subgroups that have different age distributions (20,21). Unless otherwise specified, the denominator used was all adults aged 18 and over. Calculations excluded persons with unknown information.
Estimates were compared using two-sided t tests at the 0.05 level and assuming independence. Terms such as “greater than” and “less than” indicate a statistically significant difference. Terms such as “not significantly different” or “no difference” indicate that there were no statistically detectable differences between the estimates being compared. Reliability of estimates was evaluated using the relative standard error (RSE), which is the standard error divided by the point estimate. Estimates with RSEs greater than 30% and less than or equal to 50% are considered unreliable and are preceded by a dagger symbol (†) in Table 1.
Table 1.
Trends in the use of selected complementary health approaches during the past 12 months, by type of approach: United States, 2002, 2007, and 2012
| Complementary health approach | 2002
|
2007
|
2012
|
Test for trend
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Percentage point change | Trend | |||||||||
| Number (in thousands) |
Age-adjusted percent1 (standard error) |
Number (in thousands) |
Age-adjusted percent1 (standard error) |
Number (in thousands) |
Age-adjusted percent1 (standard error) |
2002–2007 | 2007–2012 | 2002–2012 | ||
| Nonvitamin, nonmineral dietary supplements | 38,183 | 18.9 (0.28) | 38,797 | 17.7 (0.37) | 40,579 | 17.7 (0.37) | †† | 0.0 | †† | †† |
| Deep-breathing exercises2 | 23,457 | 11.6 (0.24) | 27,794 | 12.7 (0.30) | 24,218 | 10.9 (0.26) | §1.1 | †† | †† | †† |
| Yoga, tai chi, and qi gong | 11,766 | 5.8 (0.17) | 14,436 | 6.7 (0.22) | 22,281 | 10.1 (0.25) | 0.9 | §2.5 | §3.4 | * Linear |
| Chiropractic or osteopathic manipulation3 | 15,226 | 7.5 (0.19) | 18,740 | 8.6 (0.27) | 19,369 | 8.4 (0.22) | †† | −0.2 | †† | †† |
| Meditation4 | 15,336 | 7.6 (0.20) | 20,541 | 9.4 (0.27) | 17,948 | 8.0 (0.21) | §1.8 | †† | †† | †† |
| Massage therapy | 10,052 | 5.0 (0.16) | 18,068 | 8.3 (0.23) | 15,411 | 6.9 (0.15) | §3.3 | §−1.6 | §1.9 | * Quadratic |
| Special diets5 | 6,765 | 3.3 (0.12) | 6,040 | 2.8 (0.14) | 6,853 | 3.0 (0.13) | 0.1 | §−0.6 | −0.5 | ** Quadratic |
| Homeopathic treatment6 | 3,433 | 1.7 (0.09) | 3,909 | 1.8 (0.11) | 5,046 | 2.2 (0.11) | 0.1 | 0.4 | 0.5 | *** Linear |
| Progressive relaxation | 6,185 | 3.0 (0.12) | 6,454 | 2.9 (0.15) | 4,766 | 2.1 (0.10) | −0.1 | §−0.8 | §−0.9 | * Linear |
| Guided imagery | 4,194 | 2.1 (0.10) | 4,866 | 2.2 (0.16) | 3,846 | 1.7 (0.10) | 0.1 | −0.5 | −0.4 | None |
| Acupuncture | 2,136 | 1.1 (0.07) | 3,141 | 1.4 (0.10) | 3,484 | 1.5 (0.08) | 0.3 | 0.1 | 0.4 | *** Linear |
| Energy healing therapy | 1,080 | 0.5 (0.05) | 1,216 | 0.5 (0.06) | 1,077 | 0.5 (0.05) | 0.0 | 0.0 | 0.0 | None |
| Naturopathy | 498 | 0.2 (0.03) | 729 | 0.3 (0.04) | 957 | 0.4 (0.04) | 0.1 | 0.1 | 0.2 | ** Linear |
| Hypnosis | 505 | 0.2 (0.03) | 561 | 0.2 (0.04) | 347 | 0.1 (0.03) | 0.0 | −0.1 | −0.1 | None |
| Biofeedback | 278 | 0.1 (0.02) | 362 | 0.2 (0.04) | 281 | 0.1 (0.02) | 0.1 | −0.1 | 0.0 | None |
| Ayurveda | 154 | †0.1 (0.02) | 214 | †0.1 (0.03) | 241 | 0.1 (0.02) | 0.0 | 0.0 | 0.0 | None |
Estimates are considered unreliable. Data have a relative standard error greater than 30% and less than or equal to 50% and should be used with caution.
Direct comparisons are not available.
Difference between both years is statistically significant at p < 0.05.
0.0 Quantity more than zero but less than 0.05.
Significance of the chi-squared statistics is < 0.001.
Significance of the chi-squared statistics is < 0.01.
Significance of the chi-squared statistics is < 0.05.
The denominator used in the calculation of percentages was all sample adults.
In 2012, deep-breathing exercises included deep-breathing exercises as part of hypnosis; biofeedback; Mantra meditation (including Transcendental Meditation, Relaxation Response, and Clinically Standardized Meditation); mindfulness meditation (including Vipassana, Zen Buddhist meditation, mindfulness-based stress reduction, and mindfulness-based cognitive therapy); spiritual meditation (including centering prayer and contemplative meditation); guided imagery; progressive relaxation; yoga; tai chi; or qi gong. In 2002 and 2007, the use of deep-breathing exercises was asked broadly and not if used as part of other complementary health approaches. No trend analyses were conducted on the use of deep-breathing exercises.
In 2002, the use of chiropractic care was asked broadly, and osteopathic approach was not specified on the survey. No trend analyses were conducted on the use of chiropractic or osteopathic manipulation.
In 2012, meditation included Mantra meditation (including Transcendental Meditation, Relaxation Response, and Clinically Standardized Meditation); mindfulness meditation (including Vipassana, Zen Buddhist meditation, mindfulness-based stress reduction, and mindfulness-based cognitive therapy); spiritual meditation (including centering prayer and contemplative meditation); and meditation used as a part of other practices (including yoga, tai chi, and qi gong). In 2002 and 2007, the use of meditation was asked broadly and not if practiced as part of other complementary health approaches.
Respondents used one or more named special diets for 2 weeks or more in the past 12 months. Special diets included vegetarian (including vegan), macrobiotic, Atkins, Pritikin, and Ornish diets.
No distinction was made between persons who sought treatment from a homeopathic practitioner and those who self-medicated.
NOTES: Estimates were age-adjusted using the projected 2000 U.S. population as the standard population and using four age groups: 18–24, 25–44, 45–64, and 65 and over. The denominators for statistics shown exclude persons with unknown complementary and alternative medicine information. Estimates are based on household interviews of a sample of the civilian noninstitutionalized population.
SOURCE: CDC/NCHS, National Health Interview Survey, 2002, 2007, and 2012.
The SAS procedure PROC SURVEYLOGISTIC (22) with orthogonal polynomial trend contrasts was used to perform weighted linear or quadratic regressions of the annual design-adjusted rates for each variable of interest. This procedure incorporates the complex survey sample design of NHIS, including stratification, clustering, and unequal weighting. This model tests the parallel-lines assumption by simultaneously testing the equality of separate slope parameters for each variable. The variances of the regression parameters were computed using the Taylor series (linearization) method to estimate the sampling errors of estimators based on the complex sample design. This method will be used for all trend analyses in this report series.
Strengths and limitations of data
A major strength of these analyses is that the data are from a nationally representative sample of U.S. adults, allowing for population estimates. The large sample size allows for estimation of the use of complementary health approaches by a wide variety of population subgroups and other self-reported health characteristics collected in NHIS.
The data in this report also have some limitations. NHIS is a cross-sectional survey, and causal associations cannot be made. Responses are dependent on participants’ recall of complementary health approaches that they used in the past 12 months, as well as their willingness to report their use accurately. Additionally, in an effort to improve the validity of the questions asked and to meet NCCIH’s research priorities, revisions to the content and structure of some questions preclude direct comparison across years, limiting analysis of trends to approaches that were asked about consistently on each questionnaire.
Results
Adult use of selected complementary health approaches
Complementary health approaches encompass a wide range of modalities. Table 1 presents the prevalence of and trends in the use of commonly used complementary health approaches in 2002, 2007, and 2012. Although there was consistency in the types of approaches that were most popular, there was variation in the trends across time points.
Nonvitamin, nonmineral dietary supplements were the most commonly used complementary health approach at each of the three time points: 18.9% in 2002 and unchanged from 2007 to 2012 (17.7%).
Whether used independently or as a part of other approaches, deep-breathing exercises were the second most commonly used complementary health approach in 2002 (11.6%), 2007 (12.7%), and 2012 (10.9%).
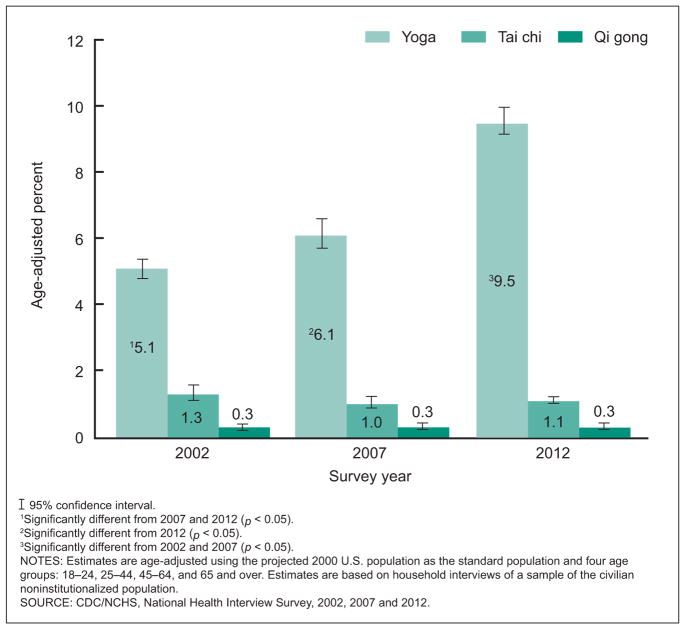
The use of yoga, tai chi, and qi gong increased linearly over the three time points, beginning at 5.8% in 2002, 6.7% in 2007, and 10.1% in 2012. Yoga was the most commonly used of these three approaches at all three time points (Figure 1).
There was a small but significant linear increase in the use of homeopathic treatment, acupuncture, and naturopathy.
The use of chiropractic care or chiropractic and osteopathic manipulation was the fourth most commonly used approach in 2002 (7.5%), 2007 (8.6%), and 2012 (8.4%).
Meditation was used by 7.6% of adults in 2002, 9.4% in 2007, and 8.0% in 2012, keeping it among the top five most commonly used approaches for each time point.
Ayurveda, biofeedback, guided imagery hypnosis, and energy healing therapy had a consistently low prevalence and had no significant changes across the three time points.
Figure 1.
Use of yoga, tai chi, and qi gong among adults in the past 12 months: United States, 2002, 2007, and 2012
Overall use of complementary health approaches, by selected characteristics
Among U.S. adults aged 18 and over in 2002, 2007, and 2012, the percentage who used any complementary health approach in the past 12 months ranged from 32.3% in 2002 to 35.5% in 2007 and was most recently 33.2% in 2012. Table 2 highlights trends in the use of complementary health approaches by sex, age group, Hispanic or Latino origin and race, education, poverty status, and health insurance coverage.
Table 2.
Trends in the use of complementary health approaches among adults aged 18 and over, by selected characteristics: United States, 2002, 2007, and 2012
| Selected characteristic | 2002
|
2007
|
2012
|
Percentage point change
|
Trend | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number (in thousands) | Age-adjusted percent1 (standard error) | Number (in thousands) | Age-adjusted percent1 (standard error) | Number (in thousands) | Age-adjusted percent1 (standard error) | 2002–2007 | 2007–2012 | 2002–2012 | ||
| Total2 | 65,169 | 32.3 (0.37) | 77,032 | 35.5 (0.48) | 76,222 | 33.2 (0.42) | †3.2 | †−2.3 | 0.9 | * Quadratic |
| Sex | ||||||||||
| Men | 27,115 | 27.9 (0.49) | 32,884 | 31.4 (0.61) | 31,818 | 28.9 (0.54) | †3.5 | †−2.5 | 1.0 | ** Quadratic |
| Women | 38,053 | 36.4 (0.48) | 44,148 | 39.4 (0.61) | 44,404 | 37.4 (0.54) | †3.0 | −2.0 | 1.0 | * Quadratic |
| Age group (years) | ||||||||||
| 18–44 | 34,842 | 33.0 (0.48) | 36,705 | 34.2 (0.63) | 34,600 | 32.2 (0.57) | 1.2 | −2.0 | −0.8 | * Linear |
| 45–64 | 23,041 | 36.5 (0.64) | 29,507 | 40.1 (0.80) | 29,048 | 36.8 (0.63) | †3.6 | †−3.3 | 0.3 | * Quadratic |
| 65 and over. | 7,286 | 22.7 (0.64) | 10,820 | 31.1 (0.92) | 11,789 | 29.4 (0.73) | †8.4 | −1.5 | †6.9 | * Quadratic |
| Hispanic or Latino origin and race | ||||||||||
| Hispanic | 5,626 | 26.4 (0.80) | 6,162 | 21.6 (0.91) | 7,525 | 22.0 (0.76) | †−4.8 | 0.4 | †−4.4 | * Quadratic |
| Non-Hispanic white | 50,219 | 34.4 (0.44) | 59,814 | 40.2 (0.60) | 57,008 | 37.9 (0.53) | †5.8 | †−2.3 | †3.5 | *** Quadratic |
| Non-Hispanic black | 5,181 | 22.9 (0.66) | 5,688 | 22.9 (0.90) | 4,957 | 19.3 (0.75) | 0.0 | †−3.6 | †−3.6 | * Linear |
| Non-Hispanic other3 | 4,142 | 41.5 (1.59) | 5,368 | 39.6 (1.66) | 5,946 | 37.3 (1.21) | −1.9 | −2.3 | −4.2 | *** Linear |
| Education | ||||||||||
| Less than high school diploma | 5,918 | 18.6 (0.68) | 6,440 | 18.9 (0.85) | 4,980 | 15.6 (0.72) | −0.3 | −2.0 | †−3.0 | *** Quadratic |
| High school diploma or GED4 | 15,777 | 26.6 (0.53) | 17,457 | 28.1 (0.85) | 14,744 | 24.4 (0.64) | −1.5 | †−3.7 | †−2.2 | *** Quadratic |
| Some college education | 14,244 | 35.6 (0.75) | 23,189 | 41.3 (0.80) | 16,762 | 36.5 (0.82) | †5.7 | †−4.8 | 0.9 | * Quadratic |
| College degree or higher | 28,953 | 42.1 (0.67) | 29,743 | 46.7 (0.82) | 39,586 | 42.6 (0.64) | †4.6 | †−4.1 | 0.5 | * Quadratic |
| Poverty status5 | ||||||||||
| Poor | 4,127 | 25.1 (0.99) | 6,107 | 26.6 (1.02) | 6,315 | 20.6 (0.76) | 1.5 | †−6.0 | †−4.5 | *** Quadratic |
| Near-poor | 6,961 | 27.7 (0.79) | 8,380 | 27.9 (0.98) | 9,283 | 25.5 (0.79) | 0.2 | −2.4 | −2.2 | *** Linear |
| Not-poor | 41,962 | 36.8 (0.48) | 55,953 | 40.3 (0.64) | 55,490 | 38.4 (0.53) | †3.5 | −1.9 | 1.6 | *** Quadratic |
| Health insurance6 | ||||||||||
| Private | 49,839 | 34.6 (0.42) | 56,900 | 39.0 (0.59) | 54,389 | 38.0 (0.50) | †4.4 | −1.0 | †3.4 | * Quadratic |
| Public | 6,402 | 25.8 (0.92) | 9,401 | 27.0 (1.00) | 11,387 | 24.8 (0.84) | 1.2 | −2.2 | −1.0 | ** Quadratic |
| Uninsured | 8,730 | 28.4 (1.21) | 10,382 | 27.8 (1.66) | 9,505 | 22.9 (1.09) | −0.6 | †−4.9 | †−5.5 | *** Quadratic |
Difference between both years is statistically significant at p < 0.05.
0.0 Quantity more than zero but less than 0.05.
Significance of the chi-squared statistics is < 0.001.
Significance of the chi-squared statistics is < 0.01.
Significance of the chi-squared statistics is < 0.05.
The denominator used in the calculation of percentages was all sample adults.
Total was defined by a “yes” response to use of one or more of the following in the past 12 months: acupuncture; Ayurveda; biofeedback; chelation therapy; chiropractic care; energy healing therapy or Reiki; vegetarian and vegan, macrobiotic, Atkins, Pritikin, and Ornish diets; folk medicine; guided imagery; homeopathic treatment; hypnosis; naturopathy; nonvitamin, nonmineral, dietary supplements; massage; meditation; progressive relaxation; qi gong; tai chi; or yoga. The use of prayer for health reasons, megavitamin supplements, and special diets not listed, was not included. Respondents may have reported using more than one type of approach.
Non-Hispanic other and persons of multiple races is a very broad and varied category of persons from a variety of races and ethnicities. This group may be more diverse than the other racial and ethnic groups.
GED is General Educational Development high school equivalency diploma.
Based on family income and family size using the U.S. Census Bureau’s poverty thresholds for the previous calendar year. Poor persons had a total annual income below the poverty threshold; near-poor persons had incomes of 100% to less than 200% of the poverty threshold; not-poor persons had incomes that were 200% of the poverty threshold or greater.
Based on a hierarchy of mutually exclusive categories. Persons with more than one type of health insurance were assigned to the first appropriate category in the hierarchy. “Uninsured” includes persons who had no coverage and those who had only Indian Health Service coverage or had only a private plan that paid for one type of service such as accidents or dental care.
NOTES: All estimates except age groups were age-adjusted using the projected 2000 U.S. population as the standard population and using four age groups: 18–24, 25–44, 45–64, and 65 and over. Estimates are based on household interviews of a sample of the civilian noninstitutionalized population.
SOURCE: CDC/NCHS, National Health Interview Survey, 2002, 2007, and 2012.
There was a quadratic change in the overall use of any complementary health approach across the three time points with a peak of 35.5% in 2007.
There was a significant quadratic trend in the use of complementary health approaches among both men and women across the three time points. The use of any complementary health approach increased by 3.5 percentage points among men from 2002 to 2007 but decreased by 2.5 percentage points from 2007 to 2012. There was a 3.0 percentage point increase in use among women from 2002 to 2007; however, there were no further significant differences between other time points.
There were no significant changes in the prevalence of any complementary health approach between each time point for adults aged 18–44 (33.0% in 2002, 34.2% in 2007, and 32.2% in 2012). There was an increase from 36.5% in 2002 to 40.1% in 2007, and then a decrease to 36.8% in 2012 among adults aged 45–64. The use of any complementary health approach also increased among adults aged 65 and over from 2002 to 2007, from 22.7% to 31.1%; but no significant change was observed between 2007 and 2012 (31.1% to 29.4%).
From 2002 to 2012, there was a significant quadratic trend for Hispanic adults (26.4% in 2002, 21.6% in 2007, and 22.0% in 2012) and non-Hispanic white adults (34.4% in 2002, 40.2% in 2007, and 37.9% in 2012). However, a significant linear trend was observed for non-Hispanic black adults (22.9% in 2002 and 2007 and 19.3% in 2012) and non-Hispanic other adults (41.5% in 2002, 39.6% in 2007, and 37.3% in 2012).
There were significant quadratic trends in the use of complementary approaches among adults with less than a high school diploma (18.6% in 2002, 18.9% in 2007, and 15.6% in 2012); adults with a high school diploma or GED (General Educational Development high school equivalency diploma) (26.6% in 2002, 28.1% in 2007, and 24.4% in 2012); adults with some college education (35.6% in 2002, 41.3% in 2007, and 36.5% in 2012); and those with a college degree or higher (42.1% in 2002, 46.7% in 2007, and 42.6% in 2012).
There was a significant quadratic trend in the use of complementary approaches among poor adults (25.1% in 2002, 26.6% in 2007, and 20.6% in 2012) and not-poor adults (36.8% in 2002, 40.3% in 2007, and 38.4% in 2012); and a linear trend among near-poor adults (27.7% in 2002, 27.9% in 2007, and 25.5% in 2012).
There was a significant quadratic trend in the use of any complementary health approach among all insured groups: those with private insurance (34.6% in 2002, 39.0% in 2007, and 38.0% in 2012) and public coverage (25.8% in 2002, 27.0% in 2007, and 24.8% in 2012) as well as the uninsured (28.4% in 2002, 27.8% in 2007, and 22.9% in 2012).
Use of selected nonvitamin, nonmineral dietary supplements in 2007 and 2012
Although there was no change in the percentage of overall use of nonvitamin, nonmineral dietary supplements among adults from 2007 to 2012, there was variability in the use of specific types of supplements. Table 3 presents the prevalence of selected nonvitamin, nonmineral dietary supplements used in the past 30 days. Estimates are limited to 2007 and 2012 because a 30-day supplement recall was not included in the 2002 questionnaire.
Table 3.
Adults aged 18 and over who used selected types of nonvitamin, nonmineral dietary supplements during the past 30 days: United States, 2007 and 2012
| Dietary supplements1 | 2007
|
2012
|
p value | ||
|---|---|---|---|---|---|
| Number (in thousands) | Age-adjusted percent2 (standard error) | Number (in thousands) | Age-adjusted percent2 (standard error) | ||
| Fish oil3 | 10,923 | 4.8 (0.17) | 18,848 | 7.8 (0.22) | † |
| Glucosamine or chondroitin | 7,236 | 3.2 (0.14) | 6,450 | 2.6 (0.11) | † |
| Probiotics or prebiotics | 865 | 0.4 (0.05) | 3,857 | 1.6 (0.09) | † |
| Melatonin | 1,296 | 0.6 (0.06) | 3,065 | 1.3 (0.08) | † |
| Coenzyme Q–10 (CoQ10) | 2,691 | 1.2 (0.08) | 3,265 | 1.3 (0.08) | †† |
| Echinacea | 4,848 | 2.2 (0.12) | 2,261 | 0.9 (0.06) | † |
| Cranberry (pills or capsules) | 1,560 | 0.7 (0.06) | 1,934 | 0.8 (0.06) | †† |
| Garlic supplements | 3,278 | 1.4 (0.09) | 1,927 | 0.8 (0.06) | † |
| Ginseng | 3,345 | 1.5 (0.10) | 1,752 | 0.7 (0.06) | † |
| Ginkgo biloba | 2,977 | 1.3 (0.10) | 1,619 | 0.7 (0.06) | † |
| Green tea pills (not brewed tea) or EGCG (pills)4 | 1,528 | 0.7 (0.06) | 1,503 | 0.6 (0.05) | †† |
| Combination herb pill | 3,446 | 1.5 (0.10) | 1,463 | 0.6 (0.05) | † |
| MSM (methylsulfonylmethane) | 1,312 | 0.6 (0.05) | 1,051 | 0.4 (0.04) | † |
| Milk thistle (silymarin) | 1,001 | 0.4 (0.05) | 988 | 0.4 (0.04) | †† |
| Saw palmetto | 1,682 | 0.7 (0.07) | 988 | 0.4 (0.04) | † |
| Valerian | 877 | 0.4 (0.05) | 801 | 0.3 (0.04) | †† |
p < 0.05.
Difference is not statistically significant.
Respondents may have used more than one nonvitamin, nonmineral dietary supplement.
The denominator used in the calculation of percentages was all sample adults.
In 2007, fish oil was described as fish oil or omega 3 or DHA fatty acid. In 2012, fish oil was described as fish oil or omega 3 or DHA or EPA fatty acid.
EGCG is epigallocatechin gallate.
NOTES: Estimates were age-adjusted using the projected 2000 U.S. population as the standard population and using four age groups: 18–24, 25–44, 45–64, and 65 and over. Estimates are based on household interviews of a sample of the civilian noninstitutionalized population.
SOURCE: CDC/NCHS, National Health Interview Survey, 2007 and 2012.
Fish oil supplements and glucosamine, chondroitin, or a combination supplement were consistently the two most common nonvitamin, nonmineral dietary supplements used in the past 30 days in 2007 and 2012.
Fish oil use among adults increased from 4.8% in 2007 to 7.8% in 2012. Probiotic or prebiotic use was four times as high in 2012 as it was in 2007 (1.6% and 0.4%, respectively), rising to the third most commonly used nonvitamin, nonmineral dietary supplement in 2012.
The use of melatonin more than doubled in use from 0.6% in 2007 to 1.3% in 2012.
There was a decrease in use of glucosamine, chondroitin, or a combination pill from 2007 to 2012, from 3.2% to 2.6%.
From 2007 to 2012, there was also a significant decline in the use of echinacea (1.3 percentage points), garlic (0.6), ginseng (0.8), ginkgo biloba (0.6), methylsulfonylmethane (MSM) (0.2), and saw palmetto (0.3).
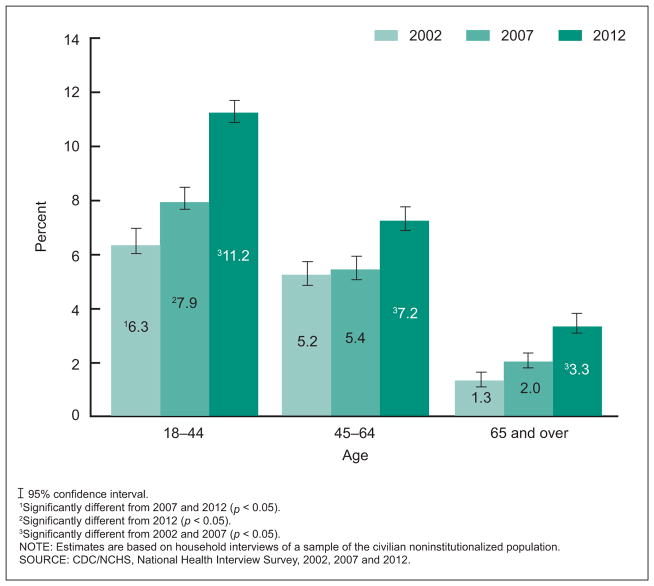
Use of yoga by age group and year
The most notable differences in the use of any complementary health approach were seen by age group. To further understand age differences, Figure 2 presents one of the most commonly used approaches, yoga, by age group for 2002, 2007, and 2012.
Figure 2.
Use of yoga among adults in the past 12 months, by age group: United States, 2002, 2007, and 2012
While all age groups showed an increased use of yoga over the 10-year period, the use of yoga decreased with age (from 6.3% in 2002 to 11.2% in 2012 among those aged 18–44; 5.2% in 2002 to 7.2% in 2012 among those 45–64; and 1.3% in 2002 to 3.3% in 2012 among those 65 and over) (Figure 2).
Adults aged 18–44 had the highest prevalence of use across all three time points. The increase in use of yoga among this group from 2007 to 2012 (3.3 percentage points) was more than twice the increase in use between 2002 and 2007 (1.6 percentage points).
There were no significant differences observed in the use of yoga between 2002 and 2007 among adults aged 45–64 and those aged 65 and over; however, there was an increase in the use of yoga between 2007 and 2012 for both age groups (1.8 and 1.3 percentage points, respectively).
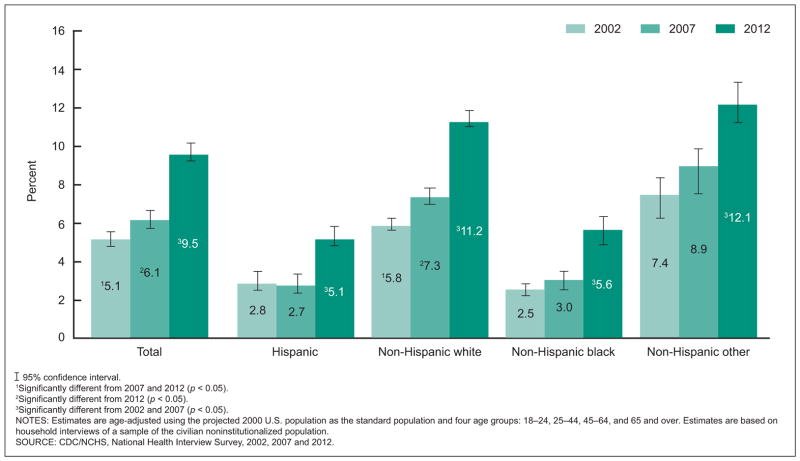
Use of yoga by Hispanic or Latino origin and race and year
The use of yoga varied by Hispanic or Latino origin and race over the three time points; Figure 3 presents these changes.
Figure 3.
Use of yoga among adults in the past 12 months, by Hispanic origin and race: United States, 2002, 2007, and 2012
There was no significant change in the use of yoga among Hispanic adults between 2002 (2.8%) and 2007 (2.7%); however, the use of yoga among this group almost doubled between 2007 and 2012 (5.1%). Non-Hispanic black adults demonstrated a similar pattern of use across time (2.5% in 2002, 3.0% in 2007, and 5.6% in 2012) (Figure 3).
Non-Hispanic white adults demonstrated a consistent increase in the use of yoga across the three time points, from 5.8% in 2002 to 11.2% in 2012.
While there was no significant difference in the use of yoga among non-Hispanic other adults from 2002 (7.4%) to 2007 (8.9%), their use increased by almost 30% from 2002 to 2012 (12.1%).
Discussion
In response to queries from researchers, practitioners, and users of complementary health approaches, this report presents data from the 2002, 2007, and 2012 NHIS on the use of complementary health approaches among civilian noninstitutionalized U.S. adults aged 18 and over. It focuses on the prevalence and trends of selected complementary health approaches used in the past 12 months, selected characteristics of adults who used any complementary health approach, and the use of selected nonvitamin, nonmineral dietary supplements in the past 30 days. The objective was to provide the most current estimates of a wide range of complementary health approaches that are used by U.S. adults, to characterize user demographics, and to monitor changes over the three time points.
This report is one of the first to estimate the prevalence of complementary health approaches among U.S. adults using the 2012 NHIS. Overall, 34% of adults used any complementary health approach in 2012. Despite the lack of a consistent definition as to which approaches are included in the measure of complementary health approaches, estimates of the overall use of any complementary health approach presented in this study are consistent with previous research (9,10,23–25). Estimates for the use of individual approaches and demographic characteristics are also consistent with previous reports (9,10). Because a narrower definition was used in this report, it is not surprising that the revised prevalence estimates for 2002 and 2007 were lower than those published previously: 32.3% compared with 35.0% for 2002 (9) and 35.5% compared with 38.0% for 2007 (10). Without taking into consideration which complementary health approaches are included in the definition of any complementary health approach, comparison of the prevalence may be misleading across studies. This confusion with definitions has led to an effort to establish an internationally accepted standard for what approaches should be included in prevalence surveys of complementary health approaches (26).
Previous research using NHIS and other surveys found that the use of any complementary health approach has been increasing, and some reports speculated that this increasing trend would continue (23–25). However, results from this report show that while the overall use of complementary health approaches displayed a slight increase between 2002 and 2007, in 2012 use among U.S. adults was not significantly different from 2002. Distinct from the trend in use of any complementary health approaches, there have been variations in the magnitude and direction of the trends of individual approaches. Nonvitamin, nonmineral dietary supplements; deep-breathing exercises; yoga, tai chi, and qi gong; and chiropractic or osteopathic manipulation were consistently popular approaches over the three time points, regardless of changes to some questions across survey time points. Among these approaches, yoga, tai chi, and qi gong showed an increase, and deep-breathing exercises and chiropractic or osteopathic manipulation had no significant change between 2002 and 2012. Although some questions have been changed every survey year, the estimates do not reflect overly abundant increases or decreases in any one approach.
In addition to comparing the prevalence in use between time points, further examination of selected approaches revealed significant differences among age and Hispanic or Latino origin and race groups. The only group of approaches to significantly increase each year was the use of yoga, tai chi, or qi gong. Given that all three often incorporate low-intensity forms of exercise that can be scaled to an individual’s abilities, the increased popularity across all ages and Hispanic origin and race groups was expected. Offered in a variety of settings ranging from self-practice to specialized studios, the yoga industry has experienced growth in recent years, making it more accessible to adults of all ages (27).
Previous research has noted variations in use of complementary health approaches by race and Hispanic origin. This report found that Hispanic and non-Hispanic black adults had a decreasing pattern of use of any complementary health approach while non-Hispanic white adults had an increasing pattern of use. Other studies have examined how length of stay in the United States and race and ethnicity may help explain differences in the use of complementary health approaches (28).
The health benefits of nonvitamin, nonmineral dietary supplements are unclear. Despite this, such supplements were consistently the most used complementary health approach across the three time points. Overall trends in the prevalence of use of any nonvitamin, nonmineral supplements need to be qualified by the observations of a significant increase in the use of certain individual supplements: fish oil; probiotics or prebiotics; and melatonin; and decreases in the use of glucosamine, chondroitin, or both; echinacea; garlic; ginseng; ginkgo biloba; MSM; and saw palmetto (Table 3).
Health advocates and physicians have been recommending fish oil supplementation (29,30), although its benefits are not well understood. Research has suggested that fish oil can reduce blood pressure (31) and inflammation (32), increase brain blood flow (33), and provide structural strength for neurons (34,35). The data for this report showed a 60% increase in the 30-day prevalence of using fish oils between 2007 and 2012. The use of other supplements such as melatonin and probiotics or prebiotics also increased. Consistent with the report’s findings, market research indicates a significant increase in sales of these products over the past 5 years (36,37).
Although beyond the scope of this report, the reasons for using complementary health approaches may help explain the differences in the trends among demographic groups. The NHIS ALT supplements were designed to help guide the NIH research agenda, and they have evolved to adapt to NCCIH’s evolution in priorities from disease treatment to a focus on symptom management and the promotion of optimal health (38,39). These supplements provide the most comprehensive source of information on complementary health approaches used by U.S. adults. Building upon previous reports, this report is helpful for monitoring changing patterns in complementary health approach use. Additionally, this report shows that looking exclusively at the overall use of complementary health approaches can miss meaningful differences in the use of individual approaches.
While substantial revisions to the content and structure of the ALT supplements since 2002 (16) preclude direct comparisons of some approaches across all three time points, it is still possible to compare the prevalence of some of these approaches between two consecutive supplements. The prevalence rates of complementary health approaches will differ by survey year and by publication without using uniformed definitions. As such, data users are advised to carefully define the broad term of complementary health approaches and recalculate specific therapies, where possible, to facilitate direct comparisons.
Contributor Information
Tainya C. Clarke, National Center for Health Statistics
Lindsey I. Black, National Center for Health Statistics
Barbara J. Stussman, National Institutes of Health
Patricia M. Barnes, National Center for Health Statistics
Richard L. Nahin, National Institutes of Health
References
- 1.McCaffrey AM, Pugh GF, O’Connor BB. Understanding patient preference for integrative medical care: Results from patient focus groups. J Gen Intern Med. 2007;22(11):1500–5. doi: 10.1007/s11606-007-0302-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greene AM, Walsh EG, Sirois FM, McCaffrey A. Perceived benefits of complementary and alternative medicine: A whole systems research perspective. Open Comp Med J. 2009;1:35–45. [Google Scholar]
- 3.Nahin RL, Byrd-Clark D, Stussman BJ, Kalyanaraman N. Disease severity is associated with the use of complementary medicine to treat or manage type-2 diabetes: Data from the 2002 and 2007 National Health Interview Survey. BMC Complement Altern Med. 2012;12:193. doi: 10.1186/1472-6882-12-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lo CB, Desmond RA, Meleth S. Inclusion of complementary and alternative medicine in US state comprehensive cancer control plans: Baseline data. J Cancer Educ. 2009;24(4):249–53. doi: 10.1080/08858190902972897. [DOI] [PubMed] [Google Scholar]
- 5.Astin JA. Why patients use alternative medicine: Results of a national study. JAMA. 1998;279(19):1548–53. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 6.Druss BG, Rosenheck RA. Association between use of unconventional therapies and conventional medical services. JAMA. 1999;282(7):651–6. doi: 10.1001/jama.282.7.651. [DOI] [PubMed] [Google Scholar]
- 7.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA. 1998;280(18):1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 8.Nahin RL, Dahlhamer JM, Stussman BJ. Health need and the use of alternative medicine among adults who do not use conventional medicine. BMC Health Serv Res. 2010;29(10):220. doi: 10.1186/1472-6963-10-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;(343):1–19. [PubMed] [Google Scholar]
- 10.Barnes PM, Bloom B, Nahin RL. National health statistics reports; no 12. Hyattsville, MD: National Center for Health Statistics; 2008. Complementary and alternative medicine use among adults and children: United States, 2007. [PubMed] [Google Scholar]
- 11.Sohn PM, Loveland Cook CA. Nurse practitioner knowledge of complementary alternative health care: Foundation for practice. J Adv Nurs. 2002;39(1):9–16. doi: 10.1046/j.1365-2648.2002.02238.x. [DOI] [PubMed] [Google Scholar]
- 12.CDC. Percentage of adults who used selected complementary health approaches in the preceding 12 months, by metropolitan status of residence—National Health Interview Survey, United States, 2012. MMWR. 2014;63(36):802. [Google Scholar]
- 13.NCHS. 2002 National Health Interview Survey (NHIS): Public use data release. NHIS survey description. 2002 Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2002/srvydesc.pdf.
- 14.NCHS. 2007 National Health Interview Survey (NHIS): Public use data release. NHIS survey description. 2007 Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2007/srvydesc.pdf.
- 15.NCHS. 2012 National Health Interview Survey (NHIS): Public use data release. NHIS survey description. 2012 Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2012/srvydesc.pdf.
- 16.Stussman BJ, Bethell CD, Gray C, Nahin RL. Development of the adult and child complementary medicine questionnaires fielded on the National Health Interview Survey. BMC Complement Altern Med. 2013;13:328. doi: 10.1186/1472-6882-13-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Botman SL, Moore TF, Moriarity CL, Parsons VL. Design and estimation for the National Health Interview Survey, 1995–2004. National Center for Health Statistics. Vital Health Stat. 2000;2(130) Available from: http://www.cdc.gov/nchs/data/series/sr_02/sr02_130.pdf. [Google Scholar]
- 18.Parsons VL, Moriarity CL, Jonas K, et al. Design and estimation for the National Health Interview Survey, 2006–2015. National Center for Health Statistics. Vital Health Stat. 2(165):2014. Available from: http://www.cdc.gov/nchs/data/series/sr_02/sr02_165.pdf. [PubMed] [Google Scholar]
- 19.RTI International. SUDAAN (release 11.0.0) [computer software] 2012 [Google Scholar]
- 20.Day JC. Population projections of the United States by age, sex, race, and Hispanic origin: 1995 to 2050. US Bureau of the Census, Current population reports. :P25–1130. [Google Scholar]
- 21.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected US population Healthy People Statistical Notes, no 20. Hyattsville, MD: National Center for Health Statistics; 2001. [Google Scholar]
- 22.SAS Institute Inc. SAS/STAT (version 9.3) [computer software] 2012. [Google Scholar]
- 23.Kessler RC, Davis RB, Foster DF, et al. Long-term trends in the use of complementary and alternative medical therapies in the United States. Ann Intern Med. 2001;135(4):262–8. doi: 10.7326/0003-4819-135-4-200108210-00011. [DOI] [PubMed] [Google Scholar]
- 24.Frass M, Strassl RP, Friehs H, Müllner M, Kundi M, Kaye AD. Use and acceptance of complementary and alternative medicine among the general population and medical personnel: A systematic review. Ochsner J. 2012;12(1):45–56. [PMC free article] [PubMed] [Google Scholar]
- 25.Harris PE, Cooper KL, Relton C, Thomas KJ. Prevalence of complementary and alternative medicine (CAM) use by the general population: A systematic review and update. Int J Clin Pract. 2012;66(10):924–39. doi: 10.1111/j.1742-1241.2012.02945.x. [DOI] [PubMed] [Google Scholar]
- 26.Quandt SA, Verhoef MJ, Arcury TA, Lewith GT, Steinsbekk A, Kristoffersen AE, et al. Development of an international questionnaire to measure use of complementary and alternative medicine (I–CAM–Q) J Altern Complement Med. 2009;15(4):331–9. doi: 10.1089/acm.2008.0521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moldvay C. IBISWorld Industry report OD4185: Pilates & yoga studios in the US. 2012 [Google Scholar]
- 28.Su D, Li L, Pagán JA. Acculturation and the use of complementary and alternative medicine. Soc Sci Med. 2008;66(2):439–53. doi: 10.1016/j.socscimed.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 29.Gebauer SK, Psota TL, Harris WS, Kris-Etherton PM. n-3 fatty acid dietary recommendations and food sources to achieve essentiality and cardiovascular benefits. Am J Clin Nutr. 2006;83(6 Suppl):S1526S–35S. doi: 10.1093/ajcn/83.6.1526S. [DOI] [PubMed] [Google Scholar]
- 30.USDA. Dietary guidelines for Americans 2010. 2010 Available from: http://www.health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf.
- 31.Fredman G, Serhan CN. Specialized proresolving mediator targets for RvE1 and RvD1 in peripheral blood and mechanisms of resolution. Biochem J. 2011;437(2):185–97. doi: 10.1042/BJ20110327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Serhan CN, Chiang N, Van Dyke TE. Resolving inflammation: Dual anti-inflammatory and pro-resolution lipid mediators. Nat Rev Immunol. 2008;8(5):349–61. doi: 10.1038/nri2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jackson PA, Reay JL, Scholey AB, Kennedy DO. DHA-rich oil modulates the cerebral haemodynamic response to cognitive tasks in healthy young adults: A near IR spectroscopy pilot study. Br J Nutr. 2012;107(8):1093–8. doi: 10.1017/S0007114511004041. [DOI] [PubMed] [Google Scholar]
- 34.Litman BJ, Niu SL, Polozova A, Mitchell DC. The role of docosahexaenoic acid containing phospholipids in modulating G protein-coupled signaling pathways: Visual transduction. J Mol Neurosci. 2001;16(2–3):237–42. doi: 10.1385/JMN:16:2-3:237. [DOI] [PubMed] [Google Scholar]
- 35.Mitchell DC, Niu SL, Litman BJ. Enhancement of G protein-coupled signaling by DHA phospholipids. Lipids. 2003;38(4):437–43. doi: 10.1007/s11745-003-1081-1. [DOI] [PubMed] [Google Scholar]
- 36.Nutrition Business Journal. Supplement Business Report. 2013 [Google Scholar]
- 37.Lindstrom A, Ooyen C, Lynch ME, Bluementhal M. Herb supplement sales increase 5.5% in 2012: Herbal supplement sales rise for 9th consecutive year; turmeric sales jump 40% in natural channel. HerbalGram. 2013;99:60–5. [Google Scholar]
- 38.National Center for Complementary and Alternative Medicine. Expanding horizons of healthcare: Five-year strategic plan 2001–2005. 2000 NIH pub no 01–5001. [Google Scholar]
- 39.National Center for Complementary and Alternative Medicine. Exploring the science of complementary and alternative medicine: Third strategic plan 2011–2015. 2011:D458. NIH pub no 11–7643. [Google Scholar]